Abstract
Background/purpose
Individuals with low income bear a number of health challenges to healthcare services. Vancouver's Downtown Eastside (DTES) is known to be a low-income community in a metropolitan city. Because it is difficult to reach, the oral health (OH) status of these residents is unknown. The objectives of this study are (1) to design a tool and strategy to collect OH information in a low-income community, (2) to characterize the OH status and related factors among low-income adults, and (3) to identify the explanatory factors for their OH status.
Materials and methods
Mobile screening clinics were established in the gathering centers of the DTES, and those of 19 years of age or older were recruited. Data were collected through survey interviews and clinical examinations. Potential explanatory factors were investigated by regression analysis.
Results
The 356 screened participants were mostly males, middle-aged, less educated, and living with low income (≤CAD$20,000/y). About 80% had dental coverage, mostly from public programs (94%). Many (86%) perceived a dental need. Among dentate participants (n = 306), on average, 3.8 decayed, 8.6 missing, 4.9 filled teeth, and a care index of 41.5% were observed. Social factors (barriers to care and length of DTES residence), dental hygiene (brushing/flossing), and personal (hepatitis C virus infection/methadone usage) factors contributed to their care index level.
Conclusion
This is the first time that comprehensive information regarding OH status has been collected from a low-income, inner-city community in Canada. Further investigations in the challenges and needs in accessing dental care may develop solutions for better OH in similar communities.
Keywords: care index, dental care service, dental insurance, inner city, low income, oral health status
Introduction
Individuals with low income face a number of health challenges and barriers to healthcare services.1 Vancouver's Downtown Eastside (DTES) is a neighborhood historically considered as poor, and is characterized by high crime rate and excessive use of substances.2, 3, 4 Residents face a series of medical challenges including human immunodeficiency virus (HIV) and hepatitis C virus (HCV) infections along with high rates of hospitalization and emergency room visits compared to the General Vancouver region, a metropolitan city in Canada.3
Oral health (OH) is an integral component of overall health and is essential to general well-being. Serious conditions such as oral cancer were shown to have associations with OH status such as poor oral hygiene, dentition status, and chronic periodontitis.5, 6, 7, 8 Our previous study has indicated that DTES residents may have a high risk for oral cancer.4 Therefore, understanding their OH status and related factors may provide insight on its impact on general health and oral cancer risk of this community.
In countries such as Canada, healthcare does not include dental care services. Individuals with financial barriers to dental care are more likely to be low income and/or without dental insurance.9 Hence, they are more likely to have poorer OH status and are less likely to visit a dentist.10 Although some public dental programs are available to certain underserved groups, coverage for services are often limited and barriers to dental care still persist.11
The overall goal of this study was to understand the OH of this community. Our objectives were: (1) to design a tool and strategy to collect OH information in a low-income community, (2) to characterize the OH status and related factors among low-income adults in the DTES community, and (3) to identify the explanatory factors for their OH status.
Materials and methods
Study design
This is a cross-sectional study using opportunistic sampling. The eligibility criteria include age of 19 years or older and currently living in the DTES for at least 3 months. This study was approved by the University of British Columbia and BC Cancer Agency Research Ethics Board (H10-02598).
Recruitment
Participants were recruited through mobile OH screenings at three main gathering centers and one community dental clinic in Oppenheimer area, the location targeting those best representing the low-income residents of the DTES.4 Low-income status was determined in accordance with the Low Income Cut-Offs established by Statistics Canada.12
Information articles and posters were placed in the gathering centers 1 week prior to the screening day. Participants at the fixed dental clinic were recruited by the clinical staff prior to and on the day of the screening. The screening consisted of a structured interview with a set of survey questionnaires, as well as a dental and oral mucosal examination by a dental clinician and a specialist in oral medicine/oral pathology, respectively. The participants received an incentive package along with a small honorarium upon completion.
Survey
A survey was designed with questions adapted from the Canadian Health Measures Survey (CHMS) and categorized into five modules: demographics, risk behaviors, perceived dental health, healthcare utilization, and clinical examination (see Appendix 1 for the surveys used in this study).10
Demographics include assessed participant's age, sex, ethnicity, education level, annual income, housing, employment, education level, and length of residency in the DTES. Risk behaviors collected include tobacco and alcohol consumption, recreational drug use, and risk behaviors associated with human papillomavirus infection.13 The dental health module examines the participant's perceived dental health status and OH issues including reported oral hygiene behaviors and oral cancer awareness. The healthcare utilization module assesses dental problems experienced, dental care utilization, and dental insurance status.
The clinical examination captures the participants' medical history and their dental and oral mucosal status. Oral mucosal examination was conducted under both white light and fluorescence visualization, a screening adjunct tool.14 Tooth conditions were classified into sound, decayed (Dt), missing (Mt), or filled teeth (Ft).10, 15
Statistical analysis
Chi-square test and Student t test with Welch's correction were used when comparing descriptive data among subgroups. The care index (CI) was used as the outcome measure when identifying dependent variables that explain OH, the ratio of Ft to total decayed-mising-filled teeth (DMF teeth or DMFT).16 Considering the use of dentures and fixed prosthetics as “filled,” CI in this context describes the extent of treatment of OH problems and conversely, the level of dental treatment needed.16 Selected variables based on clinical relevancy were used for multivariate linear regression analysis to identify potential explanatory variables for the CI. The Krippendorff's α for the intraquestionnaire reliability was tested (α = 0.868).17
Results
Participants
A total of 403 participants were recruited into the study from October 2010 to April 2013. Of this total, 47 participants were excluded—27 for their short residency in the DTES, 13 for not completing the screening process, and seven for being screened twice—leaving a total of 356 participants for analysis. Participants (Table 1) were mostly male and middle-aged. Most were low-income, unemployed, and had less than 12th grade education.
Table 1.
Demographic information.
| Variables | na | % |
|---|---|---|
| Gender | ||
| Male | 243 | 68 |
| Female | 113 | 32 |
| Age (y) | ||
| ≤44 | 104 | 29 |
| 45–65 | 227 | 64 |
| >65 | 23 | 6 |
| Ethnicity | ||
| Caucasian | 168 | 47 |
| Aboriginal/first nations | 141 | 40 |
| Other | 47 | 13 |
| Education | ||
| <12 | 186 | 52 |
| ≥12 | 169 | 47 |
| Annual income (Canadian dollars)b | ||
| ≤20,000 | 279 | 78 |
| >20,000 | 15 | 4 |
| Income assistancec | ||
| Yes | 328 | 92 |
| No | 28 | 8 |
| Residency in DTES | ||
| <1 (y) | 31 | 9 |
| 1–8 (y) | 140 | 39 |
| ≥8 (y) | 182 | 51 |
DTES = Downtown Eastside (Vancouver).
Missing values (n): Age (2), Education (l), Smoking Status (1), Alcohol (2), Recreational Drug use (8); “Don't know/declined to answer” (n): Annual Income (60).
Low Income was determined as receiving less than $20,000 per annum for an individual living in a single person household in large census metropolitan area as defined in the Low-Income Cut-off (LICO); Philip Giles (2004). Low Income Measurement in Canada: Statistics Canada, Income Research Paper Series, 75F0002MIE.
Income Assistance includes those who are on social assistance programs receiving welfare and/or disability benefits from the Provincial Government of British Columbia, Canada.
More than two-thirds were current smokers, many (47%) started smoking at a younger age, whereas a third had a high smoking history (Table 2). Many were current drinkers (51%) and almost half had a high cumulative alcohol intake. In addition, recreational drug use was high, and many were still current users.
Table 2.
Oral health related risk factors.
| Variables | na | % |
|---|---|---|
| Tobacco smoking status | ||
| Current | 249 | 70 |
| Former | 52 | 15 |
| Never | 55 | 15 |
| Age at first regular smoking (y) | ||
| <14 | 140 | 47 |
| ≥14 | 159 | 53 |
| Pack-years of smoking | ||
| <20 | 173 | 49 |
| ≥20 | 117 | 33 |
| Alcohol consumption statusa | ||
| Current | 180 | 51 |
| Former | 75 | 21 |
| Never | 101 | 28 |
| Cumulative alcohol intake (drink-years)b | ||
| 0–199 | 49 | 42 |
| ≥200 | 176 | 49 |
| Recreational drug usec | ||
| Current | 236 | 66 |
| Former | 35 | 10 |
| Never | 77 | 22 |
| Risk for HPV infection—No. of partners performing oral sex | ||
| 0–5 | 204 | 57 |
| ≥6 | 142 | 40 |
| Infectious conditions | ||
| HIV infection | 68 | 19 |
| Hep C Infection | 117 | 33 |
HPV = human papillomavirus.
Missing values (n): Smoking Status (1), Start age of smoking (1), Pack-years smoking (11), Recreational Drugs (8); Cumulative alcohol (30); HPV (10).
Number of years consuming alcohol x average alcohol consumption per week in units (unit equivalent = one bottle of beer = one glass of wine = 45 mL of spirit/liquor).
Recreational Drug Use: any injection or non-injection use of crack, cocaine, heroin, crystal methamphetamine, marijuana or any other types of illicit drugs.
Many demonstrated a behavioral risk for human papillomavirus infection (40%). A portion has reported with medical conditions such as HIV (19%) and HCV (33%). Two-thirds have previously participated in any cancer screening. Interestingly, only half (52%) have heard of oral cancer.
Perceived health, dental needs, and barriers to care
Most participants (82.6%) perceived their OH as “fair” or “poor.” Their main OH issues were eating (n = 118) and aesthetics (n = 86). The majority (86%) had at least one dental need; restorative dental care (39%), dentures (38%), preventive hygiene services (33%), and tooth extractions (29%) were commonly reported. Perceived barriers to dental care were reported by 137 participants; these were either cost related, access related, or having other competing priorities. Cost barriers were mainly attributed to “not enough insurance” coverage (78%).
OH status
Clinical examination showed that 50 participants were completely edentulous. Among them, 17 had both complete upper (UCD) and lower dentures (LCD) in place, seven with either a UCD or an LCD, whereas 26 (52%) had no dentures at all. Dental status and CI among those with teeth (n = 306) are shown in Table 3 with an average DMFT of 17.2 ± 0.8 and an average CI of 41.5 ± 31.3%. Only 41% reported brushing their teeth at least twice a day, and 36% reported that they flossed.
Table 3.
Dental indices, dental insurance, and dental usage.
| Dt | Mt | Ft | DMT | DMFT | CI | |
|---|---|---|---|---|---|---|
| Total (n = 306)a | 3.8 (3.2–4.3) | 8.6 (7.8–9.5) | 4.9 (4.4–5.4) | 11.6 (10.7–12.6) | 17.2 (16.4–18.0) | 41.5% (37.9–45.0%) |
| Dental insurance | ||||||
| Not insured (n = 50) | 3.7 (2.4–5.1) | 7.1 (5.2–9.1) | 5.3 (4.1–6.5) | 10.8 (8.4–13.2) | 16.1 (13.9–18.2) | 31.9% (30.8–47.5%) |
| Insured (n = 242) | 3.6 (3.0–4.3) | 9.0 (8.1–9.9) | 4.9 (4.4–5.5) | 11.8 (10.7–12.9) | 17.6 (16.8–18.5) | 42.2% (38.2–46.2%) |
| Public insurance type | ||||||
| Welfare (n = 146) | 3.2 (2.5–3.9)*,b | 9.6 (8.3–10.8) | 4.5 (3.9–5.2) | 12.1 (10.6–13.5) | 17.3 (16.1–18.5) | 42.3% (37.0–47.6%) |
| NIHB (n = 82) | 4.5 (3.4–5.6) | 8.4 (6.8–10.0) | 5.3 (4.3–6.4) | 11.4 (9.8–13.0) | 18.1 (16.8–19.5) | 41.0% (34.4–47.5%) |
| Last dental visit | ||||||
| ≤ 1 y (n = 194) | 2.9 (2.3–3.4)*** | 8.5 (7.6–9.6) | 5.5 (4.9–6.1)** | 11.0 (9.8–12.1) | 17.0 (16.0–17.9) | 46.6% (42.1–51.1%)* |
| > 1 y (n = 112) | 5.4 (4.3–6.5) | 8.8 (7.3–10.2) | 3.8 (3.0–4.5) | 13.1 (11.4–14.8) | 17.9 (16.5–19.4) | 33.8 (22.2–39.3%) |
CI = care index; Dt = decayed tooth; DMT = decayed-mising teeth; DMFT = decayed-mising-filled teeth; Ft = filled tooth; Mt = missing tooth.
Missing value (n): Insurance Status (14).
Significance determined by Student t test with Welch's correction: *, 0.01 < P < 0.05; ***, P < 0.0001.
Approximately one in four had an oral mucosal lesion. Lesions were mainly on the tongue (n = 53) or buccal mucosa (n = 23). These were a result of trauma (n = 64) and/or infections (n = 28). Four cases were possible oral premalignant lesions and required further investigation.
Dental insurance status, utilization, and barriers to care
Most participants had dental insurance (Table 3) that primarily stemmed from public programs, either provincial (Welfare) or federal [Non-Insured Health Benefits (NIHB) program]. However, less than two-thirds had a recent dentist visit. Most of these visits were for treatment services (n = 167) rather than routine maintenance/oral hygiene services (n = 55). Dt was significantly higher among those with NIHB than those with welfare coverage (Table 4, P = 0.02). Those who visited a dentist recently had significantly lower number of Dt (P < 0.0001) and decayed-mising teeth (DMT) (P = 0.04), including a higher number of Ft (P < 0.0004) and CI (P = 0.0003), than those who did not.
Table 4.
Perceived dental health, dental care utilization, and insurance status.
| Variables | na | % |
|---|---|---|
| Oral health | ||
| Excellent/good | 55 | 15 |
| Fair/poor | 294 | 83 |
| Oral health problems within the past 30 db | ||
| None | 137 | 38 |
| Discomfort eating or drinking | 186 | 52 |
| Persistent or ongoing pain | 154 | 43 |
| Difficulty socializing | 57 | 16 |
| Dental visit within the past 12 moc | ||
| Yes | 218 | 61 |
| No | 138 | 39 |
| Dental insurance | ||
| Yes | 284 | 80 |
| No | 56 | 16 |
| Types of dental insurance | ||
| Employee/private | 16 | 6 |
| Public insurance | 268 | 94 |
| NIHB | 95 | 35 |
| Welfare | 173 | 65 |
CI = care index; Dt = decayed tooth; DMT = decayed-mising teeth; DMFT = decayed-mising-filled teeth; Ft = filled tooth; Mt = missing tooth.
Missing variables (n): Oral Health (2), discomfort eating or drinking (2); persistent or ongoing pain (1); Difficulty socializing (1); “Don't know/declined to answer” (n): Oral Health (5).
Participants chose any that applies, results not mutually exclusive.
A measure of routine dental care utilization.
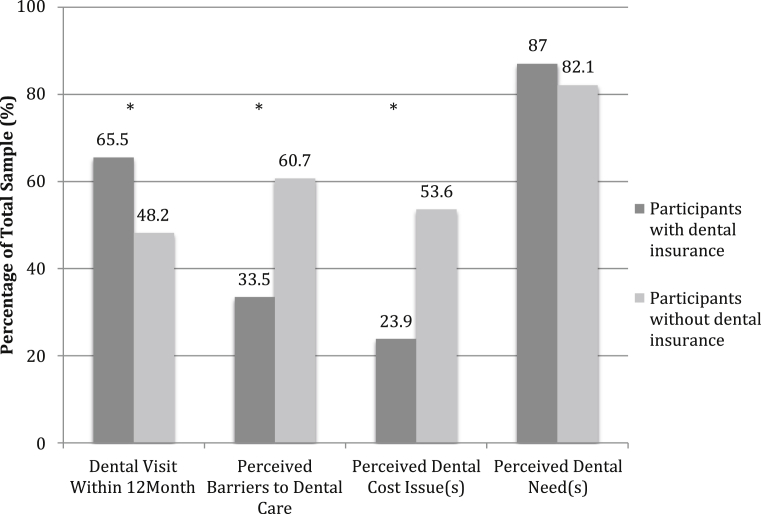
Dental insurance coverage was significantly associated with having a recent dental visit (P < 0.05; Figure 1). Reporting financial barriers or at least one barrier to dental care was significantly higher among those without dental insurance. There was no difference in the perceived need for dental care between insured and noninsured individuals. Furthermore, there was no association between having barriers to dental care and having a recent dental visit. Significantly more participants on welfare visited a dentist recently than those with NIHB (55.8% vs. 71.1%; P < 0.05). No significant difference was observed in perceived cost issue or perceived dental treatment needs among those with public coverage.
Figure 1.
Differences in dental visit within 12 months, perceived barriers to care and treatment needs among participants with and without dental insurance. The P value was determined using Chi-square test, where *P < 0.05 (two-sided).
Independent factors explain the CI
For the edentates, only three levels of CI were possible: 0% (no dentures), 50% (having only UCD or LCD), and 100% (both UCD and LCD). This is different from others as the level of CI was continuous and can range from 0% to 100%. Additionally, the health outcome of these patients indicated the different needs for dental service. For those dentate participants with 0 DMFT, CI cannot be calculated. Thus, the edentates (n = 50) and those with 0 DMFT (n = 4) were excluded in the analysis, leaving a total of 302 cases for analysis.
The variables significantly associated with CI were sex, longer DTES residency (>8 years), presence of any barrier to dental care, methadone use, HCV infection, and brushing and flossing habits (Table 5).
Table 5.
Explanatory variables for CI after multivariate linear regression adjusted for recruitment site.
| Variables | Level(s) | Coefficient | Sid. error | Pb | Level(s) | Coefficient | Std. error | P | |
|---|---|---|---|---|---|---|---|---|---|
| Sex | Brushing habitsc | ||||||||
| [Female]a | [Brush <2x/day] | ||||||||
| Male | −0.100 | 0.051 | * | Bash ≥2x/day | 0.128 | 0.049 | ** | ||
| Flossing habits | |||||||||
| Barriers to Dental Care | [Never Floss] | ||||||||
| [No barriers] | Yes, Flossing | 0.187 | 0.050 | *** | |||||
| Yes | −0.103 | 0.048 | * | Methadone | [No] | ||||
| DTES Residency | Current user | −0.235 | 0.075 | ** | |||||
| [<1 y] | HCV | ||||||||
| 1–8 y | −0.108 | 0.071 | [HCV Free] | ||||||
| >8 y | −0.208 | 0.069 | ** | HCV | −0.120 | 0.053 | * |
CI = care index; DTES = Vancouver's Downtown Eastside; HCV = hepatitis C virus.
[ ]: Reference Variable.
Significant Difference determined by multivariate linear regression analysis: *, 0.01 < P < 0.05; **, 0.001 < P < 0.01; ***, P < 0.0001.
Includes those who do not brush.
Discussion
This is the first study to collect comprehensive OH information on adults living in a low-income community in Canada. The high levels of Dt, Mt, and DMT in addition to low Ft and CI suggest that most of their dental problems and needs have not been addressed. In comparison to the Canadian low-income population, the DTES participants exhibit poorer dental status (DMFT, 17.2 vs. 10.4; Dt, 3.8 vs. 1.0; Mt, 8.6 vs. 2.9), lower CI (41.5% vs. 62.5%), and a higher prevalence of oral mucosal lesion (28% vs. 16%).10
Our clinical findings were consistent with the participants' perceived OH status and needs. Their dental problems have affected their quality of life in eating and drinking. Dental pain and aesthetics were their main OH concerns, similar to findings from another welfare group in Montreal.11
Missing teeth is prevalent: about 14% were completely edentulous, and 25% of dentate participants had 14 or more Mt. This may reflect a lack of accessible restorative options leading to tooth extractions. We observed that many participants are transitioning from dentate to edentate status. Similar low-income groups have viewed dentures as a solution to their dental problems.11 Our participants may also view acquiring dentures as a way to restore their chewing abilities and self-image.
There is a high usage of dental treatment services compared to preventive services despite coverage being provided for both services. Symptom-driven dental visits are common among people with low incomes as individuals often seek professional help when their problems become unbearable, often requiring more extensive and costly procedures.18 It might be important to develop an OH education program to break this pattern of dental care usage.
Our data support the notion that those with public dental benefits are more likely to have a recent dental visit and less likely to report barriers to dental care; however, their dental status or perceived need for dental care were not significantly different. One explanation for this is that individuals may have other priorities such as maintaining lifestyle habits and finding stable housing. Because having a recent dental visit was associated to a better dental status, one strategy may include incorporating oral disease prevention into existing education programs to increase utilization. A qualitative study with the residents and OH providers is in place to assess possible problems including competing needs and the access and adequacy of current funding sources.
After adjusting for the recruitment site, several factors were identified that partially account for poor CI. Women and those practicing oral hygiene behaviors were indicative of better CI levels. In general, women tend to have better OH awareness and demonstrate better dental care than men.19, 20 This indicates that an OH educational program should focus more on the male population. The length of DTES residency may suggest a longer low-income status and/or longer exposure to a high-risk behavior and environment that have an impact to OH. Barriers to dental care, particularly cost barriers, are an issue; however, it is not clear whether the lack of financial resources results from the need to maintain lifestyle habits or if the public coverage is simply inadequate to serve the dental needs of this population. Further interviews and focus group studies with residents and OH providers may identify the fundamental problems.
Interestingly, methadone users and individuals with HCV infection had lower CI values. Methadone is a common form of treatment for those with heroin addictions, and methadone use has been linked to dental diseases.21 However, the associations with poor OH status may be secondary to the dry mouth commonly associated with smoking and HCV infection.22, 23 Our study showed that methadone users had a high prevalence of smoking (96%) and HCV infection (80%). Poor CI may also be a result of limited resources and/or lifestyle habits as 80% of methadone users in our study were still using recreational drugs. Another possibility is that the administration of methadone is often done with a sugar-based syrup, which may increase risks for dental decay. Although methadone can be administered in a tablet form, the potential for abuse and illegal distribution limits the syrup form for high-risk communities, such as the DTES.24
A complexity of social issues exists for our participants such as lack of basic resources, housing conditions, and complex social environments that could outweigh their OH needs, resulting in poor self-care and consequently poor OH status.25, 26 A study has noted that those living in single-room occupancy housing in the DTES were more likely to incur other health risks, including HIV infection, illicit drug use, and risk of physical violence.27 Our results support the social impacts on OH. In addition, mental health status, a significant burden in this community, may also have implications on OH. These determinants are complicated and are difficult to address within the scope of this research. Further investigations through qualitative methods are needed to identify the social determinants impacting on the OH of this population. This may be important not only in reducing OH disparities but also in enabling the design of effective strategies to improve their health and social conditions.28, 29
This study has several limitations. These include the potential selection bias and representativeness of participants. The recent growth and redevelopment programs have led to changes and gentrification in the area.30 Many of the low-income adults still remain around the Oppenheimer area where we recruited our study volunteers, enabling us to target areas best representing the low-income residents within the DTES.2
The cross-sectional design limited our abilities to explain the OH outcomes. Using linear regression analysis, our data have only accounted for 27.8% of the variation in the CI level. Ideally, a longitudinal prospective study may provide better understanding of these issues and their impact on OH status. We aim to compare our results with those from the Canadian low-income group from the CHMS and initiate a qualitative study to compliment our findings.
Our study provides an overall picture of the OH status and the oral care needs of this inner-city, low-income community. An emerging challenge for dental professionals involves collaboration with other health professionals and social service providers to implement a multidisciplinary approach to address the OH complexities and related issues among similar communities.
Conflict of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
We thank Dr Rosamund Harrison for expert comments, Yi-Ping Liu for assistance with the database, and Monica Ye for the data analysis. We also thank Drs Sean Sirkoski and Bertrand Chan for their contributions in the clinical assessment. We are also grateful to the staff of the Portland Community Clinic, Lifeskill's Centre, Women's Centre, and the Vancouver Native Health Centre, for accommodating our screening activities. This work is supported by New Emerging Team Oral Health Disparities Grant (#87104) of the Canadian Institute of Health Research and BC Cancer Foundation.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jds.2016.06.008.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Baggett T.P., O'Connell J.J., Singer D.E., Rigotti N.A. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100:1326–1333. doi: 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.City of Vancouver. Downtown eastside (DTES) local area profile 2012. Vancouver, 2012. Available at: http://vancouver.ca/files/cov/profile-dtes-local-area-2012.pdf [Date accessed: January 2, 2016].
- 3.Kerr T., Wood E., Grafstein E. High rates of primary care and emergency department use among injection drug users in Vancouver. J Public Health (Oxf) 2005;27:62–66. doi: 10.1093/pubmed/fdh189. [DOI] [PubMed] [Google Scholar]
- 4.Poh C.F., Hislop G., Currie B. Oral cancer screening in a high-risk underserved community: Vancouver Downtown Eastside. J Health Care Poor Underserved. 2007;18:767–778. doi: 10.1353/hpu.2007.0106. [DOI] [PubMed] [Google Scholar]
- 5.Rosenquist K., Wennerberg J., Schildt E.-B., Bladström A., Göran Hansson B., Andersson G. Oral status, oral infections and some lifestyle factors as risk factors for oral and oropharyngeal squamous cell carcinoma. A population-based case-control study in southern Sweden. Acta Otolaryngol. 2005;125:1327–1336. doi: 10.1080/00016480510012273. [DOI] [PubMed] [Google Scholar]
- 6.Homann N., Tillonen J., Rintamäki H., Salaspuro M., Lindqvist C., Meurman J.H. Poor dental status increases acetaldehyde production from ethanol in saliva: a possible link to increased oral cancer risk among heavy drinkers. Oral Oncol. 2001;37:153–158. doi: 10.1016/s1368-8375(00)00076-2. [DOI] [PubMed] [Google Scholar]
- 7.Tezal M., Grossi S.G., Genco R.J. Is periodontitis associated with oral neoplasms? J Periodontol. 2005;76:406–410. doi: 10.1902/jop.2005.76.3.406. [DOI] [PubMed] [Google Scholar]
- 8.Elwood J.M., Gallagher R.P. Factors influencing early diagnosis of cancer of the oral cavity. Can Med Assoc J. 1985;133:651–656. [PMC free article] [PubMed] [Google Scholar]
- 9.Locker D., Maggirias J., Quiñonez C. Income, dental insurance coverage, and financial barriers to dental care among canadian adults. J Public Health Dent. 2011;71:327–334. doi: 10.1111/j.1752-7325.2011.00277.x. [DOI] [PubMed] [Google Scholar]
- 10.Health Canada. Summary report on the findings of the oral health component of the Canadian Health Measures Survey 2007–2009. Canada, 2010. Available at: http://publications.gc.ca/collections/collection_2010/sc-hc/H34-221-2010-eng.pdf [Date accessed: January 2, 2016].
- 11.Bedos C., Levine A., Brodeur J.-M. How people on social assistance perceive, experience, and improve oral health. J Dent Res. 2009;88:653–657. doi: 10.1177/0022034509339300. [DOI] [PubMed] [Google Scholar]
- 12.Statistics Canada. Low income lines, 2009–2010. In: Income Statistics Division, editor. Statistics Canada. Cat. No.: 75F0002M, vol. 2, Ottawa; 2011.
- 13.D'Souza G., Kreimer A.R., Viscidi R. Case–control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–1956. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 14.Poh C.F., Ng S.P., Williams P.M. Direct fluorescence visualization of clinically occult high-risk oral premalignant disease using a simple hand-held device. Head Neck. 2007;29:71–76. doi: 10.1002/hed.20468. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization . 5th ed. World Health Organization; Geneva, Switzerland: 2013. Oral Health Surveys: Basic Methods. [Google Scholar]
- 16.Walsh J. International patterns of oral health care: the example of new zealand. N Z Dent J. 1970;66:143–152. [PubMed] [Google Scholar]
- 17.Hayes A.F., Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. 2007;1:77–89. [Google Scholar]
- 18.Bedos C., Brodeur J.-M., Boucheron L. The dental care pathway of welfare recipients in quebec. Soc Sci Med. 2003;57:2089–2099. doi: 10.1016/s0277-9536(03)00066-2. [DOI] [PubMed] [Google Scholar]
- 19.Östberg A.-L., Halling A., Lindblad U. Gender differences in knowledge, attitude, behavior and perceived oral health among adolescents. Acta Odontol Scand. 1999;57:231–236. doi: 10.1080/000163599428832. [DOI] [PubMed] [Google Scholar]
- 20.Coda Bertea P., Staehelin K., Dratva J., Zemp Stutz E. Female gender is associated with dental care and dental hygiene, but not with complete dentition in the swiss adult population. J Public Health (Oxf) 2007;15:361–367. [Google Scholar]
- 21.Reece A.S. Dentition of addiction in queensland: poor dental status and major contributing drugs. Aust Dent J. 2007;52:144–149. doi: 10.1111/j.1834-7819.2007.tb00480.x. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy J.J., Flynn N. Hepatitis C in methadone maintenance patients: prevalence and public policy implications. J Addict Dis. 2001;20:19–31. doi: 10.1300/J069v20n01_03. [DOI] [PubMed] [Google Scholar]
- 23.Richter K.P., Gibson C.A., Ahluwalia J.S., Schmelzle K.H. Tobacco use and quit attempts among methadone maintenance clients. Am J Public Health. 2001;91:296–299. doi: 10.2105/ajph.91.2.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williamson P.A., Foreman K.J., White J.M., Anderson G. Methadone-related overdose deaths in South Australia, 1984–1994. How safe is methadone prescribing? Med J Aust. 1997;166:302. [PubMed] [Google Scholar]
- 25.Borrell L.N., Burt B.A., Warren R.C., Neighbors H.W. The role of individual and neighborhood social factors on periodontitis: the Third National Health and Nutrition Examination Survey. J Periodontol. 2006;77:444–453. doi: 10.1902/jop.2006.050158. [DOI] [PubMed] [Google Scholar]
- 26.Hwang S.W., Wilkins R., Tjepkema M., O'Campo P.J., Dunn J.R. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ. 2009;339:b4036. doi: 10.1136/bmj.b4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shannon K., Ishida T., Lai C., Tyndall M.W. The impact of unregulated single room occupancy hotels on the health status of illicit drug users in Vancouver. Int J Drug Policy. 2006;17:107–114. [Google Scholar]
- 28.Daiski I. Perspectives of homeless people on their health and health needs priorities. J Adv Nurs. 2007;58:273–281. doi: 10.1111/j.1365-2648.2007.04234.x. [DOI] [PubMed] [Google Scholar]
- 29.Patrick D.L., Lee R.S., Nucci M., Grembowski D., Jolles C.Z., Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6:S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boyle P., Haggerty K.D. Civil cities and urban governance: regulating disorder for the Vancouver Winter Olympics. Urban Stud. 2011;48:3185–3201. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.