Abstract
Physiotherapy plays a key role in the management of cerebral palsy (CP) and comprises of various therapeutic interventions in enhancing the various physiological and functional outcomes. Though physiotherapy is used widely and recommended by all members of the health-care team, the effectiveness of physiotherapy is inconsistent. The objective of this review was to summarize and evaluate the effectiveness of physiotherapy interventions in children with CP. PubMed and Cochrane database were searched from January 2006 to April 2017 using the Medical Subject Heading and general keywords. Only systematic reviews and meta-analysis on PT interventions in children diagnosed with CP were included. Two reviewers independently assessed the methodological quality and retrieved the results. Thirty-four systematic reviews were identified that distinguished 15 different interventions. Moderate evidence of effectiveness was found for constraint-induced movement therapy for upper limb recovery, goal-directed/functional training, and gait training to improve gait speed. Conflicting evidence was found for the role of exercises on strength training and cardiorespiratory training. Intervention such as neurodevelopmental therapy (NDT) was found ineffective. This review suffer from limitations such as including reviews that had small sample size and that had considered heterogeneity of treatment interventions. Hence, the effectiveness of most PT interventions is found to be limited. On the basis of the present evidence, functional goal-oriented approaches are found to be effective and future research is required to determine the best ways to improve functional outcomes in children with CP.
Keywords: Cerebral palsy, exercise therapy, muscle weakness, physical activity, physical therapy techniques, rehabilitation
Introduction
Cerebral palsy (CP) is one of the most common developmental disabilities. The incidence of CP is around 3 cases per 1000 live births in India,1 and the 2011 statistics indicate that there are about 25 lakh children with CP in India.2 CP is a bracket term given for a set of neurological disorders characterized by disorders of movement and posture causing activity limitation attributed to a static disturbance in the developing brain, often accompanied by associated impairments and secondary health conditions.3 CP is not a single pathological entity and encompasses disorders in various motor functions including but not limited to body movement, muscle control, muscle coordination, muscle tone, reflex, fine motor skills, gross motor skills, oral motor functioning, posture, and balance.4,5 This in turn leads to poor functional strength, sedentary behavior, and dependence on others to carry out activities of daily living and reduced activity in leisure and community activities.6
Physiotherapy plays a key role in the management of CP and almost all persons diagnosed as CP receive physiotherapy services.7 The goals of physiotherapy are facilitating the participation needs of the child with CP and reducing the physical impairments of the symptoms. Physiotherapy helps children with CP to achieve their maximum potential for physical independence and fitness levels and improve the quality of life of the children and their family by minimizing the effect of their physical impairments.8
Physiotherapists use various therapeutic interventions in enhancing the autonomy, strength, and coordination of voluntary movements. Physiotherapy literature for CP contains multiple interventions, expanding rapidly every year. Though physiotherapy is used widely and recommended by all members of health-care team,9 the effectiveness of physiotherapy is inconsistent.10 Health care around the world has shifted its focus toward evidence-based practice. Literature has shown that considerable amount of interventions currently used by clinicians are deemed to be ineffective and unnecessary.11 The professionals involved in providing therapy services have to consider the effectiveness of these interventions during clinical decision-making. Hence, we wanted to provide clinicians with the evidence for quick reference by comparing and contrasting the results of available systematic reviews to provide a summary of physiotherapy evidence. The objective of this work was to summarize and evaluate the evidence for the effectiveness of various therapeutic interventions employed in physiotherapy for children with CP.
Materials and Methods
The research question (what is the evidence that physiotherapy improves functional outcomes for patients with CP?)that could be answerable on the light of available evidence (systematic review and meta-analysis) was structured for searching using the population, intervention, comparison, and outcome format.
Population: Persons aged 0–20 years with a diagnosis of CP. Intervention: Use of any clinically proven physiotherapy interventions, or a combination of interventions. Comparison: Any other treatments or control groups including placebo, sham therapy, or other PT interventions. Outcome: Improved motor function, improved abilities in functional skills, and reduction in spasticity.
We searched computerized bibliographic databases for reviews on physiotherapeutic interventions in CP in English for the last decade (January 2006 to April 2017) to identify systematic reviews and meta-analysis to provide an overview of the current state of evidence using PubMed and the Cochrane Database of Systematic Reviews. These databases were searched using the Medical Subject Headings keywords (systematic review) AND cerebral palsy AND physiotherapy, physical therapy specialty, physical therapy modalities, exercise therapy, exercise movement technique, electric stimulation therapy, massage and general search terms such as exercise training (in combination with strength, fitness, working capacity, aerobic power, anaerobic power, endurance, cardiorespiratory physical training, or programme), functional training, functional therapy, neurodevelopmental treatment/Bobath, hydrotherapy, hippotherapy, and goal-setting. The search settings were kept to maximize the retrieval of references. In addition, the reference lists of identified articles and systematic reviews were screened for additional relevant publications.
Studies meeting the following criteria were included: (1) reviews should have been published between January 2006 and April 2017; (2) papers written in English; (3) the papers should have considered any physiotherapy interventions in the treatment of children and adolescents (age range: 0–20 years) with CP only; and (4) should be either systematic reviews or meta-analyses. Studies were excluded from the review if studies (1) were written with the perspective of diagnosis, prognosis, guidelines, or other interventions aimed at CP; (2) participants were adults with CP; (3) reviewed general medical neurological interventions (e.g., home care therapy, spastic medications/botulinum injections, and not physiotherapy-specific interventions); (4) if no specific outcome measures were mentioned/parents’ or caregivers’ experiences were considered as outcomes; and (5) if systematic reviews were identified in predatory journals.
All identified articles were judged for eligibility by title and abstract by two reviewers and differences any, when aroused regarding unclear articles, were resolved by consensus. The quality of the evidence obtained was graded using the National Institute for Health and Care Excellence protocol.12 Relevant studies to the research question were entered into an evidence table [Table 1].
Table 1.
Evidence table
| Study | Population/setting | Intervention/aim | Outcomes | Results | Comments | Design | Evidence level/quality |
|---|---|---|---|---|---|---|---|
| Sakzewski et al., 201313 | Studies that evaluated the efficacy of upper-limb therapy in children between 0 and 18 years of age with unilateral CP | To systematically review the efficacy of nonsurgical upper-limb therapies for children with unilateral CP | Outcomes are measured in terms of unimanual or bimanual capacity and performance, achievement of individualized goals, or self-care skills | Forty-two trials involving 13 upper-limb interventions were studied. The overall results suggested that there is modest evidence that intensive activity-based, goal-directed interventions are more effective in improving outcomes | Despite the small sample size of studies included, the result seems valid | Meta-analysis | 1++ |
| Pin et al., 200614 | Studies that included children with CP (aged younger than 18 years) with spasticity | Studies other than expert opinions that evaluated the effectiveness of passive stretching in children with spastic CP | The outcomes measured were changes in range of motion, spasticity, and gait | Seven studies including three RCTs, one crossover RCT, one before-and-after study, and two multiple single-subject studies. Results show limited evidence that manual stretching can increase range of motion, reduce spasticity, and improve walking efficiency in children with CP | Though adequate information about the included studies was provided, several studies assessed multiple outcomes and the numbers of participants were rather low | Systematic review | 1− |
| Dong et al., 201315 | Studies that involved hemiplegic children with CP aged between 2 and 16 years | Studies that randomized and compared the efficacy of constraint-induced movement therapy with bimanual training in improving impaired arm function and overall functional performance among children with hemiplegic CP | Unimanual, bimanual, and overall functional performance were measured using a variety of different measures | Seven studies including six RCTs and one quasi-randomized trial. Constraint-induced movement therapy for children with hemiplegic CP resulted in greater improvements in the unimanual capacity of the impaired arm than bimanual training; bimanual training improved bimanual performance and overall life goals | Results of the review may not be reliable as the review was restricted to studies that were published before 5 years; hence, the probability of missing other relevant studies is abundant. Further, only one of the studies had a true control group. Results may be because of lack of statistical power | Systematic review | 1− |
| Huang et al., 200916 | Studies that evaluated children (younger than 18 years) with hemiplegic CP | To investigate the effectiveness of CIMT in children with CP | Body function and structure (grasp strength and modified Ashworth Scale) and activity (Jebsen-Taylor test of hand function and caregiver functional use survey) | Twenty-one studies were included in this review. The report concludes that there is positive support for the use of CIMT to improve the upper-extremity use for children with hemiplegic CP | Inconsistencies exist around the review methodologies used, and there are high probabilities that relevant studies could be missed | Systematic review | 1− |
| Chiu and Ada, 201617 | Studies that involved hemiplegic children with CP | To compare the effectiveness of CIMT against the same dose of upper-limb therapy without restraint | Activity and participation components of the ICF, disability, and health framework | Twenty-one randomized/quasi-controlled trials were included. CIMT is no more effective than the same dose of upper-limb practice without restraint | Despite the small sample size of studies included and absence of data from some of the studies, the results seem valid and reliable | Systematic review | 1+ |
| Chen et al., 201418 | Studies that evaluated children with CP between birth and 21 years of age | To systematically examine the effectiveness of CIMT on improving arm function in children with CP | The individual outcome measures measured in RCTs were calculated in terms of Cohen’s effect size. Further, where multiple outcome measures were utilized, the outcome measures were classified in terms of the ICF | Twenty-seven RCTs were identified that met the criteria. The overall results showed that the CIMT is an effective therapy to improving arm function in children with CP. The results are more pronounced for those children who practised CIMT at home | Despite the variable intervention protocols used, the results seem to be reliable | Systematic review | 1+ |
| Hoare et al., 200719 | Children with hemiplegic CP who are under 19 years of age | To evaluate the effectiveness of CIMT, modified CIMT, or forced use in the treatment of the affected upper limb in children with hemiplegic CP | Various upper-limb motor outcome scales, with and without psychometric properties | Three trials were included for review. There is limited evidence for the use of CIMT, modified CIMT, and forced use in children with hemiplegic CP | This result is based on small trials with poor methodology and not so reliable outcome measures. Hence, results should be accepted with caution | Systematic review | 1− |
| Moreau et al., 201620 | Ambulatory children with CP who are under 18 years of age | To determine the effectiveness of interventions for improving gait speed in ambulatory children with CP | Gait speed | Twenty-four studies (only one trial was case-controlled trial; others were RCTs) were considered for review. Gait training was the most effective intervention in improving gait speed for ambulatory children with CP | Gait speed was the only parameter analyzed | Systematic review | 1++ |
| Butler et al., 201021 | Studies that included school-age children with CP | Intervention included cardiorespiratory training programs consisting of either individual activities or combination programs that were progressed in duration and intensity | Measures of aerobic fitness such as peak oxygen uptake and 6-min walk test | Three RCTs were found; there is limited evidence about the effect of cardiorespiratory training in children with CP | Results based on limited data | Systematic review | 1++ |
| Arpino et al., 201022 | Studies that included children with CP with an age range from 1 to 18 years | RCTs that compared the efficacy of intensive versus nonintensive rehabilitation in children with CP | Changes in GMFM were considered as an outcome measure | Four RCTs were included. Results showed modest effect size and limited evidence that intensive conventional therapy could improve the functional motor outcome in children with CP | Reliability of this result is uncertain as the review has reported limited trials; variation in the included trials and contribution of small samples are other limitations | Systematic review | 1++ |
| Martin et al., 201023 | Studies that included children with CP aged from 4 to 18 years | Prospective studies of any design except single-case studies were considered to evaluate the effectiveness of commonly used physiotherapy interventions, for children with CP | Measures of strength as measured on dynamometry and the GMFM, endurance, gait speed, and stride length | Thirty-four studies, of which 15 RCTs were retrieved and considered for review. The results concluded that there was strong evidence for interventions and functional training to strengthen targeted muscle groups in children with CP | Results based on studies that were small and with high risk of bias | Systematic review | 1++ |
| Verschuren et al., 200824 | Studies that included children and adolescents with CP | RCTs and observational studies were considered to assess the effectiveness of exercise programs for children with CP | The following outcomes were measured: changes in body function and structure, activity or participation in the ICF, disability and health framework | Twenty studies including five RCTs were considered for this systematic review. The review concluded that interventions focusing on lower-extremity muscle strength and cardiovascular fitness may benefit children with CP | Despite the inclusion of nonrandomized or low-quality trials, the recommendations of this review appear reliable | Systematic review | 1− |
| Scianni et al., 200925 | Studies that included children with CP aged from 4 to 19 years | Randomized, quasi-randomized, and controlled trials were evaluated to see if muscle- strengthening interventions can increase strength and improve activity in children and adolescents with CP | Outcomes were measured in terms of 10-min walk test, or GMFM | Five RCTs and one quasi-randomized trial were included in the review. Results found that strengthening interventions did not improve strength or activity in these populations | Results are likely to be reliable | Systematic review | 1++ |
| Mockford and Caulton, 200826 | Studies that included children who were ambulatory and aged from 4 to 20 years | To analyze the effects of progressive strength training on function and gait in ambulatory children and adolescents with CP | Outcomes were measured objectively | Thirteen articles were included for review. Function and gait improved in younger population | Results are questionable as the systematic review has included many uncontrolled trials for this analysis | Systematic review | 1− |
| Rogers et al., 200827 | Studies that included children with CP of any type and who were aged between 2 and 17 years | To assess the evidence regarding the effectiveness of aerobic training interventions for children with CP | Activities and participation | Thirteen studies were considered for the review. Though aerobic exercises are found to increase physiological outcomes, the translation into activities and participation are unknown | Poor methodological rigor and variable training preclude the conclusion | Systematic review | 1− |
| Mutlu et al., 200928 | Studies that included children with CP who are under 18 years of age | To evaluate the effectiveness of partial bodyweight-supported treadmill training on functional outcomes and ability to walk in children with CP | Variable outcome measures including GMFM score, the PEDI score, and measures of ambulatory status | Seven studies comprising 41 children were considered in this review. The review concluded that partial bodyweight-supported treadmill training did not result in gait improvement | Despite including studies of low-quality small studies, the results are found to be reliable | Systematic review | 1− |
| Chung et al., 200829 | Studies that included nonambulatory children with CP aged from 2 to 23 years | Studies of interventions involving adaptive seating for nonambulatory children with CP | Body structure and functions, activities, and participation components of ICF. Other outcomes that were considered were upper-extremity function, mobility, and social skills and performance in ADL | Fourteen studies, single-case and experimental designs, comprising 176 participants were included in the review. The results of the review showed that no single intervention was more effective than others in improving sitting posture or postural control in children with CP | Only English-language studies were considered. Other limitations are diversity of the studies, moderate quality of the studies included, small samples, and lack of control groups in majority of the studies | Systematic review | 1− |
| Chen et al., 201430 | Studies included children diagnosed as CP between 6 and 14 years of age | To consider studies that evaluated the effect of virtual reality on upper-extremity function in children with CP | The outcomes measured are: upper-extremity movements (such as reaching, grasping), or upper-extremity function as measured by GMFM | Fourteen studies including 122 children and three RCTs were considered for this review. The authors of this review recommended that more high-quality research is warranted in this area and the available evidence suggest that virtual reality is a viable tool to improve upper-extremity function in children with CP | Clinical and methodological differences across the studies, the statistical methods employed, and small sample sizes lead to nonreliable conclusions | Meta-analysis | 1− |
| Anttila et al., 200831 | Studies that included children with CP aged between 3 months and 20 years of age | To assess the effectiveness of physical therapy interventions on functioning in children with CP | The outcomes of the trials were classified using the ICF, disability, and health | Twenty-two RCTs utilizing eight different interventions were identified. Results of this review showed moderate, limited, and conflicting evidence for few interventions | Despite the poor quality of involved studies, the reliability of the review appears to be valid and of high quality | Systematic review | 1++ |
| Franki et al., 201232 | Studies that have included children less than 18 years of age receiving physiotherapy interventions targeting lower limb and trunk | To evaluate the effectiveness of conceptual approaches and additional therapies used in lower-limb physical therapy of children with CP | Outcomes were classified on the basis of the ICF model: body structure and function, activities and participation, personal factors, and environmental factors | Thirty-seven studies that concentrated on conceptual approaches and 21 studies on additional therapies were identified. Goal-oriented therapy and functional training were found to be effective | Only English-language studies were considered | Systematic review | 1+ |
| Snider et al., 200733 | English and German studies that evaluated the effectiveness of horseback riding in children between 2 and 12 years of age diagnosed as CP | To appraise the evidence on the effectiveness of hippotherapy and therapeutic horseback riding in children with CP | Outcomes were measured using a variety of tools including Bertoti Posture Assessment Scale, GMFM, EMG, gait parameters and kinematics, PEDI, BOTMP, PDMS, and VABS | A total of nine studies comprising 108 participants were included in this review. The review concluded that some fair evidence are found for hippotherapy on muscle symmetry in the trunk and hip | Considering the potential for error and bias in the review process, these results may not be reliable | Systematic review | 1− |
| Tseng et al., 201334 | Studies that evaluated the effectiveness of horseback riding in children who had CP and were under 18 years of age | To evaluate the efficacy of equine-assisted activities and therapies | The outcomes were represented in the ICF component of body functions and activities | Fourteen studies were considered. Though short-term effectiveness was found, the review did not find any significant benefits on the longer term in CP children | The heterogeneity of interventions provided means that the results cannot be attributed to horseback riding alone. Further, small samples and conventional sampling in the studies included limit the reliability of the results | Systematic review | 1− |
| Roostaei et al., 201635 | Studies that included children with any type of CP aged between 1 and 21 years of age | To review the literature on the effects of aquatic intervention on gross motor skills for children with CP | GMFM should serve as one of the outcomes | Eleven studies met the inclusion criteria including two RCTs. Evidence showed no adverse reaction to aquatic therapy but the effectiveness is limited | Poor quality of studies included | Systemic review | 1− |
| Güçhan and Mutlu, 201736 | Studies with all research designs that evaluated children with CP under 18 years of age | To investigate the effectiveness of taping in the children with CP | Outcome variables were grouped by the ICF, disability, and health. Model as body structure/function, activity, and participation | Nine studies including five RCTs were considered. Though the immediate effect of taping is unclear, there seems to be some long term effect on activity in children with CP | The differences in results may be attributed to the area of application of tape, variability in application techniques, the time period for which the outcomes were followed, and poor sample size renders the review nonreliable | Systematic review | 1− |
| Hadders-Algra et al., 201737 | Children/infants during the first postnatal year who are diagnosed with very high risk of CP | To review the evidence on the effect of early intervention in children at the risk of diagnosed as CP | For the evaluation of motor development, the Griffith developmental scales, Alberta Infant Motor Scale, Bayley Scales of Infant Development, Infant Motor Profile, and the Peabody Developmental Motor scales were used. Cognitive development was assessed with the Griffith Developmental scales. The Bayley Scales of Infant Development, the Neonatal Behavioral Assessment Scale, Hempel Assessment, PEDI, the Goal Attainment Scaling, and Canadian Occupational Performance Measure or a nonstandardized questionnaire | Thirteen articles were considered for review. The overall evidence is poor and the results of the review suggested that minimal application of postural support techniques is beneficial for infants with CP | Poor methodological studies and heterogeneous interventions preclude arriving at a conclusion based on the review | Systematic review | 1− |
| Morgan et al., 201638 | Children/infants diagnosed with very high risk of CP from birth to 2 years diagnosed with CP as assessed on the General Movements Assessment | To systematically review the evidence on the effectiveness of motor interventions | Any outcome assessment of motor skills/development | Thirty-four studies including ten interventions were considered. Child-initiated movement, environment modification/enrichment, and task-specific training had moderate-to-large effect on motor outcomes | Studies varied in quality, interventions, and participant inclusion criteria. Lack of high-quality studies makes the review less reliable | Systematic review | 1− |
| Saquetto et al., 201539 | Studies that evaluated the effects of whole-body vibration on motor function and functional performance in children with CP who are under 13 years of age | To evaluate the effects of whole-body vibration on physiologic and functional measurements in children with CP | The main outcomes of interest were motor function and functional performance including gait speed, GMFM, and bone density | Six studies with 176 patients compared whole-body vibration to other interventions. Whole-body vibration may improve gait speed and standing function in children with CP | Small studies and heterogeneity of analysis mean that the results can be interpreted with caution only | Systematic review | 1− |
| Dewar et al., 201540 | Studies that evaluated children diagnosed with CP, and aged between 0 and 18 years | To evaluate the efficacy and effectiveness of exercise interventions that claim to improve the postural control in children with CP | At least one outcome measure should be either postural stability (static or dynamic balance), or postural orientation (e.g., postural alignment) | Forty-five studies evaluated the effects of exercise interventions on postural control in children with CP. Gross motor task training, hippotherapy, treadmill training, trunk-specific training, and reactive balance training were supported by moderate level of evidence. Other interventions including neurodevelopmental therapy had low-quality evidence | It is possible for other interventions to have influenced the outcomes. Studies belonging to evidence range between I to V were studied that might have affected the outcomes. Despite the limitations, results seem reliable | Systematic review | 1− |
| Pavão et al., 201541 | Children and adolescents diagnosed with CP who are younger than 18 years of age | To systematically appraise the literature concerning effects of sensory information on postural control in children with CP | Outcome measures that evaluated postural control including force plate and surface electromyography | Eleven observational studies that fulfilled the criteria and studied the effect of sensory information on postural control in children with CP. The results showed a dearth of high-quality studies in this area and recommended further studies in this area to assess the role of sensory information on postural control during performance of functional activities | Considering the small samples and the heterogamous nature of studies considered, the conclusions of authors may be considered valid | Systematic review | 1− |
| Tinderholt Myrhaug et al., 201442 | Controlled trials that evaluated the effects of motor function and functional skill training in children with CP who are <7 years of age | To analyze the effects of intensive motor function and functional skill training in improving functional outcomes in children with CP | The activity and participation components of the ICF | Thirty-eight studies (including 29 RCTs) that included 1407 children were considered. The results factored the use of CIMT in improving outcomes | Consideration of studies with small samples and heterogeneity of interventions studied might affect the validity of results | Systematic review | 1− |
| Visicato et al., 201443 | Studies that evaluated reaching in children with CP who are <18 years of age | To evaluate the effectiveness of studies that had investigated on manual reaching | PEDI; Paediatric Reaching Test, GMFM, House Functional Classification, Melbourne Assessment of Unilateral Upper Limb Function Approach of Claeys | Seven studies were selected for this systematic review. The studies showed that children with CP show deficits in several spatio-temporal variables of reaching compared to typical children | Most studies included were of moderate quality. Hence, the results have to be interpreted with caution | Systematic review | 1− |
| Cauraugh et al., 201044 | Studies that evaluated the effectiveness of electrical stimulation in all children with CP from a mean age of 3 years to 12 years | To determine the effect of electrical stimulation on gait | Impairment and activity limitations as per the ICF | Seventeen studies that used electrical stimulation were considered for review. The studies showed medium effect sizes for electrical stimulation on gait parameters | Heterogeneous stimulation parameters, limited followup, and lack of blinded trials in this review may affect the reliability of this review | Systematic review | 1− |
| Chiu and Ada 201445 | Randomized controlled trials that evaluated children with spastic CP younger than 18 years of age. | To determine the effectiveness of functional electrical stimulation | Outcomes that measured either walking speed or GMFM | Five RCTs were included for review. Results suggest that the results of FES are similar to activity training | The results are not based on high-quality evidence | Systematic review | 1++ |
| Wright et al., 201246 | Children with CP between 1 and 16 years of age | To evaluate the effectiveness of NMES on gait or upper limb function in children with CP | Muscle strength, range of motion, and function in children with CP | Thirty studies were analyzed. The overall results were that NMES may be used to improve functional gains in children with CP | Lack of controlled trials and inclusion of small studies may affect the reliability of the results | Systematic review | 1− |
CP=Cerebral palsy, NMES=Neuromuscular electrical stimulation, GMFM=Gross Motor Function Measure, CIMT=Constraint-induced movement therapy, PEDI=Pediatric Evaluation of Disability Inventory, ICF=International Classification of Functioning, EMG=Electromyography, BOTMP=Bruininks-Oseretsky Test of Motor Proficiency, PDMS=Peabody Developmental Motor Scales, VABS=Vineland Adaptive Behavior Scales, ADL=Activities of daily living
Results
Considering the complexity and heterogeneous condition of CP, we included studies that considered children with CP of any classification and any functional ability level. The results of the search strategy are shown in Figure 1. The search yielded a total of 337 reviews, of which 18 reviews were retrieved from the Cochrane Database of Systematic Reviews and 319 from PubMed. Totally 298 articles were excluded based on the screening of their titles and abstracts; 34 articles were reviewed in full text.
Figure 1.
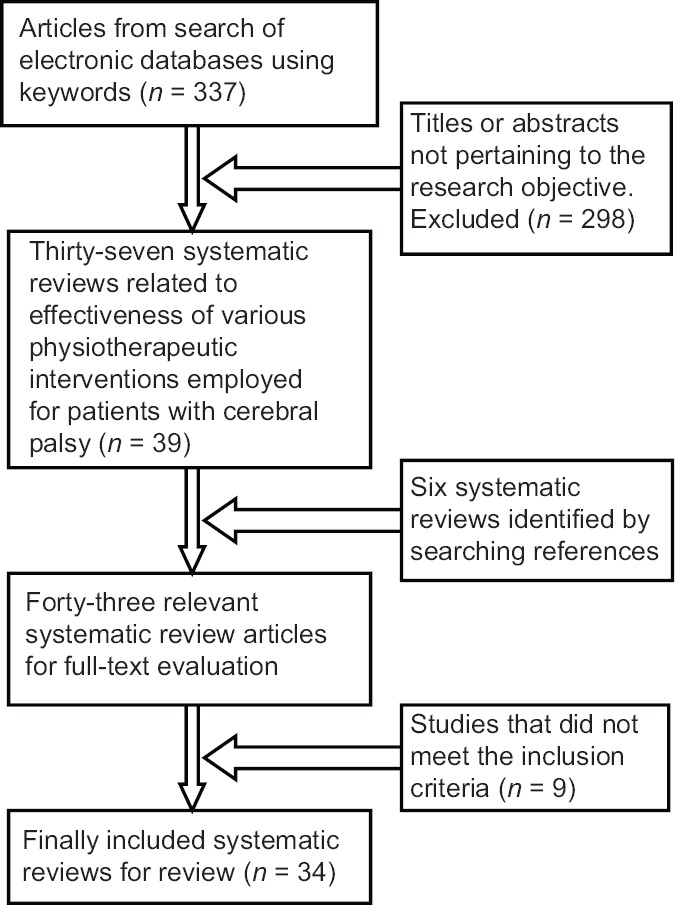
Article selection flow
An overview of the included studies is presented in Table 1. Table 2 provides a summary of the most significant findings that health care providers may wish to consider in their practice based on this review. The 34 studies included children with all types of CP classification and levels of gross and fine motor function. Out of the 34 reviews, 11 reviews appraised exercises including studies that considered processing sensory information, early intervention, upper limb training, and reaching activities. Five reviews were found that evaluated constraint induced movement therapy (CIMT); 3 reviews each on gait training, electrical stimulation, and physiotherapy in general and 2 reviews each on cardio-respiratory training and animal assisted training. Single review was identified each on whole body vibration, aquatic training, taping, passive stretching, and virtual training.
Table 2.
Most significant findings from the review
| Intensive activity-based, goal-directed interventions are more effective13,22,23,32,38 |
| The ability of manual stretching to increase range of motion and reduce spasticity is limited14 |
| There is positive support for the use of CIMT to improve the upper-extremity functioning15,16,18,42 |
| Gait speed can be improved most effectively by gait training20 |
| NDT has low-quality evidence40,47 |
| Electrical stimulation is associated with fewer functional gains44,46 |
NDT=Neurodevelopmental therapy, CIMT=Constraint-induced movement therapy
Exercises and cerebral palsy
Eleven reviews appraised the effectiveness of exercises on functional outcomes in CP. Six reviews directly evaluated the role of exercise training in CP population. Only the review by Arpino et al., 2010,22 had claimed modest evidence for the effectiveness of exercises. Results by Mockford and Caulton, 2008,26 suggested that exercises can foster functional improvement without any adverse effects. One review13 suggested that a combination of botulinum toxin and occupational therapy is more effective than occupational therapy alone in improving upper-limb outcomes and there is an overall moderate evidence to suggest that intensive activity based, goal directed interventions are effective in promoting functional outcomes.
No studied interventions have been found to be superior to another in improving trunk control and it is also not sure if improvement in postural control would lead to improvement in functional activities.29 Appraisal by Arpino et al., 2010,22 and Myrhaug et al., 2014,42 suggested that improvements may be expected from intensive exercise interventions. However, a high quality review by Scianni et al., 2009,25 reported that exercises do not improve strength or functional activities in children with CP.
The effectiveness of early interventions seems to be mixed, with Morgan et al., 2016,38 suggesting that child-initiated movement, environment modification/enrichment, and task specific training have moderate to large effect on motor outcomes (Cohen's effect size >0.7) and Hadders Algra et al., 2017,37 reporting poor effect for early interventions. However, from the evaluation of the available data, it appears that children and adolescents with CP may benefit from exercise programs that focus on lower extremity.
Exercises, gait, and cerebral palsy
A systematic review by Moreau et al., 2016,20 concluded that, among the available evidences, gait training appears to be the most effective intervention in improving gait speed in children with CP who are ambulatory. Other interventions, including strength training, have a negligible effect on gait speed and exhibit poor effectiveness. Review by Mutlu et al., 2009,28 could not conclude the effectiveness of partial bodyweight supported treadmill training in children with CP. Based on these reviews, it may be concluded that gait training alone is an effective intervention to improve gait speed in CP ambulatory children.
Constraint-induced movement therapy
Four out of the five reviews included in this review15,16,17,18 concluded that there is a definite role for CIMT to improve upper limb functions in children with CP. However, the Cochrane database, highest level of research evidence,19 reported limited evidence for the effectiveness of CIMT. Based on the results, we may conclude that there is moderate evidence for the effectiveness of CIMT on functional hand use.
Physiotherapy approaches including neurodevelopmental therapy
Reviews that had evaluated the effectiveness of commonly used physiotherapy interventions for children with CP reported that strengthening targeted muscle groups and functional training23 have the strongest evidence. These results are supported by the results of Franki et al., (2012)32 that concluded that goal oriented therapy and functional training were effective on the attainment of functional goals and participation. On the other hand, appraisal by Anttila et al., (2008)31 reported moderate evidence for the effectiveness of upper limb treatments, while the effectiveness of strength training was found limited for gross motor function.
NDT is a holistic and interdisciplinary clinical practice model that emphasizes individualized therapeutic handling based on movement analysis for habilitation and rehabilitation of individuals with neurological disorders.48 Novak et al., (2013)47 performed a systematic review of systematic reviews published on the effectiveness of NDT. Despite the widespread popularity, the authors of this review concluded the clinical evidence of NDT as poor and unfavorable.
Cardiorespiratory training and cerebral palsy
Reviews that have looked into the effects of cardiorespiratory training in children with CP have concluded that, though the training may improve aerobic fitness, the overall evidence about the effect of cardiorespiratory training in these populations is limited.21 Similar result is reflected by Rogers et al., (2008)27 that aerobic training can improve physiological outcomes, but the influence of these changes may not be translated in activity and participation domains in children with CP.
Electrical stimulation and cerebral palsy
Chiu and Ada, (2014)45 evaluated the effectiveness of functional electrical stimulation on activities in children with CP. The results of this systematic review showed that functional electrical stimulation has a similar effect as activities. Cauraugh et al., (2010)44 performed a systematic review on the effect of electrical stimulation on gait outcomes. This review identified 17 studies, and meta-analysis of the available data revealed medium effect sizes for electrical stimulation on gait outcomes. Wright et al., (2012)46 studied the performance of electrical stimulation on gait or upper-limb function in children with CP. The results of this review concluded that there is moderate evidence for electrical stimulation in improving muscle strength, range of motion, and function in children with CP. Electrical stimulation along with dynamic splinting has been shown to be further effective in improving function and posture. Though two of the three reviews showed moderate evidence for the role of electrical stimulation, these results may be subjected to study bias and we may conclude that the evidence to be limited.
Hippotherapy and cerebral palsy
Hippotherapy is commonly used to improve balance, posture, and gross and fine motor skills by placing the person on a horse's back and/or using equine movements with an objective to control the horse. Tseng et al., (2013)34 evaluated if hippotherapy or horseback riding is effective in improving the motor outcomes and body functions in children with CP. The results of the metaanalysis showed that 8–10 min of horse riding reduced asymmetrical activity of hip adductor muscles and improved postural control. However, the results showed that long term riding did not produce any statistically significant effect on improving gross motor activity status. A previous review33 had concluded that hippotherapy improved muscle symmetry in the trunk and hip, but the effectiveness was no more better compared to other therapies in improving muscle tone in children with CP. The results of this review have to be taken with caution as the methods were not properly explained and the articles considered for this review did not consider abstracts/conference proceedings and gray literature. Given the potential for error and bias and heterogeneity of interventions provided, the results may not be reliable.
Results of other studied reviews
Though the studies included in this review showed effectiveness for taping,36 aquatic therapy,35 whole-body vibration,39 virtual reality,18 and stretching,14 low quality of studies included in these reviews, multiple outcomes measured, and heterogeneity of interventions offered imply that these results have to be approached with caution.
Discussion
This study was conducted with intent to examine only the highest level of evidence by including systematic reviews or meta-analyses to provide a summary of the existing research on the effectiveness of various interventions on CP. This review of systematic reviews found that there is a lack of effectiveness in majority of the physiotherapy interventions studied. This review analyzed 34 systematic reviews on physiotherapy interventions in children with CP published after 2006. Fifteen different types of intervention categories were identified. The interventions and outcomes differed in all categories, which may limit our comparisons in the evidence synthesis.
CP is usually classified into various heterogeneous diagnostic subgroups as spastic diplegia, hemiplegia, tetraplegia, ataxic, or mixed. The study population included in this review had representations from all types of CP and it is difficult to conclude if different subtypes would respond differently to various interventions. Based on the overall results of the study, it may be concluded that intensive functional-based training will benefit this population irrespective of the type of CP.22,23 CIMT results in greater improvements in improving the functions of impaired arm in children with hemiplegic CP.15,16,18 As the goals of rehabilitation in CP are not intended at treating the primary central neurological deficit, health-care professionals shall first determine the most appropriate functional goal and then may utilize a single or combination of therapeutic approaches that are individually tailored to achieve the goals.
CIMT for upper limb recovery, goal directed/functional training, strength training for lower limb, and gait training to improve gait speed are the interventions recommended based on the available evidence. The evidences are not strong for hippotherapy, virtual training, whole body vibration, early intervention (for motor outcomes), and functional electrical stimulation. When used, these interventions should be based on clinical judgment, child and family preferences, and the child's motor control and functional abilities. Interventions such as NDT have not shown any effectiveness and may be withdrawn from standard care.
The earlier consensus that exercises in this population has to be avoided because of the adverse impact exercise on spasticity and movement patterns49 has been rebuked. Research has shown that children with CP require more energy for walking compared to healthy children.4,50 This reduced ability has been attributed to below-average aerobic and anaerobic capacity found in these populations.51,52,53 This reduced physical fitness, lower health status, and well-being lead to the development of disorders such as obesity or diabetes54,55,56 and a sedentary adulthood.57 Results of this review that cardiorespiratory training does not result in anticipated benefits are a problem for people with CP, health-care providers, and policymakers.
There are several potential limitations worth mentioning with the current review. Only PubMed and Cochrane database were searched, excluding EMBASE, Sports Discus, CINAHL, and PEDro. We did not include reviews that included children with CP along with persons suffering from other neurological disorders as part of their inclusion criteria. Similarly, we had excluded studies that included adult CP population. Another limitation is that we considered systematic reviews that had been published within the last 10 years. The search was limited to reviews published in English only because of our limited language skills. These factors might have drastically limited the numbers of systematic reviews analyzed. Further, a review of systematic reviews is a study limitation in its own right as it does not provide any new information that is not available at the first place and we have not performed any re-synthesis of the data.
Conclusion
It has been widely accepted that children with CP lack motor skills, and physiotherapy interventions should try to improve both the quantity and quality of motor control. Despite having analyzed the evidence of various techniques, it is not yet known the types of activities and/or approaches that should be encouraged and whether or not there is a need for external equipment to augment motor acquisition. Based on the results, it may be concluded that CIMT, task-oriented functional training, and gait training to be effective in this population. Other interventions have very low-quality evidence. Contrary to popular beliefs, interventions such as NDT are not backed sufficiently by evidences. Considering the importance of the role played by physiotherapy profession in the management of CP, it is of foremost importance that all clinicians involved in treating these children need to base their therapy based on the recent evidences. More research using rigorous designs is urgently needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vyas AG, Kori VK, Rajagopala S, Patel KS. Etiopathological study on cerebral palsy and its management by Shashtika Shali Pinda Sweda and Samvardhana Ghrita. Ayu. 2013;34:56–62. doi: 10.4103/0974-8520.115450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MedIndia Inc; c1997-2013. Medindia.net [homepage on the Internet]. Kathy Jones. Incidence of Cerebral Palsy Remains Constant in India on Indian Health News. [Last updated on 2010 Oct 04; Last accessed on 2013 Jan 22]. Available from: http://www.medindia.net/news/Incidence-of-Cerebral-Palsy-Remains-Constant-in-India-74912-1.htm .
- 3.Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- 4.Shamir M, Dickstein R, Tirosh E. Intensive intermittent physical therapy in infants with cerebral palsy: A randomized controlled pilot study. Isr Med Assoc J. 2012;14:737–41. [PubMed] [Google Scholar]
- 5.Dodd KJ, Taylor NF, Damiano DL. A systematic review of the effectiveness of strength-training programs for people with cerebral palsy. Arch Phys Med Rehabil. 2002;83:1157–64. doi: 10.1053/apmr.2002.34286. [DOI] [PubMed] [Google Scholar]
- 6.Fowler EG, Kolobe TH, Damiano DL, Thorpe DE, Morgan DW, Brunstrom JE, et al. Promotion of physical fitness and prevention of secondary conditions for children with cerebral palsy: Section on pediatrics research summit proceedings. Phys Ther. 2007;87:1495–510. doi: 10.2522/ptj.20060116. [DOI] [PubMed] [Google Scholar]
- 7.Damiano DL. Rehabilitative therapies in cerebral palsy: The good, the not as good, and the possible. J Child Neurol. 2009;24:1200–4. doi: 10.1177/0883073809337919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Günel MK. 1st ed. Croatia Intech Open Access Publisher, Croatia. INTECH Open Access Publisher; 2011. Physiotherapy for Children with Cerebral Palsy. Åeljka Petelin GadÅe (ed) Epilepsy in Children “Clinical and Social Aspects. [Google Scholar]
- 9.National Collaborating Centre for Women's and Children's Health (UK). Spasticity in children and young people with non-progressive brain disorders: Management of spasticity and co-existing motor disorders and their early musculoskeletal complications. London: RCOG Press; 2012. [Last accessed on 2017 Feb 24]. (NICE Clinical Guidelines, No. 145.) Available from: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0051842/pdf/PubMedHealth_PMH0051842.pdf . [PubMed] [Google Scholar]
- 10.Sewell MD, Eastwood DM, Wimalasundera N. Managing common symptoms of cerebral palsy in children. BMJ. 2014;349:g5474. doi: 10.1136/bmj.g5474. [DOI] [PubMed] [Google Scholar]
- 11.Flores-Mateo G, Argimon JM. Evidence based practice in postgraduate healthcare education: A systematic review. BMC Health Serv Res. 2007;7:119. doi: 10.1186/1472-6963-7-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence. Guideline Development Methods. [Last accessed on 2017 Jul 06]. Available from: http://www.nice.org.uk .
- 13.Sakzewski L, Ziviani J, Boyd RN. Efficacy of upper limb therapies for unilateral cerebral palsy: A meta-analysis. Pediatrics. 2013;133:e175–204. doi: 10.1542/peds.2013-0675. [DOI] [PubMed] [Google Scholar]
- 14.Pin T, Dyke P, Chan M. The effectiveness of passive stretching in children with cerebral palsy. Dev Med Child Neurol. 2006;48:855–62. doi: 10.1017/S0012162206001836. [DOI] [PubMed] [Google Scholar]
- 15.Dong VA, Tung IH, Siu HW, Fong KN. Studies comparing the efficacy of constraint-induced movement therapy and bimanual training in children with unilateral cerebral palsy: A systematic review. Dev Neurorehabil. 2013;16:133–43. doi: 10.3109/17518423.2012.702136. [DOI] [PubMed] [Google Scholar]
- 16.Huang HH, Fetters L, Hale J, McBride A. Bound for success: A systematic review of constraint-induced movement therapy in children with cerebral palsy supports improved arm and hand use. Phys Ther. 2009;89:1126–41. doi: 10.2522/ptj.20080111. [DOI] [PubMed] [Google Scholar]
- 17.Chiu HC, Ada L. Constraint-induced movement therapy improves upper limb activity and participation in hemiplegic cerebral palsy: A systematic review. J Physiother. 2016;62:130–7. doi: 10.1016/j.jphys.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Chen YP, Pope S, Tyler D, Warren GL. Effectiveness of constraint-induced movement therapy on upper-extremity function in children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2014;28:939–53. doi: 10.1177/0269215514544982. [DOI] [PubMed] [Google Scholar]
- 19.Hoare B, Imms C, Carey L, Wasiak J. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: A Cochrane systematic review. Clin Rehabil. 2007;21:675–85. doi: 10.1177/0269215507080783. [DOI] [PubMed] [Google Scholar]
- 20.Moreau NG, Bodkin AW, Bjornson K, Hobbs A, Soileau M, Lahasky K, et al. Effectiveness of rehabilitation interventions to improve gait speed in children with cerebral palsy: Systematic review and meta-analysis. Phys Ther. 2016;96:1938–54. doi: 10.2522/ptj.20150401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Butler JM, Scianni A, Ada L. Effect of cardiorespiratory training on aerobic fitness and carryover to activity in children with cerebral palsy: A systematic review. Int J Rehabil Res. 2010;33:97–103. doi: 10.1097/MRR.0b013e328331c555. [DOI] [PubMed] [Google Scholar]
- 22.Arpino C, Vescio MF, De Luca A, Curatolo P. Efficacy of intensive versus nonintensive physiotherapy in children with cerebral palsy: A meta-analysis. Int J Rehabil Res. 2010;33:165–71. doi: 10.1097/MRR.0b013e328332f617. [DOI] [PubMed] [Google Scholar]
- 23.Martin L, Baker R, Harvey A. A systematic review of common physiotherapy interventions in school-aged children with cerebral palsy. Phys Occup Ther Pediatr. 2010;30:294–312. doi: 10.3109/01942638.2010.500581. [DOI] [PubMed] [Google Scholar]
- 24.Verschuren O, Ketelaar M, Takken T, Helders PJ, Gorter JW. Exercise programs for children with cerebral palsy: A systematic review of the literature. Am J Phys Med Rehabil. 2008;87:404–17. doi: 10.1097/PHM.0b013e31815b2675. [DOI] [PubMed] [Google Scholar]
- 25.Scianni A, Butler JM, Ada L, Teixeira-Salmela LF. Muscle strengthening is not effective in children and adolescents with cerebral palsy: A systematic review. Aust J Physiother. 2009;55:81–7. doi: 10.1016/s0004-9514(09)70037-6. [DOI] [PubMed] [Google Scholar]
- 26.Mockford M, Caulton JM. Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Pediatr Phys Ther. 2008;20:318–33. doi: 10.1097/PEP.0b013e31818b7ccd. [DOI] [PubMed] [Google Scholar]
- 27.Rogers A, Furler BL, Brinks S, Darrah J. A systematic review of the effectiveness of aerobic exercise interventions for children with cerebral palsy: An AACPDM evidence report. Dev Med Child Neurol. 2008;50:808–14. doi: 10.1111/j.1469-8749.2008.03134.x. [DOI] [PubMed] [Google Scholar]
- 28.Mutlu A, Krosschell K, Spira DG. Treadmill training with partial body-weight support in children with cerebral palsy: A systematic review. Dev Med Child Neurol. 2009;51:268–75. doi: 10.1111/j.1469-8749.2008.03221.x. [DOI] [PubMed] [Google Scholar]
- 29.Chung J, Evans J, Lee C, Lee J, Rabbani Y, Roxborough L, et al. Effectiveness of adaptive seating on sitting posture and postural control in children with cerebral palsy. Pediatr Phys Ther. 2008;20:303–17. doi: 10.1097/PEP.0b013e31818b7bdd. [DOI] [PubMed] [Google Scholar]
- 30.Chen YP, Lee SY, Howard AM. Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta-analysis. Pediatr Phys Ther. 2014;26:289–300. doi: 10.1097/PEP.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 31.Anttila H, Autti-Rämö I, Suoranta J, Mäkelä M, Malmivaara A. Effectiveness of physical therapy interventions for children with cerebral palsy: A systematic review. BMC Pediatr. 2008;8:14. doi: 10.1186/1471-2431-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Franki I, Desloovere K, De Cat J, Feys H, Molenaers G, Calders P, et al. The evidence-base for conceptual approaches and additional therapies targeting lower limb function in children with cerebral palsy: A systematic review using the ICF as a framework. J Rehabil Med. 2012;44:396–405. doi: 10.2340/16501977-0984. [DOI] [PubMed] [Google Scholar]
- 33.Snider L, Korner-Bitensky N, Kammann C, Warner S, Saleh M. Horseback riding as therapy for children with cerebral palsy: Is there evidence of its effectiveness? Phys Occup Ther Pediatr. 2007;27:5–23. [PubMed] [Google Scholar]
- 34.Tseng SH, Chen HC, Tam KW. Systematic review and meta-analysis of the effect of equine assisted activities and therapies on gross motor outcome in children with cerebral palsy. Disabil Rehabil. 2013;35:89–99. doi: 10.3109/09638288.2012.687033. [DOI] [PubMed] [Google Scholar]
- 35.Roostaei M, Baharlouei H, Azadi H, Fragala-Pinkham MA. Effects of aquatic intervention on gross motor skills in children with cerebral palsy: A Systematic review. Phys Occup Ther Pediatr. 2017 Oct 20;37(5):496–515. doi: 10.1080/01942638.2016.1247938. doi: 10.1080/01942638.2016.1247938. Epub 2016 Dec 14. [DOI] [PubMed] [Google Scholar]
- 36.Güçhan Z, Mutlu A. The effectiveness of taping on children with cerebral palsy: A systematic review. Dev Med Child Neurol. 2017;59:26–30. doi: 10.1111/dmcn.13213. [DOI] [PubMed] [Google Scholar]
- 37.Hadders-Algra M, Boxum AG, Hielkema T, Hamer EG. Effect of early intervention in infants at very high risk of cerebral palsy: A systematic review. Dev Med Child Neurol. 2017;59:246–58. doi: 10.1111/dmcn.13331. [DOI] [PubMed] [Google Scholar]
- 38.Morgan C, Darrah J, Gordon AM, Harbourne R, Spittle A, Johnson R, et al. Effectiveness of motor interventions in infants with cerebral palsy: A systematic review. Dev Med Child Neurol. 2016;58:900–9. doi: 10.1111/dmcn.13105. [DOI] [PubMed] [Google Scholar]
- 39.Saquetto M, Carvalho V, Silva C, Conceição C, Gomes-Neto M. The effects of whole body vibration on mobility and balance in children with cerebral palsy: A systematic review with meta-analysis. J Musculoskelet Neuronal Interact. 2015;15:137–44. [PMC free article] [PubMed] [Google Scholar]
- 40.Dewar R, Love S, Johnston LM. Exercise interventions improve postural control in children with cerebral palsy: A systematic review. Dev Med Child Neurol. 2015;57:504–20. doi: 10.1111/dmcn.12660. [DOI] [PubMed] [Google Scholar]
- 41.Pavão SL, Silva FP, Savelsbergh GJ, Rocha NA. Use of sensory information during postural control in children with cerebral palsy: Systematic review. J Mot Behav. 2015;47:291–301. doi: 10.1080/00222895.2014.981498. [DOI] [PubMed] [Google Scholar]
- 42.Tinderholt Myrhaug H, Østensjø S, Larun L, Odgaard-Jensen J, Jahnsen R. Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC Pediatr. 2014;14:292. doi: 10.1186/s12887-014-0292-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Visicato LP, da Costa CS, Damasceno VA, de Campos AC, Rocha NA. Evaluation and characterization of manual reaching in children with cerebral palsy: A systematic review. Res Dev Disabil. 2014;36C:162–74. doi: 10.1016/j.ridd.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 44.Cauraugh JH, Naik SK, Hsu WH, Coombes SA, Holt KG. Children with cerebral palsy: A systematic review and meta-analysis on gait and electrical stimulation. Clin Rehabil. 2010;24:963–78. doi: 10.1177/0269215510371431. [DOI] [PubMed] [Google Scholar]
- 45.Chiu HC, Ada L. Effect of functional electrical stimulation on activity in children with cerebral palsy: A systematic review. Pediatr Phys Ther. 2014;26:283–8. doi: 10.1097/PEP.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 46.Wright PA, Durham S, Ewins DJ, Swain ID. Neuromuscular electrical stimulation for children with cerebral palsy: A review. Arch Dis Child. 2012;97:364–71. doi: 10.1136/archdischild-2011-300437. [DOI] [PubMed] [Google Scholar]
- 47.Novak I, McIntyre S, Morgan C, Campbell L, Dark L, Morton N, et al. Asystematic review of interventions for children with cerebral palsy: State of the evidence. Dev Med Child Neurol. 2013;55:885–910. doi: 10.1111/dmcn.12246. [DOI] [PubMed] [Google Scholar]
- 48.Instructors Group of NDTA, The NDT/Bobath (Neuro-Developmental Treatment/Bobath) Definition. NDTA Website. [Last accessed on 2017 Mar 14]. Available from: http://www.ndta.org/whatisndt.php©NDTAMay27,2016 .
- 49.Bobath K. The normal postural reflex mechanism and its deviation in children with cerebral palsy. Physiotherapy. 1971;57:515–25. [PubMed] [Google Scholar]
- 50.Levitt S. Oxford [England: Blackwell Science]: Wiley-Blackwell; 1995. Treatment of Cerebral Palsy and Motor Delay. 2010. [Google Scholar]
- 51.Lundberg A. Maximal aerobic capacity of young people with spastic cerebral palsy. Dev Med Child Neurol. 1978;20:205–10. doi: 10.1111/j.1469-8749.1978.tb15205.x. [DOI] [PubMed] [Google Scholar]
- 52.Lundberg A. Longitudinal study of physical working capacity of young people with spastic cerebral palsy. Dev Med Child Neurol. 1984;26:328–34. doi: 10.1111/j.1469-8749.1984.tb04449.x. [DOI] [PubMed] [Google Scholar]
- 53.Parker DF, Carriere L, Hebestreit H, Bar-Or O. Anaerobic endurance and peak muscle power in children with spastic cerebral palsy. Am J Dis Child. 1992;146:1069–73. doi: 10.1001/archpedi.1992.02160210071024. [DOI] [PubMed] [Google Scholar]
- 54.Balemans AC, Van Wely L, De Heer SJ, Van den Brink J, De Koning JJ, Becher JG, et al. Maximal aerobic and anaerobic exercise responses in children with cerebral palsy. Med Sci Sports Exerc. 2013;45:561–8. doi: 10.1249/MSS.0b013e3182732b2f. [DOI] [PubMed] [Google Scholar]
- 55.Hurkmans HL, van den Berg-Emons RJ, Stam HJ. Energy expenditure in adults with cerebral palsy playing Wii Sports. Arch Phys Med Rehabil. 2010;91:1577–81. doi: 10.1016/j.apmr.2010.07.216. [DOI] [PubMed] [Google Scholar]
- 56.Schuit AJ, Feskens EJ, Seidell JC. Physical activity in relation to sociodemographic variables and health status of adult men and women in Amsterdam, Doetinchem and Maastricht. Ned Tijdschr Geneeskd. 1999;143:1559–64. [PubMed] [Google Scholar]
- 57.Powell KE, Dysinger W. Childhood participation in organized school sports and physical education as precursors of adult physical activity. Am J Prev Med. 1987;3:276–81. [PubMed] [Google Scholar]


