Dear Editors,
Studies on speech abnormalities in schizophrenia suggest that atypical turn-taking during conversation is a prominent feature of speech patterns in psychosis. These studies have typically reported inappropriate pause times based on pragmatic rating scales (e.g. Colle et al., 2013). However, these subjective assessments are susceptible to rater bias and provide only a broad perceptual analysis of vocal expression; specific, quantifiable speech parameters cannot be assessed.
While impairments in turn-taking are pervasive in formal psychosis samples, it is unclear whether these anomalies exist in individuals at clinical high risk (CHR) for psychotic disorders. Because language data is easy to collect and conversation is a typical part of clinical assessments, linguistic patterns such as atypical turn-taking may be a readily-accessible domain to search for early biomarkers for psychosis risk. These patterns may also improve etiological understanding (highlighting foundational contributors to social and functional deficits) and identify novel treatment targets in the psychosis prodrome.
The present study evaluated turn-taking from speech data provided by CHR youth and healthy controls to address two goals: 1) evaluate if CHR individuals exhibit abnormalities in turn-taking and 2) investigate if turn-taking performance is correlated with symptom severity within the CHR group. Our data was taken from clinical interviews with the duration of between-turn pauses (BTPs) preceding responses as our metric. Based on findings in schizophrenia, we predicted that CHR youth would exhibit deficits in turn-taking performance. Further, consistent with Colle et al. (2013), who found a correlation between stronger clinical symptoms and poorer pragmatic performance in patients with schizophrenia, we predicted that turn-taking abnormalities would correlate with elevated prodromal symptoms. Following Cohen et al. (2016), who suggest that vocal parameters in speech of patients with schizophrenia are context- and demography-dependent, our analyses controlled for age and sex. Based on previous studies of turn-taking in the general population, we controlled for the complexity and duration of the participant’s response and the duration of the question preceding the BTP (Barthel et al., 2015; Casillas et al., 2015). Finally, we controlled for context (Cohen et al., 2016) by contrasting BTP durations following informal background questions (about daily habits, family, etc.) and structured interview questions.
Data was taken from structured clinical interviews with 34 neuroleptic-free CHR youth and 36 age-matched healthy controls. Participants were administered the Structural Interview for Prodromal Syndromes (SIPS; Miller et al., 2003), the Prodromal Inventory of Negative Symptoms (Pelletier-Baldelli et al., 2017), the Structured Clinical Interview for DSM-IV (SCID-I; First et al., 2015), the Global Functioning Scale: Social (GFS-S) (Auther et al., 2006), and the Beck Depression Inventory (Beck et al., 1996). Ten-minute sequences from each interview were annotated to measure the duration of the interviewer’s questions, each BTP, and the participant’s responses.
Two linear mixed-effects regression models were constructed with BTP duration as the dependent variable. The first included group as a predictor; the second had positive and negative symptom severity (assessed by the SIPS) as predictors. All results reported below were stable when measures of global social functioning and severity of depression were included in the models.
The first analysis yielded no significant group effect (β = 0.045, χ2(1) = 0.3, p = 0.586) or interactions (all χ2(1) < 1, p > 0.10) on BTP durations. Demographic and linguistic control variables yielded results consistent with existing literature. Response complexity was significant (β = 0.332, χ2(1) = 53.68, p < .0001); high complexity responses were preceded by longer BTPs than low complexity responses, consistent with Casillas et al. (2015). There was a significant association between BTPs and question type (β = 0.339, χ2(1) = 20.57, p < .0001). Background questions were followed by shorter BTPs than structured interview questions, consistent with the context-dependent patterns of Cohen et al. (2016). Longer response (β = 0.060, χ2(1) = 6.54, p = 0.0105) and question durations (β = 0.068, χ2(1) = 10.18, p = 0.0014) lead to longer BTPs. The latter contradicts findings that shorter BTPs follow longer turns (Barthel et al., 2015). Participant sex had also an effect (β = 0.210, χ2(1) = 5.86 p = 0.0155); BTPs were longer in male than female speech.
The second analysis (CHR speakers only) included positive and negative symptom severity as predictors. Severity of positive symptoms had a significant effect on BTP durations (β = 0.047, χ2(1) = 4.13 p = 0.0422); participants with higher positive symptoms produced longer BTPs (Figure 1). No significant interactions with positive symptoms were found (all χ2s(1) < 1, p > 0.10). Several effects from the group model were replicated: response complexity (β = 0.324, χ2(1) = 17.28, p < .0001), question type (β = 0.654, χ2(1) = 4.02, p = 0.0451), response duration (β = 0.070, χ2(1) = 8.36, p = 0.0038), and sex (β = 0.341, χ2(1) = 6.44, p = 0.0112). Younger CHR participants used marginally longer BTPs than older CHR participants (β = −0.071, χ2(1) = 2.95, p = 0.0859). There was no main effect of negative symptom severity (β = 0.015, χ2(1) = 1.42, p = 0.233); however, there was a marginal interaction between negative symptoms and response duration (β = −0.009, χ2(1) = 3.18, p = 0.0745).
Figure 1:
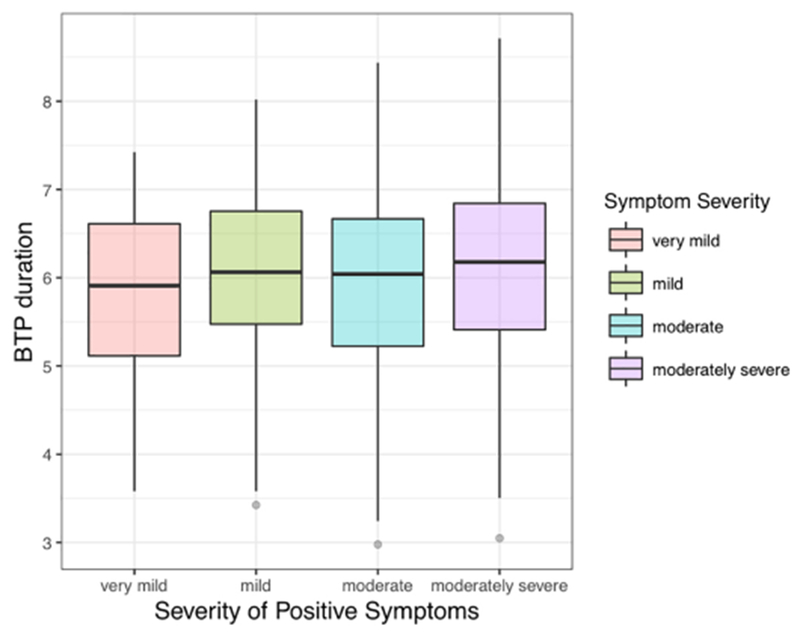
Effects of positive symptoms on BTP durations. Boxplot illustrating BTP duration in relation to the severity of positive symptoms. For ease of visualization, the x-axis groups symptom severity into four groups (very mild (score as evaluated by SIPS: 0-5), mild (6-10), moderate (11-15) and moderately severe (16-20) symptoms); note that symptom severity was treated as a continuous predictor in the model. The y-axis demonstrates log-transformed BTP durations. The severity of positive symptoms had a significant effect on BTP duration.
This study utilized specific, quantifiable speech measures to assess turn-taking behavior in CHR youth. While there were no group differences, higher positive symptoms within CHR speakers were associated with atypical patterns (longer BTPs), suggesting the clinical utility of this measure. Across all speakers, BTP durations were positively correlated with response complexity and were context-dependent, emphasizing the necessity to control these factors in conversational speech analyses. Future work should investigate turn-taking in additional naturalistic and non-clinical contexts. Furthermore, semantic and syntactic complexity are predictors for psychosis onset among CHR individuals (Bedi et al., 2015); including these variables in speech models, would enhance the predictive power of turn-taking measurements. Finally, our analytic technique can be extended to examine factors such as cognitive functioning and memory deficits; these may be implicated in aberrant turn-taking (Bögels et al., 2015) and could contribute a deeper understanding of the association between conversational pragmatics and psychosis risk.
Acknowledgement
The authors would like to thank the following research assistants, who aided in the preparation of data: Julia St. Jean, Grishma Reddy, Kimberly Rowghani, Cassandra Majewski, Kelly O’Conor, and Jennifer Weissman. Funding provided by National Institutes of Health Grants R01MH094650, R01MH112545, R21/R33MH103231, R21MH115231 and R21MH110374 to V.A.M. and a Weinberg College Research Innovation Grant to M.G. and V.A.M.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
No authors have conflicts to disclose.
References
- Auther AM, Smith CW, Cornblatt B, 2006. Global Functioning: Social Scale (GF: Social), Zucker-Hillside Hospital, New York. [Google Scholar]
- Barthel M, Sauppe S, Levinson SC, Meyer AS, 2015. The timing of utterance planning in task-oriented dialogue: Evidence from a novel list-completion paradigm. Frontiers in psychology 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G, 1996. Beck depression inventory-Ii manual San Antonio: The Psychological Corporation, Harcourt Brace & Co. [Google Scholar]
- Bedi G, Carrillo F, Cecchi GA, Slezak DF, Sigman M, Mota NB, Ribeiro S, Javitt DC, Copelli M, Corcoran CM, 2015. Automated analysis of free speech predicts psychosis onset in high-risk youths. Npj Schizophrenia. 1 15030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bögels S, Magyari L, Levinson SC, 2015. Neural signatures of response planning occur midway through an incoming question in conversation. Scientific Reports 5 12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casillas M, Bobb S, Clark E, 2015. Turn-taking, timing, and planning in early language acquisition. J. Child Lang. 43 1310–1337. [DOI] [PubMed] [Google Scholar]
- Cohen AS, Mitchell KR, Docherty NM, Horan WP, 2016. Vocal expression in schizophrenia: Less than meets the ear. Journal of Abnormal Psychology 125 (2) 299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colle L, Angeleri R, Vallana M, Sacco K, Bara BG, Bosco FM, 2013. Understanding the communicative impairments in schizophrenia: A preliminary study. Journal of Communication Disorders 46 (3) 294–308. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Benjamin LS, Spitzer R, 2015. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). VA: American Psychiatric Association, Arlington. [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, et al. , 2003. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: Predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin 29 (4) 703–715. [DOI] [PubMed] [Google Scholar]
- Pelletier-Baldelli A, Strauss GP, Visser KH, Mittal VA, 2017. Initial development and preliminary psychometric properties of the Prodromal Inventory of Negative Symptoms (PINS). Schizophrenia Research 189 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]


