Abstract
Fragility fractures of the pelvis (FFP) are an entity with an increasing frequency. The characteristics of these fractures are different from pelvic ring fractures in younger adults. There is a low energy instead of a high energy trauma mechanism. Due to a specific and consistent decrease of bone mineral density, typical fractures in the anterior and posterior pelvic ring occur. Bilateral sacral ala fractures are frequent. A new classification system distinguishes between four categories with increasing loss of stability. The subtypes represent different localizations of fractures. The primary goal of treatment is restoring mobility and independency. Depending on the amount of instability, conservative or surgical treatment is recommended. The operative technique should be as less invasive as possible. When the broken posterior pelvic ring is fixed operatively, a surgical fixation of the anterior pelvic ring should be considered as well. FFP Type I can be treated conservatively. In many cases, FFP Type II can also be treated conservatively. When conservative treatment fails, percutaneous fixation is performed. FFP Type III and FFP Type IV are treated operatively. The choice of the operation technique is depending on the localization of the fracture. Iliosacral screw osteosynthesis, transsacral bar osteosynthesis, transiliac internal fixation, and iliolumbar fixation are alternatives for stabilization of the posterior pelvic ring. Plate osteosynthesis, retrograde transpubic screw, and anterior internal fixation are alternatives for stabilization of the anterior pelvic ring. Postoperatively, early mobilization, with weight bearing as tolerated, is started. Simultaneously, bone metabolism is also analyzed and its defects compensated. Medical comorbidities should be identified and treated with the help of a multidisciplinary team.
Keywords: Characteristics, classification, fragility fractures pelvis, geriatric comanagement, minimally invasive, surgical fixation
Introduction
Life expectancy is high in industrialized countries. Incidence and number of old and very old persons is increasing. The risk of suffering cardiac insufficiency, peripheral arterial vascular disease, diabetes, chronic pulmonary obstructive disease, or malignancies also increases with age. Another typical age related disease is osteoporosis.1 Osteoporosis enhances the risk of suffering osteoporosis related fractures. Typical osteoporotic fractures are proximal femur, proximal humerus, distal radius, and vertebral compression fractures.2,3 Fragility fractures of the pelvis (FFP) comprise another entity.4 The incidence of FFP is increasing, whereas it is declining for osteoporotic hip fractures.5 A steep increase of incidence of FFP has been described in very old persons (age over 80) in the USA, Finland, the Netherlands, and Germany.6,7,8,9 Whereas, there are guidelines for the treatment of intra- and extracapsular hip fractures, these do not exist for FFP. The authors herewith present a new classification system, which provides a framework for analyzing FFP and is connected with recommendations for treatment of different fracture types.10
Specific Characteristics of Fragility Fractures of the Pelvis
Patients with FFP present not only in the emergency department of a hospital, but also in the out patient clinic of orthopedic surgeons, rehabilitation doctors, or geriatricians. Their main symptom is pain in the groin, in the symphyseal region, and/or at the low back or buttocks. The pain mostly is due to a recent domestic fall. Sometimes, a traumatic event is not memorable. In other patients, the pain exists since weeks or months. There is osteoporosis and there may be a history of long time cortisone intake, pelvic irradiation, or bone harvesting in the posterior pelvis for spine fusion. Pain leads to a reduction of mobility. There are no signs of hemodynamic instability or mechanical pelvic instability.11 Consequently, emergency measures are not needed.12 Nevertheless, monitoring during the first 24 h of all FFP patients is recommended as continuing bleeding with shock has been described in a small minority. Especially patients who take anticoagulants are at risk for ongoing bleeding.13 A specific and consistent decrease of bone mineral density in the sacral ala is responsible for sacral ala fractures.14 It has been shown that bone resorption may lead to “alar voids” which are areas with a complete lack of trabecular bone in the sacral ala at the level of S1 till S3.15 Sacral ala fractures are often present bilaterally, which is seldom seen in pelvic fractures of younger adults. Consequently, the fracture morphologies of FFP are not identical with high-energy pelvic fractures. Besides sacral ala fractures, fractures of the posterior ilium, and spinopelvic dissociations are seen. Fracture morphology may also change over time. Starting as a “simple” superior pubic ramus fracture, FFP may evolve toward a pelvic ring injury with higher instability. There is an insidious evolution to a complete collapse of the pelvic ring. While the pelvic ligaments remain stronger than the bony structures, displacement is restricted and no major dislocation of fracture fragments is seen.11,16
Comprehensive Classification of Fragility Fractures of the Pelvis
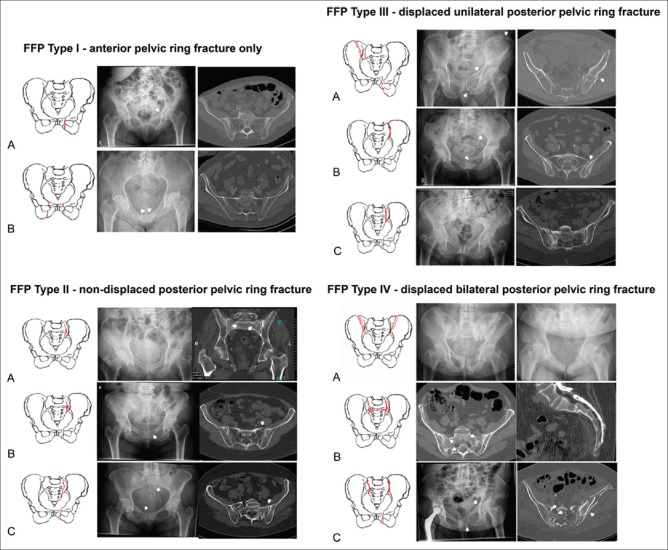
The authors developed a new classification, which provides a framework for analyzing morphology and instability of FFP.10 First criterion is loss of stability. Instability is tightly related with pain, loss of mobility, and loss of independence. It is a strong predictor for the need of operative treatment. Second criterion is the localization of the fracture [Figure 1]. Localization will be decisive for the type of surgical fixation, if needed. The classification is based on the analysis of 245 patients over the age of 65 years with FFP. All patients had conventional pelvic radiographs (AP pelvic overview, pelvic inlet, and pelvic outlet view) and a computed tomography (CT) scan. Four categories were defined.17 FFP Type I are anterior pelvic ring fractures only, FFP Type II are non-displaced posterior pelvic ring fractures with or without an anterior pelvic ring fracture, FFP Type III are unilaterally displaced posterior pelvic ring fractures, FFP Type IV are bilaterally displaced posterior pelvic ring fractures. FFP Type Ia represents a unilateral pubic ramus fracture, FFP Type Ib a bilateral pubic ramus fracture. In our series of 245 patients, FFP Type I lesions only represented 18%.10 Consequently, more than 80% had a posterior pelvic ring lesion. This data support our recommendation performing a pelvic CT scan in all patients with pubic ramus fractures on conventional pelvic X-rays. FFP Type IIa represents a non-displaced posterior pelvic ring fracture without an anterior pelvic ring fracture, FFP Type IIb a crush of the sacral ala with an anterior pelvic ring fracture, and FFP Type IIc a sacral, sacroiliac, or posterior ilium fracture with an anterior pelvic ring lesion. In our observation, this was the largest group with nearly 52%.10 FFP Type II lesions correspond with a lateral compression injury in the classifications of the Association for the Study of Internal Fixation (AO/ASIF)-Orthopaedic Trauma Association (Type 61.B2.1)18 and of Young–Burgess (LC-I)19 and are due to a fall on the side. FFP Type IIIa is a displaced posterior ilium fracture with an anterior pelvic ring fracture, FFP Type IIIb a displaced sacroiliac fracture, and FFP Type IIIc a displaced sacrum fracture with an anterior pelvic ring fracture. FFP Type III only represents 10% in our series.10 FFP Type IVa represents a bilateral displaced posterior ilium fracture, FFP Type IVb a bilateral sacral fracture (U-or H-Type sacral fracture) and FFP Type IVc a combination of posterior pelvic ring instabilities. Bilateral posterior pelvic ring fractures can or cannot be associated with anterior pelvic ring fractures also. They nevertheless remain in the same category of the classification. FFP Type IV represent 20% of all FFP and is the most unstable category.10 They represent the end result of a long process of the pelvic bone insufficiency with insidiously increasing instability, which resembles an implosion of the pelvic ring.
Figure 1.
Classification of fragility fractures of the pelvis
Goals and Methods of Treatment
The most important goal is restoring mobility and independence for activities of daily life. We, therefore, need to reduce or eliminate pain and mobilize the patient out of bed as soon as possible. While guidelines exist for the treatment of hip fractures, this is not the case for FFP. Surgical treatment is not widely accepted and there is no evidence on when and how to operate. Nevertheless, some clear recommendations can be made. Conservative treatment is acceptable when early mobilization of the patient is obtained. When mobilization is impossible, surgical stabilization should be recommended. When the decision for an operative stabilization is taken, the surgery should be as less invasive as possible. As many patients with FFP present with comorbidities and have limited physiological reserves, invasive and long lasting surgeries contain non-acceptable risks for complications and enhanced mortality. Open reduction and internal fixation through extended approaches should therefore be avoided. Restoration of anatomy is less important than restoration of stability. This practice is also used in the operative fixation of hip fractures. Shortening of the femoral neck and medialization of the femoral shaft are accepted when treating unstable trochanteric fractures with a dynamic hip screw or intramedullary device, as stability is the primary goal. Similarly, a limited malposition of fracture fragments can be accepted in FFP. The surgical procedure should be performed percutaneously whenever possible. Bridging constructs will more often be used than in high energy pelvic trauma. The fixation should provide high enough stability for early postoperative out of bed mobilization. Standing and walking with full weight bearing should be allowed when tolerated.
Besides conservative or surgical treatment, patient's general condition and bone metabolism must be analyzed and ameliorated whenever possible. This is best done in a multidisciplinary team in cooperation with a geriatrician, geriatric nurses, pain therapists, and physiotherapists. Low Vitamin D blood level is treated and intake of 1000 mg calcium daily recommended. Antiresorptive therapy should be started immediately. Bisphosphonates (Risedronate, Alendronate, Zoledronate, and Ibandronate), monoclonal antibodies (Denosumab), and teriparatide are available alternatives.20 Geriatric co-management has shown to reduce morbidity and mortality in patients with fragility fractures.21
Conservative Treatment
Conservative treatment is composed of three pillars: bed rest, pain therapy, and mobilization as tolerated. FFP Type I and FFP Type II have a limited loss of stability and can be treated without surgical intervention. Due to the additional fracture in the posterior pelvis, conservative treatment in FFP Type II will be more cumbersome than in FFP Type I. Close monitoring of the progress is indispensable. When conservative treatment fails, diagnostics should be repeated and surgical stabilization considered. FFP Type III and FFP Type IV should be treated operatively. The fractures are displaced and associated with intense pain which implicates a much longer period of bed rest when treated conservatively [Table 1].
Table 1.
Fragility fractures of the pelvis classification and recommended treatment protocol
| Type | Characteristics | Recommendation |
|---|---|---|
| FFP I | Isolated anterior pelvic ring fracture | Conservative |
| FFP II | Non-displaced posterior pelvic ring fracture | Conservative |
| Percutaneous fixation when conservative treatment fails | ||
| FFP III | Unilaterally displaced posterior pelvic ring fracture | Posterior and anterior minimal invasive fixation |
| FFP IV | Bilaterally displaced posterior pelvic ring fractures | Bilateral posterior and anterior pelvic ring fixation |
FFP=Fragility fractures of the pelvis
Bed rest is necessary until pain is under control. Complete bed rest should be kept as short as possible. Periods of prolonged bed rest are associated with muscle weakness and postural hypotension in geriatric patients and bear a higher risk of complications such as decubitus, ulcers, deep vein thrombosis, pulmonary embolism, and urinary tract infection. It also increases delirium, anxiety, and depression. Breuil et al. noticed complications in 52.5% patients during hospitalization of 60 patients with an osteoporotic pelvic fracture, of which urinary tract infections (50%), bedsores (33%), and alteration of cognitive functions (18%) were the most frequent.22 Breathing exercises and assisted physiotherapy such as careful mobilization of the extremities and motion of large joints needs to be started with the patient in bed. Sitting in the upright position helps breathing and ameliorates spatial orientation and patient's independency. Pain therapy accompanies bed rest and early physiotherapy. Centrally working analgesics are preferred over peripherally working drugs, as the last negatively influence bone healing. A combination of paracetamol and opioids has shown to be effective in our experience. When pain subsides, gradual out of bed mobilization is started. The patient is placed sitting at the bedside first, then standing with the help of a physiotherapist and with crutches, a walking frame or a rollator. Consecutively, small transfers from the bed to the dining table or lavatory are exercised. Finally, longer distances in the floor of the ward, even with steps can be covered. All exercises are meant to regain mobility and independency rather than improving muscle force or motion of single joints.23 Length of hospital stay with conservative treatment has been described to be between 21 and 45 days.24,25 Patients, who were not independent before the fracture occurred, need a longer hospital stay than patients, who were completely independent. Most patients do not return to their previous level of activity.26
Operative Procedure
In FFP Type III and FFP Type IV, surgical fixation is recommended. Some patients with FFP Type II will also need operative stabilization when conservative therapy is not successful.16
In geriatric patients, there is a higher risk of perioperative complications because of limited physiologic reserves and due to delayed and limited reactions to severe blood loss or hypothermia. Consequently, surgery should be as less invasive as possible. Principles of osteosynthesis, which are followed in younger adults, must be adapted in elderly patients. Original principles are anatomical reduction, rigid fixation, early mobilization, and soft-tissue care. In geriatric patients, these principles have to be adapted as follows: minimally invasive surgical intervention, stable fixation, early mobilization, as good as possible reduction. Anatomic reduction is not crucial anymore. Stable fixation with a minimally invasive intervention becomes the treatment of choice.
FFP II have non-displaced, FFP III and FFP IV have displaced posterior pelvic ring fractures. The extent of displacement is limited. This is because the ligaments are not disrupted and remain attached to the fracture fragments. Little fracture displacement enables the use of bony corridors such as the transsacral and anterior column corridor for fracture fixation through percutaneous procedures or small incisions.27 Stable fixation can be obtained by different surgical techniques.
The Posterior Pelvic Ring
Iliosacral screw osteosynthesis is a universally accepted technique for the fixation of sacral fractures, iliosacral dislocations, and fracture dislocations. Iliosacral screws are inserted percutaneously and provide an adequate stability for sacral ala fractures.28 Partially threaded screws provide interfragmentary compression when tightened. Fully threated screws function as positioning screws. The screws can be inserted in the S1 and S2 iliosacral space. Two screws provide higher stability than one. A thorough preoperative analysis of the morphology of the upper sacrum is indispensable.29 In dysmorphic sacra, the space for iliosacral screw insertion is smaller. The direction of the screws has to be adapted: screws start more posteriorly and distally and are directed toward anterior and superior. In non-dysmorphic sacra, the screws are placed horizontally, exactly in the coronal plane.30,31
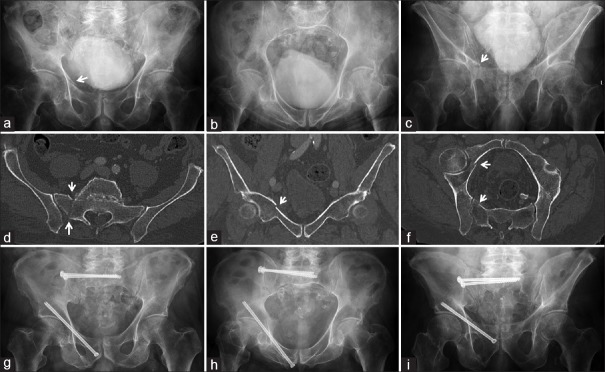
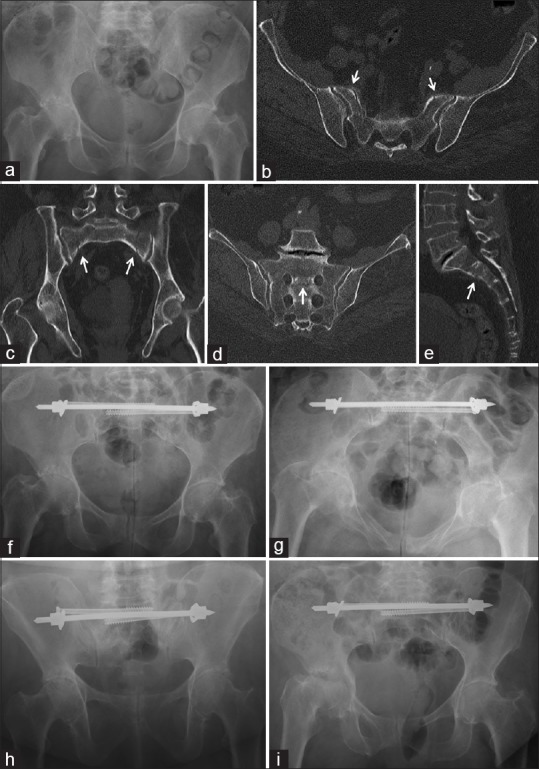
An important complication of iliosacral screw fixation in geriatric patients is screw loosening. Wagner et al. showed that the decrease in bone mineral density in the sacrum follows a consistent pattern.15 There is a more pronounced decrease in the sacral ala than in the sacral body. Decrease of bone mineral density is more pronounced in S2 than in S1.32 To prevent screw loosening, long screws, which reach the opposite sacral ala should be inserted [Figure 2a–i].33
Figure 2.
A 70-year-old male suffered a fall. (a) AP pelvic X-ray: right pubic ramus fracture (arrow). (b) Pelvic inlet. (c) Pelvic outlet: pubic ramus fracture (arrow). (d) Axial computed tomography: fracture of the right sacral ala (arrows). (e) Coronal computed tomography: superior pubic ramus fracture (arrow). (f) Oblique computed tomography reconstruction: fractures at anterior and posterior pelvis (arrows). It concerns a fragility fractures of the pelvis Type IIc. (g) AP pelvic X-ray after 3 months. Sacral fracture was stabilized with two iliosacral screws, pubic ramus fracture with long retrograde transpubic screw. (h) Pelvic inlet. (i) Pelvic outlet
Cement augmentation provides a stronger anchorage of the iliosacral screws in trabecular bone. The cement is inserted at the tip of the screw. Cannulated screws with special perforations are used. A few cc of cement is sufficient; larger amounts are associated with a higher risk of cement leakage. The cement interdigitates with the trabecular bone and provides enhanced stability of the bone-cement-implant construct.34,35,36
Sacroplasty is an alternative technique for sacral fracture fixation. The technique is derived from vertebro- and kyphoplasty. Cement is injected in the fracture site of the sacral ala. There is an immediate pain relief due to restoration of stability. Indications are mostly derived from magnetic resonance imaging – findings in patients with low back pain or pain in the buttock: bone bruise in the sacrum represents the onset of a fracture in the trabecular bone. The fracture is not yet visible on conventional X-rays and in pelvic CT. There is no interruption of the anterior or posterior sacral cortex. There is a high risk of cement leakage through the cortical fracture gap when sacroplasty is done in patients with a complete sacral fracture. While, Kortman37 reports only one cement extravasation out of 243 procedures (0.4%), there were 9 from 33 patients with cement leakage (27%) in the series of Bastian et al.38 Cement may hinder fracture healing and complicate revision surgery in case of recurrent fractures. We, therefore, do not recommend sacroplasty in patients with complete sacral fractures and prefer stabilization techniques with metal implants.
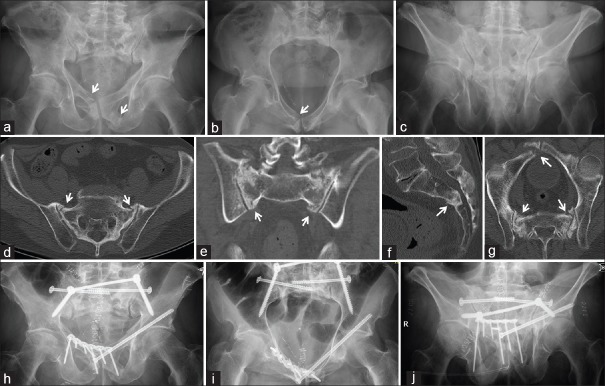
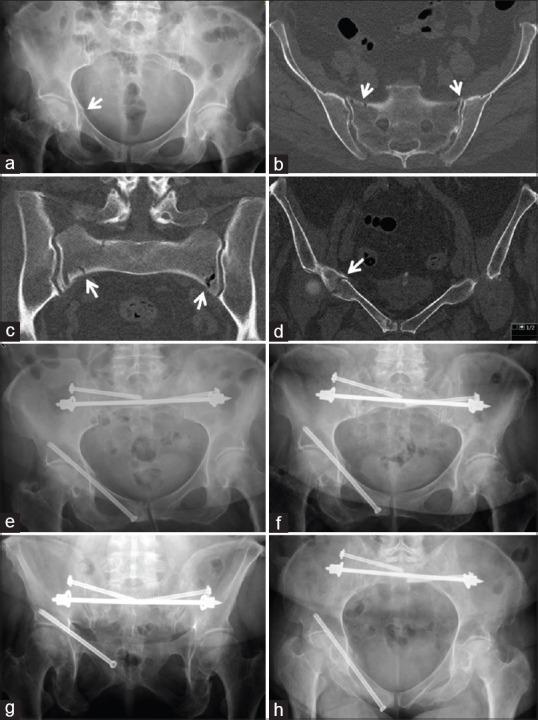
Transiliac bridging osteosynthesis is another technique for fixation of posterior pelvic ring fractures. The construct connects the left and right posterior ilium behind the sacral body. The implant can be a bridging plate with screws or an internal fixator. The shape of the plate must be adapted to the anatomy of the posterior ilium. The plate is located at the level of the posterior inferior iliac spines. The plate is inserted through two short incisions and a subcutaneous tunnel between them. Several screws attach the plate with the posterior ilium. When an angular stable construct is used, higher stability can be obtained.39 Alternatively, one long and large diameter pedicle screw is inserted from the posterior superior iliac spine toward the anterior inferior iliac spine on each side. The screw heads are connected with a transverse bar, which is inserted subcutaneously. The construct bears the name of transiliac internal fixator.40 The posterior bridging plate and transiliac internal fixator provide high stability in the broken posterior pelvis. Bilateral fractures can be stabilized. As the implant is situated behind the sacrum, there is no risk of neurological damage. Prominent parts may however cause discomfort. The posterior bridging plate or transiliac internal fixator can be combined with iliosacral screw osteosynthesis or augmented with cement [Figure 3a–j].41
Figure 3.
A 76-year-old male with pelvic irradiation after prostatectomy. (a) AP pelvic X-ray: bilateral pubic ramus fractures (arrows). (b) Pelvic inlet. (c) Pelvic outlet. (d) Axial computed tomography: bilateral sacral ala fractures (arrows). (e) Coronal computed tomography. (f) Sagittal computed tomography: horizontal fracture between S2 and S3. It concerns a fragility fractures of the pelvis Type IVb. (g) Oblique computed tomography with all fractures. (h) Postoperative pelvic X-ray. Transiliac internal fixation and two iliosacral screws for the posterior pelvis, retrograde transpubic screw for the left, plate and screws for the right anterior fracture. (i) Pelvic inlet. (j) Pelvic outlet
Transsacral bar osteosynthesis is another less invasive technique for stabilization of the posterior pelvic ring. The bar is inserted through the transsacral corridor of S1. Two small incisions at the buttocks, which are in line with the transsacral corridor, are needed. The implant is a long, threaded bar with a diameter of 6 mm. After insertion, washers and nuts are mounted on each side of the bar. Tightening the nuts puts compression on the vertical sacral fractures.42 Bilateral sacral fractures can be stabilized with one construct. Stability is not depending on the density of the trabecular bone in the sacrum but on the strength of the outer cortex of the posterior ilium. The insertion procedure is less invasive. The construct can be combined with iliosacral screws or other implants [Figures 4a–i and 5a–h]. Transsacral bar osteosynthesis is not possible in all patients. The morphology of the upper sacrum is very variable and transsacral corridor may be too small or non-existing.43 A thorough preoperative analysis of CT data of the upper sacrum in several planes is indispensable. Although no large series has been published so far, existing experience is promising with low complication rate and high stability, enabling quick rehabilitation.44
Figure 4.
A 65-year-old female with 8 months of intense pain. (a) Normal AP pelvis X-ray. (b) Axial computed tomography: bilateral sacral ala fractures (arrows). (c) Coronal computed tomography: bilateral sacral ala fractures (arrows). (d) Oblique computed tomography: Fracture between left and right S1-neuroforamen (arrow). (e) Sagittal midline computed tomography: horizontal fracture between S1 and S2 (arrow). It concerns a fragility fractures of the pelvis Type IVb. (f) Postoperative AP pelvic X-ray. Fractures were stabilized with transsacral bar and two iliosacral screws. (g) Pelvic inlet. (h) Pelvic outlet. (i) AP pelvic X-ray 2 years later showing the right acetabular fracture
Figure 5.
A 75-year-old female suffered a domestic fall. (a) AP pelvic X-ray: right superior pubic ramus fracture. (b) Transverse computed tomography: bilateral sacral ala fractures. (c) Coronal computed tomography: bilateral sacral ala fracture. (d) Coronal computed tomography: superior pubic ramus fracture on the right. It concerns a fragility fracture of the pelvis Type IIC. (e) Postoperative AP pelvic X-ray: transsacral bar, two iliosacral screws, and retrograde transpubic screw. (f) Pelvic inlet. (g) Pelvic outlet. (h) AP pelvic X-ray after 3 months. Bridging callus at the pubic ramus fracture
Lumbopelvic fixation is a technique, in which the vertebral body of L4 and/or L5 is connected with the posterior ilium. One pedicle screw is inserted in L4 or L5, another pedicle screw in the posterior superior iliac spine and is directed toward the anterior inferior iliac spine. The heads of the pedicle screws are connected with a 5 mm bar. The pedicle screw in L4 or L5 has a diameter of 5 mm and a length of up to 50 mm, the pedicle screw in the ilium has a diameter of 8 mm and a length of up to 100 mm. A transverse connector joins the left with the right side.45,46 The construct has a bridging principle. Best indications are U- or H-type fractures of the sacrum (FFP Type IVb) with intrusion of the lumbosacral segment into the small pelvis. Further vertical displacement is prevented. The pedicle screws can be inserted through small incisions and the connecting bars through subcutaneous tunnels. Lumbopelvic fixation can be combined with iliosacral screws, forming a “triangular osteosynthesis.” The last has been described for reduction and fixation of vertically unstable fractures in high-energy pelvic trauma.47
The Anterior Pelvic Ring
When surgical fixation of the posterior pelvic ring is performed, surgical fixation of the fracture(s) of the anterior pelvic ring must be considered during the same operative procedure. In our series of 245 patients, more than 80% had a combination of posterior and anterior pelvic ring fractures.10 The ultimate goal of surgery is restoring high stability in the whole fractured pelvic ring. This is not realized when only the posterior pelvis is fixed. Mobilizing the patient will induce motion in the anterior fracture. This hinders fracture healing anteriorly and presents a strain for the posterior fixation with enhanced risk of implant loosening or failure.
Principles of surgical treatment of the anterior pelvis are similar to those of fixation of the posterior pelvis i.e., surgery should be as less invasive as possible and should provide high stability. Anatomical reduction is less important although large fracture gaps should not be accepted.
External fixation is widely accepted for stabilizing unstable pelvic ring lesions. It is used for provisional stabilization of high-energy pelvic disruptions.48,49 In FFP, external fixation is more cumbersome than in younger adults. Fixation time is several weeks instead of several days. Due to reduction of bone mineral density, strength of anchorage of the pins is lower with higher risk of pin loosening. In obese patients, there is a high risk of wound breakdown and pin-track infection. Moreover, there may be a mechanical conflict between the connecting bars and the abdominal wall. Motion of the hip joints is reduced to 90°, which hinders sitting. We therefore do not recommend external fixation as a definitive fixation of anterior pelvic ring fractures in FFP.50
Retrograde transpubic screw fixation is an effective and minimally invasive technique. Optimal indications are fractures of the superior pubic ramus and of the anterior lip of the acetabulum. The screw is inserted in the anterior column corridor, its entry portal being at the pubic tubercle. The screw passes the acetabulum medially and superiorly without penetrating the joint.51 The screw may have a diameter of 7.3 mm and a length of up to 140 mm. The screw reaches its highest fixation strength and stability, when its tip passes the outer cortex of the ilium body, just above the acetabulum [Figures 2a–h, 3a–j, and 5a–h].52,53 In bilateral lesions, retrograde transpubic screw fixation can be performed on both sides.
Anterior internal fixation is the internal counterpart of anterior external fixation. Two pedicle screws are inserted through small skin incisions from the anterior inferior iliac spines toward the posterior superior iliac spines. The screw heads are connected with a long curved bar, which is passed through a subcutaneous corridor.54 The connecting bar can be felt under the skin and should, therefore, be removed after fracture healing. Care should be taken not to damage the lateral cutaneous femoral nerve, which runs very near to the anterior inferior iliac spines.55 When inserting the screw heads and the connecting bar too deep, there is a risk of direct pressure of the bar on the iliopsoas muscle and femoral nerve.56
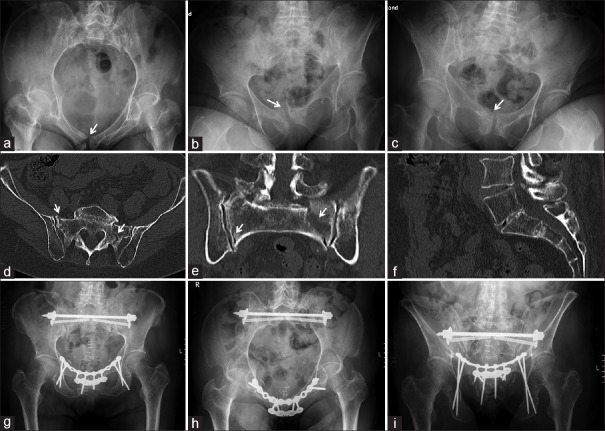
Plate and screw osteosynthesis is a valid but not minimal-invasive technique for fixation of fractures of the anterior pelvic ring. Pubic symphysis and anterior pelvic ring are exposed through a vertical midline incision or through a Pfannenstiel approach. Best indications for plate osteosynthesis are fractures of the pubic bone near to the symphysis, bilateral and largely displaced fractures of the anterior pelvic ring; and instabilities of the pubic symphysis. In such cases, only plate and screw osteosynthesis can provide the stability needed for uneventful healing.57,58 The plate bridges the pubic symphysis. The screws which are placed in the marginal holes of the plate use the infra-acetabular corridor. This enables the use of very long screws (up to 100 mm) and gives the construct a much higher stability, preventing loosening or implant failure with secondary fracture dislocation.59 In case of chronic instabilities or bone defects, which have to be filled up with bone grafts, a double-plate osteosynthesis is recommended, providing the security of a high stability for a long period of time, which is needed for fracture healing in these specific situations [Figure 6a–i].
Figure 6.
A 74-year-old female with pelvic pain. (a) AP pelvic X-ray: right pubic bone fracture (arrow). (b) Right one-leg stand: vertical instability of pubic symphysis (arrow). (c) Left one-leg stand confirms instability (arrow). (d) Axial computed tomography: bilateral sacral ala fractures (arrows). (e) Coronal computed tomography: same fractures. (f) Mid-sagittal computed tomography: normal. (g) Postoperative AP pelvic X-ray: transsacral bar and two iliosacral screws posteriorly, two plates and screws anteriorly. Marginal screws of the upper plate use infraacetabular corridor, anterior plate is angular stable. (h) Pelvic inlet. (i) Pelvic outlet
Conclusion
FFP are an emerging entity in the old and very old segment of our populations. They exhibit specific characteristics, which are not present in pelvic ring disruptions of the younger population. A new, comprehensive classification provides a frame for analyzing the morphology and degree of instability of FFP. To date, there is no consensus about the optimal treatment regimen of patients with FFP. A multidisciplinary geriatric comanagement, including treatment of comorbidities and starting prevention of secondary fractures, helps reducing morbidity and mortality. The goal of in-hospital treatment is reducing pain and regaining early mobility and independency for activities of daily life. Surgical fixation is an important pillar of treatment.60 The surgery should be as less invasive as possible and provide the stability needed for early mobilization and uneventful healing. Perfect fracture reduction is less important. There are several fixation techniques of iliosacral screw fixation, sacroplasty, transiliac bridging osteosynthesis, transsacral bar osteosynthesis, and lumbopelvic fixation for fractures of the posterior pelvic ring, which use different principles as compression, buttressing, and bridging. They have their specific advantages and limitations and may be used alternatively for the fixation of different fracture configurations. When a combination of an anterior with a posterior pelvic ring fracture exists, fixation of both locations of instability is recommended. Less invasive fixation techniques like anterior external fixation, anterior internal fixation, and retrograde transpubic screw fixation are also available for anterior pelvic ring fractures. In highly unstable FFP, a combination of fixation methods for the posterior pelvic ring and plate and screws osteosynthesis of the anterior pelvic ring provide the highest stability. There is little evidence about the outcome of patients with FFP at present. More clinical and biomechanical work is needed to shed light on the specific challenges and optimal management of patients with FFP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European union: Medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 3.Watts NB. The fracture risk assessment tool (FRAX®): Applications in clinical practice. J Womens Health (Larchmt) 2011;20:525–31. doi: 10.1089/jwh.2010.2294. [DOI] [PubMed] [Google Scholar]
- 4.Rommens PM, Wagner D, Hofmann A. Surgical management of osteoporotic pelvic fractures: A new challenge. Eur J Trauma Emerg Surg. 2012;38:499–509. doi: 10.1007/s00068-012-0224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: Divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014;37:151–7. doi: 10.3928/01477447-20140225-50. [DOI] [PubMed] [Google Scholar]
- 6.Buller LT, Best MJ, Quinnan SM. A nationwide analysis of pelvic ring fractures: Incidence and trends in treatment, length of stay, and mortality. Geriatr Orthop Surg Rehabil. 2016;7:9–17. doi: 10.1177/2151458515616250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kannus P, Parkkari J, Niemi S, Sievänen H. Low-trauma pelvic fractures in elderly Finns in 1970-2013. Calcif Tissue Int. 2015;97:577–80. doi: 10.1007/s00223-015-0056-8. [DOI] [PubMed] [Google Scholar]
- 8.Nanninga GL, de Leur K, Panneman MJ, van der Elst M, Hartholt KA. Increasing rates of pelvic fractures among older adults: The Netherlands, 1986-2011. Age Ageing. 2014;43:648–53. doi: 10.1093/ageing/aft212. [DOI] [PubMed] [Google Scholar]
- 9.Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C, et al. Epidemiology of pelvic fractures In Germany: Considerably high incidence rates among older people. PLoS One. 2015;10:e0139078. doi: 10.1371/journal.pone.0139078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 2013;44:1733–44. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 11.Rommens PM, Wagner D, Hofmann A. Fragility fractures of A the pelvis. JBJS Rev. 2017;5 doi: 10.2106/JBJS.RVW.16.00057. pii: 01874474-201703000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Rommens PM, Hofmann A, Hessmann MH. Management of acute hemorrhage in pelvic trauma: An overview. Eur J Trauma Emerg Surg. 2010;36:91–9. doi: 10.1007/s00068-010-1061-x. [DOI] [PubMed] [Google Scholar]
- 13.Dietz SO, Hofmann A, Rommens PM. Haemorrhage in fragility fractures of the pelvis. Eur J Trauma Emerg Surg. 2015;41:363–7. doi: 10.1007/s00068-014-0452-1. [DOI] [PubMed] [Google Scholar]
- 14.Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976) 2009;34:309–15. doi: 10.1097/BRS.0b013e318191ea01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM, et al. Sacral bone mass distribution assessed by averaged three-dimensional CT models: Implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am. 2016;98:584–90. doi: 10.2106/JBJS.15.00726. [DOI] [PubMed] [Google Scholar]
- 16.Rommens PM, Ossendorf C, Pairon P, Dietz SO, Wagner D, Hofmann A, et al. Clinical pathways for fragility fractures of the pelvic ring: Personal experience and review of the literature. J Orthop Sci. 2015;20:1–1. doi: 10.1007/s00776-014-0653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rommens PM, Hofmann A. Fragility fractures of the pelvis. In: Bentley G, editor. European Instructional Lectures. Vol. 15. Berlin Heidelberg: Springer; 2015. pp. 109–23. [Google Scholar]
- 18.Fracture and dislocation compendium. Orthopaedic trauma association committee for coding and classification. J Orthop Trauma. 1996;10(Suppl 1):v–ix. 1-154. [PubMed] [Google Scholar]
- 19.Dalal SA, Burgess AR, Siegel JH, Young JW, Brumback RJ, Poka A, et al. Pelvic fracture in multiple trauma: Classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:981–1000. [PubMed] [Google Scholar]
- 20.Peichl P, Holzer LA, Maier R, Holzer G. Parathyroid hormone 1-84 accelerates fracture healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011;93:1583–7. doi: 10.2106/JBJS.J.01379. [DOI] [PubMed] [Google Scholar]
- 21.Bukata SV, Digiovanni BF, Friedman SM, Hoyen H, Kates A, Kates SL, et al. A guide to improving the care of patients with fragility fractures. Geriatr Orthop Surg Rehabil. 2011;2:5–37. doi: 10.1177/2151458510397504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breuil V, Roux CH, Testa J, Albert C, Chassang M, Brocq O, et al. Outcome of osteoporotic pelvic fractures: An underestimated severity. Survey of 60 cases. Joint Bone Spine. 2008;75:585–8. doi: 10.1016/j.jbspin.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 23.Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: To ambulate or not to ambulate? Am J Phys Med Rehabil. 2000;79:404–9. doi: 10.1097/00002060-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Morris RO, Sonibare A, Green DJ, Masud T. Closed pelvic fractures: Characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad Med J. 2000;76:646–50. doi: 10.1136/pmj.76.900.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taillandier J, Langue F, Alemanni M, Taillandier-Heriche E. Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Joint Bone Spine. 2003;70:287–9. doi: 10.1016/s1297-319x(03)00015-0. [DOI] [PubMed] [Google Scholar]
- 26.Soles GL, Ferguson TA. Fragility fractures of the pelvis. Curr Rev Musculoskelet Med. 2012;5:222–8. doi: 10.1007/s12178-012-9128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rommens PM. Is there a role for percutaneous pelvic and acetabular reconstruction? Injury. 2007;38:463–77. doi: 10.1016/j.injury.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 28.Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury. 2015;46:1631–6. doi: 10.1016/j.injury.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 29.Conflitti JM, Graves ML, Chip Routt ML., Jr Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma. 2010;24:630–6. doi: 10.1097/BOT.0b013e3181dc50cd. [DOI] [PubMed] [Google Scholar]
- 30.Eastman JG, Routt ML., Jr Correlating preoperative imaging with intraoperative fluoroscopy in iliosacral screw placement. J Orthop Traumatol. 2015;16:309–16. doi: 10.1007/s10195-015-0363-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML., Jr Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma. 2010;24:622–9. doi: 10.1097/BOT.0b013e3181cf0404. [DOI] [PubMed] [Google Scholar]
- 32.Bastian JD, Bergmann M, Schwyn R, Keel MJ, Benneker LM. Assessment of the breakaway torque at the posterior pelvic ring in human cadavers. J Invest Surg. 2015;28:328–33. doi: 10.3109/08941939.2015.1016249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao Y, Li J, Wang D, Liu Y, Tan J, Zhang S. Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury. 2012;43:490–4. doi: 10.1016/j.injury.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 34.Wähnert D, Raschke MJ, Fuchs T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum: A new method using modified implants. Int Orthop. 2013;37:1147–50. doi: 10.1007/s00264-013-1875-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oberkircher L, Masaeli A, Bliemel C, Debus F, Ruchholtz S, Krüger A. Primary stability of three different iliosacral screw fixation techniques in osteoporotic cadaver specimens-a biomechanical investigation. Spine J. 2016;16:226–32. doi: 10.1016/j.spinee.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 36.König MA, Hediger S, Schmitt JW, Jentzsch T, Sprengel K, Werner CM. In-screw cement augmentation for iliosacral screw fixation in posterior ring pathologies with insufficient bone stock. Eur J Trauma Emerg Surg. 2018;44:203–10. doi: 10.1007/s00068-016-0681-6. [DOI] [PubMed] [Google Scholar]
- 37.Kortman K, Ortiz O, Miller T, Brook A, Tutton S, Mathis J, et al. Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficiency fractures or pathologic sacral lesions. J Neurointerv Surg. 2013;5:461–6. doi: 10.1136/neurintsurg-2012-010347. [DOI] [PubMed] [Google Scholar]
- 38.Bastian JD, Keel MJ, Heini PF, Seidel U, Benneker LM. Complications related to cement leakage in sacroplasty. Acta Orthop Belg. 2012;78:100–5. [PubMed] [Google Scholar]
- 39.Kobbe P, Hockertz I, Sellei RM, Reilmann H, Hockertz T. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop. 2012;36:159–64. doi: 10.1007/s00264-011-1279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dienstknecht T, Berner A, Lenich A, Nerlich M, Fuechtmeier B. A minimally invasive stabilizing system for dorsal pelvic ring injuries. Clin Orthop Relat Res. 2011;469:3209–17. doi: 10.1007/s11999-011-1922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmitz P, Baumann F, Grechenig S, Gaensslen A, Nerlich M, Müller MB. The cement-augmented transiliacal internal fixator (caTIFI): An innovative surgical technique for stabilization of fragility fractures of the pelvis. Injury. 2015;46(Suppl 4):S114–20. doi: 10.1016/S0020-1383(15)30029-2. [DOI] [PubMed] [Google Scholar]
- 42.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury. 2012;43:446–51. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 43.Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Hofmann A, et al. Morphometry of the sacrum and its implication on trans-sacral corridors using a computed tomography data-based three-dimensional statistical model. Spine J. 2017;17:1141–7. doi: 10.1016/j.spinee.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 44.Vanderschot P, Kuppers M, Sermon A, Lateur L. Trans-iliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J Orthop. 2009;43:245–52. doi: 10.4103/0019-5413.53454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML, Jr, Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–57. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]
- 46.Roetman B, Schildhauer TA. Lumbopelvic stabilization for bilateral lumbosacral instabilities: Indications and techniques. Unfallchirurg. 2013;116:991–9. doi: 10.1007/s00113-012-2338-1. [DOI] [PubMed] [Google Scholar]
- 47.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: A new concept allowing early weight-bearing. J Orthop Trauma. 1998;12:307–14. doi: 10.1097/00005131-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Bircher MD. Indications and techniques of external fixation of the injured pelvis. Injury. 1996;27(Suppl 2):B3–19. [PubMed] [Google Scholar]
- 49.Gänsslen A, Hildebrand F, Kretek C. Supraacetabular external fixation for pain control in geriatric type B pelvic injuries. Acta Chir Orthop Traumatol Cech. 2013;80:101–5. [PubMed] [Google Scholar]
- 50.Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. doi: 10.1016/j.injury.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 51.Suzuki T, Soma K, Shindo M, Minehara H, Itoman M. Anatomic study for pubic medullary screw insertion. J Orthop Surg (Hong Kong) 2008;16:321–5. doi: 10.1177/230949900801600311. [DOI] [PubMed] [Google Scholar]
- 52.Simonian PT, Routt ML, Jr, Harrington RM, Tencer AF. Internal fixation of the unstable anterior pelvic ring: A biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J Orthop Trauma. 1994;8:476–82. [PubMed] [Google Scholar]
- 53.Starr AJ, Nakatani T, Reinert CM, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: What predicts fixation failure? J Orthop Trauma. 2008;22:81–7. doi: 10.1097/BOT.0b013e318162ab6e. [DOI] [PubMed] [Google Scholar]
- 54.Hiesterman TG, Hill BW, Cole PA. Surgical technique: A percutaneous method of subcutaneous fixation for the anterior pelvic ring: The pelvic bridge. Clin Orthop Relat Res. 2012;470:2116–23. doi: 10.1007/s11999-012-2341-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Apivatthakakul T, Rujiwattanapong N. “Anterior subcutaneous pelvic internal fixator (INFIX), is it safe?” A cadaveric study. Injury. 2016;47:2077–80. doi: 10.1016/j.injury.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 56.Hesse D, Kandmir U, Solberg B, Stroh A, Osgood G, Sems SA, et al. Femoral nerve palsy after pelvic fracture treated with INFIX: A case series. J Orthop Trauma. 2015;29:138–43. doi: 10.1097/BOT.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 57.Gras F, Marintschev I, Schwarz CE, Hofmann GO, Pohlemann T, Culemann U. Screw- versus plate-fixation strength of acetabular anterior column fractures: A biomechanical study. J Trauma Acute Care Surg. 2012;72:1664–70. doi: 10.1097/TA.0b013e3182463b45. [DOI] [PubMed] [Google Scholar]
- 58.Acklin YP, Zderic I, Buschbaum J, Varga P, Inzana JA, Grechenig S. Biomechanical comparison of plate and screw fixation in anterior pelvic ring fractures with low bone mineral density. Injury. 2016;47:1456–60. doi: 10.1016/j.injury.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 59.Culemann U, Marintschev I, Gras F, Pohlemann T. Infra-acetabular corridor – Technical tip for an additional screw placement to increase the fixation strength of acetabular fractures. J Trauma. 2011;70:244–6. doi: 10.1097/TA.0b013e3181f45f91. [DOI] [PubMed] [Google Scholar]
- 60.Rommens PM, Dietz SO, Ossendorf C, Pairon P, Wagner D, Hofmann A. Fragility fractures of the pelvis: Should they be fixed? Acta Chir Orthop Traumatol Cech. 2015;82:101–12. [PubMed] [Google Scholar]