Abstract
Aims.
To describe implementation of diabetes and hypertension program in rural Dominican Republic (DR), and report six years of quality improvement process and health outcomes.
Methods.
Dominican teams at two clinics are supported by Chronic Care International with: supervision and continuing education, electronic database, diabetes and hypertension protocols, medications, self-management education materials, behavior change techniques, and equipment and testing supplies (e.g., HbA1c, lipids, blood pressure, BMI). A monthly dashboard for care processes and health outcomes guides problem solving and goal setting. Results were analyzed for quality improvement reports and by fitting the clinical data to random-effects linear models.
Results.
1191 adults were enrolled in the program at two clinics (44% men, baseline means: 56.4 years, BMI 27.4 kg/m2, HbA1c 8.8% (73 mmol/mol), BP 133/81 mmHg). Data show steady growth in clinic populations reaching capacity. Protocols for comprehensive foot examinations, BP and HbA1c assessments, and proportions reaching quality measures improved over time, especially after clinic goal setting. Modeling of BP, BMI and HbA1c values revealed important differences in outcomes by clinic over time.
Conclusions.
Improvements in process and health outcomes are attainable in rural DR when medical teams have support and access to data. Scalability and sustainability are continuing goals.
1. Introduction
Chronic non-communicable diseases (NCDs) such as diabetes, hypertension, and cardiovascular disease have rapidly emerged as leading causes of morbidity and mortality in both wealthy and developing countries. Health care systems in developing countries have traditionally been focused on the management of maternal-infant care, acute illnesses, infectious diseases, and surgical problems. The emergence of this NCD epidemic calls for new approaches in health care delivery.[1 2]
The World Health Organization (WHO) published its first Global Report on Diabetes in 2016; this report showed that the number of adults with diabetes in 2014 was 442 million, nearly four times the number in 1980. The WHO postulated that this increase was due to increases in type 2 diabetes, overweight and obesity.[3] The International Diabetes Federation (IDF) highlights the extent to which the poor are affected by diabetes, with 80% of those with diabetes globally residing in developing countries.[2] Combined with the approximately 1.4 billion individuals with hypertension, these two conditions, which often co-exist, represent an alarming health crisis.[4]
The Dominican Republic (DR) is a Caribbean country of approximately 10 million people and encompasses 2/3 of the island of Hispaniola. Much of the population lives in poverty, especially in the rural areas where access to clean water and electricity is inconsistent and variable. The World Bank estimates the poverty level in the Dominican Republic at 41.1% in 2013, and estimates 1.5 doctors per 1000 people.[5] Despite attempts by the government to address public health needs, access to health care and medications for many is inadequate or expensive. Services are often rudimentary and limited, especially in rural areas.
The prevalence of diabetes in the DR in 2015 was estimated at 8.1% [6], with the WHO estimating 9.3% diabetes prevalence in 2016.[7] Complications of diabetes and hypertension, such as ischemic heart disease and cerebrovascular disease, together with diabetes account for 57.7% of premature deaths in the DR.[8] The top four risk factors that drive the most death and disability combined include high systolic blood pressure, high body mass index, high fasting glucose, and dietary risks.[8]
The program described in this paper has been a joint effort between the Institute of Latin American Concerns (ILAC), Centro de Educación de la Salud Integral (CESI) and Chronic Care International (CCI). The ILAC non-profit organization has a history of more than 40 years of providing educational experiences for US students and professionals through health services and education for rural Dominicans. Its Dominican non-profit arm, CESI, also supports a cooperadores de salud (i.e., health promoter) program training more than 160 individuals to improve the health of their communities. Chronic Care International (CCI) is a US non-profit, non-governmental organization focusing on innovative health program implementation and quality improvement for chronic disease management in low resource countries. The diabetes and hypertension program was initiated in the DR by this partnership in 2010. The purpose of this report is to describe implementation of the CCI diabetes and hypertension program in rural DR, and to report process and intermediate health outcomes from six years of the program. This quality improvement program was approved by the Institutional Review Board of Creighton University in Omaha, Nebraska, USA, the academic institution affiliated with ILAC.
2. Subjects, Materials and Methods
2.1. Subjects and Setting.
The CCI program goal is to improve the quality of health care and outcomes for diabetes and hypertension in poor, rural, adult Dominicans. Patients evaluated and entered into the CCI program are all adults ≥ 20 years with hypertension and/or type 2 diabetes. The majority of patients are Dominican, with a small minority of Haitian origin.
2.2. The Intervention Model.
This program design draws on the key areas of the Chronic Care Model,[9] and also focuses on the larger issues of program sustainability by developing community and organizational collaborations. Key elements of the CCI program include: self-management education and support by health promoters; provider decision support; delivery system redesign; and information technology, e.g. use of an electronic disease registry. The final outcomes sought by the program are consistent with the Chronic Care Model, i.e., seeking to have improved patient outcomes through capacity-building interactions of informed, activated patients and prepared, proactive care teams within a supportive community.[10]
2.3. Program Initiation.
In 2009, a two-day needs assessment was conducted during which nearly 400 diabetes patients were screened for hypertension and eye, kidney and lower extremity complications, including their BMI and diabetes control. Due to the high prevalence of these conditions, a targeted diabetes and hypertension treatment program was begun by CCI. [11]
This program was initiated in 2010 in one rural area (or campo) in the north central region of the Dominican Republic (Clinic A), and was subsequently spread in July 2012, to a second site (clinic B) in another rural area southeast of Santiago. These CCI clinics serve at least 30 rural communities. The number of patients in the program has grown over time through community screenings and subsequently via word of mouth.
2.4. Program Implementation.
Staffing across the two clinics includes three Dominican physicians, two nurses, eight health promoters, and a Haitian program manager. The physicians were all trained in the DR, have general medical degrees and, prior to being selected, had one year of clinical experience through social service required by the Dominican government. The Dominican nurses trained in general nursing. Health promoters were trained in general community health through the established program at ILAC.
The DR health care team receives several forms of focused training every 3–4 months by the US team of physicians and nurse certified diabetes educators. A series of one-page, single-theme topic sheets covering diabetes and hypertension self-management topics was developed for both staff and patient education. In addition, the DR team utilizes audio-novella diabetes self-management education programs, e.g., “La Historia de Rosa” [12]; these are especially effective tools for lower-literacy populations. The Dominican team also receives expert coaching and worksheets for counseling techniques for promoting behavior change (e.g., for problem solving and goal setting) which they utilize in patient interactions. [13] Algorithms for evaluating and treating diabetes, hypertension and dyslipidemia were developed for standardization of patient evaluation and treatment; program physicians were trained in their use. These protocols are based on US standards of care.[14 15]
The equipment and testing supplies, along with quality assurance instructions, provided by CCI in both facilities include: automated blood pressure monitors, floor scales, point-of-care analyzers for glycosylated hemoglobin (HbA1c) (NGSP/IFCC certified) and lipids, capillary blood glucose meters and, when available, devices for assessing point-of-care kidney function and electrolytes.
2.5. Patient Care Protocols.
On entry into the program, patients undergo a complete history and physical examination by a physician, along with baseline laboratory testing including lipids, creatinine, potassium, glucose, and an HbA1c if they had a high blood glucose value or a diagnosis of diabetes. On subsequent visits, e.g., every 1 to 3 months, patients receive: weight measurement with body mass index (BMI) calculated; blood pressure, blood glucose, with HbA1c is assessed every 3 months for those with diabetes. The nurse’s role focuses on dispensing medications, counseling for medication adherence and safety (e.g., hypoglycemia self-management education), along with laboratory testing. At each clinic session health promoters present the aforementioned self-management topics which are rotated monthly; they also perform many vital clinic tasks as well as doing home visits. The patient has a physician consultation at each medical visit and appropriate oral medications are prescribed. Although insulin may be prescribed, the CCI program does not yet have the resources to provide it and patients are advised on how to obtain this medication.
Medications dispensed to patients are from a generic formulary included on the DR list of essential medications and are available in the DR. Anti-hypertensives include hydrochlorothiazide, lisinopril, losartan, amlodipine, and atenolol. Anti-diabetes medications include metformin and glipizide; insulin (NPH, regular, and 70/30) may be prescribed to selected patients for purchase in the DR. Simvastatin is provided for cholesterol management. Recently, gabapentin was added to the formulary for painful diabetic neuropathy and sertraline was added as an anti-depressant. Both conditions are frequently occurring co-morbidities of diabetes. Medications are obtained through three main sources: donations from a US-based company called Direct Relief, medications purchased by CCI in the US and Europe which are imported into the DR, and medications directly purchased by patients in the DR (e.g., insulins). All medications brought into the DR by CCI meet the country requirment of having expiration dates greater than six months from time of entry.
The program is primarily focused on prevention of diabetes and hypertension complications and, because of limited resources, less towards the treatment of advanced complications. Weight management through healthy eating and physical activity is a program priority for all diabetes and hypertension patients and as primary prevention of type 2 diabetes for those at risk. For diabetes complications such as kidney failure, vision loss and unstable cardiovascular disease, patients are referred to either the public hospital system or to the Diabetes Institute in Santiago, a multi-specialty facility for management of most of these complications. Consultations at the Diabetes Institute are provided at no cost to CCI patients; the Institute is reimbursed by CCI through in-kind medication donations.
2.6. Data Management.
Specific demographic and medical data are entered for each patient encounter on a Microsoft Access database called “Salud” developed by the CCI medical director (HJD), a physician experienced in the design and use of patient registries and electronic health records. This data management system was initiated in February of 2012; data from 2010–2012 had been captured in Microsoft Excel were imported to the Salud database at the time of its inception.
Data collection follows a standardized process in CCI clinics; data are recorded on paper forms during each patient encounter and subsequently entered on a laptop computer by a program physician. Upon closing the database daily, data are programmatically extracted to a series of Microsoft® Excel sheets by data type (e.g. demographics, labs, vital signs, etc.) and synced automatically with a shared Dropbox® folder, thereby becoming available to the US CCI medical director. Data security is managed through passwords protecting computers on which data are stored and via the Dropbox security policies and procedures utilized by this cloud storage/file sharing system.
Data are used for five purposes: quality improvement, population outreach, patient case management for Dominican and US medical teams, program operations, and transparency. Each of these areas is essential to optimize health outcomes and enhance the quality and sustainability of CCI’s program. Various reports are routinely generated from the database to support these purposes. The output from key reports is tracked on a monthly basis in an organizational dashboard. Data points tracked on the dashboard have expanded over time and include the measurements:
Total number of active patients
Number of physician visits per month
Percentage of diabetes patients who had an HbA1c performed within last 4 months
Percentage of diabetes patients whose last HbA1C was less than 9% (<75mmol/mol)
Percentage of hypertension patients who had a blood pressure checked in last 4 months
Percentage of hypertension patients whose last blood pressure was <140/90 mmHg
Percentage of diabetes patients with a documented comprehensive foot exam in last 12 months
Percentage of patients who have had a lipid panel performed in last 2 year
While medication adherence is tracked as feasible in this setting, more emphasis is put on a proactive approach of communicating with individuals about any side effects and counseling for adherence by the nurse and health promoter.
A weekly report is delivered to each clinic team listing patients overdue for their appointment enabling health promoters to contact patients for appropriate follow up. A monthly report provides quantities of each medication dispensed to patients over the course of the month; this is used to compare against the monthly inventory of medications to confirm that there is no diversion of medications and to help manage the medication supply. Problem solving and goal setting activities [16] are conducted with the multi-disciplinary DR team using the data to identify problems and set realistic goals in order to improve the quality of clinic processes and, in turn, patient outcomes.
2.7. Data Analysis.
Analysis of data for this report is accomplished in two ways. The first analytic approach involves the utilization of clinic data to produce quality improvement reports showing the proportions of patients achieving various National Quality Forum (NQF) [17] measures for diabetes and hypertension. These measures and analyses have been implemented for simplicity by the CCI program and for ease in comparison to outcomes in federally qualified health centers (FQHCs) for the underserved in the US. [18] The Uniform Data System (UDS) [18] measures used in FQHCs generally follow the NQF for measure definitions and these definitions are similar to CCI’s measure of HbA1C <9% (<75mmol/mol) and blood pressure of <140/90 mmHg as “in control” measures.
Recognizing some limitations of the quality improvement analyses in terms of adequately accounting for population turnover over years, the CCI program also examines upward or downward trends in blood pressure and metabolic indicators within patients in these measurements over time. When new patients are accrued, their health problems are often in poor control, which improves over time with treatment. They may later leave the CCI clinic when their results are more favorable, but the influx of new patients with poorer control dilutes these effects when looking at current population averages. Simple monthly averages of health statistics for the current population, therefore, may not accurately reflect the effects of treatment being given. Instead, we fit random-effects linear models to the data. In these models, HbA1c, BMI, systolic and diastolic blood pressure are the outcome variables. The main predictor variables specify the time under treatment (in years) for the patient, and these are interacted with indicators for the two clinics, allowing separate estimates of trends in each clinic, in addition to a random intercept at the patient level. The principal result in each model is the coefficient of the time under treatment which is interpreted as a rate of change in the outcome. For example, if the coefficient of time under treatment in the HbA1c model were −0.2, this would reflect an average decline of 0.2 percentage points HbA1c per year in treatment among the CCI patients. For analyses of blood pressure, because graphical exploration suggested that these data follow a biphasic pattern with a decrease during the first two years and a subsequent increase, a somewhat more complicated model that incorporates early and late time phases in a “hockey stick” model [19] was used.
After fitting this kind of model to each outcome, adjusted mean values of the outcome from times 0 through 6 years are calculated, along with standard errors, and graphed. Note that “adjusted” here means adjusted for changes in the composition of the patient population. These values represent the modeled projections of what the population mean value would have been had the entire population represented in the data been participating in care at every point in time. Accordingly, these values eliminate changes in observed values resulting from acquisition or attrition of patients.
The proportion of patients retained in care at least one year through six years after enrollment was calculated using the actuarial [20]method.
3. Results
3.1. Overview.
Results are organized by: 1) baseline characteristics of the patient population; 2) quality improvement measures over six years, and 3) analytic modeling of these clinical data to help eliminate potential biases in results due to fluctuations in the patient population over six years.
3.2. Baseline characteristics of the active patient population.
Table 1 presents the characteristics of patients at entry into the CCI program by clinic and total. The population at baseline entry into the CCI program included: 56% women; middle-aged (mean age 56.4 years); on average a BMI in the overweight range (27.4 kg/m2); with an average HbA1c of 8.8% for those with a diagnosis of diabetes. The most pronounced difference between the two clinic populations is in the HbA1c levels at baseline (9.3% vs 8.1%). The results for cholesterol and triglycerides should be viewed with caution as it is difficult for rural patients to arrive fasting when they have long distances to travel to the clinic. Average blood pressures were higher in Clinic B than Clinic A at baseline. We do not collect data on socio-economic status; these are rural, poor regions chosen specifically by the program to bring chronic disease resources to the underserved.
Table 1.
Baseline Characteristics by Clinic and Total
| Baseline Characteristics | Clinic A | Clinic B | Total |
|---|---|---|---|
| Sex N (%) | n=663 | n=528 | N=1191 |
| Female | 365 (55.0) | 298 (56.6) | 663 (55.7) |
| Male | 299 (45.0) | 229 (43.5) | 528 (44.3) |
| Education Level N (%) | n=625 | n=525 | N=1150 |
| No Formal Education | 115 (18.4) | 154 (29.3) | 269 (23.4) |
| Primary School | 427 (68.3) | 284 (54.1) | 711 (61.8) |
| Secondary School | 48 (7.7) | 61 (11.6) | 109 (9.5) |
| University | 35 (5.6) | 26 (5.0) | 61 (5.3) |
| Age (years) | n=660 | n=526 | N=1185 |
| Mean (SD) | 56.4 (12.4) | 56.4 (11.2) | 56.4 (11.9) |
| Body Mass Index (kg/m2) | n=609 | n=525 | N=1134 |
| Mean (SD) | 27.7 (5.2) | 26.9 (5.7) | 27.4 (5.4) |
| HbA1c (%) (diabetes dx only) | n=506 | n=312 | N=818 |
| Mean (SD) | 9.3 (2.5) | 8.1 (2.0) | 8.8 (2.4) |
| Systolic BP (mmHg) | n=663 | n=526 | N=1189 |
| Mean (SD) | 131.0 (24.1) | 134.7 (21.3) | 132.7 (23.0) |
| Diastolic BP (mmHg) | n=662 | n=526 | N=1188 |
| Mean (SD) | 80.2 (11.6) | 81.9 (12.0) | 80.9 (11.8) |
| Total Cholesterol * (mg/dL) | n=568 | n=476 | 1044 |
| Mean (SD) | 177.7 (49.5) | 189.6 (47.2) | 183.1 (48.8) |
| HDL Cholesterol * (mg/dL) | n=452 | n=440 | N=892 |
| Mean (SD) | 42.7 (13.9) | 42.6 (12.4) | 42.6 (13.2) |
| LDL Cholesterol * (mg/dL) | n=447 | n=429 | N=876 |
| Mean (SD) | 106.7 (39.1) | 111.5 (36.5) | 109.0 (37.9) |
| Triglycerides* (mg/dL) | n=554 | n=464 | 1018 |
| Mean (SD) | 174.2 (112.2) | 178.0 (117.2) | 176.0 (114.5) |
= Not reliably fasting laboratory test
3.3. Quality Measures for Processes of Care.
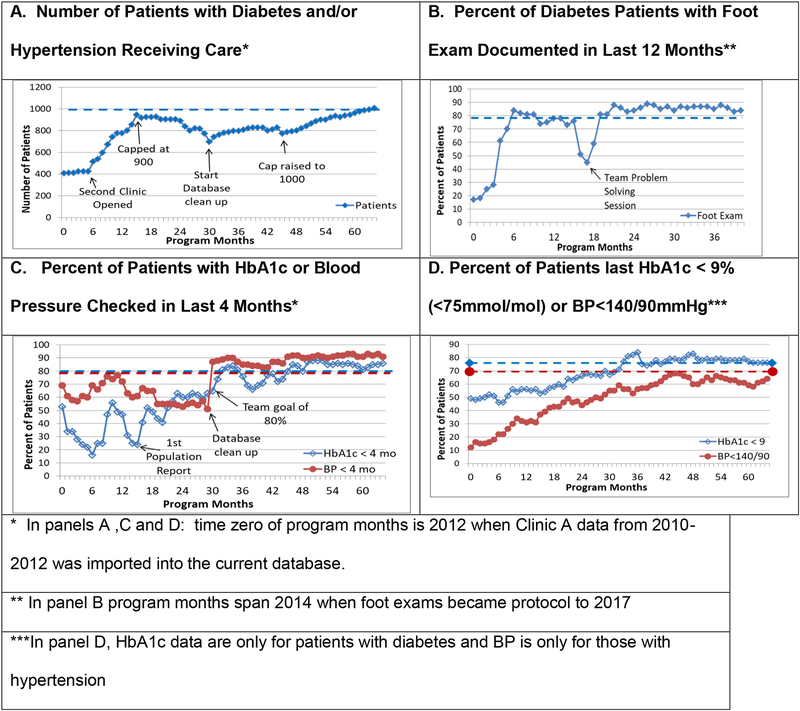
Figure 1 has four panels to show selected process and outcome measures for the diabetes and hypertension program. Panel A shows the growth in the population of patients; a downward fluctuation usually represents data clean-up efforts to identify and remove inactive patients. Clinic A accrued 400 patients between 2010 and 2012 (time zero for this Figure); Clinic B opened in mid-2012, and the combined total became over 900 in one year. An initiative to remove inactive patients from the database then resulted in opportunities to engage new eligible patients; because of expanded organizational capacity the patient population cap was raised to 1,000.
Figure 1.
Quality Improvement for Diabetes and Hypertension Metrics over Program Months Since Implementation.
Panel B portrays the proportion of patients with a comprehensive foot examination documented in the last 12 months. The protocol for foot exams was initiated in 2014; thus, just over three years of program data show the improvement in this quality measure, with a spike after team problem solving following an unexplained decline in documentation of foot exams.
Panel C shows the percent of diabetes patients with an HbA1c documented and hypertensive patients with a blood pressure documented in the last four months. Proportions of patients meeting the quality measures vacillates, but becomes more consistent and positive after a database cleanup and goal setting at each clinic.
Panel D shows the proportion of patients meeting the quality measure goals of an HbA1c <9% (<75 mmol/mol) for diabetes patients and a blood pressure <140/90 mmHg for patients with hypertension. The HbA1c goal was reached more readily and was sustained compared to the blood pressure quality measure goals for combined clinics.
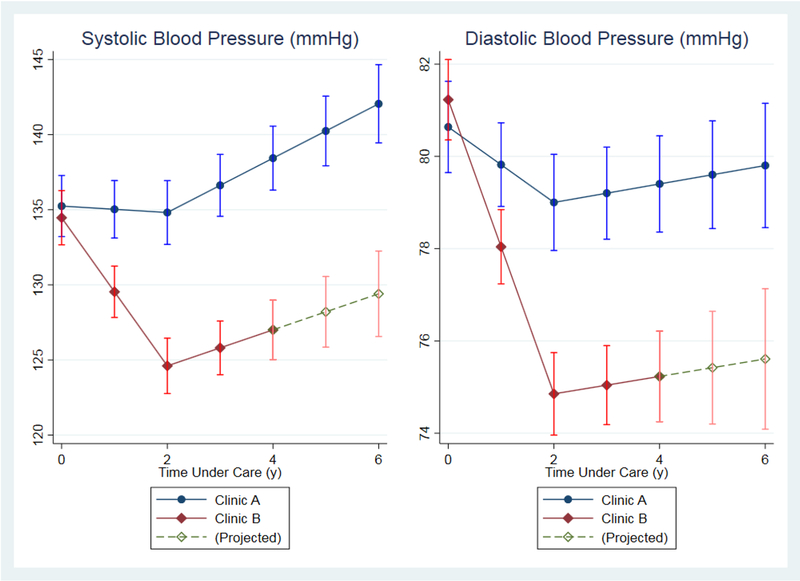
3.4. Modeled Trajectory of Systolic and Diastolic Blood Pressure.
The modeled blood pressure analyses for patients with a diagnosis of hypertension are presented in Figure 2. We exclude data from Clinic A prior to February 2012 due to the use of manual sphygmomanometers and a rounding of the result by staff when documenting it. Blood pressure among patients diagnosed with hypertension exhibits a biphasic response. During the first two years of treatment, decreases are seen, but thereafter it rises again. At Clinic A, the average decline in systolic BP during the first two years is 0.21 mmHg/year (95% CI 1.0 decline to 0.60 increase), and the subsequent increase is at a rate of 1.8 mmHg/year (95% CI 1.3 to 2.3). At Clinic B, the initial decline averages 4.9 mmHg/yr (95% CI 4.3 to 5.6), followed by an average increase of 1.2 mmHg/yr (95% CI 0.52 to 1.9). When the two clinics are combined, the decline for the first two years of treatment averages 3.5 mmHg/yr (95% CI 3.0 to 4.0), followed by an average increase of 1.7 mmHg/yr (95% CI 1.3 to 2.1).
Figure 2.
Modeled Trajectory of Systolic and Diastolic Blood Pressure by Clinic over Time Under Care
For diastolic BP, at Clinic A there is an initial decline of 0.82 mmHg/yr (95% CI 0.36 to 1.28) followed by a rise of 0.20 mmHg/yr (95% CI 0.10 decline to 0.50 increase). At Clinic B the initial decline averages 3.2 mmHg/yr (95% CI 2.8 to 3.5) and the subsequent increase averages 0.19 mmHg/yr (0.20 decline to 0.57 increase). Combining the two clinics, we see an average decrease of 2.4 mmHg/yr (95% CI 2.1 to 2.7) followed by an average increase of 0.27 mmHg/yr (95% CI 0.03 to 0.50).
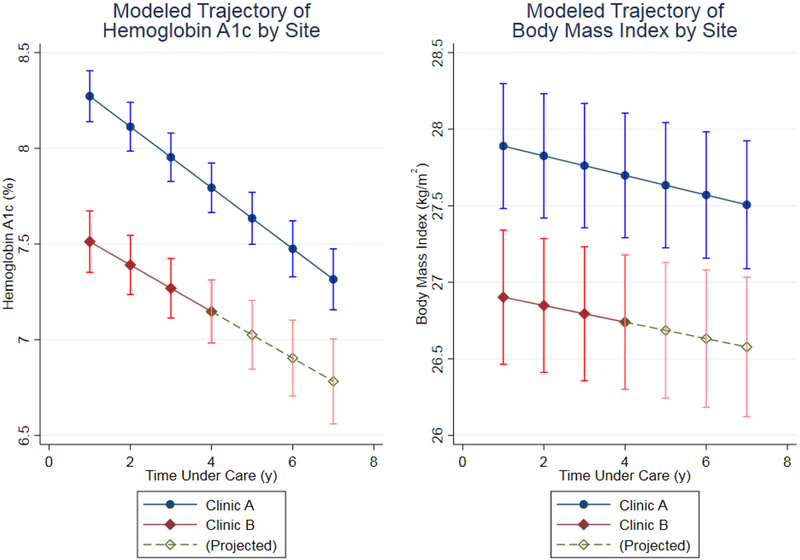
3.5. Modeled Trajectory of HbA1c Changes Over Time
At Clinic A, the average HbA1c declines by 0.16 percentage points per year (95% CI 0.14 to 0.19), and at Clinic B by 0.12 percentage points per year (95% CI 0.09 to 0.16). Combining the two sites, the average decline is 0.13 percentage points per year (95% CI 0.10 to 0.15). Trajectories of HbA1c are shown in Figure 3 left panel. Clinic A began the program with a higher average HbA1c than Clinic B, but each had declines over years in their trajectories.
Figure 3.
Modeled Trajectory of Hemoglobin A1c and Body Mass Index by Clinic over Time Under Care and Projected (for Clinic B)
3.6. Modeled Trajectories for Body Mass Index over Time
Body mass index decreased by 0.06 kg/m2 per year (95% CI 0.04 to 0.09) at Clinic A, and at Clinic B by 0.05 kg/m2 (0.03 to 0.08). For the combined sites, the average decline was .06 kg/m2, 95% CI (0.04 to 0.08). Trajectories for BMI are portrayed by Clinic in Figure 3 right panel.
3.7. Retention of Patients in the Program
Retention in the program was calculated using the actuarial method. At Clinic A, attrition of patients was 4% at one year, 12% at two years, 20% at three years, 25% at four years, 31% at five years and 35% at six years. In contrast, at Clinic B attrition was <1% at one year, 1.5% at two years, 4% at three years and 5% at four years; no additional patients left care after year four.
4. Discussion
4.1. Conclusions
This quality improvement program described here was a collaboration of Dominican and US medical teams supported by Chronic Care International. Notable baseline differences in patient populations (Table 1) included that Clinic A had on average higher BMI, higher HbA1c and lower systolic and diastolic BP’s compared to Clinic B, though each clinic served similar rural, poor communities. As CCI resources allowed, each clinic’s capacity expanded. The multi-disciplinary Dominican medical team at each clinic comprised a stable core of nurses and health promoters, although at clinic B several physicians transitioned over six years.
As viewed in Figure 1, team problem solving and goal setting sessions generally produced positive results in quality measures. These processes were led by the US team leader (HJD) during quarterly visits to CCI clinics and also by the designated Dominican medical director (e.g., JFG). Problem-solving sessions were guided by data reports and queries from the electronic record; without these pertinent data, the teams could not have appreciated fluctuations in care delivery and patient outcomes. Goals for assessing foot status, HbA1c and blood pressure were met or exceeded during the last three years reported (through May 2017). The quality measure for BP improved (Figure 1D) and after reaching an original goal of having 40% of patients under control, the quality goal was raised. Program changes continue to be made in order to reach new program goals.
Figure 2 shows that, when data are modeled analytically, diastolic BP has declined steeply at Clinic B. From a population perspective, a cumulative decline of nearly 9 mmHg over 6 years portends a potentially large impact on the incidence of complications. At Clinic A, the decrease has been slower, and cumulative progress over 6 years is accordingly less. It is worth noting that the average patient has so far spent 2.3 years under care in the CCI program so that on average, the cumulative reduction for the average patient is somewhere between the points marked at two and three years on the graphs.
Systolic BP has shown a steep initial decline over time at Clinic B. The cumulative effect on population incidence of complications is likely appreciable. By contrast, at Clinic A systolic BP decreased only modestly over time. After 2 years, however, blood pressure begins to rise again, more so at Clinic A. Combined with similar diastolic results, it seems fair to conclude that blood pressure management at Clinic A is less effective than at Clinic B. These differences between the clinics cannot be attributed to differences in patient populations and immigration or emigration effects, as these are adjusted for in the calculations. The initial blood pressure measurements were lower at Clinic A. Unmeasured variables such as specific dietary habits, exercise or medication adherence may also be at play.
The main interventions for BP control during the reporting period were the use of standardized algorithms for hypertension evaluation, medical management and self-management education. It was not until the end of the reporting period that CCI initiated other interventions designed to further improve blood pressure control, including: setting a new goal for BP control (e.g., 70% of hypertension patients to have a BP under 140/90mmHG); focused provider education on medication titration; and revisiting the self-management education most likely to impact blood pressure (e.g., sodium reduction, physical activity, dietary changes for weight loss). From the modeled trajectory, the trends in HbA1c are quite favorable at each clinic, with little difference in rates of progress between them. The baseline HbA1c levels were higher at Clinic A, and they decline slightly more readily than those at Clinic B; this phenomenon of more impressive declines in HbA1c with higher baseline values is often observed in population studies. [21] At Clinic B, the adjusted mean HbA1c after 4 years is below 7% (53 mmol/mol), a standard treatment goal.
We do not currently collect adequate data to report the proportion of individuals who have a prescription for insulin and who consistently obtain it outside of the CCI program. In the future, these data can assist CCI providers to understand insulin’s effect on metabolic control for this DR population, as well as reasons for declining to take insulin when prescribed.
The HbA1c results accord with the trends in BMI, which are also favorable though slow to decrease at both sites. Considering the difficulty patients and health care providers experience in weight loss interventions, these modest declines are very encouraging. While the CCI program includes some teaching modules on healthy eating and increasing physical activity, there is not currently a sustained, organized program for these lifestyle changes. The health promoters, however, voice enthusiasm and self-efficacy for implementing a lifestyle program for diabetes self-management [22] and diabetes prevention. [23] Access to lower carbohydrate healthier foods may be an issue for dietary problem solving in this poor rural area,[24] as it is in other low-resource countries; community gardens promoted by CCI show some promise.
The difference in retention of patients between clinics is likely multi-factorial; since Clinic A began two years before Clinic B opened, it had the benefit of learning from earlier protocols for activating patients. For example, enrolling a patient after one visit may have led to more attrition in Clinic A. Clinic B enrolled patients in the program after 3 visits. Furthermore, health promoters at Clinic B requested the program and were highly motivated. Clinic A was selected due to location and facility, but had less of a “buy in” initially. Patient retention deserves qualitative investigation to understand the dynamics at play at Clinic A.
4.2. Strengths and Limitations of the Program Results
Using the evidence-based Chronic Care Model as a heuristic for elements of the CCI program is a strength. The program has a multi-disciplinary and multi-layer approach to quality improvement for diabetes and hypertension management [10 25] and it is delivered by a Dominican-based health care team. Adoption of a disease registry shared between the DR and US teams is a strength for quality improvement. Our analyses have certain strengths: foremost is the combination of reporting quality improvement measures for comparison across many reported populations and also the use of a modeling technique which captures within-patient changes over time and adjusts for changes in patient population over time.
Limitations of this report include the program’s inability to compare outcome data and the costs of the program to public health results from other rural or urban communities in the DR, especially for the HbA1c measure for diabetes control as it is not performed in DR public The foremost limitation of the analyses is the use of a model which imposes a linear (or, in the clinics. case of blood pressure, piecewise linear) trend. Nevertheless, in-depth graphical exploration of these data (not shown here) suggest that these simple models are a reasonable representation of the actual time course of the data.
4.3. Future Directions
The CCI program plans to bolster the lifestyle diabetes prevention efforts and emotional support [26] in the clinic populations and in the surrounding rural communities; this will be implemented primarily through augmenting the role of health promoters through training and support [12]. Community engagement for program sustainability and transformation of the dietary and physical activity environment is also a goal; patient associations have now been organized at each clinic [27] They are working on community gardens, raising poultry, and other fund-raising efforts to sustain the program.
Sustainability [28] of this chronic disease management program has been an imperative since its inception; our goals include providing quality resources, training a Dominican healthcare workforce and engaging the community in health-related activities. Quality improvement is measured by our health outcomes. Finally, a long-term goal of collaboration with other DR organizations, e.g., The Dominican Ministry of Health, so that the CCI model reported here can be transferred, adapted and supported successfully for diverse settings. Adaptations may include remote interventions for training, supervision and data management to decrease the costs of the program to allow for greater sustainability.
4.4. Summary
This report describes a non-profit diabetes and hypertension chronic disease management program based on elements of the Chronic Care Model and implemented in rural communities in the Dominican Republic. Successes include clinical improvements in processes of care and in intermediate health outcomes for diabetes control, BMI, and selectively for blood pressure outcomes. Implementation includes multi-disciplinary health care teams providing care and community outreach in the DR, with support from the US team; scalability and sustainability of the program will be the central focus going forward.
Acknowledgments
Partial support for the CCI program is provided by grants from Chicago Cubs Charities and the Robert P. Heaney Family Foundation. Direct Relief, Inc., Abbott Laboratories, Siemens Inc., TEVA Pharamceuticals, and Creighton University Medical Center are acknowledged gratefully for supplies, equipment or medication donations. The Dominican Development Alliance branch of USAID partially supported early program development. We are grateful to the Joslin Diabetes Center, Boston, MA, USA for donating copies of their audio-novellas. We thank the Boards of Directors of CCI, ILAC and CESI, and individual donors supporting this work. Dr. Walker was partially supported by NIH grant P30 DK111022. We gratefully acknowledge the skillful dedication of our Dominican clinic teams and the kindness of patients who seek care at CCI clinics. Thanks to John M. Bertoni MD, PhD and Allison M. Lai, MPH for helpful comments on a manuscript draft.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest of Authors
No author reports conflicts of interest pertaining to this report.
Contributor Information
Henry J. Dethlefs, One World Community Health Centers, Inc, 4920 S 30th St. Suite 103, Omaha, NE 68107 USA.
Elizabeth A. Walker, Albert Einstein College of Medicine, 1300 Morris Park Avenue, Bronx, New York 10461, USA.
Clyde B. Schechter, Albert Einstein College of Medicine, 1300 Morris Park Avenue, Bronx, New York 10461, USA.
Rachel Dowd, CHI Creighton University Medical Center, 7500 Mercy Rd. Omaha, NE 68124 USA.
Linda Filipi, Chronic Care International, 12370 Rose Lane, Omaha, NE 68154 USA.
Juan Francisco Garcia, Chronic Care International, Centro de ILAC, Licey, Dominican Republic.
Charles Filipi, Creighton University School of Medicine, Education Building, Suite 105, 7710 Mercy Road, Omaha, NE 68124 USA.
References
- 1.Caban-Martinez AJ, Halder GE, Tellechea L, et al. Health status and behaviors among adults residing in rural Dominican Republic. Rural Remote Health 2012;12:1956. [PubMed] [Google Scholar]
- 2.International Diabetes Foundation. IDF Diabetes Atlas - 8th Edition, 2017. [Google Scholar]
- 3.World Health Organization. Global Report on Diabetes, 2016.
- 4.Mills KT, Bundy JD, Kelly TN, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 2016;134(6):441–50 doi: 10.1161/CIRCULATIONAHA.115.018912[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Bank. Dominican Republic. Secondary Dominican Republic. https://data.worldbank.org/country/dominican-republic.
- 6.International Diabetes Foundation. IDF SACA Region. Secondary IDF SACA Region 2018. https://www.idf.org/our-network/regions-members/south-and-central-america/members/82-dominican-republic.html.
- 7.World Health Organization. Country Profiles: Dominican Republic. Secondary Country Profiles: Dominican Republic 2016. http://www.who.int/diabetes/country-profiles/dom_en.pdf?ua=1.
- 8.Institute for Health Metrics and Evaluation. Health Data: Dominican Republic. Secondary Health Data: Dominican Republic 2016. http://www.healthdata.org/dominican-republic.
- 9.Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Preventing chronic disease 2013;10:E26 doi: 10.5888/pcd10.120180[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA 2002;288(15):1909–14 [DOI] [PubMed] [Google Scholar]
- 11.Cruz M, Filipi L, Estevez J, et al. Diabetes hypertension treatment program for underserved in rural Dominican Republic. Open J Int Med 2012;2:72–79 [Google Scholar]
- 12.Joslin’s Latino Diabetes Initiative. Rosa’s Story. Joslin Diabetes Center; Boston, MA, 2013. [Google Scholar]
- 13.Fisher EB, Ballesteros J, Bhushan N, et al. Key Features Of Peer Support In Chronic Disease Prevention And Management. Health Aff (Millwood) 2015;34(9):1523–30 doi: 10.1377/hlthaff.2015.0365[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 14.Whelton PK, Carey RM, Aronow WS, et al. 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71(6):e13–e115 doi: 10.1161/HYP.0000000000000065[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association. Standards of Medical Care in Diabetes-2018. Diabetes Care 2018;41(Suppl 1):S152–S53 doi: 10.2337/dc18-S015[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 16.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Annals of Behavioral Medicine 2002;24(2):80–87 [DOI] [PubMed] [Google Scholar]
- 17.National Quality Forum. National Quality Forum Measures, Reports, and Tools. Secondary National Quality Forum Measures, Reports, and Tools 2018. http://www.qualityforum.org/measures_reports_tools.aspx.
- 18.Uniform Data System (UDS). Secondary Uniform Data System (UDS) 2018. http://www.bphc.hrsa.gov/datareporting/reporting/index.html.
- 19.Bacon D, Watts D. Estimating the transition between two intersecting straight lines. Biometrika 1971;58(3):525–34 [Google Scholar]
- 20.Krakauer H, Stewart J. Actuarial or life-table analysis of time-to-event data. College Station, TX: Stata Press, 1991. [Google Scholar]
- 21.Chamany S, Walker EA, Schechter CB, et al. Telephone Intervention to Improve Diabetes Control: A Randomized Trial in the New York City A1c Registry. Am J Prev Med 2015. doi: 10.1016/j.amepre.2015.04.016[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West-Pollak A, Then EP, Podesta C, et al. Impact of a novel community-based lifestyle intervention program on type 2 diabetes and cardiovascular risk in a resource-poor setting in the Dominican Republic. Int Health 2014;6(2):118–24 doi: 10.1093/inthealth/iht039[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 23.Goldman ML, Ghorob A, Hessler D, Yamamoto R, Thom DH, Bodenheimer T. Are Low-Income Peer Health Coaches Able to Master and Utilize Evidence-Based Health Coaching? Ann Fam Med 2015;13 Suppl 1:S36–41 doi: 10.1370/afm.1756[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perez-Escamilla R, Villalpando S, Shamah-Levy T, Mendez-Gomez Humaran I. Household food insecurity, diabetes and hypertension among Mexican adults: results from Ensanut 2012. Salud Publica Mex 2014;56 Suppl 1:s62–70 [DOI] [PubMed] [Google Scholar]
- 25.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet 2012;379(9833):2252–61 doi: 10.1016/S0140-6736(12)60480-2[published Online First: Epub Date]|. [DOI] [PubMed] [Google Scholar]
- 26.Wallace DD, Gonzalez Rodriguez H, Walker EA, et al. Types and sources of social support among adults living with type 2 diabetes in rural communities in the Dominican Republic. Glob Public Health 2018:1–12 doi: 10.1080/17441692.2018.1444782[published Online First: Epub Date]|. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Restakis J Harmonizing the Economy: Co-opertives in the Age of Capital. British Columbia, Canada: New Society Publishers, 2010. [Google Scholar]
- 28.Yang A, Farmer PE, McGahan AM. “Sustainability in Global Health. Global Public Health 2010;5(2):129–35. [DOI] [PubMed] [Google Scholar]