Abstract
Recently, there has been interest in whether shift work may enhance susceptibility to infection. Our aim was to determine whether shift workers in the health-care field have a higher incidence, duration, and/or severity of influenza-like illness (ILI) and acute respiratory infection (ARI) than non–shift workers. From September 2016 to June 2017, 501 rotating and/or night-shift workers and 88 non–shift workers from the Klokwerk+ Study (the Netherlands, 2016–2017) registered the occurrence of ILI/ARI symptoms daily using a smartphone application. The incidence rate of ILI/ARI (defined as ≥2 symptoms on the same day/≥1 symptom on 2 consecutive days), the mean duration of each episode, and the incidence rate of severe episodes were compared between shift workers and non–shift workers using negative binomial regression and linear mixed-model analysis. In total, participants completed 110,347 diaries. Shift workers’ incidence rate of ILI/ARI was 1.20 (95% confidence interval (CI): 1.01, 1.43) times higher than that of non–shift workers, and for severe ILI/ARI episodes, shift workers’ incidence rate was 1.22 (95% CI: 1.01, 1.49) times higher. The mean duration of an ILI/ARI episode did not differ (ratio between means = 1.02, 95% CI: 0.87, 1.19). In conclusion, shift workers in health care had more ILI/ARI episodes and more severe ILI/ARI episodes than non–shift workers, but with a similar duration. Insight into underlying mechanisms connecting shift work and infection susceptibility will contribute to the design of preventive initiatives.
Keywords: acute respiratory infection, health-care workers, infection susceptibility, influenza-like illness, night-shift work, occupational health, respiratory infection, shift work
A large part of the labor force works outside of regular 9-to-5 working hours, with almost 1 in 5 European workers working night shifts (1). Persons engaging in shift work, especially night-shift work, experience a disruption of the natural circadian rhythm of biological functions. This circadian rhythm disruption may be an important contributor to shift workers’ increased risk for disorders such as cardiovascular diseases (2, 3). Recently, there has also been interest in whether circadian rhythm disruption may impair immune system function and thereby potentially enhance susceptibility to infection (4–7).
Influenza-like illness (ILI) (including fever) and acute respiratory infection (ARI) (e.g., common cold without fever) are highly common in the general population. Approximately 5%–15% of the population experiences ILI due to influenzavirus annually (8, 9). Because ILI and ARI are caused by a wide range of viruses and bacteria, many other pathogens contribute to the annual incidence of ILI/ARI (9). Besides the individual burden, ILI/ARI has a large societal impact because of associated productivity loss and sickness absence (10, 11) and, for a specific group of shift workers (i.e., health-care workers), creates patient safety issues resulting from potential pathogen transmission (12, 13).
Only a few studies have examined the association between shift work and infectious diseases, such as respiratory infections (14–16). These studies were all based on cross-sectional data, and they generally made use of only 1 retrospective assessment of infections (14–16). The reliability of retrospectively recalled symptoms may be low and subject to bias, in comparison with prospective monitoring of symptoms (17). To accurately determine the occurrence and duration of ILI/ARI episodes, real-time assessment of ILI/ARI symptoms among shift workers and non–shift workers for prolonged periods of time is needed (17). Our aim in this study was to determine whether shift workers in the health-care field were more susceptible to respiratory infections, as defined by incidence of ILI/ARI, than non–shift workers. Furthermore, differences between shift and non–shift workers in duration and severity of ILI/ARI episodes were studied.
METHODS
Study population and design
The present study was part of the Klokwerk+ Study. Klokwerk+ is a prospective cohort study with the main objective of studying associations of shift work with body weight and infection susceptibility (18). The study population consisted of health-care workers aged 18–65 years from 6 different hospitals in the Netherlands. During this study, there were 2 moments of contact with participants: a baseline visit in September–December 2016 and a follow-up visit at the end of the winter season, in April–June 2017. At baseline and follow-up, participants received a questionnaire on demographic characteristics, shift work, lifestyle, and health. Participants were asked to keep a daily record of their ILI/ARI symptoms for the entire period between baseline and the end of follow-up by using a diary application on their smartphone/tablet (Android (Google Inc., Mountain View, California), iOS (Apple Inc., Cupertino, California), or Windows (Microsoft Corporation, Redmond, Washington)). Two of the authors (P.B.-V./E.A.M.S.) developed a mobile phone application with which to detect parent-reported cases of ILI in children. This application appeared to be a useful tool for prospective studies and was further adjusted to make it applicable for the measurement of ILI/ARI among health-care workers in Klokwerk+. An online database was used to transmit data from the app to the researchers.
Approval of the study protocol was obtained from the institutional review board of University Medical Center Utrecht (Utrecht, the Netherlands). Informed consent was obtained from all participants.
Measures
Shift work
In the baseline and follow-up questionnaires, participants completed questions about their shift-work status capturing some of the important domains of shift work (e.g., duration and intensity) mentioned in the international consensus report by Stevens et al. (19). In short, participants reported on their current work schedule, whether they ever worked night shifts (shifts between 00.00 and 06.00 Coordinated Universal Time (UTC)) or rotating shifts (rotating between day (mostly between 07.30 and 16.00 UTC), night (mostly between 23.00 and 07.45 UTC), evening (mostly between 15.00 and 23.00 UTC), and/or sleep shifts), and the number of years they had worked in particular shifts. Participants were considered shift workers if they worked rotating shifts and/or night shifts and were considered non–shift workers if they did not work rotating shifts or night shifts (i.e., they worked day shifts only), at baseline and in the 6 months prior to baseline. For participants who changed their shift-work status during follow-up (n = 16), only the diaries completed up to that point in time were included (Figure 1). All shift workers worked rotating shifts, and the majority of shift workers also worked night shifts (n = 465). The shift workers who worked rotating shifts without night shifts (n = 36) were labeled “non–night-shift workers.” For shift workers, frequency of night shifts (i.e., average number of night shifts per month at baseline) was categorized into 4 groups: none (non–night-shift workers), 1–2 night shifts/month, 3–4 night shifts/month, or ≥5 night shifts/month. Duration of night-shift work (i.e., total number of years of night-shift work at baseline) was also categorized into 4 groups: none (non–night-shift workers), <10 years, 10–19 years, or ≥20 years.
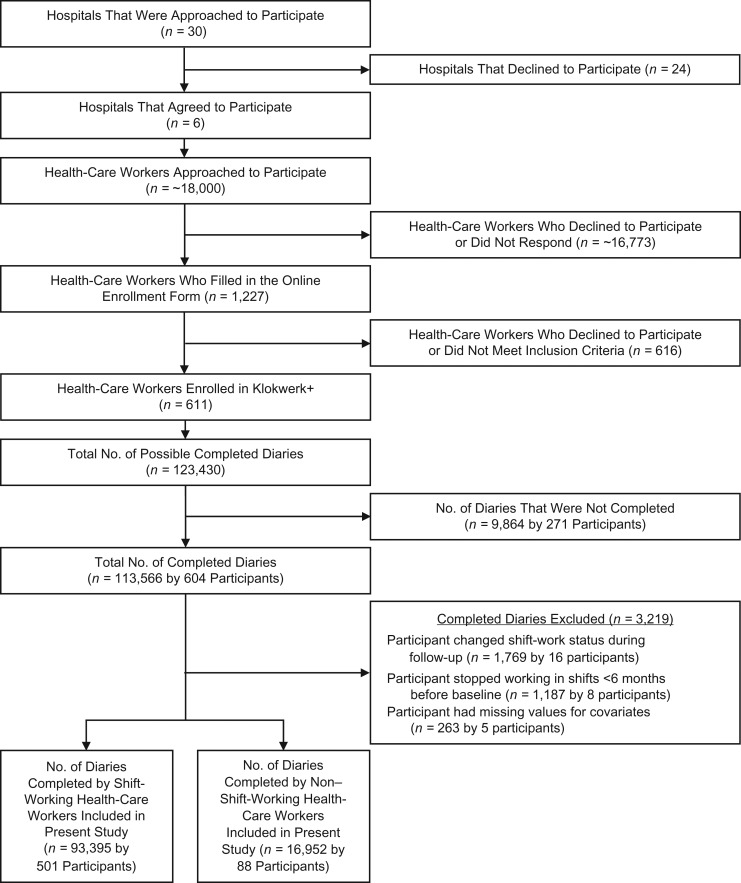
Figure 1.
Selection of participants for a study of shift work and respiratory infections in health-care workers, Klokwerk+ Study, the Netherlands, 2016–2017.
Infection susceptibility
In this study, the occurrence of ILI and ARI episodes was used as a proxy for infection susceptibility and was measured using the diary application. The app was developed for participants to self-report the presence/absence of the following ILI/ARI symptoms on a daily basis: cough, sore throat, shortness of breath, runny/blocked nose, fever, malaise, hoarseness, and coughed-up mucus (18, 20). Onset and ending of an ILI/ARI episode was automatically detected on the basis of diary entries, using built-in algorithms. Onset of an ILI/ARI episode was defined as having ≥2 symptoms on the same day or ≥1 symptom on 2 consecutive days. An episode ended when the participant did not report symptoms for 2 consecutive days. Because the definition of an ILI/ARI episode is a broad definition with a high incidence, the more severe ILI episodes with the presence of fever were also studied separately. An ILI episode was defined as having fever (>38°C (>100.4°F), based on the “Pel criteria” (21)) and ≥1 other symptom on the same day. After onset of an ILI/ARI episode, participants were also asked to report on a 4-point scale the severity (no burden, mild burden, moderate burden, or severe burden as experienced by the participant) of the aforementioned symptoms and the severity of the following additional symptoms: headache, myalgia, painful breathing, and earache. For fever, answer options were no fever (body temperature ≤38°C (≤100.4°F)), moderate fever (body temperature >38°C (>100.4°F) and <38.5°C (<101.3°F)), severe fever (body temperature ≥38.5°C (≥101.3°F)), or unknown. A severe ILI/ARI episode was defined as having ≥1 symptom graded as severe, ≥2 symptoms graded as moderate, or ≥3 symptoms of any severity at the onset of the episode.
Infection susceptibility was assessed using the following outcome measures:
Incidence rate of ILI/ARI
Mean duration of each ILI/ARI episode in days
Incidence rate of severe ILI/ARI
Occurrence of at least 1 ILI episode (including fever)
Covariates
On the basis of responses to the baseline questionnaire, participants’ age, sex, occupation (nurse vs. other health-care worker (e.g., paramedic or physician)), educational level (high = higher vocational education/university), marital status, smoking status, and general perceived health (measured on a 5-point Likert scale (excellent–bad)) were determined. General perceived health was assessed because it may be associated with shift-work status as well as infection susceptibility. To determine influenza vaccination status (yes vs. no), participants were asked at the follow-up visit whether they had received that year’s seasonal influenza vaccine. For participants whose vaccination status was unknown, vaccination status was determined on the basis of whether they had already received the influenza vaccine or had indicated that they intended to get the vaccine at baseline. Lastly, because local exposure to ILI/ARI pathogens may vary by hospital and because the calendar months in which participants completed the diaries also differed slightly by hospital, hospital of employment was also included as a potential confounder.
Statistical analysis
The independent-samples t test and the χ2 test were used to determine differences in baseline characteristics between shift workers and non–shift workers.
Incidence rate, episode duration, and severity of ILI/ARI
Our primary objective was to assess the difference in incidence rates of ILI/ARI between shift workers and non–shift workers. Negative binomial regression was used to compare the numbers of ILI/ARI episodes between shift and non–shift workers, using the number of completed diaries as an offset variable (22).
To assess the difference in duration of ILI/ARI episodes, the duration of every ILI/ARI episode (in days) was determined. Linear mixed-model analysis was used to adjust for correlation between repeated observations within participants. Because the duration of ILI/ARI episodes (in days) followed a positively skewed distribution, linear mixed-model analysis was performed on the log-transformed data to compare mean duration of an ILI/ARI episode between shift workers and non–shift workers.
To assess the difference in incidence rate of severe ILI/ARI, the numbers of severe ILI/ARI episodes were compared between shift and non–shift workers using negative binomial regression analysis. Furthermore, the occurrence of ILI episodes was studied. The variable “number of ILI episodes” was dichotomized (≥1 vs. 0), because only 4% of the study population experienced more than 1 ILI episode. Logistic regression analysis was performed to study the association between shift work and the occurrence of at least 1 ILI episode.
Sensitivity analysis: alternative longitudinal model
Because of the longitudinal character of the data, we additionally used longitudinal data analysis (i.e., including the separate daily diaries in the analyses) to study the association between shift work and ILI/ARI occurrence. Therefore, logistic generalized estimating equations analysis with robust standard errors and an exchangeable correlation structure was used (23, 24). The occurrence of an ILI/ARI episode (yes vs. no) was used as the dependent variable. As a measure of the incidence of ILI/ARI episodes, only the first day of every ILI/ARI episode was included to compare the ratio between the number of days with new onset of ILI/ARI and the number of days without ILI/ARI among shift and non–shift workers.
Confounding and effect modification
The results of the analyses were adjusted for age, sex, occupation, and influenza vaccination status, because these covariates were considered to be important confounders a priori. Possible confounding by hospital of employment, educational level, marital status, smoking, and general perceived health was assessed by adding these variables to the analyses and checking to see whether the regression coefficient for shift work changed by ≥10%. Furthermore, we examined possible effect modification by hospital of employment, age, sex, occupation, and influenza vaccination status by adding interaction terms for the interaction between shift work and possible effect modifiers to the adjusted model. Because none of these interaction terms had significant P values (P < 0.05), the results from analyses without interactions are presented.
Frequency and duration of night-shift work
We also analyzed the incidence of ILI/ARI episodes in order to compare incidence rates of ILI/ARI by frequency of night-shift work (non–night-shift worker, 1–2 night shifts/month, 3–4 night shifts/month, or ≥5 night shifts/month) and duration of night-shift work (non–night-shift worker, <10 years of night-shift work, 10–19 years of night-shift work, or ≥20 years of night-shift work), using non–shift workers as the reference group.
Two-sided P values less than 0.05 were considered statistically significant. For negative binomial and logistic regression analyses, IBM SPSS Statistics, version 24.0 (IBM Corporation, New York, New York) was used. For mixed-model and generalized estimating equations analyses, Stata/SE, version 14.2 (StataCorp LLC, College Station, Texas) was used.
RESULTS
Study population
At baseline, 611 health-care workers were included in the Klokwerk+ Study. During the period September 2016–June 2017, 113,566 daily diaries from 604 participants were completed (92% completeness). In total, 110,347 daily diaries, obtained from 501 shift workers and 88 non–shift workers, were usable for analysis (Figure 1). The additional questionnaire on severity of symptoms at the onset of an ILI/ARI episode was completed for 95% of all ILI/ARI episodes. For the analysis of severe ILI/ARI episodes, 10 participants had to be excluded because they reported having 1 or more ILI/ARI episodes during follow-up but failed to complete at least 1 severity score questionnaire.
On average, participants (n = 589) completed diaries for 187.4 (standard deviation (SD), 44.8) days; range, 1–264 days) (Table 1). There were no differences in the average number of completed daily diaries between shift workers and non–shift workers. Compared with non–shift workers, shift workers were younger (40.9 years vs. 46.3 years; P < 0.01), more often nurses (82.6% vs. 33.0%; P < 0.01), less often vaccinated against seasonal influenza (15.2% vs. 26.1%; P = 0.01), less educated (54.9% highly educated vs. 75.0% highly educated; P < 0.01), and more often smokers (12.6% vs. 4.5%; P = 0.03).
Table 1.
Characteristics of the Study Population According to Shift-Work Status, Klokwerk+ Study, the Netherlands, 2016–2017
| Characteristic | Shift-Work Status | |||||||
|---|---|---|---|---|---|---|---|---|
| Shift Workersa (n = 501) | Non–Shift Workers (n = 88) | |||||||
| % | No. of Persons | Mean (SD) | Median | % | No. of Persons | Mean (SD) | Median | |
| No. of completed diaries | 186.4 (45.7) | 200.0 | 192.6 (39.0) | 201.5 | ||||
| Age, years | 40.9 (12.2)b | 42.0 | 46.3 (11.2)b | 48.0 | ||||
| Female sex | 88.0 | 441 | 84.1 | 74 | ||||
| Nursec | 82.6b | 414 | 33.0b | 29 | ||||
| Working full-time (≥36 hours/week) | 33.1 | 166 | 33.0 | 29 | ||||
| Received influenza vaccine | 15.2b | 76 | 26.1b | 23 | ||||
| High educational leveld | 54.9b | 275 | 75.0b | 66 | ||||
| Married/living together | 73.1 | 366 | 77.3 | 68 | ||||
| Current smoker | 12.6b | 63 | 4.5b | 4 | ||||
| Very good/excellent general perceived health | 44.3 | 222 | 37.5 | 33 | ||||
| Frequency of night-shift work, no. of night shifts/month | ||||||||
| Non–night-shift workere | 7.2 | 36 | ||||||
| 1–2 | 15.8 | 79 | ||||||
| 3–4 | 44.5 | 223 | ||||||
| ≥5 | 32.5 | 163 | ||||||
| Duration of night-shift work, years | ||||||||
| Non–night-shift workere | 7.2 | 36 | ||||||
| <10 | 34.7 | 174 | ||||||
| 10–19 | 22.4 | 112 | ||||||
| ≥20 | 35.7 | 179 | ||||||
| Susceptibility to infection | ||||||||
| No. of ILI/ARI episodes | 3.4 (2.3)b | 3.0 | 2.7 (1.8)b | 2.0 | ||||
| Duration of an ILI/ARI episode, days | 8.4 (11.4) | 6.5 | 8.4 (7.4) | 6.5 | ||||
| No. of severe ILI/ARI episodesf | 2.4 (1.9)b | 2.0 | 1.9 (1.5)b | 2.0 | ||||
| No. of ILI episodes | 0.3 (0.7) | 0.0 | 0.2 (0.4) | 0.0 | ||||
| ≥1 ILI episode | 23.8 | 119 | 20.5 | 18 | ||||
Abbreviations: ARI, acute respiratory infection; ILI, influenza-like illness; SD, standard deviation.
a Worked rotating shifts and/or night shifts.
b Statistically significant difference (P < 0.05) between shift workers and non–shift workers (tested by independent-samples t test and χ2 test).
c Occupations other than nursing included physician and paramedical professions such as dietician, physiotherapist, and occupational therapist.
d A high educational level was defined as higher vocational education/university.
e Non–night-shift workers were defined as shift workers who worked rotating shifts without night shifts.
f Based on 491 shift workers and 88 non–shift workers.
Infection susceptibility: descriptive information
Web Figure 1 (available at https://academic.oup.com/aje) illustrates the proportions of shift and non–shift workers experiencing an ILI/ARI episode over time. Throughout follow-up, the proportion of shift workers with ILI/ARI was generally higher than that of non–shift workers. Shift workers had 3.4 ILI/ARI episodes (SD, 2.3) on average, as compared with 2.7 ILI/ARI episodes (SD, 1.8) for non–shift workers (P < 0.01) (Table 1). The mean duration of an ILI/ARI episode was 8.4 days for both shift workers and non–shift workers (median durations, 6.5 days (interquartile range, 4.0–9.6) and 6.5 days (interquartile range, 3.4–10.8), respectively) (P = 0.97). The incidence of severe ILI/ARI episodes was higher for shift workers (2.4 severe ILI/ARI episodes (SD, 1.9)) than for non–shift workers (1.9 severe ILI/ARI episodes (SD, 1.5)) (P = 0.02). Lastly, 23.8% of shift workers and 20.5% of non–shift workers experienced at least 1 ILI episode during follow-up (P = 0.50) (Table 1).
Association between shift work and ILI/ARI episodes
Table 2 shows that compared with non–shift workers, shift workers had a 20% higher incidence rate (incidence rate ratio (IRR) = 1.20, 95 confidence interval (CI): 1.01, 1.43) of ILI/ARI during the winter season of 2016–2017. The mean duration of an ILI/ARI episode was similar for shift workers and non–shift workers (ratio between geometric mean durations of an episode in shift and non–shift workers (eB) = 1.02, 95% CI: 0.87, 1.19). Furthermore, shift workers had a 22% higher incidence rate (IRR = 1.22, 95% CI: 1.01, 1.49) of severe ILI/ARI than non–shift workers. We observed no difference in the odds of experiencing at least 1 ILI episode between shift and non–shift workers (odds ratio = 1.17, 95% CI: 0.63, 2.18) (Table 2).
Table 2.
Effect Estimates for Differences in the Incidence Rate, Duration, and Severity of Influenza-Like Illness/Acute Respiratory Infection Episodes Between Shift Workers and Non–Shift Workers, Klokwerk+ Study, the Netherlands, 2016–2017
| Type of Analysis | Effect Estimate for Shift Workers vs. Non–Shift Workers | |||||||
|---|---|---|---|---|---|---|---|---|
| Incidence Rate of ILI/ARIa | Mean Duration of an ILI/ARI Episode, daysb | Incidence Rate of Severe ILI/ARIc | Occurrence of ≥1 ILI Episoded | |||||
| IRR | 95% CI | eBe | 95% CI | IRR | 95% CI | OR | 95% CI | |
| Crude | 1.29f | 1.09, 1.51 | 1.01 | 0.87, 1.16 | 1.29f | 1.07, 1.55 | 1.28 | 0.73, 2.24 |
| Adjustedg | 1.20f | 1.01, 1.43 | 1.02 | 0.87, 1.19 | 1.22f | 1.01, 1.49 | 1.17 | 0.63, 2.18 |
Abbreviations: ARI, acute respiratory infection; CI, confidence interval; ILI, influenza-like illness; IRR, incidence rate ratio; OR, odds ratio.
a Based on negative binomial regression analysis (n = 589).
b Based on log-transformed linear mixed-model analysis (n = 547 with a total of 1,918 ILI/ARI episodes (36 shift workers and 6 non–shift workers experienced no ILI/ARI episodes)).
c Based on negative binomial regression analysis (n = 579).
d Based on logistic regression analysis (n = 589).
e Ratio between geometric mean values (e = base of the natural logarithm; B = regression coefficient).
fP < 0.05 (for each outcome measure, the analysis used is provided in a corresponding footnote).
g Adjusted for age, sex, occupation, influenza vaccination status, and general perceived health.
Sensitivity analysis: alternative longitudinal model
Similar associations between shift work and incidence of ILI/ARI episodes were found using the generalized estimating equations analysis. Among shift workers, the ratio between the number of days with new onset of ILI/ARI and the number of days without ILI/ARI was 1.27 (95% CI: 1.05, 1.55) times higher than among non–shift workers. This indicates that shift workers had significantly higher odds of acquiring new ILI/ARI episodes compared with non–shift workers.
Frequency and duration of night-shift work
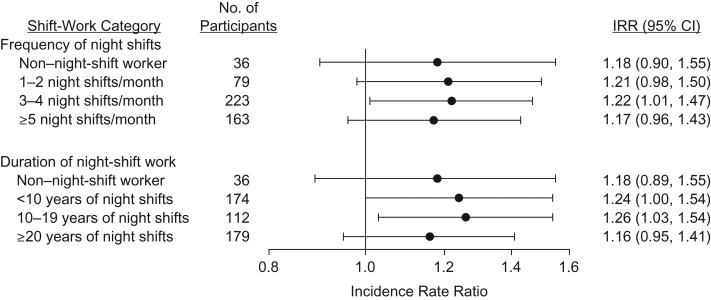
Figure 2 indicates that no clear dose-response association was found between the number of night shifts worked per month and the incidence of ILI/ARI episodes. In addition, an increased duration of night-shift work was not associated with increased risk of the occurrence of ILI/ARI episodes. Compared with non–shift workers, the incidence rate ratios for ILI/ARI were 1.24 (95% CI: 1.00, 1.54) and 1.26 (95% CI: 1.03, 1.54) for night-shift workers with <10 years of night shifts and those with 10–19 years of night shifts, respectively (Figure 2). For shift workers working ≥20 years of night shifts, this effect estimate was smaller, but it remained within the same range as for the other groups of night-shift workers (IRR = 1.16, 95% CI: 0.95, 1.41).
Figure 2.
Effect estimates for differences in incidence rates of influenza-like illness/acute respiratory infection among shift workers versus non–shift workers according to frequency of night-shift work and duration of night-shift work (negative binomial regression analysis adjusted for age, sex, occupation, influenza vaccination status, and general perceived health), Klokwerk+ Study, the Netherlands, 2016–2017. Non–shift workers (reference group) were defined as workers who did not work rotating shifts or night shifts (i.e., workers who worked only day shifts). Shift workers were defined as workers who worked rotating shifts and/or night shifts. Non–night-shift workers were defined as a subgroup of the shift-worker group who worked rotating shifts without night shifts. Bars, 95% confidence intervals (CIs). IRR, incidence rate ratio.
DISCUSSION
In this prospective study carried out among Dutch health-care workers, shift workers had a 20% higher incidence rate of ILI/ARI and a 22% higher incidence rate of severe ILI/ARI during the winter season of 2016–2017 compared with non–shift workers. The mean duration of an ILI/ARI episode was similar between shift workers and non–shift workers. No clear dose-response association was observed for the association between frequency of night shifts per month or the duration of night-shift work and the incidence rate of ILI/ARI.
Our findings are in line with those of previous studies that retrospectively measured prevalence or incidence of infectious diseases (14–16). For example, in a study of workers from different blue-collar and white-collar sectors of the economy (e.g., machine operator, electrician, nurse), shift work was associated with a higher self-reported prevalence of common infections such as ILI (defined as fever and ≥4 influenza-like symptoms) (15). Prevalence of common infections was determined by asking participants about the occurrence of these infections in the past 4 months (15). Because of the prospective measurement of ILI/ARI symptoms on a daily basis and the high level of data completeness, the risk of bias in the present study was reduced. The combined results of our study and previous studies suggest that shift work increases susceptibility to infectious diseases. The mechanisms mediating these associations have not yet been unraveled, but they most likely involve immunological pathways. The extent to which shift work might affect innate and adaptive immune responses involved in resistance to infection (e.g., antibody responses) and in containing and clearing infection after entry into the body (e.g., T-cell responses) should be the subject of future research.
To our knowledge, this study was the first to address the association between some of the major exposure aspects of shift work and infection susceptibility (19). We did not observe a dose-response relationship for frequency or duration of night-shift work. One might anticipate that shift work including night shifts would cause the strongest circadian rhythm disruption and would therefore be most strongly associated with adverse health consequences, yet non–night-shift workers experienced similar rates of ILI/ARI episodes as the night-shift workers. However, because of the small size of the non–night-shift worker group, more research differentiating between shift work with and without night shifts is needed. In addition, working night shifts more frequently did not appear to further increase the rate of ILI/ARI. This may indicate that shift work in itself is a risk factor for acquiring ILI/ARI episodes, irrespective of the frequency of night shifts, and that even occasional shift work may cause circadian rhythm disruption and increased infection susceptibility. However, this finding might also be explained by a healthy worker selection effect: Workers unable to cope with shift work may work night shifts less frequently or may selectively drop out of the shift-working study population (25). A similar selection effect could also explain our finding that for shift workers who worked night shifts for ≥20 years, the increased risk for the occurrence of ILI/ARI episodes appeared less pronounced in comparison with the other night-shift working groups.
The ILI incidence in the present study was considerably higher than ILI incidence rates derived from the traditional Dutch ILI surveillance method through primary-care consultation data and laboratory diagnostics from a network of sentinel practices (8). This can be explained by the fact that traditional surveillance relies on persons seeking health care (26). Other participatory ILI surveillance systems in large populations worldwide also found substantially higher ILI incidences than those reported by networks of sentinel practices, but they were closely correlated (26). Furthermore, although participatory disease surveillance lacks the specificity of laboratory diagnostics, it does provide a high degree of sensitivity (27). It may thereby provide a good estimation of the burden of disease experienced by the individual. In addition, our aim in the present study was not to determine actual ILI/ARI incidence but to compare ILI/ARI incidence rates between shift workers and non–shift workers, for which we believe our data were suitable.
Strengths and limitations
Strengths of the present study were its prospective design, the different exposure aspects of shift work that were taken into account, and the use of a daily diary to measure ILI/ARI episodes during an entire winter season. In comparison with other longitudinal studies, in which attrition rates of 30%–70% are common (28), the amount of missing data in the present study was very limited, with 92% of all possibly completed diaries being completed. Furthermore, because the presence of missing data was not related to shift-work status, we believe the impact of missing data on the results to have been limited.
In the present study, the participation rate of health-care workers was low (only 3% of approximately 18,000 workers approached enrolled in Klokwerk+), which may affect the generalizability of our findings. Our results apply to mostly female health-care workers. Because sex and occupational differences in infection susceptibility may exist, research in other working populations is recommended. In addition, we were not able to adjust for exposure to all possible sources of infection during the study. For example, people with young children may be at higher risk for ILI/ARI episodes (29), but we did not have information on household composition. However, adjustment for age may have partly accounted for this. Previous studies have indicated either that shift workers have fewer children than non–shift workers (30, 31) or that there are no differences in the number of children between shift workers and non–shift workers (32–35), suggesting that our findings either underestimate the true association between shift work and infection susceptibility or are unlikely to have been affected by lack of adjustment for this variable. Furthermore, no measure for level of exposure to (infectious) patients in the hospital was available. We were able to adjust for hospital of employment, but this did not appear to be a relevant confounder. Exposure may also be different for workers in different departments within a hospital and workers with different job tasks. Therefore, occupation was included as a covariate. Nonetheless, the inclusion of more (detailed) measures for infection transmission and exposure in future studies is recommended. Lastly, in the present study, most non–shift workers had a history of working night shifts, which could have diluted the reported effect estimates. Because former night-shift work might also cause immunological disturbances, the association between shift work and infection susceptibility may have been underestimated.
CONCLUSIONS
In conclusion, shift work among health-care workers was found to be associated with increased susceptibility to infection, defined as an increase in ILI/ARI episodes in comparison with non–shift workers. Studying underlying mechanisms connecting shift work and infection susceptibility may be useful in detecting targets (e.g., immune functioning, stress, sleep deprivation (36–38)) for the development of interventions to reduce health problems in shift workers. Building prevention initiatives on such targets could assist in reducing infections, protecting others (e.g., patients) from infection, and supporting sustainable employability of shift workers.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Center for Nutrition, Prevention and Health Services, National Institute for Public Health and the Environment, Bilthoven, the Netherlands (Bette Loef, Karin I. Proper); Department of Public and Occupational Health, Amsterdam University Medical Center, Vrije Universiteit Amsterdam, Amsterdam Public Health Research Institute, Amsterdam, the Netherlands (Bette Loef, Allard J. van der Beek); Centre for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven, the Netherlands (Debbie van Baarle, Elisabeth A. M. Sanders, Patricia Bruijning-Verhagen); Department of Immunology, Laboratory for Translational Immunology, University Medical Center Utrecht, Utrecht, the Netherlands (Debbie van Baarle); Department of Pediatric Immunology and Infectious Diseases, Wilhelmina Children’s Hospital, University Medical Center Utrecht, Utrecht, the Netherlands (Elisabeth A. M. Sanders); and Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, the Netherlands (Patricia Bruijning-Verhagen).
This work was supported by the Strategic Program project 24/7 Health of the Dutch National Institute for Public Health and the Environment.
The funding bodies played no role in the study design; the collection, analysis, and interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Conflict of interest: none declared.
Abbreviations
- ARI
acute respiratory infection
- CI
confidence interval
- ILI
influenza-like illness
- IRR
incidence rate ratio
- SD
standard deviation
- UTC
Coordinated Universal Time
REFERENCES
- 1. European Foundation for the Improvement of Living and Working Conditions (Eurofound) Sixth European Working Conditions Survey—Overview Report. Luxembourg City, Luxembourg: Publications Office of the European Union; 2016. https://www.eurofound.europa.eu/publications/report/2016/working-conditions/sixth-european-working-conditions-survey-overview-report. Accessed September 4, 2017.
- 2. Costa G. Shift work and health: current problems and preventive actions. Saf Health Work. 2010;1(2):112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vyas MV, Garg AX, Iansavichus AV, et al. . Shift work and vascular events: systematic review and meta-analysis. BMJ. 2012;345:e4800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Castanon-Cervantes O, Wu M, Ehlen JC, et al. . Dysregulation of inflammatory responses by chronic circadian disruption. J Immunol. 2010;185(10):5796–5805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cuesta M, Boudreau P, Dubeau-Laramée G, et al. . Simulated night shift disrupts circadian rhythms of immune functions in humans. J Immunol. 2016;196(6):2466–2475. [DOI] [PubMed] [Google Scholar]
- 6. Logan RW, Sarkar DK. Circadian nature of immune function. Mol Cell Endocrinol. 2012;349(1):82–90. [DOI] [PubMed] [Google Scholar]
- 7. Wirth MD, Andrew ME, Burchfiel CM, et al. . Association of shiftwork and immune cells among police officers from the Buffalo Cardio-Metabolic Occupational Police Stress study. Chronobiol Int. 2017;34(6):721–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Teirlinck AC, van Asten L, Brandsema PS, et al. . Annual Report Surveillance of Influenza and Other Respiratory Infections in the Netherlands: Winter 2016/2017 Bilthoven, the Netherlands: National Institute for Public Health and the Environment; 2017. https://www.rivm.nl/Documenten_en_publicaties/Wetenschappelijk/Rapporten/2017/september/Annual_report_Surveillance_of_influenza_and_other_respiratory_infections_in_the_Netherlands_Winter_2016_2017. Accessed September 4, 2017.
- 9. Regional Office for Europe, World Health Organization Influenza. Data and statistics. 2017. http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/data-and-statistics. Accessed September 21, 2017.
- 10. Keech M, Beardsworth P. The impact of influenza on working days lost: a review of the literature. Pharmacoeconomics. 2008;26(11):911–924. [DOI] [PubMed] [Google Scholar]
- 11. Tsai Y, Zhou F, Kim IK. The burden of influenza-like illness in the US workforce. Occup Med (Lond). 2014;64(5):341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Esbenshade JC, Edwards KM, Esbenshade AJ, et al. . Respiratory virus shedding in a cohort of on-duty healthcare workers undergoing prospective surveillance. Infect Control Hosp Epidemiol. 2013;34(4):373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Widera E, Chang A, Chen HL. Presenteeism: a public health hazard. J Gen Intern Med. 2010;25(11):1244–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boden K, Brasche S, Straube E, et al. . Specific risk factors for contracting Q fever: lessons from the outbreak Jena. Int J Hyg Environ Health. 2014;217(1):110–115. [DOI] [PubMed] [Google Scholar]
- 15. Mohren DC, Jansen NW, Kant IJ, et al. . Prevalence of common infections among employees in different work schedules. J Occup Environ Med. 2002;44(11):1003–1011. [DOI] [PubMed] [Google Scholar]
- 16. Vijayalaxmi MK, George A, Nambiar N. A study of general health pattern among night shift work employees in a tertiary care hospital. J Acad Ind Res. 2014;3(4):176–183. [Google Scholar]
- 17. Piasecki TM, Hufford MR, Solhan M, et al. . Assessing clients in their natural environments with electronic diaries: rationale, benefits, limitations, and barriers. Psychol Assess. 2007;19(1):25–43. [DOI] [PubMed] [Google Scholar]
- 18. Loef B, van Baarle D, van der Beek AJ, et al. . Klokwerk+ study protocol: an observational study to the effects of night-shift work on body weight and infection susceptibility and the mechanisms underlying these health effects. BMC Public Health. 2016;16:Article 692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stevens RG, Hansen J, Costa G, et al. . Considerations of circadian impact for defining ‘shift work’ in cancer studies: IARC Working Group Report. Occup Environ Med. 2011;68(2):154–162. [DOI] [PubMed] [Google Scholar]
- 20. European Centre for Disease Prevention and Control EU case definitions. Influenza. 2017. https://ecdc.europa.eu/en/infectious-diseases-public-health/surveillance-and-disease-data/eu-case-definitions. Accessed September 4, 2017.
- 21. Pel JZS. Proefonderzoek naar de frequentie en de aetiologie van griepachtige ziekten in de winter 1963–1964. Huisarts Wet. 1965;8(9):321–324. [Google Scholar]
- 22. Christensen KB, Andersen PK, Smith-Hansen L, et al. . Analyzing sickness absence with statistical models for survival data. Scand J Work Environ Health. 2007;33(3):233–239. [DOI] [PubMed] [Google Scholar]
- 23. Twisk J, de Vente W, Apeldoorn A, et al. . Should we use logistic mixed model analysis for the effect estimation in a longitudinal RCT with a dichotomous outcome variable? Epidemiol Biostat Public Health. 2017;14(3):e12613. [Google Scholar]
- 24. Twisk JWR. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide. 2nd ed Cambridge, United Kingdom: Cambridge University Press; 2013. [Google Scholar]
- 25. Gommans F, Jansen N, Stynen D, et al. . The ageing shift worker: a prospective cohort study on need for recovery, disability, and retirement intentions. Scand J Work Environ Health. 2015;41(4):356–367. [DOI] [PubMed] [Google Scholar]
- 26. Koppeschaar CE, Colizza V, Guerrisi C, et al. . Influenzanet: citizens among 10 countries collaborating to monitor influenza in Europe. JMIR Public Health Surveill. 2017;3(3):e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smolinski MS, Crawley AW, Olsen JM, et al. . Participatory disease surveillance: engaging communities directly in reporting, monitoring, and responding to health threats. JMIR Public Health Surveill. 2017;3(4):e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gustavson K, von Soest T, Karevold E, et al. . Attrition and generalizability in longitudinal studies: findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health. 2012;12:Article 918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mughini-Gras L, Pijnacker R, Enserink R, et al. . Influenza-like illness in households with children of preschool age. Pediatr Infect Dis J. 2016;35(3):242–248. [DOI] [PubMed] [Google Scholar]
- 30. Hansen J, Stevens RG. Case-control study of shift-work and breast cancer risk in Danish nurses: impact of shift systems. Eur J Cancer. 2012;48(11):1722–1729. [DOI] [PubMed] [Google Scholar]
- 31. Koppes LL, Geuskens GA, Pronk A, et al. . Night work and breast cancer risk in a general population prospective cohort study in the Netherlands. Eur J Epidemiol. 2014;29(8):577–584. [DOI] [PubMed] [Google Scholar]
- 32. Knutsson A, Alfredsson L, Karlsson B, et al. . Breast cancer among shift workers: results of the WOLF longitudinal cohort study. Scand J Work Environ Health. 2013;39(2):170–177. [DOI] [PubMed] [Google Scholar]
- 33. Vistisen HT, Garde AH, Frydenberg M, et al. . Short-term effects of night shift work on breast cancer risk: a cohort study of payroll data. Scand J Work Environ Health. 2017;43(1):59–67. [DOI] [PubMed] [Google Scholar]
- 34. Wegrzyn LR, Tamimi RM, Rosner BA, et al. . Rotating night-shift work and the risk of breast cancer in the Nurses’ Health studies. Am J Epidemiol. 2017;186(5):532–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. White L, Keith B. The effect of shift work on the quality and stability of marital relations. J Marriage Fam. 1990:52(2)453–462. [Google Scholar]
- 36. Almeida CM, Malheiro A. Sleep, immunity and shift workers: a review. Sleep Sci. 2016;9(3):164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nagai M, Morikawa Y, Kitaoka K, et al. . Effects of fatigue on immune function in nurses performing shift work. J Occup Health. 2011;53(5):312–319. [DOI] [PubMed] [Google Scholar]
- 38. Pedersen A, Zachariae R, Bovbjerg DH. Influence of psychological stress on upper respiratory infection—a meta-analysis of prospective studies. Psychosom Med. 2010;72(8):823–832. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.