Abstract
Introduction
We aimed to determine the time and predictive factors of semen quality improvement in men with severe oligospermia after microsurgical varicocelectomy.
Methods
Men with total motile sperm count (TMSC) <5 million on two semen analyses were identified from May 2015 to August 2017. Postoperative semen analysis was collected at 3–6 months and >6 months. We evaluated preoperative factors for successful semen quality upgrading based on assisted reproductive technology (ART) eligibility: in vitro fertilization [IVF] (<5 million), intrauterine insemination (IUI) (5–9 million), and natural pregnancy (>9 million). We compared men with TMSC <5 million to those with TMSC 5–9 million. Data are reported as means and standard error of the mean (SEM). Pregnancy data was collected by phone interview at >6 months postoperatively
Results
A total of 33 men were included. TMSC improved from 1.5±0.2 to 7.3±1.8 million at 3–6 months (p<0.05) and 12.2±3.6 million at >6 months (p<0.05). There was no statistical difference in TMSC between 3–6 months and >6 months. Sixteen (48.5%) men upgraded semen quality into the range of natural pregnancy. Preoperative TMSC from 2–5 million was predictive of upgrading semen quality. Twenty-four couples were contacted by phone; 20 were attempting pregnancy in the postoperative period and five (25%) of them had achieved natural pregnancy.
Conclusions
Men with TMSC <5 million can expect the largest improvement in TMSC from 3–6 months postoperatively with minimal improvement thereafter. Preoperative TMSC >2 million was most predictive of semen quality upgrading.
Introduction
Varicocele is a pathological enlargement of the testicular veins that is associated with impaired spermatogenesis and infertility. In fact, varicocele is the most common surgically correctable cause of male infertility. Varicoceles are found in up to 15% of the adult male population. While not all men with varicoceles are infertile, varicoceles are found in approximately 35% of men with primary infertility, and up to 80% of men with secondary infertility.1 The gold standard of surgical treatment for clinical varicoceles is microsurgical varicocelectomy.
Several studies have evaluated the role of varicocelectomy in men with oligospermia.2,3 However, few studies assess outcomes of varicocelectomy in men with severe oligospermia (sperm concentration <5 million/cc) and more specifically men with TMSC <5million.4 Men with severe oligospermia are normally counselled to undergo assisted reproductive technology (ART) with in vitro fertilization (IVF) since varicocelectomy may not improve semen parameters enough to achieve natural conception. Total motile sperm count (TMSC) is typically used to determine eligibility for IVF.5 Men with TMSC <5million are recommended to undergo IVF, with 5–9 million to undergo intrauterine insemination (IUI), and those with >9 million are counselled to attempt natural pregnancy.6
Couples and female fertility specialists want to know how long after varicocelectomy to expect best improvement in semen parameters. Knowledge of duration of improvement in semen parameters after varicocele repair can assist patient counselling and direct the timing or need of invasive forms of ART. Men with oligospermia showed maximal improvement at three months after varicocele repair.7 No studies have specifically evaluated time to improvement in semen parameters after varicocele repair in men with severe oligospermia. We hypothesized that men with severe oligospermia will take a longer time (>3 months) to recover spermatogenesis than men with oligospermia because of their greater degree of spermatogenic failure. Additionally, we evaluated preoperative predictors of successful upstaging of semen quality based on TMSC.
Methods
We identified consecutive men who underwent microscopic subinguinal varicocelectomy between May 2015 and August 2017 with TMSC <5 million (on at least two semen analyses). Men with azoospermia, cryptozoospermia, karyotype abnormalities, and microdeletions were excluded. We excluded men who were on additional therapies, such as clomiphene citrate or high-dose anti-oxidant therapy, and females with diagnosed female factor infertility, such as premature ovarian failure, polycystic ovarian syndrome, and endometriosis. We evaluated age, preoperative follicle-stimulating hormone (FSH) (normal 2–8 ng/dL), luteinizing hormone (LH), testosterone (T), testis size in cubic centimeters, grade of varicocele, and preoperative and postoperative semen parameters, including volume, sperm concentration, percent motility, total motile sperm count, and viability. Followup semen analyses were performed approximately 3–6 months after surgery, with additional semen analysis performed after six months. Results of semen analyses were divided into categories of those collected from 3–6 months and those collected at greater than six months postoperatively. We then evaluated time to improvement/upgrading semen parameters in men with preoperative TMSC <5 million. Upgrading of semen quality was defined as improving from the IVF category (TMSC <5 million) into IUI (5–9 million) or natural pregnancy (greater than 9 million) postoperatively. As a comparison group, we evaluated men with TMSC 5–9 million, as these men are generally recommended to pursue IUI. For this group, upgrading was defined as a postoperative sperm count >9 million. We assessed pregnancy outcomes by telephone interview performed at minimum six months after surgery.
Data is reported using means and standard error of the mean (SEM). Significance was determined using the student t-test or Mann-Whitney U-test as appropriate. Data were analyzed using Microsoft Excel; p<0.05 was considered statistically significant.
Results
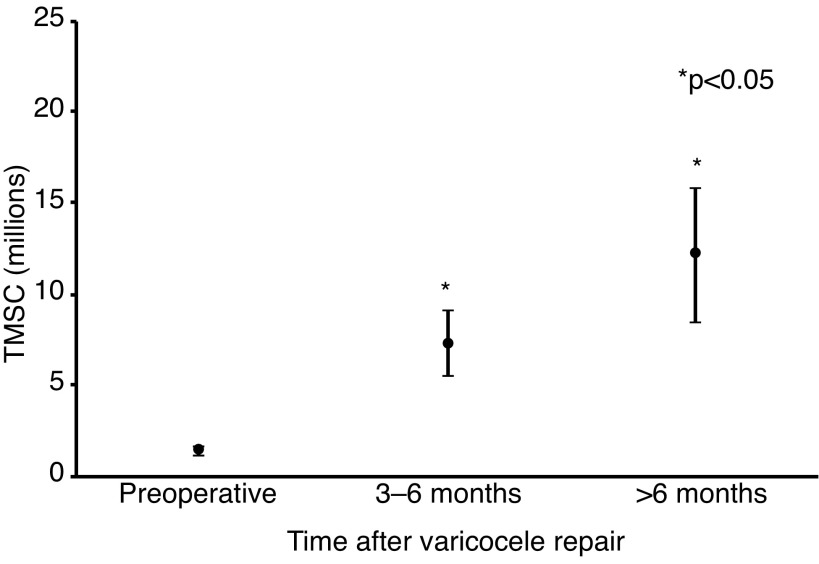
A total of 33 men with a TMSC of <5 million underwent microsurgical varicocelectomy. Median time to follow semen analysis was 4.8 months for the 3–6 month group and 7.7 months in the >6 month group. Mean TMSC improved from 1.5±0.2 million preoperatively to 7.3±1.8 million at 3–6 months (p<0.005) and 12.2±3.7 million at > 6 months (p<0.05) (Fig. 1). However, we did not notice an improvement in semen quality between 3–6 months and >6 months (p=0.6). A total of 16 men upgraded semen quality (48.5%) into the range of natural pregnancy (TMSC >9 million) (Table 1) and 15/16 of them upgraded by 3–6 months. Of the baseline characteristics, preoperative TMSC >2 million was the most significant parameter that predicted upgrading (mean preoperative TMSC 0.77 vs. 2.35; p<0.005) (Table 2). Among men with TMSC <2 million, up to one-third (7 of 21) upgraded to natural pregnancy (Table 1). At followup, there were no reported hydroceles or recurrence of varicocele on physical exam. As a comparison group, we evaluated outcomes of 10 men who underwent varicocele repair with preoperative TMSC from 5–9 million (7.1 million±0.4). Eight of 10 men upgraded semen quality to >9 million TMSC (10.2 million±1.9).
Fig. 1.
Time and degree of improvement in total motile sperm count (TMSC) for men with preoperative TMSC <5 million following microsurgical varicocelectomy (n=33).
Table 1.
Men with TMSC <5 million and varicocele
| Postoperative TMSC (%) | |||
|---|---|---|---|
|
| |||
| Preoperative | <5 million | 5–9 million | >9 million |
| TMSC <2 | 0.67 | 0 | 0.33 |
| TMSC >2 | 0.25 | 0 | 0.75 |
TMSC: total motile sperm count.
Table 2.
Comparison of preoperative characteristic of men with preoperative TMSC <5 million who upgraded to those who did not after microscopic subinguinal varicocelectomy
| Characteristic | Not upgraded (n=16) | Upgraded (n=17) | p |
|---|---|---|---|
| Preoperative characteristics | 35 | 35.5 | 0.88 |
| Age (yr) | 35 | 35.5 | 0.88 |
| Varix grade (mode) | 2 | 2 | |
| Testis volume (cc) | 13.1 | 12.6 | 0.67 |
| Total testosterone (ng/dl) | 563.7 | 471 | 0.15 |
| FSH (IU/ml) | 11.6 | 8.06 | 0.08 |
| LH (IU/ml) | 6.9 | 6.5 | 0.74 |
| Semen analysis characteristics | |||
| Volume (cc) | 2.8 | 2.6 | 0.74 |
| Concentrati on (million/c) | 1.49 | 4.1 | <0.05 |
| Total count (million) | 3.6 | 9 | <0.05 |
| Motility (%) | 13.4 | 27.6 | <0.05 |
| TMSC (million) | 0.77 | 2.35 | <0.005 |
| Viability | 31.3 | 33.1 | 0.87 |
FSH: follicle-stimulating hormone; LH: luteinizing hormone; TMSC: total motile sperm count.
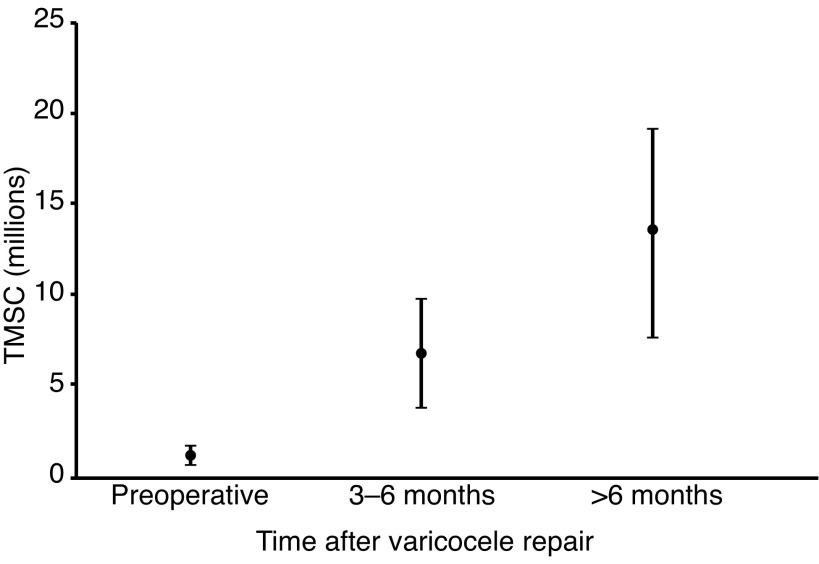
Of the 33 men with TMSC <5 million, 10 had followup semen analysis results at 3–6 month and >6 months postoperatively. Using the longitudinal data, TMSC improved from a mean of 1.1±0.5 million preoperatively, to 6.8±3.1 million at 3–6 months, to 13.4±5.8 million >6 months (Fig. 2). Among these 10 men, four men upgraded by 3–6 months, and an additional one man upgraded at >6 months. Although we noticed a continued improvement in TMSC among men with preoperative TMSC <5 million, there was no statistical difference in TMSC between 3–6 months and >6 months.
Fig. 2.
Men with preoperative total motile sperm count (TMSC) <5 million with followup semen analysis at both 3–6 month and >6 months (n=10).
We were able to reach 24 (72.7%) of the 33 men with TMSC <5 million at least six months after varicocele repair by phone interview. A total of 20 were attempting pregnancy and remaining four were not actively trying. Of these 20 couples, 5/20 (25%) had conceived naturally (mean female age 36.2±4.3 years old), one was undergoing intracytoplasmic sperm injection (ICSI), while the remaining 14 were still attempting (mean female age 32.1±3.8 years old). For men with TMSC 5–9 million, five (50%) of the 10 were contacted. Of the five couples, four were attempting pregnancy. One couple (25%) had a natural pregnancy (35-year-old partner), one had a miscarriage, and the remaining two were still attempting.
Discussion
We set out to evaluate how long it takes for men with TMSC <5 million to recover spermatogenesis after varicocelectomy, and assessed for preoperative predictors of success. We obtained preoperative physical examination, hormone and semen analysis information, as well as postoperative semen analysis at 3–6 months and >6 months postoperatively. Our data show the greatest improvement in TMSC occurs at 3–6 months postoperatively in men with severe oligospermia, with continued, although not significant improvement at >6 months. Additionally, evaluation of our data showed that the majority of men who upgraded did so by 3–6 months. Lastly, preoperative TMSC >2 million was the only predictive factor for upgrading semen quality for men with TMSC <5 million. These results are important in counselling couples on when to consider moving forward with ART and providing realistic expectations of improvement after varicocelectomy.
There has been significant reporting of the beneficial effects of varicocele repair in men with oligospermia; however, few studies focus on men with severe oligospemia and in particular those with TMSC <5 million. Men with TMSC <5 million are a challenging population because many reproductive endocrinologists believe that their only chance of pregnancy is with IVF. Previously published literature demonstrated that varicocelectomy, a procedure often covered by medical insurers, can potentially improve semen parameters enough to make couples eligible for less invasive and less expensive forms of ART or even natural pregnancy.8
A common question among infertile couples contemplating varicocele repair is, “How long does it take for semen parameters to improve”? This question is important for multiple reasons. First, knowing when to expect improvement gives the physician a timeframe to gauge success and decide if additional workup and treatment is needed. Second, depending on the severity of oligospermia and age of the female partner, the decision to pursue varicocelectomy may be abandoned for ART if the chances of improvement are low. Lastly, answering this question provides the couple and the physician with realistic expectations if semen parameters have not improved within a certain timeframe.
In our study, we used TMSC as the primary outcome for two reasons. First, TMSC is reflective of three individual semen parameters (volume, concentration, and motility) and we therefore believe this to be a better representation of overall semen quality than any other individual parameter. Second, TMSC is the parameter used when determining eligibility for ART. The cutoffs we used in this study were based on previously published data.6,9 TMSC <5 million was selected for requiring ICSI and IVF, and TMSC of 9 million was used for natural pregnancy because this is the calculated value from the 2010 WHO lower limit of normal semen analysis criteria.10,11
There are very few studies evaluating to time to spermatogenesis recovery after vaircocelectomy. Al Bakri et al7 published on men with oligospermia who showed improvements by three months (similar to duration of one speramtogenic cycle). However, what was not assessed in Bakari’s manuscript was the subgroup of men with more severe spermatogenic failure, specifically men with TMSC <5 million/cc. Additionally, Al Bakri’s study did not evaluate any long-term data for men with multiple followup semen analyses. We hypothesized that men with severe oligospermia may take longer to recover, as there may be more severe underlying pathology. However, our results suggest that recovery is greatest in the 3–6-month period, even for men with TMSC <5 million.
Identifying favourable preoperative factors of success is especially important in the group of men with TMSC <5 because we can improve patient selection and counselling. Our analysis showed that among men with TMSC <5 million, having a TMSC >2 million preoperatively has the greatest chance of upgrading. This finding makes some intuitive sense and is consistent with previously published data that evaluated preoperative TMSC.4 Other preoperative parameters, such as FSH, were not significantly predictive, in opposition to previously published studies.12 In fact, in our study 75% (9 of 12) of these men with preoperative TMSC >2 million upgraded into range suitable for natural pregnancy (> 9million) (Table 1). Interestingly, none upgraded into IUI range, instead upgrading into natural pregnancy range, however, this is likely due to our small sample size (n=33).
Our study has both strengths and limitations. Strengths of our study are that all semen analyses were performed in the same lab and at least two semen analyses were evaluated. Additionally, we present pregnancy data in men with severe oligospermia. To our knowledge, we are the first study to evaluate time to and predictors of upgrading semen quality in the subgroup of men with TMSC <5million. Limitations of our study include its retrospective nature and small sample size. Unlike previously reported data, we were able to obtain long-term followup for a small subset of men. Because of clinical practice patterns, there are several reasons why continued followup with semen analysis following varicocele repair is challenging: improvement at first semen analysis (typically between 3 and 6 months), couple becomes pregnant, couple decides to pursue ART. Therefore, there is likely a sampling bias in those with longitudinal followup, as they likely did not have adequate improvement at the first postoperative semen analysis or did not pursue ART.
Conclusion
Men with TMSC <5 million appear to have best improvement in semen parameters by six months, with modest improvements thereafter. This data can be used to counsel patients on undergoing ART if semen parameters have not improved by six months following varicocele repair in men with severe oligospermia.
Footnotes
Competing interests: Dr. Masterson has been a consultant for Aytu Biosciences; was the recipient of an investigator-initiated grant from Endo Pharmaceuticals; and participated in the University of Miami’s phase 4 clinical trial on Natesto® effects of reproductive hormones and semen parameters. The remaining authors report no competing personal or financial interest related to this work.
This paper has been peer-reviewed.
References
- 1.Wein AJ, Kavoussi LR, Campbell MF. In: Campbell-Walsh urology/editor-in-chief, Alan J. Wein. 10th ed. Kavoussi Louis R, et al., editors. Philadelphia, PA: Elsevier Saunders; 2012. [Google Scholar]
- 2.Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy. A critical analysis. Urol Clin North Am. 1994;21:517–29. [PubMed] [Google Scholar]
- 3.Smit M, Romijn JC, Wildhagen MF, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2010;183:270–4. doi: 10.1016/j.juro.2009.08.161. [DOI] [PubMed] [Google Scholar]
- 4.Enatsu N, Yamaguchi K, Chiba K, et al. Clinical outcome of microsurgical varicocelectomy in infertile men with severe oligozoospermia. Urology. 2014;83:1071–4. doi: 10.1016/j.urology.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 5.Borges E, Jr, Setti AS, Braga DPAF, et al. Total motile sperm count has a superior predictive value over the WHO 2010 cutoff values for the outcomes of intracytoplasmic sperm injection cycles. Andrology. 2016;4:880–6. doi: 10.1111/andr.12199. [DOI] [PubMed] [Google Scholar]
- 6.Samplaski MK, Lo KC, Grober ED, et al. Varicocelectomy to “upgrade” semen quality to allow couples to use less invasive forms of assisted reproductive technology. Fertil Steril. 2017;108:609–12. doi: 10.1016/j.fertnstert.2017.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Al Bakri A, Lo K, Grober E, et al. Time for improvement in semen parameters after varicocelectomy. J Urol. 2012;187:227–31. doi: 10.1016/j.juro.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 8.Dubin JM, Greer AB, Kohn TP, et al. Men with severe oligospermia appear to benefit from varicocele repair: A cost-effectiveness analysis of assisted reproductive technology. Urology. 2018;111:99–103. doi: 10.1016/j.urology.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Cayan S, Erdemir F, Ozbey I, et al. Can varicocelectomy significantly change the way couples use assisted reproductive technologies? J Urol. 2002;167:1749–52. doi: 10.1016/S0022-5347(05)65192-0. [DOI] [PubMed] [Google Scholar]
- 10.Khalil MR, Rasmussen PE, Erb K, et al. Homologous intrauterine insemination. An evaluation of prognostic factors based on a review of 2473 cycles. Acta Obstetricia Et Gynecologica Scandinavica. 2001;80:74–81. doi: 10.1080/791201839. [DOI] [PubMed] [Google Scholar]
- 11.Hajder M, Hajder E, Husic A. The effects of total motile sperm count on spontaneous pregnancy rate and pregnancy after IUI treatment in couples with male factor and unexplained infertility. Med Arch. 2016;70:39–43. doi: 10.5455/medarh.2016.70.39-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujisawa M, Dobashi M, Yamasaki T, et al. Therapeutic strategy after microsurgical varicocelectomy in the modern assisted reproductive technology era. Urol Res. 2002;30:195–8. doi: 10.1007/s00240-002-0253-6. [DOI] [PubMed] [Google Scholar]