Abstract
Background:
Arthritis is the most common form of joint disease. Total knee arthroplasty (TKA) is the most effective surgical intervention for end-stage knee osteoarthritis. The purpose of this study is to access whether patients who participated in preoperative rehabilitation before primary TKA received any postoperative benefit compared to patients who did not participate in preoperative rehabilitation.
Materials and Methods:
A comprehensive search of Medline, PubMed, Embase, CENTRAL, CINAHL, Ageline, and hand searching references and abstracts was performed. Inclusion criteria included patients undergoing primary and unilateral TKA. Exclusion criteria included patients who have bilateral, unicompartmental, or revision TKA. All studies compared preoperative exercise program versus no preoperative exercise. Outcomes included patients’ function, acute care length of stay (LOS), pain, and stiffness. The Western Ontario and McMaster Universities Osteoarthritis Index and 36-Item Short-Form Health Survey functional scales were used to assess these outcomes. Assessment was performed within 3 months of TKA.
Results:
Of 1347 articles, 1308 studies were excluded during title and abstract screening. Thirty nine articles underwent full-text screening and were narrowed to five studies matching all criteria. Two studies were combined showing a significant decrease in LOS favoring preoperative exercise (−0.93, 95% confidence interval: −1.29, −0.57). There was a lack of evidence to show any difference regarding self-reported function, stiffness, pain, and physical role.
Conclusion:
Preoperative exercise program may be beneficial and is associated with a significant decrease in length of hospital stay. No conclusive evidence can be delineated from the literature with respect to clinical outcome measures. Well-designed randomized trials would strengthen this position.
Keywords: Knee arthroplasty, outcomes, prerehabilitation, systemactic review
Introduction
Arthritis is the most common form of joint disease with radiographic evidence in up to 80% of the population by age 65. Total knee arthroplasty (TKA) is an effective method of pain relief and improving function.1,2,3,4,5,6
Patients awaiting TKA typically have advanced degenerative changes causing impaired muscle strength, decreased range of motion, altered balance, and global deconditioning.5 These contribute to physical disability and alteration in gait mechanics.7 Delayed diagnosis and treatment can lead to greater disability and deconditioning resulting in longer postoperative recovery, increased pain, and dysfunction.5,8
One method to minimize the effect of the overall deconditioning is to enroll patients into a physiotherapy program to decrease pain and increase function. These programs, often termed prehabilitation, are thought to benefit those treated nonoperatively for their arthritis. A Cochrane review of 2562 patients in 17 studies demonstrated benefits that included reduced pain and improved physical function in patients with osteoarthritis of the knee.9 Prehabilitation is thought to be one method to delay or decrease the burden of patients requiring TKA.
Previous observational and randomized clinical trials ignited interest in focusing on preoperative rehabilitation and its potential effect on postoperative recovery. Observational studies have showed poor outcomes in those deconditioned compared to those with a higher baseline functional status.5,8 The few randomized controlled trials (RCTs) focusing on prehabilitation showed an improvement while others showed little or no benefit.
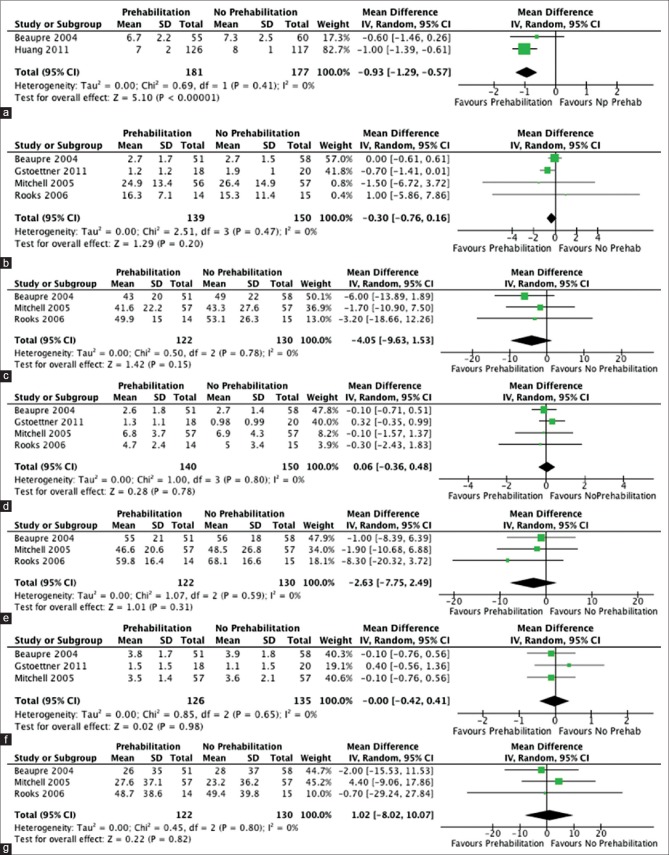
There have been attempts to assimilate the knowledge from randomized trials; however, each has their own unique challenges that limited the utilization of the information. Using the AMSTAR tool, we assessed the quality of the previous systematic reviews on the benefits of preoperative rehabilitation on postoperative recovery after TKA [Figure 1].10,11,12,13,14,15 Using the AMSTAR scoring, we found multiple flaws.
Figure 1.
Amstar categories
The objective of our study is to use randomized control trials to determine whether preoperative rehabilitation in patients who undergo TKA offered any benefit in pain, function, range of motion, and length of stay (LOS) compared to patients who did not participate in a preoperative rehabilitation or exercise regimen. Using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), 36-Item Short-Form Health Survey (SF-36) scores, and hospital LOS, our primary objective is to assess patients’ self-reported function and LOS in the hospital. Our secondary objectives are to assess function with respect to pain and stiffness.
Materials and Methods
A study protocol was created with a priori hypotheses and objectives. Patients included within the study protocol included those undergoing primary, unilateral, uncomplicated TKA. Studies that included bilateral, unicompartmental, and revision TKA were excluded from the study. Studies included trials with patients who underwent preoperative rehabilitation or an exercise program before their surgery, which was then continued postoperatively. These groups of patients were compared against a group of patients who did not participate in preoperative exercise- or rehabilitation-specific program. Primary outcomes assessed patients’ function and length of hospital stay. Secondary outcomes include pain and stiffness. WOMAC and SF-36 functional scales were used to assess the outcomes of pain, function, and stiffness. Any effect was assessed within 3 months of the TKA. Only. RCTs were included in the study.
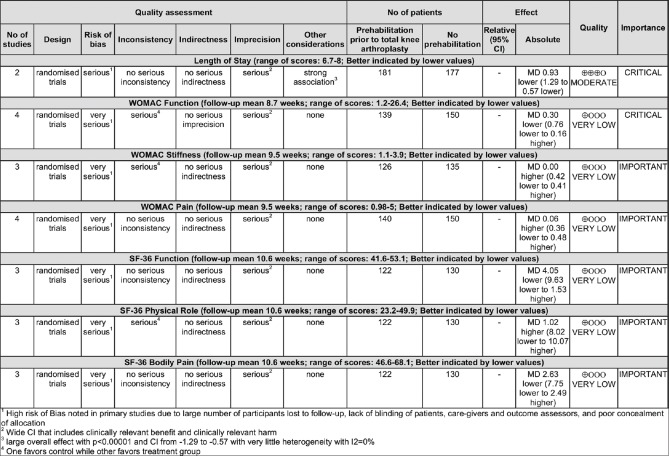
Medline (1946-2015), PubMed (1950-2015), Embase (1980-2015), CENTRAL, CINAHL (1982-2015), and Ageline (1966-2015) databases were selected to identify relevant studies. All relevant papers were hand searched and references reviewed looking for any further studies. Major orthopedic conferences’ abstracts were also scanned for any relevant unpublished studies. For any unclear studies, the authors were contacted for clarification. All searches were performed on December 5, 2015 [Figure 2].
Figure 2.
Summary of searches
All identified articles were imported into Endnote x7 software (Clarivate Analytics. Philadelphia, PA. USA). Premade title and abstract screening and full-text screening forms were made to guide selection of appropriate RCTs. Using the premade forms, screening began with a comprehensive, inclusive title and abstract screening search. The two reviewers (RS and IA) then independently performed a full-text assessment using the full-text screening forms to identify the relevant articles to include in the review. A kappa statistic was used to measure the correlation between the two reviewers for the full-text screening. Any discrepancies were discussed between two reviewers.
To gather appropriate data to answer our primary and secondary outcomes, the WOMAC and SF-36 scale values were identified. Both these scales are well-validated tools with high reliability and validity on all categories. We extracted the data from the three categories of the WOMAC (pain, stiffness, and function) and extracted three of the eight domains of the SF-36 (bodily pain, physical role, and function). Finally, we looked at length of time in an acute care facility postoperatively.
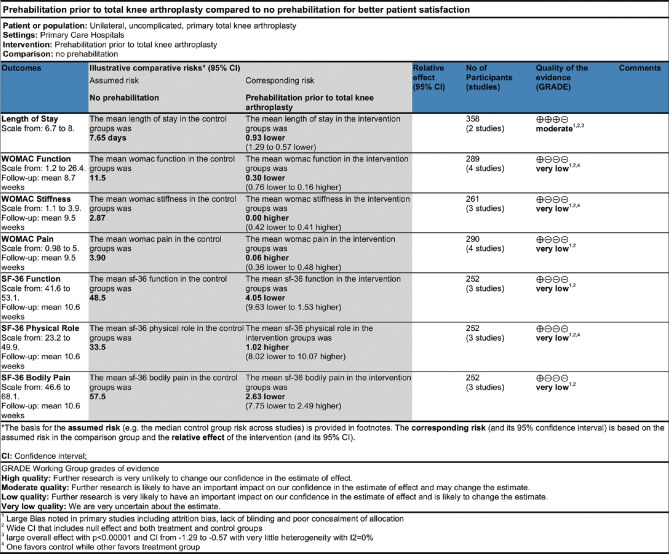
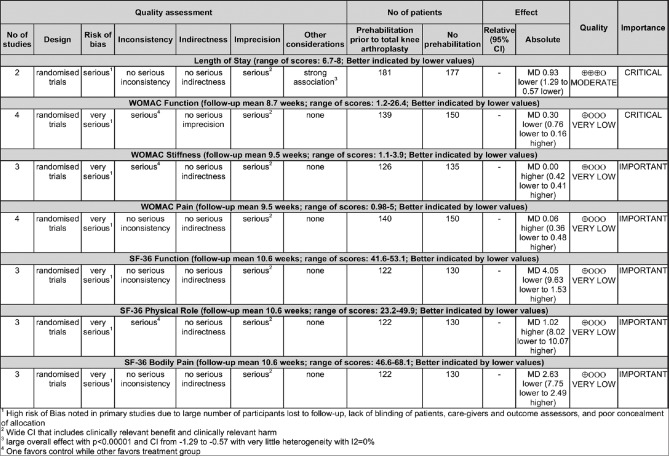
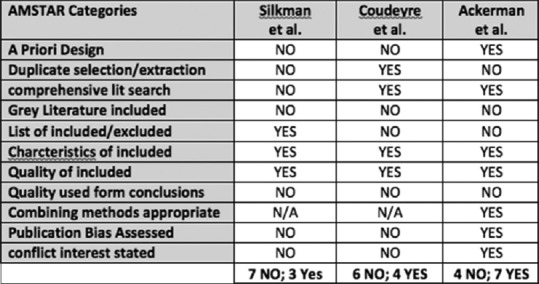
Risk of bias testing was addressed at both the study and outcome level. At the study level, the risk of bias was assessed using the Cochrane Collaboration tool for assessing the risk of bias. With respect to reviewing the level of outcomes in the studies we reviewed, the risk of bias was assessed and summarized [Figures 3 and 4]. Using these figures, the extent of bias was reviewed to determine if these results could be trusted for clinical application. Finally, within each outcome, funnel plots were examined to look for any exaggerated studies that could represent publication bias.
Figure 3.
Summary of findings
Figure 4.
Grade reporting
No discrepancies were found between the two reviewers. Once the data were collected, the principal summary measure was determined to be the mean difference, as all outcomes were deemed to be continuous variables. The data were extracted from relevant studies and imported into the Review Manager 5 software (Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Results
Detailed search produced 1594 results. Hand searching references, abstracts, and contacting authors did not produce any additional articles. After removal of 247 duplicate articles, 1347 articles were used for the title and abstract screening. Nearly 1308 studies were excluded during this process. The remaining 39 articles were used for full-text eligibility screening. Of the 39 studies, 34 were excluded from the study. Reasons for exclusion included three duplicates not previously identified, five studies reviewed included outcomes not of interest, three were systematic reviews of RCTs, ten were not randomized controlled clinical trials, ten studies only included total hip arthroplasty, and three studies involved highly specific patient population that was not amenable to be included into the systematic review [Figure 5].16,17,18,19,20,21,22,23 Kappa correlation for the full-text review was 0.87 (standard error = 0.16). This resulted from a discrepancy in one study due to the unconventional outcomes.24 However, since it contained appropriate length of hospital stay data, we agreed for it to be included within the systematic review.
Figure 5.
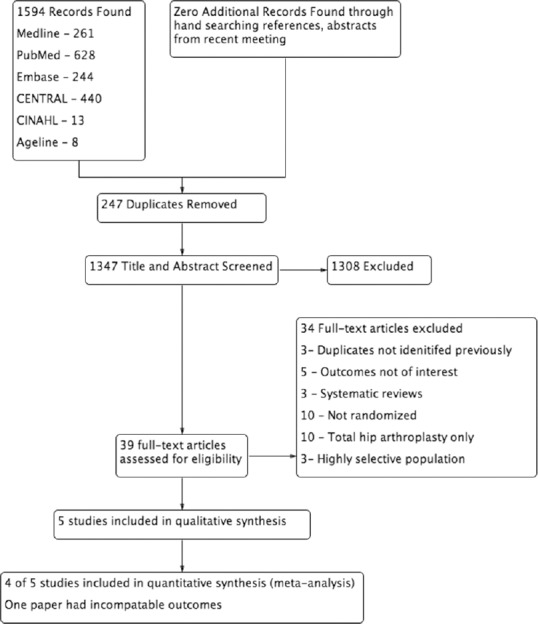
Prisma flow diagram
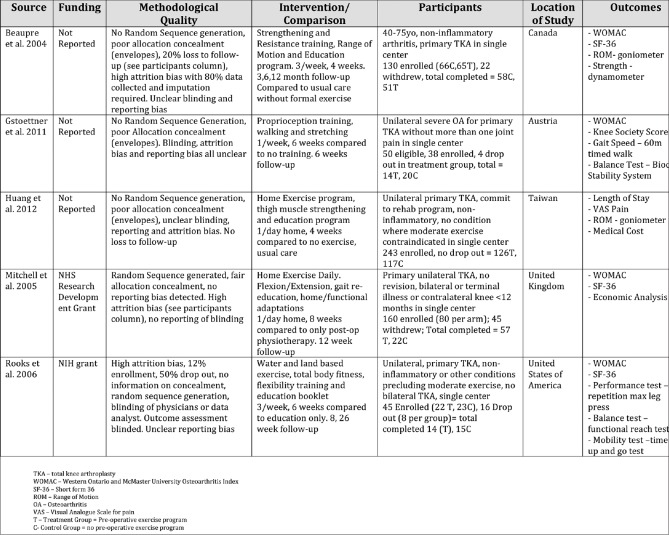
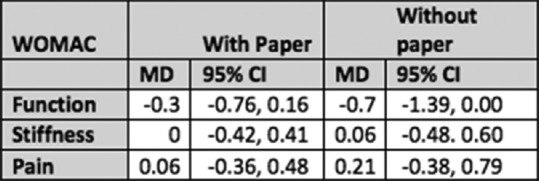
Five papers were selected for inclusion in this systematic review. To address our objectives regarding the WOMAC categories (pain, stiffness, and function), four studies qualified to be enrolled.24,25,26,27 Of the four studies, one by Beaupre et al. transformed the WOMAC data to correlate with the SF-36 scale. In order to transform this back to match the conventional 10-point visual analog format, the results of the paper required a calculated transformation. A sensitivity analysis with and without this paper was performed to verify that the calculation did not produce spurious results. The results from both inclusion and exclusion of the study lead to similar results. In addition, within the funnel plot, no study was found to be overtly different [Figure 6]. With the inclusion of these results, the confidence intervals (CIs) tightened in all three cases for the WOMAC function, pain, and stiffness and therefore leading to a stronger analysis of the results.
Figure 6.
Western Ontario and McMaster Universities Osteoarthritis index results
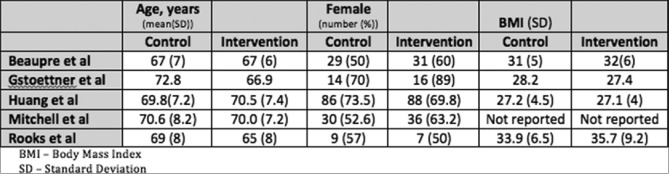
To address the three SF-36 domains of interest, three RCTs were eligible.24,26,27 To address LOS in the acute care hospital, two studies were eligible to enroll28,24 [Figure 7]. Observing the demographics of the patient population across studies, there is little difference observed [Figure 8].
Figure 7.
Enrolled studies
Figure 8.
Patient demographics
Overall, there was a high loss to followup or completion of study throughout all studies except for one (Huang et al.26). Two studies (Gstoettner et al.29 and Rooks et al.30) had very small patient populations.
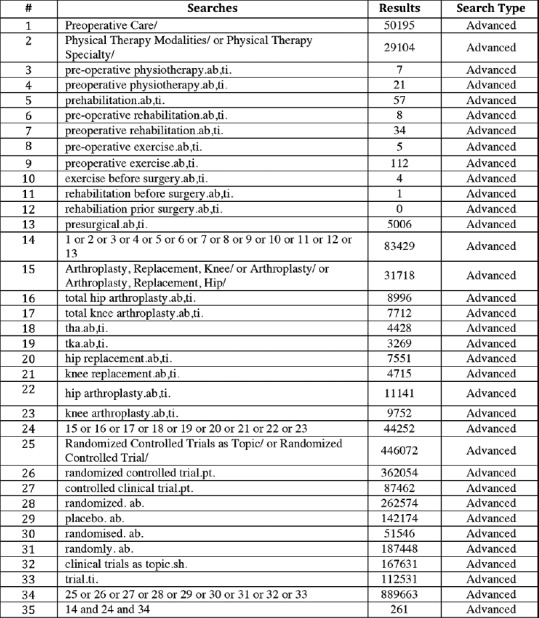
Two studies examined the LOS in an acute care facility after TKA [Figure 9a]. Combined, the studies included 181 patients in the treatment group and 177 patients in the control group. The mean difference was found to be −0.93 (95% CI: −1.29, −0.57). The CI was not found to cross the line of no effect. The test for overall effect was found to be statistically significant in favor of preoperative rehabilitation (Z = 5.10; P < 0.00001). No heterogeneity was identified (χ2 = 0.69 and I2 = 0%).
Figure 9.
(a) Length of stay. (b) Western Ontario and McMaster Universities Osteoarthritis index function. (c) 36-Item Short-Form Health Survey function. (d) Western Ontario and McMaster Universities Osteoarthritis index Pain. (e) 36-Item Short-Form Health Survey pain. (f) Western Ontario and McMaster Universities Osteoarthritis index stiffness. (g) 36-Item Short-Form Health Survey physical role
Functional outcomes were assessed using both the WOMAC and SF-36 regarding self-reported function. Four papers were applicable for the meta-analysis evaluating WOMAC function [Figure 9b]. The total sample size included 139 patients in the prehabilitation group versus 150 patients in the control group. Using the random-effects model, mean difference was found to be −0.30 (95% CI: −0.76, 0.16). The CI was found to cross the no effect line. The test for overall effect was not found to be statistically significant (P = 0.20 and Z = 1.29). No heterogeneity was found (χ2 = 0.47, I2 = 0%). Three studies were available to review with respect to SF-36 function [Figure 9c]. The total treatment population included 122 patients and 130 controls. Using the random-effects model, the mean difference was found to be − 4.05 (95% CI: − 9.63, 1.53). This CI crosses the line of no effect. The test of overall effect was not found to be significant (P = 0.15; Z = 1.42). No significant heterogeneity was found (χ2 = 0.50, I2 = 0%).
Secondary outcomes were assessed using the WOMAC pain and SF-36 bodily pain values. Four studies were appropriate to review with respect to WOMAC pain [Figure 9d]. Using the random-effects model, the mean difference was found to be 0.06 (95% CI: −0.36, 0.48). The CIs cross the line of no effect. The test for overall effect was not significant (P = 0.78, Z = 0.28). No significant heterogeneity was found (χ2 = 0.80, I2 = 0%). Three studies were included in the analysis of SF-36 bodily pain [Figure 9e]. One hundred and twenty two patients in total were in the treatment group whereas 130 patients were found in the no prehabilitation group. Using the random-effects model, the mean difference was found to be −2.63 (95% CI: −7.75, 2.49). The CI crossed the line of no significance. The test for overall effect was not significant (P = 0.31). No significant heterogeneity was found (χ2 = 0.59, I2 = 0%).
Three studies were included in the review of WOMAC stiffness [Figure 9f]. This involved 126 patients who underwent prehabilitation versus 135 control patients. Using the random-effects model, the mean difference lay on the line of no effect, 0.00 (95% CI: −0.42, 0.41). The test for overall effect was not found to be significant (P = 0.98; Z = 0.02). No significant heterogeneity was found (χ2 = 0.65, I2 = 0%).
Three studies were included in the review of SF-36 physical role [Figure 9g]. One hundred and twenty two patients were in the treatment group versus 130 patients in the no prehabilitation group. Using the random-effects model, the mean difference was found to be 1.02 (95% CI: −8.02, 10.07). The CI crosses the line of no effect. No significant heterogeneity was found (χ2 = 0.45, I2 = 0%).
The risk of bias across each outcome was performed using the GRADE criteria. The GRADE criteria aim to classify the quality of a recommendation based on the strength of evidence. The GRADE criteria use the design of the study, risk of bias, inconsistency, indirectness, imprecision, and other considerations to create a judgment on the quality of evidence [Figure 10].
Figure 10.
Quality of evidence
Due to the low quality of randomized clinical trials, all outcomes have a great risk of bias and all have imprecise results with large CIs. As a result, all outcomes except for LOS resulted in “very low” grade of evidence. LOS resulted in a “moderate” quality of GRADE evidence. This outcome was upgraded since there was a strong association and large overall effect with P < 0.00001 with very low heterogeneity (I2 = 0%).
All outcomes were homogeneous [Figure 9a–g]. All outcomes had an I2 of 0% while no overt imbalance was noted within the funnel plots. Since all studies were homogenous, no further analyses or subgroup analyses were necessary.
Discussion
This study examines whether preoperative physiotherapy improves the outcome after TKA. Our primary outcomes included LOS in the hospital and knee function as per the WOMAC and SF-36 scales. Our secondary outcomes included postoperative pain, stiffness, and physical role.
There are multiple strengths of this review. We performed a complete search of all the available literature. We did not limit our search to the English language and performed hand searches of references and abstracts from recent conferences. We also attempted to contact authors when necessary. Our study was performed in duplicate with strong agreement between reviewers. We examined risks of bias across both studies and outcomes to present the results accurately.
Limitations did exist within this paper. There was no uniformity in our preoperative exercise program. We included any program which encouraged range of motion and strengthening exercises. Second, we felt that the self-reported outcomes were most important in the 3 months following TKA and thus only included studies that offered outcomes at the 3-month postoperative mark. However, the lack of heterogeneity in the results may have alleviated the impact of these potential limitations.
In assessing the risk of bias and quality of included studies, the quality of available literature is poor. In fact, looking at the Grade profiles [Figure 10], all outcomes except for LOS in the hospital arise from very poor quality of evidence. The failure of included randomized clinical trials to reduce bias lowers the internal validity of included studies. Imprecision of estimates, wide CIs, and small patient populations that did not reach the estimated power in nearly all studies, seriously limits the applicability of RCT study results. However, the very low heterogeneity and therefore higher reliability (I2 = 0% and insignificant Chi-square test for homogeneity) across all included studies do help strengthen the overall findings of this study.
LOS in the hospital was the only outcome that rated “moderate” as per the GRADE criteria. The upgrade was accepted compared to other outcomes, as there was a large estimate of effect (P < 0.00001) and smaller CIs (−1.29, −0.57). There was very little heterogeneity across the two included studies (I2 = 0%, χ2 = 0.69).
Although limited by the quality of the studies available in the literature, this review did show that preoperative physiotherapy reduced acute care hospital stay after TKA when compared to patients who did not have preoperative therapy (−0.93, 95% CI: −1.29, −0.57, Z-test for overall effect P < 0.00001). As health care organizations are forced to work with smaller budgets and are asked to provide efficient care, this finding is significant since decreasing the postoperative hospital stay following total knee replacement can decrease the medical cost per patient.
Our second primary outcome involved examining overall patient function less than or equal to 3 months after surgery. Both the WOMAC and SF-36 had similar results. In both cases, there was no benefit noted with the CIs crossing the line of no effect. In the case of the WOMAC function, the mean difference was found to be −0.30 (95% CI: −0.76, 0.16 and Z-test for overall effect, P = 0.20). In the case of the SF-36, the mean difference was −4.05 (95% CI: −9.63, 1.53 and Z-test for overall effect P = 0.15). In both cases, there was a tendency toward favoring prehabilitation; however, there was insufficient evidence to show any effect with the current data.
Examining the secondary outcomes, SF-36 physical role (1.02 95% CI: −8.02, 10.07), WOMAC stiffness (−0.00 95% CI: −0.42, 0.41), and WOMAC pain (0.06 95% CI: −0.36, 0.48) all had the mean difference centered on the line of no significance. Limited data is available to conclude preoperative physiotherapy and any effect of it on these postoperative outcomes. There was a slight tendency for SF-36 bodily pain to favor preoperative physiotherapy (−2.63, 95% CI: −7.75, 2.49); however, the CI did cross the line of no effect, while the WOMAC pain centered more closely to the line of no effect.
Function and pain were examined both within the SF-36 and the WOMAC scales. In three out of four studies, all patients were scored using both the SF-36 and the WOMAC scales. Therefore, combining these outcomes using standardized mean difference was of little value since they represent data from the same set of patients. One study by Gstoettner et al. examined only the WOMAC. This study only included 18 patients within the treatment group and 20 within the control group. The value of combining the data using standardized mean difference was minimal.
It is unfortunate that all aspects of self-reported postoperative outcomes produced inconclusive results. In determining the success or failure of an operation, patient-perceived care outweighs all other methods of judging surgical outcomes. However, since these conclusions are derived from poor research studies, there is ample opportunity for further research to examine the effects of preoperative exercise program. Furthermore, although the evidence favored a decreased LOS in patients who had preoperative therapy, having higher quality studies would allow us to further examine this effect and narrow the CIs.
Conclusion
Preoperative physical therapy lowered acute hospital LOS following TKA. Clinical outcome measures, which included the use of SF-36 and WOMAC scores, were inconclusive; this study demonstrates the need for further research in the form of randomized control trials to improve the overall quality of evidence available.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: New insights. Part 1: The disease and its risk factors. Ann Intern Med. 2000;133:635–46. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 2.Beaupré LA, Davies DM, Jones CA, Cinats JG. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: A randomized controlled trial of patients following total knee arthroplasty. Phys Ther. 2001;81:1029–37. [PubMed] [Google Scholar]
- 3.Lucas B. Does a preoperative exercise programme improve mobility and function post-total knee replacement: A mini-review. J Orthop Nurs. 2004;8:25–33. [Google Scholar]
- 4.Livbjerg AE, Froekjaer S, Simonsen O, Rathleff MS. Preoperative patient education is associated with decreased risk of arthrofibrosis after total knee arthroplasty: A case control study. J Arthroplasty. 2013;28:1282–5. doi: 10.1016/j.arth.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today. Etiology of total knee revision in 2010 and 2011? J Arthroplasty. 2013;28:116–9. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 6.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–7. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: Preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–8. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 9.Fransen M, McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2008;4:CD004376. doi: 10.1002/14651858.CD004376.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Viton JM, Atlani L, Mesure S, Franceschi JP, Massion J, Delarque A, et al. Reorganization of equilibrium and movement control strategies in patients with knee arthritis. Scand J Rehabil Med. 1999;31:43–8. doi: 10.1080/003655099444713. [DOI] [PubMed] [Google Scholar]
- 11.Fortin PR, Penrod JR, Clarke AE, St-Pierre Y, Joseph L, Bélisle P, et al. Timing of total joint replacement affects clinical outcomes among patients with osteoarthritis of the hip or knee. Arthritis Rheum. 2002;46:3327–30. doi: 10.1002/art.10631. [DOI] [PubMed] [Google Scholar]
- 12.Fransen M, McConnell S, Bell M. Exercise for osteoarthritis of the hip or knee. Cochrane Database Syst Rev. 2003;89(3):CD004286. doi: 10.1002/14651858.CD004286. [DOI] [PubMed] [Google Scholar]
- 13.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–20. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, et al. External validation of a measurement tool to assess systematic reviews (AMSTAR) PLoS One. 2007;2:e1350. doi: 10.1371/journal.pone.0001350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ackerman IN, Bennell KL. Does preoperative physiotherapy improve outcomes from lower limb joint replacement surgery? A systematic review. Aust J Physiother. 2004;50:25–30. doi: 10.1016/s0004-9514(14)60245-2. [DOI] [PubMed] [Google Scholar]
- 17.Coudeyre E, Jardin C, Givron P, Ribinik P, Revel M, Rannou F, et al. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of french clinical practice guidelines. Ann Readapt Med Phys. 2007;50:189–97. doi: 10.1016/j.annrmp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Silkman Baker C, McKeon JM. Does preoperative rehabilitation improve patient-based outcomes in persons who have undergone total knee arthroplasty? A systematic review. PM R. 2012;4:756–67. doi: 10.1016/j.pmrj.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther. 2003;70:88–96. doi: 10.1177/000841740307000204. [DOI] [PubMed] [Google Scholar]
- 20.Hoogeboom TJ, Dronkers JJ, van den Ende CH, Oosting E, van Meeteren NL. Preoperative therapeutic exercise in frail elderly scheduled for total hip replacement: A randomized pilot trial. Clin Rehabil. 2010;24:901–10. doi: 10.1177/0269215510371427. [DOI] [PubMed] [Google Scholar]
- 21.Gill SD, McBurney H, Schulz DL. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: Results of a randomized controlled trial. Arch Phys Med Rehabil. 2009;90:388–94. doi: 10.1016/j.apmr.2008.09.561. [DOI] [PubMed] [Google Scholar]
- 22.Topp R, Swank AM, Quesada PM, Nyland J, Malkani A. The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM R. 2009;1:729–35. doi: 10.1016/j.pmrj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Memtsoudis SG, Stundner O, Yoo D, Gonzalez Della Valle A, Boettner F, Bombardieri AM, et al. Does limb preconditioning reduce pain after total knee arthroplasty? A randomized, double-blind study. Clin Orthop Relat Res. 2014;472:1467–74. doi: 10.1007/s11999-013-3106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D’Lima DD, Colwell CW, Jr, Morris BA, Hardwick ME, Kozin F. The effect of preoperative exercise on total knee replacement outcomes. Clin Orthop Relat Res. 1996;326:174–82. doi: 10.1097/00003086-199605000-00020. [DOI] [PubMed] [Google Scholar]
- 25.Berge DJ, Dolin SJ, Williams AC, Harman R. Preoperative and postoperative effect of a pain management programme prior to total hip replacement: A randomized controlled trial. Pain. 2004;110:33–9. doi: 10.1016/j.pain.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Huang SW, Chen PH, Chou YH. Effects of a preoperative simplified home rehabilitation education program on length of stay of total knee arthroplasty patients. Orthop Traumatol Surg Res. 2012;98:259–64. doi: 10.1016/j.otsr.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Beaupre LA, Lier D, Davies DM, Johnston DB. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol. 2004;31:1166–73. [PubMed] [Google Scholar]
- 28.Evgeniadis G, Beneka A, MAlliou P, Mavromoustakos S, Godolias G. Effects of pre- or postoperative therapeutic exercise on the quality of life, before and after total knee arthroplasty for osteoarthritis. J Back Musculoskelet Rehabil. 2008;21:161–9. [Google Scholar]
- 29.Gstoettner M, Raschner C, Dirnberger E, Leimser H, Krismer M. Preoperative proprioceptive training in patients with total knee arthroplasty. Knee. 2011;18:265–70. doi: 10.1016/j.knee.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 30.Rooks DS, Huang J, Bierbaum BE, Bolus SA, Rubano J, Connolly CE, et al. Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55:700–8. doi: 10.1002/art.22223. [DOI] [PubMed] [Google Scholar]