Abstract
Over recent years, new evidence has led a rethinking of the available guidance on the diagnosis and management of infective endocarditis (IE). This review compares the most recently available guidance provided by the American Heart Association (AHA) IE Writing Committee, and the Task Force for the management of IE of the European Society of Cardiology (ESC). This represents the sixth of a new series of comparative guidelines review published in the Journal.
Keywords: Infection, image-guided application, multimodality
Over recent years, new evidence has led to a rethink of the available guidance on the diagnosis and management of infective endocarditis (IE). This review compares the most recently available recommendations provided by the American Heart Association (AHA) IE Writing Committee, and the Task Force for the management of IE of the European Society of Cardiology (ESC).1,2 Class (I, II or III) and level of evidence (A, B or C) are provided for each recommendation where given by the guidelines (Tables 1, 2, 3; Figures 1, 2). As in previous comparative guidelines reviews published in the Journal,3–7 this review focuses on the role of imaging in the evaluation and management of patients with suspected IE.
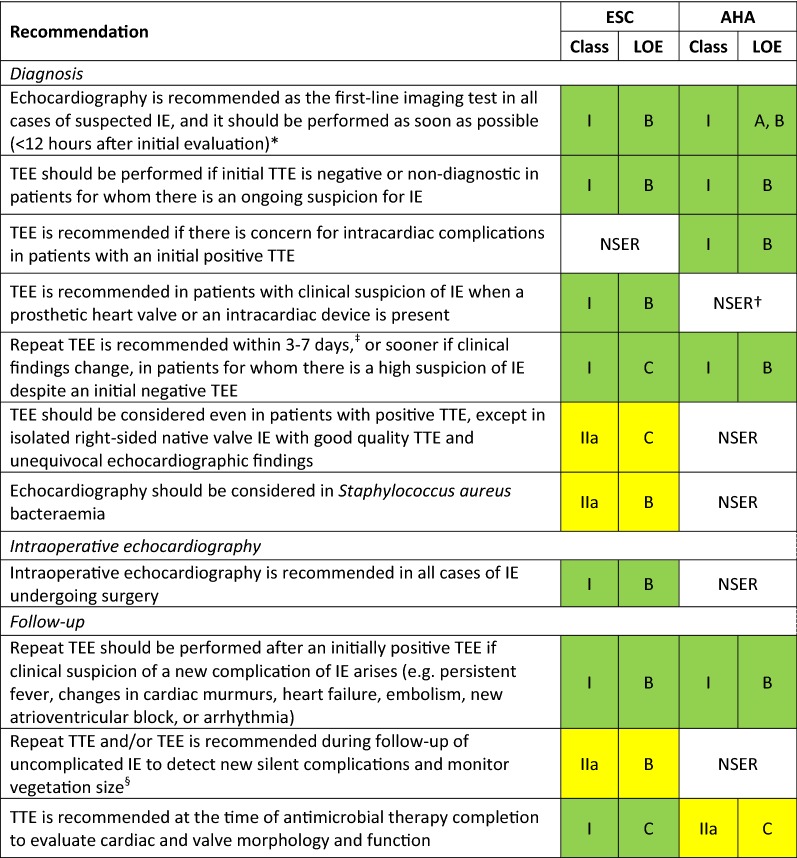
Table 1.
Indications for echocardiography in patients with suspected infective endocarditis
*According to the AHA scientific statement, TEE is preferred over TTE, but the latter should be performed if TEE is not immediately available. TTE may be sufficient in small children
†AHA statement also suggests TEE as first-line test in patients with a prosthetic valve and suspected IE
‡In this clinical scenario, the AHA statement recommends repeating the TEE in 3 to 5 days or sooner
§ESC guidelines stipulate that the timing and mode (TTE or TEE) of repeat test depend on initial findings, microorganism type, and initial response to therapy
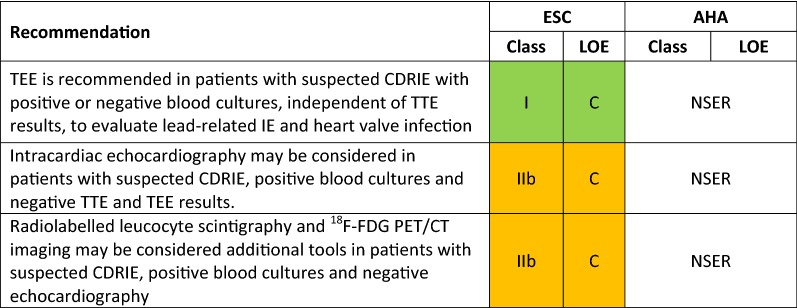
Table 2.
indications for non-invasive imaging in cardiac device-related infective endocarditis (CDREI)
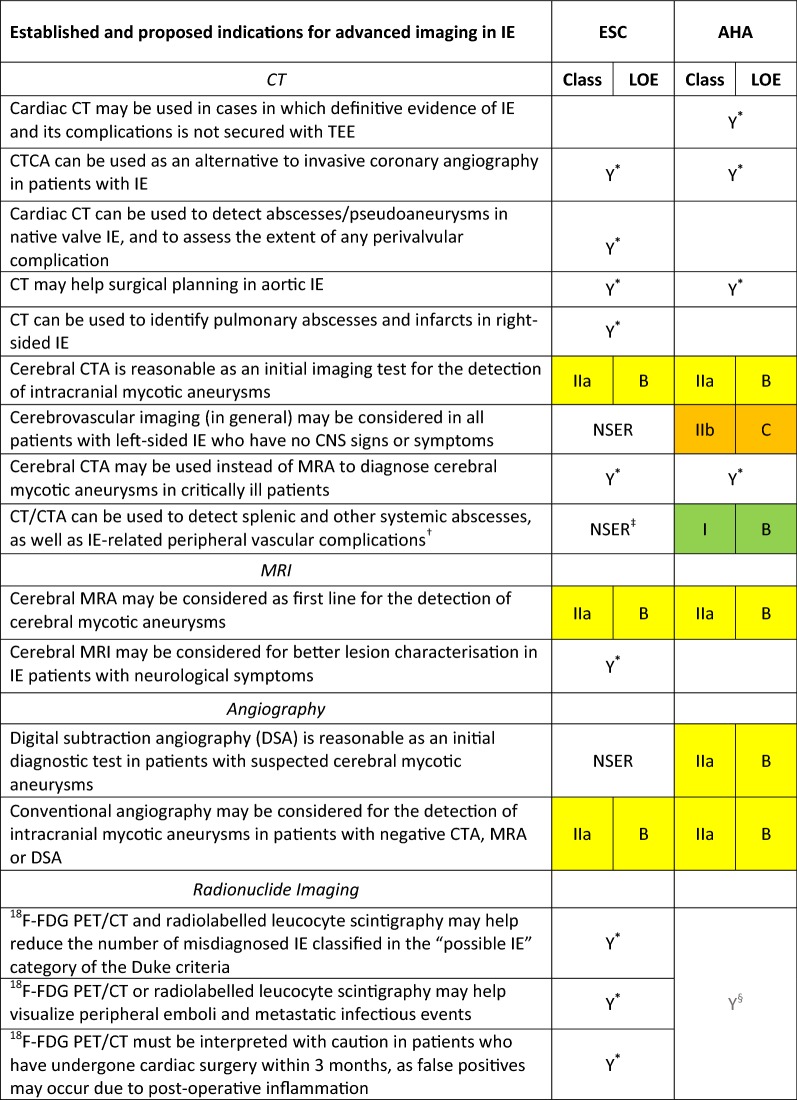
Table 3.
Role of CT, MRI, radionuclide imaging and angiography in the assessment of IE patients
*These proposed indications are discussed in the guidelines but neither the ESC guidelines nor the AHA scientific statement give specific or formal recommendation
†The AHA statement recommends that, in IE patients with suspected metastatic foci of infection, the choice of diagnostic technique (ultrasonography, CT or MRI) should be individualised for each patient (Class I; LOE, C)
‡Although there is no specific recommendation, the ESC guidelines state that patients with suspected splenic complications should be evaluated by CT, MRI or ultrasound
§The AHA statement recognises that more studies are needed to determine the role of 18F-FDG PET/CT imaging in the diagnosis and management of patients with IE, and highlights evidence on the usefulness of this technique for the detection of peripheral emboli and other extracardiac complications
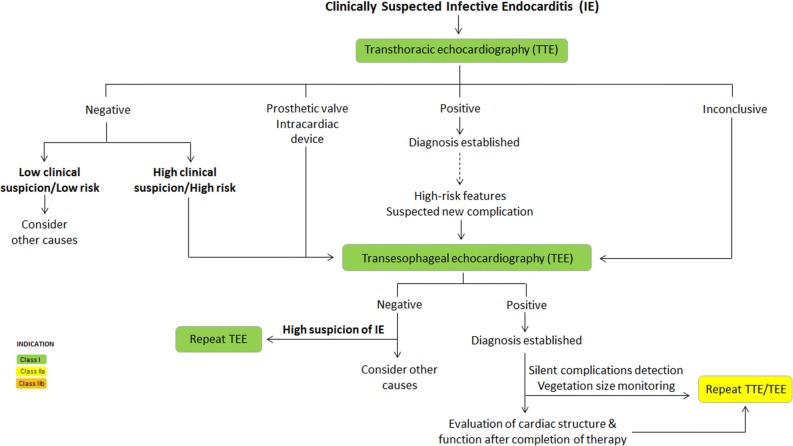
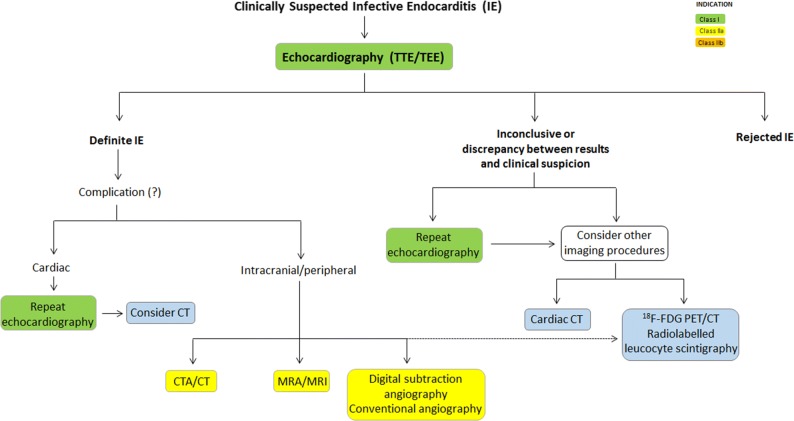
Figure 1.
ESC and AHA recommendations for the initial assessment of patients with clinically suspected infective endocarditis using echocardiography
Figure 2.
Role of advanced imaging in the assessment of patients with infective endocarditis. CTA, computed tomographic angiography; 18F-FDG, 18-fluorodeoxyglucose; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography
Acknowledgments
Disclosure
All authors have nothing to disclose.
Abbreviations
- CTCA
Computed tomographic coronary angiography
- CDRIE
Cardiac device-related infective endocarditis
- DSA
Digital subtraction angiography
- 18F-FDG
18-fluorodeoxyglucose
- IE
Infective endocarditis
- LOE
Level of evidence
- MRI
Magnetic resonance imaging
- MRA
Magnetic resonance angiography
- NSER
No specific equivalent recommendation
- PET/CT
Positron emission tomography/computed tomography
- TEE
Transesophageal echocardiography
- TTE
Transthoracic echocardiography
References
- 1.Baddour LM, Wilson WR, Bayer AS, Fowler VG, Jr, Tleyjeh IM, Rybak MJ, et al. American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Stroke Council. Infective Endocarditis in Adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 2.Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. ESC Scientific Document Group. 2015 ESC guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM) Eur Heart J. 2015;36:3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 3.Velasco A, Reyes E, Hage FG. Guidelines in review: Comparison of the 2014 ACC/AHA guidelines on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery and the 2014 ESC/ESA guidelines on noncardiac surgery: Cardiovascular assessment and management. J Nucl Cardiol. 2017;24:165–170. doi: 10.1007/s12350-016-0643-8. [DOI] [PubMed] [Google Scholar]
- 4.Stirrup J, Velasco A, Hage FG, Reyes E. Comparison of ESC and ACC/AHA guidelines for myocardial revascularization. J Nucl Cardiol. 2017;24:1046–1053. doi: 10.1007/s12350-017-0811-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velasco A, Stirrup J, Reyes E, Hage FG. Guidelines in review: Comparison between AHA/ACC and ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Nucl Cardiol. 2017;24:1902–1903. doi: 10.1007/s12350-017-0919-7. [DOI] [PubMed] [Google Scholar]
- 6.Prejean SP, Din M, Reyes E, Hage FG. Guidelines in review: Comparison of the 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes and the 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. J Nucl Cardiol. 2017 doi: 10.1007/s12350-017-1137-z. [DOI] [PubMed] [Google Scholar]
- 7.Joseph J, Velasco A, Hage FG, Reyes E. Guidelines in review: Comparison of ESC and ACC/AHA guidelines for the diagnosis and management of patients with stable coronary artery disease. J Ncl Cardiol. 2018;25:509–515. doi: 10.1007/s12350-017-1055-0. [DOI] [PubMed] [Google Scholar]