Abstract
An early warning system for dengue is meant to predict outbreaks and prevent dengue cases by aiding timely decision making and deployment of interventions. However, only a system which is accepted and utilised by the public would be sustainable in the long run. This study aimed to explore the perception and attitude of the Malaysian public towards a dengue early warning system. The sample consisted of 847 individuals who were 18 years and above and living/working in the Petaling District, an area adjacent to Kuala Lumpur, Malaysia. A questionnaire consisting of personal information and three sub-measures of; i) perception, ii) attitude towards dengue early warning and iii) response towards early warning; was distributed to participants. We found that most of the respondents know about dengue fever (97.1%) and its association with climate factors (90.6%). Most of them wanted to help reduce the number of dengue cases in their area (91.5%). A small percentage of the respondents admitted that they were not willing to be involved in public activities, and 64% of them admitted that they did not check dengue situations or hotspots around their area regularly. Despite the high awareness on the relationship between climate and dengue, about 45% of respondents do not know or are not sure how this can be used to predict dengue. Respondents would like to know more about how climate data can be used to predict a dengue outbreak (92.7%). Providing more information on how climate can influence dengue cases would increase public acceptability and improve response towards climate-based warning system. The most preferred way of communicating early warning was through the television (66.4%). This study shows that the public in Petaling District considers it necessary to have a dengue warning system to be necessary, but more education is required.
Introduction
Dengue is transmitted by infected female mosquitoes; Aedes albopictus & Aedes aegypti, the latter being the primary vector. These mosquitoes feed in the daytime with the possibility of multiple-biting of people during the feeding period. A study in rural Thailand showed that 81% of multiple blood meals during the rainy season occurred among those living in the same house [1]. Symptoms of dengue fever usually lasts for 2–7 days, and often include high fever (up to 40°C/104°F), accompanied by one or several of the following manifestations: pain behind the eyes, severe headache, rash, muscle and joint pains, and vomiting [2].
Worldwide estimation of the dengue burden from 1990–2013 yields a range of 50–100 million dengue cases per year [3]. In Southeast Asia, dengue poses an immense disease and economic burden which exceeds that for upper respiratory infections and Japanese encephalitis [4]. In Malaysia, it is regarded as the most important communicable disease surpassing HIV/AIDS and tuberculosis [5]. In 2017, there were 83,374 dengue cases in Malaysia with more than half (n = 45,026, 54%) occurring in the state of Selangor [6].
Currently there is no specific treatment for dengue fever, but proper hospital care is essential in some cases [7]. Since the lack of effectiveness and the side-effects of the dengue vaccine makes vaccination a non-viable option for the moment, vector control and surveillance are still the dominant measures in dengue prevention [8].
Dengue transmission is influenced by various factors which include weather or climate, host immunity, vector capacity and dengue control effort [9]. Several studies have documented the link between climate and dengue transmission [10–13]. The influence of weather and climate variability on dengue fever is through their direct impacts on the biological or life cycles of Aedes mosquitoes and the length of the extrinsic incubation period of the dengue virus in mosquitoes [14]. The possibility of using weather predictors such as weekly mean temperature and cumulative rainfall to forecast weekly dengue incidence up to 16 weeks in advance has been demonstrated before [15]. Thus, a climate-based dengue early warning system could potentially be useful with ample time for the community to take necessary actions.
A prototype dengue early warning system was developed to produce probabilistic forecasts of dengue risk three months ahead of the 2014 World Cup in Brazil for over 550 ‘microregions’. The early warnings were disseminated to the general public and visitors travelling to Brazil [16]. Evaluation of this system suggested that an early warning model framework may be useful for public health services, not only ahead of mass gatherings, but also before the peak dengue season each year, to control potentially explosive dengue epidemics [16, 17],
Recently, a study in Singapore demonstrated the application of a forecasting tool in dengue control program [18]. This model comprises a “real-time” schedule, with data being updated weekly and predictions sent out to the Ministry of Health and the Environmental Public Health Operations Department of the National Environment Agency. Their forecasts have been accurate enough to guide public health interventions and hospital bed management. It has facilitated early risk communication to the public and the advanced launch of the annual Dengue Campaign two months ahead of its traditional launch [18]. Apart from that, the World Health Organization (WHO) has developed an early warning system algorithm and support system which is being tested in some countries. This further highlights the importance of our present study as the WHO system also needs to take into account factors of population’s acceptance, attitude and perceptions [19].
The main goal of a dengue early warning system would be to provide prior announcement to the public and government bodies of any possible dengue outbreak to allow proper preventive measures to be taken. For such a system to be effective, a timely and understandable communication of the warning and the capacity to act on the warning, particularly at the local level are crucial. As shown through other warning systems (e.g. famine, hurricanes), a warning system will not work if there is a lack of willingness and capacity to respond to it [20, 21]. A review of early warning systems conducted for World Vision has identified systemic barriers of converting information into actions [22]. Insufficient warning interpretation at the community level; a lack of guidelines for appropriate actions; disagreement on the accuracy and appropriateness of early warning systems; and a lack of understanding on coping strategies were among internal barriers identified in the review [22]. Therefore, the perception of the community towards dengue early warning and the willingness to take preventive measures in their home environment are important determinants of their participation in community-based programs in response to the early warning system. Thus, it is important to know the public’s perception, attitude and their response towards a dengue early warning system.
Materials and methods
Participants and study area
A cross-sectional study was conducted from May 2017 to July 2017 in the Petaling District which is situated in the Malaysian state of Selangor. Petaling District has one of the highest number of dengue cases in Malaysia. The target population were members of the public studying, working, or living in the Petaling District. Participants were selected from a few public places, such as shopping malls and post office, in order to capture participants from various backgrounds in the community. Participants were approached by enumerators at various times of the day during data collection. Only those who consented were included in this study. Those aged below 18 years old were excluded. A total of 1,000 dual language (English and Malay) self-administered questionnaires were distributed. Both local and foreigners were included in this study.
Instrument
The questionnaire (S1 Text) was developed by this research team which consist of experts in public health, environmental health, and dengue modelling. The translation of the questionnaires from English to Malay language was done by two researchers from the University of Malaya and the final dual language questionnaire was reviewed by the entire research team. The team members checked the translated questionnaires and any differences raised were discussed and corrected accordingly. The final version of the questionnaire was pilot tested in a community with similarities to the study population.
The questionnaire consisted of a socio-demographic section and a three other sections. Section A) was on perception, Section B) on attitude and Section C) was on the response towards an early warning system. Section A (perception) consisted of 18 questions, where participants were asked about their knowledge of dengue infection, prevention and the effects of climate change on dengue. Section B (attitude) consisted of 14 questions on the attitude towards a dengue early warning system. Finally, Section C consisted of 18 questions on the response to and effectiveness of an early warning system.
The three sections consist of closed-ended questions with ‘yes’, ‘no’, ‘don’t know’, ‘not sure’, or a multiple choice question selection, where applicable. These sections have Cronbach’s alpha values of more than 0.60 (Section A = 0.716, Section B = 0.619, and Section C = 0.795). A review article on the application of Cronbach’s alpha has identified wide range of interpretation of alpha values. Most researchers described a value of >0.6 as acceptable and sufficient, with alpha coefficients that are less than 0.5 as unacceptable [23]. Thus the internal consistency of this questionnaire was considered acceptable. Test re-test reliability of the questionnaire was performed among a sample of 50 participants that had similar characteristics to the study population. The gap between the first and second testing was less than 5 days. Analysis using intraclass correlation coefficient (ICC) showed that all items achieved moderate to excellent reliability with ICC ranging from 0.6 to 1.0.
Ethical approval
The study was approved by the Medical Ethics Committee of the University of Malaya Medical Centre (MECID: 20143–68). The respondents were given an explanation of the objectives and benefits of the study, with verbal and written consent obtained from those who agreed to participate.
Data entry and analyses
All statistical analyses were performed using the IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Double data entry was performed to ensure data quality. Data were entered into two separate files and then cross-checked for discrepancies. Any discrepancies and missing data were referred back to the original questionnaire (hard copy). Frequency and percentages was calculated for categorical variables (e.g. gender, race), while mean and standard deviation was calculated for continuous variables (e.g. age, income). The association between categorical variables were measured using chi-square test. P-values of < 0.05 were considered significant.
Results
Socio-demographic characteristics
Out of 1000 questionnaires being distributed, only 847 were filled completely, giving a response rate of 84.7%. Most of the respondents had never had dengue fever (80.8%) but do know people who had been infected with dengue (78.1%).
The respondents were mostly females (64.7%) with an average age of 26.90 ± 9.58 years old (age range: 18–71 years old). Almost all the participants were Malaysians (98.8%) and the majority were Malays (75.7%). Less than half of the respondents lived in the Petaling District (42.8%), while the rest of them were either studying or working in the district. Of those who lived in Petaling, only 35.8% had been living in the area for more than 5 years. Many participants had at least a university degree (46.9%) and most were single (70.0%). Most of the respondents were students (52.7%), the rest were private sector workers (19.7%), civil servants (13.9%), self-employed (9.6%), unemployed (3.3%) and others (0.8%). The majority of the respondents claimed never to have had dengue fever (80.8%), but have known persons who have been infected with dengue (78.1%). Two-thirds of the respondents had less than 5 people in their household (67.8%). Further details about the demographic data of the participants are shown in Table 1.
Table 1. Socio-demographic characteristics of participants (n = 847) in Petaling District as of July 2017.
| Variable | Variable | N (%) |
|---|---|---|
| 1. Gender (n = 846) | Male | 299 (35.3) |
| Female | 547 (64.7) | |
| 2. Age (n = 823) | ≤40 years old | 751 (91.3) |
| >40 years old | 72 (8.7) | |
| 3. Nationality (n = 835) | Malaysian | 825 (98.8) |
| Non-Malaysian | 10 (1.2) | |
| 4. Race (n = 826) | Malay | 625 (75.7) |
| Chinese | 64 (7.7) | |
| Indian | 94 (11.4) | |
| Others | 43 (5.2) | |
| 5. Do you live in Petaling District? (n = 843) | Yes | 361 (42.8) |
| No | 482 (57.2) | |
| 5(a). Do you study/work in Petaling District? (n = 635) | Yes | 425 (66.9) |
| No | 210 (33.1) | |
| 5(b). Period living in Petaling District (n = 497) | < 1 year | 110 (22.1) |
| > 1–3 years | 145 (29.2) | |
| > 3–5 years | 64 (12.9) | |
| > 5 years | 178 (35.8) | |
| 5(c). Do you own your current residence? (n = 524) | Yes | 196 (37.4) |
| No | 328 (62.6) | |
| 6. What type of house do you currently reside in? (n = 834) | Individual house or bungalow | 79 (9.5) |
| Twin/semi-detached | 58 (7.0) | |
| Terrace house | 289 (34.7) | |
| Flat | 112 (13.4) | |
| Apartment/condominium | 185 (22.2) | |
| Shop house/long house/others | 111 (13.2) | |
| 7. Highest education level (n = 838) | No formal education | 3 (0.4) |
| Primary school | 5 (0.6) | |
| Secondary school | 150 (17.9) | |
| Diploma | 236 (28.2) | |
| Degree | 393 (46.9) | |
| Master’s/PhD | 51 (6.1) | |
| 8. Marital status (n = 842) | Single | 589 (70.0) |
| Married | 239 (28.4) | |
| Divorced | 9 (1.1) | |
| Widow/widower | 5 (0.6) | |
| 9. Occupation (n = 837) | Student | 441 (52.7) |
| Self-employed | 80 (9.6) | |
| Government workers | 116 (13.9) | |
| Private workers | 165 (19.7) | |
| Unemployed | 28 (3.3) | |
| Other (retired) | 7 (0.8) | |
| 10. Number of people in household (n = 818) | ≤ 5 people > 5 people |
555 (67.8) 263 (32.2) |
| 11. Average monthly income (n = 458) | ≤ MYR3000 > MYR3000 |
323 (70.5) 135 (29.5) |
| 12. Average household monthly income (n = 562) | ≤ MYR6000 > MYR6000 |
389 (69.2) 173 (30.8) |
*MYR = Malaysian Ringgit
Perception towards a climate-based dengue early warning
Table 2 summarizes the perception of the respondents towards an early warning system (Section A). The majority of respondents knew what dengue fever is (97.1%) and that it could lead to death (96.0%). More than half of them admitted to having sufficient knowledge on dengue prevention (64.1%) and would be very concerned on if they were to get an infection more than once (81.9%). Most agreed that mosquito repellents (68.2%) and removing breeding sites (83.7%) were important in protecting against dengue. The majority (90.6%) of respondents agreed that climate change affects human health and 68.9% agreed that global warming increases the chances of dengue outbreaks. They also agreed that the number of dengue cases increases after rainy days (76.2%), and that increasing temperature elevates the number of dengue cases in their area (57.8%). Finally, a majority of respondents thought that an early warning would be useful in informing the community so that timely preventive actions could be taken (80.6%).
Table 2. Perception towards an early warning system (Section A).
| Variable | N (%) | |
|---|---|---|
| 1. Do you know what dengue fever is? (n = 841) | Yes | 817 (97.1) |
| No | 24 (2.9) | |
| 2. Do you think dengue fever can cause mortality? (n = 844) | Yes | 810 (96.0) |
| No | 11 (1.3) | |
| Don’t know | 23 (2.7) | |
| 3. Do you think you and your family members could be infected with dengue fever? (n = 836) | Yes | 661 (79.1) |
| No | 62 (7.4) | |
| Don’t know | 113 (13.5) | |
| 4. In your opinion, what is your risk of being infected with dengue fever? (n = 838) | Low | 188 (22.4) |
| Medium | 457 (54.5) | |
| High | 193 (23.0) | |
| 5. Do you think you have sufficient knowledge of the ways to prevent yourself from dengue infection? (n = 844) | Yes | 541 (64.1) |
| No | 208 (24.6) | |
| Don’t know | 95 (11.3) | |
| 6. Do you think the dengue situation is serious in the area you live in? (n = 845) | Yes | 384 (45.4) |
| No | 296 (35.0) | |
| Don’t know | 165 (19.5) | |
| 7. Do you think it is possible to be infected with dengue many times? (n = 845) | Yes | 418 (49.5) |
| No | 188 (22.2) | |
| Don’t know | 239 (28.3) | |
| 8. How concerned would you be if it was the second time or more for your parents/children to be infected with dengue? (n = 843) | Very concerned | 690 (81.9) |
| Concerned | 112 (13.3) | |
| Slightly concerned | 31 (3.7) | |
| Not concerned | 10 (1.2) | |
| 9. Which methods can be used to protect yourself and your family members from dengue infection? (You may tick several options) (n = 846) | ||
| 9.1) Nothing | Yes | 8 (0.9) |
| No | 838 (99.1) | |
| 9.2) Don’t know | Yes | 33 (3.9) |
| No | 813 (96.1) | |
| 9.3) Mosquito repellent | Yes | 577 (68.2) |
| No | 269 (31.8) | |
| 9.4) Insecticide | Yes | 352 (41.6) |
| No | 494 (58.4) | |
| 9.5) Bed nets | Yes | 395 (46.7) |
| No | 451 (53.3) | |
| 9.6) Remove mosquito breeding sites | Yes | 708 (83.7) |
| No | 138 (16.3) | |
| 9.7) Others | Yes | 116 (13.7) |
| No | 730 (86.3) | |
| 10. Do you think the global climate is changing? (n = 845) | Yes | 708 (83.8) |
| No | 43 (5.1) | |
| Don’t know | 94 (11.1) | |
| 11. Do you think the climate change does not influence Malaysia climate? (n = 844) | Yes | 189 (22.4) |
| No | 503 (59.6) | |
| Don’t know | 152 (18.0) | |
| 12. Do you think the climate change affects human health? (n = 844) | Yes | 765 (90.6) |
| No | 25 (3.0) | |
| Don’t know | 54 (6.4) | |
| 13. Do you think the global warming could increase the risk of dengue outbreaks? (n = 842) | Yes | 580 (68.9) |
| No | 73 (8.7) | |
| Don’t know | 189 (22.4) | |
| 14. Do you think the climatic factors may affect the life cycle of mosquitoes but not dengue cases? (n = 841) | Yes | 405 (48.2) |
| No | 198 (23.5) | |
| Don’t know | 238 (28.3) | |
| 15. Do you think the number of dengue cases increases after rainy days? (n = 842) | Yes | 642 (76.2) |
| No | 64 (7.6) | |
| Don’t know | 136 (16.2) | |
| 16. Do you think the increasing temperature elevates the number of dengue cases in your area? (n = 843) | Yes | 487 (57.8) |
| No | 110 (13.0) | |
| Don’t know | 246 (29.2) | |
| 17. Do you think the information about previous temperature and rainfall can be used to predict dengue outbreak in future? (n = 842) | Yes | 506 (60.1) |
| No | 87 (10.3) | |
| Don’t know | 249 (29.6) | |
| 18. Do you think an early warning is a useful tool for community to take preventive actions to avoid possible infection within sufficient time? (n = 841) | Yes | 678 (80.6) |
| No | 63 (7.5) | |
| Don’t know | 100 (11.9) | |
Attitudes towards a climate-based dengue early warning
The majority of respondents wanted to help reduce the number of dengue cases in their area (91.5%). They also agreed that an early warning system was important in preventing an outbreak (94.4%) and that an advanced warning system helps in avoiding potential dengue infections (90.5%). The community needs public education about the warning system (86.6%) and want to know more about how changes in climate can be used to predict a dengue outbreak (92.7%). Most respondents would like to receive a periodical update on information of dengue early warning (91.7%) and they chose the television (66.4%) as a method to receive early warning of dengue (Table 3).
Table 3. Attitude towards an early warning system (Section B).
| Variable | N (%) | |
|---|---|---|
| 19. I want to help to reduce number of dengue cases in my area (n = 844) | Yes | 772 (91.5) |
| No | 12 (1.4) | |
| Not sure | 60 (7.1) | |
| 20. An early warning is important for the prevention of dengue outbreak (n = 843) | Yes | 796 (94.4) |
| No | 19 (2.3) | |
| Not sure | 28 (3.3) | |
| 21. It is possible to predict dengue outbreak using climate (n = 843) | Yes | 461 (54.7) |
| No | 80 (9.5) | |
| Not sure | 302 (35.8) | |
| 22. A warning of dengue in advance helps us to avoid potential dengue infections (n = 844) | Yes | 764 (90.5) |
| No | 23 (2.7) | |
| Not sure | 57 (6.8) | |
| 23. I will only believe a dengue early warning if it is based on risk factors other than climate (n = 840) | Yes | 426 (50.7) |
| No | 414 (49.3) | |
| 24. I will believe an early warning only if the information is provided by the government agency (n = 843) | Yes | 494 (58.6) |
| No | 349 (41.4) | |
| 25. The government agency should include information of early warning of dengue outbreak as and when they update dengue situations for the public (n = 838) | Yes | 776 (92.6) |
| No | 16 (1.9) | |
| Not sure | 46 (5.5) | |
| 26. We do not need an early warning since weekly dengue situations for my area is available online or social media (n = 839) | Yes | 112 (13.3) |
| No | 556 (66.3) | |
| Not sure | 171 (20.4) | |
| 27. It is a waste of time and efforts on dengue control if the predicted risk of dengue outbreak does not come true (n = 839) | Yes | 129 (15.4) |
| No | 571 (68.1) | |
| Not sure | 139 (16.6) | |
| 28. It is pointless for me to take action even with early dengue warning since my neighbours will not (n = 836) | Yes | 232 (27.8) |
| No | 604 (72.2) | |
| 29. The community in my area needs public education about dengue early warning (n = 835) | Yes | 723 (86.6) |
| No | 41 (4.9) | |
| Not sure | 71 (8.5) | |
| 30. I want to know more about how climate can be used to predict a dengue outbreak (n = 834) | Yes | 773 (92.7) |
| No | 61 (7.3) | |
| 31. I would like to receive a periodical update on information of dengue early warning (n = 833) | Yes | 764 (91.7) |
| No | 69 (8.3) | |
| 32. In what way, would you like to receive an early warning for dengue? (n = 836) | ||
| 32.1) Mobile app | Yes | 354 (42.3) |
| 32.2) SMS | Yes | 301 (36.0) |
| 32.3) Radio | Yes | 407 (48.7) |
| 32.4) Television | Yes | 555 (66.4) |
| 32.5) Facebook | Yes | 414 (49.5) |
| 32.6) Twitter | Yes | 239 (28.6) |
| 32.7) Instagram | Yes | 261 (31.2) |
| 32.8) Other media | Yes | 71 (8.5) |
| 8 (19.0) | ||
| Newspaper | 18 (42.9) | |
| Official announcements/news/campaigns/pamphlets | 9 (21.4) | |
| Social messaging apps (e.g. We Chat, WhatsApp) | 7 (16.7) | |
Response towards a climate-based dengue early warning
Table 4 shows the response of the respondents towards an early dengue warning system. Most respondents do not check the dengue situation in their area (64.6%) but are ready to take extra action if the dengue risk in their area increases (87.5%). After receiving an early warning of dengue outbreak, most will avoid outdoor activities at dawn/dusk (83.6%) and will share the information with others (92.5%).
Table 4. Response towards an early warning system (Section C).
| Variable | N (%) | |
|---|---|---|
| 33. I check current dengue situations or hotspots around my area regularly (n = 838) | Yes | 297 (35.4) |
| No | 541 (64.6) | |
| 34. I do not know what to do if someone informs me that it is very likely to have a dengue outbreak in the near future (n = 837) | Yes | 241 (28.8) |
| No | 366 (43.7) | |
| Not sure | 230 (27.5) | |
| 35. I will take extra action to prevent dengue infection if I know the risk of dengue is increasing in my area (n = 838) | Yes | 733 (87.5) |
| No | 32 (3.8) | |
| Not sure | 73 (8.7) | |
| 36. After I receive an early warning of dengue outbreak from the government agency, I will | ||
| 36.a) Increase source reduction activities (n = 832) | Yes | 590 (70.9) |
| No | 77 (9.3) | |
| Not sure | 165 (19.8) | |
| 36.b) Avoid outdoor activities at dawn or dusk (n = 836) | Yes | 699 (83.6) |
| No | 70 (8.4) | |
| Not sure | 67 (8.0) | |
| 36.c) Share information with others (n = 837) | Yes | 774 (92.5) |
| No | 25 (3.0) | |
| Not sure | 38 (4.5) | |
| 36.d) Request chemical fogging (n = 836) | Yes | 664 (79.4) |
| No | 58 (6.9) | |
| Not sure | 114 (13.6) | |
| 36.e) Call local authorities (n = 835) | Yes | 542 (64.9) |
| No | 125 (15.0) | |
| Not sure | 168 (20.1) | |
| 36.f) Use mosquito net (n = 837) | Yes | 538 (64.3) |
| No | 167 (20.0) | |
| Not sure | 132 (15.8) | |
| 37. I need to know how severe the predicted dengue outbreak will be in order to decide whether preventive measures are required (n = 840) | Yes | 606 (72.1) |
| No | 145 (17.3) | |
| Not sure | 89 (10.6) | |
| 38. I will stop action to prevent dengue infection if I know the risk of dengue in my area is low (n = 840) | Yes | 211 (25.1) |
| No | 629 (74.9) | |
| 39. The government agency will conduct mosquito control program after they receive an early warning of dengue, so individual household does not need to do anything (n = 837) | Yes | 193 (23.1) |
| No | 524 (62.6) | |
| Not sure | 120 (14.3) | |
| 40. Removal of mosquito breeding sites at my premises will reduce the chance of dengue infections among my family members (n = 837) | Yes | 679 (81.1) |
| No | 82 (9.8) | |
| Not sure | 76 (9.1) | |
| 41. The local authority has already provided sufficient effort on dengue control in my area (n = 839) | Yes | 368 (43.9) |
| No | 249 (29.7) | |
| Not sure | 222 (26.5) | |
| 42. Chemical fogging by the local authority is good enough for us to prevent from dengue infection (n = 837) | Yes | 316 (37.8) |
| No | 347 (41.5) | |
| Not sure | 174 (20.8) | |
| 43. It is not my responsibility to remove mosquito breeding sites in my residence (n = 838) | Yes | 135 (16.1) |
| No | 703 (83.9) | |
| 44. It is the responsibility of my family member to remove mosquito breeding sites in my residence (n = 839) | Yes | 732 (87.2) |
| No | 107 (12.8) | |
| 45. It is necessary to continue the removal of mosquito breeding at home even during the period when there’s no dengue outbreak (n = 838) | Yes | 766 (91.4) |
| No | 24 (2.9) | |
| Not sure | 48 (5.7) | |
| 46. I can help to reduce dengue cases in my area by removing mosquito breeding sites at home (n = 839) | Yes | 763 (90.9) |
| No | 29 (3.5) | |
| Not sure | 47 (5.6) | |
| 47. Dengue outbreak in my community can be controlled if every household is committed to remove mosquito breeding sites (n = 839) | Yes | 780 (93.0) |
| No | 17 (2.0) | |
| Not sure | 42 (5.0) | |
| 48. I will take part in a public activity for dengue control or removal of mosquitoes breeding sites (n = 836) | Yes | 672 (80.4) |
| No | 35 (4.2) | |
| Not sure | 129 (15.4) | |
| 49. In my opinion, who should be responsible for preventing the spread of dengue disease? (You may tick several options) (n = 837) | ||
| 49.1) Health authority | Yes | 707 (84.5) |
| 49.2) Local council | Yes | 595 (71.1) |
| 49.3) Community leaders | Yes | 551 (65.8) |
| 49.4) Every household | Yes | 707 (84.5) |
| 49.5) I don’t think control actions are needed | Yes | 27 (3.2) |
| 50. In your opinion, what is the most effective method to reduce dengue infections in your area? (n = 838) | ||
| 50.1) Search and destroy mosquito breeding sites | Yes | 726 (86.6) |
| 50.2) Prevent from mosquito bites | Yes | 260 (31.0) |
| 50.3) Chemical fogging | Yes | 440 (52.5) |
| 50.4) Don’t know | Yes | 26 (3.1) |
The majority of respondents agreed that removal of mosquito breeding sites in their premises would reduce the chance of dengue infections among their family members (81.1%) and that it was their responsibility to remove mosquito breeding sites in their residence (87.2%). They mostly agreed that outbreaks could be controlled if every household played a role in removing breeding sites (93.0%). They were also willing to participate in a public activity for dengue control or removal of mosquitoes breeding sites (80.4%). The respondents thought that both the health authority (84.5%) and the household (84.5%) should be responsible for preventing the spread of dengue disease, through the search and destruction of mosquito breeding sites (86.6%).
Socio-demographic factors associated with (i) Perception of the usefulness of an early warning for community to take timely preventive action; and (ii) Knowledge on actions to be taken following a notice on future dengue outbreak
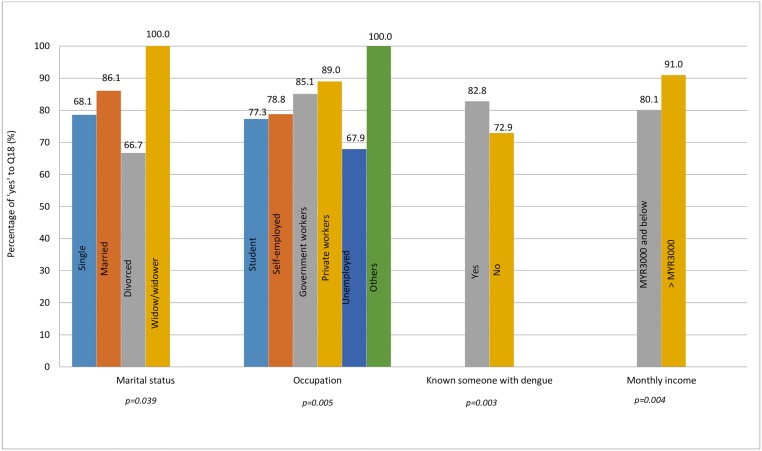
Of the demographic variables, there is a significant association between marital status, occupation, knowing someone who’s been infected with dengue, and average monthly income with Q18 (the perception that an early warning is a useful tool for community to take preventive actions to avoid possible infection within sufficient time) (Fig 1).
Fig 1. Significant demographic factors associated with the usefulness of an early warning to take timely preventive action.
Living in the Petaling District was the only significant factor associated with Q34 (the respondents’ knowledge on what to do if there is information regarding future dengue outbreak) with p-value of 0.004.
Association of Section A with (i) Perception of the usefulness of an early warning for community to take timely preventive action; and (ii) Knowledge on actions to be taken following a notice on future dengue outbreak
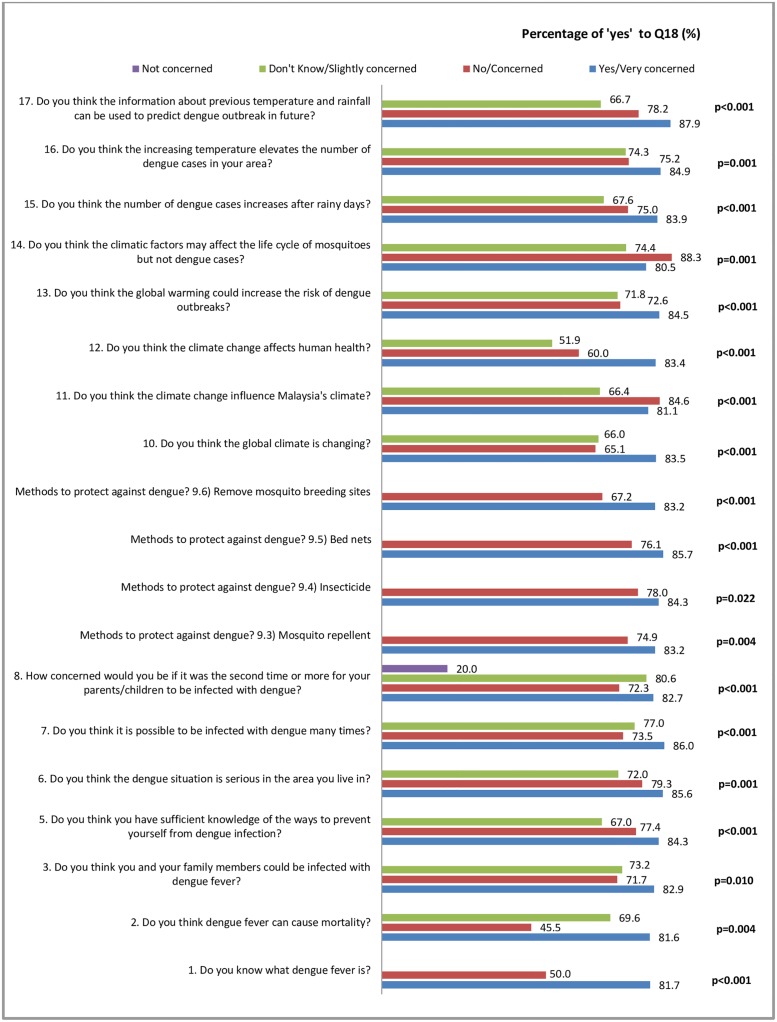
Most of the questions under perception (Section A) showed significant associations with Q18 (the perception that an early warning is a useful tool for community to take preventive actions to avoid possible infection within sufficient time) (Fig 2).
Fig 2. Significant factors in Section A associated with the usefulness of an early warning to take timely preventive action.
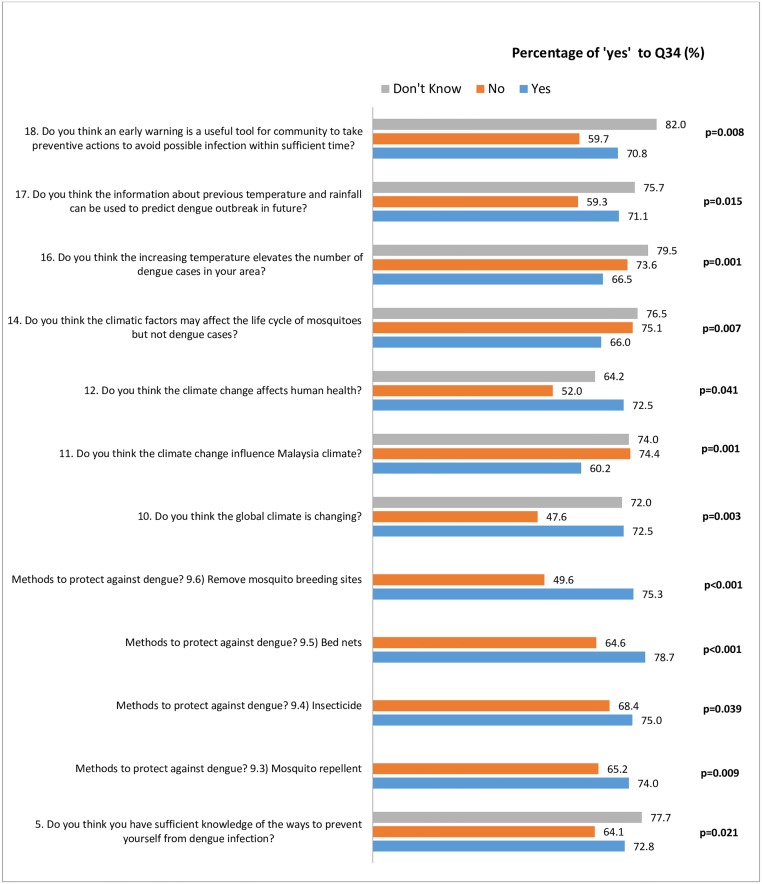
A similar pattern of association can also be seen with Q34 (the respondents’ knowledge on what to do if there is information regarding future dengue outbreak) (Fig 3).
Fig 3. Significant factors in Section A associated with knowledge on actions to be taken following a notice on future dengue outbreak.
Discussion
Knowledge on dengue and early warning system
In this study, more than half (64.1%) of the respondents think that they have sufficient knowledge to prevent dengue. They chose removal of breeding sites and mosquito repellent as the most effective methods in preventing dengue. Students and those living in the rural areas of Malaysia also have previously been shown to have good knowledge about dengue [24,25]. In terms of attitude, we found that the respondents wanted to help in reducing dengue cases. They will also share dengue information with others and will avoid outdoor activities at dawn/dusk. However, there was a small percentage of the respondents who admitted to not willing to be involved with public activities. This study also found that 64% of the respondents revealed that they did not check dengue situations or hotspots around their area regularly. This is important as public ignorance have been associated with the spread of dengue epidemics [26]. A study in China showed that participation of both the community and related department have made an exceptional difference in their dengue outbreak control. This participation includes leadership enhancement (by having a dengue control committee), daily risk assessment, and the elimination of mosquito/larvae breeding sites in high risk areas [27].
Most respondents agreed that early warning was important for the prevention of dengue outbreak; however more education about the warning system was needed. We also found that the respondents chose television as a way to receive dengue early warning. This is consistent with previous studies in Malaysia where the respondents chose television/radio as their main information source about dengue [25,28]. A good and continuous campaign about dengue prevention practices among the public is necessary as there is no specific treatment for dengue. Efforts taken by the government would be useless if there is no action taken by the public themselves. This highlights the importance of preventive actions against dengue to be made by both the public and the health authorities in Malaysia. Having better knowledge of dengue was associated with better dengue prevention practices among Malaysian public [29], including the Orang Asli (aboriginal) community [30].
Dengue and climate
Results revealed that the respondents knew that climatic changes affect human health and that the global warming increases the chances of dengue outbreaks. They were aware that rainy days and increasing temperature contributed to an increase in dengue cases. Association between climatic factors (rainfall, humidity, temperature) and increasing dengue cases have been reported in previous studies [9, 31–34]. The acceleration of mosquito development stages following an elevation in temperature increases dengue transmission. Furthermore the pooling of water due to increased rainfall contributes to an increase in the number of breeding sites for mosquitoes [15]. Humid weather allows results in perfect conditions for dengue vectors to flourish [35]. A study in Thailand showed that humidity amplified the viable transmission range of dengue at a certain range of temperature—80% of dengue cases occurred at mean temperatures of 27–29.5°C and mean humidity of >75% [36]. A study by Cheong et al (2013) in Malaysia reported a positive association between the relative risk of dengue cases with, i) increased minimum temperature of 25.4–26.5°C with delay in effect by 51 days, and ii) bi-weekly accumulated rainfall of 215–302 mm with delay in effect by 26–28 days [37].
Despite having awareness on relationship between climate and dengue, about 45% of respondents do not know or are not sure this can be used to predict dengue. Providing more information on how climate can influence dengue cases would increase public acceptability and improve response towards a climate-based warning system.
Dengue early warning system
Generally, the objective of a disease warning system is to prepare both the public health officials and the community with as much prior information as possible about the probability of a dengue outbreak, highlighting particular areas where it is likely to take place, so that the best response action can be planned [38]. By having a prior alert, it is hoped that policy makers would be able to draft the best preventive/management plan to face an upcoming predicted outbreak and reduce unnecessary fogging in some areas.
Through this study, we found that the respondents agreed that an advanced warning from the system would be useful in avoiding dengue infections by allowing them more time to take preventive actions (e.g. removing breeding sites). They are ready to take action should there be an increased dengue risk in their community.
Due to dengue’s high health and economic burden to the country, having an early warning system would allow for more cost-effective and efficient vector control efforts [19]. In Singapore, 42–59% of its total dengue economic burden cost are dedicated for control measures [39]. It was reported that in 2010, Malaysia spent a total of US$73.5 million (0.03% of Malaysia’s GDP) on its National Dengue Vector Control Program. About 92% of the amount was used for fogging [40].
Having early notice of a dengue outbreak will permit a timely action/response among the health personnel and the public, ahead of the predicted outbreak period. Alternatively, using freely available climate data would also contribute to reducing the cost of developing a warning system for developing countries. The system would also be an economical approach in planning resources and prioritising high risk areas for intensive preventive activities [9, 39].
Colombia and Singapore have published findings of their early warning systems. Colombia’s dengue early warning system managed to detect 75% of the total dengue outbreaks 1–5 months in advance, and missed some 12.5% cases. The system also classified western Colombia as a high risk area due to its dense population and the suitability of the climate conditions for the mosquitoes [41]. Meanwhile, in Singapore, its warning system forecasted an outbreak with a 3-month lag through the LASSO-derived models in their 2013 dengue control program, allowing advanced outbreak response preparations [18].
In this study, we also looked at the respondent’s perception and attitude towards the warning system. Most respondents did not check the dengue situation in their area, but they were ready to take extra actions if the dengue risk in their area increases. This suggests that a warning system on dengue risk could trigger the respondents to take preventive actions against dengue. It is helpful to know that there is a demand for such a system among the general public, as can be seen in this study. The demand would mean that the authority will have to provide such a system as a preventive measure. It is hoped that the public will respond appropriately towards an alert, so that efforts/work put into creating a system would not go to waste. Apart from that, having a demand would hopefully make it easier to get cooperation from the community and the government involving matters of campaign and other issues regarding the dengue warning system.
Although information does not automatically lead to positive decision making, it is hoped that the more information the public has about an early warning system, the more ready they will be to respond to it. An early warning system that is focused solely on information collection has been proven to not actually bring about early action [22]. Innovative approaches need to be explored by engaging multiple stakeholders to improve public response. In addition, involving the community in risk analysis, action planning and feedback on successes and challenges of early warning systems could reduce barriers to translating early warning into early action [22].
Factors associated with Q18 (Perception of the usefulness of an early warning for community to take timely preventive action) and Q34 (Knowledge on actions to be taken following a notice on future dengue outbreak)
Our findings showed that respondents who were divorced, unemployed and earning below MYR3000 did not think that an early dengue warning would be useful for the community to take timely preventive action. This could be due to a lower education status and consequently lower dengue knowledge. Those who have known people who have been infected with dengue thought that an early dengue warning would be useful for the community to take timely preventive action.
Our data revealed that people who do not live in the Petaling District have the knowledge on what to do if they were informed of a possible future dengue outbreak. This could be partly due to the fact that most respondents (60.7%) who do not live in Petaling District were students; with half of them being degree holders. They thus have better knowledge about dengue preventive action.
We also found that having knowledge about dengue, having knowledge on dengue preventive actions and knowing about dengue and climate, too, were associated with the thought that an early dengue warning would be useful for the community to take timely preventive action. This is important as active community involvement is imperative in ensuring response towards dengue warning and successful dengue prevention. Active mobilisation of the community can only be effective and sustainable with adequate knowledge and support from the authority. Continuous education and monitoring by relevant organizations should be done to ensure long-term behavioural changes among the society towards dengue prevention [42].
Subsequently, those who have sufficient knowledge on dengue prevention, and those who have knowledge about dengue and climate would know what to do following information of a possible dengue outbreak. Our results thus supports the outcome reported by Chandren et al (2015) which stated that health and educational programs should focus on enhancing dengue knowledge as to increase dengue prevention practices [31]. A study in Costa Rica reported the association of positive breeding sites with lesser knowledge of dengue symptoms, lower education level, and lower ratings in (i) the importance of preventive actions and (ii) dangers of dengue [42].
Strength and limitation
This is the first study looking at the public perceptions and attitudes towards a climate-based dengue early warning in dengue endemic country. Information from this study will be useful in exploring community needs before establishing early warning system for dengue. However, selection of study areas and participants in this study were based on non-probabilistic sampling. This might have caused some bias in the representation of our respondents. Causal relationship also cannot be established due to the cross-sectional nature of this study.
In this study, more than half of the respondents were females (64.7%) and Malays (75.7%). This is different from the population distribution in Petaling district according to the latest population census with 51.2% female and 52.6% Malay [43]. However the census was conducted in 2010, and data from the census only includes those residing in the district in contrast to the sample this study.
Conclusion
In conclusion, members of the public in the Petaling District were aware of dengue and have some knowledge of dengue. They were also aware of the relationship between climate change and dengue incidence, and would like to receive more information about how climate data can be used to develop an early dengue warning system. Our findings indicated that the public in Petaling District do think it is necessary to have an early warning system. We recommend that the implementation of a dengue warning system will need to be accompanied by public educational programs for the warning system to work effectively. Having an early dengue warning system would go some way to reduce the high economic and health burden of dengue in Malaysia.
Supporting information
(PDF)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work is supported by Swedish Research Council [348-2014-4040, E0404001] (www.vr.se) and the University of Malaya Research Grant Programme [RP034A-15HTM] (www.um.edu.my).
References
- 1.Harrington LC, Fleisher A, Ruiz-Moreno D, Vermeylen F, Wa CV, Poulson RL, et al. Heterogeneous Feeding Patterns of the Dengue Vector, Aedes aegypti, on Individual Human Hosts in Rural Thailand. PLOS Neglected Tropical Diseases. 2014;8(8):e3048 10.1371/journal.pntd.0003048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Dengue 2017. [updated 29 July 2016; cited 2017]. http://www.who.int/immunization/diseases/dengue/en/. [DOI] [PubMed] [Google Scholar]
- 3.Stanaway JD, Shepard DS, Undurraga EA, Halasa YA, Coffeng LE, Brady OJ, et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. The Lancet Infectious Diseases. 2016;16(6):712–23. 10.1016/S1473-3099(16)00026-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shepard DS, Undurraga EA, Halasa YA. Economic and Disease Burden of Dengue in Southeast Asia. PLOS Neglected Tropical Diseases. 2013;7(2):e2055 10.1371/journal.pntd.0002055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shepard DS, Lees R, Ng CW, Undurraga EA, Halasa Y, Lum L. Burden of Dengue in Malaysia. Report from a Collaboration between Universities and the Ministry of Health of Malaysia 2013. 2013:1–89. [Google Scholar]
- 6.iDengue. Maklumat Kes Denggi Terkini 2017 [15 March 2017]. http://idengue.remotesensing.gov.my/idengue/index.php.
- 7.World Health Organization. Dengue Control. Dengue/Severe dengue frequently asked questions. 2017 [updated 3 January 2017; cited 2017 27 September 2017]. http://www.who.int/denguecontrol/faq/en/index2.html.
- 8.Naing C, Ren WY, Man CY, Fern KP, Qiqi C, Ning CN, et al. Awareness of dengue and practice of dengue control among the semi-urban community: a cross sectional survey. Journal of Community Health. 2011;36(6):1044–9. Epub 2011/04/30. 10.1007/s10900-011-9407-1 . [DOI] [PubMed] [Google Scholar]
- 9.Hii YL, Zaki RA, Aghamohammadi N, Rocklöv J. Research on Climate and Dengue in Malaysia: A Systematic Review. Current Environmental Health Reports. 2016;3:81–90. 10.1007/s40572-016-0078-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jetten TH, Focks DA. Potential changes in the distribution of dengue transmission under climate warming. The American Journal of Tropical Medicine and Hygiene. 1997;57(3):285–97. Epub 1997/10/06. . [DOI] [PubMed] [Google Scholar]
- 11.Hu W, Clements A, Williams G, Tong S. Dengue fever and El Nino/Southern Oscillation in Queensland, Australia: a time series predictive model. Occupational and Environmental Medicine. 2010;67(5):307–11. Epub 2009/10/13. . [DOI] [PubMed] [Google Scholar]
- 12.Degallier N, Favier C, Menkes C, Lengaigne M, Ramalho WM, Souza R, et al. Toward an early warning system for dengue prevention: modeling climate impact on dengue transmission. Climatic Change. 2010;98(3):581–92. 10.1007/s10584-009-9747-3 [DOI] [Google Scholar]
- 13.Lowe R, Bailey TC, Stephenson DB, Graham RJ, Coelho CAS, Sá Carvalho M, et al. Spatio-temporal modelling of climate-sensitive disease risk: Towards an early warning system for dengue in Brazil. Computers & Geosciences. 2011;37(3):371–81. 10.1016/j.cageo.2010.01.008. [DOI] [Google Scholar]
- 14.Liu-Helmersson J, Stenlund H, Wilder-Smith A, Rocklöv J. Vectorial Capacity of Aedes aegypti: Effects of Temperature and Implications for Global Dengue Epidemic Potential. PLOS ONE. 2014;9(3):e89783 10.1371/journal.pone.0089783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hii YL. Climate and dengue fever: early warning based on temperature and rainfall [Umeå University Medical Dissertations]. Sweden: Umeå University; 2013. [Google Scholar]
- 16.Lowe R, Rodo X, Barcellos C, Carvalho M, Coelho C, Bailey T, et al. Dengue epidemic early warning system for Brazil. UNISDR Scientific and Technical Advisory Group. 2015. [Google Scholar]
- 17.Lowe R, Coelho CAS, Barcellos C, Carvalho MS, Catão RDC, Coelho GE, et al. Evaluating probabilistic dengue risk forecasts from a prototype early warning system for Brazil. eLife. 2016;5:e11285 10.7554/eLife.11285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi Y, Liu X, Kok S, Rajarethinam J, Liang S, Yap G, et al. Three-Month Real-Time Dengue Forecast Models: An Early Warning System for Outbreak Alerts and Policy Decision Support in Singapore. Environ Health Perspect. 2016;124(9):1369–75. 10.1289/ehp.1509981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bowman LR, Tejeda GS, Coelho GE, Sulaiman LH, Gill BS, McCall PJ, et al. Alarm Variables for Dengue Outbreaks: A Multi-Centre Study in Asia and Latin America. PLOS ONE. 2016;11(6):e0157971 Epub 2016/06/28. 10.1371/journal.pone.0157971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ververs M-T. The East African Food Crisis: Did Regional Early Warning Systems Function? The Journal of Nutrition. 2012;142:131–3. 10.3945/jn.111.150342 [DOI] [PubMed] [Google Scholar]
- 21.Macherera M, Chimbari M. A review of studies on community based early warning systems. Jàmbá: Journal of Disaster Risk Studies. 2016;8(1):a206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ibrahim Maggie, Kruczkiewicz Andrew, Learning from experience: a summarised review of early warning systems. World Vision Report December 2016. https://www.wvi.org/sites/default/files/WV_EWEA_Doc_FINAL_Web.pdf
- 23.Taber K. S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Research in Science Education. 2018; 48(6):1273 10.1007/s11165-016-9602-2 [DOI] [Google Scholar]
- 24.Al-Zurfi BMN, Fuad MD, Abdelqader MA, Baobaid MF, Elnajeh M, Ghazi HF, et al. Knowledge, attitude and practice of dengue fever and health education programme among students of Alam Shah Science School, Cheras, Malaysia. Malaysian Journal of Public Health Medicine. 2015;15(2):69–74. [Google Scholar]
- 25.Mohd Hairi F, Ong C-H, Suhaimi A, Tsung T-W, Azhar bin Anis Ahmad M, Sundaraj C, et al. A Knowledge, Attitude and Practices (KAP) Study on Dengue among Selected Rural Communities in the Kuala Kangsar District. Asia Pacific Journal of Public Health. 2003;15:37–43. 10.1177/101053950301500107 [DOI] [PubMed] [Google Scholar]
- 26.Zahir A, Ullah A, Shah M, Mussawar A. Community Participation, Dengue Fever Prevention and Control Practices in Swat, Pakistan. International Journal of MCH and AIDS. 2016;5(1):39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu T, Zhu G, He J, Song T, Zhang M, Lin H, et al. Early rigorous control interventions can largely reduce dengue outbreak magnitude: experience from Chaozhou, China. BMC Public Health. 2017;18(1):90 10.1186/s12889-017-4616-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leong TK. Knowledge, Attitude and Practice on Dengue among Rural Communities in Rembau and Bukit Pelanduk, Negeri Sembilan, Malaysia. International Journal of Tropical Disease and Health. 2014;4(7):841–8. [Google Scholar]
- 29.Wong LP, Shakir SMM, Atefi N, AbuBakar S. Factors Affecting Dengue Prevention Practices: Nationwide Survey of the Malaysian Public. PLOS ONE. 2015;10(4):e0122890 10.1371/journal.pone.0122890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chandren JR, Wong LP, AbuBakar S. Practices of Dengue Fever Prevention and the Associated Factors among the Orang Asli in Peninsular Malaysia. PLOS Neglected Tropical Diseases. 2015;9(8):e0003954 10.1371/journal.pntd.0003954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morin CW, Comrie AC, Ernst K. Climate and dengue transmission: evidence and implications. Environ Health Perspect. 2013;121(11–12):1264–72. Epub 2013/09/24. 10.1289/ehp.1306556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Choi Y, Tang CS, McIver L, Hashizume M, Chan V, Abeyasinghe RR, et al. Effects of weather factors on dengue fever incidence and implications for interventions in Cambodia. BMC Public Health. 2016;16:241 10.1186/s12889-016-2923-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebi KL, Nealon J. Dengue in a changing climate. Environmental Research. 2016;151(Supplement C):115–23. 10.1016/j.envres.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 34.Silva FD, Santos AMd, Corrêa RdGCF, Caldas AdJM. Temporal relationship between rainfall, temperature and occurrence of dengue cases in São Luís, Maranhão, Brazil. Ciência & Saúde Coletiva. 2016;21:641–6. [DOI] [PubMed] [Google Scholar]
- 35.Descloux E, Mangeas M, Menkes CE, Lengaigne M, Leroy A, Tehei T, et al. Climate-based models for understanding and forecasting dengue epidemics. PLOS Neglected Tropical Diseases. 2012;6(2):e1470 Epub 2012/02/22. 10.1371/journal.pntd.0001470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Campbell KM, Lin CD, Iamsirithaworn S, Scott TW. The Complex Relationship between Weather and Dengue Virus Transmission in Thailand. Am J Trop Med Hyg. 2013;89(6):1066–80. 10.4269/ajtmh.13-0321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheong YL, Burkart K, Leitão PJ, Lakes T. Assessing Weather Effects on Dengue Disease in Malaysia. International Journal of Environmental Research and Public Health. 2013;10(12):6319–34. 10.3390/ijerph10126319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Research Council (US) Committee on Climate E, Infectious Diseases, and Human Health,. 7, Toward the Development of Disease Early Warning Systems Under the Weather: Climate, Ecosystems, and Infectious Disease. Washington (DC): National Academies Press (US); 2001. [Google Scholar]
- 39.Carrasco LR, Lee LK, Lee VJ, Ooi EE, Shepard DS, Thein TL, et al. Economic Impact of Dengue Illness and the Cost-Effectiveness of Future Vaccination Programs in Singapore. PLOS Neglected Tropical Diseases. 2011;5(12):e1426 10.1371/journal.pntd.0001426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Packierisamy PR, Ng C-W, Dahlui M, Inbaraj J, Balan VK, Halasa YA, et al. Cost of Dengue Vector Control Activities in Malaysia. The American Journal of Tropical Medicine and Hygiene. 2015;93(5):1020–7. 10.4269/ajtmh.14-0667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee J-S, Carabali M, Lim JK, Herrera VM, Park I-Y, Villar L, et al. Early warning signal for dengue outbreaks and identification of high risk areas for dengue fever in Colombia using climate and non-climate datasets. BMC Infectious Diseases. 2017;17(1):480 10.1186/s12879-017-2577-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egedus VL, Ortega JM, Obando AA. Knowledge, perceptions, and practices with respect to the prevention of dengue in a mid-Pacific coastal village of Costa Rica. Revista de Biologia Tropical. 2014;62(3):859–67. Epub 2014/11/22. . [DOI] [PubMed] [Google Scholar]
- 43.Department of Statistics Malaysia. Petaling (District, Malaysia)—Population Statistics and Location in Malaysia 2017 [20 September 2018]. https://www.citypopulation.de/php/malaysia-mukim-admin.php?adm1id=1005.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.