Abstract
Background/purpose
The self-ligating brackets (SLB) have been introduced in modern orthodontic treatment in recent years for malocclusion patients. This study was conducted to compare two treatments, conventional brackets (CB) and SLB, in malocclusion to determine which treatment will provide better oral health-related quality of life (OHRQoL) outcomes.
Materials and methods
The research involved a prospective randomized clinical trial, composed of two sets of questionnaires, Short Form-36 (SF-36T) and oral health impact profile-14 (OHIP-14T), concerning HRQoL and OHRQoL. In total, 88 malocclusion patients who were eligible and met the inclusion and exclusion criteria from the Orthodontic Department of Mackay Memorial Hospital from June 2010 to November 2011 participated in the study, and all patients had completed a minimum follow-up of 1 week and 1 month. The quantitative analysis of the questionnaires was conducted through descriptive statistics and repeated measures of analysis of variance to indicate the differences in OHRQoL between the two sets of brackets systems.
Results
For SF-36T, the physical component score, the mental component score and all of the eight scales yielded no statistically significant differences between the CB and SLB group. For OHIP-14T, the overall score and all of the seven scales yielded no statistically significant difference between the CB and SLB group. Results of this study showed that SLB systems were not shown to be statistically superior to CB systems in improving OHRQoL for malocclusion patients during initial orthodontic treatment.
Conclusion
This study may provide the orthodontists with a better understanding how malocclusion patients experience the change of OHRQoL and discomfort for CB systems and SLB systems during the initial fixed orthodontic therapy.
Keywords: orthodontic anchorage, success rate, temporary anchorage device
Introduction
Most research in assessing the impact of malocclusion and orthodontic treatment tends to focus on traditional clinical indices and measures. Investigators prefer to use the change of cephalometric planes and angles or peer assessment rating scores before and after orthodontic treatment as outcome measures. However, the recommendation by World Health Organization that quality of life (QoL) measures should be included in clinical studies has resulted in more emphasis on inclusion of patient-centered outcome measures when studying orthodontic treatments and outcomes.
O'Brien et al1 emphasized that while clinical indicators of treatment outcomes are still important, oral health-related QoL (OHRQoL) measures that take into account these broader health concepts are important, especially since patient-oriented OHRQoL outcomes do not necessarily correlate with objective clinical findings.1 Therefore, they insist that self-reported OHRQoL instruments should be applied in the assessment of orthodontic treatment because they reflect the patient's own views and feelings as a supplement to clinical indices. Not only should research studies use OHRQoL in measuring the effectiveness of specific treatments but routine use of OHRQoL in daily practice could help the orthodontist not only better diagnose and treat malocclusion but also better understand the concerns from the patient's perspective. Buschang et al2 further commented that the more our societies pay attention to justify the need and outcome of treatment from the patient's point of view, the more information about orthodontic impact on QoLwe could discover.
New technologies and ligation strategies which have the potential to reduce patient discomfort and improve QoL outcomes are emerging. One of the most promising new technologies is the use of self-ligating brackets (SLB) that allow lighter, continuous force to align and level the crooked teeth. There are some potential advantages of SLB: full and secure archwire engagement,3 lower friction between the bracket and the archwire,4, 5, 6, 7 less chair time,8, 9, 10 improved oral hygiene,11 reduced treatment time,12, 13 and reduced patient discomfort.14, 15 However, it is still unknown whether treatment with SLB will result in better ORHQoL than that with conventional brackets (CB).
The objective of this study is to compare these two treatments in malocclusion to determine which treatment will provide the better OHRQoL outcomes for patients during the initial orthodontic treatment.
Materials and methods
This study is a prospective randomized controlled trial of SLB (Damon Q) versus CB (OPA-K) in malocclusion patients who seek orthodontic treatment recruited from the Orthodontic Department of Mackay Memorial Hospital from June 2010 to November 2011. In total, 88 eligible patients were identified and recruited at the participating clinical center, subject to the inclusion and exclusion criteria. Inclusion criteria were malocclusion patients aged 12–40 years and suitable for orthodontic treatment using either SLB or CB. Exclusion criteria including patients who satisfied any of the following conditions were ineligible for enrollment in the trial: any surgery performed in the previous 6 months; previous temporomandibular joint arthrotomies; fewer than 20 teeth in total or fewer than 10 teeth in each arch; unstable residence or travel restrictions; periodontal disease judged to be severe by the surgeon; pregnancy; previous mandibular surgery; or inability to follow instructions or the study protocol.
Assessment of HRQoL was conducted using two standardized measures: the Taiwan version of the Short Form-36 (SF-36T) and the short form of the oral health impact profile, Taiwan version (OHIP-14T).
The SF-36T is a generic short form measuring functional health and well-being. It has been extensively applied in comparing general and specific populations, estimating the burden of disease and measuring the effectiveness of treatments. The SF-36T has been shown to possess good psychometric properties (good data quality, validity, and reliability). The questionnaire consists of eight health domains: physical health (10 questions), role limitations due to physical problems (4 questions), bodily pain (2 questions), general health (5 questions), vitality (4 questions), social functioning (2 questions), role limitations due to emotional problems (3 questions), mental health (5 questions), and a question about perceived change of health during the last month. A score between 0 (worst) and 100 (best) is calculated for each domain using a standardized scoring system.16
The original version of the OHIP comprises 49 items divided into seven domains, but a recent study produced a short-form OHIP containing only 14 items. OHIP-14T is useful for taking studies as its theoretical basis is Slade's conceptual model descriptive oral health surveys of general populations. The instrument comprises the following seven domains: functional limitations, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Each domain contains two questions. For any one question, the answer uses a five-point rating scale for the frequency of occurrence of each item with categories: fairly often (scored 4), very often (scored 3), occasionally (scored 2), hardly ever (scored 1), and never (scored 0). Therefore, for each domain, the score ranged from 0 to 8. The overall score ranged from 0 to 56. These measures have been shown to be reliable and valid in samples.17 All questions were administered as a self-completed questionnaire. Assessments of HRQoL were conducted at baseline before banding and bonding of orthodontic treatment (T0), at 1 week after banding and bonding (T1), and at 1 month after banding and bonding (T2).
Statistical analysis
The study design was a prospective, randomized controlled trial of SLB (Damon Q) versus CB (OPA-K) for malocclusion patients under orthodontic treatment. Patients were followed at 1 week and 1 month postorthodontic treatment. Statistical analyses followed the intent-to-treat paradigm, which meant all patients were analyzed according to the treatment group into which they were randomized. The results were expressed as the mean ± standard deviation (SD). For statistical analysis, HRQoL data (SF-36T and OHIP-14T) were analyzed by paired t test between T1–T0 and T2–T0. Comparisons between the two groups of SF-36T and OHIP-14T according to bracket type (OPA-K and Damon Q) were performed using repeated measures analysis of variance (ANOVA). Data were analyzed using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was predetermined at α = 0.05.
Results
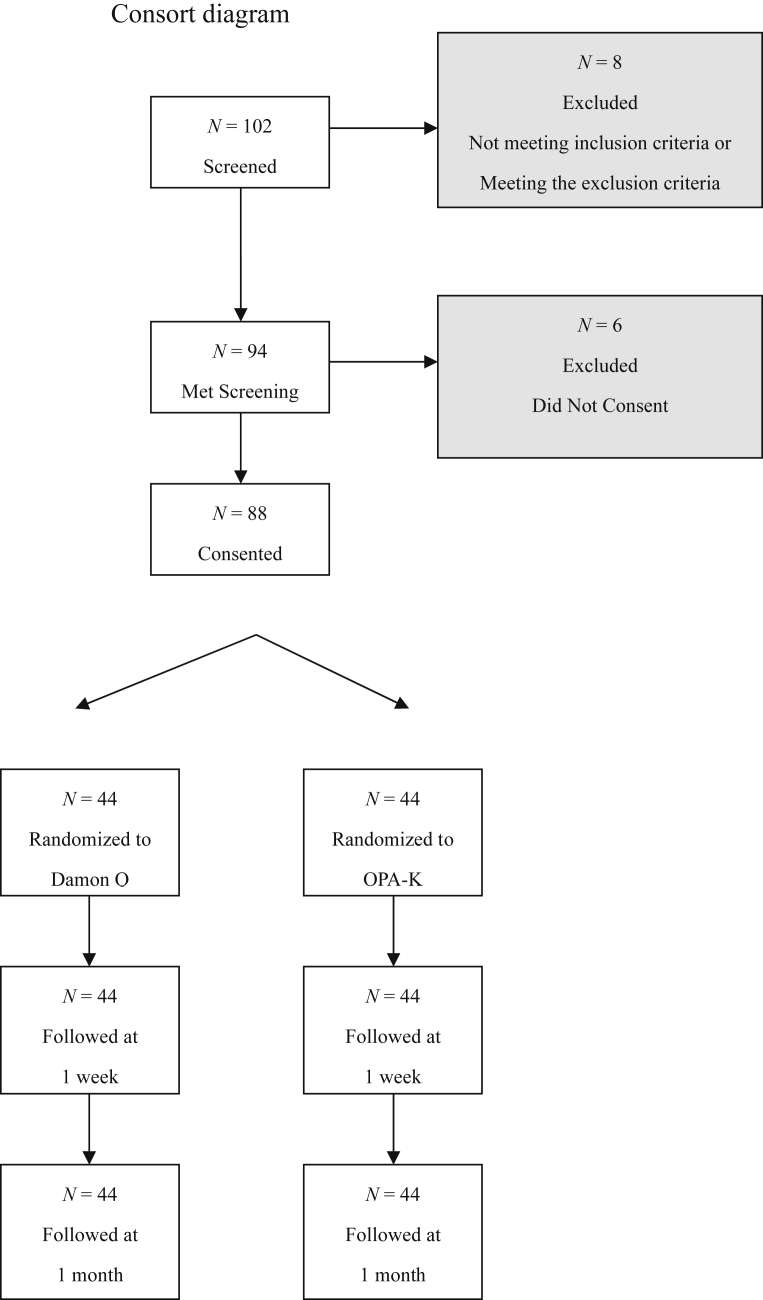
In total, 102 patients were screened from the Orthodontic Department of Mackay Memorial Hospital from June 2010 to November 2011. Eight patients were excluded as they did not meet the inclusion and exclusion criteria, whereas 94 patients met the screening criteria. Of these, six patients did not provide consent for the study and were excluded. Thus, 88 patients consented and were randomly assigned to one of the two treatment groups by random tables, with equal number in each arm (n = 44). The CONSORT diagram is shown in Figure 1.
Figure 1.
Consort diagram.
Group differences at baseline
Baseline data were analyzed to determine whether there were any significant differences between the two treatment groups. Chi-square tests were used to compare the CB group (OPA-K) and the SLB group (Damon Q) on the following categorical variables: sex and malocclusion classification. As shown in Table 1, the OPA-K and Damon Q group had approximately equal proportions by sex (P = 0.67) and malocclusion classification (P = 0.91). Independent t tests were used to compare the OPA-K group and the Damon Q group on the continuous variables: arch length discrepancy, age, height, weight, as well as SF-36T and OHIP-14T scales. There were no statistically significant differences between the OPA-K and Damon Q treatment groups on any demographic or clinical characteristics at baseline. All P values were > 0.05 (Table 1).
Table 1.
Description of sample at baseline.
| OPA-K (N = 44) |
Damon Q (N = 44) |
P | |
|---|---|---|---|
| Sex (N, %) | 0.67 | ||
| Female | 25, 48.1 | 27, 51.9 | |
| Male | 19, 52.8 | 17, 47.2 | |
| Age (Mean ± SD) | 20.77 ± 8.22 | 19.52 ± 6.40 | 0.43 |
| Malocclusion (N, %) | 0.91 | ||
| Class I | 15, 46.9 | 17, 53.1 | |
| Class II | 15, 51.7 | 14, 48.3 | |
| Class III | 14, 51.9 | 13, 48.1 | |
| ALD in mm (Mean ± SD) | 5.91 ± 4.18 | 4.96 ± 3.58 | 0.26 |
| Height in cm (Mean ± SD) | 162.07 ± 9.10 | 162.70 ± 9.31 | 0.75 |
| Weight in kg (Mean ± SD) | 51.98 ± 11.48 | 52.11 ± 9.82 | 0.95 |
| SF-36T Scales (Mean, SD) | |||
| PCS | 56.87 ± 4.61 | 55.65 ± 4.43 | 0.21 |
| MCS | 51.04 ± 9.15 | 49.16 ± 8.36 | 0.32 |
| Physical functioning | 96.82 ± 4.83 | 96.14 ± 4.56 | 0.50 |
| Role-physical | 99.43 ± 2.21 | 99.20 ± 2.40 | 0.65 |
| Bodily pain | 90.34 ± 12.72 | 88.14 ± 11.38 | 0.40 |
| General health | 72.18 ± 19.98 | 70.02 ± 16.90 | 0.59 |
| Vitality | 73.64 ± 12.17 | 70.68 ± 15.83 | 0.33 |
| Social functioning | 64.25 ± 3.60 | 66.00 ± 5.26 | 0.07 |
| Role-emotional | 94.00 ± 12.88 | 93.25 ± 13.47 | 0.80 |
| Mental health | 73.23 ± 14.18 | 70.27 ± 13.84 | 0.33 |
| OHIP-14T scales (Mean ± SD) | |||
| Overall scores | 13.84 ± 10.14 | 11.36 ± 6.88 | 0.18 |
| Functional limitation | 1.52 ± 1.52 | 1.39 ± 1.57 | 0.68 |
| Physical pain | 2.23 ± 2.12 | 1.55 ± 1.34 | 0.08 |
| 3.64 ± 2.35 | 3.57 ± 1.84 | 0.88 | |
| Physical disability | 1.61 ± 1.75 | 1.16 ± 1.41 | 0.18 |
| PDA | 2.57 ± 2.62 | 2.05 ± 1.98 | 0.29 |
| Social disability | 1.18 ± 1.66 | 0.82 ± 1.15 | 0.24 |
| Handicap | 1.09 ± 1.63 | 0.82 ± 1.19 | 0.37 |
ALD = arch length discrepancy; MCS = mental component score; OHIP = oral health impact profile; PCS = physical component score; PDA = psychological disability; PDF = psychological discomfort; SD = standard deviation.
Comparing OHRQoL before and during initial phases of orthodontic treatment
SF-36T comparisons
Table 2 summarizes the comparisons of the SF-36T sub scores between T0 and TI and between T0 and T2. With only one exception, there were no statistically significant differences in SF-36T scores between T1 and T0 or between T2 and T0. There was a significant decrease in bodily pain at T1 compared with T0 (i.e., worse pain at T1 than at T0, P < 0.01).
Table 2.
Comparisons of QoL (SF-36T) and HQoL (OHIP-14T) from baseline (T0) to orthodontic treatment 1 week (T1) and 1 month (T2).a
| T0 scores |
T1 scores |
Difference T1 vs. T0 |
T2 scores |
Difference T2 vs. T0 |
|||
|---|---|---|---|---|---|---|---|
| (Mean ± SD) | (Mean ± SD) | Difference in means | Effect size | (Mean ± SD) | Difference in means | Effect size | |
| SF-36T | |||||||
| PCS | 56.26 ± 4.53 | 55.48 ± 5.35 | −0.78 | −0.17 | 56.58 ± 5.29 | 0.32 | 0.07 |
| MCS | 50.10 ± 8.77 | 49.98 ± 9.49 | −0.12 | −0.01 | 51.08 ± 10.34 | 0.98 | 0.11 |
| Physical functioning | 96.48 ± 4.68 | 96.25 ± 5.88 | −0.23 | −0.05 | 96.36 ± 6.42 | −0.11 | −0.02 |
| Role-physical | 99.32 ± 2.30 | 98.98 ± 3.05 | −0.34 | −0.15 | 98.98 ± 3.05 | −0.34 | −0.15 |
| Bodily pain | 89.24 ± 12.05 | 82.93 ± 15.39 | −6.31* | −0.52 | 87.55 ± 12.52 | −1.69 | −0.14 |
| General health | 71.10 ± 18.43 | 71.33 ± 15.39 | 0.23 | 0.01 | 74.16 ± 18.36 | 3.06 | 0.17 |
| Vitality | 72.16 ± 14.12 | 72.50 ± 16.85 | 0.34 | 0.02 | 72.27 ± 19.24 | 0.11 | 0.01 |
| Social functioning | 65.13 ± 4.56 | 63.70 ± 6.74 | −1.42 | −0.31 | 63.40 ± 9.12 | −1.73 | −0.38 |
| Role-emotional | 93.63 ± 13.10 | 94.00 ± 12.80 | 0.38 | 0.03 | 96.26 ± 10.50 | 2.26 | 0.17 |
| Mental health | 71.75 ± 14.01 | 71.45 ± 15.74 | −0.30 | −0.02 | 73.27 ± 15.80 | 1.52 | 0.11 |
| OHIP-14T | |||||||
| Overall scores | 12.6 ± 8.70 | 18.11 ± 11.00 | 5.51* | 0.63 | 14.32 ± 10.50 | 1.72 | 0.20 |
| Functional limitation | 1.45 ± 1.54 | 2.06 ± 2.10 | 0.60* | 0.39 | 1.93 ± 1.73 | 0.48* | 0.31 |
| Physical pain | 1.89 ± 1.80 | 4.13 ± 2.40 | 2.24* | 1.25 | 2.76 ± 2.23 | 0.88* | 0.49 |
| 3.60 ± 2.10 | 3.45 ± 2.20 | −0.15 | −0.07 | 2.83 ± 1.83 | −0.77* | −0.37 | |
| Physical disability | 1.39 ± 1.60 | 3.47 ± 2.60 | 2.08* | 1.30 | 2.66 ± 2.33 | 1.27* | 0.79 |
| PDA | 2.31 ± 2.32 | 2.57 ± 2.20 | 0.26 | 0.11 | 2.13 ± 2.14 | −0.18 | −0.08 |
| Social disability | 1.00 ± 1.43 | 1.31 ± 1.40 | 0.31 | 0.21 | 1.08 ± 1.45 | 0.08 | 0.06 |
| Handicap | 0.95 ± 1.42 | 1.14 ± 1.50 | 0.18 | 0.13 | 0.93 ± 1.43 | −0.02 | −0.02 |
*P < 0.01.
HQoL = healthy quality of life; MCS = mental component score; OHIP = oral health impact profile; PCS = physical component score; PDA = psychological disability; PDF = psychological discomfort; QoL = quality of life; SD = standard deviation; SF = short form.
Effect size: <0.2 = minimal change; 0.2–0.49 = small change; 0.5–0.8 = moderate change; >0.8 = large change.
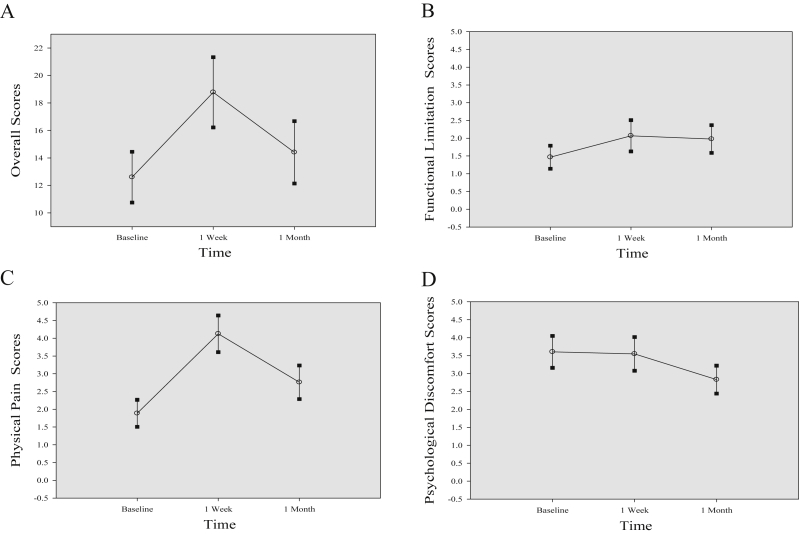
OHIP-14T comparison
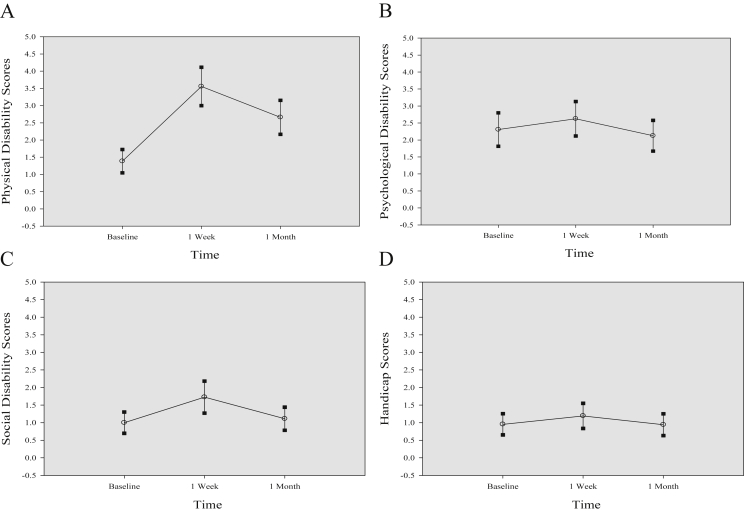
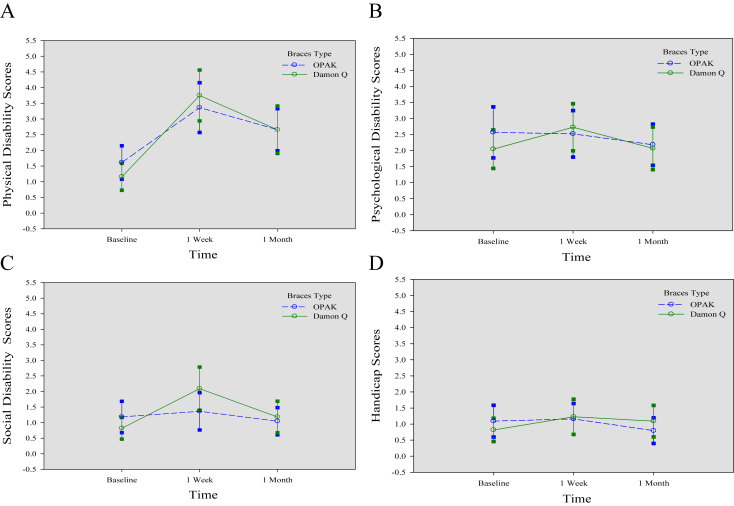
Table 2 summarizes the comparisons of the OHIP-14T overall and subscores between T0 and TI and between T0 and T2. Unlike with the SF-36T, several differences in OHIP-14T scores over time were observed. For the overall score and three of the scales (functional limitation, physical pain, and physical disability), scores were significantly worse at T1 than at T0 (Figure 2, Figure 3). No significant differences were found between T0 and T1 for the other four subscales of the OHIP-14T (psychological discomfort, psychological disability, social disability, and handicap). All P values were > 0.05.
Figure 2.
Mean OHIP-14T scales for baseline, 1 week, and 1 month (OPA-K + Damon Q) and 95% confidence intervals. (A) Overall score; (B) functional limitation; (C) physical pain; (D) psychological discomfort.
Figure 3.
Mean OHIP-14T scales for baseline, 1 week, and 1 month (OPA-K + Damon Q) and 95% confidence intervals. (A) Physical disability; (B) psychological disability; (C) social disability; (D) handicap.
Comparing changes in OHRQoL for patients treated with SLB versus CB
Differences in SF-36T scores
Repeated measures ANOVA results indicated no statistically significant group by time interaction on any of the SF-36T eight scales.
The physical component score, the mental component score, and seven of the scales (PF, RP, GH, VT, SF, RE, and MH) yielded no statistically significant differences between groups, within groups, or in group by time interaction effect; all P values were > 0.05 (Table 3).
Table 3.
Summary of the ANOVA to determine the effect of orthodontic therapy on HRQoL (SF-36T) and OHRQoL (OHIP-14T).
| Type III analysis | SF-36T |
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCS |
MCS |
Physical functioning |
Role-physical |
Bodily pain |
General health |
Vitality |
Social functioning |
Role-emotional |
Mental health |
|||||||||||||
| MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | MS | F Value | |||
| Between | ||||||||||||||||||||||
| Braces type | 41.32 | 0.77 | 298.09 | 1.30 | 9.47 | 0.16 | 18.56 | 1.41 | 504.64 | 1.52 | 700.38 | 0.96 | 985.23 | 1.48 | 2.56 | 0.04 | 3.88 | 0.02 | 318.56 | 0.60 | ||
| Error | 53.36 | 229.80 | 60.66 | 13.14 | 332.99 | 729.33 | 664.21 | 62.05 | 227.45 | 535.52 | ||||||||||||
| Within | ||||||||||||||||||||||
| Time | 29.39 | 2.13 | 36.48 | 1.61 | 1.22 | 0.06 | 3.41 | 0.64 | 937.62 | 9.13* | 255.23 | 2.75 | 2.99 | 0.03 | 74.73 | 1.70 | 179.00 | 1.61 | 83.77 | 1.04 | ||
| Time* Braces type | 8.65 | 0.63 | 5.75 | 0.25 | 6.51 | 0.32 | 1.52 | 0.28 | 33.60 | 0.33 | 36.75 | 0.40 | 16.67 | 0.16 | 39.80 | 0.90 | 28.25 | 0.25 | 45.11 | 0.56 | ||
| Error (Time) |
13.79 |
22.70 |
20.41 |
5.37 |
102.65 |
92.80 |
105.63 |
44.04 |
111.43 |
80.59 |
||||||||||||
| Type III analysis |
OHIP-14T |
|||||||||||||||||||||
| Overall score |
FL |
Physical pain |
PDF |
Physical disability |
PDA |
Social disability |
Handicap |
|||||||||||||||
| MS |
F Value |
MS |
F Value |
MS |
F Value |
MS |
F Value |
MS |
F Value |
MS |
F Value |
MS |
F Value |
MS |
F Value |
|||||||
| Between | ||||||||||||||||||||||
| Braces type | 16.00 | 0.07 | 1.37 | 0.20 | 0.97 | 0.12 | 0.97 | 0.12 | 0.10 | 0.01 | 0.74 | 0.07 | 0.14 | 0.04 | 0.00 | 0.00 | ||||||
| Error | 222.58 | 6.81 | 8.29 | 8.33 | 8.74 | 10.93 | 3.60 | 3.71 | ||||||||||||||
| Within | ||||||||||||||||||||||
| Time | 699.97 | 16.10* | 8.89 | 6.25* | 112.00 | 38.30* | 14.81 | 6.74* | 107.06 | 31.57* | 4.89 | 2.11 | 2.23 | 1.67 | 1.21 | 0.83 | ||||||
| Time* Braces type | 75.23 | 1.73 | 0.07 | 0.05 | 6.82 | 2.33 | 0.12 | 0.05 | 6.39 | 1.89 | 4.36 | 1.88 | 1.72 | 1.28 | 1.79 | 1.23 | ||||||
| Error (Time) | 43.47 | 1.42 | 2.93 | 2.20 | 3.39 | 2.32 | 1.34 | 1.46 | ||||||||||||||
ANOVA = analysis of variance; F value = Fisher–Snedecor value; FL = functional limitation; MCS = mental component score; MS = mean of square; OHIP = oral health impact profile; PCS = physical component score; PDA = psychological disability; PDF = psychological discomfort; SD = standard deviation.
*P < 0.01.
For the bodily pain subscale, there was a significant difference in pain for baseline to 1 week (P < 0.01) and 1 week to 1 month (P = 0.02). There was no significant difference in pain for baseline to 1 month (P = 0.66). (See Table 3, Table 4).
Table 4.
Summary of the means by group and time.
| N | Baseline |
1 week |
1 month |
|||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Change %a | Cohen's d | Mean (SD) | Change %a | Cohen's d | ||
| SF-36T: Bodily pain scale | ||||||||
| OPA-K | 44 | 90.34 (12.72) | 85.02 (15.45) | −5.9 | −0.42 | 88.50 (11.81) | −2.0 | −0.14 |
| Damon Q | 44 | 88.14 (11.38) | 80.84 (15.20) | −8.3 | −0.64 | 86.59 (13.26) | −2.0 | −0.14 |
| Total | 88 | 89.24 (12.05) | 82.93 (15.39) | −7.1 | −0.52 | 87.55 (12.52) | −1.9 | −0.14 |
| OHIP-14T: Overall score | ||||||||
| OPA-K | 44 | 13.84 (10.14) | 17.52 (10.64) | 26.6 | 0.36 | 14.41 (9.33) | 4.1 | 0.06 |
| Damon Q | 44 | 11.36 (6.88) | 18.70 (11.52) | 64.6 | 1.07 | 14.23 (11.66) | 25.2 | 0.42 |
| Total | 88 | 12.60 (8.70) | 18.11 (11.04) | 43.7 | 0.63 | 14.32 (10.50) | 13.6 | 0.20 |
| OHIP-14T: Functional limitation | ||||||||
| OPA-K | 44 | 1.52 (1.52) | 2.16 (2.18) | 41.8 | 0.42 | 1.98 (1.58) | 29.9 | 0.30 |
| Damon Q | 44 | 1.39 (1.57) | 1.95 (1.94) | 41.0 | 0.36 | 1.89 (1.88) | 36.1 | 0.32 |
| Total | 88 | 1.45 (1.54) | 2.06 (2.05) | 41.4 | 0.39 | 1.93 (1.73) | 32.8 | 0.31 |
| OHIP-14T: Physical pain | ||||||||
| OPA-K | 44 | 2.23 (2.12) | 3.91 (2.42) | 75.5 | 0.79 | 2.82 (2.11) | 26.5 | 0.28 |
| Damon Q | 44 | 1.55 (1.34) | 4.34 (2.46) | 180.9 | 2.09 | 2.70 (2.38) | 75.0 | 0.87 |
| Total | 88 | 1.89 (1.80) | 4.13 (2.43) | 118.7 | 1.25 | 2.76 (2.23) | 46.4 | 0.49 |
| OHIP-14T: Psychological discomfort | ||||||||
| OPA-K | 44 | 3.64 (2.35) | 3.50 (2.21) | −3.8 | −0.06 | 2.93 (1.63) | −19.4 | −0.30 |
| Damon Q | 44 | 3.57 (1.84) | 3.41 (2.21) | −4.5 | −0.09 | 2.73 (2.03) | −23.6 | −0.46 |
| Total | 88 | 3.60 (2.10) | 3.45 (2.20) | −4.1 | −0.07 | 2.83 (1.83) | −21.5 | −0.37 |
| OHIP-14T: Physical disability | ||||||||
| OPA-K | 44 | 1.61 (1.76) | 3.18 (2.55) | 97.2 | 0.89 | 2.66 (2.20) | 64.8 | 0.60 |
| Damon Q | 44 | 1.16 (1.41) | 3.75 (2.67) | 223.5 | 1.83 | 2.66 (2.49) | 129.4 | 1.06 |
| Total | 88 | 1.39 (1.60) | 3.47 (2.61) | 150.0 | 1.30 | 2.66 (2.33) | 91.8 | 0.80 |
OHIP = oral health impact profile; SD = standard deviation; SF = short form.
% change from baseline.
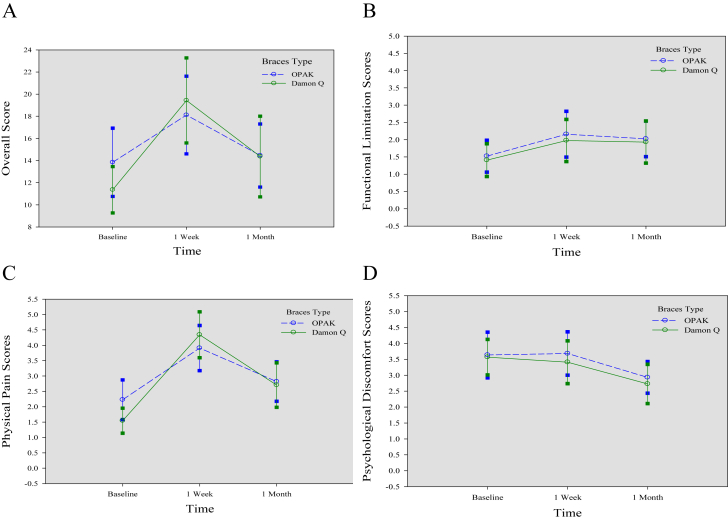
Differences in OHIP-14T scores
Three of the scales (Psychological disability, Social disability, and Handicap) yielded no statistically significant difference between groups, within groups, or group by time interaction effect; all P values were > 0.05. For the overall scores and four of the subscales, the only significant finding was a difference across time regardless of group membership (Overall, Functional limitation, Physical pain, Psychological discomfort, and Physical disability; Table 3, Figure 4, Figure 5).
Figure 4.
Mean OHIP-14T scales for baseline, 1 week, and 1 month (OPA-K vs. Damon Q) and 95% confidence intervals. (A) Overall score; (B) functional limitation; (C) physical pain; (D) psychological discomfort.
Figure 5.
Mean OHIP-14T scales for baseline, 1 week, and 1 month (OPA-K vs. Damon Q) and 95% confidence intervals. (A) Physical disability; (B) psychological disability; (C) social disability; (D) handicap.
For the overall scores of OHIP-14T, there was a significant difference for baseline to 1 week and 1 week to 1 month (P < 0.01). For the functional limitation scale, there was a significant difference for baseline to 1 week (P = 0.01) and baseline to 1 month (P = 0.03). For the physical pain scale, there was a significant difference for baseline to 1 week, baseline to 1 month, and 1 week to 1 month (all P < 0.01). For the psychological discomfort scale, there was a significant difference for baseline to 1 month (P < 0.01) and 1 week to 1 month (P = 0.02). For the physical disability scale, there was a significant difference for baseline to 1 week, baseline to 1 month, and 1 week to 1 month (all P < 0.01; Table 3, Table 4, Figure 4, Figure 5).
Discussion
The generic SF-36T was not sensitive to changes over time; however, the condition-specific OHIP-14T highlighted the differences in functional limitation, physical pain, psychological discomfort, and physical disability among the baseline, 1 week, and 1 month assessments. For the generic HRQoL, the SF-36T could not discriminate among patients in seven out of its eight domains among the baseline, 1 week, and 1 month. This result was in accordance with findings of previous studies that showed generic health measures are less responsive than condition-specific health measures.18, 19, 20, 21, 22 However, the use of generic measures provides an assessment of impact compared with that of other systemic disease and conditions. Furthermore, the condition-specific OHIP-14T showed small to moderate significant correlations compared with the generic SF-36T. This suggests and confirms with other studies that the generic health approach assesses different constructs than the condition-specific health approach.23 Some researchers further pointed out that both HRQoL measures are complementary rather than alternative sources of information.20, 21
Significant differences over time in OHRQoL as measured by the OHIP-14T are in accordance with previous studies that have shown that wearing a fixed orthodontic appliance has real impacts on patients' OHRQoL.24, 25, 26, 27 For OHIP-14T overall scores, statistically significant differences were observed between baseline to 1 week and 1 week to 1 month, except for baseline to 1 month (Table 3). Compared with baseline, the OHIP-14T overall score deteriorated at 1 week (43.7%) and at 1 month (13.6%) (Table 4).
For functional limitation scales, statistically significant differences were found between baseline to 1 week and baseline to 1 month, but not for 1 week to 1 month (Table 3). This indicated that 1 week after orthodontic treatment, the patients suffered from more oral functional limitation in trouble pronouncing words (46.59%; Table 5). Those impacts subsided around 1 month after orthodontic therapy but still showed statistically significant differences compared with those at baseline. These findings were in agreement with a previous study, although the researchers used different measures.24
Table 5.
Frequency (%) distribution of reported impacts on the 14 items of the oral health impact profile measure (OHIP-14T) at three times (N = 88).
| T0 | T1 | T2 | |
|---|---|---|---|
| Item 1: Trouble pronouncing words | 37.50 | 46.59 | 47.73 |
| Item 2: Taste worse | 5.68 | 14.77 | 7.95 |
| Item 3: Uncomfortable to eat | 39.77 | 68.18 | 39.77 |
| Item 4: Sore jaw | 25.00 | 67.05 | 51.14 |
| Item 5: Self-consciousness | 73.86 | 70.45 | 57.95 |
| Item 6: Psychological discomfort in worries | 40.91 | 45.45 | 28.41 |
| Item 7: Avoiding eating | 20.45 | 42.05 | 30.68 |
| Item 8: Interrupting meals | 35.23 | 65.91 | 52.27 |
| Item 9: Concentration affected | 31.82 | 37.50 | 28.41 |
| Item 10: Been embarrassed | 40.91 | 40.91 | 40.91 |
| Item 11: Irritable with others | 13.64 | 21.59 | 17.05 |
| Item 12: Difficulty doing job | 9.09 | 21.59 | 15.91 |
| Item 13: Life unsatisfying | 17.05 | 22.73 | 18.18 |
| Item 14: Unable to work | 6.82 | 10.23 | 10.23 |
T0 = baseline; T1 = 1 week after orthodontic treatment; T2 = 1 month after orthodontic treatment.
For physical pain scales, statistically significant differences were observed between baseline to 1 week, 1 week to 1 month, and baseline to 1 month (Table 3). This revealed that 1 week after orthodontic treatment, the patients suffered from more physical pain in finding it uncomfortable to eat (68.18%) and having a sore jaw (67.05%; Table 5). Those symptoms subsided 1 month later, but there were statistically significant differences compared with those at baseline. These results confirmed those of some previous studies.24, 28
For psychological discomfort scales, statistically significant differences were observed between baseline to 1 month and 1 week to 1 month, except for baseline to 1 week (Table 3). This implied that 1 month after orthodontic treatment, the patients suffered from less psychological discomfort in worries (from 40.91% to 28.41%) and self-consciousness (from 73.86% to 57.95%) than those at baseline (Table 5).
For physical disability scales, statistically significant differences were found between baseline to 1 week, 1 week to 1 month, and baseline to 1 month (Table 3). This indicated that 1 week after orthodontic treatment, the patients suffered from more physical disability in avoiding eating (42.05%) and interrupting meals (65.91%). Those impacts subsided at 1 month after orthodontic therapy (Table 5).
The OHIP-14T overall score was the highest among all three different intervals at 1 week. Examination of these findings revealed that the most frequently reported impacts were trouble pronouncing words (46.59%), discomfort eating (68.18%), sore jaw (67.05%), avoiding eating (42.05%), and interrupting meals (65.91%; Table 5). Our findings suggest that orthodontic therapy does influence patients' daily performance, particularly when eating meals and pronouncing words. These findings are in accordance with those of previous studies that reported diet limitations and pain sensation are the chief complaints for most patients under orthodontic therapy during the initial phase.29, 30, 31 Sergl et al26 found that difficulty in speech, difficulty in swallowing, and low self-confidence in public are common complaints for most patients experiencing orthodontic therapy, no matter whether fixed or removable appliances were placed. It implied that foreign (fixed or removable) orthodontic appliances are the main factors causing the above symptoms.26
Some impacts declined and the scores of OHRQoL were similar when compared with the baseline at 1 month. As the orthodontic therapy went on, the overall scores decreased; however, the scores of functional limitation, physical pain, psychological discomfort, and physical disability were still somewhat compromised (Table 5). Our findings are in agreement with those of previous researchers.29, 32 This indicates that adaptation to orthodontic therapy actually reduced the impacts with trouble pronouncing words, discomfort eating, sore jaw, avoiding eating, and interrupting meals, no matter what the patients felt or experienced during treatment.29 Surprisingly, on the other hand, worries (from 40.91% to 28.41%) and self-consciousness (from 73.86% to 57.95%) both declined at 1 month (Table 5). The possible reason is that patients felt worried and were self-conscious about the pending orthodontic treatment. After wearing a fixed orthodontic appliance for a period of time, they found it was not as terrible as they originally expected. Therefore, their worries and self-consciousness were gradually relieved as the treatment progressed.
The results provide important information for orthodontists to share with their patients prior to orthodontic treatment. Patients may encounter a temporary deterioration in overall OHRQoL around 1 week. OHRQoL will improve around 1 month later, especially with regard to eating discomfort and sore jaws. As for trouble pronouncing words, decreased sense of taste, avoiding eating, and interrupting meals, these impacts will improve after 1 week. In terms of worrying and self-consciousness, these impacts will continue to improve after 1 month.
In our study, patients with malocclusion who were treated with Damon Q showed no statistically significant differences in OHIP-14T score in functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicaps compared with those treated with OPA-K during initial phase of orthodontic treatment.
Our results were in disagreement with the previous claims of most SLB companies. The manufacturers advocated that the SLB design would reduce friction between brackets and archwire and allow lighter forces to move the teeth. In this way, it would result in less physical discomfort to the malocclusion patients during the initial fixed orthodontic therapy (http://www.damonbraces.com). However, in our study, from patients' perceptive, the lighter forces still cause some discomfort similar (even higher) to those of CB. Since it is very difficult to simulate the real oral cavity situations that include speech, mastication, and swallowing, the results from in vitro studies are difficult to generalize to in vivo studies. Furthermore, perceived pain is very subjective; it varies among different individuals. Pain has been shown to be related to an individual's past experiences, education level, socioeconomic class, cultural background, and sometimes psychological status.33
Although this study is a prospective, randomized controlled trial with adequate sample size, we only observed HRQoL and OHRQoL for the orthodontic patients for the initial 1 month. We should conduct long-term longitudinal studies to observe the entire orthodontic treatment and compare the difference between SLB systems (Damon Q) and CB system (OPA-K).
The results of this randomized clinical trial did not support the primary hypothesis of this study. SLB (Damon Q) are not shown to be statistically superior to CB (OPA-K) in improving HRQoL in patients with malocclusion during initial orthodontic treatment.
The oral health assessment measurement (OHIP-14T) proved to be superior (more sensitive) to generic health assessment measurements (SF-36T) in detecting OHRQoL differences in patients with malocclusion during initial orthodontic therapy.
The findings provide important information for orthodontists to inform the patients before orthodontic treatment that they may experience a temporary deterioration in the overall OHRQoL after 1 week of fixed orthodontic therapy and that it would recover about 1 month later, especially for eating discomfort, sore jaw, irritability toward others, and difficultly with job performance. As for trouble pronouncing words, worsening taste, worries, and self-consciousness, these impacts improve after 1 week of fixed orthodontic therapy.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This study was performed in the Mackay Memorial Hospital. The authors wish to acknowledge the support and encouragement of their colleagues in the Orthodontic Division of Dental Department. The authors are indebted to Professor Ellen J. MacKenzie and Professor Leiyu Shi for the thesis advice. The authors also appreciate the statistical advice given by Professor Marie Diener-West, Miss Fang-Ju Sun, and Mr. Jing-Yang Huang.
References
- 1.O'Brien K., Kay L., Fox D., Mandall N. Assessing oral health outcomes for orthodontics–measuring health status and quality of life. Community Dent Health. 1998;15:22–26. [PubMed] [Google Scholar]
- 2.Buschang P.H., Stroud J., Alexander R.G. Differences in dental arch morphology among adult females with untreated Class I and Class II malocclusion. Eur J Orthod. 1994;16:47–52. doi: 10.1093/ejo/16.1.47. [DOI] [PubMed] [Google Scholar]
- 3.Harradine N.W. Self-ligating brackets: where are we now? Br J Orthod. 2003;30:262–273. doi: 10.1093/ortho/30.3.262. [DOI] [PubMed] [Google Scholar]
- 4.Cacciafesta V., Sfondrini M.F., Ricciardi A., Scribante A., Klersy C., Auricchio F. Evaluation of friction of stainless steel and esthetic self-ligating brackets in various bracket-archwire combinations. Am J Orthod Dentofacial Orthop. 2003;124:395–402. doi: 10.1016/s0889-5406(03)00504-3. [DOI] [PubMed] [Google Scholar]
- 5.Read-Ward G.E., Jones S.P., Davies E.H. A comparison of self-ligating and conventional orthodontic bracket systems. Br J Orthod. 1997;24:309–317. doi: 10.1093/ortho/24.4.309. [DOI] [PubMed] [Google Scholar]
- 6.Thorstenson G.A., Kusy R.P. Comparison of resistance to sliding between different self-ligating brackets with second-order angulation in the dry and saliva states. Am J Orthod Dentofacial Orthop. 2002;121:472–482. doi: 10.1067/mod.2002.121562. [DOI] [PubMed] [Google Scholar]
- 7.Shivapuja P.K., Berger J. A comparative study of conventional ligation and self-ligation bracket systems. Am J Orthod Dentofacial Orthop. 1994;106:472–480. doi: 10.1016/S0889-5406(94)70069-9. [DOI] [PubMed] [Google Scholar]
- 8.Turnbull N.R., Birnie D.J. Treatment efficiency of conventional vs self-ligating brackets: effects of archwire size and material. Am J Orthod Dentofacial Orthop. 2007;131:395–399. doi: 10.1016/j.ajodo.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Shivapuja P.K., Berger J. A comparative study of conventional ligation and self-ligation bracket systems. Am J Orthod Dentofacial Orthop. 1994;106:472–480. doi: 10.1016/S0889-5406(94)70069-9. [DOI] [PubMed] [Google Scholar]
- 10.Maijer R., Smith D.C. Time savings with self-ligating brackets. J Clin Orthod. 1990;24:29–31. [PubMed] [Google Scholar]
- 11.Forsberg C.M., Brattstrom V., Malmberg E., Nord C.E. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and lactobacilli. Eur J Orthod. 1991;13:416–420. doi: 10.1093/ejo/13.5.416. [DOI] [PubMed] [Google Scholar]
- 12.Eberting J.J., Straja S.R., Tuncay O.C. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001;4:228–234. doi: 10.1034/j.1600-0544.2001.40407.x. [DOI] [PubMed] [Google Scholar]
- 13.Harradine N.W. Self-ligating brackets and treatment efficiency. Clin Orthod Res. 2001;4:220–227. doi: 10.1034/j.1600-0544.2001.40406.x. [DOI] [PubMed] [Google Scholar]
- 14.Pringle A.M., Petrie A., Cunningham S.J., McKnight M. Prospective randomized clinical trial to compare pain levels associated with 2 orthodontic fixed bracket systems. Am J Orthod Dentofacial Orthop. 2009;136:160–167. doi: 10.1016/j.ajodo.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Miles P.G., Weyant R.J., Rustveld L. A clinical trial of Damon 2 vs conventional twin brackets during initial alignment. Angle Orthod. 2006;76:480–485. doi: 10.1043/0003-3219(2006)076[0480:ACTODV]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Tseng H.M., Lu J.F.R., Tsai Y.J. Assessment of health-related quality of life in Taiwan (II): norming and validation of SF-36 Taiwan version. Taiwan J Public Health. 2003;22:512–518. [Google Scholar]
- 17.Kuo H.C., Chen J.H., Wu J.H., Chou T.M., Yang Y.H. Application of the oral health impact profile (OHIP) among Taiwanese elderly. Qual Life Res. 2011;20:1707–1713. doi: 10.1007/s11136-011-9901-z. [DOI] [PubMed] [Google Scholar]
- 18.Allen F., Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446–450. [PubMed] [Google Scholar]
- 19.Lee S., McGrath C., Samman N. Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int J Oral Maxillofac Surg. 2007;36:488–492. doi: 10.1016/j.ijom.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 20.McMillan A.S., Leung K.C., Leung W.K., Wong M.C., Lau C.S., Mok T.M. Impact of Sjogren's syndrome on oral health-related quality of life in southern Chinese. J Oral Rehabil. 2004;31:653–659. doi: 10.1111/j.1365-2842.2004.01384.x. [DOI] [PubMed] [Google Scholar]
- 21.Shugars D.A., Gentile M.A., Ahmad N., Stavropoulos M.F., Slade G.D., Phillips C. Assessment of oral health-related quality of life before and after third molar surgery. J Oral Maxillofac Surg. 2006;64:1721–1730. doi: 10.1016/j.joms.2006.03.052. [DOI] [PubMed] [Google Scholar]
- 22.Al-Bitar Z.B., Al-Omari I.K., Al-Ahmad H.T., El Maaytah M.A., Cunningham S.J. A comparison of health-related quality of life between Jordanian and British orthognathic patients. Eur J Orthod. 2009;31:485–489. doi: 10.1093/ejo/cjp034. [DOI] [PubMed] [Google Scholar]
- 23.Bennett M.E., Phillips C.L. Assessment of health-related quality of life for patients with severe skeletal disharmony: a review of the issues. Int J Adult Orthodon Orthognath Surg. 1999;14:65–75. [PubMed] [Google Scholar]
- 24.Zhang M., McGrath C., Hagg U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy. Am J Orthod Dentofacial Orthop. 2008;133:25–29. doi: 10.1016/j.ajodo.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 25.Erdinc A.M., Dincer B., Erdinc A.M.E., Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 26.Sergl H.G., Klages U., Zentner A. Functional and social discomfort during orthodontic treatment—effects on compliance and prediction of patients' adaptation by personality variables. Eur J Orthod. 2000;22:307–315. doi: 10.1093/ejo/22.3.307. [DOI] [PubMed] [Google Scholar]
- 27.Bernabe E., de Oliveira C.M., Sheiham A. Comparison of the discriminative ability of a generic and a condition-specific OHRQoL measure in adolescents with and without normative need for orthodontic treatment. Health Qual Life Outcomes. 2008;6:64. doi: 10.1186/1477-7525-6-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen M., Wang D.W., Wu L.P. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang M., McGrath C., Hägg U. Patients' expectations and experiences of fixed orthodontic appliance therapy. Angle Orthod. 2007;77:318–322. doi: 10.2319/0003-3219(2007)077[0318:PEAEOF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Mandall N., Lowe C., Worthington H., Sandler J., Derwent S., Abdi-Oskouei M. Which orthodontic archwire sequence? A randomized clinical trial. Eur J Orthod. 2006;28:561–566. doi: 10.1093/ejo/cjl030. [DOI] [PubMed] [Google Scholar]
- 31.Lew K.K. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent Oral Epidemiol. 1993;21:31–35. doi: 10.1111/j.1600-0528.1993.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 32.Chen M., Wang D.W., Wu L.P. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010;80:49–53. doi: 10.2319/010509-9.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ngan P., Kess B., Wilson S. Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96:47–53. doi: 10.1016/0889-5406(89)90228-x. [DOI] [PubMed] [Google Scholar]