Abstract
Background
Urinary incontinence in women is associated with poor quality of life and difficulties in social, psychological and sexual functioning. The condition may affect up to 15% of middle‐aged or older women in the general population. Conservative treatments such as lifestyle interventions, bladder training and pelvic floor muscle training (used either alone or in combination with other interventions) are the initial approaches to the management of urinary incontinence. Many women are interested in additional treatments such as yoga, a system of philosophy, lifestyle and physical practice that originated in ancient India.
Objectives
To assess the effects of yoga for treating urinary incontinence in women.
Search methods
We searched the Cochrane Incontinence and Cochrane Complementary Medicine Specialised Registers. We searched the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) and ClinicalTrials.gov to identify any ongoing or unpublished studies. We handsearched Proceedings of the International Congress on Complementary Medicine Research and the European Congress for Integrative Medicine. We searched the NHS Economic Evaluation Database for economic studies, and supplemented this search with searches for economics studies in MEDLINE and Embase from 2015 onwards. Database searches are up‐to‐date as of 21 June 2018.
Selection criteria
Randomised controlled trials in women diagnosed with urinary incontinence in which one group was allocated to treatment with yoga.
Data collection and analysis
Two review authors independently screened titles and abstracts of all retrieved articles, selected studies for inclusion, extracted data, assessed risk of bias and evaluated the certainty of the evidence for each reported outcome. Any disagreements were resolved by consensus. We planned to combine clinically comparable studies in Review Manager 5 using random‐effects meta‐analysis and to carry out sensitivity and subgroup analyses. We planned to create a table listing economic studies on yoga for incontinence but not carry out any analyses on these studies.
Main results
We included two studies (involving a total of 49 women). Each study compared yoga to a different comparator, therefore we were unable to combine the data in a meta‐analysis. A third study that has been completed but not yet fully reported is awaiting assessment.
One included study was a six‐week study comparing yoga to a waiting list in 19 women with either urgency urinary incontinence or stress urinary incontinence. We judged the certainty of the evidence for all reported outcomes as very low due to performance bias, detection bias, and imprecision. The number of women reporting cure was not reported. We are uncertain whether yoga results in satisfaction with cure or improvement of incontinence (risk ratio (RR) 6.33, 95% confidence interval (CI) 1.44 to 27.88; an increase of 592 from 111 per 1000, 95% CI 160 to 1000). We are uncertain whether there is a difference between yoga and waiting list in condition‐specific quality of life as measured on the Incontinence Impact Questionnaire Short Form (mean difference (MD) 1.74, 95% CI ‐33.02 to 36.50); the number of micturitions (MD ‐0.77, 95% CI ‐2.13 to 0.59); the number of incontinence episodes (MD ‐1.57, 95% CI ‐2.83 to ‐0.31); or the bothersomeness of incontinence as measured on the Urogenital Distress Inventory 6 (MD ‐0.90, 95% CI ‐1.46 to ‐0.34). There was no evidence of a difference in the number of women who experienced at least one adverse event (risk difference 0%, 95% CI ‐38% to 38%; no difference from 222 per 1000, 95% CI 380 fewer to 380 more).
The second included study was an eight‐week study in 30 women with urgency urinary incontinence that compared mindfulness‐based stress reduction (MBSR) to an active control intervention of yoga classes. The study was unblinded, and there was high attrition from both study arms for all outcome assessments. We judged the certainty of the evidence for all reported outcomes as very low due to performance bias, attrition bias, imprecision and indirectness. The number of women reporting cure was not reported. We are uncertain whether women in the yoga group were less likely to report improvement in incontinence at eight weeks compared to women in the MBSR group (RR 0.09, 95% CI 0.01 to 1.43; a decrease of 419 from 461 per 1000, 95% CI 5 to 660). We are uncertain about the effect of MBSR compared to yoga on reports of cure or improvement in incontinence, improvement in condition‐specific quality of life measured on the Overactive Bladder Health‐Related Quality of Life Scale, reduction in incontinence episodes or reduction in bothersomeness of incontinence as measured on the Overactive Bladder Symptom and Quality of Life‐Short Form at eight weeks. The study did not report on adverse effects.
Authors' conclusions
We identified few trials on yoga for incontinence, and the existing trials were small and at high risk of bias. In addition, we did not find any studies of economic outcomes related to yoga for urinary incontinence. Due to the lack of evidence to answer the review question, we are uncertain whether yoga is useful for women with urinary incontinence. Additional, well‐conducted trials with larger sample sizes are needed.
Plain language summary
Yoga for urinary incontinence in women
Review question
We examined whether yoga is useful for treating urinary incontinence in women. We compared yoga to no treatment and to other treatments for incontinence. We also compared yoga added to other treatments to other treatments alone. We focused on incontinence symptoms, quality of life and adverse effects. We also looked for information on the value for money of yoga treatment.
Background
Up to 15% of women who are middle‐aged or older may have urinary incontinence. Incontinence can be categorised as urgency urinary incontinence, defined as an involuntary loss of urine associated with a sudden strong desire to urinate, or stress urinary incontinence, where an activity such as sneezing triggers an involuntary leak of urine. Both types can negatively affect quality of life and social, psychological and sexual functioning. Treating incontinence usually begins with advice on lifestyle changes such as lowering caffeine use, behavioural interventions such as bladder training or exercises for the pelvic floor muscles. However, many women are interested in additional treatments such as yoga, a system of philosophy, lifestyle and physical practice that originated in ancient India.
How up‐to‐date is this review?
The evidence is current to 21 June 2018.
Study characteristics
We found two studies involving a total of 49 women. One was a six‐week study comparing yoga to a waiting list (delayed treatment) in women with either stress or urgency urinary incontinence. The other was an eight‐week study comparing yoga to mindfulness‐based stress reduction (MBSR) in women with urgency urinary incontinence. We also identified an ongoing study involving 50 women that aims to compare yoga with stretching; we will include this study when the results are reported.
Key results
The trial comparing yoga to a waiting list did not report the number of women reporting cure but did report on symptoms, condition‐specific quality of life and adverse effects. While this comparison generally favoured the yoga intervention, we are uncertain whether yoga improves urinary incontinence due to the very low certainty of the evidence. There was no difference between groups in the number of women reporting an adverse event and no serious adverse events were reported, but we are uncertain whether yoga increases harms as the certainty of the evidence is very low.
The trial comparing yoga to MBSR reported on symptoms and condition‐specific quality of life but did not report the number of women reporting cure. While this comparison generally favoured the MBSR intervention, we are uncertain whether yoga improves urinary incontinence due to the very low certainty of the evidence. There was no information on adverse events.
We did not find any information on the value for money of yoga for urinary incontinence.
Quality of the evidence
Although we identified some evidence on yoga treatment for treating urinary incontinence in women, the included studies were very small and there were issues with the way they were conducted, which limits our confidence in the results. Due to the nature of the treatments, the participants and staff of the trial comparing yoga to a waiting list were aware of which groups the participants were assigned and it is possible that the women in the yoga group reported some benefits because they expected yoga to be helpful. The trial comparing yoga to MBSR did not intend to test yoga as a treatment for incontinence. Instead, the trial tested MBSR as a treatment and used yoga classes to ensure that women in the comparison group received attention from the study staff. In addition, the trial comparing yoga to MBSR did not collect outcomes on all women and it is possible that the women who reported outcomes had either better or worse results than the women who did not report outcomes. There is currently insufficient good‐quality evidence to judge whether yoga is useful for women with urinary incontinence.
Summary of findings
Background
Description of the condition
The International Continence Society (ICS) and the International Urogynecological Association define urinary incontinence as "the complaint of involuntary loss of urine" (Bø 2017; Haylen 2010). Estimates of the prevalence of urinary incontinence are contested and vary widely according to case definitions as well as methods of ascertainment. Women often delay seeking help for urinary incontinence, and it is likely that this stigmatised condition is under‐reported (Wójtowicz 2014). In pregnant or postpartum women, estimates of the prevalence of urinary incontinence are 30% or higher (Milsom 2017). In women in the general population who are middle‐aged or older, daily urinary incontinence is estimated to be between 5% and 15%, while the prevalence of any incontinence symptoms among all adult women is estimated to be between 25% and 45% (Milsom 2017). Increasing age is the most widely accepted risk factor, although parity (particularly assisted vaginal births), obesity and menopausal status are also often considered to be important risk factors (Milsom 2017).
There are three major types of urinary incontinence, which are defined according to symptoms: stress urinary incontinence (SUI), urgency urinary incontinence (UUI) and mixed urinary incontinence (MUI). Although the specific prevalence rates are inconsistent between studies, SUI is consistently the most common type of urinary incontinence, responsible for approximately half of all cases of urinary incontinence, followed by MUI and then by UUI (Milsom 2017).
Stress urinary incontinence is defined as the involuntary loss of urine on effort or physical exertion, or on sneezing or coughing (Bø 2017; Haylen 2010). Stress urinary incontinence occurs when intra‐abdominal pressure rises with exertion or during a sneeze or cough, and the pressure upon the bladder is greater than the closure pressure of the urethral sphincter (Cannon 2004). Although SUI may involve a number of causes, it is often associated with weakened pelvic muscles and collagen‐dependent tissue, which can lead to a lack of urethral support and the inability to maintain urethral sphincter pressure (Long 2008).
Urgency urinary incontinence is defined as involuntary loss of urine associated with urgency (Bø 2017; Haylen 2010). Urgency is defined as a sudden and compelling desire to void urine, which is difficult to defer (Abrams 2013). Urgency urinary incontinence is a form of overactive bladder, which includes symptoms of urgency, frequency and waking at night to urinate (nocturia). The causes of overactive bladder and UUI specifically are unclear, but it is believed that the underlying pathophysiological factors include disturbances in the urothelium and overactivity of the detrusor smooth muscle and nerves (Steers 2002).
Mixed urinary incontinence is defined as the presence of both SUI and UUI symptoms (Bø 2017; Haylen 2010).
Urinary incontinence in women is associated with poor quality of life, and negatively impacts social, psychological and sexual functioning (Sinclair 2011). Depression appears to be associated with urinary incontinence, although it is unclear whether the physical and social effects of incontinence lead to development of depression or the presence of depression accentuates the bother of incontinence symptoms (Abrams 2013). Although all forms of urinary incontinence are associated with poor quality of life, and more severe incontinence appears to have a greater impact on quality of life, women with UUI or MUI may be more likely than women with SUI to report 'great' bother due to incontinence. Additionally, women with severe levels of MUI may experience greater impact upon their quality of life compared to women with severe levels of UUI or SUI (Minassian 2013; Monz 2007).
Description of the intervention
Yoga, a system of philosophy, lifestyle and physical practice that originated in ancient India, has become popular in the West during the last century. Although yoga is traditionally described as having eight 'limbs' or 'rungs' of practice, many currently practised styles of yoga primarily emphasise the integration of physical poses (asanas), controlled breathing (pranayama) and concentration (dharana) or meditation (dhyana) (Hewitt 2001; Taneja 2014). The popularity of yoga in the West has continued to increase over the past decade. For example, according to the US National Health Interview Survey (NHIS) conducted in 2002, 2007 and 2012, the reported use of yoga in the USA increased from approximately 5.1% of adults in 2002 to over 9.5% in 2012 (Clarke 2015). In the 2012 NHIS, use of yoga was higher among women than men, and higher among adults aged 18 to 44 years than for older age groups (Cramer 2016).
Yoga has been suggested to be useful in managing a range of medical conditions, including musculoskeletal conditions, cardiovascular conditions, stress, depression and anxiety (Taneja 2014). In the 2012 NHIS, the most common therapeutic uses of yoga were for back pain (19.7%), stress (6.4%) and arthritis (6.4%) (Cramer 2016).
Yoga appears to be a relatively safe practice. A review of case reports and case series of adverse events of yoga identified musculoskeletal issues as the most common adverse events, and the headstand, shoulder stand, lotus position and forceful breathing as the most common yoga techniques associated with adverse events (Cramer 2013). Cramer 2013 advised that yoga practices should be adapted to pre‐existing medical conditions and practised under the supervision of a qualified teacher. A recent review of randomised trials of yoga found that yoga is associated with a greater risk of intervention‐related and non‐serious adverse effects than psychological or educational interventions, but not with an increased risk of serious adverse events. The review also stated that yoga is associated with the same risk of serious, non‐serious and intervention‐related adverse effects as usual care or non‐yoga exercise interventions (Cramer 2015). The overall rate of serious adverse events in the yoga arms of the trials was 0.6% (Cramer 2015).
How the intervention might work
Urinary incontinence is usually initially managed by conservative therapies (Abrams 2013). These include lifestyle interventions, bladder training and pelvic floor muscle training (used either alone or in combination with other active treatments such as biofeedback) (Ayeleke 2015; Dumoulin 2018; Herderschee 2011; Imamura 2015; Wallace 2004).
There is good evidence to support the use of pelvic floor muscle training as a first approach to managing urinary incontinence, particularly SUI (Dumoulin 2018). With pelvic floor muscle training, appropriately timed conscious pelvic floor muscle contractions may increase urethral pressure and prevent the urinary leakage associated with SUI (DeLancey 1988; Miller 1998). Strengthening of the pelvic floor muscles may also improve support of the bladder neck, which may reduce urinary incontinence (Bø 2004). Finally, pelvic floor muscle contractions may inhibit detrusor muscle contractions, which could prevent the urinary leakage associated with UUI (Bø 2000).
Some studies suggest that some yoga breathing, relaxation and muscle control techniques may assist in the strengthening of the pelvic floor (Bø 2013; Tenfelde 2014). Specific yoga poses that are believed to be helpful and have been tested include the Utkatasana (chair pose), Trikonasana (triangle pose) and the Malasana (squat pose) (Huang 2014b). Yoga may help improve general body alignment, flexibility, strength, control and awareness, all of which are thought to assist in strengthening the pelvic floor muscles (Tenfelde 2014). Yoga may therefore function as either an alternative method of pelvic floor muscle training or as a supplement to training. Yoga may also address mental health and quality of life issues through potential effects on depression, stress and anxiety, and help patients manage their medical condition.
Why it is important to do this review
Urinary incontinence is a highly prevalent and distressing condition in women. Although many treatments are available for urinary incontinence, there is no universally effective and acceptable treatment and additional approaches to treatment may be of value. Yoga is a mind‐body practice that is increasingly popular in the West, and is particularly popular with women. A pre‐post trial of pelvic floor muscle training with adjunctive Hatha yoga in women with stress incontinence reported that the combined intervention was effective in improving incontinence (Kim 2015). Also, at least one randomised trial of Iyengar yoga for urinary incontinence has provided promising results in the treatment of SUI and UUI with yoga (Huang 2014b). However, there is a paucity of evidence on the effectiveness of yoga for incontinence and no available guidance for clinicians or the public. It is therefore important to assess whether yoga may be effective as either a primary or adjuvant treatment for urinary incontinence in women.
Objectives
To assess the effects of yoga for treating urinary incontinence in women.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and the first period of cross‐over RCTs. We excluded quasi‐randomised controlled trials (i.e. trials in which assignment to treatment was made using a non‐random method such as alternation) because the method of allocation may lead to biased estimates of effect. We did not restrict study eligibility by language or publication status.
We only included health economic studies conducted alongside studies that were included in the clinical component of this systematic review (Shemilt 2011).
Types of participants
We included studies with women aged 18 years or more who were diagnosed as having urinary incontinence on the basis of symptoms, signs or urodynamic evaluation (as defined by the trial authors). We only included trials that recruited both men and women if at least 90% of participants were women or if the trial provided demographic and outcome data separately for women. We included trials with women diagnosed as having stress, urgency or mixed urinary incontinence, as well as trials with participants who had mixed or unclassified types of urinary incontinence.
We included trials carried out on women who were experiencing urinary incontinence during the antenatal or postnatal period. Because this group has physiological differences from women who are not pregnant or postpartum, and the natural history of incontinence in this population differs from that in non‐pregnant women, the observed effects of the intervention may differ in this group. We therefore did not group this population with women who were not pregnant or postpartum and we planned to analyse the studies separately throughout the review.
We excluded studies of women who had urinary incontinence thought to be due to factors beyond the urinary tract such as neurological or psychiatric disorders, cognitive impairment, or mobility problems. We also excluded studies that focused on women who were experiencing nocturnal enuresis.
Types of interventions
We included studies of yoga as a treatment for urinary incontinence, where the study report specified that the intervention was 'yoga' provided at any dose, with any frequency and for any duration, because we believe these factors are likely to vary in practice.
We included interventions that belonged to any yoga tradition but excluded studies in which the yoga intervention did not include a physical practice component. We included studies that compared yoga to no treatment or to another active treatment. We also included studies that compared yoga as an adjunct to other treatments versus those same treatments without yoga. The types of included comparisons were as follows.
Yoga versus no specific active intervention (e.g. usual care, waiting list).
Yoga versus an active intervention (e.g. lifestyle intervention or pelvic floor muscle training), for which we considered different active comparators separately (e.g. yoga versus lifestyle advice, yoga versus pelvic floor muscle training).
Yoga plus an intervention versus the same intervention without yoga (e.g. yoga as an add‐on intervention to pelvic floor training versus pelvic floor training alone), for which we considered different interventions separately.
We included studies in which co‐interventions were provided if they were similar between intervention groups (e.g. both the yoga and the comparison groups received advice on behavioural management techniques).
Studies that compare yoga to a sham yoga intervention do not appear to be common (Park 2014). However, we planned that we would consider such studies to represent an additional type of comparison (i.e. yoga versus sham yoga) and would analyse them separately.
We excluded studies of interventions based on yoga (e.g. exercises based on yoga postures) but not characterised as yoga, as well as studies of multimodal interventions in which yoga is only one component amongst others, such as mindfulness‐based stress reduction (MBSR).
Types of outcome measures
We used outcomes suggested by the Standardisation Committee of the International Continence Society (Bø 2017; Haylen 2010). The following five categories of outcomes are recommended for research investigating the effect of therapeutic interventions for women with urinary incontinence (Lose 2001):
The woman’s observations (e.g. symptoms);
Quantification of the woman's symptoms (e.g. urine loss);
The clinician’s observations (anatomical and functional signs);
The woman's quality of life (urinary incontinence ‐ specific and general);
Economic measures.
In this review, we considered at least one outcome from each of the first four categories. We included specific outcomes that are commonly found in other Cochrane Incontinence reviews for urinary incontinence in women so that this review may produce results that are easily compared to or combined with those of other reviews of treatment for the same condition.
Primary outcomes
Number of women who report they are cured (they no longer experience urinary incontinence).
Number of women who report cure or improvement of urinary incontinence.
Urinary incontinence condition‐ or symptom‐specific quality of life, as measured by any relevant scale (e.g. the Urinary Incontinence Quality of Life scale (Patrick 1999), the Incontinence Impact Questionnaire (Uebersax 1995), the International Consultation on Incontinence Modular Questionnaire Lower Urinary Tract Symptoms Quality of Life (ICIQ‐LUTSqol) (Nystrom 2015), or the Pelvic Floor Distress Inventory (PFDI) and the Pelvic Floor Impact Questionnaire (PFIQ) (Barber 2001)).
Secondary outcomes
-
Quantification of symptoms
Number of micturitions (daily).
Number of episodes of incontinence (daily).
Urine loss as measured with a pad or paper towel weight test (either the short‐ or long‐term test).
Symptoms as reported by study participants on any condition‐specific scale (e.g. the Severity Index for Urinary Incontinence in Women (Sandvik 1993)).
-
Clinician's observations (anatomical and functional signs)
Clinical assessment of presence of incontinence, such as urine leakage during a cough test.
Measurement of pelvic floor muscle function, such as by electromyography, vaginal squeeze pressure, pelvic floor muscle force, and morphological measurements (dynamometry, ultrasound).
-
Quality of life
Quality of life measured on a scale that is not condition‐ or symptom‐specific (e.g. the 36‐Item Short Form Health Survey (SF‐36)).
Depression, anxiety or distress as measured on relevant scales (e.g. Beck Depression Inventory (BDI), Hospital Anxiety and Depression Scale (HADS)).
Other measures of emotional and social impact of the disorder such as the bothersomeness of the condition, the social impact of the condition and sexual functioning.
-
Adverse effects
Number of adverse effects (e.g. pain, discomfort).
Main outcomes for 'Summary of findings' tables
The GRADE working group recommends including up to seven critical outcomes in a systematic review (Guyatt 2011a; Guyatt 2011b). We therefore considered the following outcomes for assessing the certainty of the evidence:
Number of women who report they are cured (they no longer experience urinary incontinence);
Number of women who report cure or improvement of urinary incontinence;
Urinary incontinence condition‐specific or symptom‐specific quality of life;
Number of micturitions (daily);
Number of episodes of incontinence (daily);
Adverse effects.
Timing of outcome assessment
We grouped all outcomes into three time points: short‐term (closest to three months after randomisation), intermediate‐term (closest to six months after randomisation) and long‐term (closest to one year after randomisation). When an included trial presented multiple time points, we considered the short‐term time point as primary and other time points as secondary.
Search methods for identification of studies
We did not impose any restrictions, for example language or publication status, on the literature searches described below.
Electronic searches
Cochrane Incontinence Specialised Register
We drew on the search strategy developed for Cochrane Incontinence. We identified relevant trials from the Cochrane Incontinence Specialised Register. For more details of the search methods used to build the Specialised Register, please see the Group's webpages where details of the Register's development (from inception) and the most recent searches performed to populate the Register can be found. To summarise, the register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE In‐Process, MEDLINE Epub Ahead of Print, CINAHL, the US National Institutes of Health Ongoing Trials Register, ClinicalTrials.gov, the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) and handsearches of journals and conference proceedings. Many of the trials in the Cochrane Incontinence Specialised Register are also contained in CENTRAL.
The terms used to search the Cochrane Incontinence Specialised Register are provided in Appendix 1. The search is up‐to‐date as of 21 June 2018.
We searched for all eligible published and unpublished trials in all languages. We planned to translate any non‐English language abstracts for potential inclusion. We based our search strategy on concepts of types of study population, types of study design and symptoms of urinary incontinence such as leakage of urine.
Other electronic bibliographic databases
We also used the terms in Appendix 1 to search the Cochrane Complementary Medicine Field Specialised Register for relevant trials of yoga. The Complementary Medicine Field Specialised Register contains trials identified from CENTRAL, Chinese databases, Korean databases and multiple small databases that have been identified as good sources of complementary medicine trials (Wieland 2013). The search was last updated on 21 June 2018.
We performed searches of the NHS Economic Evaluation Database (NHS EED) in order to identify potential economic studies. As the last database searches for NHS EED were carried out in December 2014, we used the NHS EED search filters on 25 September 2017 to search MEDLINE and Embase for economics studies from January 2015 onwards. To retrieve the maximum number of potentially relevant records, we searched the NHS EED for 'yoga' and combined the term 'yoga' with the NHS EED search filters when searching MEDLINE and Embase. See Appendix 2 for the NHS EED search filters. A further updated search of MEDLINE and Embase was conducted on 22 January 2019 adding an additional set of terms to identify urinary incontinence related studies. This set of urinary incontinence related terms was combined with the NHS EED filters and the yoga terms ‐ further details can be found in Appendix 2.
We did not search AMED (Allied and Complementary Medicine Database), CINAHL (Cumulative Index to Nursing and Allied Health Literature) and IndMED for this version of the review because we ran preliminary test searches of these databases for the protocol and, after de‐duplication against the Cochrane Incontinence Specialised Register, they did not yield any additional records that met our inclusion criteria (Wieland 2017). For full details, please see Appendix 3 (AMED), Appendix 4 (CINAHL) and Appendix 5 (IndMED).
Searching other resources
We checked the reference lists of all included studies and systematic reviews for additional references. We contacted experts in the field and authors of included studies to identify additional unpublished studies. We also checked the proceedings of the following conferences for relevant research:
International Congress on Complementary Medicine Research (ICCMR) (2010 to 2017); and
European Congress for Integrative Medicine (ECIM) (2009, 2011 to 2017).
Data collection and analysis
Per our published protocol (Wieland 2017), we conducted the following data collection and analysis in accordance with the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Selection of studies
Two review authors independently screened the titles and abstracts of all retrieved references in Covidence (Covidence 2017). We retrieved the full‐text study reports for all citations that at least one review author considered potentially relevant. Two review authors independently screened the full‐text articles and identified studies for inclusion and identified and recorded reasons for excluded studies in the Characteristics of excluded studies. Any disagreements were resolved by discussion.
We collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009).
Data extraction and management
We used a standardised piloted data collection form in Microsoft Excel 2018 for Mac Version 16.20 and extracted the following study characteristics and outcome data.
Methods: study design.
Participants: number randomised, number with each type(s) of incontinence and how incontinence was diagnosed, if participants were pregnant or postpartum, how many were pregnant and how many were postpartum, severity and duration of urinary incontinence if reported, study participant mean age or age range, study location and setting, recruitment methods and inclusion and exclusion criteria.
Interventions: description of yoga intervention characteristics, dose and duration of yoga intervention, description of comparison intervention characteristics, adherence to the yoga and comparison interventions, description of any co‐interventions, length of follow‐up, number of withdrawals and reasons for withdrawal.
Outcomes: description of primary and secondary outcomes in the review that were reported in the trial, and listing of other outcomes collected in the trial.
Notes: funding for trial and notable conflicts of interest of trial authors.
'Risk of bias' assessment.
Two review authors independently extracted outcome data from the included studies into Microsoft Excel 2018 spreadsheets and compared the data to identify any discrepancies in data entry. Any disagreements were resolved by consensus. We noted in the Characteristics of included studies if a trial did not report outcome data in a usable way. We transferred all outcome data into Cochrane’s Review Manager 5 software (Review Manager 2014).
In addition to extracting data from included studies as described above, we planned to include an appendix of bibliographic detail of any identified economic studies. As such, we did not conduct a further review of potential economic studies.
Assessment of risk of bias in included studies
Two review authors (LSW, ZSL) independently assessed the risk of bias for each included trial using Cochrane's 'Risk of bias' tool (Higgins 2011a). Any disagreements were resolved by discussion. We assessed the risk of bias for the following domains: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment for each outcome (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other bias (such as validity of outcome measure and baseline comparability).
We assessed each potential source of bias as either high, low, or unclear and provided a quotation from the study report together with a justification for our judgement in the 'Risk of bias’ tables. We summarised the judgements across different studies for each of the domains listed.
The participants and personnel in most yoga trials are not blinded. As the primary outcomes of this review depended upon the perception and reporting of the study participant, we have not included blinding of personnel, participants or outcome assessors in our dichotomising of trials into higher versus lower risk of bias. Instead, for our sensitivity analyses of the primary outcomes by higher versus lower risk of bias, we classified studies as having a relatively lower risk of bias if they had a low risk of bias for random allocation, allocation concealment and incomplete outcome assessment, and did not have a high risk of bias for selective outcome reporting or other bias (see Sensitivity analysis).
Measures of treatment effect
We uploaded the outcome data for each study into the data tables in Review Manager 5 to calculate treatment effects (Review Manager 2014). We used the risk ratio (RR) for dichotomous outcomes related to benefit of treatment (e.g. cure). We used the absolute risk difference (RD) for adverse events. We used the mean difference (MD) for continuous outcomes reported on the same scale, and the standardised mean difference (SMD) for continuous outcomes measured on different scales in different trials included in the same meta‐analysis. We expressed the uncertainty with 95% confidence intervals (CIs) for all effect estimates.
If the included studies only reported effect estimates and their CIs, standard errors or exact P values, we uploaded these data into Review Manager 5 in order to apply the generic inverse variance method (Review Manager 2014). We ensured that higher scores for continuous outcomes had the same meaning for a given outcome and explained the direction to the reader. When we were unable to enter the results in either of the above ways, we described them in the Characteristics of included studies or entered the data into the Additional tables.
Unit of analysis issues
Where appropriate, we planned to include the first period of cross‐over studies. We also planned to include cluster‐randomised studies if they were suitable according to the guidance in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Dealing with missing data
We contacted investigators or study sponsors in order to verify key study characteristics and to obtain missing numerical outcome data where possible. If numerical outcome data such as standard deviations (SDs) or correlation coefficients were missing, we attempted to calculate them from other available statistics, such as P values, according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). If we were unable to obtain a full report even after contacting the study authors, we listed the study as 'awaiting classification'.
Assessment of heterogeneity
We assessed clinical heterogeneity (i.e. differences in study populations, interventions and outcomes) between studies qualitatively. For studies that we judged to have sufficient clinical homogeneity to combine in a meta‐analysis, we planned to assess heterogeneity in three ways: visual examination of the forest plots; the Chi² test (P ≤ 0.10) for heterogeneity; and the I² statistic, which describes the per cent of the variability in the estimate that is due to clinical or methodological heterogeneity rather than to chance. We planned to consider the implications of the observed value of the I² statistic as follows:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity (Deeks 2011).
We planned to assess the importance of the value of the I² statistic in light of the range and direction of effects as observed from the forest plots and the strength of the evidence for heterogeneity based upon the Chi² test (Deeks 2011). We planned to seek and discuss plausible explanations for observed statistical heterogeneity. We planned to investigate causes of heterogeneity between trials, qualitatively assessing any differences between individual trials in the populations and interventions. We also planned to explore heterogeneity through the use of subgroup and sensitivity analyses.
Assessment of reporting biases
We searched study registries of prospectively registered trials to identify completed, but not published, trials. We planned to use a funnel plot and Egger's test to assess the potential for publication bias in meta‐analyses with more than 10 trials (Egger 1997; Sterne 2011).
Data synthesis
Where trials were clinically comparable (i.e. clinical comparability of population, intervention, comparison, outcome and timing of measurement), we planned to combine the outcome data from the individual trials in a meta‐analysis using Review Manager 5 (Review Manager 2014). We planned to analyse pregnant and postpartum women separately in call cases. However, for non‐pregnant, non‐postpartum populations, we planned to group together women with SUI, UUI, MUI and mixed or unclear urinary incontinence diagnoses in the primary analysis, and examine different types of urinary incontinence diagnoses using subgroup analyses (see Subgroup analysis and investigation of heterogeneity).
As yoga is a complex intervention with variations in practice components and implementation and we expected some between‐study variation due to these factors, we planned to use the random‐effects model for meta‐analysis.
When outcome data from individual trials were not sufficiently similar to be combined quantitatively, we planned to narratively describe the results from clinically comparable trials.
Subgroup analysis and investigation of heterogeneity
As the mechanisms of SUI and UUI are different, the effects of yoga may vary across types of urinary incontinence. We planned that if there were sufficient data, we would carry out subgroup analyses by type of urinary incontinence in the following groups:
SUI;
UUI;
MUI; and
a range of urinary incontinence diagnoses, where data are not reported separately by urinary incontinence subgroup.
If sufficient data become available, we also plan to conduct subgroup analyses of trials conducted in older (mean age 65 years or greater) versus younger populations, as populations from different age groups may vary in their ability to perform yoga. Among women who are pregnant or postpartum, we plan to perform subgroup analyses of trials conducted in women who are pregnant versus postpartum, as the natural history of incontinence is different in the two states. We also intend to carry out subgroup analyses by style (e.g. Iyengar yoga, Viniyoga, Yin yoga), dose and duration of yoga intervention to determine whether type of yoga, amount of yoga or duration of yoga modifies the effect of the yoga intervention.
Sensitivity analysis
When both endpoint and change data were available, we used endpoint data for our primary analysis and carried out a sensitivity analysis to check whether the results varied according to endpoint versus change data. In cases where study participants were lost to follow‐up and intention‐to‐treat analyses were conducted using imputation alongside available‐case analyses, we used the observed data for our primary analysis and performed a sensitivity analysis to check whether the results varied according to imputed versus available‐case data. In cases where both unadjusted and adjusted data were available, we used the unadjusted data for our primary analysis and performed a sensitivity analysis to check whether the results varied according to adjusted versus unadjusted data.
If sufficient data become available, we plan to assess the robustness of our conclusions by excluding studies that we judge to have a high risk of bias from our meta‐analyses for the primary outcomes.
'Summary of findings' tables
We created a 'Summary of findings' table using the GRADE criteria (Guyatt 2011a; Guyatt 2011b). We planned to prepare separate 'Summary of findings' tables for trials carried out with women who were pregnant or postpartum.
Two review authors (LSW and ZSL) independently undertook GRADE assessments and compared results. Consensus was reached through discussion when necessary. We justified all decisions to downgrade the certainty of the evidence using footnotes and made comments to aid readers’ understanding of the review.
We considered the following factors in our assessment of the certainty of the evidence.
Limitations in the study design and conduct (i.e. risk of bias).
Inconsistency of results.
Indirectness of evidence.
Imprecision.
Publication bias.
We downgraded the certainty of the evidence for a given outcome by one level according to the performance of the included studies against each of the five factors.
Results
Description of studies
Results of the search
The search produced a total of 42 titles and abstracts, from which 14 records were selected for full‐text review. Two trials in seven reports were eligible for inclusion in the review. The full report of one study for which we were able to obtain a trial register record and an unpublished abstract was not available, therefore we assessed this study as 'awaiting classification' as per our protocol (Huang 2018). We excluded five studies in five reports; the reasons for exclusion are provided in the Characteristics of excluded studies. The PRISMA flow chart in Figure 1 illustrates the flow of literature through the search and selection process.
1.
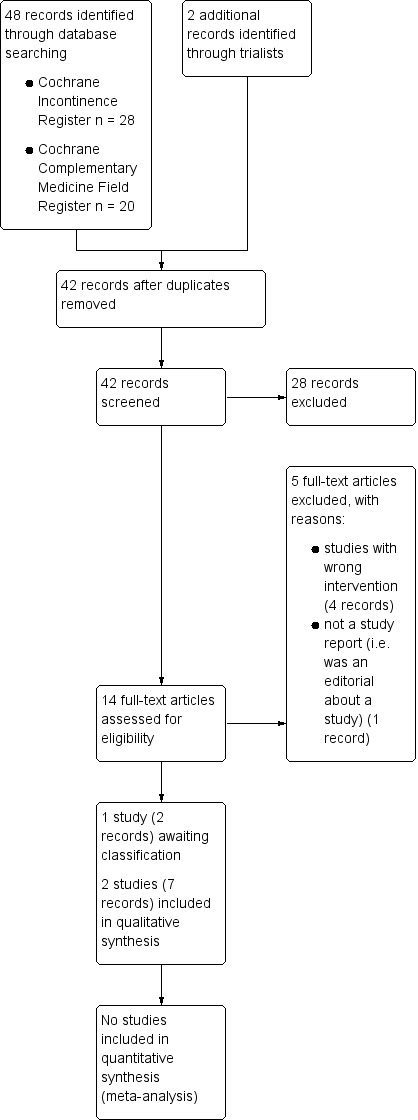
PRISMA study flow diagram.
Our search for economic studies produced a total of 608 titles and abstracts, from which none were selected for further assessment. The PRISMA flow chart in Figure 2 illustrates the flow of economic literature through the search and selection process. Economic studies are not considered further in this review.
2.
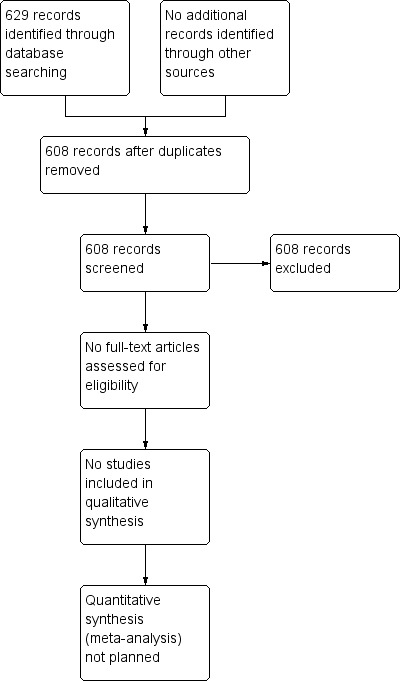
Study flow diagram for economics studies.
Included studies
Both included trials were two‐arm parallel randomised controlled trials conducted in the USA (Baker 2014; Huang 2014a). The trials included a total of 49 women.
Sample characteristics
Baker 2014 included participants ranging in age from 22 to 79 years, with a median age of 58 years in the yoga group and 59 years in the comparison group. Huang 2014a required participants to be aged at least 40, resulting in a sample with a mean age of 61 years. Most participants in Baker 2014 were postmenopausal, while pregnancy during the past year was an exclusion criterion for Huang 2014a.
In Baker 2014, all participants had urge‐predominant urinary incontinence. In Huang 2014a, 63% of participants had urge‐predominant urinary incontinence and 37% of participants had stress‐predominant urinary incontinence. Neither trial specified how urinary incontinence was diagnosed.
Interventions and comparators
The comparisons to yoga differed in the two trials. In Baker 2014, yoga was an active control for mindfulness‐based stress reduction (MBSR), which was the intervention of interest. The yoga intervention was described as following the basic principles of yoga and focusing on asanas and relaxation. It did not include any postures or muscle contractions designed to treat incontinence. In Huang 2014a, which was a pilot study to determine the feasibility of a group‐based yoga therapy intervention for women with urinary incontinence, a specially designed yoga program based on Iyengar yoga was compared to a wait‐list control.
Outcomes
Both trials collected and reported information on improvement in incontinence, condition‐ or symptom‐specific quality of life, daily episodes of incontinence, and other measures of emotional and social impact of incontinence. Huang 2014a reported additional information on daily micturitions and adverse events. Baker 2014 reported all outcomes other than improvement in incontinence using medians and ranges, and these data were not extracted for analysis.
Further details about participants, interventions, comparators and outcomes are provided in the Characteristics of included studies.
Excluded studies
We excluded four trials in which yoga was not an intervention. We excluded an additional article because it was not a primary study report but rather an editorial on an included study (Huang 2014a). Reasons for exclusion of the five records are provided in the Characteristics of excluded studies.
Risk of bias in included studies
Figure 3 and Figure 4 summarise the risk of bias of the included trials.
3.
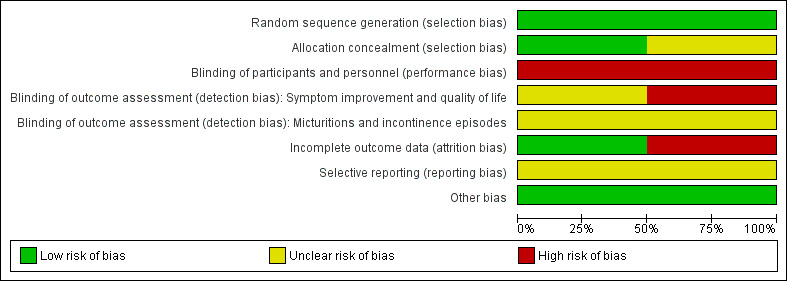
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.
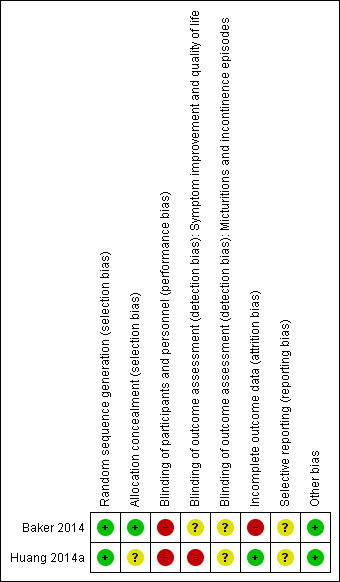
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We considered the risk of bias for random sequence generation to be low for one trial reporting that random sequence generation was carried out by computer (Huang 2014a). However, allocation concealment was not described, therefore we considered the risk of bias for allocation concealment to be unclear. In the other trial, the shuffling of 'security tint' envelopes containing the group assignment was used to generate the random sequence (Baker 2014). We therefore considered the risk of bias for both random sequence generation and allocation concealment to be low, given the processes followed.
Blinding
There was no indication in either study that participants and personnel were unaware of the intervention assignments and, given the nature of yoga interventions, we considered blinding to be highly unlikely. We therefore considered the risk of performance bias to be high in both studies. Because participants were not blinded and the control condition in Huang 2014a was a waiting list, we considered outcomes that relied upon participant judgement (e.g. overall improvement) to be at high risk of detection bias. We considered more objective outcomes that relied upon participant identification of events (e.g. diary recording of incontinence episodes) to be at unclear risk of detection bias, despite the use of masked assessors to extract diary data. In Baker 2014, both interventions were active and, because it is possible that the participants were unaware whether MBSR or yoga was the intervention of interest, we considered that the risk of detection bias was unclear for all outcomes.
Incomplete outcome data
In Baker 2014, there were high rates of loss to follow‐up and, as the rates of loss to follow‐up differed between groups and reasons for loss to follow‐up were not described, we considered the study to be at high risk of attrition bias. In Huang 2014a, only one participant was lost to follow‐up, and we considered the study to be at low risk of attrition bias.
Selective reporting
Both included studies were registered at ClinicalTrials.gov and reported primary outcomes consistent with the trial registration, but also reported secondary outcomes that were not included in the trial registration. We considered the risk of reporting bias to be unclear for both trials.
Other potential sources of bias
We identified no other potential sources of bias for either trial.
Effects of interventions
Summary of findings for the main comparison. Yoga versus no specific active intervention.
| Yoga compared with wait‐list for urinary incontinence in women | ||||||
|
Patient or population: women with either stress‐predominant or urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: wait‐list | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (six weeks) | 111 per 1000 | 703 per 1000 (160 to 1000) | RR 6.33 (1.44 to 27.88) | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | Number of women who reported satisfaction with change in urine leakage. |
|
Urinary incontinence condition‐ or symptom‐specific quality of life at short term (6 weeks) Measured by Incontinence Impact Questionnaire Short Form (IIQ‐7) (lower = better) |
The mean change in the control group was a decrease of 31 units. | The mean change in the intervention group was 1.74 units higher (33.02 units lower to 36.50 units higher). | Not applicable | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
|
Number of micturitions (daily) at short term (6 weeks) |
The mean change in the control group was a decrease of 0.13 micturitions. | The mean change in the intervention group was 0.77 fewer micturitions (2.13 fewer to 0.59 more). | Not applicable | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
|
Number of episodes of incontinence (daily) at short term (6 weeks) |
The mean change in the control group was a decrease of 0.27 episodes. | The mean change in the intervention group was 1.57 fewer episodes (2.83 to 0.31 to fewer). | Not applicable | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
|
Bothersomeness of symptoms at short term (6 weeks) Measured by Urogenital Distress Inventory 6 (UDI‐6) (lower = better) |
The mean change in the control group was a decrease of 0.1 units. | The mean change in the intervention group was 0.90 units lower (0.34 to 1.46 lower). | Not applicable | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | |
|
Adverse effects at short term (6 weeks) |
222 per 1000 | 222 per 1000 (0 to 600) | RD 0% (‐38% to 38%) | 18 (1 study) | ⊕⊝⊝⊝ very low1,2 | 2 women in each group reported an adverse effect. However, there were 7 adverse effects overall and the distribution of adverse effects between groups is not reported. None of the adverse effects were considered to be potentially related to the study and none were serious. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RD: risk difference; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||||
1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and outcome was self assessed and self recorded by participants (risk of detection bias). 2Downgraded one level for imprecision (< 400 participants).
Summary of findings 2. Yoga versus an active intervention.
| Yoga compared with mindfulness‐based stress reduction (MBSR) for urinary incontinence in women | ||||||
|
Patient or population: women with urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: mindfulness‐based stress reduction (MBSR) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| MBSR | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
|
Number of women who report cure or improvement of urinary incontinence at short term (8 weeks) |
461 per 1000 | 42 per 1000 (5 to 660) | RR 0.09 (0.01 to 1.43) | 24 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | |
|
Urinary incontinence condition‐ or symptom‐specific quality of life at short term (8 weeks) Measured by the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale (higher per cent improvement = better) |
‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ very low1,2,3 | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was 8.70 (IQR 1.75 to 20.59) in the yoga group (n = 11) and 29.27 (IQR 8.11 to 93.33) in the MBSR group (n = 13) (reported P value = 0.03). |
| Number of micturitions (daily) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
|
Number of episodes of incontinence (daily) at short term (8 weeks) |
‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ very low1,2,3 | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was ‐33.33 (IQR ‐50.00 to 16.67) in the yoga group (n = 11) and ‐60 (IQR ‐88.89 to ‐50.00) in the MBSR group (n = 13) (reported P value = 0.03). |
|
Bothersomeness of symptoms at short term (6 weeks) Measured by the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF) (lower = better) |
‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ very low1,2,3 | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent change at 8 weeks was ‐25.0 (IQR ‐35 to 20) in the yoga group (n = 11) and ‐55.6 (IQR ‐50 to ‐87) in the MBSR group (n = 13) (reported P value = 0.005). |
| Adverse effects | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report on adverse effects. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IQR: interquartile range; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: Further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: We are very uncertain about the estimate. | ||||||
1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and there was a high percentage of loss to follow‐up that was unbalanced across study arms (risk of attrition bias). 2Downgraded one level for indirectness because the yoga intervention was not designed to treat urinary incontinence. 3Downgraded one level for imprecision (< 400 participants).
The two included trials compared yoga to a wait‐list condition (one trial with 19 women) and to a mindfulness‐based stress reduction (MBSR) intervention (one trial with 30 women). Neither trial included information on the number of women reporting continence, but both trials reported data on the number of women who reported improvement in urinary incontinence. Both trials also reported condition‐ or symptom‐specific quality of life outcomes. Both trials reported on the change in number of episodes of incontinence, but neither trial reported data on clinical observations of clinical or anatomical functioning. The following results were reported.
Yoga versus no specific active intervention
One small trial (n = 19) compared the effects of a yoga intervention to a waiting list in women with urge‐predominant urinary incontinence (n = 12) or stress‐predominant urinary incontinence (n = 7) (Huang 2014a). All outcomes were measured at six weeks after randomisation, and all evidence was assessed as of very low certainty due to the very small sample size and lack of blinding of study participants, personnel and outcome assessors. See Table 1 for a summary of the main results.
Primary outcome measures
Number of women who report they are cured (they no longer experience incontinence)
Not reported.
Number of women who report cure or improvement of urinary incontinence
Women were not asked directly whether their incontinence had been cured or improved but were asked whether they were satisfied with the change in urine leakage, which is an indirect measure of improvement of urinary incontinence. There was very low‐certainty evidence that women in the yoga group were six times more likely than women in the wait‐list group to be at least moderately satisfied with the change in their urine leakage (risk ratio (RR) 6.33, 95% confidence interval (CI) 1.44 to 27.88; Analysis 1.1).
1.1. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks).
Urinary incontinence condition‐ or symptom‐specific quality of life
There was very low‐certainty evidence of no difference between the yoga and wait‐list groups in quality of life as measured on the Incontinence Impact Questionnaire Short Form (IIQ‐7) (mean difference (MD) 1.74, 95% CI ‐33.02 to 36.50; Analysis 1.2). At baseline, the yoga group had lower mean scores on the IIQ‐7 and, after adjusting for the baseline scores, the difference in changes between groups was in the opposite direction favouring the wait‐list group, but there was still no difference between groups (MD ‐27.70, 95% CI ‐66.80 to 11.40; Analysis 1.3).
1.2. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks).
1.3. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks).
Secondary outcome measures
Number of micturitions (daily)
There was very low‐certainty evidence of little or no difference in the frequency of total daily micturitions between groups (MD ‐0.77, 95% CI ‐2.13 to 0.59; Analysis 1.4). At baseline, the yoga group had a slightly higher mean number of total daily micturitions compared to the wait‐list group and, after the analysis adjusted for baseline micturitions, the difference in changes between groups was further reduced (MD ‐0.12, 95% CI ‐1.73 to 1.49; Analysis 1.5).
1.4. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 4 Number of micturitions (daily) (at short term ‐ 6 weeks).
1.5. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 5 Adjusted analysis for number of micturitions at short term (6 weeks).
Number of episodes of incontinence (daily)
There was very low‐certainty evidence of a greater reduction in the yoga group compared to the wait‐list group in the frequency of total daily episodes of incontinence (MD ‐1.57, 95% CI ‐2.83 to ‐0.31; Analysis 1.6). After adjusting for baseline outcome levels, the difference between groups was consistent with the unadjusted analysis (MD ‐1.40, 95% CI ‐2.79 to ‐0.01; Analysis 1.7).
1.6. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks).
1.7. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks).
Urine loss as measured with a pad or paper towel weight test
Not reported.
Symptoms as reported by study participants on any condition‐specific scale
Not reported.
Clinical assessment of presence of incontinence
Not reported.
Measurement of pelvic floor muscle function
Not reported.
Quality of life measured on a scale that is not condition‐ or symptom‐specific
Not reported.
Depression, anxiety or distress
Not reported.
Other measures of emotional and social impact of the disorder
There was very low‐certainty evidence of a greater reduction in the yoga group compared to the wait‐list group in the subjective bothersomeness of incontinence symptoms as measured on the Urogenital Distress Inventory 6 (UDI‐6) (MD ‐0.90, 95% CI ‐1.46 to ‐0.34; Analysis 1.8). After adjusting for baseline outcome levels, the difference between groups was nearly identical to the unadjusted analysis (MD ‐0.90, 95% ‐1.40 to ‐0.40; Analysis 1.9).
1.8. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 8 Bothersomeness of symptoms (at short term ‐ 6 weeks).
1.9. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks).
Adverse effects
There was very low‐certainty of no evidence of a difference between yoga and wait‐list groups in the number of women who experienced one or more adverse events (risk difference (RD) 0.00, 95% CI ‐0.38 to 0.38; Analysis 1.10).
1.10. Analysis.
Comparison 1 Yoga versus no specific active intervention, Outcome 10 Adverse effects (at short term ‐ 6 weeks).
Yoga versus an active intervention
One small trial (n = 30) compared the effects of a yoga intervention to a mindfulness‐based stress reduction (MBSR) intervention in women with urgency urinary incontinence (Baker 2014). The yoga intervention was conceived as an active control for the MBSR intervention, which was the treatment of interest. The yoga intervention did not include any postures, techniques or instructions intended to improve bladder control or reduce incontinence. All outcomes were measured at eight weeks, six months and one year and were reported in the publication as medians and ranges, likely due to highly skewed data and a small sample size, with the exception of the number of women reporting improvement in incontinence. We extracted data on improvement in incontinence into Review Manager 5; all other data reported below are as presented in the study publication. We assessed all evidence as of very low certainty due to the very small sample size, lack of blinding (i.e. performance bias), attrition bias and indirectness (i.e. the yoga intervention was not an intervention designed to improve incontinence). See Table 2 for a summary of the main results.
Primary outcome measures
Number of women who report they are cured (they no longer experience incontinence)
Not reported.
Number of women who report cure or improvement of urinary incontinence
There was very low‐certainty evidence of no difference between women in the MBSR group and women in the yoga group in improvement in incontinence, as measured on the Patient Global Impression of Improvement (PGI‐I) at eight weeks (RR 0.09, 95% CI 0.01 to 1.43; Analysis 2.1); six months (RR 0.20, 95% CI 0.03 to 1.42; Analysis 2.2); and one year (RR 0.22, 95% CI 0.03 to 1.53; Analysis 2.3).
2.1. Analysis.
Comparison 2 Yoga versus an active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks).
2.2. Analysis.
Comparison 2 Yoga versus an active intervention, Outcome 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months).
2.3. Analysis.
Comparison 2 Yoga versus an active intervention, Outcome 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year).
Urinary incontinence condition‐ or symptom‐specific quality of life
There was very low‐certainty evidence that women in the MBSR group had greater improvement in urinary incontinence‐specific quality of life compared to women in the yoga group, as measured on the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale. The median per cent improvement at eight weeks was 8.70 in the yoga group (interquartile range (IQR) 1.75 to 20.59, n = 11) and 29.27 in the MBSR group (IQR 8.11 to 93.33, n = 13; reported P value = 0.03). The median per cent improvement at six months was 8.0 in the yoga group (IQR 5.17 to 17.39, n = 10) and 43.90 in the MBSR group (IQR 2.92 to 84.62, n = 10; reported P value = 0.38). The median per cent improvement at one year was 13.04 in the yoga group (IQR 10.34 to 20.75, n = 9) and 36.09 in the MBSR group (IQR 4.55 to 79.76, n = 12; reported P value = 0.52). The trialists carried out intention‐to‐treat (ITT) analyses in which baseline values were carried forward for missing participants and results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Secondary outcome measures
Number of micturitions (daily)
Not reported.
Number of episodes of incontinence (daily)
There was very low‐certainty evidence that women in the MBSR group had a greater reduction in number of daily urinary incontinence episodes compared to women in the yoga group at each outcome assessment time. The median per cent improvement at eight weeks was ‐33.33 in the yoga group (IQR ‐50.00 to 16.67, n = 11) and ‐60 in the MBSR group (IQR ‐88.89 to ‐50.00, n = 13; reported P value = 0.03). The median per cent improvement at six months was ‐22.62 in the yoga group (IQR ‐50.00 to ‐16.67, n = 10) and ‐71.43 in the MBSR group (IQR ‐100.00 to ‐40.00, n = 10; reported P value = 0.01). The median per cent improvement at one year was ‐41.67 in the yoga group (IQR ‐66.67 to ‐28.57, n = 9) and ‐69.11 in the MBSR group (IQR ‐91.43 to ‐49.17, n = 12; reported P value = 0.04). The trialists carried out ITT analyses in which baseline values were carried forward for missing participants and the results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Urine loss as measured with a pad or paper towel weight test
Not reported.
Symptoms as reported by study participants on any condition‐specific scale
Not reported.
Clinical assessment of presence of incontinence
Not reported.
Measurement of pelvic floor muscle function
Not reported.
Quality of life measured on a scale that is not condition‐ or symptom‐specific
Not reported.
Depression, anxiety or distress
Not reported.
Other measures of emotional and social impact of the disorder
There was very low‐certainty evidence that women in the MBSR group had greater reductions in bothersomeness compared to women in the yoga group, as measured on the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF). The score from this six‐item scale is transformed into a 0‐to‐100 scale in which higher scores reflect greater bother and impact. The median per cent change at eight weeks was ‐25.0 in the yoga group (IQR ‐35 to 20, n = 11) and ‐55.6 in the MBSR group (IQR ‐50 to ‐87, n = 13; reported P value = 0.005). The median per cent improvement at six months was ‐25 in the yoga group (IQR ‐30 to ‐11.67, n = 10) and ‐54.13 in the MBSR group (IQR ‐66.67 to 0, n = 10; reported P value = 0.13). The median per cent improvement at one year was ‐35.29 in the yoga group (IQR ‐50 to ‐8.33, n = 9) and ‐73.91 in the MBSR group (IQR ‐80 to ‐9.52, n = 12; reported P value = 0.14). The trialists carried out ITT analyses in which baseline values were carried forward for missing participants and the results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Adverse effects
Not reported.
Yoga plus an intervention versus the same intervention without yoga
We did not find any eligible trials for this comparison.
Sensitivity analyses
We planned to assess the robustness of our conclusions by excluding studies that we judged to have a high risk of bias from our meta‐analyses for the primary outcomes. However, only a single study was included for each comparison.
For one included study, both available‐case and imputed data were reported but we were unable to extract data from any analyses into Review Manager 5. We have reported both available‐case and imputed analysis information from the study publication.
For the other study, we extracted information for analyses adjusted for outcomes at baseline and included this sensitivity analysis in the reporting of results from the study.
Discussion
Summary of main results
We identified two small, short‐term studies examining yoga for women with incontinence for inclusion in the review. One study compared six weeks of yoga to a waiting list in women with either urgency or stress urinary incontinence (Huang 2014a), while the other study compared eight weeks of MBSR to a yoga intervention in women with urgency urinary incontinence (Baker 2014). Comparisons between yoga and a waiting list generally favoured the yoga intervention, while comparisons between MBSR and yoga generally favoured the MBSR intervention. However, both studies were very small and had issues related to risk of bias. We did not find any trials that compared yoga plus an intervention against the same intervention without yoga. Consequently, there was insufficient information to draw conclusions about whether yoga is effective in treating either urgency or stress urinary incontinence in women. We identified no potentially relevant economic evaluations.
Overall completeness and applicability of evidence
The included studies involved women with a minimum frequency of urinary incontinence. One study included women with urgency urinary incontinence (Baker 2014). Huang 2014a included women with either urgency or stress urinary incontinence, although the majority had urgency incontinence. The study comparing yoga to MBSR was designed to test the effects of MBSR, with yoga as an active control arm that was not intended to improve incontinence. Both studies provided short‐term interventions of eight weeks or less, and although one study followed participants for one year after randomisation (Baker 2014), there was substantial attrition from both study arms at all outcome assessment times. There is very limited evidence on the short‐ or long‐term effectiveness of yoga compared to no intervention or MBSR, and a lack of evidence concerning yoga compared to other active interventions or as an adjunct to active interventions.
Quality of the evidence
Study limitations (risk of bias)
We identified no serious concerns about randomisation, allocation concealment or selective reporting. Both studies were unblinded and were therefore susceptible to performance bias. In Huang 2014a, all outcomes were self‐assessed and we therefore judged this study to be at risk of detection bias due to outcome assessment by unblinded participants. While Baker 2014 also relied upon participant‐assessed outcomes, the study had two active intervention groups, which may have mitigated bias resulting from outcome assessment by unblinded participants. However, Baker 2014 had high levels of attrition, which varied between study groups, at each outcome assessment time. We downgraded the certainty of the evidence from Huang 2014a once for risk of performance bias and once for risk of detection bias, and downgraded the certainty of the evidence from Baker 2014 once for risk of performance bias and once for risk of attrition bias.
Consistency
As there was only one study for each comparison, consistency could not be assessed.
Indirectness
There was no indirectness in Huang 2014a. The study comparing MBSR and yoga included yoga as an 'active' control group for MBSR, which was the intervention of interest (Baker 2014). The yoga intervention was a restorative yoga programme that was not designed to improve incontinence. We therefore downgraded the certainty of the evidence for each outcome from Baker 2014 for indirectness.
Imprecision
The studies were very small, therefore we downgraded the certainty of the evidence from both studies once for imprecision.
Publication bias
We consulted with experts, handsearched conference proceedings, and searched trial registers and identified no additional unpublished studies aside from a recently completed trial, which we will assess for inclusion when the authors publish the results in full. We did not downgrade the certainty of the evidence for publication bias.
We downgraded the certainty of the evidence for each outcome in the comparison of yoga to a waiting list to very low (Huang 2014a). We downgraded the evidence one level due to risk of performance bias, one level due to risk of detection bias and one level due to imprecision. We downgraded the certainty of the evidence for each outcome in the comparison of yoga to MBSR to very low (Baker 2014). We downgraded the evidence one level due to risk of performance bias, one level due to risk of attrition bias, one level due to indirectness and one level due to imprecision.
Potential biases in the review process
The Cochrane Incontinence Specialised Register and the Cochrane Complementary Medicine Field Specialised Register draw upon multiple sources of trials and we believe that our searches of these registers, together with searches of trial registers, identified all existing relevant trials. However, we cannot rule out that searches of additional specialised databases might have identified additional trials.
Agreements and disagreements with other studies or reviews
There are no other systematic reviews focusing on yoga for incontinence in women. We found one systematic review of non‐surgical treatments for incontinence in women that mentioned yoga and identified the same two trials that are included in this review (AHRQ 2018). The review grouped yoga with other interventions such as education, biofeedback, electroacupuncture and weight loss into the category of behavioural interventions, and did not report conclusions specific to yoga.
Authors' conclusions
Implications for practice.
Comparisons between yoga and a waiting list generally favoured the yoga intervention, while comparisons between mindfulness‐based stress reduction (MBSR) and yoga generally favoured the MBSR intervention, based on studies with very low‐certainty evidence. However, the limited number and size of studies prevented us from drawing any firm conclusions about the effectiveness of yoga for treating incontinence in women. Regarding safety, the included trial that assessed adverse events found very low‐certainty of no evidence of a difference between yoga and wait‐list groups in the number of women who experienced one or more non‐serious adverse events (Huang 2014a). This is consistent with previous evidence from observational studies and randomised trials indicating that yoga is a relatively safe practice (Cramer 2013; Cramer 2015). Consequently, if women wish to try yoga for treating incontinence, it may be safe for them to do so but there is no reliable evidence for its effectiveness.
Implications for research.
There is a need for additional well‐conducted trials with sufficient sample sizes to determine the effectiveness of yoga as a primary or adjunct intervention for urinary incontinence in women. Future trials should either compare yoga to an active intervention that is supported by good evidence, such as pelvic floor muscle training, or compare yoga plus such active interventions to those interventions alone. It should also be noted that the available trials were conducted primarily in women with urge‐predominant urinary incontinence, which is less common than stress‐predominant urinary incontinence (Milsom 2017). Further research should therefore include women with stress‐predominant urinary incontinence. Finally, the outcomes of greatest relevance to women, including cure, improvement in symptoms, quality of life, and adverse effects, should be clearly and completely reported, together with clinician's observations and economic measures. Until such additional studies are conducted, it will not be possible to judge the effectiveness of yoga for urinary incontinence in women.
Acknowledgements
We are grateful to Dan Brundson, Chantale Dumoulin, Suzanne Hagen, Juliana Esther Martin‐Lopez, Vinutha P, Shaun Treweek and Luke Vale for valuable comments on drafts of this review.
We would like to thank Muhammad Imran Omar, Sheila Wallace and Soumyadeep Bhaumik for assistance in the development of the protocol. In addition, we are grateful for the contribution of Seveka Bali at the protocol stage. We also thank the editors and peer reviewers for Cochrane Incontinence and the staff of the Cochrane Editorial Unit for their input into the protocol.
Appendices
Appendix 1. Cochrane Incontinence Group Specialised Register search strategy
We used the following strategy to search the Cochrane Incontinence Specialised Register.
(({DESIGN.CCT*} OR {DESIGN.RCT*})
AND ({TOPIC.URINE.INCON*} OR {TOPIC.URINE.OVERACTIVE*} OR {TOPIC.URINE.frequency*} OR {TOPIC.URINE.URGENCY*})
AND {INTVENT.LIFESTYLE.YOGA.} OR {INTVENT.PHYS.YOGA.} OR {INTVENT.PHYS.Exercise.Yoga.} OR {INTVENT.PHYS.RELAXATION.} OR {INTVENT.PSYCH.Relaxation.} OR {INTVENT.PSYCH.MEDITATION.})
(All searches were of the keyword field of Reference Manager 2012.)
Appendix 2. NHS EED search strategies and searches for economic evaluations
NHS EED search strategies for economics evidence, developed by the Centre for Reviews and Dissemination (CRD) to populate NHS EED, are referenced in Section 15.3.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Shemilt 2011), and the most current versions can be found online at www.crd.york.ac.uk/crdweb/searchstrategies.asp.
The original broad searches for economic evaluations were conducted in MEDLINE, Embase and NHS EED on 25 September 2017 by a medical librarian. Further updated searches were run but due to the lack of relevant studies identified by the original broad searches a further updated search run on 22 January 2019 was more focused and included a set of urinary incontinence related terms that were combined with the economic evaluation filters and the set of yoga terms in both MEDLINE and Embase. The search of NHS EED was not updated as this database has not been updated since the original search.
MEDLINE search for NHS EED using OvidSP (developed by CRD)
| 1 | Economics/ |
| 2 | exp "costs and cost analysis"/ |
| 3 | Economics, Dental/ |
| 4 | exp economics, hospital/ |
| 5 | Economics, Medical/ |
| 6 | Economics, Nursing/ |
| 7 | Economics, Pharmaceutical/ |
| 8 | (economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. |
| 9 | (expenditure$ not energy).ti,ab. |
| 10 | value for money.ti,ab. |
| 11 | budget$.ti,ab. |
| 12 | or/1‐11 |
| 13 | (energy or oxygen) adj cost).ti,ab. |
| 14 | (metabolic adj cost).ti,ab. |
| 15 | ((energy or oxygen) adj expenditure).ti,ab. |
| 16 | or/13‐15 |
| 17 | 12 not 16 |
| 18 | letter.pt. |
| 19 | editorial.pt. |
| 20 | historical article.pt. |
| 21 | or/18‐20 |
| 22 | 17 not 21 |
| 23 | exp animals/ not humans/ |
| 24 | 22 not 23 |
| 25 | bmj.jn. |
| 26 | "cochrane database of systematic reviews".jn. |
| 27 | health technology assessment winchester england.jn. |
| 28 | or/25‐27 |
| 29 | 24 not 28 |
| 30 | limit 29 to yr="2014 ‐Current" |
MEDLINE on OvidSP (1946 to January Week 2 2019) ‐ searched 22 January 2019
1. Economics/
2. exp "costs and cost analysis"/
3. Economics, Dental/
4. exp economics, hospital/
5. Economics, Medical/
6. Economics, Nursing/
7. Economics, Pharmaceutical/
8. (economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab.
9. (expenditure$ not energy).ti,ab.
10. value for money.ti,ab.
11. budget$.ti,ab.
12. or/1‐11
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. or/13‐15
17. 12 not 16
18. letter.pt.
19. editorial.pt.
20. historical article.pt.
21. or/18‐20
22. 17 not 21
23. exp animals/ not humans/
24. 22 not 23
25. (incontinen$ or continen$).tw.
26. exp urinary incontinence/
27. nycturia.tw.
28. ((bladder or detrusor or vesic$) adj5 (instability or stab$ or unstable or irritab$ or hyperreflexia or dys?ynerg$ or dyskinesi$ or irritat$)).tw.
29. (urin$ adj2 (leak$ or urge$ or frequen$)).tw.
30. dribbl$.tw.
31. bladder, neurogenic/
32. ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw.
33. (spinal adj2 bladder$).tw.
34. (bladder$ adj2 (neuropath$ or neurogen$ or neurolog$)).tw.
35. (nervous adj1 (pollakisur$ or pollakiur$)).tw.
36. urinary bladder, overactive/
37. exp enuresis/
38. enure$.tw.
39. bedwet$.tw.
40. bed‐wet$.tw.
41. (bed adj5 wet$).tw.
42. (diurnal adj5 wet$).tw.
43. diurnal‐wet$.tw.
44. ((daytime or day‐time or nighttime or night‐time or nightime) adj5 wet$).tw.
45. (void$ adj2 dysfunct$).tw.
46. ((urin$ or bladder) adj5 sphincter$).tw.
47. (urethra$ adj2 sphincter$).tw.
48. (bladder adj2 neck).tw.
49. (vesic$ adj1 (neck$ or cervi$)).tw.
50. (detrusor adj1 sphincter$).tw.
51. or/25‐50
52. 24 and 51
53. 2014$.ed.
54. 2015$.ed.
55. 2016$.ed.
56. 2017$.ed.
57. 2018$.ed.
58. 2019$.ed.
59. 53 or 54 or 55 or 56 or 57 or 58
60. 52 and 59
61. yoga/
62. yoga.tw.
63. 61 or 62
64. 60 and 63
Embase search for NHS EED using OvidSP (developed by CRD)
| 1 | Health Economics/ |
| 2 | exp Economic Evaluation/ |
| 3 | exp Health Care Cost/ |
| 4 | pharmacoeconomics/ |
| 5 | 1 or 2 or 3 or 4 |
| 6 | (econom$ or cost or costs or costly or costing or price or prices or pricing or parmacoeconomic$).ti,ab. |
| 7 | (expenditure$ not energy).ti,ab. |
| 8 | (value adj2 money).ti,ab. |
| 9 | budget$.ti,ab. |
| 10 | 6 or 7 or 8 or 9 |
| 11 | 5 or 10 |
| 12 | letter.pt. |
| 13 | editorial.pt. |
| 14 | note.pt. |
| 15 | 12 or 13 or 14 |
| 16 | 11 not 15 |
| 17 | (metabolic adj cost).ti,ab. |
| 18 | ((energy or oxygen) adj cost).ti,ab. |
| 19 | ((energy or oxygen) adj expenditure).ti,ab. |
| 20 | 17 or 18 or 19 |
| 21 | 16 not 20 |
| 22 | animal/ |
| 23 | exp animal experiment/ |
| 24 | nonhuman/ |
| 25 | (rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. |
| 26 | 22 or 23 or 24 or 25 |
| 27 | exp human/ |
| 28 | human experiment/ |
| 29 | 27 or 28 |
| 30 | 26 not (26 and 29) |
| 31 | 21 not 30 |
| 32 | 0959‐8146.is. |
| 33 | (1469‐493X or 1366‐5278).is. |
| 34 | 1756‐1833.en. |
| 35 | 32 or 33 or 34 |
| 36 | 31 not 35 |
| 37 | conference abstract.pt. |
| 38 | 36 not 37 |
| 39 | limit 38 to yr="2014 ‐Current" |
Embase on OvidSP (1974 to 2019 Week 03) was searched on 22 January 2019
| 1. | Health Economics/ |
| 2. | exp Economic Evaluation/ |
| 3. | exp Health Care Cost/ |
| 4. | pharmacoeconomics/ |
| 5. | (econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. |
| 6. | (expenditure$ not energy).ti,ab. |
| 7. | (value adj2 money).ti,ab. |
| 8. | budget$.ti,ab. |
| 9. | or/1‐8 |
| 10. | letter.pt. |
| 11. | editorial.pt. |
| 12. | note.pt. |
| 13. | or/10‐12 |
| 14. | 9 not 13 |
| 15. | (metabolic adj cost).ti,ab. |
| 16. | ((energy or oxygen) adj cost).ti,ab. |
| 17. | ((energy or oxygen) adj expenditure).ti,ab. |
| 18. | 15 or 16 or 17 |
| 19. | 14 not 18 |
| 20. | animal/ |
| 21. | exp animal experiment/ |
| 22. | nonhuman/ |
| 23. | (rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. |
| 24. | 20 or 21 or 22 or 23 |
| 25. | exp human/ |
| 26. | human experiment/ |
| 27. | 25 or 26 |
| 28. | 24 not (24 and 27) |
| 29. | 19 not 28 |
| 30. | conference abstract.pt. |
| 31. | 29 not 30 |
| 32. | incontinence/ or mixed incontinence/ or stress incontinence/ or urge incontinence/ or urine incontinence/ |
| 33. | continence/ |
| 34. | overactive bladder/ |
| 35. | micturition disorder/ or lower urinary tract symptom/ or pollakisuria/ |
| 36. | urinary dysfunction/ or bladder instability/ or detrusor dyssynergia/ or neurogenic bladder/ or urinary urgency/ or urine extravasation/ |
| 37. | (incontinen$ or continen$).tw. |
| 38. | ((bladder or detrusor or vesic$) adj5 (instab$ or stab$ or unstab* or irritab$ or hyperreflexi$ or dys?ynerg$ or dyskinesi$ or irritat$)).tw. |
| 39. | (urin$ adj2 leak$).tw. |
| 40. | ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw. |
| 41. | (bladder$ adj2 (neuropath$ or neurogen* or neurolog$)).tw. |
| 42. | (nervous adj pollakisur$).tw. |
| 43. | or/32‐42 |
| 44. | 31 and 43 |
| 45. | "2015".yr. |
| 46. | "2016".yr. |
| 47. | "2017".yr. |
| 48. | "2018".yr. |
| 49. | 45 or 46 or 47 or 48 |
| 50. | 44 and 49 |
| 51. | 44 and 49 |
| 52. | limit 51 to (conference abstracts or embase) |
| 53. | yoga/ |
| 54. | yoga.tw. |
| 55. | 53 or 54 |
| 56. | 52 and 55 |
Appendix 3. AMED test search strategy
AMED (Allied and Complementary Medicine): We performed a preliminary test search on AMED on OvidSP (covering 1985 to November 2015) on 30 November 2015 using the broad search strategy below to gauge roughly how many randomised trials there might be in the area of urinary incontinence, overactive bladder, or enuresis. After de‐duplication against the Cochrane Incontinence Group Specialised Register, we did not identify any additional records, therefore we will not search this database for the first version of this Cochrane Review.
| 1. | controlled clinical trial.pt. |
| 2. | randomized controlled trial.pt. |
| 3. | randomized controlled trials/ |
| 4. | random allocation/ |
| 5. | double blind method/ |
| 6. | single blind method/ |
| 7. | clinical trial$.pt. |
| 8. | exp clinical trial/ |
| 9. | placebos/ |
| 10. | placebo$.tw. |
| 11. | random$.tw. |
| 12. | research design/ |
| 13. | volunteer$.tw. |
| 14. | (clin$ adj25 trial$).tw. |
| 15. | ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw. |
| 16. | factorial.tw. |
| 17. | cross‐over studies/ |
| 18. | crossover.tw. |
| 19. | latin square.tw. |
| 20. | (balance$ adj2 block$).tw. |
| 21. | (animals not humans).sh. |
| 22. | or/1‐20 |
| 23. | 22 not 21 |
| 24. | exp clinical trial/ |
| 25. | (clinical trial or clinical trial phase iii or clinical trialb or clinical trials or comparative studies or comparative study or controlled clinical trial or controlled trial or evaluation studies or multicenter study or multicentre study or randomised controlled trial or randomized controlled trial).pt. |
| 26. | or/1‐20,24‐25 |
| 27. | 26 not 21 |
| 28. | toilet$.tw. |
| 29. | (incontinen$ or continen$).tw. |
| 30. | exp urinary incontinence/ or urination disorders/ |
| 31. | incontinence pads/ |
| 32. | urodynamics/ |
| 33. | urinary sphincter, artificial/ |
| 34. | urodynamic$.tw. |
| 35. | urinary catheterization/ or Urinary Catheters/ |
| 36. | bladder fistula/ or urinary fistula/ or urinary bladder fistula/ |
| 37. | toilet training/ |
| 38. | cutaneous fistula/ |
| 39. | vaginal fistula/ |
| 40. | vesicovaginal fistula/ |
| 41. | "pelvic floor"/ |
| 42. | pelvic floor disorders/ |
| 43. | (pelvi$ adj2 floor).tw. |
| 44. | perineomet$.tw. |
| 45. | interferential.tw. |
| 46. | cystitis, interstitial/ |
| 47. | nycturia.tw. |
| 48. | ((vesic$ or bladder or vagina$) adj5 (support$ or prosthes$)).tw. |
| 49. | (bladder adj6 (train$ or retrain$ or empt$)).tw. |
| 50. | mmk.tw. |
| 51. | marshall marchetti krantz.tw. |
| 52. | burch.tw. |
| 53. | ((bladder or neck or vesic$) adj5 suspen$).tw. |
| 54. | colposuspension$.tw. |
| 55. | guittes.tw. |
| 56. | colporrhaph$.tw. |
| 57. | pereyra.tw. |
| 58. | urethrosuspension$.tw. |
| 59. | cystoplast$.tw. |
| 60. | urethropex$.tw. |
| 61. | lyodura$.tw. |
| 62. | colpoperineoplast$.tw. |
| 63. | urethrocervicopex$.tw. |
| 64. | stamey.tw. |
| 65. | interstitial cystitis.tw. |
| 66. | (fistula$ adj5 (bladder or vesic$ or bladder‐vagina$ or urin$ or vagina$ or uretero‐vagina$ or ureterovagina$ or urogenital or genitourin$)).tw. |
| 67. | raz.tw. |
| 68. | ((urin$ or bladder) adj5 sphincter$).tw. |
| 69. | ((bladder or detrusor or vesic$) adj5 (instability or stab$ or unstable or irritab$ or hyperreflexia or dys?ynerg$ or dyskinesi$ or irritat$)).tw. |
| 70. | (void$ adj5 (prompt$ or diar$)).tw. |
| 71. | urethral syndrome.tw. |
| 72. | (urethra$ adj2 sphincter$).tw. |
| 73. | (bladder adj2 neck).tw. |
| 74. | (urin$ adj2 (leak$ or urge$ or frequen$)).tw. |
| 75. | urinary fistula/ |
| 76. | dribbl$.tw. |
| 77. | diaper$.tw. |
| 78. | bladder, neurogenic/ or bladder neurogenic/ or bladder disease/ |
| 79. | (bladder adj1 ulcer$).tw. |
| 80. | (hunner? adj1 ulcer$).tw. |
| 81. | (vesic$ adj1 (neck$ or cervi$)).tw. |
| 82. | cystostomy.tw. |
| 83. | cystostomy/ |
| 84. | vesicostom$.tw. |
| 85. | cystostom$.tw. |
| 86. | colporraph$.tw. |
| 87. | (fistula$ adj1 (urethra$ or colovesic$ or cystocol$ or cystovagina$ or vagino$)).tw. |
| 88. | (sling$ adj1 procedure$).tw. |
| 89. | (pelvi$ adj5 rehab$).tw. |
| 90. | ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw. |
| 91. | (urin$ adj2 extravasat$).tw. |
| 92. | ((urin$ or bladder or urethra$) adj1 (prosthes$ or endoprosthes$)).tw. |
| 93. | (detrusor adj1 sphincter$).tw. |
| 94. | (spinal adj2 bladder$).tw. |
| 95. | (bladder$ adj2 (neuropath$ or neurogen$ or neurolog$)).tw. |
| 96. | bodyworn$.tw. |
| 97. | underpad$.tw. |
| 98. | (nervous adj1 (pollakisur$ or pollakiur$)).tw. |
| 99. | urinary bladder, overactive/ |
| 100. | or/28‐99 |
| 101. | *prostate/ |
| 102. | *prostatectomy/ |
| 103. | *prostatic hyperplasia/ |
| 104. | *prostatic neoplasm/ |
| 105. | *prostatic neoplasms/ |
| 106. | *bladder neoplasms/ |
| 107. | *prostatitis/ |
| 108. | *prostatic diseases/ |
| 109. | or/101‐108 |
| 110. | 100 not 109 |
| 111. | 27 and 110 |
| 112. | exp enuresis/ |
| 113. | enure$.tw. |
| 114. | bedwet$.tw. |
| 115. | bed‐wet$.tw. |
| 116. | (bed adj5 wet$).tw. |
| 117. | (diurnal adj5 wet$).tw. |
| 118. | diurnal‐wet$.tw. |
| 119. | ((daytime or day‐time or nighttime or night‐time or nightime) adj5 wet$).tw. |
| 120. | urotherap*.tw. |
| 121. | (void$ adj2 dysfunct$).tw. |
| 122. | or/112‐121 |
| 123. | 27 and 122 |
Appendix 4. CINAHL preliminary search strategy
CINAHL (Cumulative Index to Nursing and Allied Health Literature): We tested the following search strategy in CINAHL (on EBSCOhost) on 2 December 2015 (covering December 1981 to the most recent entry date 1 December 2015). After de‐duplication against the Cochrane Incontinence Group Specialised Register, we did not retrieve any additional records, therefore we will not search CINAHL for this Cochrane Review.
| # | Query |
| S44 | S31 AND S43 |
| S43 | S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 |
| S42 | TX pranayama |
| S41 | TX kundalini |
| S40 | TX qigong |
| S39 | TX relax* |
| S38 | TX meditat* |
| S37 | TX yogic |
| S36 | TX yoga |
| S35 | (MH "Qigong") |
| S34 | (MH "Relaxation") OR (MH "Muscle Relaxation") |
| S33 | (MH "Relaxation Techniques") OR (MH "Meditation") |
| S32 | (MH "Yoga+") |
| S31 | S23 AND S30 |
| S30 | S24 OR S25 OR S26 OR S27 OR S28 OR S29 |
| S29 | TI overactiv* N3 bladder* OR AB overactiv* N3 bladder* |
| S28 | TI urin* N3 leak* OR AB urin* N3 leak* |
| S27 | TI ( incontinen* OR continen* ) OR AB ( incontinen* OR continen* ) |
| S26 | MH incontinence |
| S25 | MH overactive bladder |
| S24 | MH Urinary incontinence+ |
| S23 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 |
| S22 | TI ( singl* N25 blind* OR singl* N25 mask* OR doubl* N25 blind* or doubl* N25 mask* OR trebl* N25 blind* OR trebl* N25 mask*OR tripl* N25 blind* OR tripl* N25 mask* ) or AB ( singl* N25 blind* OR singl* N25 mask* OR doubl* N25 blind* or doubl* N25 mask* OR trebl* N25 blind* OR trebl* N25 mask*OR tripl* N25 blind* OR tripl* N25 mask* ) |
| S21 | (MH "Comparative Studies") |
| S20 | (MH "Clinical Research+") |
| S19 | (MH "Static Group Comparison") |
| S18 | (MH "Quantitative Studies") |
| S17 | (MH "Crossover Design") or (MH "Solomon Four‐Group Design") |
| S16 | (MH "Factorial Design") |
| S15 | (MH "Community Trials") |
| S14 | (MH "Random Sample") |
| S13 | TI balance* N2 block* or AB balance* N2 block* |
| S12 | TI "latin square" or AB "latin square" |
| S11 | TI factorial or AB factorial |
| S10 | TI clin* N25 trial* or AB clin* N25 trial* |
| S9 | (MH "Study Design") |
| S8 | (AB random*) OR (TI random*) |
| S7 | (AB placebo*) OR (TI placebo*) |
| S6 | (MH "Placebos") |
| S5 | PT Clinical Trial OR (PT "randomized controlled trial") |
| S4 | (MH "Clinical Trials+") |
| S3 | MH (random assignment) OR (crossover design) |
| S2 | cross‐over |
| S1 | crossover |
Appendix 5. IndMED preliminary strategy
IndMED: We performed a preliminary search of IndMED (www.indmed.nic.in/) on 2 December 2015 using the following terms in Advanced Strategy, applying no limits, and using the default setting to search in: Any Where.
yoga OR yogic OR meditation OR relaxation OR kundalini OR pranayama
AND
incontinent OR incontinence OR continent OR incontinence
Data and analyses
Comparison 1. Yoga versus no specific active intervention.
Comparison 2. Yoga versus an active intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks) | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.43] |
| 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months) | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.42] |
| 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year) | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.53] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Baker 2014.
| Methods |
Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified |
|
| Participants | 30 women with urge‐predominant urinary incontinence Types of incontinence: all women had urge‐predominant UI Diagnostic criteria for incontinence: not specified Severity and duration of incontinence: at baseline, the 3‐day average number of UI episodes for yoga participants was median 2.67 (range 1.67 to 6.33) and for MBSR participants was median 3.00 (1.67 to 9.33) Age: yoga median age 58 (range 22 to 79) years; MBSR median age 59 (range 34 to 74) years Pregnant/postpartum/menopausal status: "most were postmenopausal" Weight: BMI range 20.34 to 36.15 kg/m²; yoga median 25.82 (range 20.90 to 36.15) kg/m²; MBSR median 26.15 (range 20.34 to 33.22) kg/m² Recruitment: radio and newspaper within the community and poster advertisements at the university hospital, outpatient clinics and campus sites Inclusion criteria: "[W]omen aged 18 years or older who had 5 or more UUI episodes, with urge predominance (urge >50% of total incontinent episodes), on a 3‐day voiding diary." Exclusion criteria: "...anticholinergic medication use within 2 weeks of baseline assessments and past nonpharmacologic treatment of UUI such as supervised behavioral therapy, supervised or unsupervised physical therapy, supervised biofeedback transvaginal electrical stimulation, tibial nerve stimulation, sacral neuromodulation, and botulinum toxin bladder injections. Women were also excluded if they had a past diagnosis of painful bladder, interstitial cystitis, and/or neurological disorder.” |
|
| Interventions |
Yoga group: 8 weekly yoga classes following "basic principles of yoga" and focusing on physical poses and relaxation. "Information was given on restorative yoga that emphasized the use of gravity, props, and floor poses for muscle relaxation. No education was given on breathing techniques in this yoga control program. Class time was also spent on education about the 7 chakras, self‐massage, and essential oils and how they can also assist in muscle relaxation."
Teacher(s): the classes were taught by a certified massage therapist/yoga instructor Home practice: not described Mindfulness‐based stress reduction (MBSR) group: 8 weekly group meetings following the traditional protocol of the Center for Mindfulness at the University of Massachusetts Medical Center. "The 8‐week MBSR program is a structured program that teaches participants a variety of meditation practices, mindful‐yoga, walking meditation, and discussions on the relationship between stress, illness, and health." Teacher(s): the classes were taught by a licensed occupational therapist with teacher training in mindfulness‐based therapy Home practice: women were given 'A Mindfulness‐Based Stress Reduction Workbook' and 15‐ to 30‐minute tapes to listen to. Women were asked to record instances of formal and informal techniques used in home practice sessions. "On average, the participants did a structured practice 5 times/wk (range, <1‐15.4 times/wk) and unstructured practice 9.7 times/wk (range, <1‐22 times/wk)." Adherence to yoga and comparison interventions: 11/15 (73%) yoga participants and 13/15 (87%) MBSR participants completed at least 5 of 8 sessions Common interventions: women were asked not to seek any other incontinence treatment while participating in the study. No women received any of the usual treatments of UUI, including bladder education, fluid management, or pelvic floor muscle exercises. None of the group sessions focused on bladder control. Co‐interventions: no mention of included or excluded co‐interventions Duration and follow‐up: interventions were provided for 8 weeks with follow‐up visits at 6 and 12 months Number of withdrawals, with reasons: loss to follow‐up in the yoga group was 4/15 (27%) at 8 weeks, 5/15 (33.3%) at 6 months and 6/15 (40%) at 1 year. Loss to follow‐up in the MBSR group was 2/15 (13%) at 8 weeks, 5/15 (33.3%) at 6 months, and 3/15 (20%) at 1 year. It was not reported whether the women who did not complete follow‐up included withdrawals from treatment. Reasons for loss to follow‐up were not reported. |
|
| Outcomes |
Participant report of continence or improvement. Patient Global Impression of Improvement (PGI‐I). Women self reported their overall impression of improvement, and the outcome was dichotomised as much better or very much better versus other responses. Information reported at 8 weeks, 6 months and 1 year. Condition‐ or symptom‐specific quality of life. Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL). The OAB‐HRQL score is obtained from summing the 13 items on the HRQL subscales of the Overactive Bladder Symptom and Health‐Related Quality of Life Questionnaire (OAB‐q). This score is transformed to a 0‐to‐100 scale in which higher scores reflect better quality of life. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Quantification of symptoms: number of incontinence episodes. The 3‐day average of incontinence episodes was collected from a diary. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Other measures of social or emotional impact of incontinence. Bothersomeness, as measured on the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF). The score from this 6‐item scale is transformed to a 0‐to‐100 scale in which higher scores reflect greater bother and impact. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Other outcomes collected: urge incontinence episodes, daytime voids, nighttime voids and pad use |
|
| Notes | Adverse events: no discussion of safety or adverse events Measurement of expectations or treatment preferences at baseline: none Unpublished data: Dr Jan Baker emailed LSW the statistical analysis report and details of the calculation and interpretation of the OAB‐HRQL and the OABq‐SF measures, including the questionnaire and scoring manual, on 27 September 2017. No unpublished baseline or outcome data were used in the review. Funding: university and government. “This study was funded by an unrestricted grant from the University of Utah and was also supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant 8UL1TR000105 (formerly UL1RR025764).” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by shuffling 'security tint' envelopes; the Cochrane Handbook for Systematic Reviews of Interventions indicates that shuffling envelopes corresponds to a low risk of bias for sequence generation. "Randomization was completed by block randomization at each of the 3 periods to maintain an equal number in each group. When an accurate count was obtained of women who signed the consent for participation in a group session, group assignments were placed in security envelopes and shuffled. Subjects were then allowed to pick an envelope. The envelope was opened in front of the research personnel and was noted on the randomization key along with the subjects’ study number. This randomization key was then placed in a sealed envelope. The randomization key was given to the data manager and was noted as either group 1 or group 2 on the data spread sheet. The statistician was given the randomization key." |
| Allocation concealment (selection bias) | Low risk | "When an accurate count was obtained of women who signed the consent for participation in a group session, group assignments were placed in security envelopes and shuffled. Subjects were then allowed to pick an envelope." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | All participants and personnel were aware of the interventions being delivered. Study personnel may have been aware that MBSR was the intervention of interest and yoga considered an active control condition. |
| Blinding of outcome assessment (detection bias) Symptom improvement and quality of life | Unclear risk | All outcomes were assessed by the participants themselves, who were not blinded to the interventions. However, since both interventions were active, it is unclear to what extent this may have biased outcome assessment. |
| Blinding of outcome assessment (detection bias) Micturitions and incontinence episodes | Unclear risk | All outcomes were assessed by the participants themselves through diary entries, and the participants were not blinded to the interventions. However, since both interventions were active, it is unclear to what extent this may have biased outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were high rates of loss to follow‐up, and rates differed between groups. Loss to follow‐up in the yoga group was 4/15 (27%) at 8 weeks, 5/15 (33.3%) at 6 months, and 6/15 (40%) at 1 year. Loss to follow‐up in the MBSR group was 2/15 (13%) at 8 weeks, 5/15 (33.3%) at 6 months, and 3/15 (20%) at 1 year. Reasons for loss to follow‐up are not described. |
| Selective reporting (reporting bias) | Unclear risk | Study was registered and the primary and secondary outcomes from the trial registration are reported. However, only 2 of the secondary outcomes reported in the article are listed in the protocol. |
| Other bias | Low risk | Groups were comparable on baseline characteristics and the study appeared to be free of conflicts of interest related to funding. |
Huang 2014a.
| Methods |
Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified |
|
| Participants | 19 women with either stress or urgency urinary incontinence Types of incontinence: urgency‐predominant: all 12/19 (63%); yoga 6/10 (60%); control 6/9 (67%). Stress‐predominant: all 7/19 (37%); yoga 4/10 (40%); control 3/9 (33%). Diagnostic criteria for incontinence: not specified Severity and duration of incontinence: total incontinence episodes/day (based on 7‐day voiding diary) at baseline: yoga mean (SD) 2.77 (1.3); control mean (SD) 2.16 (1.2). Duration of incontinence not specified, but duration of 3 months or longer was an inclusion criterion. Age: yoga mean (SD) age 60.5 (8.4) years; control mean (SD) age 62.4 (8.3) years. Pregnant/postpartum/menopausal status: pregnancy in the last year was an exclusion criterion; menopausal status was not reported Weight: yoga BMI mean (SD) 24.7 (2.7) kg/m²; control BMI mean (SD) 25.8 (3.8) kg/m² Recruitment: "combination of newspaper advertisements, flyers posted in local community centers and businesses, and direct recruitment from clinician offices." Inclusion criteria: "[W]omen had to be at least aged 40 years, report experiencing incontinence for at least 3 months, and document at least 7 episodes of incontinence on a screening 7‐day voiding diary, with at least half of those episodes being stress‐type or urgency‐type incontinence." Exclusion criteria: "Women were excluded if they had severe mobility limitations that would prevent them from participating in a yoga therapy program (inability to walk up a single flight of stairs or at least 2 city blocks on level ground or an inability to stand up from a supine position unaided within 10 seconds) or if they reported formal yoga instruction within the past year or any prior use of yoga specifically to treat incontinence. Other exclusion criteria included pregnancy within the past 6 months; current urinary tract infection or hematuria (assessed by urine dipstick testing) or history of 3 or more urinary tract infections in the past year; major neurologic condition such as stroke, multiple sclerosis, or Parkinson disease; history of congenital defect leading to incontinence, fistula in the bladder or rectum, pelvic cancer or radiation, or interstitial cystitis or chronic pelvic pain; current symptomatic pelvic organ prolapse; body mass index greater than 35 kg/m2; or prior surgery to the urinary tract. Participants also could not have used practitioner‐supervised behavioral, pharmacological, or other clinical treatments (e.g. pessary) for incontinence within the past 3 months or be planning to initiate new clinical incontinence treatments during the study.” |
|
| Interventions |
Yoga group: 90‐minute Iyengar yoga classes were provided twice per week for 6 weeks. The class focus was on physical poses and relaxation. "Tadasana (mountain
pose), Utkatasana (chair pose), Trikonasana (triangle pose), Malasana (squat pose), Viparita Karani Variation (legs up the wall pose), Salamba Set Bandhasana (supported bridge pose), Supta Baddha Konasana (reclined cobbler’s pose), and Savasana (corpse pose). While teaching these postures, instructors emphasized specific ways of practicing each posture to foster awareness of the pelvic floor structures and increase control over the pelvic floor muscles, in addition to improving general fitness and conditioning and promoting mindfulness, deep breathing, and relaxation."
Teacher(s): classes were taught by an experienced certified instructor and an assistant Home practice: "Participants were also instructed to practice yoga at home for at least 1 additional hour per week and to record the dates and duration of practice in a home yoga diary. Participants were given a limited set of yoga props (mat, belt, and block) to take home and a manual with written descriptions and pictures depicting each of the key yoga postures featured in the classes. Tips on how to practice each posture safely and comfortably and how to adapt each posture to improve incontinence and pelvic floor function were also provided in the manual." Wait‐list control group: "Women randomized to the control group did not attend group yoga therapy classes and were instructed to avoid outside yoga instruction for 6 weeks. At the end of the 6‐week study, control group participants were given a $180 gift certificate for yoga classes at a local yoga studio and a limited set of home yoga props (block, mat, and strap) to take home." Adherence to yoga and comparison interventions: 9 (100%) women attended at least 1 group class, and 6/9 (67%) attended all group classes. 9 women (100%) completed at least 1 hour/week of home practice (self reported). Common interventions: women were given a pamphlet with standard education and behavioural management strategies for incontinence Co‐interventions: no mention of included or excluded co‐interventions Duration and follow‐up: interventions were provided for 6 weeks, and there was a telephone call at 3 weeks and a clinic visit at 6 weeks Number of withdrawals, with reasons: "After the randomization, but before the start of the yoga therapy program, 1 yoga therapy participant dropped out of the study citing worsened health." No other women in either group withdrew or were lost to follow‐up. |
|
| Outcomes |
Participant report of continence or improvement. Overall satisfaction with change in urine leakage was measured on a 5‐point Likert scale, ranging from ‘‘very unsatisfied’’ to ‘‘very satisfied’’, dichotomised as "moderately satisfied" or more versus less than "moderately satisfied". Assessed at 6 weeks. Condition‐ or symptom‐specific quality of life. “Incontinence Impact Questionnaire Short Form (IIQ‐7), a 7‐item measure of the impact of incontinence on physical activities, emotional health, travel, and social relationships.” The IIQ‐7 is measured on a scale from 0 to 100, with higher scores indicating more negative impact of incontinence upon activities, relationships and feelings. Mean (SD) of change is reported at 6 weeks. Quantification of symptoms: number of micturitions. The mean episodes/day of voiding in the toilet, as measured on a 7‐day voiding diary. Mean (SD) of change is reported at 6 weeks. Quantification of symptoms: number of incontinence episodes. The mean episodes/day of urinary incontinence, as measured on a 7‐day voiding diary. Mean (SD) of change is reported at 6 weeks. Other measures of social or emotional impact of incontinence. Bothersomeness, as assessed on the Urogenital Distress Inventory 6 (UDI‐6) (a 6‐item questionnaire that assesses subjective bother associated with incontinence‐related symptoms). Scale is 0 to 100, with higher scores indicating more negative impact of incontinence upon activities, relationships and feelings. Mean (SD) of change is reported at 6 weeks. Other outcomes collected: yoga adherence, yoga self efficacy, the Patient Perception for Bladder Condition (PPBC) ("a single‐item questionnaire assessing the degree to which participants consider their bladder condition to be a problem"), stress incontinence episodes/day, urgency incontinence episodes/day, daytime incontinence, nighttime incontinence, daytime voids and nighttime voids |
|
| Notes | Adverse events: “During a 3‐week telephone call and a 6‐week clinic visit, coordinators asked participants about any negative changes in their health and recorded any reported negative changes as adverse events on standardized forms. Adverse events were considered 'serious adverse events' if they met the standard definition of resulting in death, disability, or hospitalization. Participants were also encouraged to call study staff to report any negative changes in their health between scheduled calls or visits.” Measurement of expectations or treatment preferences at baseline: none Unpublished data: none Funding: university/non‐profit. "This research was supported by a University of California San Francisco Osher Center for Integrative Medicine Pilot Award from the Mt Zion Health Fund." Investigators also report receiving support from the National Institutes of Health and the American Federation for Aging Research. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Eligible participants were randomly assigned by a computer in a 1:1 ratio to participate in a 6‐week group‐based yoga therapy program (yoga therapy group) or receive no yoga instruction for 6 weeks followed by a gift certificate for local yoga studio classes (control group). Randomization was stratified by incontinence type (stress or stress‐predominant vs urgency or urgency‐predominant).” |
| Allocation concealment (selection bias) | Unclear risk | Although randomisation was carried out by computer, the exact procedures surrounding allocation were unclear. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and providers were aware of treatment assignment. |
| Blinding of outcome assessment (detection bias) Symptom improvement and quality of life | High risk | Participants self reported symptom improvement, bothersomeness and quality of life. They were not masked to their treatment assignments and the control condition was an inactive, waiting‐list control. |
| Blinding of outcome assessment (detection bias) Micturitions and incontinence episodes | Unclear risk | Participants recorded micturitions and incontinence episodes on 7‐day diaries, and the data were abstracted by masked assessors. However, since the participants were aware of treatment assignment, it is possible that this affected their assessment and recording of micturition and incontinence episodes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition from yoga group at follow‐up was 10% (1/10), and there was no attrition from the control group. |
| Selective reporting (reporting bias) | Unclear risk | Study appears to be free of selective reporting. The primary outcome was prespecified in the trial registration, however none of the reported secondary outcomes are mentioned in the trial registration. |
| Other bias | Low risk | Although groups were different on the IIQ‐7 and in frequency of voiding in toilets at baseline, this is consistent with simple randomisation of a small sample. Funding is university, non‐profit and government, and there is no indication of researcher bias. First author was previously funded by pharma, which is disclosed. |
BMI: body mass index IQR: interquartile range MBSR: mindfulness‐based stress reduction SD: standard deviation UI: urinary incontinence UUI: urgency urinary incontinence
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Burgio 2003 | Not an intervention of interest |
| Burgio 2006 | Not an intervention of interest |
| Felsted 2017 | Not an intervention of interest |
| Wein 2015 | Not a primary study report (i.e. editorial about study) |
| Wells 1999 | Not an intervention of interest |
Characteristics of studies awaiting assessment [ordered by study ID]
Huang 2018.
| Methods |
Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified |
| Participants | 50 women with at least daily urinary incontinence Types of incontinence: not reported Diagnostic criteria for incontinence: not reported Severity and duration of incontinence: not reported Age: mean 65 (8) years (range 55 to 83 years) Pregnant/postpartum/menopausal status: age greater than 50 was an inclusion criterion; menopausal status was not reported Weight: not reported Recruitment: not reported Inclusion criteria: "[A]mbulatory women aged 50 years or older who reported at least daily UI, were not already engaged in yoga, and were willing to temporarily forgo using clinical UI treatments." Exclusion criteria: not reported |
| Interventions |
Yoga group: twice‐weekly Iyengar yoga classes were provided twice per week for 3 months. The class focus was on specialised Iyengar‐style yoga techniques.
Teacher(s): not reported Home practice: once weekly Stretching control group: "a non‐specific muscle stretching/strengthening program designed to provide a rigorous time‐and‐attention control for the yoga program." Adherence to yoga and comparison interventions: 75% of women attended > 90% of group classes, and 88% of women completed > 90% of home practice hours. Adherence by group was not reported. Common interventions: women were given a brief instruction and written information on behavioural management strategies for incontinence Co‐interventions: no mention of included or excluded co‐interventions Duration and follow‐up: interventions were provided for 3 months, and outcomes were assessed at 3 months after baseline Number of withdrawals, with reasons: 6/56 (11%) of women withdrew. Withdrawals by group and withdrawal reasons were not reported. |
| Outcomes |
Quantification of symptoms: number of incontinence episodes. Change in mean episodes of urinary incontinence; how this was measured is not reported. Data for decrease in total UI frequency in the 2 groups are provided, together with P value for comparison between groups, but this cannot be used in a data analysis because the number of participants in each group is unclear. Other outcomes collected: not reported |
| Notes | Adverse events: no discussion of safety or adverse events Measurement of expectations or treatment preferences at baseline: not reported Unpublished data: Dr Margaret Chesney emailed LSW a submitted conference abstract on 1 December 2017 Funding: not reported. Trial registration states that sponsors and collaborators are University of California, San Francisco and the National Center for Complementary and Integrative Health. |
UI: urinary incontinence
Differences between protocol and review
We originally planned to use Covidence to extract study data but chose to use a piloted data extraction spreadsheet in Microsoft Excel 2018 for ease of use. However, we did use Covidence for study screening.
We originally planned to search all conference proceedings for European Congress for Integrative Medicine (ECIM) and International Congress on Complementary Medicine Research (ICCMR) but were unable to obtain ECIM proceedings for 2008 and 2010 or ICCMR proceedings for 2006 to 2009.
We originally planned to include the secondary outcomes of 'urine loss as measured with a pad or paper towel weight test' and 'quality of life measured on a scale that is not condition‐ or symptom‐specific' in the 'Summary of findings' tables. However, as neither of the included studies reported these outcomes, we therefore chose to include the secondary outcomes of 'number of micturitions (daily)' and 'number of episodes of incontinence (daily)' in the 'Summary of findings' tables.
Contributions of authors
LSW: searched for studies, screened studies, extracted data, and carried out GRADE assessments. Contributed to writing the review and approved the final draft. NS: conceived the protocol, screened studies and extracted data. Contributed to writing the review and approved the final draft. ZSL: screened studies, extracted data, and carried out GRADE assessments. Contributed to writing the review and approved the final draft SP: conceived the protocol and screened studies. Contributed to writing the review and approved the final draft. DC: contributed to writing the review and approved the final draft. NS: screened studies, contributed to writing the review and approved the final draft.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research (NIHR), UK.
This project was supported by the National Institute for Health Research via Infrastructure funding to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health. The NIHR is the largest single funder of Cochrane Incontinence.
-
National Institutes of Health (NIH), USA.
This project was supported by the National Center for Complementary and Integrative Health (NCCIH) grant R24 AT001293. The views and opinions expressed herein are those of the protocol authors and do not necessarily reflect those of the NIH or the NCCIH.
Declarations of interest
LSW: none known. NS: none known. ZSL: none known. SP: none known. DC: none known. NS: none known.
New
References
References to studies included in this review
Baker 2014 {published and unpublished data}
- Baker J, Costa D, Guarino JM, Nygaard I. Comparison of mindfulness‐based stress reduction versus yoga on urinary urge incontinence: a randomized pilot study with 6‐month and 1‐year follow‐up visits. Female Pelvic Medicine & Reconstructive Surgery 2014;20(3):141‐6. [sr‐incont60609; PUBMED: 24763155] [DOI] [PubMed] [Google Scholar]
- NCT01470560. Mindfulness‐based stress reduction techniques and yoga for treatment of urinary urge incontinence (MBSR‐Yoga). clinicaltrials.gov/ct2/show/NCT01470560 (first received 11 November 2011). [sr‐incont49230]
Huang 2014a {published data only}
- Huang AJ, Chesney MA, Schembri M, Subak LL. Yoga to treat urinary incontinence in women: results of a pilot randomized trial. Female Pelvic Medicine & Reconstructive Surgery 2013;19(5 Suppl):S72‐3. [sr‐incont72783] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. A group‐based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. Female Pelvic Medicine & Reconstructive Surgery 2014;20(3):147‐54. [sr‐incont60608; PUBMED: 24763156] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. Yoga for urinary incontinence in middle‐aged and older women: results of a pilot randomized trial. Journal of General Internal Medicine 2014;29(1 Suppl):S261. [Abstract: Tracking ID #1926774; sr‐incont61847] [Google Scholar]
- Jenny HE, Subak LL, Chesney MA, Schembri M, Huang AJ. Yoga for urinary incontinence in middle‐aged and older women: results of a pilot randomized trial. Journal of the American Geriatrics Society 2014;62(Suppl s1):S98. [Abstract number B27; sr‐incont61850] [Google Scholar]
- NCT01672190. Lessening incontinence by learning yoga (LILY). clinicaltrials.gov/ct2/show/NCT01672190 (first received 24 August 2012). [sr‐incont49228]
References to studies excluded from this review
Burgio 2003 {published data only}
- Burgio KL, Goode PS, Locher JL, Richter HE, Roth DL, Wright KC, et al. Predictors of outcome in the behavioral treatment of urinary incontinence in women. Obstetrics and Gynecology 2003;102(5 Pt 1):940‐7. [sr‐incont17367; PUBMED: 14672467] [DOI] [PubMed] [Google Scholar]
Burgio 2006 {published data only}
- Burgio KL, Goode PS, Richter HE, Locher JL, Roth DL. Global ratings of patient satisfaction and perceptions of improvement with treatment for urinary incontinence: validation of three global patient ratings. Neurourology and Urodynamics 2006;25(5):411‐7. [sr‐incont22346; PUBMED: 16652380] [DOI] [PubMed] [Google Scholar]
Felsted 2017 {published data only}
- Felsted K, NCT03176901. Comparing approaches to treat older adult women's urge incontinence: pilot feasibility and randomized controlled trial (SHUW) [Comparing mindfulness‐based stress reduction with the health enhancement program in the treatment of urinary urge incontinence in older adult women: a pilot feasibility and randomized controlled trial]. clinicaltrials.gov/show/NCT03176901 (first received 6 June 2017). [NCT03176901; sr‐incont76187]
Wein 2015 {published data only}
Wells 1999 {unpublished data only}
- Wells T, Mayer R, Brink C, Brown R. Pelvic muscle exercise: a controlled clinical trial [notification of unpublished manuscript via personal communication]. Email to: Jean Hay‐Smith. 3 November 2008. [sr‐incont26977]
References to studies awaiting assessment
Huang 2018 {unpublished data only}
- Huang A, Chesney M, Schembri M, Subak L. A randomized trial of a group‐based therapeutic yoga program for ambulatory women with urinary incontinence. Journal of Urology 2018;199(4 Suppl):e645. [DOI: 10.1016/j.juro.2018.02.1544; Abstract number PD32‐01; sr‐incont77829] [DOI] [Google Scholar]
- NCT02342678. Lessening incontinence through low‐impact activity (LILA) [Lessening incontinence through low‐impact activity, a.k.a. yoga to enhance behavioral self‐management of urinary incontinence in women]. clinicaltrials.gov/ct2/show/NCT02342678 (first received 21 January 2015). [sr‐incont67528]
Additional references
Abrams 2013
- Abrams P, Andersson KE, Artibani W, Birder I, Bliss D, Brubaker L, et al. Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Incontinence: 5th International Consultation on Incontinence. Paris: ICUD‐EAU 2013, 2013:1895‐945.
AHRQ 2018
- Balk E, Adam GP, Kimmel H, Rofeberg V, Saeed I, Jeppson P, et al. Nonsurgical treatments for urinary incontinence in women: a systematic review update. Rockville (MD): Agency for Healthcare Research and Quality (AHRQ); 2018 August. Comparative Effectiveness Review No. 212. (Prepared by the Brown Evidence‐based Practice Center under Contract No. 290‐2015‐00002‐I for AHRQ and PCORI.) AHRQ Publication No.: 18‐EHC016‐EF. PCORI Publication No.: 2018‐SR‐03. Available at effectivehealthcare.ahrq.gov/topics/urinary‐incontinence‐update/final‐report‐2018. [DOI: 10.23970/AHRQEPCCER212] [DOI] [PubMed]
Ayeleke 2015
- Ayeleke RO, Hay‐Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD010551.pub3; PUBMED: 26526663] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barber 2001
- Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition‐specific quality of life instruments for women with pelvic floor disorders. American Journal of Obstetrics and Gynecology 2001;185(6):1388‐95. [PUBMED: 11744914] [DOI] [PubMed] [Google Scholar]
Bø 2000
- Bø K, Berghmans LC. Nonpharmacologic treatments for overactive bladder ‐ pelvic floor exercises. Urology 2000;55(5A Suppl):7‐11; discussion 14‐6. [PUBMED: 10767443] [PubMed] [Google Scholar]
Bø 2004
- Bø K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work?. International Urogynecology Journal and Pelvic Floor Dysfunction 2004;15(2):76‐84. [PUBMED: 15014933] [DOI] [PubMed] [Google Scholar]
Bø 2013
- Bø K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. Journal of Physiotherapy 2013;59(3):159‐68. [PUBMED: 23896331] [DOI] [PubMed] [Google Scholar]
Bø 2017
- Bø K, Frawley HC, Haylen BT, Abramov Y, Almeida FG, Berghmans B, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. International Urogynecology Journal 2017;28(2):191‐213. [PUBMED: 27921161] [DOI] [PubMed] [Google Scholar]
Cannon 2004
- Cannon TW, Damaser M. Pathophysiology of the lower urinary tract: continence and incontinence. Clinical Obstetrics and Gynecology 2004;47(1):28‐35. [PUBMED: 15024270] [DOI] [PubMed] [Google Scholar]
Clarke 2015
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002‐2012. Hyattsville (MD): National Center for Health Statistics. National Health Statistics Reports; no. 79. www.cdc.gov/nchs/data/nhsr/nhsr079.pdf (accessed 14 May 2018).
Covidence 2017 [Computer program]
- Veritas Health Innovation. Covidence. Version accessed 26 June 2018. Melbourne, Australia: Veritas Health Innovation, 2017.
Cramer 2013
- Cramer H, Krucoff C, Dobos G. Adverse events associated with yoga: a systematic review of published case reports and case series. PLoS ONE 2013;8(10):e75515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cramer 2015
- Cramer H, Ward L, Saper R, Fishbein D, Dobos G, Lauche R. The safety of yoga: a systematic review and meta‐analysis of randomized controlled trials. American Journal of Epidemiology 2015;182(4):281‐93. [PUBMED: 26116216] [DOI] [PubMed] [Google Scholar]
Cramer 2016
- Cramer H, Ward L, Steel A, Lauche R, Dobos G, Zhang Y. Prevalence, patterns, and predictors of yoga use: results of a U.S. nationally representative survey. American Journal of Preventive Medicine 2016;50(2):230‐5. [PUBMED: 26497261] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
DeLancey 1988
- DeLancey JOL. Anatomy and mechanics of structures around the vesical neck: how vesical position may affect its closure. Neurourology and Urodynamics 1988;7:161‐2. [Google Scholar]
Dumoulin 2018
- Dumoulin C, Cacciari LP, Hay‐Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2018, Issue 10. [DOI: 10.1002/14651858.CD005654.pub4; PUBMED: 30288727] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction ‐ GRADE evidence files and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso‐Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence ‐ imprecision. Journal of Clinical Epidemiology 2011;64(12):1283‐93. [DOI] [PubMed] [Google Scholar]
Haylen 2010
- Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. International Urogynecology Journal 2010;21(1):5‐26. [PUBMED: 19937315] [DOI] [PubMed] [Google Scholar]
Herderschee 2011
- Herderschee R, Hay‐Smith EJ, Herbison GP, Roovers JP, Heineman MJ. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009252; PUBMED: 21735442] [DOI] [PubMed] [Google Scholar]
Hewitt 2001
- Hewitt J. The Complete Yoga Book. New York: Schocken Books Inc, 2001. [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG, editor(s). Chapter 16: Special topics in statistics. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Huang 2014b
- Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. A group‐based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. Female Pelvic Medicine & Reconstructive Surgery 2014;20(3):147‐54. [PUBMED: 24763156] [DOI] [PMC free article] [PubMed] [Google Scholar]
Imamura 2015
- Imamura M, Williams K, Wells M, McGrother C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2015, Issue 12. [DOI: 10.1002/14651858.CD003505.pub5; PUBMED: 26630349] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2015
- Kim GS, Kim EG, Shin KY, Choo HJ, Kim MJ. Combined pelvic muscle exercise and yoga program for urinary incontinence in middle‐aged women. Japan Journal of Nursing Science: JJNS 2015;12(4):330‐9. [PUBMED: 25705816] [DOI] [PubMed] [Google Scholar]
Long 2008
- Long RM, Giri SK, Flood HD. Current concepts in female stress urinary incontinence. Surgeon 2008;6(6):366‐72. [PUBMED: 19110826] [DOI] [PubMed] [Google Scholar]
Lose 2001
- Lose G, Fantl JA, Victor A, Walter S, Wells TL, Wyman J, et al. Outcome measures for research in adult women with symptoms of lower urinary tract dysfunction. Acta Obstetricia et Gynecologica Scandinavica 2001;80(11):981‐5. [DOI: 10.1034/j.1600-0412.2001.801102.x] [DOI] [PubMed] [Google Scholar]
Microsoft Excel 2018 [Computer program]
- Microsoft Corporation. Microsoft Excel for Mac. Version 16.20. Redmond, WA, USA: Microsoft Corporation, 2018.
Miller 1998
- Miller JM, Ashton‐Miller JA, DeLancey JO. A pelvic muscle precontraction can reduce cough‐related urine loss in selected women with mild SUI. Journal of the American Geriatrics Society 1998;46(7):870‐4. [PUBMED: 9670874] [DOI] [PubMed] [Google Scholar]
Milsom 2017
- Milsom I, Altman D, Cartwright R, Lapitan MC, Nelson R, Sjöström S, et al. Epidemiology of urinary incontinence (UI) and other lower urinary tract symptoms (LUTS), pelvic organ prolapse (POP) and anal (AI) incontinence. Incontinence: 6th International Consultation on Incontinence. Bristol UK: International Continence Society, 2017:5‐93. [ISBN: 978‐0‐9569607‐3‐3]
Minassian 2013
- Minassian VA, Devore E, Hagan K, Grodstein F. Severity of urinary incontinence and effect on quality of life in women by incontinence type. Obstetrics and Gynecology 2013;121(5):1083‐90. [PUBMED: 23635747] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Monz 2007
- Monz B, Chartier‐Kastler E, Hampel C, Samsioe G, Hunskaar S, Espuna‐Pons M, et al. Patient characteristics associated with quality of life in European women seeking treatment for urinary incontinence: results from PURE. European Urology 2007;51(4):1073‐81; discussion 1081‐2. [PUBMED: 17081676] [DOI] [PubMed] [Google Scholar]
Nystrom 2015
- Nystrom E, Sjostrom M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourology and Urodynamics 2015;34(8):747‐51. [PUBMED: 25154378] [DOI] [PubMed] [Google Scholar]
Park 2014
- Park CL, Groessl E, Maiya M, Sarkin A, Eisen SV, Riley K, et al. Comparison groups in yoga research: a systematic review and critical evaluation of the literature. Complementary Therapies in Medicine 2014;22(5):920‐9. [PUBMED: 25440384] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patrick 1999
- Patrick DL, Martin ML, Bushnell DM, Yalcin I, Wagner TH, Buesching DP. Quality of life of women with urinary incontinence: further development of the incontinence quality of life instrument (I‐QOL). Urology 1999;53(1):71‐6. [PUBMED: 9886591] [DOI] [PubMed] [Google Scholar]
Reference Manager 2012 [Computer program]
- Thomson Reuters. Reference Manager Professional Edition. Version 12. New York: Thomson Reuters, 2012.
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sandvik 1993
- Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. Journal of Epidemiology and Community Health 1993;47(6):497‐9. [PUBMED: 8120507] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shemilt 2011
- Shemilt I, Mugford M, Byford S, Drummond M, Eisenstein E, Knapp M, et al. Chapter 15: Incorporating economics evidence. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Sinclair 2011
- Sinclair AJ, Ramsay IN. The psychosocial impact of urinary incontinence in women. Obstetrician & Gynaecologist 2011;13(3):143‐8. [DOI: 10.1576/toag.13.3.143.27665] [DOI] [Google Scholar]
Steers 2002
- Steers WD. Pathophysiology of overactive bladder and urge urinary incontinence. Reviews in Urology 2002;4 Suppl 4:S7‐18. [PUBMED: 16986023] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta‐analyses of randomised controlled trials. BMJ (Clinical research ed.) 2011;343:d4002. [PUBMED: 21784880] [DOI] [PubMed] [Google Scholar]
Taneja 2014
- Taneja DK. Yoga and health. Indian Journal of Community Medicine 2014;39(2):68‐72. [PUBMED: 24963220] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tenfelde 2014
- Tenfelde S, Logan R, Abernethy M. Yoga from the pelvic floor. Beginnings (American Holistic Nurses' Association) 2014;34(1):24‐6. [PUBMED: 24683704] [PubMed] [Google Scholar]
Uebersax 1995
- Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourology and Urodynamics 1995;14(2):131‐9. [PUBMED: 7780440] [DOI] [PubMed] [Google Scholar]
Wallace 2004
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD001308.pub2; PUBMED: 14973967] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wieland 2013
- Wieland LS, Manheimer E, Sampson M, Barnabas JP, Bouter LM, Cho K, et al. Bibliometric and content analysis of the Cochrane Complementary Medicine Field specialized register of controlled trials. Systematic Reviews 2013;2:51. [PUBMED: 23826877] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wójtowicz 2014
- Wójtowicz U, Plaszewska‐Zywko L, Stangel‐Wójcikiewicz K, Basta A. Barriers in entering treatment among women with urinary incontinence. Ginekologia Polska 2014;85(5):342‐7. [PUBMED: 25011214] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Wieland 2017
- Wieland LS, Shrestha N, Lassi ZS, Panda S, Chiaramonte D, Skoetz N. Yoga for treatment of urinary incontinence in women. Cochrane Database of Systematic Reviews 2017, Issue 5. [DOI: 10.1002/14651858.CD012668] [DOI] [PMC free article] [PubMed] [Google Scholar]


