Abstract
Introduction
This single-centre, retrospective study aimed to assess the efficacy and safety of flexible ureteroscopy (FURS) combined with holmium laser lithotripsy in treating children with upper urinary tract stones.
Methods
From June 2014 to October 2015, a total of 100 children (74 boys and 26 girls) with upper urinary tract stones were treated using FURS. A 4.7 Fr double-J stent was placed two weeks before operation. Patients were considered stone-free when the absence of residual fragments was observed on imaging studies. The preoperative, operative, and postoperative data of the patients were retrospectively analyzed.
Results
A total of 100 pediatric patients with a mean age of 3.51±1.82 years underwent 131 FURS and holmium laser lithotripsy. Mean stone diameter was 1.49±0.92 cm. Average operation time was 30.8 minutes (range 15–60). The laser power was controlled between 18 and 32 W, and the energy maintained between 0.6 and 0.8 J at any time; laser frequency was controlled between 30 and 40 Hz. Complications were observed in 69 (69.0 %) patients and classified according to the Clavien system. Postoperative hematuria (Clavien I) occurred in 64 (64.0 %) patients. Postoperative urinary tract infection with fever (Clavien II) was observed in 8/113 (7.1%) patients. No ureteral perforation and mucosa avulsion occurred. The overall stone-free rate of single operation was 89/100 (89%). Stone diameter and staghorn calculi were significantly associated with stone-free rate.
Conclusions
FURS and holmium laser lithotripsy is effective and safe in treating children with upper urinary tract stones.
Introduction
Urinary stone disease (USD) remains a clinical challenge. Indeed, about one in 11 individuals in the U.S. are affected by kidney stones in their lifetime;1 with a prevalence similar to that of diabetes, USD represents one of the most expensive urological conditions, with healthcare charges exceeding $10 billion annually.2 Unfortunately, its incidence has increased among young patients, particularly women and black patients in the past few years.3,4 Treatment of children with urinary stones has always been a challenge for urologists.5 The current treatment for pediatric patients with urinary calculi is based on adult procedures, including extracorporeal shockwave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), ureteroscopy lithotripsy (URL), and laparoscopic ureterolithotomy.6–9 Due to their particular physiological characteristics, surgical intervention methods for pediatric nephrolithiasis should be approached differently compared to adults.
Flexible ureteroscopy (FURS) has been applied in recent years to the treatment of urinary stones. FURS presents overt advantages over other techniques, including improved resolution and increased optical field, high stone-free rate, reduced risk of bleeding, limited surgical injury, good repeatability, and speedy recovery; in addition, further miniaturization is possible.10–12 In children and infants, who have a relatively high stone recurrence rate,13 FURS could be performed repeatedly. FURS and holmium laser lithotripsy in treating infants and children has been previously assessed in the literature;14–16 however, most reports were limited in sample size.
Methods
This was a retrospective study of 100 children (74 boys and 26 girls) who underwent FURS and holmium laser lithotripsy (FURL) for upper urinary tract stones between June 2014 and October 2015 at our hospital, Beijing Friendship Hospital.
The selection criteria for the procedure included SWL-refractory stones, upon parent’s and/or surgeon’s preference. Preoperative imaging scans, including a plain abdominal radiograph (KUB), urinary ultrasound (USG), low-dose non-contrast computerized tomography (NCCT), and/or intravenous urogram (IVP) were obtained from all patients. The stone size was taken as the longest diameter measured on CT or cumulative stone diameter defined as the sum of longest diameter of each stone. A urine sample was obtained for routine urinalysis and bacterial culture before the operation. An indwelling 4.7 Fr double J-stent (Bloomington, COOK Company, U.S.) was placed for two weeks in advance, with the length derived as age+10 (cm), according to a previous report.17
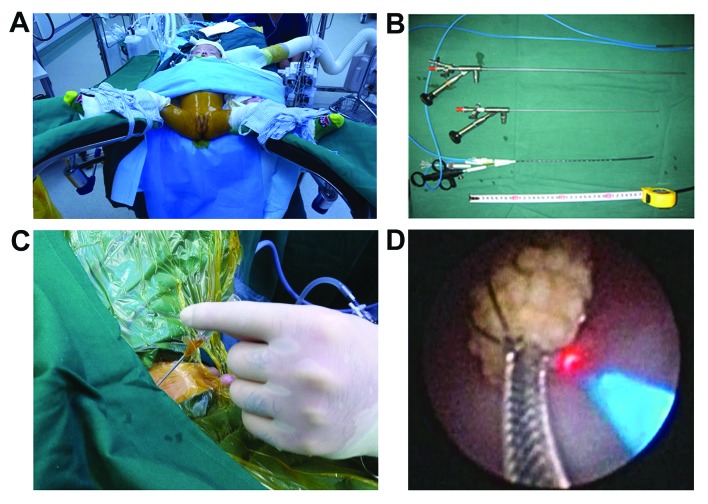
The operations were completed by a urologic surgeon (JL) with more than 10 years’ experience in treating urolithiasis. After induction of general anesthesia using a laryngeal mask for airway management, prophylactic intravenous antibiotics (200 mg/kg/d fosfomycin dissolved in 5% glucose solution or glucose-sodium chloride solution) were administered. Then, a pediatric forced-air warming blanket (Fig. 1A) was placed, with the surgical field disinfected with iodine prewarmed to 36°C. The double J-stent was removed with an 8.0/9.8 Fr or 4.5/6.5 Fr rigid ureteroscope (WOLF Company, Germany). A 14 G trocar (outer diameter 2.108 mm) was used to perform a suprapubic puncture cystostomy to allow fluid drainage from the bladder during operation (Fig. 1B),which was first introduced for such operations.
Fig. 1.
Surgical procedure and key materials.
The ureter was explored through an 8.0/9.8 Fr or 4.5/6.5 Fr ureteroscope, and stones located in the ureteropelvic junction were pushed into the renal pelvis softly. For stones located in other places, FURL was performed directly if the ureter was not narrow or circuitous. A POLY flexible ureteroscope (PolyDiagnost, Germany) (Fig. 1C) was placed into the target ureter or renal pelvis alongside the ureteral access sheath (UAS) (9.5/11.5 Fr). All stones were thoroughly smashed, and the fragments were flushed into the renal pelvis. A 200 μm holmium laser optical fiber was connected to the ureteroscope to perform lithotripsy. The stones in lower calyx were moved by the nickel-titanium reticular basket before laser lithotripsy (Fig. 1D). Laser frequency was 30–40 Hz and energy was 0.6–0.8 J. Low-energy laser was used for lithotripsy, which could shatter the stones into powder, promote the excretion of stone debris, and reduce the incidence of “stone street” after the operation. The laser power could be increased to 0.8 J for cystine stones. During surgery, perfusion pressure of the irrigating fluid did not exceed 40 cmH2O, with irrigating fluid volume ≤1000 ml.
All children underwent abdominal radiography on the first postoperative day to confirm the position of the double J-stent. The double J-stent was removed four weeks after operation if retained intraoperatively. Kidney ultrasound and KUB were reexamined every three months in the first year, and every six months the following years. Clinically insignificant residual fragments (CIRFs) were recorded.18
Patients were considered stone-free if residual fragments <4 mm were observed on imaging studies, which were performed at one month following the operation. If residual calculi >4 mm were observed, second-stage retrograde intrarenal surgery (RIRS) was performed. Patients with residual calculi <4 mm continued to the followup.
General information, perioperative signs and symptoms, laboratory data, respective examination results, operation safety indicators (such as operation time, laser power, perfusion volume), and postoperative followup data were collected for all patients.
Quantitative data were expressed as mean±standard deviation (SD). Multivariate logistic regression was performed to identify the factors associated with stone-free status. Data were analyzed with SPSS ver. 17.0 (IBM Co., Armonk, NY, U.S). P<0.05 was considered statistically significant.
Results
There were 25, 45, and 30 cases of ureteral-, kidney-, and coexisting renal and ureteral calculi, respectively. The mean age of the patients was 3.51±1.82 years, (range 4–168); mean stone diameter was 1.49±0.92 cm (range 0.5–3). Table 1 shows the patient and stone characteristics.
Table 1.
Baseline characteristics of patients and stone
| Mean age (years) | 3.51±1.82 (4–168 months) |
| Male/female | 74/26 |
| Stone diameter (cm) | 1.49±0.92 (0.5–3) |
| Lateralization (L/R/B) | 42/39/19 |
| Stone location | |
| Renal pelvis | 23 |
| Upper pole calyx | 11 |
| Mid pole calyx | 13 |
| Lower pole calyx | 28 |
| Ureter | 55 |
| Symptom | |
| Back pain | 26 |
| Hematuria | 26 |
| Fever | 8 |
| Symptomless | 40 |
B: bilateral; L: left; R: right.
A total of 100 pediatric patients underwent 131 FURL. Nineteen patients had bilateral stones and we recorded it as two FURS if the patient had lithotripsy on both sides in stage I. Twelve patients required repeat operations and only one needed a third operation. Average operation time was 30.8 min (range 15–60), with a mean volume of perfusate of 442.7 ml (200–1000). The laser power was controlled between 18 and 32 W, and the energy maintained between 0.6 and 0.8 J at any time; laser frequency was controlled between 30 and 40 Hz. Complications were observed in 69 (69.0 %) patients and classified according to the Clavien system. Postoperative hematuria (Clavien I) occurred in 64 (64.0%) patients and was resolved with hydration. Postoperative urinary tract infection with fever (Clavien II) was observed in 8/113 (7.1%) patients and treated with antibiotics. No ureteral perforation and mucosa avulsion occurred (Table 2).
Table 2.
Perioperative and operative outcome (n=100)
| Operative time (min) | 30.8±8.78 (15–60) |
| Volume of perfusate (ml) | 442.7±109.72 (200–1000) |
| Laser time (sec) | 370.09±51.98 |
| Laser frequency (Hz) | 32.21±4.24 (30–40) |
| Laser power (W) | 25.25±4.60 (18–32) |
| Duration of hospitalization (d) | 3.30±0.84 |
| Complication rate | 69 (69%) |
| Stone-free rate | 89 (89%) |
Data are mean ± standard deviation (range).
The overall stone-free rate of single operation was 89/100 (89%). Several factors were assessed for their associations with stone-free rate, including age, gender, stone diameter, stone location, staghorn calculi, and hydronephrosis. Only stone diameter and staghorn calculi were significantly associated with stone-free rate; these two variables were confirmed as significant risk factors for stone-free rate (stone diameter odds ratio [OR] 3.274; 95% confidence interval [CI] 1.124–9.533; p=0.03; staghorn calculi OR 13.193; 95% CI 1.881–92.537; p=0.009) (Table 3).
Table 3.
Univariate and multivariate analyses for the identification of factors associated with stone-free rate
| Risk factors | Univariate OR (95% CI) | p | Multivariate OR (95% CI) | p |
|---|---|---|---|---|
| Age | 1.010 (0.860–1.185) | 0.907 | ||
| Gender | 2.538 (0.705–9.135) | 0.154 | ||
| Stone diameter (cm) | 4.178 (1.156–11.292) | 0.005 | 3.274 (1.124–9.533) | 0.030 |
| Stone location | 1.051 (0.502–2.198) | 0.896 | ||
| Staghorn calculi | 24.857 (3.855–160.296) | 0.001 | 13.193 (1.881–92.537) | 0.009 |
| Hydronephrosis | 0.856 (0.290–2.527) | 0.779 |
CI: confidence interval; OR: odds ratio.
Stone analysis was available in 65 patients. The stone composition was calcium oxalate in 38 patients, cystine in 10 patients and magnesium ammonium phosphate in 17 patients. Two children were diagnosed with primary hyperoxaluria.
Discussion
The standard procedures to treat stones in children are similar to those used in adults.6–9 A prospective study of 60 preschool children demonstrated that FURL is as safe as ESWL, but with a higher stone-free rate (86.6% vs. 70.0%).19 In a recent study, 100 SWL and 46 FURS were conducted in 69 children. The stone-free rate after one procedure was almost two times higher in the FURS group compared with the SWL group (37% vs. 21%; p=0.04) without increasing the complication rate (21.7% vs. 16%; p=0.31).20 For large or complex renal stones in pediatric patients, PCNL monotherapy has the advantage of improved stone-free rates, while RIRS decreases radiation exposure, complications, and hospital stay.21 As in adults, PCNL is recommended as a first-line treatment of choice for renal stones larger than 2 cm in children.22 In children with urinary calculi, kidney volume is only about half that of an adult, making puncture more challenging with increased risk of hemorrhage and other complications. The development of scar tissues after PCNL23 may also affect development of the infant kidney. Also, many infant urinary calculi are caused by metabolic disturbance and are therefore likely to recur.24–26 In this study, we found two children had primary hyperoxaluria, an autosomal-recessive disease, and 10 children presented with cystine calculi. These children may need more than one operation in their lifetime.
Although 50 years have elapsed since Marshall first described the inspection of a ureteral calculus with a flexible ureteroscope, the wide application of this technique in the diagnosis and treatment of upper urinary tract disease is relatively recent.27 FURS is considered the first choice for children with lower calyceal stones <15 mm in diameter.28 Galal and colleagues reported that the main FURS complications in children with ureteral calculi were clinically insignificant hematuria, renal colic, and fever.29 Jurkiewicz and colleagues reported a stone-free rate of 85.3% in a cohort of 157 juveniles (10 months to 17 years) using FURL.30
Stone size is a critical factor influencing the primary stone-free rate. The largest and smallest stones in the current cohort measured 3.5×2.5 cm and 0.4×0.5 cm, respectively, and an overall stone-free rate of 89% was obtained. Stone diameter is a significant risk factor for stone-free rate. The Children’s Hospital of Philadelphia (U.S.) reported stone-free rates of 100% and 97% for individuals with stones <10 mm and ≥10 mm in diameter, respectively; analysis of recurrence and complications over a median followup of 19.7 months suggested that FURS is a safe and effective means of treating upper ureteral stones and stones in the lower renal calyx.17 Unsal and colleagues reported a stone-free rate of 100% for stones <10 mm diameter and 81.8% for larger stones in a group of 16 children who underwent FURS and holmium laser lithotripsy.14 Jurkiewicz and colleagues reported a stone-free rate of 85.3% in their cohort of 157 juveniles (aged between 10 months and 17 years) using FURS and holmium laser lithotripsy: primary stone-free rate reached 85.3%, and total stone-free rate was 98.1%; only three patients had complications.30 Furthermore, Chedgy assessed 21 patients, and 13 (62%) were stone-free after the first procedure, 17 (81%) after a second one, and 20 (95%) after a third operation.15 Ishii carried out a meta-analysis of six studies, including 282 cases of juveniles (0.25–17 years) that underwent FURL.16 The primary stone-free rate in three articles was 85.8% (58.0–93.0%), while total complication rate was 12.4%; only five cases had Clavien class III complications. Taken together, these findings demonstrate that FURL is safe and effective in pediatric patients with stone dimeter around 1 cm.
In our study, we had a double J-stent placed in advance. This made ureteral access sheath (UAS) placement successful in all patient. According to previous study, a UAS placement is possible in 94.1 % of pre-stented patients, but in only 50 % of non-stented patients.31 The use of a UAS during RIRS has been associated with reduced intrarenal pressure, decreased operative time, and improved stone-free rates in adult patients.32 We therefore placed a double J-stent in all patients in advance. No ureteral wall injury occurred in our patients.
The limiting pressure within the urinary tract is also critical; the outflow must be unobstructed. Suprapubic puncture cystostomy may be required to achieve constant drainage. Close attention should be paid to preventing intraoperative hypothermia. We recommended using prewarming irrigation, a forced-air warming blanket, insulating the head, and maintaining a relatively high operating room temperature. Finally, we recommend that laser power be limited to 32 W to avoid mucosal damage while disrupting calculi. It is better to modulate the laser with high frequency and low power.
A few limitations should be mentioned for this study. It was a single-centre, retrospective cohort study with a relatively short followup time. Also, a control group of patients treated with PCNL or ESWL was not included. The suprapubic puncture cystotomy was for decompression of the bladder. More research should prove that this procedure decreases complication rates. Further randomized controlled studies are warranted to compare the two methods for advantages and disadvantages.
Conclusion
With sufficient preoperative preparation and skilled operative manipulation, FURL has a high stone-free rate and is clinically safe for upper urinary tract stones in children.
Acknowledgments
This work was supported by the Research Foundation of Beijing Friendship Hospital, Capital Medical University (NO. yyqdkt2017-2) and the Beijing Municipal Administration of Hospital’s Youth Program (QML20150103).
Footnotes
Competing interests: The authors report no competing personal or financial interest related to this work.
This paper has been peer-reviewed.
References
- 1.Scales CD, Jr, Smith AC, Hanley JM, et al. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–5. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scales CD, Jr, Tasian GE, Schwaderer AL, et al. Urinary stone disease: Advancing knowledge, patient care, and population health. Clin J Am Soc Nephrol. 2016;11:1305–12. doi: 10.2215/CJN.13251215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hesse A. Reliable data from diverse regions of the world exist to show that there has been a steady increase in the prevalence of urolithiasis. World J Urol. 2005;23:302–3. doi: 10.1007/s00345-005-0033-3. [DOI] [PubMed] [Google Scholar]
- 4.Tasian GE, Ross ME, Song L, et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol. 2016;11:488–96. doi: 10.2215/CJN.07610715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minevich E, Sheldon CA. The role of ureteroscopy in pediatric urology. Curr Opin Urol. 2006;16:295–8. doi: 10.1097/01.mou.0000232053.74342.e9. [DOI] [PubMed] [Google Scholar]
- 6.Sen H, Seckiner I, Bayrak O, et al. Treatment alternatives for urinary system stone disease in preschool-aged children: Results of 616 cases. J Pediatr Urol. 2015;11:34e1–5. doi: 10.1016/j.jpurol.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Ishii H, Griffin S, Somani BK. Ureteroscopy for stone disease in the pediatric population: A systematic review. BJU Int. 2015;115:867–73. doi: 10.1111/bju.12927. [DOI] [PubMed] [Google Scholar]
- 8.Thomas JC. How effective is ureteroscopy in the treatment of pediatric stone disease? Urol Res. 2010;38:333–5. doi: 10.1007/s00240-010-0293-2. [DOI] [PubMed] [Google Scholar]
- 9.Smaldone MC, Docimo SG, Ost MC. Contemporary surgical management of pediatric urolithiasis. Urol Clin North Am. 2010;37:253–67. doi: 10.1016/j.ucl.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Almeras C, Daudon M, Ploussard G, et al. Endoscopic description of renal papillary abnormalities in stone disease by flexible ureteroscopy: A proposed classification of severity and type. World J Urol. 2016;34:1575–82. doi: 10.1007/s00345-016-1814-6. [DOI] [PubMed] [Google Scholar]
- 11.Zhu X, Song L, Xie D, et al. Animal experimental study to test application of intelligent pressure control device in monitoring and control of renal pelvic pressure during flexible ureteroscopy. Urology. 2016;91:242.e11–5. doi: 10.1016/j.urology.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 12.Rassweiler J, Rassweiler MC, Klein J. New technology in ureteroscopy and percutaneous nephrolithotomy. Curr Opin Urol. 2016;26:95–106. doi: 10.1097/MOU.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 13.Oral I, Nalbant I, Ozturk U, et al. Our experience with percutaneous nephrolithotomy in pediatric renal stone disease. Turk J Urol. 2013;39:35–8. doi: 10.5152/tud.2013.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unsal A, Resorlu B. Retrograde intrarenal surgery in infants and preschool-age children. J Pediatr Surg. 2011;46:2195–9. doi: 10.1016/j.jpedsurg.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Chedgy EC, Griffin SJ, Dyer JP, et al. Ureteroscopy for paediatric renal tract stones — outcomes from a tertiary European centre. Urol Int. 2015;95:320–3. doi: 10.1159/000380857. [DOI] [PubMed] [Google Scholar]
- 16.Ishii H, Griffin S, Somani BK. Flexible ureteroscopy and lasertripsy (fursl) for pediatric renal calculi: Results from a systematic review. J Pediatr Urol. 2014;10:1020–5. doi: 10.1016/j.jpurol.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Kim SS, Kolon TF, Canter D, et al. Pediatric flexible ureteroscopic lithotripsy: The Children’s Hospital of Philadelphia experience. J Urol. 2008;180:2616–9. doi: 10.1016/j.juro.2008.08.051. [DOI] [PubMed] [Google Scholar]
- 18.Assimos DG. Re: Clinically insignificant residual fragments: Is it an appropriate term in children? J Urol. 2016;195:170. doi: 10.1016/j.juro.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Mokhless IA, Abdeldaeim HM, Saad A, et al. Retrograde intrarenal surgery monotherapy vs. shock wave lithotripsy for stones 10–20 mm in preschool children: A prospective, randomized study. J Urol. 2014;191:1496–9. doi: 10.1016/j.juro.2013.08.079. [DOI] [PubMed] [Google Scholar]
- 20.Freton L, Peyronnet B, Arnaud A, et al. Extracorporeal shockwave lithotripsy vs. flexible ureteroscopy for the management of upper tract urinary stones in children. J Endourol. 2017;31:1–6. doi: 10.1089/end.2016.0313. [DOI] [PubMed] [Google Scholar]
- 21.Saad KS, Youssif ME, Al Islam Nafis Hamdy S, et al. Percutaneous nephrolithotomy vs. retrograde intrarenal surgery for large renal stones in pediatric patients: A randomized controlled trial. J Urol. 2015;194:1716–20. doi: 10.1016/j.juro.2015.06.101. [DOI] [PubMed] [Google Scholar]
- 22.Turk C, Petrik A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–82. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 23.Wood K, Keys T, Mufarrij P, et al. Impact of stone removal on renal function: A review. Rev Urol. 2011;13:73–89. [PMC free article] [PubMed] [Google Scholar]
- 24.Copelovitch L. Urolithiasis in children: Medical approach. Pediatr Clin North Am. 2012;59:881–96. doi: 10.1016/j.pcl.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Granberg CF, Baker LA. Urolithiasis in children: Surgical approach. Pediatr Clin North Am. 2012;59:897–908. doi: 10.1016/j.pcl.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Alpay H, Ozen A, Gokce I, et al. Clinical and metabolic features of urolithiasis and microlithiasis in children. Pediatr Nephrol. 2009;24:2203–9. doi: 10.1007/s00467-009-1231-9. [DOI] [PubMed] [Google Scholar]
- 27.Marshall VF. Fiber optics in urology. J Urol. 1964;91:110–4. doi: 10.1016/S0022-5347(17)64066-7. [DOI] [PubMed] [Google Scholar]
- 28.Gecit I, Pirincci N, Gunes M, et al. Should ureteroscopy be considered as the first choice for proximal ureter stones of children? Eur Rev Med Pharmacol Sci. 2013;17:1839–44. [PubMed] [Google Scholar]
- 29.Galal EM, Fath El-Bab TK, Abdelhamid AM. Outcome of ureteroscopy for treatment of pediatric ureteral stones. J Pediatr Urol. 2013;9:476–8. doi: 10.1016/j.jpurol.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 30.Jurkiewicz B, Zabkowski T, Samotyjek J. Ureterolithotripsy in a pediatric population: A single institution’s experience. Urolithiasis. 2014;42:171–6. doi: 10.1007/s00240-013-0634-z. [DOI] [PubMed] [Google Scholar]
- 31.Erkurt B, Caskurlu T, Atis G, et al. Treatment of renal stones with flexible ureteroscopy in preschool age children. Urolithiasis. 2014;42:241–5. doi: 10.1007/s00240-013-0636-x. [DOI] [PubMed] [Google Scholar]
- 32.L’Esperance O, Ekeruo WO, Scales CD, Jr, et al. Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology. 2005;66:252–5. doi: 10.1016/j.urology.2005.03.019. [DOI] [PubMed] [Google Scholar]