Abstract
Internal resorption is a rare condition in permanent teeth, and may result from trauma, caries, or restorative procedures. Internal resorption is usually asymptomatic and is first identified as a round-shaped enlargement of a root-canal space on routine radiographs. Large resorption defects may result in penetration of the tooth into the periodontium through the cementum. The gold-standard treatment consists of debridement and obturation of the pulp space, sealing of the external communication, and restoration of the normal function of the tooth through a nonsurgical or surgical method. In this case presentation, we report on two methods for repair of internal resorption with perforation. The first method consisted of treating the lower right second premolar by conventional endodontic therapy under a microscope, followed by repair with mineral trioxide aggregate. The second method consisted of surgical treatment of the upper right central incisor. The choice of treatment depends on the size of the perforation, its location, and the ability to approach it for repair.
Keywords: Ca(OH)2, internal root resorption, microscope, mineral trioxide aggregate (MTA), radiography
Introduction
Internal resorption is an unusual condition in permanent teeth. The exact causes of the damage it produces are still unknown. However, it has been proposed that trauma, pulpitis, pulpotomy, a cracked tooth, tooth transplantation, restorative procedures, invagination, orthodontic treatment, and even herpes zoster viral infection are all likely predisposing factors.1
The pulpal side of the dentin is lined by odontoblasts and predentin. Odontoblasts have no resorptive ability and, in combination with the unmineralized predentin, appear to form a barrier against dentin resorption. Internal resorption is preceded by chronic pulpal inflammation, loss of or damage to odontoblasts and the predentin, and invasion of the pulp by macrophage-like resorbing cells.2, 3
Full expansion of the resorption area requires that the pulp is vital. By contrast, partially or completely necrotic coronal pulp areas allow the entrance of microbial antigens via the root canal, thereby favoring continuous bacterial infection.1
Most teeth with internal root resorption are symptom free and are first clinically recognized through routine radiographs. However, when resorption actively progresses, the tooth is only partially vital and may present typical symptoms of pulpitis. If perforation occurs, the infection may prove difficult to control. Teeth with a perforation also have a weaker structure as a result of loss of hard tissue. Although most patients complain of only mild or no pain, perforation is often accompanied by sinus tract formation and swelling.1
The original canal shape is lost at the site of resorption. Therefore, internal resorption is readily identified as a radiolucent, round, symmetrical widening of the root-canal space. Not all cases of internal root resorption progress in a similar fashion, thus, oval and asymmetrical shapes may also be found. Internal resorption is frequently observed in the cervical region but may occur throughout the entire root-canal system. Teeth with coronal resorption may show a pinkish hue due to resorption of the coronal dentin and enamel by prolific capillaries in the pulpal inflammatory tissue.1, 2
Here, we report two cases of perforating internal resorption in which the diagnosis justified the application of two different treatment methodologies.
Case reports
Case 1
A 12-year-old girl was referred to the Endodontic Department of the Taipei Medical University Dental Clinic because of a resorptive lesion in her lower right second premolar. The lesion was identified on a periapical radiograph, which was taken by the referring dentist for observation of a sinus tract in the buccal area. The tooth had been treated at a local dental clinic 2 weeks prior to this examination.
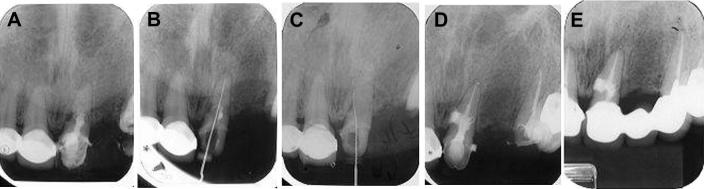
Clinical examination revealed that tooth number 45 was slightly tender to percussion but showed no abnormal sensitivity to palpation or biting. No sinus tract was found in this quadrant. The periodontal condition was normal, with no gingivitis or pocket depths exceeding 3 mm. Her medical history was noncontributory. A radiographic examination revealed an irregular radiolucency in the coronal one-third to two-thirds of the root next to a crescent-shaped radiolucent lesion in the alveolar bone (Fig. 1). Based on the radiographic findings and history, a lesion was diagnosed as perforating internal resorption; the patient had previously been diagnosed with asymptomatic apical periodontitis and therapy had been initiated.
Figure 1.

An irregular radiolucency in the coronal third to middle third of the root next to a crescent-shaped radiolucent lesion in the alveolar bone.
At the first appointment, we removed the temporary sealing under the rubber dam and observed bleeding from the canal. The size of the perforation was unknown, therefore, we used normal saline for irrigation but failed to negotiate the canal. Ca(OH)2 was administered as an intracanal medicament, and the canal was temporarily restored with intermediate restorative material (IRM, Dentsply International/L.D. Caulk Division, Dentsply International Inc., Milford, DE, USA).
The bleeding was controlled, and the canal was negotiated. The perforated site was located under the microscope on the second visit. The working length was determined electronically using an Elements Apex Locator (SybronEndo, Anaheim, CA, USA) and confirmed by radiography (Fig. 2). The canal was cleaned, shaped, and irrigated with 2.5% NaOCl and endosonic instrument (Suprasson P5, Satelec, France). Ca(OH)2 was again administered as an intracanal medicament. Two weeks later, at the third appointment, the canal was irrigated with 2.5% NaOCl and endosonic, and the Ca(OH)2 was replaced in the canal. On the fourth visit, the canal from the apex to the perforation site was obturated using the lateral compaction method with gutta percha and sealer (Sealapex; SybronEndo). The perforation site and the canal above it were sealed with mineral trioxide aggregate4 (MTA, ProRoot; Dentsply/Tulsa Dental, Tulsa, OK, USA) (Fig. 3). Two weeks later, after checking the condition of the MTA, the access cavity was restored with composite resin. The prognosis was positive after 19 months with no symptoms (Fig. 4).
Figure 2.
The canal was negotiated and the perforation site was located under a microscope. The working length was 22 mm, initial apical file (IAF) number 10.
Figure 3.
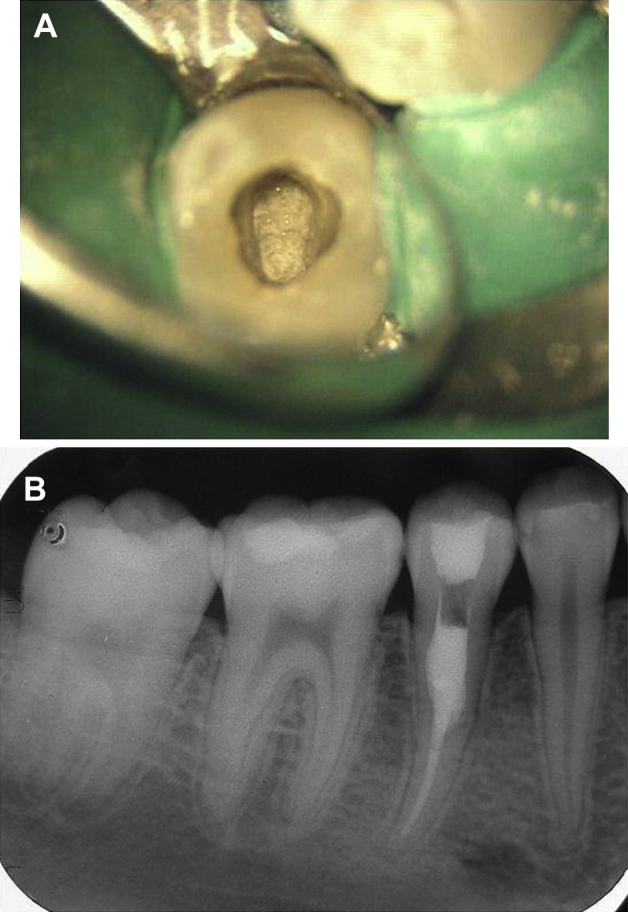
(A) The perforation site and canal above were sealed with mineral trioxide aggregate (MTA). (B) After MTA was applied, the coronal third was sealed with wet cotton and intermediate restorative material.
Figure 4.
After 19 months, there were no symptoms or signs. The prognosis was good.
Case 2
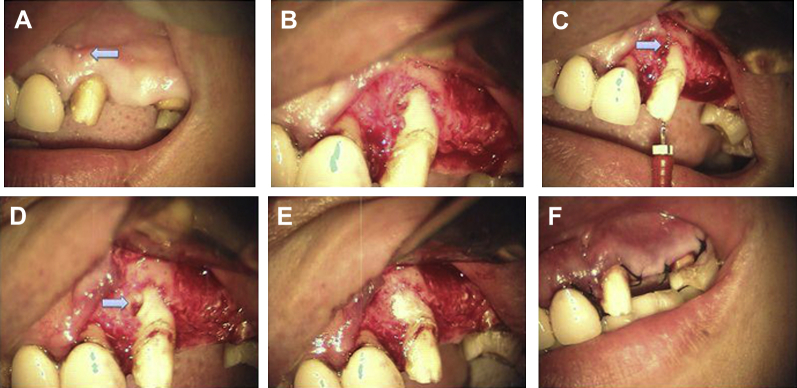
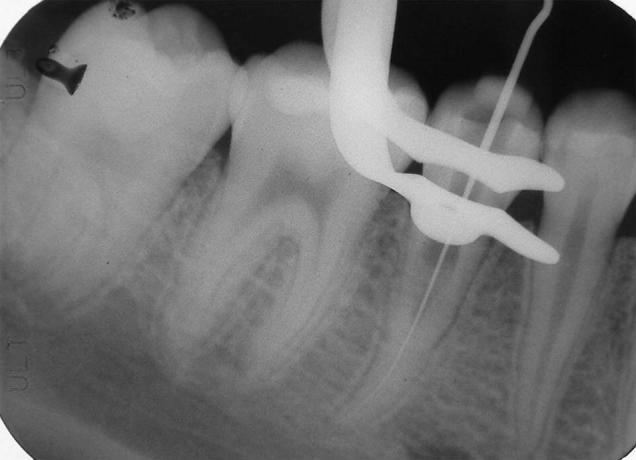
A 49-year-old woman was referred to the Endodontic Department of the Taipei Medical University Dental Clinic because of the presence of a sinus tract and labial gingival swelling after root-canal treatment of the upper left central incisor. Clinical examination revealed that tooth number 21 was sensitive to percussion and palpation. We observed a sinus tract and gingival swelling in the labial side. Pocket depths were within the normal limits. The medical history was noncontributory. A radiographic examination revealed a well-circumscribed, fairly oval, radiopaque lesion in the middle third of the root next to a radiolucent lesion in the alveolar bone. A 2 mm × 3 mm apical lesion surrounded the root apex (Fig. 5A). There was a temporary fixed prosthetic device (FPD) over teeth number 21 and number 23. The coronal portion of tooth number 21 was filled with IRM. Based on the clinical findings, the tooth was diagnosed as having previously been treated, and now having an apical abscess with perforating internal resorption.
Figure 5.
(A) A well-circumscribed, fairy oval radiopaque area in the middle third of the root next to a radiolucent lesion in the alveolar bone. (B) The working length was determined and checked by radiography. (C) The file could go through the perforated site. (D) There was no bleeding from the canal after removing the granulation tissue, and the canal was filled with gutta percha and Grossman's sealer. Seven days later, the condition of the tooth was stable without particular symptoms or signs. (E) After 28 months, there were no symptoms or signs. The prognosis was good.
The tooth was isolated under a rubber dam and accessed without anesthesia. The working length was determined and confirmed by radiography (Fig. 5B and C). The old filling materials were removed, which led to gross canal bleeding. The canal was cleaned, shaped, and irrigated with 2.5% NaOCl and endosonic (Satelec P5). After the bleeding was controlled, Ca(OH)2 was used as an intracanal medicament, and it was changed every 2 weeks. The sinus tract persisted after the canal was cleaned for 2 months. However, the canal could not be completely dried because of continuous exudation and hemorrhage. Thus, we completed treatment by surgical means.
On July 30, 2008, a triangular flap was reflected from tooth number 11 distal to tooth number 23 with vertical release over the distal line angle of tooth number 23 under block anesthesia (Fig. 6A and B). The perforation site was detected at the mesial–labial area of the middle third of the root (Fig. 6C). A bone window was created by a high-speed carbide bur, and the granulation tissue was curetted and sent for specimen analysis (Fig. 6D). No bleeding from the canal occurred after removal of the granulation tissue, and the canal was filled with gutta percha and Grossman's sealer by the lateral compaction method. MTA powder (ProRoot; Dentsply/Tulsa Dental) was mixed according to the manufacturer's instructions with an MTA carrier. The MTA was firmly condensed into the resorption cavity using a plugger and wet cotton pellets under a microscope (Fig. 6E). After the bleeding was totally controlled, the surgical site was sutured with four stitches (Fig. 6F). Seven days later, the stitches were removed. The condition of the surgical site was stable and showed no particular symptoms or signs (Fig. 5D). The patient has routinely been followed up, and further treatment is due. After 28 months, there were no symptoms or signs, and the prognosis was good (Fig. 5E).
Figure 6.
(A) Intraoral photograph prior to surgery. The sinus tract was still there (arrow). (B) The triangular flap was reflected from tooth number 11 to number 23 with vertical release over the distal line angle of tooth number 23. (C) The perforation site was detected (mesial–labial, middle third). (D) A bone window was created with a high-speed bur, and the soft tissue was curetted and sent for examination. (E) The perforation area was restored with mineral trioxide aggregate under a microscope. (F) Suturing with four stitches.
Discussion
Clinical detection of internal resorption is followed by endodontic treatment to arrest and prevent further resorption. When resorption involves external communication with the periodontal ligament space, the perforation site should be repaired prior to completion of treatment.2 Complex surgical procedures may be necessary to gain access to the perforation site. By contrast, traditional procedures may be applied in combination with microscopic methods.
The shape of a resorbed root canal may prevent instrument access to all areas of the canal. However, creating a straight-line access to the resorption site might not be possible in cases in which the tooth is structurally weakened. To circumvent this problem, ultrasound has been suggested for treating internal resorptions. Ultrasound can facilitate penetration of an irrigant to all areas of the root-canal system, while releasing the necrotic tissue in the canal.5
Use of hypochlorite helps control the bleeding from perforation sites. Moreover, it disinfects the perforating area, as previously experienced during accidental perforation complications. However, in the case of large perforations, low-concentration hypochlorite solutions should be used, and other irrigants such as chlorhexidine should be considered.1 For this reason, we used normal saline as an irrigant on the first appointment for Case 1, when the size of the perforation was still unknown.
Ca(OH)2 is used to treat internal resorptions to control bleeding, necrotize the residual pulp tissue, and make the necrotic tissue more soluble to NaOCl. As a result of the limited access by instruments to all areas of a resorption cavity, chemical means are needed to clean the canal. In our treatment protocol, we chose MTA to repair the perforation site because of its good biocompatibility, sealing ability, less leakage, lower overfilling tendency, and non-cytotoxicity. MTA can also stimulate dentin bridge formation. Nevertheless, MTA possesses some disadvantages: a long setting time (2 hours 45 minutes), low compressive strength (should be 3–5 mm thick, it must not be used as permanent filling material as a coronal restoration), and sensitivity to the technique used.6, 7
In the near future, treatment of perforating internal resorptions will consist of a thorough chemomechanical cleaning and disinfection of the root canal and resorption area (including the perforation site), followed by short-term Ca(OH)2 treatment. At the second appointment, in the absence of any clinical symptoms, the resorption cavity can be filled with MTA. In cases of clinical symptoms or complications in the canal, surgical repair and treatment should be considered.1
In the majority of previous studies, the root-canal filling was placed after repair of the perforation defect. By contrast, Hsien et al., Yildirim et al., and Altundasar et al. repaired a root perforation with MTA after root-canal filling had been completed.8, 9, 10 In the present cases, we also preferred sealing the root canal prior to placement of MTA. This procedure has several advantages: it prevents MTA from blocking the root canal space; it allows successful condensation of MTA; and it decreases the risk of displacing MTA from the perforation site during condensation of the gutta percha. Here, we showed that it is possible to provide a sufficiently thick layer of MTA (3–5 mm; Case 1). Finally, we suggest the use of the microscope to perform the procedure better.
The prognosis of treating internal tooth resorption depends on the clinical experience, the structure of the remaining tooth, and the extent of perforation. First, the dentist needs to determine the treatment that offers the best prognosis based on the diagnosis. Second, the remaining tooth should not be structurally too weak. Third, the prognosis of a perforating resorption may be fairly good, yet it depends on the size of the perforation, its location, and possibility of repair. With proper treatment and use of modern endodontic techniques and materials, the treatment outcome of internal tooth resorption is expected to be good.11
References
- 1.Haapasalo M., Endal U. Internal inflammatory root resorption: the unknown resorption of the tooth. Endod Topics. 2006;14:60–79. [Google Scholar]
- 2.Gunra M.N. Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:647–653. doi: 10.1016/s1079-2104(99)70002-8. [DOI] [PubMed] [Google Scholar]
- 3.Hargreaves K.M., Goodis H.E., editors. Seltzer and Bender's Dental Pulp. 3rd ed. Quintessence Publishing; Chicago, IL: 2002. [Google Scholar]
- 4.Torabinejad M., Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25:197–205. doi: 10.1016/S0099-2399(99)80142-3. [DOI] [PubMed] [Google Scholar]
- 5.Stamos D.E., Stamos D.G. A new treatment modality for internal resorption. J Endod. 1986;12:315–319. doi: 10.1016/S0099-2399(86)80116-9. [DOI] [PubMed] [Google Scholar]
- 6.Torabinejad M., Watson T.F., Pitt Ford T.R. The sealing ability of a mineral trioxide aggregate as a retrograde root filling material. J Endod. 1993;19:591–595. doi: 10.1016/S0099-2399(06)80271-2. [DOI] [PubMed] [Google Scholar]
- 7.Torabinejad M., Hong C.U., Pitt Ford T.R. Physical properties of a new root end filling material. J Endod. 1995;21:349–353. doi: 10.1016/S0099-2399(06)80967-2. [DOI] [PubMed] [Google Scholar]
- 8.Hsien H.C., Cheng Y.A., Lee Y.L., Lan W.H., Lin C.P. Repair of perforating internal resorption with mineral trioxide aggregate: a case report. J Endod. 2003;29(8):538–539. doi: 10.1097/00004770-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Yildirim G., Dalci K. Treatment of lateral root perforation with minieral trioxide aggregate: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(5):e55–e58. doi: 10.1016/j.tripleo.2006.04.001. Epub 2006 Sep 7. [DOI] [PubMed] [Google Scholar]
- 10.Altundasar E., Demir B. Management of a perforating internal resorptive defect with mineral trioxide aggregate: a case report. J Endod. 2009;35(10):1441–1444. doi: 10.1016/j.joen.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Caliskan M.K., Turkun M. Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol. 1997;13:75–81. doi: 10.1111/j.1600-9657.1997.tb00014.x. [DOI] [PubMed] [Google Scholar]