Abstract
Over the past decade, hip arthroscopy has become increasingly popular in managing hip conditions in a minimally invasive approach. The development of specialist equipment and training in this field has allowed indications for hip arthroscopy to be extended to a range of conditions. However, the need for special equipment and training has also limited the use of hip arthroscopy to specialized centers. This article will outline the evolution of hip arthroscopy, the pathology of hip conditions, what it has been used for and how this technique has now been extended to help manage these conditions in a minimally invasive approach, limiting the complications of open surgery.
Keywords: Arthroscopy, femoroacetabular impingement, hip arthroscopy
Introduction
With the increasing evidence that the acetabular labrum could be the source of hip pain in otherwise normal looking radiographs, surgeons revisited hip arthroscopy after the technique was described and laid to rest in the early 1990s. With improved surgical techniques and better understanding of hip pathologies, more surgeons started performing hip arthroscopic procedures for both diagnostic and therapeutic purposes. Femoroacetabular impingement (FAI) remains the most common indication for therapeutic hip arthroscopy, while, over the years, more indications which are outlined in this article, have emerged.
Hip Arthroscopy – How is it Performed?
Pathology of the hip can be largely divided into three distinct regional groups: The central articular, peripheral articular, and the periarticular components. The procedure can be performed either in a lateral or supine position.1,2
In the supine position, the patient is positioned on a traction table with the perineum against a well-padded vertical post and the feet secured in padded boots. In the lateral position (senior author's preferred position), the patient is positioned on a radiolucent table in a lateral decubitus position, with a horizontal perineal post [Figure 1]. Controlled traction is applied to the operative leg and continued under fluoroscopy until approximately 8 mm–10 mm of hip joint distraction is obtained. The amount of traction required is recorded, and the traction is reduced, while the operative field is prepared. Traction is re-applied before establishing arthroscopy portals. This technique reduces the traction time and decreases the risk of nerve injuries secondary to a prolonged traction time.3
Figure 1.

Lateral position for hip arthroscopy
Portal Placement
Several different portals have been described which can be used in both the supine and lateral position. In general, the position of portals is slightly more posterior in the lateral position. A safe triangle for portal placement has been described.1
Anterolateral portal – usually approximately 2 cm proximal and anterior to the tip of the greater trochanter, angled slightly anteriorly. The needle is aimed to penetrate the capsule at 12 o’clock position (superior) through the joint capsule, avoiding the labrum and aimed toward the cotyloid fossa. The camera is inserted through this portal.
Anterior portal – the arthroscopic needle is introduced about four finger breaths medial to the anterolateral portal forming an angle of about 45°–60° to it. The capsular penetration is done under direct visualization, with the camera aiming at a narrow gap between the femoral head and labrum anteriorly.
Proximal Anterolateral Portal – popularized by Dienst et al.,4 this portal allows access to both the peripheral and central compartment. A skin incision is performed 1/3 the distance between the anterior superior iliac spine and the tip of the greater trochanter. The needle is then directed onto the neck under image guidance. A nitinol guidewire is then introduced until it hits the medial capsule.
Distal anterolateral portal – This portal is useful to work on the lateral and anterolateral neck.
The proximal and distal anterolateral portals can be used for the treatment of lesions at the head-neck junction within the peripheral compartment. A few less frequently used other portals have been described. The most common combination of portals used is the anterolateral and anterior portals.5
A capsulotomy can be performed to facilitate the movement of the camera and arthroscopic instruments. The capsulotomy is ideally performed under direct vision6 using either a Beaver blade, banana knife, or a radiofrequency probe. Care should be taken to perform a limited capsulotomy rather than a capsulectomy as complications related to an extensive capsulectomy have been reported.3,7
Femoroacetabular Impingement
Ever since the initial work of Murray and his team in 1964,8 FAI has been attributed to the possible early onset of osteoarthritis (OA). Harris9 and Solomon10 revisited the theory of FAI and the relationship of OA, but it was not until Ganz et al.11 and his technique of surgical hip dislocation was developed that this theory gained significant credibility.
The theory of FAI, as proposed by Ganz et al.,11 postulates that certain anomalous morphological features of the hip will lead to abnormal contact between the proximal femur and the acetabular rim during the end range of hip movements. The acetabular labrum is present at the acetabular rim and has a seamless continuity with the hyaline cartilage on the articular side. FAI results in repetitive abnormal contact to the labrum and the adjacent hyaline cartilage resulting in damage. These early labral and chondral lesions result in progression of chondral damage leading to early OA unless this abnormal contact is halted.
Ganz et al.12 described three different types of FAI. A CAM impingement lesion is a bone prominence at the femoral head-neck junction, often seen in the anterolateral aspect, due to the reduction or absence of a waist in this area, thereby locally increasing the radius of the femoral head causing it to jam into the acetabular rim at the end of hip motion, especially internal rotation in flexion.12,13 These morphological changes have been termed pistol grip14 or tilt deformity.8 This leads to shear forces on the hyaline cartilage leading to avulsion of the cartilage at the chondrolabral junction.15 This eventually results in tearing of the labrum at the affected area.
Pincer impingement describes the overhang of the acetabular rim resulting in “deepening” of the acetabulum and decreasing the arc of motion before the femoral neck meets the acetabular rim. This is usually due to an abnormality in the development of the whole acetabulum (coxa profunda) or local anterior over-coverage (acetabular retroversion). In this situation, the labrum is squashed between the acetabular rim and the femoral neck during the end range of motion, resulting in degeneration of the labrum. Degeneration takes place either by cyst formation or by ossification of the rim, leading to additional deepening of the acetabulum. The repetitive injury to the labrum leads to adjacent chondral damage.
There is a distinct difference in the severity of chondral damage between pincer and cam impingement. The chondral damage is usually less significant and more benign in the cam type. It is important to note that if the pincer effect is significant, “contra-coup” lesions may be present in the posterior aspect of the acetabular hyaline cartilage. In a study by Beck et al.,15 this contra-coup lesion was observed in the femoral head in 62% and in the posteroinferior acetabulum in 31%.
These two different types of impingement rarely occur in isolation and most of the time the damage is a combination of both mechanisms.15
There is now good histological evidence that the hyaline cartilage degeneration at the site of impingement has the same molecular changes as those seen in advanced OA.16,17 Advances in arthroscopic techniques, mainly the intraoperative dynamic assessment of the hip joint, have allowed surgeons to manage FAI with a less invasive procedure than surgical hip dislocation.
Central Compartment
This compartment is easily visualized while the hip is distracted [Figure 2]. A diagnostic round is first performed, looking at the acetabular and femoral head cartilage in a systematic manner. Any signs of hyaline cartilage damage including blistering, wave sign, chondrolabral detachment, and cartilage defects should be identified. The labrum should be visualized and probed in its entirety looking for labral tears, and more importantly labral detachments at the chondrolabral junction. The ligamentum teres is then visualized and examined under direct vision in internal and external rotation of the hip to assess for instability, detachment, and tears.18 Once the central compartment is treated, the hip traction is released and the traction time documented.
Figure 2.
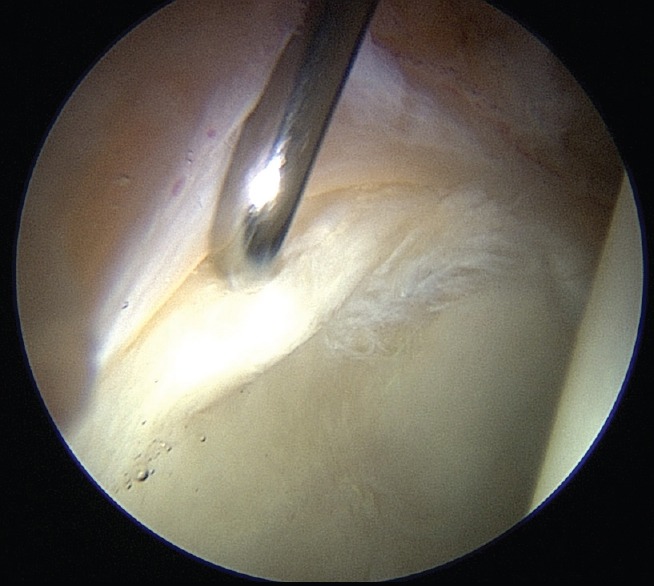
Central compartment with labral tear at the chondrolabral junction
Peripheral Compartment
The peripheral compartment allows the surgeon to visualize the anterior head-neck junction where most cam lesions are present. To visualize the lesion, the hip is flexed to about 45° and a further capsulotomy may need to be performed to improve its access as needed. A T capsulotomy with the distal limb going along the neck has been described.5 Other options include utilizing a different portal to visualize the cam such as a Dienst portal.4 This portal allows visualization of the neck directly from the proximal end of the hip. The anterior portal can then be used to create a more distal track onto the neck and utilize it as the working portal. The camera can be swapped if the surgeon wants to visualize the neck from the distal end. This setup allows the surgeon to visualize the cam up to the medial synovial fold which is the most medial aspect of the neck.
Following the portals placement and limited capsulotomy, the hip joint is maneuvered into external rotation and flexion, as required, to bring the cam lesion into the capsulotomy and field of vision [Figure 3]. Dynamic assessment is then performed throughout the range of motion for detailed mapping of the cam lesion. The cam lesion is visualized and identified by its convex appearance, color (purple/gray), and chondral texture.6
Figure 3.
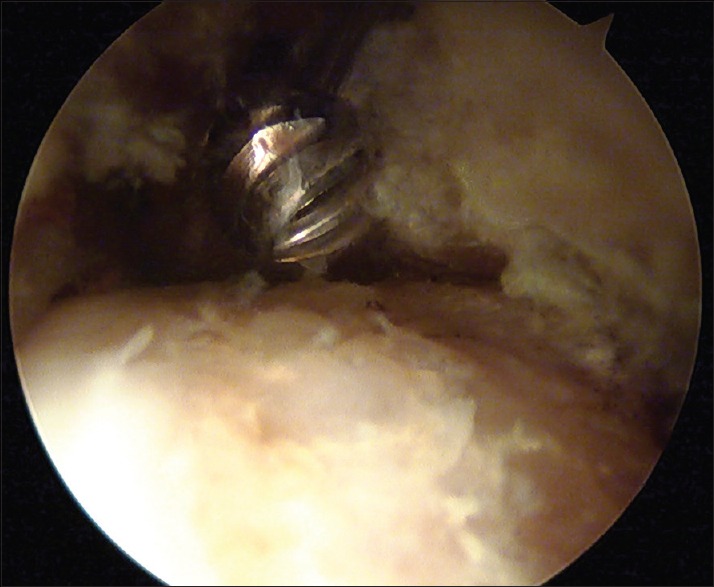
Cam lesion within peripheral compartment
The cam resection is performed inferior and medially (6-o’clock) to superior at (12-o’clock) and distally to the zona orbicularis. The mapped head-neck junction is stripped off the fibrous cartilage, and the bone is excised, using a burr, changing the area from a convex to a concave surface. The depth of the cam is predetermined preoperatively. It is usually 5 mm–7 mm deep and the burr diameter can be used as guidance. Clearance of the resection can then be assessed under direct vision by periodic dynamic assessment [Figure 4].
Figure 4.
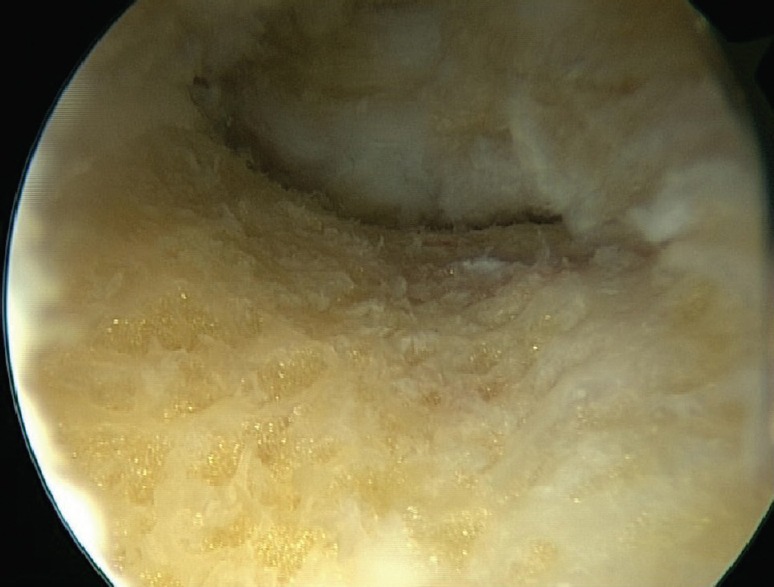
Cam excision and dynamic assessment of impingement
Pincer Impingement Treatment
There are two aspects of pincer impingement [Figure 5a and b] which require surgical management; (1) labral damage and (2) acetabular bony overhang. A periacetabular synovectomy is usually required to visualize the acetabular overhang. The technique of resection initially involves detaching the labrum, excising the bony overhang, and re-attaching the labrum.19 The labrum should be repaired using bioabsorbable anchors with polyester sutures. These are placed 2 mm off the acetabular rim and the stability of the labrum reassessed.6
Figure 5.
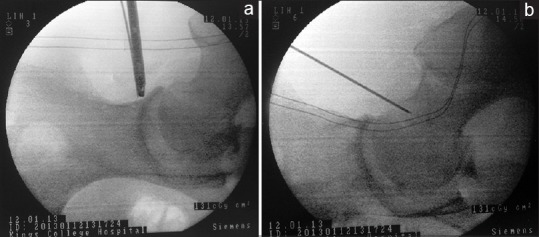
Pincer impingement before (a) and after (b) resection
Labral detachment is not always necessary to treat the pincer deformity. Small pincer resection can be achieved with the labrum still intact. Rim trimming is performed using a burr removing about 3 mm–5 mm of rim. The labrum is then attached to the new resected margin using anchor sutures without the need of detaching the labrum. In some patients with small pincer lesions and an intact, healthy labrum, cam excision may be sufficient to relieve the impingement.6
Hyaline Cartilage Treatment
Hyaline cartilage damage can be managed in multiple ways. However, extensive hyaline cartilage damage carries unfavorable prognosis.20,21,22 Murphy et al.21 showed that advanced OA with joint space narrowing is a relative contraindication for surgical correction of FAI. Skendzel et al.22 reported a prospective study looking at joint space on preoperative radiographs and outcome following hip arthroscopy. This showed that 86% of patients with a joint space of ≤2 mm converted to a THA within 5 years.
Microfracture
Hyaline cartilage damage can be present on both the acetabulum and femoral head. Nearly 90% of acetabular hyaline cartilage damage occurs in the anterosuperior region. Outerbridge Grade 2 and 3 lesions are treated with partial debridement and thermal shrinkage. Grade 4 lesions with full-thickness defects and unstable cartilage flaps overlying subchondral bone are treated with flap excision and microfracture. In this technique, the cartilage lesion is prepared with a curette to achieve a stable cartilage around the defect. Multiple holes are then created using a small diameter awl23 3 mm–4 mm apart. The aim is to allow bone marrow cells and growth factors into the chondral defect. Pluripotent cells from bone marrow will form fibrocartilage which fills the defect.
The results of microfracture have been reported in the following papers. Byrd and Jones24 reported a series of 207 patients who had arthroscopic management of FAI. Fifty-eight hips had microfracture for the management of Grade 4 chondral defects with an intact subchondral plate and healthy surrounding cartilage. They showed an improvement in the Modified Harris Hip Score (MHHS) from 65 preoperatively to 85 at a 2-year followup. Karthikeyan et al.25 reported a series of twenty patients with FAI and acetabular chondral defects who underwent hip arthroscopy and microfracture followed by a second-look arthroscopy. None of the patients had developed diffuse OA. The mean-percent fill was 91%, with good-quality cartilage. The mean percent fill at second-look arthroscopy was 93% ± 17%, with good-quality cartilage macroscopically. The Nonarthritic Hip Score was 55 points before the initial procedure and 54 points before second-look arthroscopy. After the second arthroscopy, the score improved to 78 points at a mean followup of 21 months. These promising results have been achieved in patients who have minimal or no evidence of OA. Reports of microfracture in patients with advanced OA are less promising.20
Autologous Chondrocyte Implantation
The technique of autologous chondrocyte implantation (ACI) has been successfully performed in the knee. However, ACI is more challenging in the hip joint as a surgical hip dislocation will need to be performed. The development of collagen scaffolds to retain the cultivated chondrocytes has enabled the chondrocyte implantation to be performed arthroscopically. This procedure of matrix-assisted chondrocyte implantation (MACI) is being used in Europe with promising results.26 Another technique of autologous matrix-induced chondrogenesis (AMIC)27 combines the pluripotent stem cells present after microfracture together with injection of a collagen Type 1 and 3 matrix into the defect after microfracture to stabilized the chondrogenic blood clot. The added benefit of this procedure is that this can be performed as a single stage. Mancini and Fontana28 reported a 5-year followup in patients undergoing MACI and AMIC. Significant improvement was observed in the MHHS after 6 months and continued to have a positive result up to 3 years at which the scores remained the same up to the 5-year followup. There was no significant difference between the two treatment regimens.
Repair of the Articular Cartilage
Delamination of the articular cartilage is commonly associated with FAI. This involves a full-thickness separation of the cartilage from the subchondral bone. If the defect is small, this can be debrided to the subchondral bone and microfracture performed. However, management of large defects can be challenging. Some authors have successfully been able to salvage macroscopically healthy cartilage by reattaching the cartilage flap to the subchondral bone using suture29 or fibrin glue.30,31 Stafford et al.30 reported the 1–3-year results for using fibrin glue to re-attach large cartilage flaps in 43 patients. The mid-term MHHS for pain showed a statistically significant improvement at a mean of 28 months postoperatively. More similar studies need to be performed to ascertain the long term benefit of this procedure.
Labral Management
Any surgical intervention on the hip joint should aim to achieve a seal between the labrum and the femoral head as this emerging concept has been identified as an essential component for proper hip function.32 Loss of the hydrostatic pressure within the hip joint leads to an abnormal load distribution and microinstability leading to damage to cartilage. A biomechanical study showed that the labral reconstruction or reattachment restores the intraarticular pressure to the intact state.32
Labral tears without detachment can be treated with a radiofrequency probe ablation of the unstable part. In the presence of detachment and if the labral tissue is of good quality and repairable, then every attempt is made to reattach and obtain a secure seal.
Any bone deformity should be corrected using a burr to create a base for the labral re-attachment. Sutures anchors are then placed on the rim about 2 mm away from the cartilage surface. The sutures are looped around or pierced through the labrum to secure to the acetabulum. Philippon et al.32 suggest that if the labrum is deficient and the seal is not restored, then augmentation with the adjacent iliotibial band should be performed. It involves placing a graft on top of the remaining labral tissue and a suture around both the native tissue and the graft.
When the labrum is irreparable or has been excised in previous procedures, then labral reconstruction is advised. Different types of grafts have been advocated including iliotibial band, semitendinosus, gracilis, tibialis anterior, and human acetabular labrum. All these tissues show similar cyclic elongation behavior in response to simulated physiological forces, but their response is varied.33 Early results (mean follow time of 41 months) have been reported in a case series by Boykin et al.34 which suggest that labral reconstruction using iliotibial graft in a group of 21 elite athletes have shown promising good results with an improvement in the MHHS from 67 preoperatively to 84 postoperatively. Mid-term results published by Geyer35 also revealed satisfactory results. The author also concluded that a joint space narrowing of <2 mm is a contraindication for labral reconstruction.35
Capsule Management
The joint capsule is intimately related to four confluent ligaments (pubofemoral, iliofemoral, ischiofemoral, and zona orbicularis) which together with other periarticular soft-tissue stabilizers (labrum, transverse acetabular ligament, pulvinar, ligamentum teres, and iliocapsularis muscle) provide a static constraint to the hip joint. Hip arthroscopy routinely uses capsulotomy or capsulectomy to visualize and treat the underlying pathology. As opposed to the open surgical hip dislocation where a Z capsulotomy is repaired at the end of the procedure, the capsule is normally left open during hip arthroscopy. Some studies have also suggested that a capsulotomy will also prevent postoperative hip stiffness.6
With the resurgence of understanding on microinstability posthip arthroscopy, the interest in capsular repair and the results from such has increased. In a systematic review, Domb et al.7 reviewed the evidence available for capsulotomy and capsulectomy with or without closure and capsular plication. They concluded that biomechanical data strongly favor maintaining or repairing the capsule to an intact state to normalize the hip kinematics and reduce the risk of microinstability. It is, therefore, advisable that capsular repair (partially or fully) should be routinely considered in all patients except the ones who have a stiff hip preoperatively. Capsular plication or capsulorrhaphy can be performed if the capsule is lax. Capsular reconstruction has also been reported36 using iliotibial graft and the short-term results are promising.
Ligamentum Teres
There is growing evidence that the ligamentum teres is the cause of hip pain in a third of athletes with hip pain.37 Hip arthroscopy has been key to diagnose ligamentum teres problems with some papers quoting between 4% and 15% of pathology.37,38
The growing knowledge about the function of the ligamentum teres and its significance in hip pain is still developing. The structure can be easily visualized within the central compartment and tears and avulsions can be diagnosed. Tears or partial ruptures can be treated either by debridement or thermal shrinkage. However, complete rupture is amenable for reconstruction.39 This is performed using iliotibial graft,39 semimembranosus tendon,40 tibialis anterior allograft,41 or ligament augmentation and reconstruction system.42 However, this procedure is being performed in specialized centers and has a steep learning curve.
In a systematic review looking at the indication, surgical options, and outcomes of ligamentum teres injuries, de Sa et al.43 concluded that ligamentum teres debridement is indicated for short term relief of hip pain caused by partial-thickness tears (Type 2) failing conservative management. Reconstruction with autografts, allografts, or synthetic grafts may be indicated for Type 1 (full-thickness) ligamentum teres tears that cause instability, have failed previous debridement, or a combination of these factors.
Hip Arthroscopy in Trauma
In the setting of hip trauma, hip arthroscopy can be used for both diagnostic and therapeutic purposes. Khanna et al.,44 concluded that plain X-rays and computed tomography scans appear to underestimate the true incidence of loose bodies and step deformities within the joint when compared with hip arthroscopy after a traumatic injury of the hip.
The open surgical management of cases such as femoral head fractures, acetabular fractures, and hip dislocation is associated with a degree of complications leading to significant morbidity. Hip arthroscopy reduces such complications and can be an adjunct in managing these conditions.
Niroopan et al.45 investigated the clinical indications, management, and outcomes of hip arthroscopy in trauma. Six indications have been identified in this systemic review: (1) Bullet extraction (2) Removal of intraarticular loose bodies (3) Femoral head fracture fixation (4) Arthroscopic-assisted or all-arthroscopic acetabular fracture fixation (5) Treatment of labral pathology (6) Debridement of a ligamentum teres avulsion.
The study45 also shows a 96% success rate with limited risks. However, one major risk reported is abdominal compartment syndrome secondary to fluid extravasation since the integrity of anatomic compartments is compromised. High-pressure irrigation system in a trauma setting should, therefore, be used cautiously.
Hip Arthroscopy in Arthroplasty
Evaluation of the painful hip replacement can be a diagnostic and therapeutic challenge, more so when investigations to rule out infection and/or loosening are negative. The use of hip arthroscopy in this setting is becoming increasingly helpful to manage these cases. In a case report by Khanduja and Villar,46 hip arthroscopy was useful to confirm the diagnosis of a loose acetabular component in a patient with a previous hip resurfacing. Other authors have reported on the use of hip arthroscopy to remove extra cement after total hip replacement47 and to assess wear and remove wear debris.48 Arthroscopic iliopsoas tenotomy in patients with a painful total hip replacement has also been reported.49
Hip Arthroscopy and Infection
The gold standard management for septic arthritis of the hip remains open arthrotomy and washout of the joint. However, the complications including avascular necrosis of the femoral head and postoperative hip stiffness can cause significant morbidity. Proponents of the use of hip arthroscopy in this setting argue that patients may benefit from this minimally invasive procedure. In a systemic review looking at the indications for arthroscopic hip washout and its complications and outcomes, de Sa et al.(53)50 conclude that there are no specific indications on when to perform an arthroscopic washout. The outcome of clearing the infection is similar in both open and arthroscopic arthrotomy and washout. However, hip arthroscopy will have the least amount of rehab time and the least complications. Currently, no long term followup published evidence exists to suggest that arthroscopic management of septic hip has a better outcome than open arthrotomy and more research is required.
Conclusion
The indications of hip arthroscopy have become increasingly wide over the past decades. Complications from a less invasive procedure, when compared to open surgical management, have made hip arthroscopy the preferred approach in managing this cohort of patients. As the indications expand and new techniques emerge, long term outcomes and benefits of these novel surgical techniques should be reported and published.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Byrd JW, Pappas JN, Pedley MJ. Hip arthroscopy: An anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–23. doi: 10.1016/0749-8063(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 2.Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy. 1987;3:4–12. doi: 10.1016/s0749-8063(87)80003-8. [DOI] [PubMed] [Google Scholar]
- 3.Simpson J, Sadri H, Villar R. Hip arthroscopy technique and complications. Orthop Traumatol Surg Res. 2010;96:S68–76. doi: 10.1016/j.otsr.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Dienst M, Seil R, Kohn DM. Safe arthroscopic access to the central compartment of the hip. Arthroscopy. 2005;21:1510–4. doi: 10.1016/j.arthro.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Ekhtiari S, de Sa D, Haldane CE, Simunovic N, Larson CM, Safran MR, et al. Hip arthroscopic capsulotomy techniques and capsular management strategies: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:9–23. doi: 10.1007/s00167-016-4411-8. [DOI] [PubMed] [Google Scholar]
- 6.Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M, et al. Arthroscopic management of femoroacetabular impingement: Osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–80. doi: 10.1177/0363546507300258. [DOI] [PubMed] [Google Scholar]
- 7.Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–73. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 8.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–24. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 9.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 10.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–83. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 11.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–24. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 13.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–6. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 14.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–72. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–8. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 16.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, et al. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–18. doi: 10.1016/s1063-4584(03)00075-x. [DOI] [PubMed] [Google Scholar]
- 17.Chinzei N, Hashimoto S, Fujishiro T, Hayashi S, Kanzaki N, Uchida S, et al. Inflammation and degeneration in cartilage samples from patients with femoroacetabular impingement. J Bone Joint Surg Am. 2016;98:135–41. doi: 10.2106/JBJS.O.00443. [DOI] [PubMed] [Google Scholar]
- 18.Bardakos NV, Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg Br. 2009;91B:8–15. doi: 10.1302/0301-620X.91B1.21421. [DOI] [PubMed] [Google Scholar]
- 19.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005;21:1496–504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010;26:623–9. doi: 10.1016/j.arthro.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: Indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–81. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 22.Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med. 2014;42:1127–33. doi: 10.1177/0363546514526357. [DOI] [PubMed] [Google Scholar]
- 23.Orth P, Duffner J, Zurakowski D, Cucchiarini M, Madry H. Small-diameter awls improve articular cartilage repair after microfracture treatment in a translational animal model. Am J Sports Med. 2016;44:209–19. doi: 10.1177/0363546515610507. [DOI] [PubMed] [Google Scholar]
- 24.Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739–46. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karthikeyan S, Roberts S, Griffin D. Microfracture for acetabular chondral defects in patients with femoroacetabular impingement: Results at second-look arthroscopic surgery. Am J Sports Med. 2012;40:2725–30. doi: 10.1177/0363546512465400. [DOI] [PubMed] [Google Scholar]
- 26.Fontana A, Bistolfi A, Crova M, Rosso F, Massazza G. Arthroscopic treatment of hip chondral defects: Autologous chondrocyte transplantation versus simple debridement – A pilot study. Arthroscopy. 2012;28:322–9. doi: 10.1016/j.arthro.2011.08.304. [DOI] [PubMed] [Google Scholar]
- 27.Fontana A. Autologous membrane induced chondrogenesis (AMIC) for the treatment of acetabular chondral defect. Muscles Ligaments Tendons J. 2016;6:367–71. doi: 10.11138/mltj/2016.6.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mancini D, Fontana A. Five-year results of arthroscopic techniques for the treatment of acetabular chondral lesions in femoroacetabular impingement. Int Orthop. 2014;38:2057–64. doi: 10.1007/s00264-014-2403-1. [DOI] [PubMed] [Google Scholar]
- 29.Sekiya JK, Martin RL, Lesniak BP. Arthroscopic repair of delaminated acetabular articular cartilage in femoroacetabular impingement. Orthopedics. 2009;32:9. doi: 10.3928/01477447-20090728-44. [DOI] [PubMed] [Google Scholar]
- 30.Stafford GH, Bunn JR, Villar RN. Arthroscopic repair of delaminated acetabular articular cartilage using fibrin adhesive. Results at one to three years. Hip Int. 2011;21:744–50. doi: 10.5301/HIP.2011.8843. [DOI] [PubMed] [Google Scholar]
- 31.Tzaveas AP, Villar RN. Arthroscopic repair of acetabular chondral delamination with fibrin adhesive. Hip Int. 2010;20:115–9. doi: 10.1177/112070001002000117. [DOI] [PubMed] [Google Scholar]
- 32.Philippon MJ, Nepple JJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, et al. The hip fluid seal–Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22:722–9. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 33.Ferro FP, Philippon MJ, Rasmussen MT, Smith SD, LaPrade RF, Wijdicks CA, et al. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med. 2015;43:1222–7. doi: 10.1177/0363546514568086. [DOI] [PubMed] [Google Scholar]
- 34.Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41:2296–301. doi: 10.1177/0363546513498058. [DOI] [PubMed] [Google Scholar]
- 35.Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: Outcome and survivorship analysis at minimum 3-year followup. Am J Sports Med. 2013;41:1750–6. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 36.Trindade CA, Sawyer GA, Fukui K, Briggs KK, Philippon MJ. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4:e71–4. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Byrd JW, Jones KS. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385–91. doi: 10.1016/j.arthro.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 38.Rao J, Zhou YX, Villar RN. Injury to the ligamentum teres.Mechanism, findings, and results of treatment. Clin Sports Med. 2001;20:791–9, vii. doi: 10.1016/s0278-5919(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 39.Philippon MJ, Pennock A, Gaskill TR. Arthroscopic reconstruction of the ligamentum teres: Technique and early outcomes. J Bone Joint Surg Br. 2012;94:1494–8. doi: 10.1302/0301-620X.94B11.28576. [DOI] [PubMed] [Google Scholar]
- 40.Amenabar T, O’Donnell J. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: Surgical technique and an unusual outcome. Arthrosc Tech. 2012;1:e169–74. doi: 10.1016/j.eats.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Menge TJ, Mitchell JJ, Briggs KK, Philippon MJ. Anatomic arthroscopic ligamentum teres reconstruction for hip instability. Arthrosc Tech. 2016;5:e737–42. doi: 10.1016/j.eats.2016.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simpson JM, Field RE, Villar RN. Arthroscopic reconstruction of the ligamentum teres. Arthroscopy. 2011;27:436–41. doi: 10.1016/j.arthro.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 43.de Sa, Phillips M, Philippon MJ, Letkemann S, Simunovic N, Ayeni OR, et al. Ligamentum teres injuries of the hip: A systematic review examining surgical indications, treatment options, and outcomes. Arthroscopy. 2014;30:1634–41. doi: 10.1016/j.arthro.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 44.Khanna V, Harris A, Farrokhyar F, Choudur HN, Wong IH. Hip arthroscopy: Prevalence of intraarticular pathologic findings after traumatic injury of the hip. Arthroscopy. 2014;30:299–304. doi: 10.1016/j.arthro.2013.11.027. [DOI] [PubMed] [Google Scholar]
- 45.Niroopan G, de Sa D, MacDonald A, Burrow S, Larson CM, Ayeni OR, et al. Hip arthroscopy in trauma: A Systematic review of indications, efficacy, and complications. Arthroscopy. 2016;32:692–7030. doi: 10.1016/j.arthro.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 46.Khanduja V, Villar RN. The role of arthroscopy in resurfacing arthroplasty of the hip. Arthroscopy. 2008;24:3. doi: 10.1016/j.arthro.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 47.Mah ET, Bradley CM. Arthroscopic removal of acrylic cement from unreduced hip prosthesis. Aust N Z J Surg. 1992;62:508–10. doi: 10.1111/j.1445-2197.1992.tb07241.x. [DOI] [PubMed] [Google Scholar]
- 48.Fontana A, Zecca M, Sala C. Arthroscopic assessment of total hip replacement and polyethylene wear: A case report. Knee Surg Sports Traumatol Arthrosc. 2000;8:244–5. doi: 10.1007/s001679900102. [DOI] [PubMed] [Google Scholar]
- 49.Gédouin JE, Huten D. Technique and results of endoscopic tenotomy in iliopsoas muscle tendinopathy secondary to total hip replacement: A series of 10 cases. Orthop Traumatol Surg Res. 2012;98:S19–25. doi: 10.1016/j.otsr.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 50.de Sa D, Cargnelli S, Catapano M, Peterson D, Simunovic N, Larson CM, et al. Efficacy of hip arthroscopy for the management of septic arthritis: A Systematic review. Arthroscopy. 2015;31:1358–70. doi: 10.1016/j.arthro.2014.12.028. [DOI] [PubMed] [Google Scholar]


