Abstract
Background
Traditional ankle-foot orthoses (AFOs) are not effective in treating plantar fasciitis, while customized 3-dimensional (3D) printed ankle-foot orthoses are effective in treating many ankle-foot diseases. This study investigated the effects of customized 3D printed AFOs on biomechanics and comfort of the plantar foot in plantar fasciitis.
Material/Methods
Sixty patients with bilateral plantar fasciitis aged 31–60 years participated in this study. At week 0, patients were randomly assigned into 2 groups: the control group consisting of those wearing separate shoes with prefabricated AFOs; and the experimental group consisting of those wearing a separate shoe and customized 3D-printed AFO. The Footscan® system recorded maximum pressure, maximum strength, and contact area of patients’ hallux, toes 2–5, first to fifth metatarsal, midfoot, lateral heel, and midfoot heel at weeks 0 and 8. Patients used visual analogue scale scores at weeks 0 and 8 to assess overall comfort of foot orthosis, to determine the credibility and comfort of both orthopedic insole conditions.
Results
At week 0, in the experimental group, peak pressure in the hallux and first metatarsal area was significantly higher than the control group (P<0.05), while mid-heel and lateral heel peak pressures were significantly lower than the control group (P<0.05). After 8 weeks, all groups reported more comfort compared with the same group in week 0 (P<0.05). The comfort scores reported by the experimental group were significantly lower than those of the control group (P<0.05).
Conclusions
This study supports the efficiency of customized 3D printing AFO for reducing damage associated with plantar lesions and improving comfort in patients with plantar fasciitis compared with prefabricated AFO. Customized AFO is useful in the treatment of plantar fasciitis compared with prefabricated AFOs.
MeSH Keywords: Fasciitis, Plantar; Foot Orthoses; Imaging, Three-Dimensional; Pain Clinics; Rehabilitation
Background
The ankle-foot orthosis (AFO) is an important component of lower limb orthoses, providing cushioning and support [1–3]. AFOs are designed based on biomechanical principles to reduce stress, relieve pain, correct deformities, and enhance the stability of the foot. They are used to prevent and treat diseases of the feet and lower limbs [4,5]. Studies have shown that orthopedic insoles help prevent and correct knee arthritis as well as lumbar pain and foot deformities, improving gait in patients with lower extremity arthritis and improving walking function [6,7]. Plantar fasciitis (PF) is also called jogger’s heel, tennis foot, and police foot. It is a common foot musculoskeletal disease; PF is caused by aseptic inflammation of the tendon or fascia of the foot [8]. PF leads to reduced daily activities, and patients’ feet often feel hot and painful. Initial treatment of PF includes filling, foot straps, orthopedic insoles, and topical corticosteroid injections [9–11]. If the symptoms persist after 1 year of first-line treatment, surgery is required [12,13]. AFOs are the most common method of rehabilitation for the initial treatment of PF [8,14]. Compared with personalized AFOs, traditional methods of AFO have many deficiencies, including complicated manufacturing processes, long production time, and problems related to patients wearing AFOs. They are prone to causing discomfort, making it difficult for patients to integrate them into use [3,6]. 3D printing technology is essentially a computer-aided design and computer-aided manufacturing process (CAD-CAM). 3D printing technology has the advantages of fast construction and on-demand production that meets the needs of individualized medical treatment [1,7]. 3D printed AFOs have been in the research and experimental stage in recent years, and actual use is primarily based on commercial customization without clinical verification [15]. Based on these preconditions, the aim of the study was to test whether customized 3D printed AFOs might have a better effect on improving comfort and changing foot biomechanics in people with plantar fasciitis compared with conventional prefabricated insoles.
Material and Methods
General information
Seventy-five patients with PF were recruited from the Bethune Second Hospital of Jilin University from January 2018 to October 2018 by random sampling. Informed consent was obtained from all participants. The Ethics Committee of the Second Hospital of Jilin University approved the study. Subsequently, 60 patients (30 females and 30 males) met the inclusion criteria and agreed to participate in the study. Participants were between the ages of 31 and 60 years. The course of disease was 5–10 months (mean ± standard deviation, 20.5±6.4 months). The sample size of 60 participants was chosen because it proved to be large enough to allow parameter statistics during data analysis [4,16–19]. A power calculation was not performed because of the uncertainty surrounding the minimal important difference for plantar pressure changes. Table 1 lists the demographics of the participants. Patients were divided into an experimental group and a control group according to the random number table method. There were no significant differences with respect to age and weight, body mass index (BMI), and AFO wearing time (P>0.05).
Table 1.
Demographics of participants (N=60).
| Characteristics | Experimental group | Control group | ||
|---|---|---|---|---|
| Average (SD) | Range | Average (SD) | Range | |
| Age (years) | 40.31 (5.21) | 31–58 | 42.52 (6.18) | 33–60 |
| Sex | 15 males, 15 females | 15 males, 15 females | ||
| Weight (Kg) | 62.17 (10.52) | 49.42–88.94 | 65.28 (9.72) | 50.92–86.42 |
| BMI (Kg/m2) | 26.56 (12.42) | 15.93–29.74 | 25.71 (10.42) | 17.44–28.33 |
| Wearing time (hours/day) | 6.41 (3.32) | 3.32–9.72 | 5.11 (2.54) | 4.31–8.72 |
SD – standard deviation.
Inclusion and exclusion criteria
The following inclusion/exclusion criteria were used to determine eligibility for enrollment in this clinical trial. Inclusion criteria were: 1) males or females with a diagnosis of PF, 2) aged 31–60 years, and 3) the diagnosis was made upon the finding of tenderness to pressure at the origin of the plantar fascia on the medial tubercle of the calcaneus, as well as complaint of heel pain greater than or equal to 3 on a 1–10 visual analogue scale (VAS). Exclusion criteria were: 1) previous fracture or surgery of the foot, and 2) specific metabolic and connective tissue disorders associated with or contributing to the diagnosis of PF (e.g., rheumatoid arthritis, gout, and lupus).
Study design
This study had a single-blind, randomized, controlled design. Randomization was performed by one independent therapist (TM). The patients were subsequently randomized to either the experimental group (customized AFO-wearing group) or the control group (prefabricated-AFO wearing group). We used a computer-generated table of random numbers which were encrypted and not readable until allocation. One independent research assistant (RX) performed all assessments and data entry. Except for the interview, the assistant worked at another location and did not participate in the treatment, allowing the single-blind treatment allocation to be maintained. Before each measurement, the assistant was asked to confirm a lack of knowledge regarding the treatment allocations. Assessments were performed at baseline and at the end of the 8-week treatment.
Experimental and control groups
All participants wore standardized thin cotton socks and their commonly-used shoes during the test, as well as flat shoes and socks that are uniformly purchased by the hospital 1 month before the experiment. The sole was flat and did not significantly change the original pressure and contact area of the patient’s sole. The control group wore commonly used shoes + traditional pre-made sponge orthopedic insoles (control group). The experimental group wore commonly used shoes + customized vinyl acetate (EVA) orthopedic insoles (experimental group).
Customized foot orthoses were manufactured by the commercial orthosis manufacturer (Bodyarch), using computer-aided design and computer-aided manufacturing (CAD-CAM). The patient’s foot model was first obtained using a 0.5 m2 plantar pressure plate-pressure collection device. The Footscan® 3D gait analysis system (RSscan International, Olen, Belgium) was used to obtain patient gait, the Bodyarch cloud data acquisition system was used to summarize these data, and we used the Bodyarch function insole cloud design system. The 3D AFO was made using the Bodyarch X1 printer, where each orthosis was cast on the front side and the material was polyethylene acetate (EVA). In order to eliminate psychological factors, the control group patients also underwent this procedure; however, we did not make a customized orthosis for them, and the printed orthoses and pre-made orthoses were inserted into the corresponding participants’ shoes, with the participants not knowing the insert status. They were only informed that the purpose of the study was to evaluate the effects of 2 different types of shoe inserts [20] that were considered to have different therapeutic mechanisms. After each test was completed under each insertion condition, participants assessed the overall comfort of their foot orthosis during the test (0=completely uncomfortable, 10=most comfortable). We also evaluated the ease of use and stability of each insole. Participants did not know the measurement results and ratings. After completing each insertion condition, the participants rated the shoes separately. The interval between the shoe insertion conditions was approximately 10 minutes, during which time the participants walked barefoot around the laboratory at a slow pace of their choice. Figure 1 shows a customized ankle orthosis and pre-made ankle orthosis.
Figure 1.

(A) Experimental group: customized ankle orthosis. (B) Control group: pre-made ankle orthosis.
Experimental process
Footscan® 7-gait 2nd generation system (2096×472×18 mm, 16 384 resistance sensors arranged in a 256×64 matrix with a resolution of 2 sensors/cm2) captured the dynamic pressure of the foot data. The system has been shown to accurately test plantar pressure [21,22]. The acquisition frequency was 125 Hz and the pressure range was 0–200 N/cm2; the system was connected to the computer using the supplied cable. The platform was located in the center of the floor to provide a “full platform” of 4 meters [23]. Following the manufacturer’s manual, the Footscan® system was calibrated prior to each measurement. According to a study by Xu et al. [21], in order to obtain more accurate parameters, no walking mat was placed above the flat plate. During calibration, the patient’s weight was entered into the computer and the patient was asked to pass across the plate at a normal rate while barefoot; the software automatically calibrated all parameters. Because the Footscan® system can measure the distribution of foot pressure, the pressure change of the lesion area can be detected, which means that the system can be used as an auxiliary means to measure comfort when wearing AFOs [24–26].
After correction conditions, the plantar pressure data were recorded (i.e., week 0). The participant was told that they were undergoing a foot orthosis test and were not provided additional information. The experimental group and the control group were analyzed in random order to minimize potential errors. Participants were unaware of the conditions tested in the initial data collection. Because it was difficult to conceal the condition of each orthosis, the researchers did not use the blinded method. They inserted the orthopedic insole into the shoe under each test condition, and zeroed the system according to the manufacturer’s instructions before the first walk test. After 2 minutes of acclimatization of standing and walking, the participants completed 3 walks along each 10-m walkway under each condition, and each test involved a stopwatch to control walking speed. If the trial was not within 5% of the original walking time, the trial was repeated to minimize the effect of walking speed on plantar pressure [27]. The average walking speed of all trials was 3.5 km/hour (±3.0 km/hour). Once the initial plantar pressure was collected, orthoses were then provided to the participants so that they could begin to wear them within the next 8 weeks. During the subsequent 8 weeks, participants were instructed to wear each orthosis at the same time. No rehabilitation treatment was carried out between the 8 weeks. After 8 weeks, participants returned for a second data collection of plantar pressure based on the identical data collection protocol used initially. Similar to the initial data collection, participants were unaware of the 8th week of data collection testing specific grouping information.
Visual analogue scale (VAS)
A VAS was used to measure comfort when wearing AFOs [28–30]. VAS is a numerical scale with marked points at 0 and 10, in which 0 indicates no discomfort and 10 indicates the highest level of discomfort. The scale was 10-cm long and was on a single piece of white paper. Patients were requested to rate their comfort based on their initial steps at week 0 and week 8 by putting a vertical mark on the scale representing the level of comfort. The patient was only shown a single scale on each visit to avoid prejudice.
Data analysis
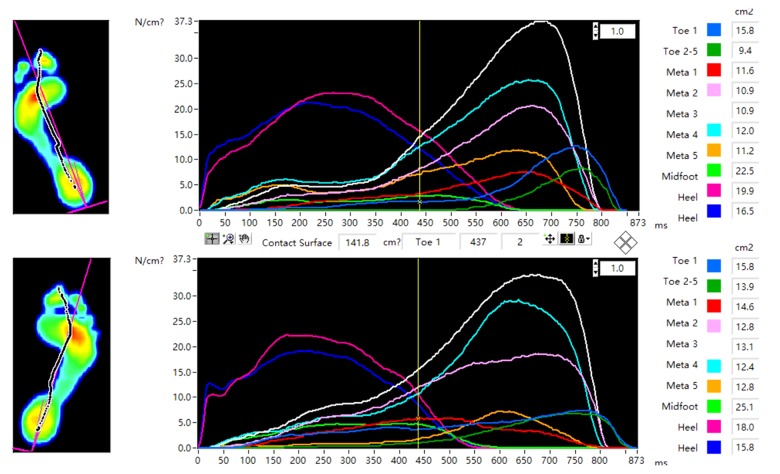
Using the Footscan® system to analyze plantar pressure data, the software automatically divided the foot into 10 coverage areas: the big toe (T1), toes 2–5 (T2–T5), the first to fifth metatarsal (M1, M2, M3, M4, and M5), midfoot (MF), medial heel (H1), and lateral heel (H2) (Figure 2). The primary data collected were peak pressure, contact area, and maximum force at T1, T2–T5, M1, M2, M3, M4, M5, and MF at zero and 8 weeks. Statistical analysis was performed using Social Science Statistics Program (SPSS) 20th Edition (SPSS Inc., Chicago, IL, USA). One-way analysis of variance (ANOVA) was used to compare the mean and significance between test conditions. In order to maintain data independence, only the left foot of each participant was selected for evaluation [31].
Figure 2.
The Footscan® system divides the sole into 10 coverage areas: the hallux (T1), toes 2–5 (T2–T5), the first to fifth metatarsal (M1, M2, M3, M4, and M5), midfoot (MF), medial heel (H1, MH), and lateral heel (H2, LH).
The statistical significance of the test was set to the conventional level of P<0.05. To reduce the effects of body acceleration and deceleration at the beginning and end of the walking test, 5 intermediate steps were selected by the step analysis software of the Footscan® system. VAS scores of the experimental and control groups were collected at weeks 0 and 8 and were compared between groups.
Results
Comfort score
After wearing the AFO at week 0, the VAS of the experimental group was 7.34± 3.43 and the VAS of the control group was 8.72±3.93. There was no significant difference between the experimental group and the control group (P>0.05). After 8 weeks, all participants reported comfort increase. The comfort score reported by the experimental group (3.12± 0.51) was significantly lower than that of the control group (5.25±1.22, P<0.05) (0=most comfortable, 10 = completely uncomfortable).
Biomechanical analysis
The comparison of the experimental group and the control group at week 0 is shown in Table 2. The overall differences were small for peak pressure, peak strength, and contact area of the 10 regions of the experimental group and the control group at week 0. Walking with a customized AFO, the peak pressure of the hallux, and first metatarsal area was much higher than the peak pressure generated when using the prefabricated AFO (P<0.05). In the mid-heel and lateral foot, the peak pressure was much lower in the experimental group than in the control group (P<0.05). In other areas, there were no significant differences between the experimental group and the control group. There were no significant differences between the experimental group and the control group with respect to peak strength or contact area.
Table 2.
Comparison of the experimental group and the control group at week 0.
| Areas | Peak pressure (kPa) | Maximum force (N) | Contact area (cm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CAFO | PCAFO | P | CAFO | PCAFO | P | CAFO | PCAFO | P | |
| T1 | 90.0±19.5 | 59.0±26.1 | 0.012* | 93.0±21.8 | 95.9±44.0 | 0.912 | 10.0±1.3 | 16.4±4.8 | 0.112 |
| T2–T5 | 46.7±19.0 | 31.0±26.8 | 0.532 | 65.2±57.3 | 39.9±52.2 | 0.623 | 12.1±5.8 | 8.1±7.1 | 0.521 |
| M1 | 125.0±51.0 | 34.2±31.3 | 0.041* | 90.7±30.4 | 36.9±40.0 | 0.112 | 7.6±3.5 | 8.1±3.3 | 0.822 |
| M2 | 223.1±38.2 | 316.6±335.6 | 0.623 | 172.0±39.7 | 128.3±108.7 | 0.541 | 7.3±0.5 | 8.1±3.1 | 0.631 |
| M3 | 241.2±78.1 | 350.3±287.5 | 0.421 | 169.0±65.8 | 288.1±271.4 | 0.443 | 6.6±1.0 | 7.5±0.8 | 0.221 |
| M4 | 239.3±93.5 | 296.4±166.1 | 0.643 | 184.2±80.2 | 241.0±140.7 | 0.522 | 7.3±0.9 | 7.9±0.85 | 0.134 |
| M5 | 192.1±95.3 | 152.4±93.2 | 0.623 | 241.2±132.7 | 183.9±96.2 | 0.631 | 12.1±2.4 | 12.2±1.3 | 0.942 |
| MF | 119.2±21.6 | 61.2±67.0 | 0.212 | 396.0±143.0 | 314.2±416.0 | 0.714 | 31.8±8.9 | 42.6±10.8 | 0.221 |
| MH | 119±13.7 | 196±37.6 | 0.042* | 211.1±125.2 | 243.5±75.5 | 0.622 | 14.1±4.5 | 11.8±1.6 | 0.242 |
| LH | 128.2±29.3 | 207.1±47.2 | 0.021* | 220.9±162.8 | 220.2±73.2 | 0.942 | 12.7±4.8 | 10.1±1.4 | 0.232 |
P<0.05 is considered a significant difference; values are expressed as means ± standard deviation;
CAFO – customized AFO; PCAFO – pre-customized AFO; T1 – hallux; T2–T5 – toes 2–5; M1 – first metatarsal; M2 – second metatarsal; M3 – third metatarsal; M4 – fourth metatarsal; M5 – fifth metatarsal; MF – midfoot; MH – medial heel; LH – lateral heel.
The comparison of the experimental group and the control group in the 8th week is shown in Table 3.
Table 3.
Comparison of the experimental and the control groups at week 8.
| Areas | Peak pressure (kPa) | Maximum force (N) | Contact area (cm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CAFO | PCAFO | P | CAFO | PCAFO | P | CAFO | PCAFO | P | |
| T1 | 129.7±24.3 | 165.5±151.4 | 0.611 | 157.0±48.9 | 126.8±48.9 | 0.312 | 11.5±1.3 | 13.2±9.3 | 0.712 |
| T2–T5 | 50.2±8.4 | 62.5±66.1 | 0.725 | 66.2±34.8 | 43.8±38.7 | 0.723 | 12.1±5.2 | 10.7±7.0 | 0.521 |
| M1 | 140.0±0.8 | 176.5±229.7 | 0.754 | 134.5±50.9 | 97.9±19.7 | 0.322 | 9.3±3.7 | 12.6±7.5 | 0.523 |
| M2 | 204.2±29.4 | 282.5±285.9 | 0.623 | 189.2±69.7 | 177.8±62.3 | 0.841 | 8.8±2.2 | 10.7±6.2 | 0.622 |
| M3 | 408.0±454.9 | 287.2±129.8 | 0.632 | 111.1±65.7 | 233.7±133.9 | 0.223 | 7.3±0.7 | 9.5±5.4 | 0.421 |
| M4 | 174.2±8.7 | 160.7±77.2 | 0.742 | 138.0±25.2 | 138.2±111.8 | 0.912 | 7.6±1.4 | 9.3±5.3 | 0.623 |
| M5 | 109.5±30.3 | 72.2±39.5 | 0.232 | 140.0±60.7 | 82.9±84.1 | 0.332 | 11.8±2.9 | 11.8±7.1 | 0.921 |
| MF | 106.7±9.9 | 62.7±41.2 | 0.114 | 334.5±131.4 | 146.8±162.5 | 0.123 | 29.9±10.8 | 27.5±17.5 | 0.834 |
| MH | 229.2±38.5 | 191.0±100.4 | 0.554 | 303.5±71.0 | 218.4±123.8 | 0.412 | 12.4±3.1 | 14.3±8.5 | 0.723 |
| LH | 215.±3.6 | 227.5±140.4 | 0.832 | 258.2±96.6 | 232.4±155.3 | 0.825 | 11.3±2.7 | 13.1±7.7 | 0.742 |
P<0.05 is considered a significant difference; values are expressed as means ± standard deviation;
CAFO – customized AFO; PCAFO – pre-customized AFO; T1 – hallux; T2–T5 – toes 2–5; M1 – first metatarsal; M2 – second metatarsal; M3 – third metatarsal; M4 – fourth metatarsal; M5 – fifth metatarsal; MF – midfoot; MH – medial heel; LH – lateral heel.
The 3 parameters of the experimental and control groups showed no significant differences in all regions.
The comparison between week 0 and week 8 of the control group is shown in Table 4.
Table 4.
Comparison of week 0 and week 8 in the control group.
| Areas | Peak pressure (kPa) | Maximum force (N) | Contact area (cm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0PCAFO | 8PCAFO | P | 0PCAFO | 8PCAFO | P | 0PCAFO | 8PCAFO | P | |
| T1 | 59.5±26.2 | 165.5±151.4 | 0.312 | 95.9±44.0 | 126.8±48.9 | 0.323 | 16.4±4.8 | 13.2±9.3 | 0.612 |
| T2–T5 | 31.0±26.9 | 62.5±66.1 | 0.532 | 39.9±52.2 | 43.8±38.7 | 0.835 | 8.1±7.1 | 10.7±7.0 | 0.553 |
| M1 | 34.7±31.0 | 176.5±229.7 | 0.343 | 36.9±40.0 | 97.9±19.7 | 0.042* | 8.1±3.3 | 12.6±7.5 | 0.223 |
| M2 | 316.7±335.3 | 282.5±285.9 | 0.934 | 128.3±108.7 | 177.8±62.3 | 0.435 | 8.1±3.1 | 10.7±6.2 | 0.543 |
| M3 | 350.0±287.0 | 287.2±129.8 | 0.734 | 288.1±271.4 | 233.7±133.9 | 0.635 | 7.5±0.8 | 9.5±5.4 | 0.523 |
| M4 | 296.2±166.0 | 160.7±77.2 | 0.223 | 241.0±140.7 | 138.2±111.8 | 0.264 | 7.9±0.8 | 9.3±5.3 | 0.643 |
| M5 | 152.2±9.3 | 72.2±39.5 | 0.082 | 183.9±96.2 | 82.9±84.1 | 0.033* | 12.2±1.3 | 11.8±7.14 | 0.923 |
| MF | 61.0±67.4 | 62.7±41.2 | 0.925 | 314.2±416.0 | 146.8±162.5 | 0.234 | 42.6±10.8 | 27.5±17.5 | 0.143 |
| MH | 119.2±13.0 | 191.0±100.4 | 0.263 | 211.0±125.2 | 218.4±123.8 | 0.953 | 14.1±4.5 | 14.3±8.5 | 0.932 |
| LH | 128.0±29.7 | 227.5±140.4 | 0.223 | 220.9±162.8 | 232.4±155.3 | 0.923 | 12.7±4.8 | 13.1±7.7 | 0.934 |
P<0.05 is considered a significant difference; values are expressed as means ± standard deviation;
0PCAFO – week 0 pre-customized AFO; 8PCAFO – week 8 pre-customized AFO; T1 – hallux; T2–T5 – toes 2–5; M1 – first metatarsal; M2 – second metatarsal; M3 – third metatarsal; M4 – fourth metatarsal; M5 – fifth metatarsal; MF – midfoot; MH – medial heel; LH – lateral heel.
At weeks 0 and 8, there were no significant differences in all areas except for the difference in the contact area of the first fifth metatarsal area.
Table 5 displays the experimental group comparison between weeks 0 and 8 in terms of peak pressure. The peak pressure in the big toe area of patients wearing a customized AFO at week 8 was significantly higher than the peak pressure in the corresponding region at week 0 (T1: P=0.02). There were no significant differences between the experimental groups at weeks 0 and 8 in terms of peak strength or contact area.
Table 5.
Comparison of week 0 and week 8 in the experimental group.
| Areas | Peak pressure (kPa) | Maximum force (N) | Contact area (cm2) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0PCAFO | 8PCAFO | P | 0PCAFO | 8PCAFO | P | 0PCAFO | 8PCAFO | P | |
| T1 | 105.7±27.8 | 141.1±34.9 | 0.022* | 131.0±62.6 | 171.4±57.0 | 0.123 | 11.5±2.6 | 11.5±1.0 | 0.964 |
| T2–T5 | 48.1±16.9 | 54.4±19.5 | 0.342 | 65.0±45.7 | 63.4±30.0 | 0.842 | 12.1±4.8 | 11.1±4.2 | 0.432 |
| M1 | 134.0±39.7 | 150.2±15.6 | 0.324 | 118.2±61.0 | 144.1±44.4 | 0.324 | 8.8±4.0 | 9.3±2.9 | 0.635 |
| M2 | 221.2±38.6 | 204.2±38.1 | 0.123 | 196.7±68.7 | 201.8±83.2 | 0.753 | 8.4±1.9 | 9.2±2.2 | 0.232 |
| M3 | 238.2±77.4 | 346.5±336.6 | 0.321 | 187.0±84.6 | 159.3±101.0 | 0.323 | 7.3±1.6 | 7.5±0.9 | 0.553 |
| M4 | 226.0±84.5 | 172.5±34.8 | 0.132 | 183.2±78.1 | 149.2±49.6 | 0.254 | 7.7±1.1 | 8.2±1.6 | 0.072 |
| M5 | 163.1±80.5 | 116.2±55.7 | 0.142 | 190.8±116.8 | 127.2±63.0 | 0.124 | 11.0±2.3 | 10.3±2.9 | 0.133 |
| MF | 111.1±26.7 | 99.7±18.6 | 0.123 | 390.4±150.0 | 360.0±148.5 | 0.253 | 33.1±8.3 | 34.5±12.5 | 0.523 |
| MH | 195.7±27.6 | 220.5±33.5 | 0.143 | 272.0±88.9 | 314.0±90.6 | 0.073 | 13.2±3.3 | 13.8±3.6 | 0.442 |
| LH | 196.2±36.7 | 212.4±32.4 | 0.121 | 234.7±76.6 | 269.1±96.8 | 0.082 | 11.5±3.1 | 12.1±2.9 | 0.343 |
P<0.05 is considered a significant difference; values are expressed as means ± standard deviation;
0CAFO – week 0 customized AFO; 8CAFO – week 8 customized AFO; T1 – hallux; T2–T5 – toes 2–5; M1 – first metatarsal; M2 – second metatarsal; M3 – third metatarsal; M4 – fourth metatarsal; M5 – fifth metatarsal; MF – midfoot; MH – medial heel; LH – lateral heel.
Discussion
The concept of making an AFO
The purpose of the AFO is to support the arch and increase the contact area. In addition to compensating for the drop of the arch, the AFO can also reduce the recoil force when the heel strikes, improving the pressure distribution of the plantar region, and helping to reconstruct external rotation to obtain proper thrust [32]. It has a positive effect on improving comfort and assisting rehabilitation in patients with plantar fasciitis. This study was designed to compare the effects of customized 3D printed AFOs with those of conventional prefabricated insoles on biomechanics and comfort in the plantar foot in patients with plantar fasciitis.
Comparison of biomechanical effects of 2 orthoses on plantar fasciitis in patients with plantar fasciitis
In the midfoot area, there were no significant within-group differences between the experimental group and the control group. This indicates that, for patients with plantar fasciitis, a rehabilitation effect in the mid-foot area occurred regardless of the type of AFO used.
In the heel area, because patients with plantar fasciitis primarily develop heel pain and the heel is the lesion area, the distribution of the heel load has a positive effect on alleviating the pressure and improving the condition of the patient. Compared with the foot orthosis, the customized AFO significantly reduced the heel pressure at time zero; however, the long-term effect was not significantly different from that of the control group, suggesting that the customized AFO can have orthotic effect in a shorter time. However, it requires long-term wear to produce a stable healing effect.
In the metatarsal region, the peak pressure of the first metatarsal was much higher in the experimental group at week 0 than in the control group, suggesting that the customized AFO transfers the load from the forefoot region to the hind foot to improving comfort, while the prefabricated AFO has a slower effect on the transfer load. It has been experimentally demonstrated that foot orthoses can decompress the metatarsal region [33]. Guldemond et al. [34] found that the reason for the reduction of the first metatarsal pressure was the use of a metatarsal pad and the improved height of the arch support; these results indicate that the printed insole is more suitable for actual foot conditions. In this experiment, the lesion of the plantar fasciitis was primarily in the hind foot. By reducing forefoot pressure, the hind foot load can be relieved [9]; in the study of Farzadi et al. [35], the direct effect of the foot orthosis was not significant; however, after using the foot orthosis for 1 month, the pressure and strength were significantly reduced in these areas. We believe that, because the customized AFO is more in line with the actual foot condition of the patient, the correction effect is produced in a short time, and the correction effect is enhanced as time passes.
In the toe area, similar to the metatarsal area, only at week 0 was the peak pressure of the toe area of the experimental group much higher than that of the control group, possibly because of the increased pressure of the toe area caused by the plantar lesion. Simply distributing the load to the toe area through the orthosis does not provide an effective therapeutic effect [36] and needs to be combined with other rehabilitation methods.
Comfort is also a factor affecting the use of the foot orthosis. Uncomfortable orthoses can have a negative impact on lower limb balance control and patient mood [1,31], especially for the elderly [37]. This experiment shows that the comfort of the customized AFO is much higher than the prefabricated AFO, and has a long-term effect, potentially improving the treatment effect.
The results of this study have some limitations. First, this study only covered the comparison of 2 types of foot orthoses, without considering other types of materials [7,16] and the shape of the AFO [38]; second, although Footscan® has been shown to be an effective and reliable plantar pressure system [21,22,31], the technique of measuring the pressure inside the shoe continues to produce errors [39]. For example, when measuring the contact area, the full surface of the foot cannot be fully obtained. Finally, our sample size was not sufficient and there were certain errors.
Conclusions
This study supports the efficiency of customized 3D printing AFO for reducing damage associated with plantar lesions and improving comfort in patients with plantar fasciitis compared with prefabricated AFO.
Footnotes
Source of support: Departmental sources
References
- 1.Cha YH, Lee KH, Ryu HJ, et al. Ankle-foot orthosis made by 3D printing technique and automated design software. Appl Bionics Biomech. 2017;2017 doi: 10.1155/2017/9610468. 9610468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen YC, Lou SZ, Huang CY, Su FC. Effects of foot orthoses on gait patterns of flat feet patients. Clin Biomech (Bristol, Avon) 2010;25:265–70. doi: 10.1016/j.clinbiomech.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Zhai JN, Wang J, Qiu YS. Plantar pressure differences among adults with mild flexible flatfoot, severe flexible flatfoot and normal foot when walking on level surface, walking upstairs and downstairs. J Phys Ther Sci. 2017;29:641–46. doi: 10.1589/jpts.29.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bok SK, Lee H, Kim BO, et al. The effect of different foot orthosis inverted angles on plantar pressure in children with flexible flatfeet. PLoS One. 2016;11:e0159831. doi: 10.1371/journal.pone.0159831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dombroski CE, Balsdon ME, Froats A. The use of a low-cost 3D scanning and printing tool in the manufacture of custom-made foot orthoses: A preliminary study. BMC Res Notes. 2014;7:443. doi: 10.1186/1756-0500-7-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rasenberg N, Riel H, Rathleff MS, et al. Efficacy of foot orthoses for the treatment of plantar heel pain: A systematic review and meta-analysis. Br J Sports Med. 2018;52:1040–46. doi: 10.1136/bjsports-2017-097892. [DOI] [PubMed] [Google Scholar]
- 7.Ligon SC, Liska R, Stampfl J, et al. Polymers for 3D printing and customized additive manufacturing. Chem Rev. 2017;117:10212–90. doi: 10.1021/acs.chemrev.7b00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li L, Yang L, Yu F, et al. 3D printing individualized heel cup for improving the self-reported pain of plantar fasciitis. J Transl Med. 2018;16:167. doi: 10.1186/s12967-018-1547-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bishop C, Thewlis D, Hillier S. Custom foot orthoses improve first-step pain in individuals with unilateral plantar fasciopathy: A pragmatic randomised controlled trial. BMC Musculoskelet Disord. 2018;19:222. doi: 10.1186/s12891-018-2131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beeson P. Plantar fasciopathy: Revisiting the risk factors. Foot Ankle Surg. 2014;20:160–65. doi: 10.1016/j.fas.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Singh P, Madanipour S, Bhamra JS, Gill I. A systematic review and meta-analysis of platelet-rich plasma versus corticosteroid injections for plantar fasciopathy. Int Orthop. 2017;41:1169–81. doi: 10.1007/s00264-017-3470-x. [DOI] [PubMed] [Google Scholar]
- 12.Malliaropoulos N, Crate G, Meke M, et al. Success and recurrence rate after radial extracorporeal shock wave therapy for plantar fasciopathy: A retrospective study. Biomed Res Int. 2016;2016 doi: 10.1155/2016/9415827. 9415827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsikopoulos K, Vasiliadis HS, Mavridis D. Injection therapies for plantar fasciopathy (‘plantar fasciitis’): A systematic review and network meta-analysis of 22 randomised controlled trials. Br J Sports Med. 2016;50:1367–75. doi: 10.1136/bjsports-2015-095437. [DOI] [PubMed] [Google Scholar]
- 14.Rasenberg N, Fuit L, Poppe E, et al. The STAP-study: The (cost) effectiveness of custom-made orthotic insoles in the treatment for plantar fasciopathy in general practice and sports medicine: Design of a randomized controlled trial. BMC Musculoskelet Disord. 2016;17:31. doi: 10.1186/s12891-016-0889-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YC, Lin G, Wang MJ. Comparing 3D foot scanning with conventional measurement methods. J Foot Ankle Res. 2014;7:44. doi: 10.1186/s13047-014-0044-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munteanu SE, Scott LA, Bonanno DR, et al. Effectiveness of customised foot orthoses for Achilles tendinopathy: A randomised controlled trial. Br J Sports Med. 2015;49:989–94. doi: 10.1136/bjsports-2014-093845. [DOI] [PubMed] [Google Scholar]
- 17.Chapman GJ, Halstead J, Redmond AC. Comparability of off the shelf foot orthoses in the redistribution of forces in midfoot osteoarthritis patients. Gait Posture. 2016;49:235–40. doi: 10.1016/j.gaitpost.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee HJ, Lim KB, Yoo J, et al. Effect of custom-molded foot orthoses on foot pain and balance in children with symptomatic flexible flat feet. Ann Rehabil Med. 2015;39:905–13. doi: 10.5535/arm.2015.39.6.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hahni M, Hirschmuller A, Baur H. The effect of foot orthoses with forefoot cushioning or metatarsal pad on forefoot peak plantar pressure in running. J Foot Ankle Res. 2016;9:44. doi: 10.1186/s13047-016-0176-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCormick CJ, Bonanno DR, Landorf KB. The effect of customised and sham foot orthoses on plantar pressures. J Foot Ankle Res. 2013;6:19. doi: 10.1186/1757-1146-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu C, Wen XX, Huang LY, et al. Reliability of the Footscan® platform system in healthy subjects: A comparison of without top-layer and with top-layer protocols. Biomed Res Int. 2017;2017 doi: 10.1155/2017/2708712. 2708712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu C, Wen XX, Huang LY, et al. Normal foot loading parameters and repeatability of the Footscan® platform system. J Foot Ankle Res. 2017;10:30. doi: 10.1186/s13047-017-0209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu C, Yan YB, Zhao X, et al. Pedobarographic analysis following pemberton’s pericapsular osteotomy for unilateral developmental dysplasia of the hip: An observational study. Medicine (Baltimore) 2015;94:e932. doi: 10.1097/MD.0000000000000932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Li B, Hu K, et al. Adding an arch support to a heel lift improves stability and comfort during gait. Gait Posture. 2017;58:94–97. doi: 10.1016/j.gaitpost.2017.07.110. [DOI] [PubMed] [Google Scholar]
- 25.Sinclair J, Hobbs SJ, Taylor PJ, et al. The influence of different force and pressure measuring transducers on lower extremity kinematics measured during running. J Appl Biomech. 2014;30:166–72. doi: 10.1123/jab.2012-0238. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Li B. Influence of in-shoe heel lifts on plantar pressure and center of pressure in the medial-lateral direction during walking. Gait Posture. 2014;39:1012–16. doi: 10.1016/j.gaitpost.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 27.Blasimann A, Eichelberger P, Brulhart Y, et al. Non-surgical treatment of pain associated with posterior tibial tendon dysfunction: Study protocol for a randomised clinical trial. J Foot Ankle Res. 2015;8:37. doi: 10.1186/s13047-015-0095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mills K, Blanch P, Vicenzino B. Influence of contouring and hardness of foot orthoses on ratings of perceived comfort. Med Sci Sports Exerc. 2011;43:1507–12. doi: 10.1249/MSS.0b013e31820e783f. [DOI] [PubMed] [Google Scholar]
- 29.Kristo I, Stift A, Staud C, et al. The type of loose seton for complex anal fistula is essential to improve perianal comfort and quality of life. Colorectal Dis. 2016;18:O194–98. doi: 10.1111/codi.13335. [DOI] [PubMed] [Google Scholar]
- 30.Lindorfer J, Kroll J, Schwameder H. Comfort assessment of running footwear: Does assessment type affect inter-session reliability? Eur J Sport Sci. 2019;19:177–85. doi: 10.1080/17461391.2018.1502358. [DOI] [PubMed] [Google Scholar]
- 31.Zammit GV, Menz HB, Munteanu SE. Reliability of the TekScan MatScan® system for the measurement of plantar forces and pressures during barefoot level walking in healthy adults. J Foot Ankle Res. 2010;3:11. doi: 10.1186/1757-1146-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khodaei B, Saeedi H, Jalali M, et al. Comparison of plantar pressure distribution in CAD-CAM and prefabricated foot orthoses in patients with flexible flatfeet. Foot (Edinb) 2017;33:76–80. doi: 10.1016/j.foot.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Umehara J, Ikezoe T, Nishishita S, et al. Effect of hip and knee position on tensor fasciae latae elongation during stretching: An ultrasonic shear wave elastography study. Clin Biomech (Bristol, Avon) 2015;30:1056–59. doi: 10.1016/j.clinbiomech.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 34.Guldemond NA, Leffers P, Schaper NC, et al. The effects of insole configurations on forefoot plantar pressure and walking convenience in diabetic patients with neuropathic feet. Clin Biomech (Bristol, Avon) 2007;22:81–87. doi: 10.1016/j.clinbiomech.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 35.Kitaoka HB, Luo ZP, Kura H, An KN. Effect of foot orthoses on 3-dimensional kinematics of flatfoot: A cadaveric study. Arch Phys Med Rehabil. 2002;83:876–79. doi: 10.1053/apmr.2002.32681. [DOI] [PubMed] [Google Scholar]
- 36.Whittaker GA, Munteanu SE, Menz HB, et al. Corticosteroid injections compared to foot orthoses for plantar heel pain: protocol for the SOOTHE heel pain randomised trial. Contemp Clin Trials Commun. 2017;5:1–11. doi: 10.1016/j.conctc.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sidon E, Shemesh S, Rosenthal Y, et al. Medial forefoot fillet flap for primary closure of transmetatarsal amputation: A series of four cases. Foot (Edinb) 2017;33:53–56. doi: 10.1016/j.foot.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 38.Luo XD, Xue CH, Li Y. Study on the foot shape characteristics of the elderly in China. Foot (Edinb) 2017;33:68–75. doi: 10.1016/j.foot.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 39.Dessery Y, Belzile E, Turmel S, Corbeil P. Effects of foot orthoses with medial arch support and lateral wedge on knee adduction moment in patients with medial knee osteoarthritis. Prosthet Orthot Int. 2017;41:356–63. doi: 10.1177/0309364616661254. [DOI] [PubMed] [Google Scholar]