Abstract
Osteoid osteoma is a benign skeletal neoplasm most frequently observed in young individuals. The tumor most commonly occurs in the femur, the tibia, and the phalanges; however, jaw lesions are very rare. Herein, we report a rare case of osteoid osteoma that presented in the mandible of a 20-year-old boy. This report also reviews the cases of osteoid osteomas of the jaws that have been reported in the English literature so far.
Keywords: bone, mandible, nidus, osteoid, pain
Introduction
Osteoid osteoma is a unique benign tumor of the bones, which has seldom been described in the jaws. Although the true nature of this lesion is unknown, various reports suggest it usually occurs in young adults under 30 years of age.1 Lichtenstein defined osteoid osteoma as a “small, oval or roundish tumor like nidus which is composed of osteoid and trabeculae of newly formed bone deposited within a substratum of highly vascularized osteogenic connective tissue.”2 Pain is a distinguishing feature of this lesion and is accompanied by vasomotor disturbances. Herein, we report a case of osteoid osteoma of the mandible that occurred in a young individual. In addition, we also review the cases reported in English literature so far.
Case presentation
A 20-year-old male presented with a complaint of experiencing pain and swelling in the lower left posterior region of the jaw for the past year. The pain was severe and intermittent in nature. It was present early in the morning on waking up, aggravated on consuming meals, and subsided on its own after a few seconds. The pain radiated to the left temporal region. One year previously, the patient underwent a mandibular left first molar extraction. Results of an extraoral examination revealed a diffuse, bony hard swelling extending superoinferiorly from the left lower border of the mandible to 2 cm below it. The anteroposterior extension was from the left corner of the mouth to the left angle of the mandible. The overlying skin was normal with no local rise in temperature. One left submandibular lymph node was palpable, slightly mobile, and tender. Results of an intraoral examination revealed a localized, bony hard swelling in the region of the mandibular left first molar. Buccolingually, the swelling was 3 cm in diameter. Mesiodistally, it extended from the mandibular left first premolar region to the first molar region (Fig. 1). The involved teeth were neither tender on percussion nor mobile. There was no obliteration of the buccal vestibule. From this clinical picture, a differential diagnosis of infected residual cyst, osteomyelitis, and benign bone neoplasm were taken into consideration.
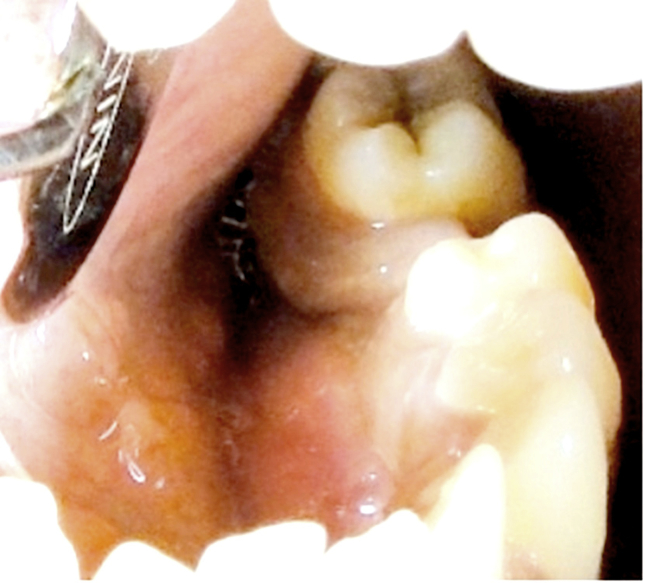
Figure 1.
A photograph showing lingual cortex expansion in the 34–35 region.
Radiographic findings
An orthopantomogram scan revealed a well-defined radiopacity in the mandible with respect to regions 33, 34, 35, and 37 surrounded by a radiolucent rim (Fig. 2). The radiopaque mass consisted of a radiopaque nidus measuring 1.5 cm in diameter surrounded by the formation of subperiosteal new bone. The whole mass measured 3.5 cm (maximum) in diameter. No changes were observed with respect to the inferior border of the mandible. A mandibular cross-sectional occlusal radiograph revealed a well-defined radiopacity in the mandible extending from region 34 to 37 causing an expansion of the lingual cortex (Fig. 3). Based on the results of the radiographic analysis, osteoid osteoma, cementoblastoma, complex odontoma, ossifying fibroma, osteoblastoma, and idiopathic osteosclerosis were considered in the differential diagnosis. Surgical excision of the lesion was done as a part of the treatment. The lesional tissue was sent for histopathological analysis. The postoperative healing was uneventful and the patient was followed-up for a period of 6 months. The pain was completely relieved.
Figure 2.

An orthopantomogram showing well-defined radiopacity with a radiolucent rim showing a central radiopaque nidus surrounded by a radiolucent border.
Figure 3.

A mandibular occlusal radiograph showing the radiopaque lesion causing expansion of the lingual cortex.
Histopathological findings
A histopathological analysis of the lesional tissue revealed irregular bony trabeculae lined with plump osteoblasts. The bony trabeculae showed varying degrees of calcification and reversal lines. The trabeculae comprised of lacunae with osteocytes within them. The stroma was fibrocellular and consisted of many dilated vascular channels and areas of hemorrhage (Fig. 4). Based on these findings, the diagnosis of osteoid osteoma was made.
Figure 4.

A photomicrograph showing irregular bony trabeculae lined by plump osteoblasts. Many dilated blood vessels are seen in the stroma (hematoxylin and eosin, 40×).
Discussion
Jaffe was the first to describe osteoid osteoma as a specific entity in 1935.11 About 80% of osteoid osteoma cases occur in long bones while less than 1% occur in the jaws.6 Various studies to date have reported only 19 cases of osteoid osteomas that involved the jaw bones (Table 1).3, 4, 5, 6, 7, 8, 9, 10 By analyzing the reported cases, we infer that a majority of osteoid osteomas of the jaws occurred in the second and third decades of life. Reports suggest that females were more affected often than males at a ratio of 1.2:1 and a majority of cases were reported in the mandible rather than in the maxilla. This is because the posterior body of the mandible, especially the molar region, was more prone to the development of this lesion. In our case, the tumor was present in the molar region of the left mandible of a 20-year-old boy.
Table 1.
Reported cases of osteoid osteomas of the jaws.
| Author and date | Age | Gender | Location | Signs and symptoms | Radiographic description | Clinical size (cm) | Radio size (cm) |
|---|---|---|---|---|---|---|---|
| Rushton et al3, 4 (1951) | 27 | M | Left posterior mandible | Tender | No findings | NS | NS |
| Foss et al3, 4 (1955) | 26 | F | Left posterior mandible | Pain | Translucent nidus surrounded by sclerotic bone | 4 × 1.7 | 1.5 × 0.7 |
| Nelson et al3, 4 (1955) | 17 | M | Right posterior maxilla | Pain, swelling | Radiolucent center with radiating spicules of trabecular bone | 2.5 | NS |
| Stoopack et al3, 4 (1958) | 25 | M | Left posterior mandible | Asymptomatic | Central radiopacity surrounded by thin radiolucency | NS | NS |
| Lind et al3, 4 (1965) | 48 | M | Right TMJ | Pain | NS | NS | NS |
| Hillman et al3, 4 (1965) | 4 | F | Left posterior maxilla | Swelling | NS | NS | NS |
| Greene et al3, 4 (1968) | 45 | F | Right posterior maxilla | Pain, tender | Central radiopacity surrounded by less densely trabeculated bone | NS | NS |
| Brynolf et al4 (1969) | 77 | M | Anterior maxilla | NS | Central density with radiolucent ring surrounded by increased radiopacity | NS | 0.4 |
| Dechaume et al4 (1985) | 22 | M | Mandible left angle | NA | NA | 1 | NA |
| Gupta et al3, 4 (1985) | 18 | F | Left posterior mandible | Pain, swelling | Ill-defined radiolucency surrounded by sclerotic bone | 3 | NS |
| Lolli et al4 (1987) | 46 | F | Mandible right angle | NA | NA | 1 | NA |
| Festa et al4 (1992) | 50 | F | Mandible left ramus | NA | NA | 1.5 | NA |
| Yang and Qiu4 (2001) | 24 | F | Left TMJ | Pain, swelling | Central radiopacity with alternating zones of sclerosis and radiolucency | 4 × 3.5 | 1.2 |
| Tochihara et al5 (2001) | 21 | F | Left TMJ | Pain | Sclerosed nodule | 0.8 | 0.8 |
| Ida et al6 (2002) | 26 | F | Left posterior mandible | Pain | Diffuse sclerosis with an ill-defined circular radiopacity | 0.8 | 1 |
| Liu et al7 (2002) | 18 | M | Mandibular symphysis | Pain, swelling | Mixed radiolucent/radiopaque lesion | 1.2 | 1.5 |
| Badauy et al8 (2007) | 26 | M | Left posterior mandible | Pain, swelling | Central radiopacity surrounded by sclerotic border | 1 | NS |
| Chaudhary and Kulkarni9 (2007) | 43 | F | Left posterior mandible | Pain, swelling | Well-defined radiolucency surrounded by corticated border | NS | NS |
| Manjunatha and Nagarajappa10 (2009) | 43 | F | Mandible right angle | Pain, swelling | Well-defined radiopaque mass | 1 | NS |
NA = data not available; NS = not specified; TMJ = temporomandibular joint.
The most frequently reported symptom of osteoid osteoma is pain, which could be either continuous or intermittent. The pain is often dull and boring, and frequently becomes worse at night. Golding12 believed that the marked vascular elements were responsible for both the pain and the osseous reaction that occurs in the lesion. Jaffe regarded the curious pain seen in osteoid osteoma as being attributable to the arteriolar blood supply of the lesion.11 In the current case, the pain was intermittent, severe in nature, and radiated to the left temporal region. Although these symptoms clinically implied a periapical inflammatory pathology, the absence of a carious tooth or any periodontal pathology turned our attention toward bone pathology. Pain is also a feature of malignancy, but because the lesion had a growth period of 1 year and there were no signs of paresthesia or anesthesia or perforation of the cortical bone, a benign bone tumor was suspected.
The radiographic appearance of osteoid osteoma helps in its diagnosis. Jaffe stated that the nidus was more radiolucent than radiopaque and that it was surrounded by a reactive radiopacity that extended for a variable distance from the nidus. The less mature lesion was more likely to have radiopaque nidus, whereas the fully mature osteoid osteoma had a radiolucent nidus. Prichard and Mckay13 reported that the calcification of osteoid in the later developmental stages resulted in a central opaque body, which varied in density as the calcification progressed. Stafne described the roentgenographic features as a radiopaque nidus surrounded by an area of dense bone.9 In our case, the radiographic picture was that of a well-defined radiopacity with radiolucent rim showing a central radiopaque nidus surrounded by a radiolucent border.
During radiographic analysis, differential diagnosis including ossifying fibroma, idiopathic osteosclerosis, cementoblastoma, complex odontoma, osteoblastoma, and osteoid osteoma were considered. While ossifying fibromas are asymptomatic, can cause bone expansion, root resorption or displacement of teeth, osteoid osteomas are symptomatic and do not cause resorption or displacement of teeth. Idiopathic osteosclerosis and complex odontoma could be ruled out as these are usually asymptomatic and do not cause bone expansion. Cementoblastomas are asymptomatic and characterized by the proliferation of cementum in close association with the tooth root. Although the osteoid osteoma did comprise a radiopaque mass, it was not associated with the roots of any tooth and it was symptomatic. Performing a differential radiographic diagnosis between osteoid osteoma and osteoblastoma is difficult because their clinical and histological findings frequently overlap, but the presence of radiopaque nidus surrounded by sclerotic new bone formation favors a diagnosis of osteoid osteoma. Along with this, osteoid osteoma is more painful than osteoblastoma but this criterion can be subjective, and therefore, a clear history regarding pain should be derived from the patient.
Histopathologically, Huvos describes three distinct evolutionary stages of ossification. The initial stage is characterized by the presence of actively proliferating, densely packed prominent osteoblasts in a highly vascularized stroma. In the intermediate phase, the osteoid is deposited between the osteoblasts. In the mature stage of the lesion, the osteoid is transformed into a well-calcified, compact trabeculae of an atypical bone, which are histologically peculiar because they are neither typically woven nor typically lamellar.9 In this case, the pathology corresponds to the mature stage of the lesion.
In a majority of patients, osteoid osteomas present with typical clinical symptoms. However, clinical, radiographic, and pathological correlations are essential in some cases to arrive at the correct diagnosis. Jaffe had set a few criteria for the diagnosis of osteoid osteoma. Normally, once the lesion is excised, they do not recur. Although malignant transformation is very rare, one case has been reported in literature, which transformed into an aggressive (low grade) osteoblastoma.14
Osteoid osteoma is a benign bone lesion that occurs very rarely in the jaw bones. Herein, we reported a case of osteoid osteoma that occurred in the mandible of a young adult. Clinical, radiographic, and pathological features were considered to arrive at the correct diagnosis. The small number of cases reported in this regard necessitates an increased awareness among the dentists worldwide to report additional cases in literature. It will provide a medium for better understanding and show a clear picture of such rare bony lesions so that they could be diagnosed at a much earlier stage.
Footnotes
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
References
- 1.Rajendran R., Sivapathasundaram Shafer B, Hine, Levy, editors. Shafer's Textbook of Oral Pathology. 5th ed. Elsevier; India: 2006. pp. 151–152. [Google Scholar]
- 2.Lichtenstein L. C. V. Mosby Comp; Saint Louis: 1965. Bone tumors. pp. 104–20. [Google Scholar]
- 3.Jones A.C., Prihoda T.J., Kacher J.E., Odingo N.A., Freedman P.D. Osteoblastoma of the maxilla and mandible: a report of 24 cases, review of literature, and discussion of its relationship to osteoid osteoma of jaws. Oral Surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:639–650. doi: 10.1016/j.tripleo.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Yang C., Qiu N. Osteoid osteoma of the eminence of the temporomandibular joint. Brit J Oral Max Surg. 2001;39:404–406. doi: 10.1054/bjom.2001.0660. [DOI] [PubMed] [Google Scholar]
- 5.Tochihara S., Sato T., Yamamoto H., Asada K., Ishibashi K. Osteoid osteoma in mandibular condyle. J Oral Maxillofac Surg. 2001;30:445–447. doi: 10.1054/ijom.2001.0121. [DOI] [PubMed] [Google Scholar]
- 6.Ida M. Osteoid osteoma in the mandible. Dento maxillofacial Radiology. 2002;31(3):85–387. doi: 10.1038/sj.dmfr.4600725. [DOI] [PubMed] [Google Scholar]
- 7.Liu C.J., Chang K.W., Chang K.M., Cheng C.Y. A variant of osteoid osteoma of the mandibl – report of a case. J Oral Maxillofac Surg. 2002;60:219–221. doi: 10.1053/joms.2002.29830. [DOI] [PubMed] [Google Scholar]
- 8.Badauy C. Radiopaque mass of the posterior mandible with lingual expansion. J Oral Maxillofac Surg. 2007;65:2498–2502. doi: 10.1016/j.joms.2007.06.624. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhary M., Kulkarni M. Case report – osteoid osteoma of mandible. J Oral Maxillofac Pathol. June-December 2007;11:52–55. [Google Scholar]
- 10.Manjunatha B.S., Nagarajappa D. Osteoid osteoma. Indian J Dent Res. 2009;20:514–515. doi: 10.4103/0970-9290.59438. [DOI] [PubMed] [Google Scholar]
- 11.Jaffe H.L. Osteoid osteoma. Arch Surg. 1935;31:709–728. [Google Scholar]
- 12.Golding J.S. Natural history of osteoid osteoma with a report of 20 cases. J Bone Joint Surg Br. 1954;36(2):218–229. doi: 10.1302/0301-620X.36B2.218. [DOI] [PubMed] [Google Scholar]
- 13.Pritchard J.E., Mckay J.W. Osteoid osteoma. Can Med Assoc J. 1948;58(6):567–575. [PMC free article] [PubMed] [Google Scholar]
- 14.Pieterse A.S., Vernon-Roberts B., Paterson D.C., Cornish B.L., Lewis P.R. Osteoid osteoma transforming to aggressive (low grade malignant) osteoblastoma: a case report and literature review. Histopathology. 2007;7:789–800. doi: 10.1111/j.1365-2559.1983.tb02291.x. [DOI] [PubMed] [Google Scholar]