Abstract
Enhanced Recovery after Surgery (ERAS) protocols are multimodal perioperative care pathways designed to accelerate recovery by minimizing the physiologic stress of a surgical procedure. Benefits of ERAS implementation in colorectal surgery include reduced length of stay and decreased complications without an increase in readmissions. Though there is evidence associating individual ERAS protocol elements (e.g., preoperative carbohydrate loading, judicious perioperative fluid administration, and early initiation of postoperative nutrition) with improved outcomes, ensuring high compliance with all elements of an ERAS protocol will maximize benefits to the patient. After ERAS implementation, data collection on protocol process measures can help providers target education and interventions to improve protocol compliance and patient outcomes.
Keywords: Enhanced Recovery after Surgery, fast-track surgery, outcomes
Enhanced Recovery after Surgery (ERAS) protocols are multimodal perioperative care pathways designed to accelerate recovery by minimizing the physiologic stress of a surgical procedure. ERAS protocols permit standardization of care on a surgical service incorporating evidence-based practices and also foster an interdisciplinary approach to the management of the surgical patient. Benefits of ERAS implementation to the patient include decreased surgical stress, decreased length of stay (LOS), and reduced complications.
Because ERAS protocols have traditionally included several elements spanning the preoperative, intraoperative, and postoperative phases of care, there has been interest in identifying which specific protocol components are responsible for improved patient outcomes. The benefits of specific ERAS protocol elements, including preoperative carbohydrate loading, judicious fluid administration in the perioperative period, and early initiation of postoperative nutrition, have been explored in the literature. Though there are data to suggest that individual protocol elements may be associated with improved outcomes, it is clear that one or two elements are not sufficient to achieve the maximum benefits of an ERAS protocol. Similarly, having a protocol in place with several important ERAS elements is not enough if individual patients are not compliant with all elements of the protocol. To achieve the full benefit of an ERAS program, data on protocol compliance are necessary along with a strategy for improvement when elements with poor compliance are identified.
Length of Stay
ERAS is synonymous with “fast-track” surgery, and in studies of ERAS implementation, LOS is often the primary outcome. Evidence from several randomized controlled trials (RCTs) and observational studies has demonstrated that ERAS protocol implementation reduces LOS after surgery ( Fig. 1 ). Three meta-analyses of RCTs comparing outcomes after colorectal (CR) surgery with traditional perioperative care compared with fast-track care found a reduction in LOS with fast-track protocol implementation. 1 2 3 The meta-analysis by Lv et al included seven RCTs with a total of 852 patients and reported a mean LOS difference of −1.88 days (95% confidence interval [CI]: −2.91 to −0.86) with fast-track surgery. 1 The meta-analysis by Adamina et al included six RCTs and a total of 452 patients and reported that patients on an ERAS protocol had a LOS 2.5 days shorter (95% CI: -3.92 to -1.11) than patients receiving traditional care. 2 An additional meta-analysis evaluating ERAS outcomes following laparoscopic CR surgery included four RCTs (486 patients total) and reported a pooled weighted mean difference in LOS of -1.22 days (95% CI -1.57 to -0.87 days). 3 Single-institution observational studies comparing LOS pre- and post-ERAS implementation in CR surgery patients describe LOS reductions ranging from 1 to 3 days. 4 5 6
Fig. 1.
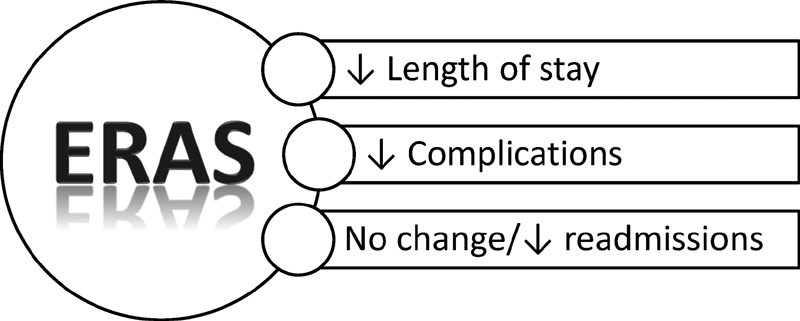
Outcomes of Enhanced Recovery after Surgery implementation.
The LOS benefits of ERAS implementation in CR surgery have been replicated in a variety of hospital settings, including international as well as American, teaching as well as nonteaching, and in resource-poor settings. Most of the previously discussed studies reporting LOS reductions after ERAS implementation were conducted in American teaching hospital settings. A retrospective review of outcomes following CR ERAS implementation in five European centers demonstrated a LOS reduction of 3 days compared with traditional care in the same hospitals. 7 8 A retrospective review of CR ERAS implementation in eight community hospitals reported that overall, LOS decreased by 1.5 days ( p < 0.001). 9 In a retrospective review of CR ERAS implementation at a county hospital with limited resources, Rona et al reported a 3-day reduction in LOS with high compliance to the protocol. 10
Although overall LOS reductions following ERAS implementation are well described in the literature, not all patients qualify for early discharge. Two observational studies have explored patient and procedure factors that predict early discharge failure after CR surgery on an ERAS protocol. 11 12 Keller et al defined early discharge failure as LOS greater than 4 days, and concluded that patients with more comorbidities, including higher body mass index, and those who underwent longer procedures were less likely to be discharged early. 11 Feroci et al found that age greater than 75 years, ASA grade 3 or 4, and the presence of an ileostomy were independent predictors of longer LOS. 12
Postoperative Complications
In addition to evaluating LOS, most ERAS implementation studies have also looked at clinical outcomes like urinary tract infection (UTI), overall morbidity, and mortality. The majority of CR ERAS literature supports a reduction in postoperative complications with ERAS implementation, though some studies show no difference in postoperative complications between traditional care and ERAS cohorts ( Fig. 1 ).
All three meta-analyses cited previously evaluated the effect of ERAS implementation on postoperative complications. 1 2 3 Lv et al reported reduced total complication rates (relative risk [RR]: 0.69, 95% CI: 0.51–0.93) with ERAS compared with traditional care. 1 When study results were pooled, the rate of total complications in the ERAS group was 31.7% compared with 43.0% in the traditional care group. 1 No statistically significant difference in mortality was seen between ERAS and traditional care groups (RR: 1.02, 95% CI: 0.40–2.57). 1 Adamina et al reported decreased 30-day morbidity in the ERAS group with an RR of 0.52 (95% CI: 0.36–0.73). 2 In contrast, the meta analysis (MA) by Tan et al of RCTs evaluating ERAS in laparoscopic CR surgery failed to show a statistically significant difference with ERAS compared with traditional care in morbidity (pooled odds ratio [OR]: 0.68, 95% CI: 0.44–1.04) or mortality (OR: 1.51, 95% CI: 0.29–7.77). 3
Among the observational studies previously cited, four reported on postoperative complication and/or mortality rates. 4 5 10 One study reported decreased overall complications (15 vs. 30%, p = 0.007) in an ERAS cohort compared with historical controls, 4 and another reported decreased rates of UTI (9.8 vs. 20.2%, p = 0.02). 5 A third study reported decreased morbidity (14.8 vs. 33.6%) in ERAS patients, and found no statistically significant difference in mortality. 6 At a county hospital with limited resources, ERAS was associated with a trend in decreased postoperative morbidity, though this was not statistically significant. 10
Overall, evidence from both observational and RCTs supports reduced morbidity with the implementation of ERAS, including reduction in specific postoperative complications like UTI, and no difference in mortality rates between patients treated with an ERAS protocol and those receiving traditional care.
Readmission
An initial concern with the implementation of ERAS was that the emphasis on reducing LOS after surgery would lead to increased readmissions. Every study that has evaluated the effects of ERAS implementation on LOS, therefore, has also evaluated readmission rates. Overall, CR ERAS literature has demonstrated that readmission rates following ERAS implementation remain stable compared with historical readmission rates with traditional care despite the decreases seen in LOS ( Fig. 1 ).
All three meta-analyses reviewed included readmission rates as an outcome of interest, and none of them reported a statistically significant difference in readmission rates between patients treated with ERAS versus traditional care. 1 2 3 Overall, observational studies have reproduced these results, 4 6 9 10 although the study by Miller et al reported lower readmission rates in ERAS patients compared with those receiving traditional care (9.8 vs. 20.2%, p = 0.02). 5 In summary, data from both observational studies and RCTs demonstrate stable readmission rates after implementation of ERAS, despite a reduction in LOS.
Effectiveness of Specific ERAS Protocol Components
ERAS protocols contain a variety of elements spanning all phases of the perioperative experience. After early studies demonstrated the effectiveness of ERAS in decreasing LOS and complications, interest arose in identifying the individual elements of ERAS responsible for these clinical benefits. Most studies have been observational, and typically use multivariable logistic regression to identify ERAS protocol elements that are independent predictors of an outcome (e.g., LOS). To date, no randomized studies have attempted to isolate the effect of individual protocol elements in the setting of ERAS.
Carbohydrate Loading
The administration of preoperative oral carbohydrates may be associated with attenuation of the perioperative catabolic state and reduced postoperative insulin resistance. 13 There are limited data evaluating the role of preoperative carbohydrate loading in the setting of ERAS specifically, though the role of carbohydrate loading has been evaluated in patients undergoing abdominal surgery.
A systematic review of RCTs comparing preoperative carbohydrate loading to placebo and/or fasting included 18 studies in elective abdominal surgery. 14 Subgroup analysis of major abdominal surgery concluded that carbohydrate loading was associated with a lower LOS compared with preoperative fasting or placebo (mean difference: −1.66 days, 95% CI: −2.97 to −0.34 days). 14 Analysis of secondary outcomes in all procedures concluded that carbohydrate loading was not associated with a statistically significant difference in complications or patient-reported fatigue, well-being, or postoperative nausea/vomiting. 14 Carbohydrate loading was associated with increased insulin sensitivity (mean difference: 0.76, 95% CI: 0.24–1.29), faster return of bowel function (mean difference: −0.39 days, 95% CI: −0.70 to −0.07 days), and a nonstatistically significant trend toward decreased postoperative insulin resistance (mean difference: −1.59, 95% CI: −3.35 to 0.17). 14
Fluid Management
Fluid administration with a goal to achieve a near zero fluid balance is a hallmark of ERAS, as excessive fluid administration may be associated with increased cardiac demand, pulmonary edema, bowel edema leading to ileus, and delayed recovery. 13
The effect of goal-directed fluid therapy (GDFT) devices on outcomes including LOS and complications has been evaluated in CR patients on ERAS protocols in several RCTs. The most recent meta-analyses of RCTs examining the effect of GDFT in major abdominal surgery also performed subgroup analysis on ERAS patients (primarily CR). 15 This meta-analysis concluded that there were trends toward decreased LOS (mean difference: −0.71 days, 95% CI: −1.91 to 0.49 days), decreased morbidity (risk ratio: 0.86, 95% CI: 0.70–1.05), and decreased ileus (risk ratio: 0.63, 95% CI: 0.32–1.22) with the use of GDFT devices, though none of these effects was statistically significant. 15
Additional observational studies of CR patients on an ERAS protocol have used multivariable logistic regression to identify independent predictors of outcomes like early discharge and complications. In a study by Larson et al including 541 ERAS patients, compliance with ERAS protocol fluid management (discontinuation of intravenous [IV] fluid at 8 am postoperative day 1) was associated with reduced LOS (mean LOS: 3.1 vs. 4.2 days, p < 0.001) and decreased complications (8.1 vs. 19.6%, p = 0.001). 16 Of note, it was standard for ERAS patients in this study to receive intraoperative GDFT. 16 A second observational study by Aarts et al including 336 CR ERAS patients from seven institutions concluded that intraoperative fluid restriction was independently associated with LOS ≤ 5 days on adjusted analysis (OR: 1.26, 95% CI: 1.15–1.37. 17
Overall, there is evidence from observational studies of CR ERAS patients that judicious intraoperative fluid administration and early postoperative discontinuation of IV fluids may be associated with shorter LOS and decreased complications. Though intraoperative GDFT is one means of maintaining euvolemia during surgery, evidence from RCTs fails to demonstrate a statistically significant improvement in outcomes with this modality for ERAS patients.
Early Nutrition
Early initiation of per os (PO) nutrition is hypothesized to speed gastrointestinal recovery following CR surgery without increasing complications, and thus contribute to decreased LOS. No RCTs have evaluated the effect of early nutrition in the setting of ERAS, but many RCTs have explored this effect in elective abdominal and CR surgery.
Four meta-analyses have compared outcomes after elective abdominal surgery with early versus traditional feeding. The largest of these included 13 RCTs and almost 1,200 patients undergoing intestinal surgery and compared initiation of PO nutrition within 24 hours of surgery to nil per os (NPO) status. 18 Early feeding was associated with decreased mortality, but increased postoperative vomiting. 18 A nonstatistically significant trend toward shorter LOS and decreased complications was seen in the early nutrition patients. 18 A smaller meta-analysis of RCTs in CR surgery included seven studies and almost 600 patients. 19 In this meta-analysis, early feeding was associated with reduced complications (RR: 0.70; 95% CI: 0.50–0.98; p = 0.04) and LOS (weighted mean difference: −1.58 days; 95% CI: −2.77 to −0.39). 19 No statistically significant difference was seen in the risk of adverse outcomes like anastomotic dehiscence, pneumonia, rate of nasogastric tube reinsertion, vomiting, or mortality. 19 Of note, the definition of early feeding in the included RCTs was not uniform, though most protocols were to give liquids or solids within 24 hours of surgery. 19
As with fluid management, observational studies on CR ERAS populations have used adjusted analysis to isolate the effect of early feeding. Larson et al demonstrated that ERAS patients compliant with early PO intake had a shorter LOS (3.1 vs. 4.4 days, p < 0.001) and fewer complications. 16 Similarly, Aarts et al demonstrated reduced LOS in ERAS patients who began clear liquids on the day of surgery; though in this study, the trend toward decreased complications was not statistically significant. 17
Evidence from RCTs in CR surgery supports reduced LOS and complications with early initiation of nutrition and no resultant increase in complications. Evidence from observational studies in the CR ERAS population supports LOS reductions with early feeding, though not all studies have shown a decrease in complications. Though each study defines early nutrition differently, many provide clear liquid or regular diets within 24 hours of surgery.
ERAS Protocol Compliance and Outcomes
Though there is support in the literature for individual elements of CR ERAS protocols, there is also evidence from multiple studies that low protocol compliance or implementation of only a few ERAS elements is insufficient to achieve the full benefits of an ERAS program. A retrospective study of CR ERAS patients by Agrafiotis et al examined how varying compliance with an ERAS protocol (i.e., compliance with only a few items vs. most items) impacted outcomes including LOS. 20 Deviations from additional ERAS protocol elements resulted in longer LOS, leading authors to conclude that there was stepwise benefit to implementing more components in an ERAS protocol. 20 Data from an ERAS Pilot in the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) included 16 hospitals that implemented ERAS on over 1,500 patients and found that average LOS increased as adherence to the ERAS protocol decreased ( p < 0.001). Patients with high protocol compliance also had fewer complications than patients with low protocol compliance. After adjusting for preoperative (demographics, comorbidities), operative (indication, approach, oral antibiotic, or mechanical bowel prep), and postoperative characteristics (complications), adherence to five or fewer ERAS protocol components (0–5) increased the odds of prolonged LOS threefold (OR: 3.5, 95% CI: 2.4–5.8). 21 A multicenter study out of Europe echoed these findings. Maessen et al reported that even after ERAS protocol implementation, compliance with many of the postoperative protocol elements remained low, and as a result, many patients did not benefit from expected reductions in LOS. 8
To ensure high compliance for all patients on an ERAS protocol, data collection is critical. Collecting data on ERAS protocol compliance at the individual patient level allows providers to identify which protocol components are problematic and to target education and interventions to improve compliance ( Fig. 2 ). Recently, the Agency for Healthcare Research and Quality (AHRQ) launched the Safety Program for Optimal Surgical Recovery in partnership with the ACS. This program will support implementation of ERAS pathways, and robust data collection in collaboration with the ACS is a key program feature. The Optimal Surgical Recovery Program will develop ERAS protocols and implementation materials for five procedural cohorts, including CR surgery, hysterectomy, joint replacement/hip fracture, emergency general surgery, and bariatric surgery. Hospitals enrolling in the program will have access to a free, robust data registry built on the NSQIP platform. This ERAS registry will allow hospitals to collect basic risk-adjustment variables, ERAS process measures, and outcomes relevant to ERAS like LOS, readmission, and complications.
Fig. 2.
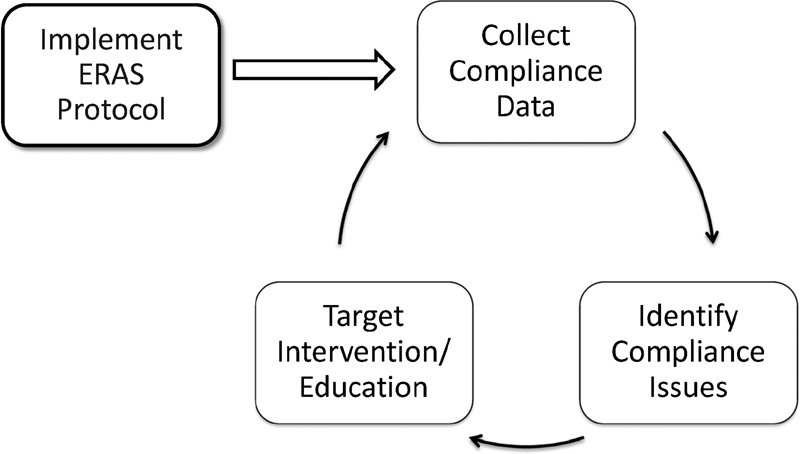
Data collection and targeted interventions to improve compliance with Enhanced Recovery after Surgery Protocols.
Summary
The benefits of ERAS in the CR population have been well defined, and include reduced LOS, reduced postoperative complications, and no difference in readmission rates compared with traditional care. Each element of a CR ERAS protocol is designed to decrease the physiologic stress of surgery, and there is evidence in the literature that individual protocol elements are associated with improved outcomes. Overall, however, the sum of ERAS protocol implementation is greater than its parts, and increasing compliance with all elements of an ERAS protocol will yield the greatest clinical benefits. Robust data collection on ERAS protocol compliance and a process to identify and target areas of poor compliance are two elements that can improve the success and benefits of a CR ERAS program.
Footnotes
Conflict of Interest Dr. Kristen Ban receives salary support through a contract with the Agency for Healthcare Research and Quality.
References
- 1.Lv L, Shao Y F, Zhou Y B. The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Colorectal Dis. 2012;27(12):1549–1554. doi: 10.1007/s00384-012-1577-5. [DOI] [PubMed] [Google Scholar]
- 2.Adamina M, Kehlet H, Tomlinson G A, Senagore A J, Delaney C P. Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery. 2011;149(06):830–840. doi: 10.1016/j.surg.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Tan S J, Zhou F, Yui W K et al. Fast track programmes vs. traditional care in laparoscopic colorectal surgery: a meta-analysis of randomized controlled trials. Hepatogastroenterology. 2014;61(129):79–84. [PubMed] [Google Scholar]
- 4.Thiele R H, Rea K M, Turrentine F E et al. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220(04):430–443. doi: 10.1016/j.jamcollsurg.2014.12.042. [DOI] [PubMed] [Google Scholar]
- 5.Miller T E, Thacker J K, White W D et al. Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118(05):1052–1061. doi: 10.1213/ANE.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 6.Teeuwen P H, Bleichrodt R P, Strik C et al. Enhanced recovery after surgery (ERAS) versus conventional postoperative care in colorectal surgery. J Gastrointest Surg. 2010;14(01):88–95. doi: 10.1007/s11605-009-1037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nygren J, Hausel J, Kehlet H et al. A comparison in five European Centres of case mix, clinical management and outcomes following either conventional or fast-track perioperative care in colorectal surgery. Clin Nutr. 2005;24(03):455–461. doi: 10.1016/j.clnu.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Maessen J, Dejong C H, Hausel J et al. A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg. 2007;94(02):224–231. doi: 10.1002/bjs.5468. [DOI] [PubMed] [Google Scholar]
- 9.Archibald L H, Ott M J, Gale C M, Zhang J, Peters M S, Stroud G K. Enhanced recovery after colon surgery in a community hospital system. Dis Colon Rectum. 2011;54(07):840–845. doi: 10.1007/DCR.0b013e31821645bd. [DOI] [PubMed] [Google Scholar]
- 10.Rona K, Choi J, Sigle G, Kidd S, Ault G, Senagore A J. Enhanced recovery protocol: implementation at a county institution with limited resources. Am Surg. 2012;78(10):1041–1044. [PubMed] [Google Scholar]
- 11.Keller D S, Bankwitz B, Woconish D et al. Predicting who will fail early discharge after laparoscopic colorectal surgery with an established enhanced recovery pathway. Surg Endosc. 2014;28(01):74–79. doi: 10.1007/s00464-013-3158-2. [DOI] [PubMed] [Google Scholar]
- 12.Feroci F, Lenzi E, Baraghini M et al. Fast-track surgery in real life: how patient factors influence outcomes and compliance with an enhanced recovery clinical pathway after colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2013;23(03):259–265. doi: 10.1097/SLE.0b013e31828ba16f. [DOI] [PubMed] [Google Scholar]
- 13.Feldheiser A, Aziz O, Baldini G et al. Enhanced Recovery after Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand. 2016;60(03):289–334. doi: 10.1111/aas.12651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith M D, McCall J, Plank L, Herbison G P, Soop M, Nygren J. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev. 2014;(08):CD009161. doi: 10.1002/14651858.CD009161.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rollins K E, Lobo D N. Intraoperative goal-directed fluid therapy in elective major abdominal surgery: a meta-analysis of randomized controlled trials. Ann Surg. 2016;263(03):465–476. doi: 10.1097/SLA.0000000000001366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larson D W, Lovely J K, Cima R R et al. Outcomes after implementation of a multimodal standard care pathway for laparoscopic colorectal surgery. Br J Surg. 2014;101(08):1023–1030. doi: 10.1002/bjs.9534. [DOI] [PubMed] [Google Scholar]
- 17.Aarts M A, Okrainec A, Glicksman A, Pearsall E, Victor J C, McLeod R S. Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc. 2012;26(02):442–450. doi: 10.1007/s00464-011-1897-5. [DOI] [PubMed] [Google Scholar]
- 18.Lewis S J, Andersen H K, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009;13(03):569–575. doi: 10.1007/s11605-008-0592-x. [DOI] [PubMed] [Google Scholar]
- 19.Zhuang C L, Ye X Z, Zhang C J, Dong Q T, Chen B C, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30(03):225–232. doi: 10.1159/000353136. [DOI] [PubMed] [Google Scholar]
- 20.Agrafiotis A C, Corbeau M, Buggenhout A, Katsanos G, Ickx B, Van de Stadt J. Enhanced recovery after elective colorectal resection outside a strict fast-track protocol. A single centre experience. Int J Colorectal Dis. 2014;29(01):99–104. doi: 10.1007/s00384-013-1767-9. [DOI] [PubMed] [Google Scholar]
- 21.Berian J R, Ban K A, Mohanty Set al. “Adherence with Enhanced Recovery Components Contributes to Improved Outcomes.” Scientific Forum #05: Quality, Safety and Outcomes I, 10/17/2016ACS Clinical Congress Annual Conference, October 16–20, 2016 Washington, DC. Published Abstract: JACS 223(4)S105–S106


