Abstract
This study explores the relationship between mental health and place at microgeographic units of analysis. We examine self-reported symptomology for depression and PTSD for 2,724 survey respondents interviewed in three types of randomly selected street segments: violent crime hot spots, cool spots, and cold spots. We find that the mean symptomology score is 61% higher for depression in violent crime hot spots than cold spots, and 85 percent higher for PTSD. Overall, we estimate that 14.8% of residents of violent crime hot spots meet thresholds for moderate depression or a diagnosis of PTSD. This can be compared to only 6.5% of residents at the cold spots. Using PSM and weighted negative binomial regression approaches we show that observable selection factors are not responsible for the relationships identified. Examining geographic influences, we find an important area effect of violent crime for both mental health measures, and an additional impact of the specific street of residence for PTSD.
Keywords: PTSD, Depression, Violence, Mental Health, Hot Spots
In recent years, researchers have begun to examine the relationship between violence, crime and mental health in neighborhoods and communities. Underlying this interest is a recognition that disadvantage and crime can have an impact on public health outcomes (Curry, Latkin, & Davey-Rothwell, 2008; Diez Ruiz, & Mair, 2010; Franco, Diez Roux, & Glass, 2008; LaVeist & Wallace, 2000; O’Campo, Xue, Wang, & Caughy, 1997). Living in an area with high levels of violence is hypothesized to lead to high levels of stress, which is in turn seen to increase the likelihood of the development of mental health problems. Overall, studies suggest that neighborhood conditions such as crime and violence have strong impacts on mental health (Curry et al., 2008; Dustmann & Fasani, 2016; Stockdale, Wells, Tang, Belin, Zhang & Sherbourne, 2007). For example, witnessing community violence is strongly related to symptoms of depression and anxiety (Buckner, Beardslee, & Bassuk, 2004). Exposure to community level violence also has been documented to increase rates of depression and anxiety and can lead to developmental problems among youths (Berman, Kurtines, Silverman, & Serafini, 1996; Fitzpatrick, Piko, Wright, & LaGory, 2005; Smith & Tolan, 1998). Violent victimization has also been found to increase depression among low-income African-American youth (Fitzpatrick & Boldizar, 1993).
Individual-level risk factors associated with mental health problems, particularly depression, have been noted often in research, but more recently, attention has shifted to examining neighborhood-level risk factors, predominately neighborhood socioeconomic status, but also measures of residential mobility, physical and social environment, access to resources, and social capital (Echeverría, Diez-Roux, Shea, Borrell, & Jackson, 2008; Galea, Ahern, Nandi, Tracy, Beard, & Vlahov, 2007; Ross, 2000; Silver, Mulvey, and Swanson, 2002; Weich, Twigg, Holt, Lewis, & Jones, 2003). Studies have also started to examine the causal mechanisms through which these macro-level forces impact individuals’ mental health and well-being (Curry et al., 2008; Dupéré & Perkins, 2007; Latkin & Curry, 2003; Mair, Diez Roux, & Morenoff, 2010; O’Campo, Wheaton, Nisenbaum, Glazier, Dunn, & Chambers, 2015; Ross & Mirowsky, 2001; Stockdale et al., 2007). Kim (2008) conducted a systematic review of 28 studies that examined the relationship between neighborhood characteristics and adult depression, finding mixed results regarding the association between community-level factors and individual-level depression. About half of the studies found that neighborhood socioeconomic status and other SES-related characteristics like physical environment and neighborhood services, were related to depression in the expected direction, while the other half found null results.
Mair, Diez Roux and Galea (2008) also conducted a review of 45 studies on neighborhood characteristics and depression or depressive symptoms, with similar findings with regard to structural characteristics like socioeconomic status, racial composition, and residential mobility. Measures of social processes, such as disorder, social interactions, and exposure to violence were more consistent, with many studies finding significant relationships with depression in the expected direction (Mair et al., 2008). Overall, these reviews conclude that neighborhood characteristics, both risk and protective factors, contribute to mental health and well-being at the individual-level beyond individual characteristics. However, the authors discuss the difficulty of making comparison across studies due to factors such as the variation in populations studied, measurement of neighborhood characteristics, and size of geographic units. Studies that examine community-level factors on health are often not designed to examine these questions more generally, focusing specifically on vulnerable groups such as minority women (Cutrona, Russeell, Brown, Clark, Hessling, & Gardner, 2005), youth and adolescents (Aneshensel & Sucoff, 1996; Fitzpatrick & Boldizar, 1993; Simons, Murry, & McLoyd, 2002; Smith & Tolan, 1998), older adults (Aneshensel, Wight, Miller-Martinez, Botticello, Karlamangla, & Seeman, 2007; Kubzansky, Subramanian, Kawachi, Fay, Soobader, & Berkman, 2005), or drug users (Curry et al., 2008). Additionally, while studies have examined neighborhood characteristics that are strongly related to crime, much less research has examined the direct impact that crime at the community-level may have on mental health, particularly very high crime areas. Living in high crime areas may, for example, increase exposure to violence, victimization, fear, withdrawal and avoidance behavior, that can subsequently have negative impacts on residents’ mental health (Braakman, 2013; Diez Roux & Mair, 2010; Fitzpatrick et al., 2005; Mair et al., 2010; Pearson, Breetzke, & Ivory, 2015; Stockdale et al., 2015).
Furthermore, much of the research has been done at census block groups and census tracts, or units of similar size in other countries, and we are not aware of any studies that focus on mental health at micro-geographic units of space. Mair et al. (2008) recommended examining various spatial areas to better understand the spatial patterning of health outcomes and improve theory on the role of one’s immediate or broader spatial context on health. It may be, for example, that findings are mixed and less consistent than expected due to the spatial scale of these large community areas, where if we were to examine more closely the place surrounding someone’s residence, we may see more consistent findings.
The assumption that links these studies is that the influence of place is at a meso or macro geographic level. Over the last two decades there has been a growing recognition of the importance of micro-geographic areas in the production of crime problems (Braga & Clark, 2014; Weisburd, Bushway, Lum, & Yang, 2004). Beginning with a seminal study by Sherman and colleagues (1989), criminologists have begun to recognize that crime is very concentrated at small micro-geographic units. Sherman, Gartin, & Bruerger (1989) found that just 3.5 percent of the addresses in Minneapolis produced 50 percent of all calls for crime to the police. Similar levels of concentration have been found in a series of studies examining different indicators of crime at micro-geographic units such as street segments, facilities and small clusters of street segments (e.g. see Andresen & Malleson (2011); Eck, Clark, & Guerette, 2007; Linnell, 1988; Pierce, Spaar & Briggs, 1988; Sherman, 1995; Taylor, 1997; Weisburd & Green, 1995; Weisburd, Groff, & Yang, 2012; Wheeler, Warden & Mclean, 2016). In a recent study, Weisburd (2015) examined 5 large cities and using a similar measure of crime and geography (street segments) found that about 5 percent of streets in larger cities produce 50 percent of recorded crime and about 1 percent of streets produce 25 percent of recorded crime. He argues for a “law of crime concentration” at micro-geographic units.
Violent crime has also been shown to cluster in crime hot spots. For example, in Boston, Braga, Papachristos and Hureau (2010) examined incidents of gun violence between 1980 and 2008. They found incidents of gun violence were stable and concentrated at less than 5 percent of street segments and intersections. They also reported that between 1 percent and 8 percent of street segments and intersections were responsible for nearly 50 percent of all commercial robberies and 66 percent of all street robberies (Braga, Hureau, & Papachristos, 2011).
It is important to note in this regard that the concentration of crime more generally, and violent crime specifically, at crime hot spots is not simply a rarefication of meso or micro area trends. A number of studies now show that crime hot spots are spread throughout the city, and not concentrated in a specific neighborhood or area (Andresen & Malleson, 2011; Groff Weisburd, & Yang, 2010; Oberwittler & Wikström, 2009; Steenbeek & Weisburd, 2016; Weisburd et al., 2012). In a sixteen-year longitudinal study of crime in Seattle, Washington, it was found that higher crime street segments are not distributed at random, and are more likely to be closer to each other than would be predicted simply by chance (Weisburd et al., 2012). But these indications of macro geographic influences were much outweighed by evidence of the importance of looking at crime at the micro-level:
These maps, as well as others reviewed in this section, reinforce the spatial heterogeneity at the street segment level that we illustrated with simple descriptive maps earlier in the chapter. Street segments of one pattern are very likely to be surrounded by street segments of a different crime trajectory pattern. While there is evidence of clustering, or positive autocorrelation of trajectory patterns (especially for crime free and low stable crime patterns that include a large proportion of the street segments in the city), our analyses overall suggest that crime patterns are interspersed throughout the city. (Weisburd et al., 2012)
Based on this work, our study seeks to examine whether a relationship can be found between violent crime and mental health problems at a micro-geographic unit of analysis. Drawing from a large National Institutes of Health survey conducted at street segments in Baltimore, MD, we look at the relationship between self-reported symptomology for depression and post-traumatic stress disorder (PTSD) and living within a violent crime hot spot. Our findings support the hypothesis that mental health and violent crime are strongly related at micro-geographic units of analysis. We then examine to what extent this relationship is due to selection factors that bring residents to specific types of streets, and whether it is violent crime on those specific streets or violent crime in the nearby area that influences mental health outcomes. Our findings suggest that observable selection factors do not account for the salience of the street segment environment for both self-reported depression and PTSD. Regarding geographic influences, we find an important area effect for both mental health measures, and additional impact of the specific street of residence for PTSD.
The Study
In this paper, we examine 2,724 subjects surveyed in 2013–2014 in Baltimore, Maryland, a large Eastern Seaboard City with serious crime problems. The city includes a population of over 630,000 people living within 80.8 square miles. Baltimore is 64% African American, and has a poverty rate of 24% (U.S. Census Bureau, accessed 2015). Violent crime has declined significantly in the city since the mid-1990s following national trends.
This paper focuses on 328 of the 25,045 street segments in the city: 181 violent crime hot spots; and 147 comparison segments that reflected cool (N=100) and cold spots (N=47) of crime (see below).1 A street segment was defined as both sides of the street between two intersections. Street segment type was based on police calls for service. We used calls for service as our measure of crime because they are likely to capture a broader array of information on citizen concerns about crime, and less likely to be censored by police processing than crime arrests or crime incidents (Black, 1970; Sherman et al., 1989; Weisburd et al., 2012). Our threshold for violent crime hot spots was 17 violent crimes in the selection year (2012; about the top 3% of violent crime segments in the city). We included only residential streets that had at least 20 residences in our sampling frame, because we were interested in developing a minimum survey sample of seven respondents on each street segment. The goal of the survey was to understand the impact of living in crime hot spots on a number of social outcomes, including mental health, from a large representative sample of residents living on these streets.
Non-hot spot or comparison segments included all streets that did not meet the hot spot street thresholds (in addition to being below the violent crime threshold they also were required to be below a drug crime threshold of 18 calls). Based on a review of the distribution of crime, we selected out streets with 3 or fewer crime calls for drug or violent crime, and defined them as “cold” spots. The remaining non-hot spot streets are defined as “cool spots” in our study.
Street segments were chosen from the final universe of streets in that category through a random sampling procedure developed in Model Builder (in ArcGIS) that prevented any two sample streets from being within a one block buffer area. Figure 1 shows the location of the different types of street segments within the city studied. As is apparent from Figure 1 there is a good deal of mixture within areas between the segments of different types, though hot spots are more likely to be located in the central areas of the city.
Figure 1.
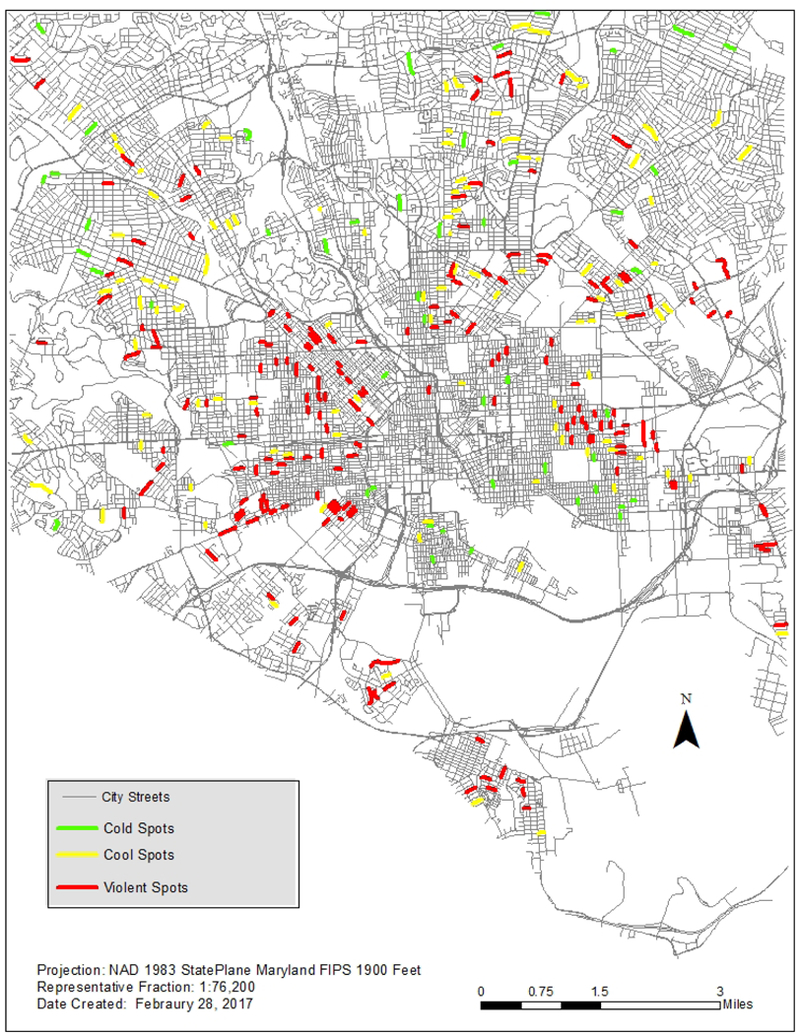
Geography of Sampled Street Segments
Face to face surveys were carried out at a random sample of residences on the sampled streets. Interviewers went to the identified streets in random order (identified within small area clusters), and interviewed the first adult resident contacted who had lived on the street for at least three months. They returned to the same streets an average of four times and as many as 25 times. The interviewing time frame included mornings, afternoons and early evenings. After accounting for abandoned housing, our contact rate was 71.2%. The cooperation rate was 60.5%, which is above average for door to door surveying (Babbie, 2007; Holbrook, Krosnick, & Pfent, 2008). Surveys took an average of 20 minutes and respondents were given $15 for their participation. The survey was conducted between September of 2013 and May of 2014 with an average of 8 surveys completed on each street (Min=6; Max=14). Appendix A shows the survey measures that were used in this paper.
Mental Health Measures
Post-traumatic stress symptomology was assessed using a short screening scale for post-traumatic stress disorder based on the DSM-IV (Breslau, Peterson, Kessler & Schultz, 1999; Kimerling, Ouimette, Prins, Nisco, Lawler, Cronkite, & Moos 2006). First, respondents were asked whether they had experienced a traumatic event such as abuse, a serious accident, or an act of violence at some point in his or her life. When a respondent indicated that he or she did not experience such an event they were scored a 0 on our scale. When respondents indicated that they had experienced such an event, the interviewer followed up with the seven-question scale, which asks the respondent to indicate ‘yes’ or ‘no’ to items that measure PTSD symptoms such as avoidance, numbing, and hyperarousal. A count measure of the number of positive responses to the seven items was used in the analyses for PTSD symptomatology.
For the depression symptomology measure (PHQ9) respondents were asked a series of nine questions that measured affect or mood: including behavior such as social withdrawal, cognitive symptoms such as the inability to concentrate or make decisions, and physical symptoms such as difficulty sleeping (Kroenke, Spitzer, & Williams, 2001). Responses were scored based on the frequency that the reported symptom occurred in the past month (0 = not at all, 1 = several days, 2 = more than half the days, 3 = almost every day), and these scores were summed to a scale that ranged between 1 and 27.
Methods
For our examination of variation in depression and PTSD symptomology we compared the average means for the three groups of street segments: violent crime hot spots, cool spots and cold spots. One-way analysis of variance and chi-square analyses were used to examine statistical significance. We used a two-stage method to address potential bias due to selection into street segments. First, we used propensity score matching (PSM) to identify similar sets of subjects from the three street segment types studied (Cochrane & Rubin, 1973; Imbens, 1999; Rosenbaum & Rubin, 1983). In Appendix B, we show the PSM models and characteristics used to match respondents. These included socio-demographic characteristics (race, education, gender, income, education, and work status), family characteristics (marital status, number of children), information on why they moved to the street, tenure on the block, and whether they rent or own. The matching reduced potential bias due to selection into street segments of different types on observable characteristics also related to mental health. We ran two PSMs; the first model was used to match cold and cool spot respondents, and the second model was used to match cool and violent crime spot respondents. We used a caliper of 0.01 to match subjects across street segment types during propensity score analysis and omitted those subjects for whom there were no similar residents in the comparison segment type from the analysis.
This approach produced a sample of 2,136 subjects. 588 subjects were omitted from further analysis due to large dissimilarities in comparison to cool street segment residents or missing data (324 violent crime street subjects; 182 cool spot subjects; 82 cold spot subjects).2 In the second step, to obtain doubly robust results, we ran weighted negative binomial regression models on successfully matched subjects with errors clustered at the street segment level (Lunceford & Davidian, 2004; Robins, Hernán, & Brumback, 2000). These models included all the covariates used in the propensity score models, and incorporated inverse probability weights calculated from the propensity score model results to more closely balance the distribution of covariates between the matched groups. The model results can be interpreted as the impact on mental health outcomes of moving between segment types, for the type of cool spot resident that could live in any street segment type (if the propensity or model assumptions hold). We also developed a second model, which included area wide impacts of violent crime at a 3000-foot radius reflecting routine activity spaces near to the hot spots (Andresen & Malleson, 2011; Duany & Plater-Zyberk, 1994; Larsen, El-Genediy, & Yasmin, 2010). Because we had a strong hypothesis that the violent crime hot spots will have higher rates of depression and PTSD symptomology, we used a one-tailed significance threshold for the impact of violent crime hot spots, and the area wide spatial lag.
Results
Table 1 includes the crime call counts for the selection year for each type of street segment. The violent crime hot spot streets on average had 27 violent crime calls (and 160 crime calls overall) in the selection year. In contrast, the cool spots had on average 6 violent crime calls (and 42 crime calls overall), and the cold spots averaged only 1 violent crime call (and 17 crime calls overall). We also found that the likelihood of being a victim of a violent crime, which would be expected to exacerbate the symptoms we observed, was much higher for people who live on high crime streets (see Table 2). People who lived in the violent crime hot spot group were twice as likely to report violent victimization in the past year when compared to people who lived in cool or cold spots.
Table 1:
Mean (standard deviation) of crime calls in sampled street segments
| Type of Segment | N | Violent Crime | Other Crimes | Total Crime |
|---|---|---|---|---|
| Cold Spot | 47 | 1.45 (1.04) | 15.91 (8.76) | 17.36 (9.33) |
| Cool Spot | 100 | 6.30 (3.59) | 35.96 (16.54) | 42.26 (18.57) |
| Violent Spot | 181 | 27.19 (11.19) | 132.83 (129.83) | 160.03 (134.19) |
Table 2:
Mental health, victimization and demographic indicators for sampled respondents
| Cold Spot | Cool Spot | Violent Spot | |||
|---|---|---|---|---|---|
| Variables | N | Mean (SD)/ % | Mean (SD)/ % | Mean (SD)/ % | F/ChiSquare |
| Mental Health Measures | |||||
| Depression Symptomology | 2,661 | 2.28 (3.26) | 2.99 (4.27) | 3.68 (4.83) | 16.71*** |
| Post-Traumatic Stress Symptomology |
2,684 |
0.39 (1.13) |
0.57 (1.44) |
0.72 (1.63) |
7.93** |
| Violent Victimization | |||||
| Victimized in past year | 2,718 | 2.71% | 2.94% | 6.27% | 16.99*** |
| Demographic Characteristics | |||||
| African American | 2,682 | 43.09% | 74.38% | 77.71% | 176.91*** |
| Did Not Complete High School | 2,719 | 6.50% | 16.79% | 22.77% | 54.63*** |
| Household Income 25,000 or Less | 2,721 | 13.28% | 29.04% | 54.55% | 159.04*** |
| % Unemployed | 2,718 | 15.45% | 29.20% | 38.31% | 76.56*** |
p<.05,
p<.01,
p<.001
Table 2 reports depression and PTSD symptomology across the three groups. The differences are large and statistically significant. Mean depression symptomology was 61% higher for individuals in violent crime hot spots than in the cold spots (3.68 versus 2.28). The mean PTSD symptomology scale measure was .39 for respondents in the cold spots, and .72 for respondents in violent crime spots. This means that post-traumatic stress symptomology is almost 85% higher for residents in the hot spots than the places where there is little crime.
The PHQ-9 and DSM-IV provide guidance on the scaling of depression and post-traumatic stress symptomology that is useful for contextualizing the overall symptomology differences between respondents who live on low and high violent crime segments. For instance, the PHQ-9 defines a person with a sum of 15–27 depression symptoms as having moderately severe to severe depression (Kroenke et al., 2001). In our sample, 1.7% of the residents of cold spots had moderately severe or severe depression, and 4.5% of the residents of the violent spots had moderately severe or severe depression. Looking at the moderate threshold for a diagnosis of depression (a score of 10 or higher), we find that 10.8% of residents at violent crime hot spots meet this threshold, but only 3.3% of residents in cold spots meet this threshold. In regard to PTSD, a cut score of 4 symptoms is used to identify persons with PTSD (Breslau et al., 1999; Kimerling et al., 2006). In our sample, 9.3% of respondents living in violent spots met this criterion, as compared to 4.7% of respondents in cold spots. The rate for the cold spots is similar to national estimates of PTSD (see Kilpatrick, Resnick, Milanak, Miller, Keyes, & Friedman, 2013). Overall, we estimated that 14.8% of residents of violent crime hot spots met thresholds for moderate depression or a diagnosis of PTSD. This can be compared to only 6.5% of residents at the cold spots.
Our second research question asked to what extent the relationships observed can be explained by selection factors. Indeed, our data showed higher levels of minorities, poorer and younger residents on these streets (see Table 2). For example, respondents who lived in the violent crime hot spots are 77.7% African American as compared to cold spots which were 43.1% African American. Likewise, respondents were less likely to have completed high school, with 22.8% of persons in crime hot spots lacking a high school education as compared to 6.5% in cold spots. Respondents on the violent hot spot streets were also more likely to be unemployed (38.3%) when compared with residents of cold spots (15.5%).
As described earlier we used PSM and weighted regression approaches to identify the impact of selection on our findings. Using PSM in a first step, the samples were balanced according to observed covariates. The percentage of bias of comparisons after omitting non-matched subjects was rarely above 10 and never above 20 (see Appendix B). As a second step, we used weighted negative binomial regression models for the reduced sample. In Table 3, we report the model values only for depression and PTSD when controlling for a series of characteristics and attitudes of the respondents without a spatial lag term (see Appendix C for full model results). We then took into account potential area impacts with a spatial lag term at 3000 feet.3
Table 3:
Incidence rate ratios (and statistical significance) for post-traumatic stress and depression symptomology after modeling for selection and spatial dependence (see Full Models Appendix C)
| PTSD Symptomology | Depression Symptomology | |||
|---|---|---|---|---|
| IRR (SD) | Z | IRR (SD) | Z | |
| No Spatial Lag | ||||
| Cool Spots | 1.35 (0.26) | 1.60 | 1.04 (0.11) | 0.39 |
| Violent Spots | 1.71 (0.32) | 2.91** | 1.19 (0.12) | 1.66* |
| N = 2,136 | N = 2,136 | |||
| 3000 ft Spatial Lag | ||||
| Cool Spots | 1.31 (0.25) | 1.45 | 1.02 (0.10) | 0.19 |
| Violent Spots | 1.46 (0.28) | 1.95* | 1.11 (0.11) | 1.00 |
| Spatial Lag | 1.17 (0.08) | 2.24* | 1.07 (0.03) | 2.33** |
| N=2,136 | N=2,136 | |||
p<.05,
p<.01,
p<.001
Reference Category: Cold Spot; One tailed tests of statistical significance are reported
Respondents in violent crime hot spots in the sample continued to have significantly higher levels of depression symptomology than similar respondents on streets with little crime (p<.05) after addressing selection on observables. The incidence rate ratio (IRR) indicated that respondents in the violent crime hot spots have about a 19% higher rate of depression than respondents in cold spots. After introducing the spatial lag term the relationship was no longer statistically significant.4 The spatial lag, however, is statistically significant (p<.01). This suggests that it is the level of violent crime in the local area (including the street segment), which is important in understanding depression symptomology, rather than the classification of the street segment itself as a violent crime hot spot.
Respondents in the violent crime hot spots had a 71% higher rate of PTSD than respondents in the cold spots (p<.01) after addressing selection. Including the spatial lag at 3000 feet, the magnitude of the relationship declined to a 46% higher rate than cold spots and remained statistically significant (p<.05). The spatial lag for the nearby area was again statistically significant (p<.05). Accordingly, in the case of PTSD there is both an influence of the local area level of violence, and the specific level of violence (as defined by being in the violent crime hot spot group) of the street.
Discussion
There has been a growing interest in the relationship between mental health and place, though places have generally been defined in the context of meso and macro geographies. In studies using these larger geographic units of analysis, people who live in high violence and high crime neighborhoods have been found to have higher risks of mental health problems (Aneshensel & Sucoff, 1996; Clark et al., 2008; Curry et al., 2008; Mair et al., 2008; Wandersman & Nation, 1998; White, Kasl, Stanislav & Zahner, 1987). Our findings reinforce the hypothesis that there is a relationship between mental health, place and violent crime, but we are the first to show this relationship at a micro-geographic level.
We began our paper by asking whether there was a relationship between depression or post-traumatic stress symptomology and violent crime hot spots. Our data showed that residents of hot spots have significantly higher average symptomology scores for both depression and post-traumatic stress disorder than residents of non-hot spot streets. These differences in turn are meaningful in magnitude. We estimated that the percent of residents of violent crime hot spots in our sample that reach a moderate depression symptomology level or a PTSD diagnosis level is more than double that of residents of cold spots. This suggests that there is a strong concentration of needs for mental health services at crime hot spots.
More generally, a focus on crime hot spots provides an opportunity to “lower the scale” of health interventions and provide services more efficiently (Weisburd, Groff, &Yang, 2014). It is one thing to attempt to increase mental health services in an entire neighborhood. It is another to try to reduce problems on specific blocks. Indeed, just as prior studies have found that the application of generalized preventive police patrol across large areas is ineffective and fails to concentrate police at the hot spots where crime is concentrated (Kelling et al., 1974; Sherman & Weisburd, 1995), we might speculate that mental health programs aimed at large areas like communities are not concentrating resources efficiently. The concentration of mental health problems we observed suggests that we may also want to concentrate health services.
Moreover, the identification of high levels of mental health problems at crime hot spots suggests the importance of teaming police and mental health professionals on violent crime streets. Over the last decade a number of crisis response (Crisis Intervention Teams, CIT) and “co-responder” programs have been developed that seek to team police and mental health workers to deal with emergency responses to mental health crises. Additionally, proactive police practices targeted at crime hot spots have been found to be effective in reducing crime on the street (Braga, Papachristos, & Hureau, 2014). Our data suggest the relevance of considering such co-response teams more generally for proactive problem oriented responses at crime hot spots. Such teams could play a role in providing much needed services to residents of high crime streets (see White & Weisburd, 2017).5 A focus on mental health and service needs may also provide an effective way of increasing cooperation with the police on high crime streets, and for problem solving to reduce crime and disorder problems (White & Weisburd, 2017; see also Vaughan, Hewitt, Andresen, & Brantingham, 2016).
We also noted at the outset the importance of considering selection factors in drawing conclusions about the causal relationship between mental health problems and living in crime hot spots. While one question is whether high violent crime streets have higher levels of mental health problems, another is whether the problems are caused by living on these streets. There is certainly strong theoretical justification for assuming that living on high crime streets could be a causal factor in producing mental health problems (Curry et al., 2008; Latkin & Curry, 2003; Mair et al., 2010; O’Campo et al., 2015; Ross & Mirowsky, 2001; Stockdale et al., 2007). As we noted earlier, living in places with high levels of violence is seen as likely to lead to high levels of stress which in turn increases the likelihood mental health problems (Berman et al., 1996; Buckner et al., 2004; Dupéré & Perkins, 2007; Latkin & Curry, 2003; Stockdale et al., 2007). We found that in the case of both depression and PTSD symptomology, the relationship to living in a violent crime hot spot remained statistically significant even after taking into account observable selection factors. While there may be unobservable factors that condition this relationship, our survey captured a large number of potential confounding factors. This suggests that there may be something about living on these streets, rather than the background characteristics of residents that leads to mental health problems. This is an important finding, though we recognize that our data are observational, and though we tried to take into account selection bias, potential unmeasured biases may still exist.
While background characteristics did not explain the differences we observed, we did find a strong association with cumulative violent crime in nearby areas that are likely to be part of the respondent’s routine activities, on both mental health measures. This suggests the importance of placing streets in their contexts, and recognizing that it may be the overall level of violence in the immediate surroundings of a hot spot street that influences mental health outcomes on a street. We measured this by placing a 3000 ft spatial lag from the center of each street examined. The fact that this spatial lag was a significant factor in our models suggests it is capturing important variation. Nonetheless, it may be that specific juxtapositions of streets in a small area have particular influence on social outcomes. Grannis (1998; 2005), for example, found that specific types of streets have influence on homogeneity of populations in an area. We encourage future research to explore more directly these influences.
After taking into account violence in nearby areas, living in the hot spot further aggravated PTSD symptomology (though it did not add to depression symptomology). We suspect that this reflects the importance of more immediate and frequent stresses of living on a street where violence is common. As we noted earlier, victimization is much higher on the hot spot streets, and such victimization may be a catalyst for PTSD symptoms. Our work highlights the importance of immediate and frequent stresses associated with living on a high violence street itself (Gapen et al., 2011; Garvin et al., 2013).
Conclusions
Our study comparing hot spot, cool spots and cold spots of crime reinforces the importance of place in understanding mental health problems. Following upon studies of mental health and community, suggesting a relationship between violence and mental health, we set out to examine whether there was a relationship between violent crime hot spots and mental health at a micro-geographic level. Our data show that depression symptomology and PTSD are much higher on violent crime hot spots than at other streets. This suggests the importance of targeting violent crime hot spots for mental health services. At the same time, we examined whether the large differences we observed were due to selection factors. Our data suggest that even after accounting for social characteristics of residents, those who live on violent crime hot spots are significantly more likely to evidence mental health problems. We also found that the immediate context of violence on a street is particularly important in understanding PTSD.
Our study is the first we know of to allow the examination of the relationship between specific types of mental health problems and crime at the micro-geographic level. It suggests more generally the importance of taking into account place and crime in understanding mental health. Future research will need to develop methods for unraveling the causal mechanisms underlying this relationship, and better specifying the ways in which different levels of geography interact in influencing mental health outcomes. For now, our study suggests that it is time for public health practitioners to take into account violent crime hot spots in considering how to effectively allocate health services in the city.
Supplementary Material
Acknowledgements
Funding: This work was funded by the National Institutes of Health [grant number 5R01DA032639–03, 2012].
Footnotes
In the study we examined hot spots for violent crime, and hot spots that had high rates of both violent and drug crime. Those categories are combined here. A detailed description of the data and sample selection can be found at http://cebcp.org/wp-content/cpwg/NIDA-Methodology.
110 cases had a missing value for one of the variables needed to calculate the depression or PTSD scales; 86 cases were missing at least one depression measure and 31 cases were missing at least one PTSD measure.
We created the spatial lag by first creating a centroid for each street segment in the Baltimore city street file with the violent crime counts using the BPD 2012 CFS data in ArcMap. This was done after cleaning the centerline file to remove random breaks in addition to breaks where a true intersection does not exist (e.g., a street changes name in the middle of a street, but where a true intersection with another street does not exist). Those centroids were then loaded into GeoDa to create a spatial lag for each point using a 3000 ft Euclidean distance threshold. Some researchers have emphasized the importance of Manhattan rather than Euclidean distance when assessing area influences (e.g. see Grannis, 1998, 2005). We agree with this concern for the specific geographies of a city, and recognize the importance of local factors in our identification of street segments as a key unit of study. However, we do not have qualitative information on the access points and specific nature of the street network that would allow a strong modelling of the specific geographies. At the same time, Apparicio et al. (2008) shows that the correlation between a Euclidean approach and Manhattan approach (recognizing actual street grid distances) is very high, and generally would lead to similar findings when used as a regression control.
We report these models with a spatial lag term for violent crime, but without the violent crime variable used to create the spatial lag at the hot spot itself. This is because the type of hot spot (violent crime) already takes this factor into account. We also estimated the models with a violent crime count measure at the hot spots added and found the results to be similar.
Drawing from these findings, we developed and pilot tested a new program—The Co-responder Hot Spot Outreach Team (see White and Weisburd, 2017). This program sought to recognize the importance of mental health problems in police interventions at crime hot spots. It draws from key elements of co-responder teams and CIT, as well as problem solving in crime hot spots to address mental health treatment needs of residents, prevent mental health crises, improve evaluations of police, and potentially reduce crime problems.
References
- Andresen MA & Malleson N (2011). Testing the stability of crime patterns: Implications for theory and policy. Journal of Research in Crime and Delinquency, 48, 58–82. [Google Scholar]
- Aneshensel CS, Sucoff CA (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37, 293–310. [PubMed] [Google Scholar]
- Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL Karlamangla AS, & Seeman TE (2007). Urban neighborhoods and depressive symptoms among older adults. Journal of Gerontology: Series B, 62, S52–S59. [DOI] [PubMed] [Google Scholar]
- Apparicio P, Abdelmajid M, Riva M & Shearmur R (2008). Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. International Journal of Health Geographics, 7, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babbie E.(2007). The practice of social research. 11 ed. Wadsworth, Belmont.
- Breslau N, Peterson EL, Kessler RC, & Schultz LR (1999). Short screening scale for DSM-IV Posttraumatic Stress Disorder. The American Journal of Psychiatry, 156, 908–911. [DOI] [PubMed] [Google Scholar]
- Berman SL, Kurtines WM, Silverman WK & Serafini LT (1996). The impact of exposure to crime and violence on urban youth. American Journal of Orthopsychiatry, 66, 329–336. [DOI] [PubMed] [Google Scholar]
- Black DJ (1970). Production of crime rates. American Sociological Review, 35, 733–48. [PubMed] [Google Scholar]
- Braakman N (2013). How do individuals deal with victimization and victimization risk? Longitudinal evidence from Mexico. Journal of Economic Behavior and Organization, 84, 335–44. [Google Scholar]
- Braga AA & Clarke RV (2014). Explaining high-risk concentrations of crime in the city: Social Disorganization, Crime opportunities, and important next steps. Journal of Research in Crime and Delinquency, 51, 480–498. [Google Scholar]
- Braga AA, Hureau DM, & Papachristos AV (2010). The concentration and stability of gun violence at micro places in Boston, 1980–2008. Journal of Quantitative Criminology, 26, 33–53. [Google Scholar]
- Braga AA, Hureau DM, & Papachristos AV (2011). The relevance of micro places to citywide robbery trends: A longitudinal analysis of robbery incidents at street corners and block faces in Boston. Journal of Research in Crime and Delinquency, 48, 7–32. [Google Scholar]
- Braga AA, Papachristos AV, & Hureau DM (2014). The Effects of Hot Spots Policing on Crime: An Updated Systematic Review and Meta-Analysis. Justice Quarterly, 31, 633–63. [Google Scholar]
- Brantingham PL, Brantingham PJ, (1999). A theoretical model of crime hot spot generation. Studies on Crime & Crime Prevention, 8, 7–26. [Google Scholar]
- Breslau N, Peterson EL, Kessler RC, & Schultz LR (1999). Short screening scale for DSM-IV Posttraumatic stress disorder. American Journal of Psychiatry, 156, 908–11. [DOI] [PubMed] [Google Scholar]
- Buckner JC, Beardslee WR, Bassuk EL, (2004). Exposure to violence and low-income children's mental health: Direct, moderated, and mediated relations. American Journal of Orthopsychiatry, 74, 413–23. doi: 10.1037/0002-9432.74.4.413 [DOI] [PubMed] [Google Scholar]
- Butcher F, Galanek JD, Kretschmar JM, & Flannery DJ (2015). The impact of neighborhood disorganization on neighborhood exposure to violence, trauma symptoms, and social relationships among at-risk youth. Social Science and Medicine, 146, 300–306. [DOI] [PubMed] [Google Scholar]
- Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, & Wright RJ (2008). Witnessing community violence in residential neighborhoods: A mental health hazard for urban women. Journal of Urban Health, 85, 22–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane W & Rubin D (1973). Controlling bias in observational studies. Sankyha, 35, 417–46. [Google Scholar]
- Curry A, Latkin C, Davey-Rothwell M (2008). Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Social Science & Medicine, 67, 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, & Gardner KA (2005). Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology, 114, 3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV & Mair C (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125–45. [DOI] [PubMed] [Google Scholar]
- Duany A & Plater-Zyberk E (1994). The neighborhood, the district and the corridor. In Katz P, ed. The new urbanism; New York. [Google Scholar]
- Dupéré V & Perkins DD (2007). Community types and mental health: a multilevel study of local environmental stress and coping. American Journal of Community Psychology, 39, 107–119. [DOI] [PubMed] [Google Scholar]
- Dustmann C & Fasani F (2016). The effect of local area crime on mental health. The Economic Journal, 126, 978–1017. [Google Scholar]
- Echeverría S, Diez-Roux AV, Shea S, Borrell LN & Jackson S (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health & Place, 14, 853–865. [DOI] [PubMed] [Google Scholar]
- Eck JE, Clarke RV & Guerette RT, (2007). Risky facilities: Crime concentration in homogeneous sets of establishments and facilities. Crime Prevention Studies, 21, 225–264. [Google Scholar]
- Fitzpatrick KM & Boldizar JP (1993). The Prevalence and Consequences of Exposure to Violence among African-American Youth. Journal of the American Academy of Child & Adolescent Psychiatry, 32, 424–30. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KM, Piko BF, Wright DR, & LaGory M (2005). Depressive symptomatology, exposure to violence, and the role of social capital among African American adolescents. American Journal of Orthopsychiatry, 75, 262–74. [DOI] [PubMed] [Google Scholar]
- Franco M, Diez-Roux AV, Glass TA, Caballero B & Brancati FL (2008). Neighborhood Characteristics and Availability of Healthy Foods in Baltimore. American Journal of Preventive Medicine, 35, 561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Nandi A, Tracy M, Beard J & Vlahov D (2007). Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Annals of Epidemiology, 17, 171–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gapen M, Cross D, Ortigo K, Graham A, Johnson E, Evces M, Ressler KJ, & Bekh B (2011). Perceived Neighborhood Disorder, Community Cohesion, and PTSD Symptoms Among Low-Income African Americans in an Urban Health Setting. American Journal of Orthopsychiatry, 81, 31–37. [DOI] [PubMed] [Google Scholar]
- Garvin E, Branas C, Keddem S, Sellman J, & Cannuscio C (2013). More than just an eyesore: Local insights and solutions on vacant land and urban health. Journal of Urban Health, 90, 412–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grannis R (1998). The importance of trivial streets: Residential streets and residential segregation. American Journal of Sociology, 103, 1530–1564. [Google Scholar]
- Grannis R (2005). T-communities: Pedestrian street networks and residential segregation in Chicago, Los Angeles, and New York. City & Community, 4, 295–321. [Google Scholar]
- Groff ER, Weisburd DL, & Yang S-M. (2010). Is it important to examine crime trends at a local “micro” level?: A longitudinal analysis of street to street variability in crime trajectories.” Journal of Quantitative Criminology, 26, 7–32. [Google Scholar]
- Holbrook A, Krosnick J, & Pfent A (2008). The causes and consequences of response rates in surveys by the news media and government contractor survey research firms In: Lepkowski JM, Tucker C, Brick JM, et al., eds. Advances in telephone survey methodology. New York Advances in telephone survey methodology, p. 499–528. [Google Scholar]
- Imbens G (1999). The Role of the Propensity Score in Estimating Dose-Response Functions. National Bureau of Economic Research, Cambridge. [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D (2008). Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews, 30, 101–117. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Ouimette P, Prins A, Nisco P, Lawler C, Cronkite R & Moos RH (2006). Brief report: Utility of a short screening scale for DSM‐IV PTSD in Primary Care. Journal of General Internal Medicine, 21, 65–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky LD, Subramanian SV, Kawachi I, Fay ME, Soobader M J., & Berkman LF(2005). Neighborhood contextual influences on depressive symptoms in the elderly. American Journal of Epidemiology, 162, 253–260. [DOI] [PubMed] [Google Scholar]
- Kroenke. K, Spitzer RL, & Williams JBW. (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen J, El-Geneidy A, Yasmin F (2010). Beyond the quarter mile: Re-examining travel distances by active transportation. Canadian Journal of Urban Research: Canadian Planning and Policy.;19(1) supplement:70–88. [Google Scholar]
- Latkin CA & Curry AD (2003). Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior, 44, 34–44. [PubMed] [Google Scholar]
- LaVeist TA & Wallace JM Jr. (2000). Health risk and inequitable distribution of liquor stores in African American neighborhood. Social Science & Medicine, 51, 613–7. [DOI] [PubMed] [Google Scholar]
- Linnell D, (1988). The geographic distribution of hot spots of robbery, rape, and auto theft in Minneapolis. Unpublished MA, University of Maryland, College Park. [Google Scholar]
- Lunceford JK & Davidian M (2004). Stratification and weighting via the propensity score in estimation of causal treatment effects: A comparative study. Statistics in Medicine, 19, 2937–2960. [DOI] [PubMed] [Google Scholar]
- Mair C, Diez-Roux AV, & Galea S (2008). Are neighborhood characteristics associated with depressive symptoms? A review of evidence. Journal of Epidemiology and Community Health, 62, 940–946. [DOI] [PubMed] [Google Scholar]
- Mair C, Diez-Roux AV & Morenoff J (2010). Neighborhood stressors and social support as predictors of depressive symptoms in the Chicago Community Adult Health Study. Health & Place, 16, 811–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberwittler D & Wikström PH (2009). Why small is better: advancing the study of the role of behavioral contexts in crime causation In: Weisburd D, Bernasco W, Bruinsma GJN. (Eds.), Putting Crime in its Place. Units of Analysis in Geographic Criminology. Springer, New York, NY. [Google Scholar]
- O'Campo P, Xue X, Wang MC, & Caughy M (1997). Neighborhood risk factors for low birthweight in Baltimore: A multilevel analysis. American Journal of Public Health, 87, 1113–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Campo P, Wheaton B, Nisenbaum R, Glazier RH, Dunn JR, & Chambers C (2015). The neighborhood effects on health and well-being (NEHW) study. Health & Place, 31, 65–74. [DOI] [PubMed] [Google Scholar]
- Pearson AL, Breetzke G, & Ivory V (2015). The effect of neighborhood recorded crime on fear: Does neighborhood social context matter? American Journal of Community Psychology, 56, 170–179. [DOI] [PubMed] [Google Scholar]
- Pierce G, Spaar S, & Briggs LR (1988). The character of police work: Strategic and tactical implications Boston: Center for Applied Social Research, Northeastern University. [Google Scholar]
- Robins JM, Hernán MÁ, & Brumback B, (2000). Marginal Structural Models and Causal Inference in Epidemiology. Epidemiology, 11, 550–60. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55. [Google Scholar]
- Ross CE (2000). Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior, 41, 177–187. [PubMed] [Google Scholar]
- Ross CE & Mirowsky J (2001). Neighbourhood disadvantage, disorder, and health. Journal of Health and Social Behavior, 42, 258–76. [PubMed] [Google Scholar]
- Sherman LW (1995). Hot spots of crime and criminal careers of places. In: Eck J & Weisburd DL (eds) Crime and Place, vol 4 Willow Tree Press, Monsey. [Google Scholar]
- Sherman LW. & Eck JE, (2003). Policing for crime prevention In: Farrington DP, MacKenzie DL, Sherman LW, et al. , eds. Evidence-Based Crime Prevention. Routledge, New York. [Google Scholar]
- Sherman LW, Gartin PR, & Buerger ME, (1989). Hot spots of predatory crime: Routine activities and the criminology of place. Criminology, 27, 27–56. [Google Scholar]
- Sherman LW & Weisburd DL, (1995). General deterrent effects of police patrol in crime ‘hot spots’: A randomized, controlled trial. Justice Quarterly, 12, 625–48. [Google Scholar]
- Silver E, Mulvey EP, & Swanson JW (2002). Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Social Science & Medicine, 55, 1457–70.Skogan, W. & Frydl, K. (2004). Fairness and effectiveness in policing: The evidence. National Academy of Science. [DOI] [PubMed] [Google Scholar]
- Simons RL, Murry V, McLoyd V, Lin KH (2002). Discrimination, crime, ethnic identity, and parenting as correlates of depressive symptoms among African American children: a multilevel analysis. Development and Psychopathology, 14, 371–393. [DOI] [PubMed] [Google Scholar]
- Smith DG & Tolan P, (1998). The role of exposure to community violence and developmental problems among inner-city youth. Development and Psychopathology, 10, 101–16. [DOI] [PubMed] [Google Scholar]
- Steenbeek W Weisburd, D. (2016). Where the Action is in Crime: An Examination of Variability of Crime Across Different Spatial Units in The Hague, 2001–2009. Journal of Quantitative Criminology 32 (3): 449–469. [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L & Sherbourne CD (2007). The importance of social context: Neighborhoods stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social Science & Medicine, 65, 1867–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RB (1997). Social order and disorder of street blocks and neighborhoods: ecology, microecology, and the systemic model of social disorganization. Journal of Research in Crime and Delinquency, 34, 113–155. [Google Scholar]
- U.S. Census Bureau. Accessed 20 July 2015 U.S. Census, State, and County QuickFacts. http://quickfacts.census.gov/qfd/states/24/24510.html.
- Vaughan AD, Hewitt AN, Andresen MA, & Brantingham PL (2016). Exploring the role of environmental context in the spatial distribution of calls-for-service associated with emotionally disturbed persons. Policing, 10, 121–133. [Google Scholar]
- Wandersman A & Nation M (1998). Urban neighborhoods and mental health. American Psychologist, 53, 647–56. [PubMed] [Google Scholar]
- Weich S, Twigg L, Holt G, Lewis G, & Jones K (2003). Contextual risk factors for the common mental disorders in Britain: a multilevel investigation of the effects of place. Journal of Epidemiology & Community Health, 57, 616–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisburd DL (2015). The law of crime concentration and the criminology of place. Criminology, 53, 133–57. [Google Scholar]
- Weisburd D, Bushway S, Lum C & Yang S-M. (2004). Trajectories of crime at places: A longitudinal study of street segments in the city of Seattle. Criminology, 42, 283–322. [Google Scholar]
- Weisburd DL & Green L, (1995). Policing drug hot spots: The Jersey City drug market analysis experiment. Justice Quarterly, 12, 711–35. [Google Scholar]
- Weisburd DL, Groff ER, & Yang S-M(2012). The Criminology of Place: Street segments and our understanding of the crime problem. Oxford University Press, New York. [Google Scholar]
- Weisburd DL, Groff ER & Yang SM (2014). Understanding and controlling hot spots of crime: The importance of formal and informal social controls. Prevention Science, 15, 31–43. [DOI] [PubMed] [Google Scholar]
- Wheeler AP, Worden RE, & McLean SJ (2016). Replicating group- based trajectory models of crime at micro- places in Albany, NY. Journal of Quantitative Criminology, 32, 589–612. [Google Scholar]
- White M, Kasl SV, Zahner GE, & Will JC (1987). Perceived Crime in the Neighborhood and Mental Health of Women and Children. Environment and Behavior, 19, 588–613. [Google Scholar]
- White C & Weisburd D (2017). A Co-Responder Model for Policing Mental Health Problems at Crime Hot Spots: Findings from a Pilot Project. Policing: A Journal of Policy and Practice, 1–16. doi: 10.1093/police/pax010. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


