Abstract
Background
People with chronic venous insufficiency who develop leg ulcers face a difficult condition to treat. Venous leg ulcers may persist for long periods of time and have a negative impact on quality of life. Treatment requires frequent health care provider visits, creating a substantial burden across health care settings.
The objective of this health technology assessment was to evaluate the effectiveness, safety, cost-effectiveness, budget impact, and patient experiences of compression stockings for prevention of venous leg ulcer recurrence.
Methods
We conducted a systematic review of the literature to identify randomized trials and observational studies examining the effectiveness of compression stockings in reducing the risk of recurrence of venous leg ulcers after healing and/or reported on the quality of life for patients and any adverse events from the wearing of compression stockings. We performed a literature search to identify studies and evaluated the quality of the evidence using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach.
We conducted a cost–utility analysis with a 5-year time horizon from the perspective of the Ontario Ministry of Health and Long-Term Care. We compared compression stockings to usual care (no compression stockings) and simulated a hypothetical cohort of 65-year-old patients with healed venous ulcers, using a Markov model. Model input parameters were obtained primarily from the published literature. In addition, we used Ontario costing sources and consultation with clinical experts. We estimated quality-adjusted life years gained and direct medical costs. We conducted sensitivity analyses and a budget impact analysis to estimate the additional costs required to publicly fund compression stockings in Ontario. All costs are presented in 2018 Canadian dollars.
We spoke to people who recently began using compression stockings and those who have used them for many years to gain an understanding of their day-to-day experience with the management of chronic venous insufficiency and compression stockings.
Results
One randomized controlled trial reported that the recurrence rate was significantly lower at 12 months in people who were assigned to the compression stocking group compared with people assigned to the control group (risk ratio 0.43, 95% CI, 0.27–0.69; P = .001) (GRADE: Moderate). Three randomized controlled trials reported no significant difference in recurrence rates between the levels of pressure. One randomized controlled trial also reported that the risk of recurrence was six times higher in those who did not adhere to compression stockings than in those who did adhere. One single-arm cohort study showed that the recurrence rate was considerably higher in people who did not adhere or had poor adherence (79%) compared with those who adhered to compression stockings (4%).
Compared with usual care, compression stockings were associated with higher costs and with increased quality-adjusted life years. We estimated that, on average, the incremental cost-effectiveness ratio of compression stockings was $27,300 per quality-adjusted life year gained compared to no compression stockings. There was some uncertainty in our results, but most simulations (> 70%) showed that the incremental cost-effectiveness ratio remained below $50,000 per quality-adjusted life-year. We estimated that the annual budget impact of funding compression stockings would range between $0.95 million and $3.19 million per year over the next five years.
People interviewed commonly reported that chronic venous insufficiency had a substantial impact on their day-to-day lives. There were social impacts from the difficulty or inability to walk and emotional impacts from the loss of independence and fear of ulcer recurrence. There were barriers to the wearing of compression stockings, including replacement cost and the difficulty of putting them on; however, most people interviewed reported that using compression stockings improved their condition and their quality of life.
Conclusions
The available evidence shows that, compared with usual care, compression stockings are effective in preventing venous leg ulcer recurrence and likely to be cost-effective. In people with a healed venous leg ulcer, wearing compression stockings helps to reduce the risk of recurrence by about half. Publicly funding compression stockings for people with venous leg ulcers would result in additional costs to the Ontario health care system over the next 5 years. Despite concerns about cost and the daily chore of wearing compression stockings, most people interviewed felt that compression stockings provided important benefits through reduction of swelling and prevention of recurrence.
OBJECTIVE
This health technology assessment looks at the effectiveness, safety, cost-effectiveness, budget impact, and patient experiences of compression stockings for prevention of venous leg ulcer recurrence.
BACKGROUND
Health Condition
Venous leg ulcers are open wounds in the skin of the lower leg due to high pressure of the blood in the leg veins. Venous leg ulcers commonly result from a cycle of events in the leg's venous system. When functioning normally, valves in the deep and superficial veins of the leg prevent backflow of the blood. But if a person has chronic venous insufficiency, the blood can pool and the venous pressure increase. The higher pressure stretches and damages the one-way valves inside the veins, affecting functioning. In a feedback effect, this compromised functioning further increases pressure in the venous system, affecting the surrounding tissues. The sustained high pressure leads to a backflow of the blood into the thin wall of the superficial veins, forcing them to stretch and dilate. These changes lead to capillary distension, which in turn allows plasma to leak into the skin tissue, causing inflammation, edema, eczema, lipodermatosclerosis, and skin damage. Finally, an ulcer develops around the damaged skin.
Venous leg ulcers often develop in the legs of older adults with venous leg insufficiency and can lead to pain, loss of function, and distress. The ulcers may become chronic and persist for long periods of time, affecting quality of life. Recurrence of the healed venous leg ulcer is a challenging issue for health care providers and particularly for community nursing providers who are involved in the care of people with venous leg ulcers.
Some people might be candidates for surgical correction of the underlying pathology. Surgical methods, as well as a variety of minimally invasive methods that correct the underlying cause can lead to marked improvement in the condition.
Venous leg ulcers have been shown to heal faster when care is delivered by a team of specially trained professionals following an evidence-informed protocol. The majority of venous leg ulcers heal if proper compression is applied. The Canadian Bandaging Trial,1 which compared two types of compression bandages, reported a 12-month healing rate of 92% with short stretch bandages and 83% with four-layer bandages.
Classification of Venous Leg Disorders
Accurate classification of venous leg disorders is critically important for standardization of venous disease severity and appropriate treatment.2 The Clinical, Etiology, Anatomy, and Pathophysiology (CEAP) classification system, introduced in 1994 and revised in 2004, forms the basis for chronic venous disease documentation.2 The CEAP classification is as follows:
| CO | No visible or palpable signs of venous disease |
| C1 | Telangiectasies or reticular veins |
| C2 | Varicose veins |
| C3 | Edema |
| C4a | Pigmentation or eczema |
| C4b | Lipodermatosclerosis or atrophy blanche |
| C5 | Healed venous ulcers |
| C6 | Active venous ulcers |
Clinical Need and Target Population
Venous leg ulcers may cause social, personal, financial, and psychological burdens on patients and are a significant burden on the health care system. People with leg ulcers commonly report pain, itching, and sleep disturbance.3,4 The majority of people with venous leg ulcers are of advanced age, have a higher body mass index,5 and suffer from other health problems and/or impaired mobility that could affect their overall well-being as well as the healing process.6 The high recurrence rate of venous leg ulcers creates a clinical challenge, adding to the burden on clinicians and on the health care system.
Incidence and Prevalence of Venous Leg Ulcers
Prevalence studies undertaken nationally and internationally have produced estimates that between 1.5 and 3.0 per 1,000 people have active leg ulcers.7,8 In Ontario, the prevalence of active lower limb ulcers in people over the age of 25 years was estimated to be 1.8 per 1,000 people,9 with about three quarters over the age of 65. Harrison et al1 found that in Ontario, 50% of people with lower limb ulcers had leg ulcers, 35% had foot ulcers, and 15% had leg and foot ulcers.9 A large Swedish population-based study showed that 36% of all leg ulcers are caused by abnormalities in the venous system.10 Based on these findings, we estimate that 0.65 per 1,000 people in Ontario over the age of 25 years have active venous leg ulcers.
International studies that provide estimates for either leg ulcers or venous leg ulcers are comparable with the Ontario study.9 A large study from the United Kingdom11 that examined a database of about 13.5 million people reported prevalence rates of active venous leg ulcers at 0.8 to 1.2 per 1,000 for women and 0.5 to 0.8 per 1,000 for men. In a population-based study from Australia12 that included 238,000 people, the prevalence of active venous leg ulcers was 0.62 per 1,000 people, and 3.3 per 1,000 for people over the age of 60.
Epidemiological studies by Nelzen et al8 in Skarborg County, Sweden (population 270,800), show that introducing a new strategy consisting of multidisciplinary cooperation and team work, and that also includes compression stockings after healing, can decrease the prevalence of leg ulcers. Over a 14-year period after introduction of the program, the prevalence of venous leg ulcers reduced from 1.6 per 1,000 to 0.9 per 1,000, a reduction of 46%.
Venous ulcer prevalence and incidence are greater in the long-term care population than in the community at large.13 In a study of long-term care homes in Missouri,13 the prevalence of venous leg ulcer on admission was 2.5%. The incidence of venous leg ulcer for those admitted without an ulcer was 1.0%, 1.3%, 1.8%, and 2.2% at 90, 180, 270, and 365 days after admission, respectively.
The incidence of venous leg ulcer was reported by a large study from the United Kingdom11 that used The Health Improvement Network (THIN) database, which contains data prospectively collected from general practice between 2001 and 2006 for adult patients. The incidence of venous leg ulcer was 1.0 per 1,000 people.
Current Treatment Options
Compression therapy is an important component of venous leg ulcer treatment and prevention of recurrence.2,14 It helps lower venous hypertension, decrease venous stasis and inflammation, and enhance tissue vascularization. After healing, preventive measures need to be followed to prevent ulcers from recurring. Patient education along with well-fitting compression stockings and regular checkups are the standard preventive measures to minimize the risk of recurrence. Strategies to help clinicians effectively manage patients with venous leg ulcers should be considered a priority for the health system.
Recurrence is a major concern in people who have been successfully treated for venous leg ulcers owing to the underlying chronic venous insufficiency. A variety of surgical methods are used in clinical practice to correct the underlying cause of reflux and increased pressure in the veins. These surgical methods treat incompetent superficial, deep, and perforating veins of the leg. The most intractable ulcers occur when the valves of the deep veins are incompetent.15 A combination of surgical correction of the underlying cause and continued application of compression has been shown to significantly reduce recurrence of venous leg ulcers, compared with compression alone.16,17 Clinicians use a variety of minimally invasive techniques, including endovenous laser ablation, endovenous radiofrequency ablation, and sclerotherapy, to correct the underlying cause of venous hypertension.18
Health Technology Under Review
Medical-grade graduated compression stockings apply higher pressure to the ankle region, gradually decreasing the pressure in higher areas of the leg. Recent studies have also examined the potential benefits of progressive compression, where the pressure increases in the higher areas of the leg.19 Compression therapy is an essential concept in the treatment of venous and lymphatic insufficiency.15 The most commonly used compression therapy systems for venous leg ulcers are compression bandages that can provide sustained compression and aid ulcer healing. Other forms of compression therapy for venous leg ulcers include boots and intermittent pneumatic devices. Once a venous leg ulcer is healed, compression stockings are used to reduce edema and ulcer recurrence.
There is no worldwide standard to grade the level of compression pressure. Medical-grade compression stockings are categorized by the manufacturers according to the pressure they are supposed to apply to the leg; however, the described pressure may not accurately reflect the actual level of compression because there are other factors that can influence the pressure actually applied. For example, the elasticity of the stocking can break down with use. The technique used to put on and remove the stocking, as well as patient characteristics such as the shape and circumference of the leg, can also affect the level of compression achieved.14
In Ontario, class I stockings (defined as < 20 mm Hg) that provide lower pressure are available without a prescription. These are used mainly by people who stand on their feet for long periods of time or who sit in confined spaces, such as on an airplane. Medical-grade stockings offering higher pressure are dispensed by a prescription that indicates the recommended pressure. To ensure proper compression, stockings need to be replaced at regular intervals (usually every 4 months).
Before starting compression therapy, the clinician should ensure that there is adequate arterial supply to the foot. The arterial perfusion pressure is determined by the arterial brachial pressure index (ABPI). Some guidelines recommend an ABPI of 0.8 or higher for compression therapy.14 Other guidelines recommended the threshold of 0.9.2 Limb ischemia and pulmonary edema are contraindications for compression therapy.20
Regulatory Information
In Canada, compression stockings are considered Class 1 devices and they do not require a medical device licence (Personal communication, Health Canada Medical Devices Bureau).
Ontario Context
Compression stockings are not routinely publicly funded in Ontario for recurrence of venous leg ulcers. They are publicly funded in part through the provincial assistive devices program (ADP) for people with lymphedema. Funding requires diagnosis by an approved prescriber, authorization by an approved authorizer, and provision by an approved vendor. Many insurance companies provide coverage through employee benefit plans.
CLINICAL EVIDENCE
Research Questions
In people with healed venous leg ulcers:
Is there any difference in the frequency of venous leg ulcer recurrence in people who wear compression stockings compared with those who do not?
What level of compression is most effective in preventing recurrence of the healed venous leg ulcer?
What length of compression stocking is most effective in preventing recurrence of the healed venous leg ulcer?
What is the adherence rate with compression stockings at different compression levels?
What is the effect of a compression stocking on the quality of life of the person wearing it?
What are the adverse effects of compression stockings when used after venous leg ulcer healing?
Methods
We developed the research questions in consultation with patients, health care providers, clinical experts, and other health system stakeholders.
Clinical Literature Search
We performed a literature search on November 21, 2017, to retrieve studies published from inception to the search date. We used the Ovid interface in the following databases: MEDLINE, Embase, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, CRD Health Technology Assessment, and National Health Service Economic Evaluation Database (NHS EED). We used the EBSCOhost interface to search the Cumulative Index to Nursing & Allied Health Literature (CINAHL).
Medical librarians developed the search strategy using controlled vocabulary (i.e., Medical Subject Headings) and relevant keywords. The final search strategy was peer reviewed using the PRESS Checklist.21 We created database auto-alerts in MEDLINE, Embase, and CINAHL and monitored them for the duration of the assessment period.
We performed targeted grey literature searching of health technology assessment agency sites and clinical trial registries. See Appendix 1 for literature search strategies, including all search terms.
Literature Screening
Two review authors conducted the initial screening of the titles and abstracts using DistillerSR management software (Evidence Partners, Ottawa, ON) and then obtained the full text of studies that appeared eligible for the review according to the inclusion criteria. Discrepancies between the reviewers were resolved by discussion and consensus. The reviewers then examined the full text articles and selected studies that were eligible for inclusion. They also examined reference lists of the included studies for any additional relevant studies not identified through the search.
Inclusion Criteria
English-language full-text publications
Studies published from inception to November 21, 2017
Randomized controlled trials (RCTs) and prospective cohort studies that compared the recurrence rate in people with a healed venous leg ulcer with and without the use of compression stockings
RCTs that compared results of different compression levels in people with a healed venous leg ulcer
RCTs that compared results of different lengths of stockings (e.g., below vs. above knee/thigh length) in people with a healed venous leg ulcer
Studies that examined the effect of compression stockings on the quality of life of people with a healed venous leg ulcer
Studies that examined the adverse effects or mortality caused by compression stockings in people with a healed venous leg ulcer
Exclusion Criteria
Studies on compression bandages and devices such as boots and pneumatic devices
Studies in which the origin of the ulcer was not venous
Studies that compared different brands of stockings or compared compression stockings with other compression methods
Editorials, case reports, or commentaries
Outcomes of Interest
Primary Outcome
Recurrence of the healed venous leg ulcer or the occurrence of a new venous leg ulcer on either leg
Secondary Outcomes
Time to recurrence of the healed venous leg ulcer
Time to occurrence of a new venous leg ulcer
Adherence rate
Quality of life
Adverse effects of compression stockings
Mortality
Out of Scope
There are minimally invasive and other surgical methods to correct the underlying pathology that causes venous leg ulcer recurrence, but they are out of scope for this review.
Data Extraction
We extracted relevant data on study and patient characteristics, outcomes, and risk-of-bias items using a data form to collect information about the following:
Source (citation information)
Methods (study design, study place, follow-up, participant characteristics, and randomized groups)
Outcomes (recurrence rate, time to recurrence, adherence to compression stockings, number of participants for each outcome, number of participants missing for each outcome, and time points at which the outcomes were assessed)
Items for risk of bias for RCTs (method of sequence generation, method of allocation concealment, blinding of participants and personnel, incomplete outcome data, and selective reporting of outcomes)
Items for risk of bias for cohort studies
Statistical Analysis
We used STATA 11 (StataCorp LLC, College Station, Texas) to perform a meta-analysis on the reported recurrence rates and produced a forest plot. We used the risk ratio and its 95% confidence interval as the summary statistic to display the difference between groups. We used a random effects model to pool the data and the chi-square test to determine statistical heterogeneity among the studies.
Critical Appraisal of Evidence
For randomized controlled trials, we assessed risk of bias using the Cochrane risk of bias tool.22 For observational cohort studies, we used Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I).23 We evaluated the quality of the body of evidence for each outcome according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Handbook.24 The body of evidence was assessed based on the following considerations: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The quality score reflects our assessment of the reliability of the evidence presented.
Expert Consultation
We solicited expert feedback from a variety of organizations involved in the management of ulcers in Ontario. We consulted dermatologists, nurses specialized in wound care, and chiropodists who routinely visit patients with venous leg ulcers. The role of the expert advisors was to provide feedback on our questions, to provide advice on the appropriate use of the technology, and to review the clinical review plan and the health technology assessment report.
Results
Literature Search
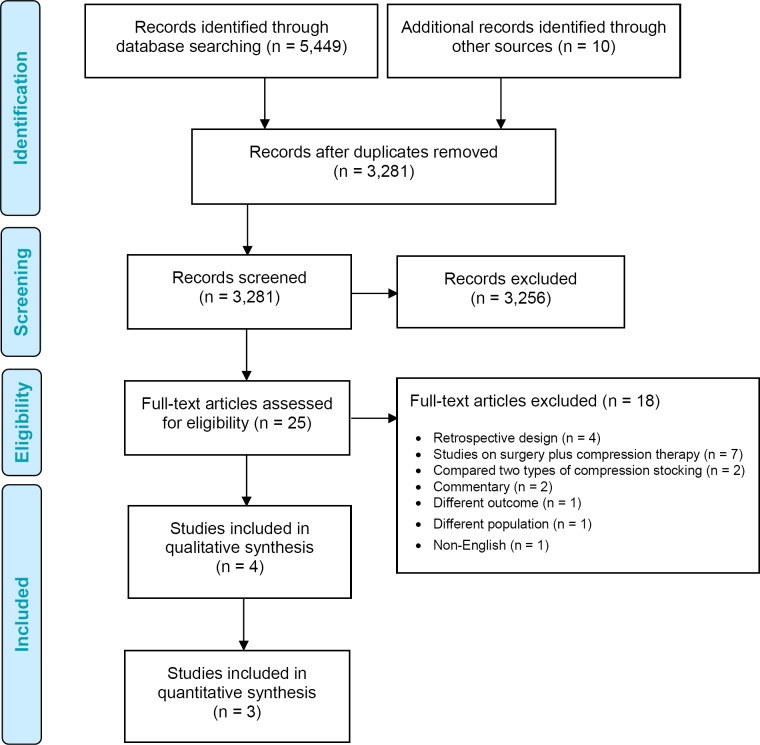
The literature search yielded 3,281 citations published from inception to November 21, 2017, after removing duplicates. Seven studies (four randomized control trials25–28 and three prospective cohort studies29–31) met the inclusion criteria.
Figure 1 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
Figure 1: PRISMA Flow Diagram—Clinical Search Strategy.
Source: Adapted from Moher et al.32
Study and Patient Characteristics
Four RCTs25–28 and three single-arm observational cohort studies29–31 met our inclusion criteria. One RCT compared compression with no compression and three RCTs compared two levels of compression pressure. Two observational cohort studies compared the recurrence rate of those who adhered to stockings with the recurrence rate of those who did not, or with people who dropped out. One prospective observational study reported on patients' quality of life.
We did not find any study reporting on mortality resulting from the wearing of compression stockings. Also, we did not find any study that compared compression stockings of different lengths.
Tables 1 and 2 show study design, patient characteristics, adherence rate, and recurrence rate for RCTs and observational studies.
Table 1:
Study, Patient, and Intervention Characteristics: Randomized Controlled Trials on Compression Stockings
| Author, Year | Country | Study Objective | Randomized Groupsa | Stocking Type | Patients Na | Female/Male N | Mean Age Years (SD)a | Outcome Measured |
|---|---|---|---|---|---|---|---|---|
| Kapp et al, 201326 | Australia | To compare the effect of moderate pressure with high pressure on recurrence of VLU and patient adherence | 23–32 mm Hg vs. 34–46 mm Hg |
Venosan 5000 range, Salzmann, MEDICO, St Gallen, Switzerland Below knee length Participants were provided with two stockings for wear on the study leg only |
93 Moderate: 49 High: 44 |
68/25 | 23–32 mm Hg: 79.04 (10.40) 34–46 mm Hg: 78.27 (10.56) |
Recurrence rate Time to recurrence Adherence rate Adverse effects |
| Clarke-Moloney et al, 201425 | Ireland | To compare the effect of two European classes of MCS on recurrence of VLU and patient adherence | 18–21 mm Hg vs. 23–32 mm Hg |
Mediven elegance (closed toe) or Mediven plus (open toe) | 100 18–21 mm Hg: 50 23–32 mm Hg: 50 |
NA | 18–21 mm Hg: 69.7 23–32 mm Hg: 68.9 |
Recurrence rate Adherence rate |
| Nelson et al, 200627 | United Kingdom | To compare the effect of two European classes of MCS on recurrence of VLU and patient adherence | 18–24 mm Hg vs. 25–35 mm Hg |
Jobst or Medi Knee or thigh length |
300 18–24 mm Hg: 151 25–35 mm Hg: 149 |
18–24 mm Hg: 92/59 25–35 mm Hg: 83/66 |
18–24 mm Hg: 65.1 (12.9) 25–35 mm Hg: 63.6 (11.4) |
Recurrence rate Time to recurrence Adherence rate |
| Vandongen & Stacey, 200028 | Australia | To compare the effect of MCS with no MCS on reducing the area of lipodermatosclerosis and recurrence of VLU | MCS with pressure of 35–45 mm Hg vs. no MCS | Venosan 2003 Below knee length |
153 MCS: 72 No MCS: 81 |
NA | 67 (range, 37–85) | Recurrence rate Adherence rate |
Abbreviations: MCS, medical compression stocking; NA, not available; SD, standard deviation; VLU, venous leg ulcer.
mm Hg stocking pressure.
Table 2:
Study, Patient, and Intervention Characteristics: Single Arm Prospective Trials on Compression Stockings
| Author, Year | Country | Study Objective | Subgroup Analysis | Stocking Type | Patients N | Female/Male n | Mean Age, Years |
|---|---|---|---|---|---|---|---|
| Samson & Showalter, 199631 | USA | To evaluate MCS for treatment of VLU and prevention of recurrence | Adherence vs. nonadherence | UlcerCare System (Jobst) | 53 | 28/25 | 71 (range, 45–94) |
| Dinn & Henry, 199229 | Ireland | To determine whether use of MCS can reduce the risk of VLU recurrence | Adherents vs. dropped out | Scholl Soft Grip elastic stockings | 126 (VLUs were healed by sclerotherapy) | 91/35 | 59.5 (range 26–80) |
| Reich-Schupke et al 200930 | Germany | To assess whether there are differences in the treatment behaviour and the quality of life of patients experiencing compression therapy | NA | NA | 110 | 72/38 | 66.2 (SD, 13.57) |
Abbreviations: MCS, medical compression stocking; NA, not applicable; SD, standard deviation; VLU, venous leg ulcer.
Recurrence Rate
Recurrence rates reported by the four RCTs are shown in Table 3. Vandongen and Stacey28 randomized participants into compression stocking and no compression stocking groups. Compression stockings reduced the risk of recurrence by half after 12 months (24% vs. 54% in the compression stocking vs. no compression stocking groups, respectively; risk ratio 0.43, 95% CI, 0.27–0.69; P = .001). The primary outcome of this study was an assessment of the effectiveness of compression stockings in reducing the area of lipodermatosclerosis (considered a precursor of venous leg ulcers) in participants with healed venous ulcers. Participants were given two pairs of stockings with pressure of 35–45 mm Hg every 6 months and were instructed to wear each pair on alternate days. Participants who did not adhere to the instructions were withdrawn from the study. In the stocking group, there were 12 stocking-related withdrawals at 6 months and 16 at 12 months. In the no-stocking group, three participants withdrew so that they could wear stockings. Other causes of withdrawal after 12 months in the no-stocking group were personal/medical (n = 7), death (n = 3), lost to follow-up (n = 3).
Table 3:
Recurrence Rates in Randomized Controlled Trials
| Author, Year | Recurrence Rate | P |
|---|---|---|
| Kapp et al, 201326 |
6 months leg locationa 23–32 mm Hg: 7/49 (14.3%) 34–46 mm Hg: 6/44 (13.6%) |
1.00 |
|
6 months study ulcera 23–32 mm Hg: 7/49 (14.3%) 34–46 mm Hg: 4/44 (9.1%) |
.65 | |
| Clarke-Moloney et al, 201425 |
12 months 18–21 mm Hg: 10/50 (20%) 23–32 mm Hg: 6/50 (12%) |
.29 |
| For those adhered to MCS: 9/85 (10.6%) 18–21 mm Hg: 6/43 (14%) 23–32 mm Hg: 3/45 (7%) |
.31 | |
| For those not adhered to MCS: 7/11 (63.6%) Risk ratio: 6.2 (95% CI, 2.9–13.5; P < .001) |
||
| Nelson et al, 200627 |
5 years 18–24 mm Hg: 59/151 (39%) 25–35 mm Hg: 48/149 (32%) |
.13 |
| Vandongen & Stacey, 200028 |
6 months MCS: 15/72 (21%) No MCS: 37/81 (46%) 12 months MCS: 17/72 (24%) No MCS: 44/81 (54%) Median percentage change in lipodermatosclerosis area in participants who did not develop ulcers 12 months (n = 46) MCS: −33.1 (95% CI, −61.9–15.07) No MCS: +11.9 (95% CI, −24.6–122.2) |
.04 |
Abbreviation: MCS, medical compression stocking.
Study ulcers develop in the same anatomical location as the previous ulcer. Leg location ulcers develop in a different anatomical location as the previous ulcer.
Vandongen and Stacey28 found that in participants whose ulcer did not recur, the area of lipodermatosclerosis was significantly reduced after 6 and 12 months in the stockings group, while it increased in the control group. The median percentage change in the area of lipodermatosclerosis at 6 months was −22% in the stocking group and +7.8% in the no-stocking group (indicating an increase in the area). At the 12-month follow-up, the change in the area was −33.1 (95% CI, −61.9–15.07) for the stocking group, and +11.9 (95% CI, −24.6–122.2) for the no-stocking group (P = .04). The initial area of lipodermatosclerosis was significantly larger in participants whose ulcer recurred within 2 years of entering the study compared with those whose ulcer did not recur (median area of 293.4 cm2 vs. 49.5 cm2, respectively).
The two observational studies included in this review were single arm cohort studies, but they provided indirect comparison of compression use and also provided data on longer term follow-up.29,31 Although the findings from these studies are based on their subgroup analysis, they may provide support for the findings of the RCT.28 Samson and Showalter31 included only people with documented deep venous insufficiency whose ulcer had healed. This observational study evaluated a new type of compression stocking that consisted of a liner that provided mild pressure and an outer layer with zipper to provide 40 mm Hg pressure. They found the risk of recurrence at follow-up (mean of 28 months) was 20 times higher in participants who had poor or no adherence to the compression stockings than in those who had good adherence (RR 18.4, 95% CI 2.68–126.16, P < .001).
The other observational study, by Dinn and Henry,29 had a 5-year follow-up that compared the recurrence rate between those who adhered to stockings and those who dropped out of the study. The rationale for this comparison was that it would be unrealistic to request people in a varicose vain clinic to not wear compression stockings. In this study, a high degree of adherence was obtained by exact fitting of the stockings and regular review by the same clinician. At the end of the 5 years, 21 participants had dropped out. Of the 21, 7 were untraceable and 2 had died. Ten of the 12 traceable people had ulcer recurrence. Of the 105 people who adhered to stockings, 33 (31%) had ulcer recurrence over a 5-year period of follow-up.
In studies that compared the effectiveness of two levels of compression pressure, recurrence rates ranged from 14% to 39% for stockings with lower pressure and from 12% to 32% for stockings with relatively higher pressure. None of the studies found a significant difference between the two groups. Recurrence rates reported by RCTs are shown in Table 3.
Table 4 shows risk ratios that we calculated for recurrence rates in RCTs.
Table 4:
Risk Ratios for Recurrence
| Author, Year | Follow-Up (Months) | Group 1 | Recurrence | Group 2 | Recurrence | Risk Ratio (95% CI) |
|---|---|---|---|---|---|---|
| Kapp et al, 201326 | 6 | 34–46 mm Hg | 6/44 (13.6%) | 23–32 mm Hg | 7/49 (14.3%) | 0.73 (0.23–2.3) P = .59 |
| Clarke-Moloney et al, 201425 | 12 | 25–35 mm Hg | 6/50 (12%) | 18–24 mm Hg | 10/50 (20%) | 0.60 (0.23–1.52) P = .28 |
| Nelson et al, 200627 | 60 | 25–35 mm Hg | 48/149 (32%) | 18–24 mm Hg | 59/151 (39%) | 0.82 (0.61–1.12) P = .23 |
| Vandongen & Stacey, 200028 | 12 | MCS | 17/72 (24%) | No MCS | 44/81 (54%) | 0.43 (0.27–0.69) P = .001 |
Abbreviations: CI, confidence interval; MCS, medical compression stocking.
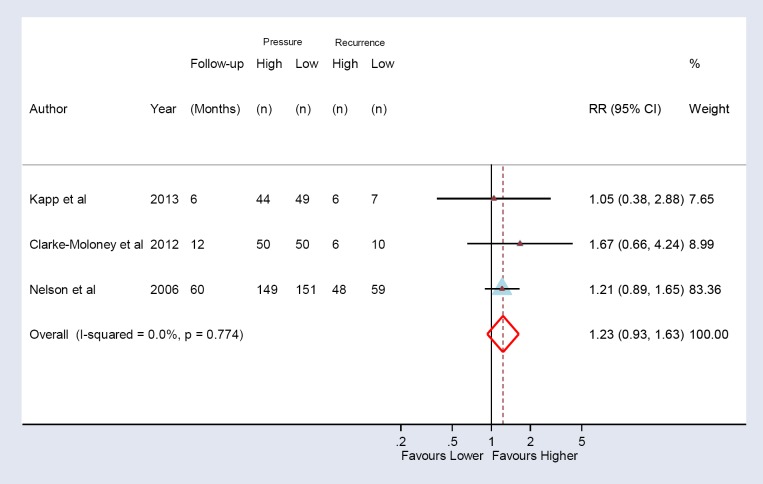
We meta-analyzed the recurrence rate of three RCTs comparing the effectiveness of different levels of compression pressure for the prevention of venous leg ulcer recurrence. The pooled estimate showed that recurrence rates were slightly higher for stockings with lower pressure than those for stockings with higher pressure, but the results did not reach statistical significance (Figure 2).
Figure 2: Recurrence Rate for Compression Stockings With Higher and Lower Compression Pressure.
Sources: Nelson et al, 200627; Kapp et al, 201326; Clark-Moloney et al, 2014.25
Time to Recurrence
Only one RCT reported data for time to recurrence for any ulcer on the leg. In a group randomized to compression stockings of 23–32 mm Hg pressure, ulcers recurred in 78 ± 59 days.26 In a comparison group with compression stockings of 34–46 mm Hg pressure, ulcers recurred in 57 ± 61 days. However, a significantly higher percentage of participants in the 34–46 mm Hg group did not adhere to the compression protocol compared with those who were assigned to the 23–32 mm Hg group (61.4% vs. 28.6%; P = .003). Another RCT27 reported no difference between lower and higher pressure stockings in time to recurrence (P = .14).
Adherence Rate
We found three RCTs that compared stockings with different levels of pressure, and one observational study that reported adherence. In one RCT, the adherence rate was higher for stockings with lower pressure than for stockings with higher pressure. Table 5 provides a summary of the adherence rates reported by the RCTs.
Table 5:
Adherence Rate: Compression Stockings With Different Pressure
| Author, Year | Follow-Up (Months) | Pressure (mm Hg) | Adherence | Pressure (mm Hg) | Adherence | P |
|---|---|---|---|---|---|---|
| Kapp et al, 201326 | 6 | 34–46 | 38.6% | 23–32 | 71.4% | .003 |
| Clarke-Moloney et al, 201425 | 12 | 25–35 | 90% | 18–24 | 86% | .76 |
| Nelson et al, 200627 | 60 | 25–35 | Stopped wearing MCS: 2% Switched to other group: 40% |
18–24 | Stopped wearing MCS: 2% Switched to other group: 25% |
NA |
Abbreviations: MCS, medical compression stocking; NA, not available.
In the observational study, participants wearing stockings of 40 mm Hg pressure were categorized as good, poor, and none with respect to their adherence to protocol.31 Twenty five of 53 participants (47%) had good adherence and 28 (53%) had either poor or no adherence to the stocking protocol.
Quality of Life
Reich-Schupke et al30 reported on a prospective observational study on the quality of life and adverse effects of compression therapy. A questionnaire was sent to adults with stages C2–C6 chronic venous insufficiency who were being treated with compression therapy at a vein centre in Germany.
Two hundred questionnaires were sent and 110 were returned (55%). Seventy-two (65.5%) respondents were female and 38 (34.5%) were male. The respondents were being treated with compression therapy due to sclerotherapy (41.8%), venous surgery (37.3%), leg ulcer (13.6%), conservative therapy for venous insufficiency (12.7%), post-thrombotic syndrome (11.8%), deep vein thrombosis (4.5%), and other reasons (8.2%). Some respondents qualified under more than one category. Compression therapy was applied mostly through compression stockings (97%). The mean duration of compression therapy was 61.5 ± 135.5 months for those who had leg ulcers, 23.63 ± 56.02 months for those who had surgery, and 22.53 ± 61.39 months for those who had sclerotherapy.
Life quality items were scored from 0 to 4, with 0 indicating no problem and 4 indicating discomfort or concern. Responses to quality of life experiences are shown in Table 6.
Table 6:
Quality of Life Scores
| Life Quality Items | Median Score |
|---|---|
| Global health | 1.36 |
| Handling of symptoms | 1.32 |
| Global life quality | 1.29 |
| Symptoms of the legs | 1.25 |
| Anxiety and worries | 1.21 |
| Life satisfaction | 1.18 |
| Functional status | 0.84 |
The results suggest that compression therapy did not have a substantial negative impact on quality of the life for most respondents. Reported impressions of stockings included functional (56.4%), comfortable (29.1%), uncomfortable (19.1%), and intolerable (1.8%).
The authors performed a subgroup analysis according to the duration of treatment (< 2 mo, 2–12 mo, 13–48 mo, and > 48 mo).30 All groups reported improvement in their symptoms. There were no significant differences between the groups for acceptance of use or changes they felt in their legs. The primary complaint across all groups was suboptimal fitting of stockings that caused slipping or uncomfortable contraction.
Adverse Effects
One RCT26 reported that 9% of participants experienced adverse effects. Eight (8%) reported discomfort with the stockings due to tightness and one (1%) had skin irritation due to sensitivity, which was resolved in 3 days by removing the stocking. All participants who experienced adverse effects agreed to remain in the study for follow-up.
Respondents to the questionnaire from Reich-Schupke et al30 reported dryness (58.5%), itching of the legs (32.7%), slipping (29.1%), constriction of the leg (24.5%), scaling (24.5%), sweating (19.1%), feeling of cold (15.5%), redness (10.9%), pain (6.4%), paresthesia (5.5%), restriction of the movement in the ankle region (4.5%), and a burning sensation (1.8%).
Critical Appraisal of the Evidence
We used the Cochrane risk of bias tool22 to assess the risk of bias for RCTs and ROBINS-I23 for non-randomized studies. We evaluated the quality of the body of evidence for each outcome according to the GRADE methodology. Randomized controlled trials were downgraded due to the high rate of nonadherence to the study or to the randomized group. Tables A1 and A2 (Appendix 2) show our evaluation of the risk of bias and Tables A3–A5 (Appendix 2) show the overall quality of evidence.
Discussion
We found that compression stockings are an effective intervention to reduce the risk of ulcer recurrence. One RCT that randomized participants into compression stockings and no compression showed that the recurrence rate at 12 months was two times higher among participants in the no-compression group (GRADE: Moderate).28 The pooled estimate for 3 RCTs that compared compression stockings with different levels of pressure did not show a statistically significant difference in ulcer recurrence rates.
Generally, stockings with a 25–35 mm Hg pressure have a clear effect on superficial veins, but less or no effect on the deep veins of the leg. Higher pressure stockings, such as 35–45 mm Hg or higher, show benefits for both the superficial and deep veins and are more effective when deep venous systems are involved.31 In a study by Clarke-Moloney,25 one third of participants who had both superficial and deep vein incompetence and were assigned to low pressure stockings developed ulcers.
Patient adherence to compression stockings is an important factor for the intervention to be effective. One RCT25 showed that the risk of ulcer recurrence was six times higher in those who did not adhere to stockings than in those who adhered. One observational study31 demonstrated that the recurrence rate was much lower in people who adhered to compression stockings (4% recurrence) than in those who did not (79% recurrence). High-pressure compression stockings were associated with lower adherence levels due to higher rates of discomfort. There is insufficient evidence to determine whether the lower adherence rate for high pressure stockings is offset by their higher effectiveness.
Overall, patients reported improvement in their leg symptoms without a substantial negative impact on their quality of life. However, 19% reported discomfort and about 2% reported that the discomfort was intolerable. The main problem people found with their stockings was suboptimal fitting that caused slipping or uncomfortable contraction. The use of compression stockings is usually safe, although some adverse effects may occur, including allergic reaction and damage to the skin tissue. However, most adverse effects can be minimized or prevented.
Our results are comparable with a previous Cochrane systematic review by Nelson and Bell-Syer.7 Their search was conducted in 2014, when only three RCTs and one abstract were available for assessment.
Limitations
There are few published studies investigating the effect of compression therapy in the prevention of venous leg ulcer recurrence. Most studies of venous leg ulcers focus on ulcer treatment strategies rather than on prevention of recurrence.
Conclusions
The available evidence shows that compression stockings are safe and effective in preventing venous leg ulcer recurrence. In people with a healed venous leg ulcer, wearing a compression stocking helps to reduce the risk of recurrence by about half (GRADE: Moderate).
ECONOMIC EVIDENCE
Research Question
What is the cost-effectiveness of compression stockings for the prevention of venous leg ulcer recurrence in people with a healed venous ulcer, based on the published literature?
Methods
We performed an economic literature search on November 23, 2017, for studies published from inception to the search date. To retrieve relevant studies, the search was developed using the clinical search strategy with an economic filter applied.
We created database auto-alerts in MEDLINE, Embase, and CINAHL and monitored them for the duration of the HTA review. We performed targeted grey literature searching of health technology assessment agency websites, clinical trial registries, and Tufts Cost-Effectiveness Analysis Registry. See Clinical Literature Search, page 13, above, for further details on methods used, and Appendix 1 for literature search strategies, including all search terms.
Literature Screening
A single reviewer reviewed titles and abstracts, and, for those studies likely to meet the eligibility criteria, we obtained full-text articles and performed further assessment for eligibility.
Inclusion Criteria
English-language full-text publications
Studies published from inception to November 23, 2017
Studies examining compression stockings for the prevention of venous leg ulcer recurrence in people with a healed venous ulcer
Cost–utility, cost-effectiveness, or cost-benefit analyses
Exclusion Criteria
Reviews, letters or editorials, case reports, commentaries, abstracts, and posters
Studies that conducted an economic evaluation on people with unhealed leg ulcers
Outcomes of Interest
Costs
Quality-adjusted life-years (QALYs) or time without recurrence
Incremental cost and incremental effectiveness
Incremental cost per QALY or per other health outcome gained
Data Extraction
We extracted relevant data on the following:
Source (i.e., name, location year)
Population and comparator
Interventions
Outcomes (i.e., health outcomes, costs, and incremental cost-effectiveness ratio) We contacted authors of the studies to provide clarification as needed.
Study Applicability
We determined the usefulness of each identified study for decision-making by applying a modified applicability checklist for economic evaluations that was originally developed by the National Institute for Health and Care Excellence (NICE) in the United Kingdom.33 The original checklist is used to inform development of clinical guidelines by NICE. We retained questions from the NICE checklist related to study applicability and modified the wording of the questions to remove references to guidelines and to make it Ontario-specific. A summary of the number of studies judged to be directly applicable, partially applicable, or not applicable to the research question is presented.
Results
Literature Search
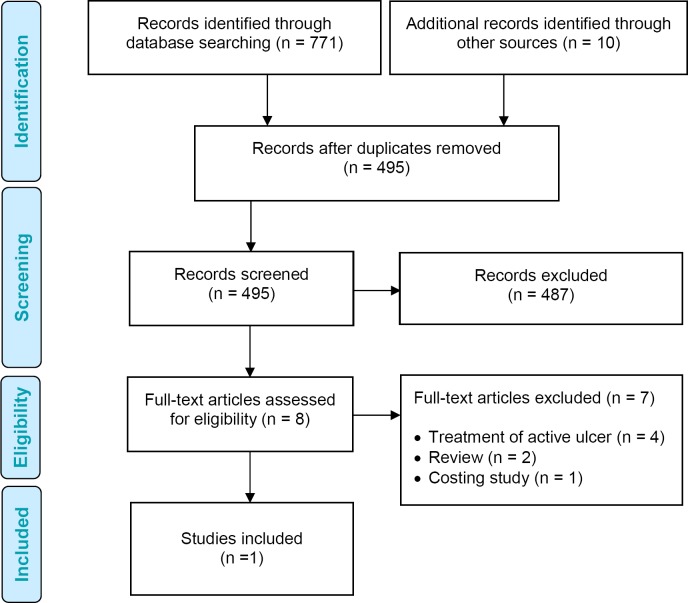
The literature search yielded 495 citations published between inception and November 23, 2017, after removing duplicates. We excluded a total of 487 articles based on information in the title and abstract. We then obtained the full texts of eight potentially relevant articles for further assessment.34–40 Figure 3 presents the flow diagram for the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
Figure 3: PRISMA Flow Diagram—Economic Search Strategy.
Source: Adapted from Moher et al.32
After review of the eight full-text articles, we found that one study34 met the inclusion criteria. We reviewed the reference list for any additional studies not identified through the systematic search. Excluded studies included two reviews,35,36 four cost-effectiveness analyses that evaluated treatment of active venous ulcers,37–40 and one costing study31 that estimated only the costs of healing in people with primary and recurred ulcers.
Review of Included Economic Studies
Table 7 provides a summary of the included study,34 a model-based cost–utility analysis conducted over a lifetime horizon from a United States health payer perspective. The results indicate that ulcer prevention with compression stockings and patient education is dominant (less costly and more effective) compared with no intervention in people with healed venous ulcers. In the study, compression stockings plus patient education led to 0.37 more QALYs and saved $5,904 USD per patient, compared to no intervention.34 The authors conducted several sensitivity analyses. When the cost of amputations or ulcer treatment was excluded, or when the cost of stockings were increased by 600%, compression stockings with patient education remained cost-effective at a willingness-to-pay threshold below $60,000 USD per QALY gained. Compression stockings were no longer cost-effective when the mean time to ulcer recurrence for people using stockings was shorter (21.1 months).
Table 7:
Results of Economic Literature Review—Summary
| Author, Year, Location | Study Design, Analytic Technique, Perspective, and Time Horizon | Population | Intervention/Comparator | Results | ||
|---|---|---|---|---|---|---|
| Health Outcomes | Costsa | Cost-Effectiveness | ||||
| Korn et al., 2002, United States34 |
|
55-year-old patients with prior leg ulcer |
|
Total QALYs:
|
Total cost:
|
CS with PE dominated (more effective, less costly) no intervention |
Abbreviations: CS, compression stockings; PE, patient education; QALY, quality-adjusted life-year.
All costs in US dollars.
Perspective of Medicare and other insurers.
Applicability of the Included Study
The results of the applicability checklist for economic evaluations applied to the included study is presented in Appendix 2 (Table A6). The study was deemed partially applicable to the research question.
Discussion
Our systematic review identified one study evaluating the cost–utility of prevention with compression stockings and patient education compared to no intervention in 55-year-old patients with prior venous leg ulcers.34 Authors obtained recurrence rates and patient adherence data from a published retrospective review of clinic records41 and clinical trials with 15 years follow up.42 Costs were derived from the cost accounting system at the New York Presbyterian Hospital (Transition Systems, Inc, Boston, MA) and the published literature. The authors concluded that compression stockings plus patient education was effective and cost saving, even under conservative assumptions.34
The study by Korn et al34 has several limitations that may limit the applicability of the study results to the Ontario setting. First, the study was conducted from a US health payer perspective. Second, although the specified target population was people with healed ulcers, some transition probabilities for the analysis were obtained from studies of patients with active ulcers. Third, amputation was included in the model as a potential complication, but it is unclear how the risk of amputation was derived for this population. Finally, Korn et al evaluated prophylactic compression stockings combined with patient education.34 Our review examines the effectiveness and cost-effectiveness of compression stockings alone, and not in combination with a patient education program.
Conclusions
One study showed that compression stockings with patient education for the prevention of venous leg ulcers was effective and cost saving, at least in the US context. No studies identified were directly applicable to the Ontario or Canadian health system perspective.
PRIMARY ECONOMIC EVALUATION
The published economic evaluation identified in the literature review examined the cost-effectiveness of compression stockings for the prevention of venous leg ulcers, but the study did not take a Canadian perspective. Further, the study looked at compression stockings in combination with a patient education program. Owing to these limitations, we conducted a primary economic evaluation.
Research Question
What is the cost-effectiveness of compression stockings compared with usual care (no compression stockings) in preventing the recurrence of venous leg ulcers from the perspective of the Ontario Ministry of Health and Long-Term Care?
Methods
The information presented in this report follows the reporting standards set out by the Consolidated Health Economic Evaluation Reporting Standards Statement.43
Type of Analysis
We conducted a reference case analysis and various types of sensitivity analyses. Our reference case analysis adhered to the Canadian Agency for Drugs and Technologies in Health (CADTH) guidelines,44 where appropriate, and represents the analysis with the most likely set of input parameters and model assumptions. In sensitivity analyses, we explored how the results are affected by varying input parameters and model assumptions.
We performed a cost–utility analysis that assessed the cost per QALY gained.
Target Population
The study population of interest was people aged 65 with a healed venous leg ulcer who are at risk of ulcer recurrence.
Our target population was based on a randomized controlled trial with a 5-year follow-up.27 The study was conducted in leg ulcer clinics in two hospitals in Scotland.27 The study included 300 outpatients (71% female) with recently healed venous ulcers and no significant arterial disease, rheumatoid disease, or diabetes mellitus. The average age and sex ratio from this study is similar to that for venous leg ulcer patients in Ontario.40
Perspective
We conducted this analysis from the perspective of the Ontario Ministry of Health and Long-Term Care.
Intervention and Comparator
We compared preventative treatment with compression stockings to no compression stockings. Compression stockings come in different classes, based on the pressure (measured in mm Hg) provided at the ankle.
Currently, there are no international standards on the classification of compression stockings. Our analysis used clinical data from the previously described RCT conducted in Scotland.27 That study adopted the UK classification of compression therapies45:
Class 1 represents compression at the ankle of 13–17 mm Hg
Class 2 represents compression at the ankle of 18–24 mm Hg
Class 3 represents compression at the ankle 25–35 mm Hg
North American classification46 includes the following compression classes:
Support represents compression at the ankle of 15–20 mm Hg
Class 1 represents compression at the ankle of 20–30 mm Hg
Class 2 represents compression at the ankle of 30–40 mm Hg
Class 3 represents compression at the ankle of 40–50 mm Hg
In practice, North American Class 3 is infrequently prescribed or tolerated by patients (Laura Teague, written communication, Dec 11, 2017).
For clarity, throughout this report we discuss the level of compression by reference to mm Hg at the ankle and we assume that UK clinical evidence and classifications are generalizable to Ontario.
Our intention was to examine the cost-effectiveness of compression therapy. We did not attempt to determine the relative cost-effectiveness of specific compression values (classes) versus other compression values. We assumed that the compression class prescribed would be determined based on patient history and preferences. Table 8 summarizes the interventions evaluated in the economic model.
Table 8:
Disease Interventions and Comparators Evaluated in the Primary Economic Model
| Intervention | Comparator | Patient Population | Outcomes | Reference |
|---|---|---|---|---|
| Compression stockings | No compression stockings | People with a healed venous leg ulcer, aged 65 y, 71% female | QALYs | Nelson et al, 200627 |
Abbreviation: QALY, quality-adjusted life-year.
Outcomes of Interest
Effectiveness outcomes: QALYs
Direct medical costs
-
Incremental cost-effectiveness/cost–utility ratio (ICER): cost per QALY gained
∘ The ICER is given by the difference in mean expected costs (i.e., incremental cost, ΔC) between the two compared strategies divided by the difference in mean expected outcomes (i.e., incremental effect, ΔE) between these strategies (ICER = ΔC/ΔE)
Discounting and Time Horizon
We applied an annual discount rate of 1.5% to both costs and QALYs based on the most recent CADTH economic guidelines.44 We used a 5-year time horizon in all analyses based on the longest follow up time reported in our clinical review and a recent Cochrane review on ulcer prevention.7
Model Structure
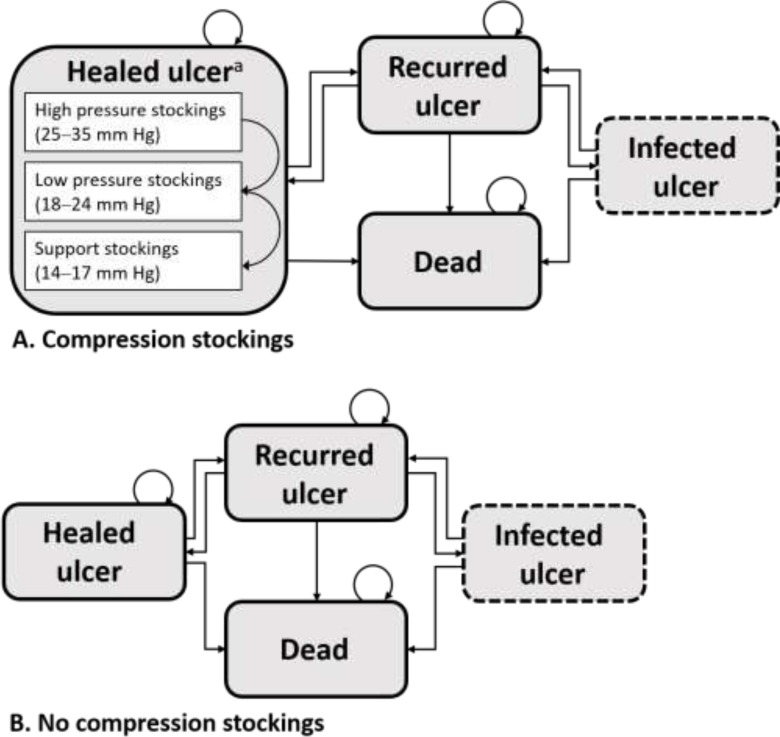
We developed a state-transition Markov model to determine the incremental cost per QALY (Figure 4). The model was adapted from a model structure developed by Nherera et al.47 for people with the chronic venous leg ulcers. We used 1-month cycles to follow people over 5 years.
Figure 4: Markov Model Structure.
aNonadherent patients switch to lower pressure stockings.
The main Markov health states are as follows:
Healed ulcer: people with a healed venous leg ulcer
Recurred ulcer: people who develop a venous leg ulcer on the reference limb (the limb with the healed ulcer)
Infected ulcer: people with a venous leg ulcer exposed to bacterial infection with the symptoms of worsening pain, a green or unpleasant discharge coming from the ulcer, redness and swelling of the skin around the ulcer, and/or a high temperature (fever)48
Dead: Death could be the result of comorbidities or any other cause
Further health states are used to capture adherence to compression stockings
Everyone entered the Markov model in the healed ulcer health state. People in the compression stockings arm were treated with compression stockings for the duration of the model (Figure 4A). People in the no compression stockings arm did not receive any compression stockings for the duration of the model (Figure 4B).
We considered three ranges of compression stockings in our model, based on the UK classes:
High pressure (25–35 mm Hg compression at the ankle)
Low pressure (18–24 mm Hg compression at the ankle)
Support (13–17 mm Hg compression at the ankle)
We excluded 40–50 mm Hg compression at the ankle as it is rarely used in clinical practice (see Intervention and Comparator, above).
Based on the RCT conducted by Nelson and colleagues,27 we assumed that all individuals would initially be prescribed high pressure or low pressure compression stockings. That is, some individuals in the compression stockings arm would start in the high-pressure range and others in the low-pressure range.
Over the course of the study, people could transition between states if events warranted. For instance, a person who had a leg ulcer recurrence would transition from the healed ulcer health state to the recurred ulcer health state. The infected ulcer health state is a temporary condition. We assumed people who move from the recurred ulcer health state to the infected ulcer health state would heal after 1 month and return to their previous (recurred ulcer) health state. Because the infected ulcer health state is of shorter duration, we distinguish it from the other health states in Figure 4 with a dashed border.
People in the compression stockings group could adhere (i.e., wear the prescribed compression stockings) or not adhere (i.e., fail to wear the prescribed compression stockings) with the intervention. Those who did not adhere to the prescribed treatment were changed to lower pressure stockings (those originally prescribed high pressure would switch to low pressure and those originally prescribed low pressure would switch to support; see Figure 4A). We assumed that nonadherence would occur at a steady rate over the 5-year time horizon. We also assumed that all patients would adhere with second-line compression stockings. This was consistent with the trial conducted by Nelson and colleagues,27 which found only 2.7% of patients did not adhere to any compression level over the 5-year time horizon. We tested this assumption in a sensitivity analysis. Further, we assumed that people with a recurrence and subsequent healing of an ulcer would return to the previous level of compression and that this would hold for the duration of the model unless they did not adhere.
People in the no compression stocking group (usual care) had a similar model structure (Figure 4B).
Main Assumptions
The major assumptions for this model are:
Everyone has a healed venous leg ulcer before entering the model
People who get an ulcer during the model will go back to the same compression grade once healed
People (alone or with the help of a caregiver) are responsible for putting on and removing their own compression stockings
Compression stockings are replaced every four months
All infections require treatment with antibiotics, but there are no other complications that affect QALYs or cost
People with infected ulcers spend no more than 1 month in the infected ulcer health state
People who change to a lower pressure stocking because they did not adhere to treatment will adhere to this lower pressure treatment
The adherence rate does not change over time
Classes in Ontario are equivalent with those used in the model
Everyone starts on low pressure (18–24 mm Hg) or high pressure (25–35 mm Hg) compression stockings
Clinical Input Parameters
We obtained our clinical input parameters from the published literature and expert opinion (Table 9).
Table 9:
Input Parameters: Probabilities and Risks
| Model Parameter | Mean | Rangea | Reference |
|---|---|---|---|
| Initial distribution of people in compression stockings arm | |||
| High pressure (25–35 mm Hg) | 0.3 | 0.1–0.5 | Expert opinion |
| Low pressure (18–24 mm Hg) | 0.7 | 0.4–0.9 | Expert opinion |
| Support (14–17 mm Hg) | 0 | 0.1–0.3 | Expert opinion |
| Monthly probabilities and rates | |||
| Probability of nonadherence: | |||
| High pressure (25–35 mm Hg) | 0.009 | 0.006–0.012 | Nelson et al, 200627 |
| Low pressure (18–24 mm Hg) | 0.005 | 0.003–0.007 | Nelson et al, 200627 |
| Support (14–17 mm Hg) | 0.0005b | 0.0002–0.0008 | Nelson et al, 200627 |
| Probability of ulcer recurrence, compression stockings: | |||
| High pressure (25–35 mm Hg) | 0.006 | 0.004–0.008 | Nelson et al, 200627 |
| Low pressure (18–24 mm Hg) | 0.008 | 0.006–0.010 | Nelson et al, 200627 |
| Support (14–17 mm Hg) | 0.010 | 0.008–0.012 | Assumption |
| Weighted average | 0.0077 | 0.0070–0.0085 | Calculation based on above |
| Risk of ulcer recurrence: | |||
| Compression stockings vs. no compression stockings | 0.43 | 0.27–0.69 | Vandongen & Stacey, 200028 |
| Probability of ulcer healing with compression bandages | 0.163 | 0.147–0.179 | Pham et al, 201240 |
| Probability of infection | 0.05 | 0.1–0.01 | Carter et al, 201449 |
Ranges were used in one-way sensitivity analyses.
In the reference case analysis, we assume no one starts on support; therefore, this value is used only in the sensitivity analyses.
In the compression stockings arm of our model, people may be prescribed stockings of different compression pressures (18–24 and 25–35 mm Hg). We used expert opinion (Alexandria Crowe, written communication, Dec 22, 2017; David Keast, written communication, Jan 1, 2018) to estimate the distribution of compression classes prescribed in Ontario. To test the robustness of our model, we varied the distribution in sensitivity analysis, including an assumption that some individuals start compression at support level. Among individuals wearing stockings, the 5-year probability of nonadherence was obtained from an RCT conducted by Nelson et al.27 In the RCT, 42% of people with high pressure stockings and 28% with low pressure stockings did not adhere to their prescribed class of compression stockings. We calculated the monthly probability of nonadherence and assumed that it remained constant over the 5-year time horizon. People who did not adhere with the prescribed treatment were switched to lower pressure stockings as described previously (people at the support level went to no stockings).
We used data from a randomized controlled trial with a 5-year follow-up conducted in Scotland27 to determine ulcer recurrence rates. We converted 5-year ulcer recurrence rates to monthly transition probabilities (Appendix 4, Table A8). In people consistently receiving support stockings (14–17 mm Hg), we used expert opinion to estimate ulcer recurrence rates that are higher than in those consistently receiving low pressure (18–24 mm Hg) compression stockings (Laura Teague, written communication, Jan 16, 2018).
To determine the ulcer recurrence rate in the no compression stockings arm of our model, we obtained the relative risk of ulcer recurrence from our clinical evidence review based on an Australian randomized control trial.28 The authors compared compression stockings with no compression stockings and reported the time to ulcer recurrence over a 2-year follow-up. We multiplied the inverse relative risk by the weighted probability of ulcer recurrence in the compression stockings arm to derive ulcer recurrence in the no compression stocking group. We determined the weighted probability of ulcer recurrence based on the distribution of people in each compression class at the beginning of the model multiplied by the corresponding probability of ulcer recurrence. We assumed that all people with a recurred ulcer were treated with bandages and were adherent to treatment. We obtained the probabilities of acute ulcer healing from the Canadian Bandaging Trial.40 This trial followed 424 people with venous insufficiency and a healed leg ulcer, who were ≥ 65 years of age, for 1 year.
Infection rates were estimated based on a previous economic model.49 We assumed that patients would recover from infection after 1 month.
Lastly, our model accounted for age-dependent background mortality in Ontario. We used the results of a 5-year prospective cohort study showing that survival in people with venous ulcers was not significantly different from control50 to assume a mortality rate that is the same for all health states.
Utility Parameters
We quantified health outcomes as QALYs. The utility values used to derive QALYs can be found in Table 10. These values were obtained by Pham et al,40 who collected health utility data from 424 people with healed or active venous leg ulcers using the EQ5D questionnaire. We assumed the utility of an infected ulcer to be the same as an unhealed ulcer (Laura Teague, written communication, Jan 16, 2018). We varied the utility of infected ulcers in sensitivity analyses.
Table 10:
Utility Parameters Used in the Economic Model
| Health State | Utility (Base Case) | Rangea | Reference |
|---|---|---|---|
| Recurred ulcer | 0.77 | 0.74–0.79 | Pham et al, 201240 |
| Healed ulcer | 0.87 | 0.79–0.94 | Pham et al, 201240 |
| Infected ulcer | 0.77 | 0.70–0.90 | Assumption |
Ranges were used in one-way sensitivity analyses.
Costs and Resource Use
All cost and resource use parameters included in our study were obtained from consultation with experts, the Ontario Schedule of Benefits for Physician Services, the Ontario drug benefit formulary, Registered Nurses' Association of Ontario, an online compression stocking vendor, and the Canadian Bandaging Trial (see Table 11).
Table 11:
Resource Utilization and Costs Used in the Economic Model
| Variable | Value (Reference Case)a | Rangea,b | Reference |
|---|---|---|---|
| Healed ulcer health state resource use and costs | |||
| Compression stockings cost: | |||
| High pressure (25–35 mm Hg) | $82.1 | $54.0–$110.0 | |
| Low pressure (18–24 mm Hg) | $66.9 | $43.2–$91.8 | |
| Support (13–17 mm Hg) | $33.1 | $25.2–$44.2 | Vendor51 |
| Annual pairs of compression stockings required for preventing venous leg ulcer | 3 | 2–4 | Alexandria Crowe, written communication, Dec 22, 2017 Afsaneh Alavi, written communication, Jan 7, 2018 |
| Total monthly stockings cost: | |||
| High pressure (25–35 mm Hg) | $20.5 | $9.0–$36.7 | Calculation based on above |
| Low pressure (18–24 mm Hg) | $16.7 | $7.2–$30.6 | Calculation based on above |
| Support (13–17 mm Hg) | $8.3 | $4.2–$14.7 | Calculation based on above |
| Nursing cost: | |||
| Nurse hourly rate | $40.8 | $34.1–$45.2 | RNAO,52 includes 13% benefits; ONA Collective agreement53 |
| Length of each nursing visit | 30 min | 20–40 min | Alexandria Crowe, written communication, Dec 22, 2017 |
| Cost per nursing visit | $20.4 | $11.4–$30.1 | Calculation based on above |
| Annual number of nursing visits | |||
| Compression stockings | 1 | 0–2 | Alexandria Crowe, written communication, Feb 8, 2018; David Keast, written communication, Feb 14, 2018 |
| No compression stockings | 1 | 0–2 | Alexandria Crowe, written communication, Feb 8, 2018; David Keast, written communication, Feb 14, 2018 |
| Total monthly nursing cost: | |||
| Compression stockings | $1.7 | $0.0–$5.0 | Calculation based on above |
| No compression stockings | $1.7 | $0.0–$5.0 | Calculation based on above |
| Physician cost: | |||
| Family physician repeat consultation Annual physician visits |
$45.9 | Schedule of benefits54 (Code A006) | |
| Compression stockings | 1 | 0–2 | Alexandria Crowe, written communication, Feb 8, 2018; David Keast, written communication, Feb 14, 2018 |
| No compression stockings | 1 | 0–2 | Alexandria Crowe, written communication, Feb 8, 2018; David Keast, written communication, Feb 14, 2018 |
| Total monthly physician cost: | |||
| Compression stockings | $3.8 | $0–$7.7 | Calculation based on above |
| No compression stockings | $3.8 | $0–$7.7 | Calculation based on above |
| Total monthly cost in healed ulcer health state: | |||
| Compression stockings | |||
| High pressure (25–35 mm Hg) | $26.1 | $9.0–$49.3 | Calculation based on above |
| Low pressure (18–24 mm Hg) | $22.2 | $7.2–$43.3 | Calculation based on above |
| Support (13–17 mm Hg) | $13.8 | $4.2–$27.4 | Calculation based on above |
| No compression stockings | $5.5 | $0–$12.7 | Calculation based on above |
| Recurred ulcer health state resource use and costs | |||
| Total monthly cost in recurred ulcer health state | $128 | $116–$149 | Pham et al. 201240 |
| Infected ulcer health state resource use and costs | |||
| Monthly cost of recurred ulcer | $128 | $116–$149 | Pham et al. 201240 |
| Additional physician cost: | |||
| Debridement of ulcer | $20 | Schedule of benefits,54 (Code Z080) | |
| Monthly visits, debridement of ulcer, n | 1 | 0–2 | |
| Application of Unna's paste | $14.9 | Schedule of benefits,54 (Code Z200) | |
| Monthly visits, application Unna's paste, n | 4 | 2–6 | |
| Total additional monthly physician cost | $79.6 | $29.8–$129.4 | Calculation based on above |
| Antibiotic cost: | |||
| 1st line | |||
| Keflex (cephalexin monohydrate) 500 mg, 4 times per d for 1 wk | $15.2 | $10.0–$30.0 | Ontario drug benefit formulary55 |
| 2nd linec | |||
| Clindamycin 300 mg, 3 times per d for 1 wk | $9.3 | $7.0–$12.0 | Ontario drug benefit formulary55 |
| 3rd linec | |||
| Azithromycin 500 mg for 1 d, then 250 mg/d for 4 d | $7.8 | $5.0–$10.0 | Ontario drug benefit formulary55 |
| Total monthly cost in infected ulcer health state | $222.9 | $155.7–$308.5 | Calculation based on above |
All costs given in 2018 Canadian dollars.
Ranges were used in one-way sensitivity analyses.
2nd and 3rd line therapy costs were used in scenario analyses.
To determine the monthly cost in each health state, we multiplied the expected resource use by unit costs (Table 11). In the healed ulcer health state, we included the costs of compression stockings (if applicable) and visits with health care professionals. Several types of health care professional may be involved in the prescribing and fitting of stockings. We included the costs of a physician and a nurse but acknowledge that, depending on the health care setting, these costs may vary. The cost in the recurred ulcer health state was obtained from the Canadian Bandaging Trial.40 In this trial, people with venous leg ulcers were treated over a 12-month period. We included the community care costs and visit costs to outpatient services, family physicians, specialists, and emergency rooms from the trial. Finally, in the infected ulcer health state, we included the costs associated with having a recurred ulcer (i.e., recurred ulcer health state) and an infection (i.e., additional physician and antibiotic costs). All costs are inflated, where applicable, and reported in 2018 Canadian dollars.
Analysis
In the reference case analysis, we applied a probabilistic approach and used actual values or mean values and distributions as the model inputs (Appendix 4, Table A7). We presented the results as incremental costs (difference in costs) and incremental QALYs (difference in QALYs) of compression stockings compared with no compression stockings.
We performed sensitivity analyses to address the uncertainty of model inputs and clinical scenarios. We assessed variability and uncertainty in several ways.
Probabilistic Sensitivity Analyses
We conducted a probabilistic sensitivity analysis (PSA) by assigning distributions to model parameters, where applicable. In the PSA, because cost data are skewed and cannot be negative,56 we used gamma distributions to represent the uncertainty of the cost parameters. We used beta distributions for probabilities and utilities because those estimates are confined to a range of 0 to 1.57 Input parameters used for our PSA are presented in Table A7 (Appendix 4). In Monte Carlo simulations, all parameters were randomly sampled from their assigned distributions, for a cohort of 1,000 patients. We presented the results graphically and then estimated the likelihood of each treatment strategy being optimal across a range of willingness-to-pay thresholds.
One-Way Sensitivity Analyses
We conducted one-way sensitivity analyses using the plausible ranges of our model inputs (Tables 9–11). This allowed us to examine the influence of individual parameters on our results.
Scenario Analyses
Our scenario analyses examined the robustness of our results given increased nonadherence, variation in health care service use, a lifetime horizon, and more expensive treatments for infection.
Scenario 1: All Nonadherent Patients Do Not Wear Compression Stockings
In our reference case analysis, we assumed that nonadherent patients will switch to stockings with lower compression. In scenario 1, we assume that people who are nonadherent would stop wearing stockings entirely. In this scenario, nonadherent patients incur the same costs as people in the no compression stockings arm.
Scenario 2: Greater Health Care Service Use by People Using Compression Stockings
In our reference case analysis, we assumed that all patients with a healed venous leg ulcer will have the same annual number of visits with health care professionals. This could underestimate the number of visits by people using compression stockings if people must connect with their health care provider more often (e.g., for new compression stockings, to switch pressure). In scenario 2, we assumed that people using compression stockings will have one additional nursing and physician visit per year than people who do not use compression stockings.
Scenario 3: Application of Lifetime Horizon
In our reference case analysis, we used a 5-year time horizon. This was based on the follow-up time of the RCT that provided our ulcer recurrence rates.27 The occurrence of venous leg ulcers is a chronic condition; therefore, in scenario 3, we examine the costs and effectiveness of compression stockings on a lifetime horizon.
Scenario 4: Intensive Infection Treatment
In our reference case analysis, we assumed that all patients whose leg venous ulcers were infected were treated by first-line therapy (cephalexin, see Table 11). In scenario 4, we assume that patients will not be treated with first line therapy, but instead are treated using second-(clindamycin) and third-line (azithromycin) therapies.58
Generalizability
The findings of this economic analysis cannot be generalized to all people with venous leg ulcers.
Expert Consultation
We solicited expert consultation on the resource use and costs associated with the use of compression stockings. The consultation included health care professionals who had experience working with people with venous leg ulcers. The role of the expert advisors was to advise on compression stocking use for the prevention of venous leg ulcer recurrence and the typical treatment trajectories of patients.
Results
Reference Case Analysis
The results from the reference case cost–utility analysis are presented in Table 12. On average, costs and QALYs were higher in people treated with compression stockings compared with usual care (no compression stockings). We estimated that the ICER was $27,300 per QALY and therefore that stockings can be considered cost-effective below a willingness-to-pay amount of $27,300 per QALY.
Table 12:
Reference Case Analysis Results
| Strategy | Average Total Costs (95% CI) | Incremental Costa (95% CI) | Average Total Effects, QALYsa(95% CI) | Incremental Effect,a QALYs (95% CI) | ICER, $/QALY |
|---|---|---|---|---|---|
| No compression stockings | 971 (342–2,197) | 4.040 (3.870–4.187) | |||
| Compression stockings | 1,518 (1,204–2,159) | 546 (−326 to 1,206) | 4.060 (3.891–4.202) | 0.02 (0.00–0.073) | 27,300 |
Abbreviations: CI, confidence interval; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year.
Incremental cost = average cost (strategy B) – average cost (strategy A).
Incremental effect = average effect (strategy B) – average effect (strategy A).
Note: All costs in 2018 Canadian dollars.
Sensitivity Analysis
Probabilistic Sensitivity Analysis
The majority (97.1%) of our simulations showed that compression stockings were more effective than no compression stockings. We also found that, in 8.5% of simulations, compression stockings were both more effective and less costly than no compression stockings.
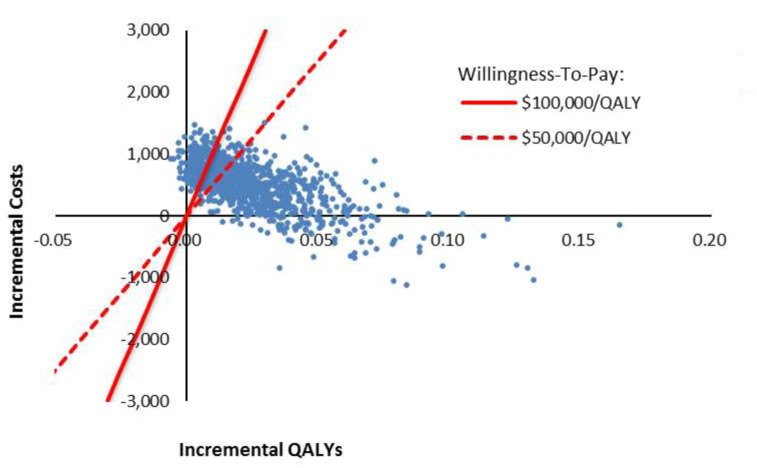
Compression stockings were cost-effective below willingness-to-pay amounts of $50,000 per QALY and $100,000 per QALY in 70.4% and 85.8% of simulations, respectively.
Figure 5 illustrates the uncertainty around the incremental costs and incremental QALYs of compression stockings compared with no compression stockings.
Figure 5: Incremental Costs Versus Incremental Quality-Adjusted Life-Years, Compression Stockings Versus No Compression Stockings.
Abbreviation: QALY, quality-adjusted life-year.
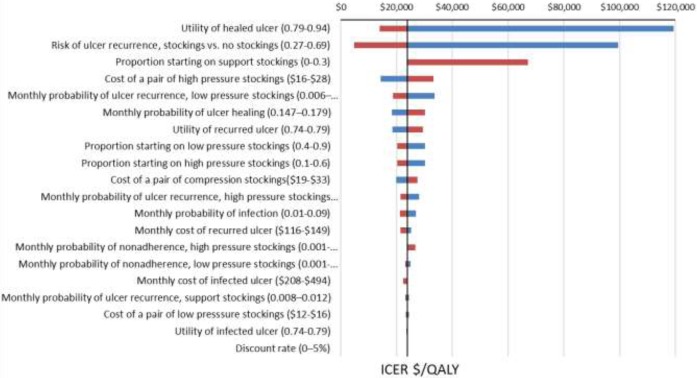
One-Way Sensitivity Analysis
Figure 6 presents the results of the one-way sensitivity analysis. When the utility of a healed ulcer was decreased, the ICER increased to more than $100,000 per QALY. Additionally, when the risk of ulcer recurrence for people with compression stockings or the proportion of people wearing lower-pressure (support) stockings was increased, the ICER increased to more than $50,000 per QALY.
Figure 6: One-Way Sensitivity Analysis, Reference Case, Compression Stockings Versus No Compression Stockings.
Abbreviations: ICER, incremental quality-adjusted life-year; QALY, quality-adjusted life-year.
Scenario Analysis
Table 13 presents the results from the scenario analysis. The ICER increased to $48,229 per QALY when we assumed people using compression stockings would visit health care providers more frequently than people not using stockings. The ICERs did not change dramatically across other scenarios.
Table 13:
Scenario Analysis Results, Stockings Versus No Stockings
| Scenario | Incremental Cost ($) | Incremental Effect, QALYs | Results ($/QALY) |
|---|---|---|---|
| Scenario 1: All nonadherent patients do not wear compression stockings | 495 | 0.020 | 24,750 |
| Scenario 2: Greater health care service use by people using compression stockings | 1,115 | 0.023 | 48,229 |
| Scenario 3: Application of lifetime horizon | 1,568 | 0.084 | 18,667 |
| Scenario 4: Intensive infection treatment | 549 | 0.023 | 23,767 |
Discussion
Our model-based cost–utility analysis showed that using compression stockings for the prevention of venous leg ulcer recurrence is likely a cost-effective intervention. The use of compression stockings led to a small increase in costs and health outcomes.
Our analysis has several strengths. We used a Markov model, and thus were able to capture clinical consequences, including ulcer recurrence, nonadherence, and the use of various ranges of compression over time. The probability of ulcer recurrence and nonadherence included in our model was based on the largest and longest RCT conducted to date on the prevention of leg ulcer recurrence.27 We used Ontario-specific costing data.
Our model also has several limitations. We assumed that adherence to compression stockings would occur at a constant rate. However, studies from our clinical review,25,26,31 including Nelson et al,27 reported mean adherence over the entire follow-up period without including data on patterns of nonadherence. Actual nonadherence rates may fluctuate over time. In some people, adherence may be related to the ease with which stockings can be put on and removed. We assumed that people (with or without the help of a caregiver) could put on and remove their stockings. In reality, some people may require assistance through equipment (i.e., doffing and donning aids) or health care providers (e.g., through home care). While providing such supports could result in additional costs, these additional costs may be offset through increased adherence to stockings.
Additionally, we assumed that people who do not adhere with their initially prescribed treatment would switch to and stay on lower pressure stockings. We base this assumption on Nelson et al,27 the primary RCT used in our analysis. Nelson and colleagues reported that a very small proportion of patients (2.7% over 5 years) did not adhere to any stockings, while a large proportion (35% over five years) switched to lower pressure stockings and adhered to the new protocol. We recognize that RCTs are usually well-controlled studies that may not reflect real-world practice settings and that real-world rates of nonadherence may be higher than assumed in our model. However, we used RCT nonadherence rates obtained from the same source and population as our recurrence rate estimates. Nonadherence was validated by the nurses and physicians involved in the trial. In addition, we conducted a scenario analysis showing the impact of nonadherent patients not using any stockings (as opposed to switching to lower stockings). In this scenario, compression stockings remained cost-effective with an ICER of $24,750 per QALY.
We did not take into consideration the impact of compression stockings on other downstream venous insufficiency treatments. If compression stockings reduce the occurrence of venous leg ulcers, they may also reduce the need for other treatments (e.g., ablation or surgical intervention). However, we took a conservative approach focusing only on the impact of decreasing ulcer occurrence. Additional benefits could improve the cost-effectiveness of compression stockings.
Our results were sensitive to a few parameters, including the risk of ulcer recurrence. There was a scarcity of evidence on the risk of recurrence between people with and without compression stockings. Our clinical review and a recently published Cochrane review7 identified only one study28 that compared people using preventive compression stockings with people treated without stockings. Previous economic evaluations have used similar rates for ulcer recurrence.34
When considering uncertainty in several parameters simultaneously through the probabilistic sensitivity analysis, there was a high probability (>70%) that compression stockings were cost-effective at willingness-to-pay amounts of $50,000 per QALY and $100,000 per QALY. The stockings may reduce ulcer recurrence and treatment costs for those who adhere to the treatment.
Conclusions
Our economic evaluation suggests that compression stockings may provide good value for money compared with no compression stockings for the prevention of venous leg ulcers. There was some uncertainty in our results, but most simulations (>70%) showed that the incremental cost-effectiveness ratio remained below $50,000 per QALY.
BUDGET IMPACT ANALYSIS
Research Question
What is the 5-year budget impact of publicly funding compression stockings for the prevention of venous leg ulcer recurrence, from the perspective of the Ontario Ministry of Health and Long-Term Care?
Methods
Analytic Framework
The budget impact of compression stockings for the prevention of venous leg ulcer recurrence was estimated as the cost difference between two scenarios:
The current scenario, which is no public funding for compression stockings, and
The anticipated clinical practice with public funding for compression stockings
Target Population
The target population in our reference case analysis was adults with healed venous leg ulcers. Our primary economic evaluation focused on adults over 65, while the budget impact captures the full population that may be eligible for compression stockings if it were publicly funded. In our scenario analysis, we focus on public funding for compression stockings in the over-65 population.
Using population data from the Ministry of Finance,59 we determined that the current size of the Canadian population over 25 years of age is about 10,338,000. We assumed that leg ulcers are very rare in people below the age of 25. We used epidemiologic inputs (Table 14) to determine the target population and predicted changes in the target population over the budget impact time horizon.
Table 14:
Ontario Population and Estimated Prevalence of Venous Leg Ulcers
| Year | ||||||
|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2022 | Reference | |
| Ontario population ≥ 25 y | 10,338,325 | 10,515,459 | 10,683,585 | 10,836,972 | 10,982,651 | Ministry of Finance59 |
| Prevalence of active lower limb ulcers | 0.0018 | 0.0018 | 0.0018 | 0.0018 | 0.0018 | Petherick et al11 |
| Proportion of lower limb ulcers that are venous leg ulcers | 0.36 | 0.36 | 0.36 | 0.36 | 0.36 | Forssgren & Nelzen10 |
| People with active venous leg ulcers | 6,699 | 6,814 | 6,923 | 7,022 | 7,117 | Calculation |
| Annual healing rate | 0.92 | 0.92 | 0.92 | 0.92 | 0.92 | Pham et al40 |
| New patients with healed venous leg ulcer eligible for stockings | 4,622 | 4,702 | 4,777 | 4,845 | 4,911 | Calculation |
| New patients ≥ 25 y with healed venous leg ulcers who are eligible for stockings (adding those with previously healed leg ulcers, n = 13,398 in 1st year) | 19,561 | 6,269 | 6,369 | 6,461 | 6,547 | Calculation |
| Cumulative number of people ≥ 25 y who are eligible for stockings | 19,561 | 28,530 | 32,199 | 38,660 | 45,207 | Calculation |
| Cumulative number of people ≥ 65 y who are eligible for stockings | 14,671 | 19,373 | 24,150 | 28,995 | 33,906 | Calculationa |
Assumes 75% of venous leg ulcer patients are ≥ 65 years of age.9
Based on a prevalence study from Ontario, we estimated the number of people with lower limb ulcers to be 1.8 per 1,000 people over 25 years old.9,60 Due to the short healing time and lack of Ontario incidence data, we used this prevalence to estimate incidence over the remaining 4 years. Our approach is consistent with Margolis et al,61 who found that the incidence and prevalence of venous leg ulcers was similar in the United Kingdom over the 8-year study period. Finally, we assumed that only a proportion (0.36) of these ulcers would be venous leg ulcers, based on a large (N = 8,070) study conducted in Sweden.10
We were interested in costing compression stockings for those with healed venous leg ulcers. To isolate this figure, we calculated the number of people who had active ulcers that healed during the time horizon of our analysis plus the number of people who had ulcers that already healed before the first year of the budget impact analysis. Based on results from the Canadian Bandaging Trial,40 we assumed that 92% of ulcers heal within 1 year. Therefore, each year, 92% of people who had an active venous leg ulcer would be eligible for prevention with compression stockings. For the first year of our budget impact analysis, we also took into consideration individuals with a previously healed ulcer. According to Forssgren and Nelzen,10 the ratio of previous leg ulcers to active leg ulcers is 2:1. Assuming this ratio holds for venous leg ulcers, we calculated the number of individuals with a previously healed ulcer as two times the total number of active ulcers in the first year.
The cumulative number of people25 years of age or older and eligible for compression stockings is presented in Table 14. In addition, we present the total number of people 65 years of age or older and eligible for compression stockings. The latter population was used for our scenario analysis.
Uptake and Expected Number of People Using Compression Stockings
We assumed, based on the discussions with a compression stocking manufacturer (Bonnie Phillips, BSN Medical, written communication, Feb 23, 2018), that 20% of people who have previously had a venous leg ulcer have used compression stockings to prevent ulcer recurrence. We assume these patients pay out-of-pocket or through private insurance. With public funding, we assume this uptake would increase to 50% over 5 years (Table 15). In our reference case analysis, we assumed that the rate of increase would be lower in the first years (5%), increasing to 10% by the fifth year. The uptake rates and resulting number of people using compression stockings are presented in Table 15.
Table 15:
Uptake and Expected Number of People Using Compression Stockings to Prevent Ulcer Recurrence
| Year | |||||
|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2022 | |
| Total annual people eligible for stockings | 19,561 | 28,530 | 32,199 | 38,660 | 45,207 |
| New people eligible for stockings | 19,561 | 6,269 | 6,369 | 6,461 | 6,547 |
| Current scenario: compression stockings uptake, not publicly funded | |||||
| Proportion of people with compression stockings | 0.20 | 0.20 | 0.20 | 0.20 | 0.20 |
| Cumulative number of people with compression stockings | 3,912 | 5,166 | 6,440 | 7,732 | 9,041 |
| New scenario: compression stockings uptake, publicly funded | |||||
| Proportion of people with compression stockings | 0.25 | 0.30 | 0.35 | 0.40 | 0.50 |
| Cumulative number of people with compression stockings | 4,890 | 7,749 | 11,270 | 15,464 | 22,604 |
Canadian Costs
Costs were derived from our primary economic evaluation and include the cost of stockings, visits with health care professionals, and treatment for recurrent and infected ulcers. Based on direct medical cost estimates obtained from our model (deterministic cost–utility analysis without discounting), we calculated the average annual costs per patient over 5 years (Table 16). In the current scenario, we estimate the costs among those with and without compression stockings. The system has lower direct medical costs from people using compression stockings because compression led to fewer episodes of treatment from recurrence, while the patients paid for the compression stockings out-of-pocket or though insurance.
Table 16:
Estimated Annual Per-Patient Costs, Reference Case Analysis
| Per-Person Costs, $a | |||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Current scenario: no public funding for stockings | |||||
| Cost without compression stockings (80% of population) | 165 | 213 | 216 | 214 | 211 |
| Cost with compression stockings (20% of population) | 110 | 134 | 136 | 136 | 135 |
| New scenario: public funding for stockings | |||||
| Cost with compression stockings | 315 | 328 | 323 | 316 | 308 |
All costs are in 2018 Canadian dollars.
In both the current and new scenarios, the costs consider nonadherence to prescribed compression hosiery. We assumed all costs from our economic model, based on those 65 years or older, were applicable to those under 65 years old.
Analysis
We calculated the net budget impact by estimating the difference between the new scenario total costs and the current scenario total costs. Total costs were calculated by multiplying the expected number of patients by the per-person costs over time. We conducted a reference case scenario, using the inputs described above and several scenario analyses as described below.
Scenario 1: People65 Years of Age or Older With Venous Leg Ulcers
People 65 years and older with venous leg ulcers. This decreased our target population by 25% (Table 14).
Scenario 2: Greater Initial Uptake and Ongoing Uptake Rate
An initial uptake rate of 50% in year 1 that increases by 6% each year to a total uptake rate of 80% at the end of 5 years.
Scenario 3: Greater Use of Total Health Care Resources by Users of Compression Stockings
For this scenario, we assumed people receiving compression stockings have greater resource use than people not receiving compression stockings. We assumed people with compression stockings have one additional physician or nursing visit. The per-patient costs for this scenario are presented in Table 17.
Table 17:
Estimated Annual Per-Patient Costs, Scenario Analyses
| Per-Person Costs, $a | |||||
|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
| Scenario 3: greater use of total health care resources by users of compression stockings | 436 | 446 | 440 | 431 | 422 |
| Scenario 4: 25% of stocking cost is paid by the patient | 261 | 277 | 274 | 269 | 263 |
| Scenario 5: Cost of compression stockings only | 204 | 194 | 186 | 180 | 173 |
| Scenario 6: Nonadherent patients do not wear any stockings | 311 | 319 | 310 | 300 | 290 |
All costs in 2018 Canadian dollars.
Scenario 4: 25% of Stocking Cost Is Paid by the Patient
Patients pay 25% of the cost of compression stockings. This scenario can also be used to calculate the net budget impact for a device cost reduction of 25%. The per-patient costs for this scenario are presented in Table 17.
Scenario 5: Cost of Compression Stockings Only
Only the average annual cost of compression stockings is included. We did not include the cost of visits with health care professionals or other treatment costs. This scenario considered different compression pressures and nonadherence as described in our primary economic evaluation. The average annual costs for this scenario are presented in Table 17.
Scenario 6: Nonadherent Patients Do Not Wear Any Stockings
We assumed all nonadherent patients do not wear compression stockings. The per-patient costs for this scenario are presented in Table 17.
Results
Reference Case
The budget impact of publicly funding compression stockings would range from $0.95 million to $3.19 million per year over the next 5 years (Table 18).
Table 18:
Net Budget Impact of Publicly Funding Compression Stockings in Ontario
| Budget Impacta | |||||
|---|---|---|---|---|---|
| Funding Strategy | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Public funding of stockings | 3,955,064 | 6,141,168 | 7,919,088 | 9,715,829 | 11,817,423 |
| No public funding of stockings | 3,007,201 | 4,820,782 | 6,126,152 | 7,380,741 | 8,625,511 |
| Net Budget Impact | 947,862 | 1,320,386 | 1,792,936 | 2,335,088 | 3,191,913 |
All costs in 2018 Canadian dollars.
Scenario Analysis
The results from our scenario analyses are presented in Table 19. The largest budget impact came when we assumed that people with compression stockings had additional physician and nursing visits (greater resource use). The smallest budget impact came when we assigned 25% of the stocking cost to the patient as a co-pay.
Table 19:
Net Budget Impact of Publicly Funding Compression Stockings in Ontario
| Budget Impacta | |||||
|---|---|---|---|---|---|
| Funding Strategy | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
| Scenario 1: People ≥ 65 years old with venous leg ulcers | |||||
| Public funding of stockings | 2,966,399 | 4,605,999 | 5,939,443 | 7,287,000 | 8,863,199 |
| No public funding of stockings | 2,255,478 | 3,615,685 | 4,594,714 | 5,535,655 | 6,469,231 |
| Net Budget Impact | 710,921 | 990,314 | 1,344,729 | 1,751,345 | 2,393,968 |
| Scenario 2: Greater initial uptake and ongoing uptake rate | |||||
| Public funding of stockings | 4,261,068 | 6,631,218 | 8,485,839 | 10,329,178 | 12,375,665 |
| No public funding of stockings | 3,007,201 | 4,820,782 | 6,126,152 | 7,380,741 | 8,625,511 |
| Net Budget Impact | 1,253,866 | 1,810,436 | 2,359,687 | 2,948,437 | 3,750,155 |
| Scenario 3: Greater use of total health care resources by users of compression stockings | |||||
| Public funding of stockings | 4,547,981 | 7,066,288 | 9,256,605 | 11,538,476 | 14,476,218 |
| No public funding of stockings | 3,007,201 | 4,820,782 | 6,126,152 | 7,380,741 | 8,625,511 |
| Net Budget Impact | 1,540,779 | 2,245,506 | 3,130,453 | 4,157,735 | 5,850,708 |
| Scenario 4: 25% of stocking cost is paid by the patient | |||||
| Public funding of stockings | 3,692,174 | 5,739,545 | 7,345,562 | 8,942,711 | 10,692,839 |
| No public funding of stockings | 3,007,201 | 4,820,782 | 6,126,152 | 7,380,741 | 8,625,511 |
| Net Budget Impact | 684,973 | 918,763 | 1,219,410 | 1,561,970 | 2,067,329 |
| Scenario 5: Cost of compression stockings only | |||||
| Public funding of stockings | 998,387 | 1,529,924 | 2,183,057 | 2,948,626 | 4,285,305 |
| No public funding of stockings | 0 | 0 | 0 | 0 | 0 |
| Net Budget Impact | 998,387 | 1,529,924 | 2,183,057 | 2,948,626 | 4,285,305 |
| Scenario 6: Nonadherent patients do not wear any stockings | |||||
| Public funding of stockings | 3,936,690 | 6,087,875 | 7,817,716 | 9,554,804 | 11,573,385 |
| No public funding of stockings | 3,007,201 | 4,820,782 | 6,126,152 | 7,380,741 | 8,625,511 |
| Net Budget Impact | 929,489 | 1,267,093 | 1,691,564 | 2,174,063 | 2,947,875 |
All costs in 2018 Canadian dollars.
Discussion
We conducted a model-based budget impact analysis to examine the cost of publicly funding compression stockings in Ontario. Funding compression stockings over the next 5 years would cost the province between $0.95 million and $3.19 million annually in people with a healed venous leg ulcer. Although the clinical evidence and costs used in this analysis were derived from an older population, we included all patients in the budget impact analysis. We did this to estimate the total cost of treating the entire eligible population in Ontario. The budget impact decreases slightly when only people over 65 were considered.
When the analysis focused solely on the cost of stockings, the budget impact ranged from $1 million to $4.29 million per year. This does not include possible cost offsets such as reduced treatment costs for recurred and infected ulcers.
Our analysis has several strengths. We used model-based costs that take into consideration disease history, nonadherence, Ontario treatment patterns, and Ontario costs. We examined different scenarios to estimate the budget impact given varying population sizes, costs, resource use, and uptake.
Our analysis also has some limitations. First, we were unable to find the current uptake rate of compression stockings in the published literature or in administrative data. People who currently use compression stockings likely pay for them out-of-pocket or through private insurance. Based on the available evidence, we estimated that the current uptake rate is 20% and that it will increase if compression stockings are publicly funded. The rate of increased uptake is also unclear and may depend on the mechanism through which stockings are funded. However, we preformed sensitivity analyses to look at different initial and ongoing uptake rates. Second, our analysis incorporates nonadherence rates obtained from an RCT27 that may underestimate real-world adherence. We examined an additional nonadherence scenario in our sensitivity analysis. Third, we obtained compression stocking costs from an online vendor,51 which might not reflect the actual cost of stockings to the Ministry of Health and Long-Term Care. Our budget impact analysis results were sensitive to both cost and uptake parameters. Finally, we used Ontario prevalence data to predict the number of people with healed venous leg ulcers over time.11 Due to the short healing time of venous leg ulcers (less than a year), the incidence of ulcers could be higher than prevalence. However, we did not find an estimate of Ontario incidence in the literature. We also did not find other published budget impact analyses on compression stockings to compare our findings.
Conclusions
We estimate that the additional cost to provide public funding for compression stockings to people with a healed venous leg ulcer would range from $0.95 million to $3.19 million per year over the next 5 years. If stockings were funded only for people 65 years of age and older, the required funding would be lower, ranging from $0.71 million to $2.39 million per year over the next 5 years.
PATIENT PREFERENCES AND VALUES
Objective
The objective of this analysis was to explore the underlying values, needs, impacts, and preferences of those who have lived experience with chronic venous insufficiency. The treatment focus was on compression stockings versus no compression stockings to prevent the recurrence of healed venous leg ulcers.
Background
Patient, caregiver, and public engagement provides a unique source of information about people's experiences of a health condition and the health technologies or interventions used to manage or treat that health condition. This information includes the impact of the condition and its treatment on the patient, the patient's family and other caregivers, and the patient's personal environment. Engagement also provides insights into how a health condition is managed by the province's health system.
Information shared by people with lived experience can also identify gaps or limitations in published research (sometimes typical outcome measures do not reflect what is important to those with lived experience).62–64 Additionally, lived experience can provide information and perspectives on the ethical and social values implications of health technologies or interventions.
Because the needs, priorities, preferences, and values of those with lived experience in Ontario are not often adequately explored in published literature, we contact and speak directly with people who live with a given health condition, including those who may have experience with the intervention we are exploring.
Chronic venous insufficiency has significant impact on individuals and their families, and it can substantially affect their quality of life. It is estimated that more than 5,000 people in Ontario have an active venous leg ulcer due to chronic venous insufficiency. Chronic venous leg ulcers disproportionately affect the senior population (≥ 65 years of age)5 and require daily management.
We spoke with a range of people living with chronic venous insufficiency, including those who recently began using compression stockings and those who have been using compression stockings for many years. Gaining an understanding of the day-to-day experience of managing chronic venous insufficiency, including people's experience with compression stockings, helps us assess the potential value of this technology from the perspective of patients and caregivers.
Methods
Engagement Plan
The engagement plan for this health technology assessment focused on examining the experiences of people with chronic venous insufficiency and those of their caregivers, including their experiences with compression stockings. We engaged people via phone interviews.
We used a qualitative interview, as this method of engagement allowed us to explore the experiences of people with chronic venous insufficiency, as well as those of their families and caregivers. Our main task was to understand what people told us and to gain an understanding of the story behind their experiences.65 The sensitive nature of exploring people's experiences of a health condition and their quality of life are other factors that supported our choice of an interview methodology.
Participant Outreach
We used an approach called purposive sampling,66–69 which involves actively reaching out to patients, families, and caregivers with direct experience of the health condition and health technology or intervention being reviewed. We approached 55 organizations and health clinics involved in the care or coordination or support of persons with chronic venous insufficiency to spread the word about this engagement opportunity.
Inclusion Criteria
We sought patients and caregivers who have been actively managing chronic venous insufficiency through a treatment program that includes using compression stockings to prevent the recurrence of healed venous leg ulcers.
Exclusion Criteria
We did not set specific exclusion criteria.
Participants
We conducted interviews over the telephone with 14 individuals. Those interviewed included adults with chronic venous insufficiency and caregivers of people with chronic venous insufficiency.
We spoke with people from Hamilton, Windsor, and the Greater Toronto Area who had direct experience with compression stockings. Individuals interviewed had been using compression stockings for a varied period ranging from 2 weeks to over 20 years. Many had also experimented with different kinds of compression therapies, including compression bandages. Despite extensive engagement efforts, 8 of the 14 people interviewed shared the same health care provider and all reside in a similar region of Ontario. Consequently, there may be selection bias in the results reported.
Approach
At the beginning of the interview, we explained the role of Health Quality Ontario, the purpose of the health technology assessment, the risks of participation, and how participants' personal health information would be protected. We gave this information to participants both verbally and in a printed letter of information. See Appendix 5 for our letter of information. We obtained participants' verbal consent before starting the interview. With participants' consent, we audio-recorded and then transcribed the interviews.
Interviews lasted approximately 20 to 40 minutes. Interviews were loosely structured and consisted of a series of open-ended questions. Questions were based on a list developed by the Health Technology Assessment International Interest Group on Patient and Citizen Involvement in Health Technology Assessment.70 Questions focused on the impact of chronic venous insufficiency on patients' and families' quality of life, their experiences with treatment options, and their perceptions of the benefits or limitations of using compression stockings to manage the recurrence of venous leg ulcers. See Appendix 6 for our interview guide.
Data Extraction and Analysis
We used a modified version of a grounded-theory methodology to analyze interview transcripts. The grounded-theory approach allowed us to organize and compare information on experiences across participants. This method consists of a repetitive process of obtaining, documenting, and analyzing responses while simultaneously collecting, analyzing, and comparing information.71,72 We used the qualitative data analysis software program NVivo (QSR International, Doncaster, Victoria, Australia) to identify and interpret patterns in interview data. The patterns we identified then allowed us to highlight the impact of chronic venous insufficiency and compression stockings on the patients, family members, and caregivers we interviewed.
Results
Lived Experience of People With Chronic Venous Insufficiency
Day to Day Impact of Chronic Venous Insufficiency
The people we interviewed commonly reported that chronic venous insufficiency had an overwhelming impact on their daily lives. People with chronic venous insufficiency and caregivers for people with chronic venous insufficiency emphasized the daily burden of managing their condition. Most of those interviewed referred to their quality of life in terms of the significant challenges they faced and changes that needed to be made to manage their chronic venous insufficiency. This impact fell into two categories: social and emotional.
Social Impact
Many interviewees spoke of their limited ability to conduct day-to-day activities as a result of their condition. Sometimes they were unable to work. Most participants also reported that they had other diseases that added to their difficulties in managing their health. Despite their chronic conditions, many participants expressed a desire to continue their daily activities.
I had to go to the nurse to bathe my legs and put the stockings on. But I can't walk that far, so they had to come to me. They started to send the nurses everyday. For almost a year, this thing was [on my ulcers]…. I couldn't walk with [ulcers] from my left toe up to the knees. It took a year to heal.
I did work at one time, but I haven't worked because my legs have been really bad. I have fibromyalgia, restless legs, diabetic neuropathy…. Right now, I can't work because my legs are really bad, and my hips are bad, and my back is bad. But I still go out and walk. I try to walk every day. I try to do my stuff. I go into the grocery store. But it hurts all the time.
Emotional Impact
Most individuals reported on the emotional impact of chronic venous insufficiency and resulting venous leg ulcers for themselves and their loved ones. Many of them expressed the pain and frustration they felt when they had active venous leg ulcers.
It's hard to change clothes. Like, those stockings don't slide down the pant legs too well. So I'm spending most of my life in pyjamas.
I didn't bring on this sickness. I didn't do this to myself. I would appreciate some help…. If I can get this [ulcer] healed up, then get knee surgery done, get hip surgery done, snap on my compression stockings, and live a normal life. I can stand in the shower and take a shower like a normal human being would do it. That is what I would like for myself.
One caregiver described the experience of caring for a person with venous leg ulcer.
It breaks my heart to see them when they are full blown because they are so painful. It is heartbreaking to see him in the amount of pain he is in.
The fear of venous leg ulcer recurrence pushed some participants to continue using compression stockings. They expressed their desire to heal the ulcers as quickly as possible to return to normal day-to-day activities.
After about two and a half years, the wounds started to close up. There is a real connection between the compression helping the wound care. But it was a long slog…. Most of the ulcers healed. What we have to do now is, every day we watch the legs. We are into prevention now because we know that if we don't treat them [blisters] right away, they will develop into ulcers. So, we have all become pretty aware of danger areas. Anything that is like a water blister, anything that breaks, anything that looks red or whatever, gets treated right away…. We really realize that we have to catch that in the bud.
I would never want the [ulcers] I had before to come back…. I went to the doctor, and I told him that I have this wicked, wicked thing. It was on my toe all the way to my knees.
Use of Compression Stockings
Despite the burden of maintaining and changing the stockings, most participants reported that compression stockings improved their condition, and consequently their quality of life. Overall, participants focused on the medical benefits of using compression stockings.
Medical Benefits
Most people with chronic venous insufficiency reported that they perceived added medical benefits of using compression stockings to reduce leg swelling and prevent the recurrence of venous leg ulcers.
If I go two days without stockings while my compression stockings are drying, then my legs will swell…. Compression stockings have been a godsend.
Caregivers also reported that compression stockings were important for improving quality of life.
For him, they are an absolute requirement. Without compression, he will always have ulcers on his legs.
The problem that he still has is, if he doesn't wear the compression then he ends up breaking out in these ulcers on his ankles…. He often would end up going for extended periods of time with these ulcerated lesions on his ankles. At one point we were told he was going to have to have his legs amputated.
He got [ulcers] because there was not enough leg movement … Now the ulcers have healed and he is using compression stockings to prevent the recurrence of them…. He had to wear [compression stockings] because he would get into trouble if the swelling didn't go down.
Some people also mentioned different types of compression therapies that were prescribed to manage their chronic venous insufficiency, including compression wraps and Velcro compression stockings. Usually, these other compression therapies were prescribed because compression stockings were not able to improve the symptoms of the chronic venous insufficiency (primarily leg swelling).
I started using compression socks about 20 years ago, but one leg still swelled. Then I got another wound and they told me to get new [compression stockings]. I was using those, but now they have given me the compression wraps. They seem to be working better.
Barriers to Using Compression Stockings
Although patients reported improvements to their condition as a result of compression stockings, they also reported significant barriers to using compression stockings on a regular basis. The descriptions of barriers to use fell into two major categories: difficulty using the stockings and financial burden.
Difficulties in Using Compression Stockings
Almost all the people we interviewed reported that the greatest barrier to using compression stockings was the difficulty in putting them on. Many people needed help to put on the compression stockings and some mentioned using rubber gloves to ease the process.
You have to have fingers and hands that are strong like a wrestler because you have to stretch to pull them on. It's a real workout. I had a real struggle.
I've had to have help just recently. My wife has been helping me because I had the IV in my arm and I was afraid too much pressure on it would blow the line…. Normally, I don't need help putting them on at all. I can do it myself…. I remember when I first started wearing them and not being used to it, I was just like, “Oh my God, I have to have a shower after putting them on!” because you just break into a sweat…. They're really hard to put on when they're brand new.
Some caregivers also reported difficulty with the physical demands of using compression stockings.
It is really hard to get the stockings on. He has neuropathy in his hands, so I am helping him to put them on. I just have to wear rubber gloves.
Many individuals also admitted that they were not using the compression stockings as directed by their health care providers because they were uncomfortable, especially in the summer. In some cases, these difficulties led people to stop using the compression stockings altogether.
I remember when I took them [compression stockings] home. My wife and I struggled to get them on, which I understand is very common, getting them on for the first couple of times until you have a process to do it…. It took about half an hour to get them on. I was very frustrated…. I'm embarrassed to say I stopped using them after two weeks. It was too much trouble.
I don't wear them [compression stockings] in my home. It's only when I am going out, because it takes me 10 to 15 minutes to put them on … I was telling the nurse that if I have to wear these things in the summer, Lord have mercy! In the summer, they're so hot. I like to walk in the summer because I don't drive…. Maybe I will wear them [compression stockings] every other day. I don't know … it just gets so hot and feels very uncomfortable. If you're in a hurry to put these things [compression stockings] on, you'd never put them on because it's so hard.
I don't wear it [compression stockings] all the time, but I wear it when I need it. I don't know, I just seem to find certain times of the year are better than others. I guess the heat, the hot weather in the summertime seems to make it worse.
Several individuals also discussed the extensive washing process that had to be completed every night to keep the compression stockings intact for longer periods of time. But other people felt that the washing process made the stockings wear out more quickly.
Because he is in a long-term care facility, we have to make sure that it [compression stockings] don't go through the commercial washers and dryers. I have to make sure that they are brought home and washed by hand and hanged to dry. A couple of times through industrial washer and dryer and these will not be good. I have to get them cleaned at least two to three times a week…. It's been frustrating.
Another person with the condition agreed.
After about a month of wearing them [compression stockings] or after washing them, I find that they tend to fall apart. So, I don't know what the deal is with that. I mean, maybe I'm the only person who has that issue, but I've been wearing them for a long time.
Many of the people who consistently used compression stockings as recommended were able to do so because they had extra support and did not have put on the compression stockings themselves. This added home care support was a significant facilitator to using compression stockings on a regular basis.
Every morning, I have a PSW, a personal support worker, who comes in…. They put them [the compression stockings] on me and then then later at night take them off. They wash them and hang them for me.
Financial Barriers
Several participants did not have private insurance or qualify for disability insurance and had to pay out-of-pocket for their compression stockings. Individuals who purchased compression stockings out-of-pocket consistently cited the financial burden this had on their quality of life and on their future.
I don't care about the cost anymore. He has to have what he needs. If that means that I'm paying for it, I don't care … We had to get him more stockings in 2017, but we didn't have coverage. He was wearing some of the older stockings and some of the newer ones. We have to switch it up until we can get another prescription and go back…. The total cost was $400 for two pairs of stockings…. We are not rich, but as his power of attorney, I make the decisions as to what is important and I have decided that I don't care what it costs, he needs this.
We've been on pension for 20 years. It's tough to throw out $200, but if the doctor says you need it or they're going to amputate your leg, what are you going to do? You're going to buy the damn socks, right?
Some people with chronic venous insufficiency spoke about the compromises they made to afford compression stockings, such as extending their use beyond the recommended time; that is, after the compression stockings wore out and their level of elasticity significantly decreased.
I just can't afford to put $200 down on something that's only going to last me three months…. So, unfortunately, I don't know if it's just me, but people end up wearing them maybe twice as long as they should because they're not cheap and they wear out fast.
I haven't worked for about 6 years now, so it is a financial burden. You do without something else. I finally applied for disability and they said they were going to give it to me. I just did without it until now. I have five more years to do the disability because then I'll be 65, and then I'll go on old age pension.
Some of those interviewed expressed their gratitude that they had private insurance to purchase compression stockings regularly.
I think we are very fortunate for the health benefits that my husband has through his employer. We are probably in a better place than most people. But there are probably so many people who don't have this advantage and they are being seriously disadvantaged.
Discussion
Extensive outreach for this HTA yielded interviews with 14 patients and caregivers in Southern Ontario. We interviewed many individuals with chronic venous insufficiency who had a history of venous leg ulcers. Adults and caregivers who had direct experience using compression stockings to manage their chronic venous insufficiency were able to compare it with care that does not include compression stockings.
Those interviewed were supportive of compression stockings to prevent the recurrence of venous leg ulcers. However, almost all participants complained about the difficulty of putting on compression stockings and the challenges of wearing them during hot summer months. Some people discontinued using compression stockings due to the daily frustration associated with the time and energy required to put on the stockings every morning. Personal or nursing support offered through home care services was a significant facilitator to using compression stockings as recommended. The financial burden of buying prescription-grade stockings without private insurance or other financial assistance was also cited as a significant barrier.
Conclusions
People with chronic venous insufficiency as well as caregivers reported some improvements as a result of wearing compression stockings. Many of those interviewed felt that compression stockings provided medical benefits by preventing the recurrence of venous leg ulcers and reducing leg swelling.
The daily struggle of putting on the compression stockings was perceived as the greatest barrier to more widespread and regular use. The high cost of compression stockings that must be replaced every few months was also a concern.
CONCLUSIONS OF THE HEALTH TECHNOLOGY ASSESSMENT
The available evidence shows that, compared with usual care, compression stockings are effective in preventing venous leg ulcer recurrence and likely to be cost-effective. In people with a healed venous leg ulcer, wearing a compression stocking helps to reduce the risk of recurrence by half (GRADE: Moderate).
Our economic evaluation suggests that compression stockings are likely cost-effective compared with no compression stockings in preventing venous leg ulcers. We estimated that the additional cost to provide public funding for compression stockings to people with a healed venous leg ulcer would range from $0.95 million to $3.19 million per year over the next 5 years. If stockings were funded only for people 65 years of age and older, the required funding would be lower, ranging from $0.71 million to $2.39 million per year over the next 5 years.
People interviewed reported benefits through the prevention of ulcer recurrence and reduction of leg swelling, despite the daily struggle to put on compression stockings. The difficulty in using compression stockings was perceived as the greatest barrier to more widespread and regular use. The high cost of regular replacement of stockings is also seen as a barrier to use by the people we interviewed.
Acknowledgments
The medical editor was Timothy Maguire. Others involved in the development and production of this report were Merissa Mohamed, Kellee Kaulback, Kathryn Schwarz, Kara Cowan, Claude Soulodre, Andrée Mitchell, Sarah McDowell, Vivian Ng, Amy Lang, Nancy Sikich, and Irfan Dhalla.
We are grateful to Afsaneh Alavi, Alexandria Crowe, Ann-Marie McLaren, David Keast, Janice Hon, Kali Barrett, Laura Teague, Mariam Botros, Patricia Coutts, and Ruth Thompson for their input into the development of this report.
The statements, conclusions, and views expressed in this report do not necessarily represent the views of the consulted experts.
ABBREVIATIONS
- GRADE
Grading of Recommendations Assessment, Development, and Evaluation
- ICER
Incremental cost-effectiveness ratio
- QALY
Quality-adjusted life-year
- RCT
Randomized controlled trial
- ROBINS-I
Risk of Bias in Non-randomized Studies of Intervention
GLOSSARY
- Budget impact analysis
A technique to estimate the financial impact of a planned action over a specified time period by calculating the costs and savings of different options.
- Cost–utility analysis
A type of analysis that estimates the value for money of an intervention by weighing the cost of the intervention against the improvements in length of life and quality of life. The result is expressed as a dollar amount per “quality-adjusted life-year” or QALY.
- Discount rate
Health economists assume that value is affected by the timing of when a benefit is received or a cost is incurred (specifically, present benefits and costs are more valuable than future benefits and costs). To compare different benefits and costs across different time frames, they calculate the present value by adjusting the future value by a specified percentage. For instance, a discount rate of 1.5% per year will reduce the value of benefit that won't be realized for a year by 1.5%. A benefit or cost that won't be realized for two years would be adjusted by 3% (2 years × 1.5% per year).
- Incremental cost-effectiveness ratio (ICER)
Determines “a unit of benefit” for an intervention by dividing the incremental cost by the effectiveness. The incremental cost is the difference between the cost of the treatment under study and an alternative treatment. The effectiveness is usually measured as additional years of life or as “quality-adjusted life years.”
- Markov model
A type of modelling that measures the health state of a patient over the course of treatment. A patient may stay in one health state or move from one health state to another, depending on the effect of the treatment and the progression of the disease.
- Monte Carlo simulation
Determines the uncertainty in an economic model by running many trials of the model. In each trial, random numbers are assigned wherever values are uncertain to see how the model result changes.
- Probabilistic sensitivity analysis
A type of analysis where the value of one or more unknown factors is estimated through the use of a technique that determines the most likely value or range of values for that factor. For instance, the Monte Carlo simulation will run a scenario many times using randomly assigned numbers where the value of a particular factor is unknown. The simulation indicates which outcomes are most common, and therefore most probable.
- Quality-adjusted life-year (QALY)
A measurement that takes into account both the number of years gained by a patient from a procedure and the quality of those extra years (ability to function, freedom from pain, etc.). The QALY is commonly used as an outcome measure in cost–utility analyses.
- Utility
The perceived benefit (value) placed on a treatment by a person or by society.
APPENDICES
Appendix 1: Literature Search Strategies
Clinical Evidence Search
Databases searched: All Ovid MEDLINE, Embase, Cochrane Database of Systematic Reviews, CRD Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, NHS Economic Evaluation Database, CINAHL
Ovid
Database: EBM Reviews - Cochrane Central Register of Controlled Trials <November 2017>, EBM Reviews - Cochrane Database of Systematic Reviews <2005 to November 16, 2017>, EBM Reviews - Health Technology Assessment <4th Quarter 2016>, EBM Reviews – NHS Economic Evaluation Database <1st Quarter 2016>, Embase <1980 to 2017 Week 47>, All Ovid MEDLINE(R) <1946 to Present>
Search Strategy:
-
1
Varicose Ulcer/ (12064)
-
2
(((venous or varicose or varicosis or stasis) adj3 ulcer∗) or (venous adj disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs).ti,ab,kf. (17783)
-
3
Venous Insufficiency/ (10854)
-
4
(((venous or vein) adj2 insufficienc∗) or CVI).ti,ab,kf. (15912)
-
5
Postphlebitic Syndrome/ (4043)
-
6
((postphlebitic or post-phlebitic) adj2 (ulcer∗ or syndrome∗ or disease∗)).ti,ab,kf. (950)
-
7
Leg Ulcer/ (21242)
-
8
((leg∗ or lower extremit∗) adj2 ulcer∗).ti,ab,kf. (16695)
-
9
Saphenous Vein/ (29240)
-
10
(saphenous adj vein∗).ti,ab,kf. (32184)
-
11
(Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP).ti,ab,kf. (2413)
-
12
or/1–11 (100890)
-
13
exp Compression Bandages/ (4487)
-
14
((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom∗) adj3 (therap∗ or wrap∗ or stocking∗ or hosiery or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multi-layer∗ or multicomponent or multi-component)).ti,ab,kf. (22178)
-
15
(((elastic or nonelastic or inelastic) adj3 compress∗) or elastocompress∗ or elasto-compress∗).ti,ab,kf. (2725)
-
16
or/13–15 (26028)
-
17
12 and 16 (5181)
-
18
Case Reports/ or Comment.pt. or Editorial.pt. or Letter.pt. or Congresses.pt. (5102335)
-
19
17 not 18 (4915)
-
20
exp Animals/ not Humans/ (14965945)
-
21
19 not 20 (4022)
-
22
limit 21 to english language [Limit not valid in CDSR; records were retained] (3101)
-
23
22 use ppez,coch,cctr,clhta,cleed (1864)
-
24
leg varicosis/ (1416)
-
25
(((venous or varicose or varicosis or stasis) adj3 ulcer∗) or (venous adj disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs).tw,kw. (17863)
-
26
exp vein insufficiency/ (9223)
-
27
(((venous or vein) adj2 insufficienc∗) or CVI).tw,kw. (16390)
-
28
((postphlebitic or post-phlebitic) adj2 (ulcer∗ or syndrome∗ or disease∗)).tw,kw. (993)
-
29
leg ulcer/ (21242)
-
30
((leg∗ or lower extremit∗) adj2 ulcer∗).tw,kw. (16626)
-
31
saphenous vein/ (29240)
-
32
(saphenous adj vein∗).tw,kw. (32328)
-
33
(Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP).tw,kw. (2450)
-
34
or/24–33 (95031)
-
35
exp compression therapy/ (7894)
-
36
compression garment/ (2150)
-
37
compression stocking/ (3615)
-
38
((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom∗) adj3 (therap∗ or wrap∗ or stocking∗ or hosiery or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multi-layer∗ or multicomponent or multi-component)).tw,kw,dv. (22719)
-
39
(((elastic or nonelastic or inelastic) adj3 compress∗) or elastocompress∗ or elasto-compress∗).tw,kw,dv. (2783)
-
40
or/35–39 (32110)
-
41
34 and 40 (6152)
-
42
Case Report/ or Comment/ or Editorial/ or Letter/ or conference abstract.pt. (9702718)
-
43
41 not 42 (5226)
-
44
(exp animal/ or nonhuman/) not exp human/ (10665690)
-
45
43 not 44 (5221)
-
46
limit 43 to english language [Limit not valid in CDSR; records were retained] (4091)
-
47
46 use emez (2313)
-
48
23 or 47 (4177)
-
55
remove duplicates from 48 (2580)
CINAHL
| # | Query | Results |
|---|---|---|
| S1 | (MH “Venous Ulcer”) | 2,048 |
| S2 | (((venous or varicose or varicosis or stasis) N3 ulcer∗) or (venous N1 disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs or CVDL) | 3,599 |
| S3 | (MH “Venous Insufficiency”) | 1,175 |
| S4 | (((venous or vein) N2 insufficienc∗) or CVI) | 1,908 |
| S5 | ((postphlebitic or post-phlebitic) N2 (ulcer∗ or syndrome∗ or disease∗)) | 23 |
| S6 | (MH “Leg Ulcer”) | 2,986 |
| S7 | ((leg∗ or lower extremit∗) N2 ulcer∗) | 4,424 |
| S8 | (MH “Saphenous Vein”) | 1,144 |
| S9 | (saphenous N1 vein∗) | 1,590 |
| S10 | (Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP) | 114 |
| S11 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 | 9,042 |
| S12 | (MH “Elastic Bandages”) | 98 |
| S13 | (MH “Compression Garments”) | 1,904 |
| S14 | ((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom) N3 (therap∗ or wrap∗ or stocking∗ or hosiery or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multilayer∗ or multicomponent or multi-component)) | 5,614 |
| S15 | (((elastic or nonelastic or inelastic) N3 compress∗) or elastocompress∗ or elasto-compress∗) | 172 |
| S16 | S12 OR S13 OR S14 OR S15 | 5,684 |
| S17 | S11 AND S16 | 1,520 |
| S18 | PT Case Study or Commentary or Editorial or Letter or Proceedings | 406,160 |
| S19 | S17 NOT S18 | 1,302 |
| S20 | S17 NOT S18 Limiters - English Language |
1,272 |
Economic Evidence Search
Databases searched: All Ovid MEDLINE, Embase, Cochrane Database of Systematic Reviews, CRD Health Technology Assessment Database, Cochrane Central Register of Controlled Trials, NHS Economic Evaluation Database, CINAHL
Ovid
Database: EBM Reviews - Cochrane Central Register of Controlled Trials <November 2017>, EBM Reviews - Cochrane Database of Systematic Reviews <2005 to November 22, 2017>, EBM Reviews - Health Technology Assessment <4th Quarter 2016>, EBM Reviews - NHS Economic Evaluation Database <1st Quarter 2016>, Embase <1980 to 2017 Week 47>, All Ovid MEDLINE(R) <1946 to Present>
Search Strategy:
-
1
Varicose Ulcer/ (12064)
-
2
(((venous or varicose or varicosis or stasis) adj3 ulcer∗) or (venous adj disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs).ti,ab,kf. (17783)
-
3
Venous Insufficiency/ (10854)
-
4
(((venous or vein) adj2 insufficienc∗) or CVI).ti,ab,kf. (15912)
-
5
Postphlebitic Syndrome/ (4043)
-
6
((postphlebitic or post-phlebitic) adj2 (ulcer∗ or syndrome∗ or disease∗)).ti,ab,kf. (950)
-
7
Leg Ulcer/ (21242)
-
8
((leg∗ or lower extremit∗) adj2 ulcer∗).ti,ab,kf. (16694)
-
9
Saphenous Vein/ (29241)
-
10
(saphenous adj vein∗).ti,ab,kf. (32187)
-
11
(Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP).ti,ab,kf. (2413)
-
12
or/1–11 (100893)
-
13
exp Compression Bandages/ (4487)
-
14
((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom∗) adj3 (therap∗ or wrap∗ or stocking∗ or stockings or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multi-layer∗ or multicomponent or multi-component)).ti,ab,kf. (22180)
-
15
(((elastic or nonelastic or inelastic) adj3 compress∗) or elastocompress∗ or elasto-compress∗).ti,ab,kf. (2725)
-
16
or/13–15 (26030)
-
17
12 and 16 (5181)
-
18
economics/ (255188)
-
19
economics, medical/ or economics, pharmaceutical/ or exp economics, hospital/ or economics, nursing/ or economics, dental/ (796531)
-
20
economics.fs. (420227)
-
21
(econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗).ti,ab,kf. (800626)
-
22
exp “costs and cost analysis”/ (561680)
-
23
(cost or costs or costing or costly).ti. (244840)
-
24
cost effective∗.ti,ab,kf. (287366)
-
25
(cost∗ adj2 (util∗ or efficacy∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)).ab. (186736)
-
26
models, economic/ (11710)
-
27
markov chains/ or monte carlo method/ (75943)
-
28
(decision adj1 (tree∗ or analy∗ or model∗)).ti,ab,kf. (37298)
-
29
(markov or markow or monte carlo).ti,ab,kf. (119039)
-
30
quality-adjusted life years/ (35546)
-
31
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).ti,ab,kf. (61397)
-
32
((adjusted adj (quality or life)) or (willing∗ adj2 pay) or sensitivity analys∗s).ti,ab,kf. (99537)
-
33
or/18–32 (2379052)
-
34
17 and 33 (645)
-
35
34 use ppez,coch,cctr,clhta (308)
-
36
17 use cleed (4)
-
37
35 or 36 (312)
-
38
Case Reports/ or Comment.pt. or Editorial.pt. or Letter.pt. or Congresses.pt. (5102308)
-
39
37 not 38 (297)
-
40
limit 39 to english language [Limit not valid in CDSR; records were retained] (241)
-
41
leg varicosis/ (1416)
-
42
(((venous or varicose or varicosis or stasis) adj3 ulcer∗) or (venous adj disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs).tw,kw. (17862)
-
43
exp vein insufficiency/ (9223)
-
44
(((venous or vein) adj2 insufficienc∗) or CVI).tw,kw. (16388)
-
45
((postphlebitic or post-phlebitic) adj2 (ulcer∗ or syndrome∗ or disease∗)).tw,kw. (993)
-
46
leg ulcer/ (21242)
-
47
((leg∗ or lower extremit∗) adj2 ulcer∗).tw,kw. (16624)
-
48
saphenous vein/ (29241)
-
49
(saphenous adj vein∗).tw,kw. (32331)
-
50
(Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP).tw,kw. (2450)
-
51
or/41–50 (95033)
-
52
exp compression therapy/ (7894)
-
53
compression garment/ (2150)
-
54
compression stocking/ (3615)
-
55
((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom∗) adj3 (therap∗ or wrap∗ or stocking∗ or stockings or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multi-layer∗ or multicomponent or multi-component)).tw,kw,dv. (22720)
-
56
(((elastic or nonelastic or inelastic) adj3 compress∗) or elastocompress∗ or elasto-compress∗).tw,kw,dv. (2783)
-
57
or/52–56 (32111)
-
58
51 and 57 (6151)
-
59
Economics/ (255188)
-
60
Health Economics/ or Pharmacoeconomics/ or Drug Cost/ or Drug Formulary/ (130229)
-
61
Economic Aspect/ or exp Economic Evaluation/ (430210)
-
62
(econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗).tw,kw. (824998)
-
63
exp “Cost”/ (561680)
-
64
(cost or costs or costing or costly).ti. (244840)
-
65
cost effective∗.tw,kw. (298275)
-
66
(cost∗ adj2 (util∗ or efficac∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)).ab. (187880)
-
67
Monte Carlo Method/ (61295)
-
68
(decision adj1 (tree∗ or analy∗ or model∗)).tw,kw. (41013)
-
69
(markov or markow or monte carlo).tw,kw. (123996)
-
70
Quality-Adjusted Life Years/ (35546)
-
71
(QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs).tw,kw. (65159)
-
72
((adjusted adj (quality or life)) or (willing∗ adj2 pay) or sensitivity analys∗s).tw,kw. (118829)
-
73
or/59–72 (2016329)
-
74
58 and 73 (837)
-
75
74 use emez (463)
-
76
Case Report/ or Comment/ or Editorial/ or Letter/ or conference abstract.pt. (9702688)
-
77
75 not 76 (407)
-
78
limit 77 to english language [Limit not valid in CDSR; records were retained] (359)
-
86
remove duplicates from 79 (398)
CINAHL
| # | Query | Results |
|---|---|---|
| S1 | (MH “Venous Ulcer”) | 2,048 |
| S2 | (((venous or varicose or varicosis or stasis) N3 ulcer∗) or (venous N1 disease∗) or VLU or VLUs or CVLU or CVLUs or CVU or CVUs or CVDL) | 3,600 |
| S3 | (MH “Venous Insufficiency”) | 1,175 |
| S4 | (((venous or vein) N2 insufficienc∗) or CVI) | 1,908 |
| S5 | ((postphlebitic or post-phlebitic) N2 (ulcer∗ or syndrome∗ or disease∗)) | 23 |
| S6 | (MH “Leg Ulcer”) | 2,987 |
| S7 | ((leg∗ or lower extremit∗) N2 ulcer∗) | 4,426 |
| S8 | (MH “Saphenous Vein”) | 1,145 |
| S9 | (saphenous N1 vein∗) | 1,590 |
| S10 | (Clinical∗ Etiology∗ Anatomy∗ Pathophysiology or CEAP) | 114 |
| S11 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 | 9,044 |
| S12 | (MH “Elastic Bandages”) | 99 |
| S13 | (MH “Compression Garments”) | 1,905 |
| S14 | ((compress∗ or elastic or nonelastic or inelastic or elastom∗ or nonelastom∗) N3 (therap∗ or wrap∗ or stocking∗ or stockings or hose or garment∗ or sock∗ or tights or dressing∗ or system∗ or device∗ or short-stretch∗ or long-stretch∗ or four-layer∗ or three-layer∗ or two-layer∗ or bilayer∗ or bi-layer∗ or multilayer∗ or multi-layer∗ or multicomponent or multi-component)) | 5,615 |
| S15 | (((elastic or nonelastic or inelastic) N3 compress∗) or elastocompress∗ or elasto-compress∗) | 172 |
| S16 | S12 OR S13 OR S14 OR S15 | 5,686 |
| S17 | S11 AND S16 | 1,521 |
| S18 | (MH “Economics”) | 11,531 |
| S19 | (MH “Economic Aspects of Illness”) | 7,112 |
| S20 | (MH “Economic Value of Life”) | 527 |
| S21 | MH “Economics, Dental” | 110 |
| S22 | MH “Economics, Pharmaceutical” | 1,822 |
| S23 | MW “ec” | 147,132 |
| S24 | (econom∗ or price or prices or pricing or priced or discount∗ or expenditure∗ or budget∗ or pharmacoeconomic∗ or pharmaco-economic∗) | 227,877 |
| S25 | (MH “Costs and Cost Analysis+”) | 88,943 |
| S26 | TI cost∗ | 41,902 |
| S27 | (cost effective∗) | 31,150 |
| S28 | AB (cost∗ N2 (util∗ or efficacy∗ or benefit∗ or minimi∗ or analy∗ or saving∗ or estimate∗ or allocation or control or sharing or instrument∗ or technolog∗)) | 21,961 |
| S29 | (decision N1 (tree∗ or analy∗ or model∗)) | 5,654 |
| S30 | (markov or markow or monte carlo) | 3,858 |
| S31 | (MH “Quality-Adjusted Life Years”) | 3,031 |
| S32 | (QOLY or QOLYs or HRQOL or HRQOLs or QALY or QALYs or QALE or QALEs) | 7,513 |
| S33 | ((adjusted N1 (quality or life)) or (willing∗ N2 pay) or sensitivity analys?s) | 13,362 |
| S34 | S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 | 305,676 |
| S35 | S17 AND S34 | 202 |
| S36 | PT Case Study or Commentary or Editorial or Letter or Proceedings | 405,930 |
| S37 | S35 NOT S36 | 177 |
| S38 | S35 NOT S36 Limiters - English Language |
171 |
Grey Literature Search
Performed: November 8–9, 2017
Websites searched:
HTA Database Canadian Repository, Alberta Health Technologies Decision Process reviews, Canadian Agency for Drugs and Technologies in Health (CADTH), Institut national d'excellence en santé et en services sociaux (INESSS), Institute of Health Economics (IHE), McGill University Health Centre Health Technology Assessment Unit, National Institute for Health and Care Excellence (NICE), Agency for Healthcare Research and Quality (AHRQ) Evidence-based Practice Centers, Australian Government Medical Services Advisory Committee, Centers for Medicare & Medicaid Services Technology Assessments, Institute for Clinical and Economic Review, Ireland Health Information and Quality Authority Health Technology Assessments, Washington State Health Care Authority Health Technology Reviews, ClinicalTrials.gov, Tufts Cost-Effectiveness Analysis Registry, Sick Kids Paediatric Economic Database Evaluation (PEDE)
Keywords used: Compression, ulcer, ulcers, venous, varicose
Results: 10
18 clinical trials not counted in PRISMA
Appendix 2: Critical Appraisal of Clinical Evidence
Table A1:
Risk of Bias for Randomized Controlled Trials Investigating the Effectiveness of Compression Stockings
| Author, Year | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Incomplete Outcome Data | Selective Reporting | Other Bias |
|---|---|---|---|---|---|---|
| Kapp et al 201326 | No limitations | No limitations | No limitations | Limitationsa | No limitations | No limitations |
| Clarke-Moloney et al, 201225 | No limitations | No limitations | No limitationsb | No limitations | No limitations | No limitations |
| Nelson et al, 200627 | No limitations | No limitations | No limitationsb | Limitationsa | No limitations | No limitations |
| Vandongen & Stacey, 200028 | Unclear | No limitations | No limitationsb | Limitationsa | No limitations | No limitations |
High rate of nonadherence to the study or to the randomized group.
Outcomes selected for this review were objective and unlikely to be influenced by lack of blinding.
Table A2:
Risk of Bias for Non-randomized Studies Investigating the Effectiveness of Compression Stockings
| Selective Reporting | Selection of Participants | Confounding Variablesa | Classification of Interventions | Deviation From Intended Interventions | Incomplete Outcome Data | Measurement Outcomes | Selective Reporting |
|---|---|---|---|---|---|---|---|
| Samson & Showalter 199631 | No limitations | Unclear | No limitations | No limitations | No limitations | No limitations | No limitations |
| Dinn & Henry29 | No limitations | Unclear | No limitations | No limitations | No limitations | No limitations | No limitations |
| Reich-Schupke 200930 | No limitations | Unclear | No limitations | No limitations | No limitations | No limitations | No limitations |
Lack of control for confounding variables is an inherent limitation in observational studies.
Table A3:
GRADE Evidence Profile for Comparison of Compression Stockings With No Compression Stockings
| No. of Studies(Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Recurrence rate | |||||||
| 1 RCT28 | Serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕⊕ Moderate |
| Adherence rate | |||||||
| 1 RCT28 | Serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕⊕ Moderate |
Abbreviation: RCT, randomized controlled trial.
Incomplete accounting of patients.
Table A4:
GRADE Evidence Profile for Comparison of Compression Stockings With Different Levels of Pressure
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Recurrence rate | |||||||
| 3 RCTs25–27 | Serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕⊕ Moderate |
| Adherence rate | |||||||
| 3 RCTs25–27 | Serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕⊕ Moderate |
| Adverse effects | |||||||
| 1 RCT26 | Serious limitationsa | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕⊕ Moderate |
Abbreviations: RCT, randomized controlled trial.
Incomplete accounting of patients.
Table A5:
GRADE Evidence Profile for Non-randomized Studies Investigating the Effect of Patient Adherence on Outcomes, Quality of Life, and Adverse Effects
| No. of Studies (Design) | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Upgrade Considerations | Quality |
|---|---|---|---|---|---|---|---|
| Recurrence rate | |||||||
| 2 observational29,31 | No serious limitations | No serious limitations | No serious limitations | No serious limitations | Not detected | No serious limitations | ⊕⊕ Low |
| Quality of life | |||||||
| 1 observational30 | No serious limitations | No serious limitations | Serious limitationsa | No serious limitations | Not detected | No serious limitations | ⊕ Very low |
| Adverse effects | |||||||
| 1 observational30 | No serious limitations | No serious limitations | Serious limitationsa | No serious limitations | Not detected | No serious limitations | ⊕ Very low |
Population was similar but not identical to those under consideration.
Note: Absence of randomization and control for confounding, an inherent limitation of the observational studies, is factored in the last column when we graded the quality.
Appendix 3: Results of Applicability for Studies Included in Economic Literature Review
Table A6:
Assessment of the Applicability of the Study Assessing the Cost-Effectiveness of Compression Stockings
| Author, Year, Country | Is the Study Population Similar to the Question? | Are the Interventions Similar to the Question? | Is the Health Care System Studied Sufficiently Similar to Ontario? | Were the Perspectives Clearly Stated? What Were They? | Are Estimates of Relative Treatment Effect From the Best Available Source? |
|---|---|---|---|---|---|
| Korn et al, 2002,34 United States | Yes Patients with prior venous ulcers | Partially Prophylactic compression stockings plus patient education | No US health care system different from Ontario context | Yes US health care perspective | Yes |
| Author, Year, Country | Are All Future Costs and Outcomes Discounted? At What Rate? | Is the Value of Health Effects Expressed in Terms of Quality-Adjusted Life-Years? | Are Costs and Outcomes From Other Sectors Fully and Appropriately Measured and Valued? | Overall Judgement: Directly Applicable/ Partially Applicable/ Not Applicable |
|---|---|---|---|---|
| Korn et al, 2002,34 United States | Yes Both costs and outcomes are discounted at 3% | Yes | NA | Partially applicable |
Note: Response options for all items were yes, partially, no, unclear, and NA (not applicable).
Appendix 4: Primary Economic Evaluation
Table A7:
Input Parameters Used for Probabilistic Sensitivity Analysis
| Model Parameter | Mean (SE) | Distribution | Reference |
|---|---|---|---|
| Monthly probabilities and rates | |||
| Probability of nonadherence: | |||
| High pressure (25–35 mm Hg) | 0.009 (0.008) | Beta | Nelson et al, 200627 |
| Low pressure (18–24 mm Hg) | 0.005 (0.006) | Beta | Nelson et al, 200627 |
| Support (14–17 mm Hg) | 0.0005 (0.0002) | Beta | Nelson et al, 200627 |
| Probability of ulcer recurrence, compression stockings: | |||
| High pressure (25–35 mm Hg) | 0.006 (0.0065) | Beta | Nelson et al, 200627 |
| Low pressure (18–24 mm Hg) | 0.008 (0.0073) | Beta | Nelson et al, 200627 |
| Support (14–17 mm Hg) | 0.010 (0.0097) | Beta | Assumption |
| Risk of ulcer recurrence: | |||
| Compression stockings vs. no compression stockings | 2.30 (0.24) | Log-normal | Vandongen & Stacey, 200028 |
| Ulcer healing with compression bandages | 0.163 (0.0179) | Beta | Pham et al, 201240 |
| Infection rate | 0.05 (0.0358) | Beta | Carter et al, 201449 |
| Utilities | |||
| Recurred ulcer | 0.77 (0.0086) | Beta | Pham et al, 201240 |
| Healed ulcer | 0.87 (0.0055) | Beta | Pham et al, 201240 |
| Infected ulcer | 0.77 (0.0086) | Beta | Assumption |
| Costs | |||
| Healed ulcer health state, high pressure (25–35 mm Hg) | 26.1 (6.5) | Gamma | Calculation |
| Healed ulcer health state, low pressure (18–24 mm Hg) | 22.2 (5.6) | Gamma | Calculation |
| Healed ulcer health state, support (13–17 mm Hg) | 13.8 (3.5) | Gamma | Calculation |
| Healed ulcer health state, no compression stockings, $a | 5.5 (1.4) | Gamma | Calculation |
| Recurred ulcer health state,a | 128 (32.0) | Gamma | Pham et al, 201240 |
| Infected ulcer health state, $a | 222.9 (55.7) | Gamma | Calculation |
Abbreviation: SE, standard error.
All costs given in 2018 Canadian dollars.
Table A8:
Transition Probabilities of Ulcer Recurrence for People With Healed Venous Ulcers
| Author, Year | Intervention | Participants (N) | Age (% Male) | Follow-Up | Recurrence (N) | Probability of recurrence (%) | Rate (per mo) | Probability (per mo) |
|---|---|---|---|---|---|---|---|---|
| Nelson et al, 200627 | Class 2 stockings | 151 | 65 yr (59) | 5 yr | 59 | 39.1 | 0.008 | 0.008 |
| Class 3 stockings | 149 | 64 yr (66) | 5 yr | 48 | 31.8 | 0.006 | 0.006 |
Note: rmo = −(In[1 − pyr])/t; pmo = 1 − exp(−rmo) where pyr = annual probability of recurrence, t = 1/12, rmo = rate per month and pmo = monthly probability of recurrence.
Appendix 5: Call for Participation
Appendix 6: Interview Guide
Interview for Compression Therapy for Venous Insufficiency/Venous Ulcers
Intro
Explain the purpose of Health Quality Ontario, the health technology assessment process, and the purpose of the interview
History of chronic venous insufficiency—diagnosis and background (general only)
Lived Experience
Day-to-day routine
Any impact of chronic venous insufficiency on quality of life?
History of venous ulcers?
Impact on loved ones/caregivers, work, etc.?
Therapies
What current therapies/treatments are used and what is their impact?
Is accessibility to therapies/treatments an issue? (Are you able to take advantage of all potential therapies?)
What are the expectations from current therapies?
Compression Therapy
Information surrounding compression therapy?
Expectations?
Any challenges? Access? Re-use? Cost (for medical grade)? Getting prescription (for medical grade)?
Result, impact, change in quality of life (if applicable)
Recurrence of venous ulcers (if applicable)
Author contributions
This report was developed by a multidisciplinary team from Health Quality Ontario. The clinical epidemiologist was Shayan Sehatzadeh, the health economists were Sandjar Djalalov and Lindsey Falk, the patient engagement specialists were Sunita Kheterpal and David Wells, and the medical librarians were Caroline Higgins and Melissa Walter.
KEY MESSAGES
What Is This Health Technology Assessment About?
People with poor circulation in the veins of their legs sometimes develop a type of ulcer called a venous leg ulcer. This is a difficult-to-treat condition and even after successful healing, the ulcer may return. Venous leg ulcers are difficult to manage due to poor healing and high recurrence rates. Compression stockings, which provide support for the veins in the leg and help prevent blood from pooling, may be used to prevent the recurrence of healed ulcers.
This assessment looked at the effectiveness, safety, cost-effectiveness, budget impact of, and patient experiences with compression stockings for the prevention of venous leg ulcer recurrence.
What Did This Health Technology Assessment Find?
The evidence shows that ulcer recurrence rates are lower when people with a healed leg ulcer wear compression stockings. Our economic analyses show that compression stockings are likely to be cost-effective. Publicly funding compression stockings for eligible people in Ontario is estimated to cost between $0.95 million and $3.19 million per year over the next five years. People using compression stockings and caregivers of people using compression stockings reported that compression stockings not only reduced ulcer recurrence, but also reduced swelling. The high cost of medical-grade compression stockings (which need to be replaced every few months) was a concern.
Contributor Information
Health Quality Ontario:
Shayan Sehatzadeh, Sandjar Djalalov, Lindsey Falk, Sunita Kheterpal, David Wells, Caroline Higgins, and Melissa Walter
About Health Quality Ontario
Health Quality Ontario is the provincial lead on the quality of health care. We help nurses, doctors and other health care professionals working hard on the frontlines be more effective in what they do – by providing objective advice and data, and by supporting them and government in improving health care for the people of Ontario.
We focus on making health care more effective, efficient and affordable through a legislative mandate of:
Reporting to the public, organizations, government and health care providers on how the health system is performing,
Finding the best evidence of what works, and
Translating this evidence into clinical standards; recommendations to health care professionals and funders; and tools that health care providers can easily put into practice to make improvements.
Health Quality Ontario is governed by a 12-member Board of Directors with a broad range of expertise – doctors, nurses, patients and from other segments of health care – and appointed by the Minister of Health and Long-Term Care.
In everything it does, Health Quality Ontario brings together those with first-hand experience to hear their experiences and views of how to make them better. We partner with patients, residents, families and caregivers to be full participants in designing our programs and services, to ensure they are aligned to their needs and priorities. We work collaboratively with organizations across the province to encourage the spread of innovative and proven programs to support high quality care, while also saving money and eliminating redundancy. And, we work with clinicians on the frontlines to use their collective wisdom and experience to bring about positive change in areas important to Ontario – such as addressing the challenges of hallway health care and mental health.
For example, 29 Ontario hospitals participated in a pilot program last year that reduced infections due to surgery by 18% – which in turn reduces the number of patients returning to hospital after surgery and alleviating some of the challenges faced in hallway health care. This program enabled surgeons to see their surgical data and how they perform in relation to each other and to 700 other hospitals worldwide. We then helped them identify and action improvements to care. Forty-six hospitals across Ontario are now part of this program, covering 80% of hospital surgeries.
Health Quality Ontario also develops quality standards for health conditions that demonstrate unnecessary gaps and variations in care across the province, such as in major depression or schizophrenia. Quality standards are based on the best evidence and provide recommendations to government, organizations and clinicians. They also include a guide for patients to help them ask informed questions about their care.
In addition, Health Quality Ontario's health technology assessments use evidence to assess the effectiveness and value for money of new technologies and procedures, and incorporate the views and preferences of patients, to make recommendations to government on whether they should be funded.
Each year, we also help hospitals, long-term care homes, home care and primary care organizations across the system create and report on the progress of their annual Quality Improvement Plans, which is their public commitment on their priorities to improve health care quality.
Health Quality Ontario is committed to supporting the development of a quality health care system based on six fundamental dimensions: efficient, timely, safe, effective, patient-centred and equitable.
Our goal is to challenge the status quo and to focus on long-lasting pragmatic solutions that improve the health of Ontarians, enhance their experience of care, reduce health care costs, and support the well-being of health care providers. A quality health system results in Ontarians leading healthier and more productive lives, and a vibrant society in which everyone benefits.
REFERENCES
- (1).Harrison MB, Vandenkerkhof EG, Hopman WM, Graham ID, Carley ME, Nelson EA. The Canadian Bandaging Trial: evidence-informed leg ulcer care and the effectiveness of two compression technologies. BMC Nurs. 2011;10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).O'Donnell TF, Jr., Passman MA, Marston WA, Ennis WJ, Dalsing M, Kistner RL, et al. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2014;60(2 Suppl):3S–59S. [DOI] [PubMed] [Google Scholar]
- (3).Paul J. A cross-sectional study of chronic wound-related pain and itching. Ostomy Wound Manage. 2013;59(7):28–34. [PubMed] [Google Scholar]
- (4).Upton D, Andrews A. Sleep disruption in patients with chronic leg ulcers. J Wound Care. 2013;22(8):389–90, 92, 94. [DOI] [PubMed] [Google Scholar]
- (5).Nelzen O, Bergqvist D, Lindhagen A. Venous and non-venous leg ulcers: clinical history and appearance in a population study. Br J Surg. 1994;81(2):182–7. [DOI] [PubMed] [Google Scholar]
- (6).Hellstrom A, Nilsson C, Nilsson A, Fagerstrom C. Leg ulcers in older people: a national study addressing variation in diagnosis, pain and sleep disturbance. BMC Geriatr. 2016;16:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Nelson EA, Bell-Syer SE. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev. 2014;9:CD002303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Nelzen O. Prevalence of venous leg ulcer: the importance of the data collection method. Phlebolymphology. 2008; 15(4):143–50. [Google Scholar]
- (9).Harrison MB, Graham ID, Friedberg E, Lorimer K, Vandevelde-Coke S. Regional planning study. Assessing the population with leg and foot ulcers. Can Nurse. 2001;97(2):18–23. [PubMed] [Google Scholar]
- (10).Forssgren A, Nelzen O. A repeat validated population questionnaire of a defined Swedish population verifies reduction in leg ulcer prevalence over time. Acta Derm Venereol. 2015;95(6):725–9. [DOI] [PubMed] [Google Scholar]
- (11).Petherick ES, Cullum NA, Pickett KE. Investigation of the effect of deprivation on the burden and management of venous leg ulcers: a cohort study using the THIN database. PLoS One. 2013;8(3):e58948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Baker SR, Stacey MC, Jopp-McKay AG, Hoskin SE, Thompson PJ. Epidemiology of chronic venous ulcers. Br J Surg. 1991;78(7):864–7. [DOI] [PubMed] [Google Scholar]
- (13).Wipke-Tevis DD, Rantz MJ, Mehr DR, Popejoy L, Petroski G, Madsen R, et al. Prevalence, incidence, management, and predictors of venous ulcers in the long-term-care population using the MDS. Adv Skin Wound Care. 2000;13(5):218–24. [PubMed] [Google Scholar]
- (14).Australian Wound Management Association Inc., New Zealand Wound Care Society Inc. Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers [Internet]. Osborne Park (Western Australia, Australia): Cambridge Publishing; 2011. [cited 2017 Dec]. Available from: http://www.woundsaustralia.com.au/publications/2011_awma_vlug.pdf [Google Scholar]
- (15).McDaniel HB, Marston WA, Farber MA, Mendes RR, Owens LV, Young ML, et al. Recurrence of chronic venous ulcers on the basis of clinical, etiologic, anatomic, and pathophysiologic criteria and air plethysmography. J Vasc Surg. 2002;35(4):723–8. [DOI] [PubMed] [Google Scholar]
- (16).Gohel MS, Barwell JR, Taylor M, Chant T, Foy C, Earnshaw JJ, et al. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. BMJ. 2007;335(7610):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).van Gent W, Wittens C. Influence of perforating vein surgery in patients with venous ulceration. Phlebology. 2015;30(2):127–32. [DOI] [PubMed] [Google Scholar]
- (18).White-Chu EF, Conner-Kerr TA. Overview of guidelines for the prevention and treatment of venous leg ulcers: a US perspective. J Multidiscip Healthc. 2014;7:111–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Shepherd J. Progressive compression versus graduated compression for the management of venous insufficiency. Br J Community Nurs. 2016;21:S13–S8. [DOI] [PubMed] [Google Scholar]
- (20).Andriessen A, Apelqvist J, Mosti G, Partsch H, Gonska C, Abel M. Compression therapy for venous leg ulcers: risk factors for adverse events and complications, contraindications: a review of present guidelines. J Eur Acad Dermatol Venereol. 2017;31(9):1562–8. [DOI] [PubMed] [Google Scholar]
- (21).McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. [DOI] [PubMed] [Google Scholar]
- (22).Cochrane Collaboration. Assessing risk of bias in included studies [Internet]. London: Cochrane Collaboration; 2018. [cited 2017 Dec]. Available from: http://methods.cochrane.org/bias/assessing-risk-bias-included-studies [Google Scholar]
- (23).Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Schünemann H, Brożek J, Guyatt G, Oxman A, eds. GRADE handbook [Internet]. Hamilton (ON): GRADE Working Group; 2013. [cited 2017 Dec]. Available from: http://gdt.guidelinedevelopment.org/app/handbook/handbook.html. [Google Scholar]
- (25).Clarke-Moloney M, Keane N, O'Connor V, Ryan MA, Meagher H, Grace PA, et al. Randomised controlled trial comparing European standard class 1 to class 2 compression stockings for ulcer recurrence and patient compliance. Int Wound J. 2014;11(4):404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Kapp S, Miller C, Donohue L. The clinical effectiveness of two compression stocking treatments on venous leg ulcer recurrence: a randomized controlled trial. Int J Low Extrem Wounds. 2013;12(3):189–98. [DOI] [PubMed] [Google Scholar]
- (27).Nelson EA, Harper DR, Prescott RJ, Gibson B, Brown D, Ruckley CV. Prevention of recurrence of venous ulceration: randomized controlled trial of class 2 and class 3 elastic compression. J Vasc Surg. 2006;44(4):803–8. [DOI] [PubMed] [Google Scholar]
- (28).Vandongen YK, Stacey MC. Graduated compression elastic stockings reduce lipodermatosclerosis and ulcer recurrence. Phlebology. 2000;15(1):33–7. [Google Scholar]
- (29).Dinn E, Henry M. Treatment of venous ulceration by injection sclerotherapy and compression hosiery: a 5-year study. Phlebology. 1992;7(1):23–6. [Google Scholar]
- (30).Reich-Schupke S, Murmann F, Altmeyer P, Stucker M. Quality of life and patients' view of compression therapy. Int Angiol. 2009;28(5):385–93. [PubMed] [Google Scholar]
- (31).Samson RH, Showalter DP. Stockings and the prevention of recurrent venous ulcers. Dermatol Surg. 1996;22(4):373–6. [DOI] [PubMed] [Google Scholar]
- (32).Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(e1000097). [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).National Institute for Health and Care Excellence. Methods for the development of NICE public health guidance. 3rd ed. Appendix I: Quality appraisal checklist—Economic evaluations [Internet]. London: The Institute; 2012. [cited 2017 Dec 8]. [PubMed] [Google Scholar]
- (34).Korn P, Patel ST, Heller JA, Deitch JS, Krishnasastry KV, Bush HL, et al. Why insurers should reimburse for compression stockings in patients with chronic venous stasis. J Vasc Surg. 2002;35(5):950–7. [DOI] [PubMed] [Google Scholar]
- (35).Rippon M, Davies P, White R, Bosanquet N. The economic impact of hard-to-heal leg ulcers. Wounds UK. 2007;3(2):58–69. [Google Scholar]
- (36).Meissner MH. Venous ulcer care: which dressings are cost effective? Phlebology. 2014;29:174–80. [DOI] [PubMed] [Google Scholar]
- (37).Ashby RL, Gabe R, Ali S, Adderley U, Bland JM, Cullum NA, et al. Clinical and cost-effectiveness of compression hosiery versus compression bandages in treatment of venous leg ulcers (venous leg ulcer study IV, VenUS IV): a randomised controlled trial. Lancet. 2014;383(9920):871–9. [DOI] [PubMed] [Google Scholar]
- (38).Guest JF, Fuller GW, Vowden P. Clinical outcomes and cost-effectiveness of three different compression systems in newly-diagnosed venous leg ulcers in the UK. J Wound Care. 2017;26(5):244–54. [DOI] [PubMed] [Google Scholar]
- (39).Guest JF, Gerrish A, Ayoub N, Vowden K, Vowden P. Clinical outcomes and cost-effectiveness of three alternative compression systems used in the management of venous leg ulcers. J Wound Care. 2015;24(7):300, 2–5, 7–8, passim. [DOI] [PubMed] [Google Scholar]
- (40).Pham B, Harrison MB, Chen MH, Carley ME, Canadian Bandaging Trial Group. Cost-effectiveness of compression technologies for evidence-informed leg ulcer care: results from the Canadian Bandaging Trial. BMC Health Serv Res. 2012;12:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Erickson CA, Lanza DJ, Karp DL, Edwards JW, Seabrook GR, Cambria RA, et al. Healing of venous ulcers in an ambulatory care program: the roles of chronic venous insufficiency and patient compliance. J Vasc Surg. 1995;22(5):629–36. [DOI] [PubMed] [Google Scholar]
- (42).Mayberry JC, Moneta GL, Taylor LM, Jr., Porter JM. Fifteen-year results of ambulatory compression therapy for chronic venous ulcers. Surgery. 1991;109(5):575–81. [PubMed] [Google Scholar]
- (43).Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. ISPOR health economic evaluation publication guidelines—CHEERS Good Reporting Practices Task Force. Value Health. 2013. Mar-Apr;16(2):231–50. [DOI] [PubMed] [Google Scholar]
- (44).Canadian Agency for Drugs and Technologies in Health. Guidelines for the economic evaluation of health technologies: Canada. 4th ed. [Internet]. Ottawa (ON): The Agency; 2017. [cited 2017 Dec]. Available from: https://www.cadth.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf [Google Scholar]
- (45).Derbyshire Medicines Management Shared Care and Guidelines Group. Guidelines for the use of compression hosiery [Internet]. South Derbyshire (UK): National Health Service; 2016. [cited 2017 Dec]. Available from: http://www.derbyshiremedicinesmanagement.nhs.uk/assets/Clinical_Guidelines/Formula_ry_by_BNF_chapter_prescribing_guidelines/Appendix_5/Compression_hosiery.pdf [Google Scholar]
- (46).Morrison T. American classification of compression stockings [Internet]. Phoenix: Terri Morrison; ND; [cited 2017 Dec]. Available from: http://www.tagungsmanagement.org/icc/images/stories/PDF/morrison_american_classification.pdf [Google Scholar]
- (47).Nherera LM, Woodmansey E, Trueman P, Gibbons GW. Estimating the clinical outcomes and cost differences between standard care with and without cadexomer iodine in the management of chronic venous leg ulcers using a Markov model. Ostomy Wound Manage. 2016;62(6):26–40. [PubMed] [Google Scholar]
- (48).Bianchi C, Cazzell S, Vayser D, Reyzelman AM, Dosluoglu H, Tovmassian G, et al. A multicentre randomised controlled trial evaluating the efficacy of dehydrated human amnion/chorion membrane (EpiFix) allograft for the treatment of venous leg ulcers. Int Wound J. 2017;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (49).Carter MJ, Waycaster C, Schaum K, Gilligan AM. Cost-effectiveness of three adjunct cellular/tissue-derived products used in the management of chronic venous leg ulcers. Value Health. 2014;17(8):801–13. [DOI] [PubMed] [Google Scholar]
- (50).Nelzen O, Bergqvist D, Lindhagen A. Long-term prognosis for patients with chronic leg ulcers: a prospective cohort study. Eur J Vasc Endovasc Surg. 1997;13(5):500–8. [DOI] [PubMed] [Google Scholar]
- (51).Starkmans Health Care Depot. Compression stockings [Internet]. Toronto (ON): Starkmans Health Care Depot; 2018. [cited 2017 Dec]. Available from: https://starkmans.com/compression-stockings.html [Google Scholar]
- (52).Registered Nurses' Association of Ontario. Dollars and sense: What are nurses paid? [Internet]. Toronto (ON): The Association; 2017. [cited 2017 Dec]. Available from: http://careersinnursing.ca/new-grads-and-job-seekers/find-nursing-job/dollars-and-sense-what-are-nurses-paid [Google Scholar]
- (53).Swoboda SJ, Schumann H, Kiritsi D. A leg ulcer with pulsating varicose veins–from the legs to the heart. Int Wound J. 2017;07:07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (54).Ministry of Health and Long-Term Care. Schedule of benefits for physician services under the Health Insurance Act [Internet]. Toronto (ON): Queen's Printer for Ontario; 2015. [cited 2017 Dec]. Available from: http://www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/sob_master20_151221.pdf [Google Scholar]
- (55).Ministry of Health and Long-Term Care. Ontario drug benefit formulary/comparative drug index [Internet]. Toronto (ON): Queen's Printer for Ontario; 2016. [cited 2017 Dec]. Available from: https://www.formulary.health.gov.on.ca/formulary/ [Google Scholar]
- (56).Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006. [Google Scholar]
- (57).Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005. [Google Scholar]
- (58).Anti-infective Review Panel. Anti-infective guidelines for community acquired infections Toronto (ON): MUMS Health; 2013. [Google Scholar]
- (59).Venclauskas L, Maleckas A, Arcelus JI, Force EVGT. European guidelines on perioperative venous thromboembolism prophylaxis: Surgery in the obese patient. Eur J Anaesthesiol. 2017;06:06. [DOI] [PubMed] [Google Scholar]
- (60).Lorimer KR, Harrison MB, Graham ID, Friedberg E, Davies B. Assessing venous ulcer population characteristics and practices in a home care community. Ostomy Wound Manage. 2003;49(5):32–4, 8–40, 2–3. [PubMed] [Google Scholar]
- (61).Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol. 2002;46(3):381–6. [DOI] [PubMed] [Google Scholar]
- (62).Barham L. Public and patient involvement at the UK National Institute for Health and Clinical Excellence. Patient. 2011;4(1):1–10. [DOI] [PubMed] [Google Scholar]
- (63).Messina J, Grainger DL. A pilot study to identify areas for further improvements in patient and public involvement in health technology assessments for medicines. Patient. 2012;5(3):199–211. [DOI] [PubMed] [Google Scholar]
- (64).OHTAC Public Engagement Subcommittee. Public engagement for health technology assessment at Health Quality Ontario—final report from the Ontario Health Technology Advisory Committee Public Engagement Subcommittee [Internet]. Toronto (ON): Queen's Printer for Ontario; 2015. [cited 2018 April]. Available from: http://www.hqontario.ca/Portals/0/documents/evidence/special-reports/report-subcommittee-20150407-en.pdf [Google Scholar]
- (65).Kvale S. Interviews: an introduction to qualitative research interviewing. Thousand Oaks (CA): Sage Publications; 1996. [Google Scholar]
- (66).Kuzel AJ. Sampling in qualitative inquiry. In: Miller WL, Crabtree BF, editors. Doing Qualitative Research. Thousand Oaks (CA): Sage Publications; 1999. p. 33–45. [Google Scholar]
- (67).Morse J. Emerging from the data: cognitive processes of analysis in qualitative research. In: Morse J, editor. Critical Issues in Qualitative Research Methods Thousand Oaks (CA): Sage Publications; 1994. p. 23–41. [Google Scholar]
- (68).Patton MQ. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks (CA): Sage Publications; 2002. [Google Scholar]
- (69).Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures of developing a grounded theory. 2nd ed. Thousand Oaks (CA): Sage Publications; 1998. [Google Scholar]
- (70).Health Technology Assessment International Interest Group on Patient and Citizen Involvement in HTA. Introduction to health technology assessment [Internet]. Edmonton (AB): Health Technology Assessment International; 2015. [cited 2018 April]. Available from: http://www.htai.org/fileadmin/HTAi_Files/ISG/PatientInvolvement/v2_files/Resource/PCISG-Resource-Intro_to_HTA__KFacey__Jun13.pdf [Google Scholar]
- (71).Strauss AL, Corbin JM. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3–21. [Google Scholar]
- (72).Strauss AL, Corbin JM. Grounded theory methodology: an overview. In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. Thousand Oaks (CA): Sage Publications; 1994. p. 273–85. [Google Scholar]