KBP-7072 is a novel aminomethylcycline antibiotic in clinical development for community-acquired pneumonia. The goal of present studies was to determine which pharmacokinetic/pharmacodynamic (PK/PD) parameter magnitude correlated with efficacy in the murine pneumonia infection model against Staphylococcus aureus and Streptococcus pneumoniae.
KEYWORDS: KBP-7072, Staphylococcus aureus, Streptococcus pneumoniae, pharmacodynamics
ABSTRACT
KBP-7072 is a novel aminomethylcycline antibiotic in clinical development for community-acquired pneumonia. The goal of present studies was to determine which pharmacokinetic/pharmacodynamic (PK/PD) parameter magnitude correlated with efficacy in the murine pneumonia infection model against Staphylococcus aureus and Streptococcus pneumoniae. KBP-7072 pharmacokinetic measurements were performed in plasma and epithelial lining fluid (ELF) at 4-fold-increasing doses from 1 to 256 mg/kg of body weight subcutaneously. Pharmacokinetic parameters were calculated using a noncompartmental model and were linear over the dose range. Penetration into ELF ranged from 82% to 238% comparing ELF drug concentrations to plasma free drug concentrations. Twenty-four-hour dose-ranging efficacy studies were then performed in the neutropenic murine pneumonia model against 5 S. aureus (3 methicillin-resistant and 2 methicillin-susceptible) and 6 S. pneumoniae (2 Tetr and 2 Penr) strains. KBP-7072 demonstrated potent in vivo activity resulting in a 3- to 5-log10 kill in CFU burden compared to the start of therapy for all strains. The PK/PD index area under the concentration-time curve (AUC)/MIC corelated well with efficacy (R2, 0.80 to 0.89). Net stasis was achieved at plasma 24-h free drug AUC/MIC values of 1.13 and 1.41 (24-h ELF AUC/MIC values of 2.01 and 2.50) for S. aureus and S. pneumoniae, respectively. A 1-log10 kill was achieved at 24-h plasma AUC/MIC values of 2.59 and 5.67 (24-h ELF AUC/MIC values of 4.22 and 10.08) for S. aureus and S. pneumoniae, respectively. A 2-log10 kill was achieved at 24-h plasma AUC/MIC values of 7.16 and 31.14 (24-h ELF AUC/MIC values of 8.37 and 42.92) for S. aureus and S. pneumoniae, respectively. The results of these experiments will aid in the rational design of dose-finding studies for KBP-7072 in patients with community-acquired bacterial pneumonia (CAP).
INTRODUCTION
KBP-7072 is a novel aminomethylcycline exhibiting broad-spectrum activity, including methicillin-resistant Staphylococcus aureus (MRSA), penicillin-resistant Streptococcus pneumoniae (PRSP), and vancomycin-resistant enterococci (VRE) (1). KBP-7072 is available in both oral and injectable formulations. Two ascending-dose pharmacokinetic (PK) studies, single dose and multiple dose, have demonstrated dose-proportional increases in drug exposure and relatively prolonged half-life (25 to 46 h), and KBP-7072 was safe and generally well tolerated at the highest dose tested (300 mg once a day [QD] and 200 mg twice daily) (2, 3). KBP-7072 has been granted qualified infectious disease product (QIDP) and fast-track designations based on treatment of community-acquired bacterial pneumonia (CAP).
The goal of our experiments was to characterize the in vivo pharmacokinetic/pharmacodynamic (PK/PD) properties of KBP-7072. Specifically, we sought to determine (i) the serum and epithelial lining fluid (ELF) pharmacokinetics of KBP-7072 in the murine model and (ii) the magnitude of the PK/PD parameter area under the concentration-time curve (AUC)/MIC required for efficacy against multiple S. aureus and S. pneumoniae strains in the murine neutropenic pneumonia model.
RESULTS
In vitro susceptibility studies and in vivo fitness.
The MICs of KBP-7072 and fitness in the animal model for the selected 5 S. aureus and 6 S. pneumoniae strains are listed in Table 1. KBP-7072 showed potent activity against both S. aureus and S. pneumoniae regardless of resistance to methicillin, penicillin, tetracycline, and minocycline. The organisms also exhibited similar in vivo fitnesses as measured by growth in untreated control animals. At the start of therapy, animals infected with S. aureus had 106.1±0.4 log10 CFU/lungs, and the burden increased to 108.0±0.2 log10 CFU/lungs over 24 h. Similarly, at the start of therapy, animals infected with S. pneumoniae had 106.5±0.4 log10 CFU/lungs and the burden increased to 108.6±0.3 log10 CFU/lungs over 24 h (Table 1).
TABLE 1.
Study organisms, KBP-7072 susceptibility results, and in vivo fitness
| Species | Strain | MIC (mg/liter) |
Control growth (log10 CFU/lung) | Comment | |
|---|---|---|---|---|---|
| KBP-7072 | Minocycline | ||||
| S. aureus | ATCC 33591 | 0.25 | 8 | 2.05 | MRSA |
| ATCC 25923 | 0.25 | 0.125 | 1.80 | MSSA | |
| ATCC 29213 | 0.25 | 0.06 | 1.62 | MSSA | |
| MW2 | 0.25 | 2 | 1.60 | MRSA | |
| R2527 | 0.25 | 2 | 2.55 | MRSA | |
| S. pneumoniae | ATCC 10813 | 0.016 | 0.03 | 2.73 | Wild type |
| 1293 | 0.016 | 2 | 2.35 | Penr Tetr | |
| 1199 | 0.016 | 4 | 1.81 | Tetr | |
| 140 | 0.016 | 0.016 | 1.97 | Pens | |
| 673 | 0.008 | 0.004 | 1.62 | Penr | |
| 1285 | 0.016 | 0.03 | 2.01 | Peni | |
Pharmacokinetics.
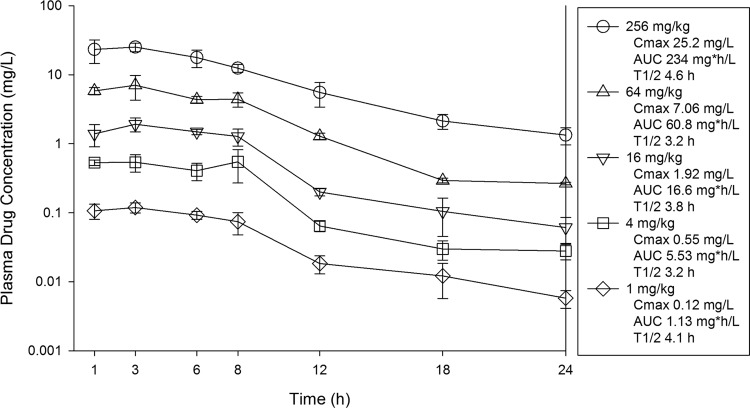
The time course of plasma concentrations of KBP-7072 in mice after subcutaneous doses of 1, 4, 16, 64, and 256 mg/kg are shown in Fig. 1. Peak levels ranged from 0.12 to 25.2 mg/liter, AUC from 0 h to infinity (AUC0–∞) values ranged from 1.13 to 234 mg · h/liter, and the elimination half-life (t1/2) ranged from 3.2 to 4.6 h. Over the dose range, the pharmacokinetics were relatively linear (AUC R2 = 0.999; maximum concentration of drug in serum [Cmax] R2 = 0.999).
FIG 1.
Plasma concentrations of KBP-7072 in mice following single subcutaneous doses. Samples were obtained at seven time points over 24 h. Each symbol represents the mean ± SD for three animals. Shown in the key are the maximum plasma concentration (Cmax), the area under the concentration-time curve from 0 h to infinity (AUC), and the elimination half-life (t1/2) for each dose.
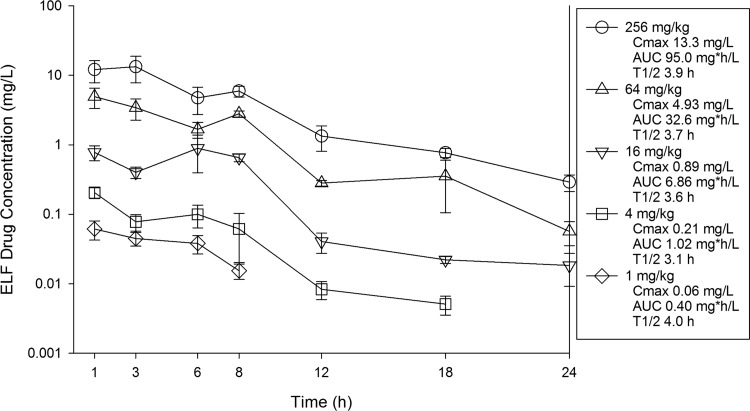
ELF concentrations were determined by urea correction methodology (4) and are presented in Fig. 2. Peak levels ranged from 0.06 to 13.3 mg/liter. AUC0–∞ values ranged from 0.40 to 95.0 mg · h/liter. The elimination half-life ranged from 3.1 to 4.0 h. Over the dose range, ELF pharmacokinetics were also relatively linear (AUC R2 = 0.99; Cmax R2 = 0.98). The penetration of KBP-7072 into ELF relative to free plasma drug concentrations was evaluated for each dose. Over the dose range, the percent penetrations based on AUC exposure were 159% at 1 mg/kg, 82% at 4 mg/kg, 183% at 16 mg/kg, 238% at 64 mg/kg, and 181% at 256 mg/kg.
FIG 2.
ELF concentrations of KBP-7072 in mice following single subcutaneous doses. Samples were obtained at seven time points over 24 h. ELF concentrations were determined using urea concentration correction methods. Each symbol represents the mean ± SD for three animals. Shown in the key are the maximum ELF concentration (Cmax), the area under the concentration-time curve from 0 h to infinity (AUC), and the elimination half-life (t1/2) for each dose.
Relationship between PK/PD parameter AUC/MIC and efficacy.
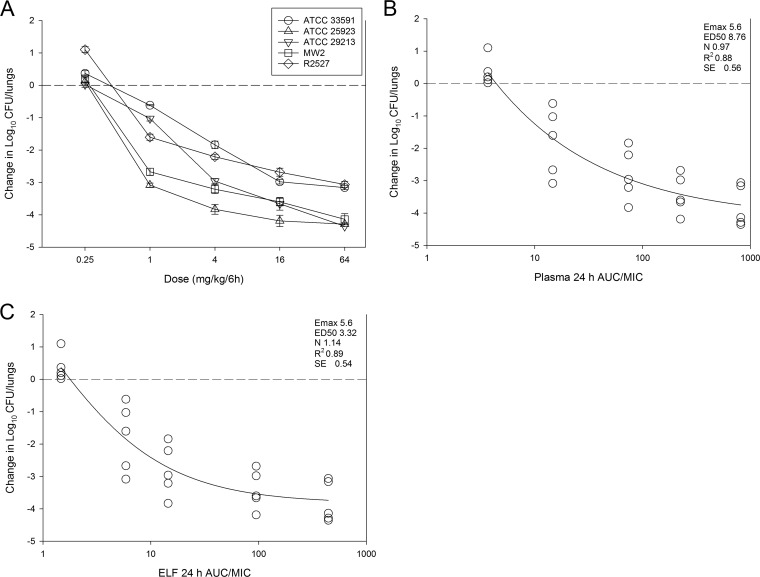
The in vivo dose-response curves for five S. aureus strains are shown in Fig. 3A. KBP-7072 exhibited dose-dependent potent activity against selected methicillin-susceptible (MSSA) and methicillin-resistant (MRSA) S. aureus strains over the dose range studied (0.25 to 64 mg/kg/6 h). Bactericidal activity was noted at ≥1 mg/kg/6 h for all five strains, a 3-log10 kill was achieved for all strains, and a maximal kill of 4-log10 was noted in 3 of 5 strains. The relationship between the log10 CFU in lungs and the 24-h plasma AUC/MIC ratio is illustrated in Fig. 3B. The relationship between 24-h plasma AUC/MIC and treatment effect was strong, with an R2 of 0.88 (standard error of the estimate, 0.56). Also shown in the figure are the maximum effect (Emax), the 50% maximal effect point (ED50), and the slope (N) of the best-fit line based on the sigmoid (Hill) Emax model. Results for the same PK/PD analysis for ELF exposures are shown in Fig. 3C.
FIG 3.
In vivo dose effect of KBP-7072 against 5 selected S. aureus strains using a neutropenic murine pneumonia infection model. Each symbol represents the mean and SD for lungs in three mice. Five total drug dose levels were fractionated into an every-6-h regimen. The burden of organisms was measured at the start and end of therapy. The study period was 24 h. The horizontal dashed line at 0 represents the burden of organisms in the lungs of mice at the start of therapy. Data points below the line represent bactericidal activity, and points above the line represent net growth. (A) Dose-response curves; (B) plasma 24-h total drug AUC/MIC in relation to treatment outcome; (C) ELF 24-h AUC/MIC in relation to treatment outcome. The curved line is the best-fit line based on the Hill equation. Also shown are the PD parameters maximal effect (Emax), 50% maximal effect (ED50), slope of the curve (N), coefficient of determination (R2), and SE of the estimate.
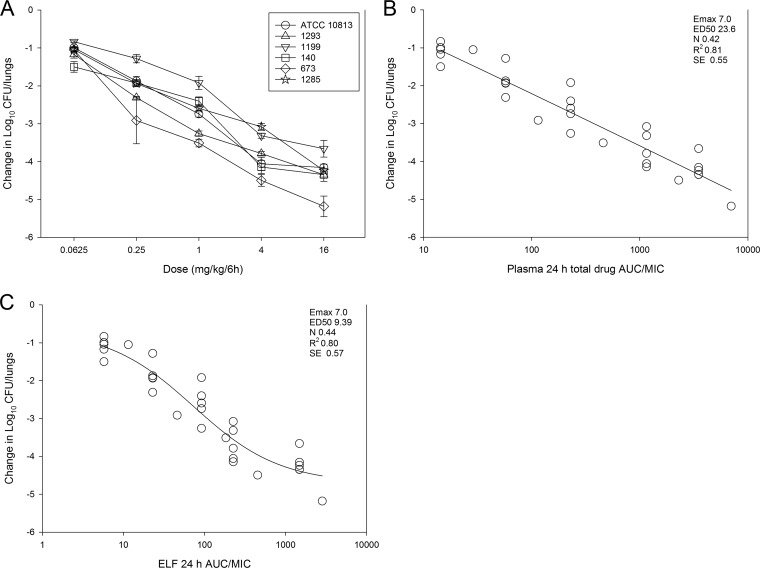
The in vivo dose-response curves for six S. pneumoniae strains are shown in Fig. 4A. Once again, KBP-7072 displayed potent activity, with even greater microbiological activity noted against S. pneumoniae than against S. aureus in the lung model at each dose. Indeed, a net reduction in organism burden (compared to the start of therapy) was demonstrated across all the doses studied (0.0625 to 16 mg/kg/6 h). There was a ≥3-log10 kill achieved against all strains; a maximal kill of 4 log10 was achieved against 5 of 6 strains. The relationship between the log10 CFU in lungs and the 24-h plasma and ELF AUC/MIC ratio is illustrated in Fig. 4B and C. The relationship between 24-h AUC/MIC and treatment effect was similarly compelling, with an R2 of 0.81 (standard error of the estimate, 0.55) for 24-h plasma AUC/MIC ratio and an R2 of 0.80 (standard error of the estimate, 0.57) for the 24-h ELF AUC/MIC ratio. Also shown in the figure are the Emax, ED50, and the N of the best-fit line based on the sigmoid (Hill) Emax model.
FIG 4.
In vivo dose effect of KBP-7072 against 6 selected S. pneumoniae strains using a neutropenic murine pneumonia infection model. Each symbol represents the mean and SD for lungs in three mice. Five total drug dose levels were fractionated into an every-6-h regimen. The burden of organisms was measured at the start and end of therapy. The study period was 24 h. Negative numbers on the y axis represent net killing activity, which was observed for all strains at all dosed studied. (A) Dose-response curves; (B) plasma 24-h total drug AUC/MIC in relation to treatment outcome, (C) ELF 24 h AUC/MIC in relation to treatment outcome. The curved line is the best-fit line based on the Hill equation. Also shown are the PD parameters Emax, ED50, N, R2, and SE.
Pharmacodynamic target AUC/MIC associated with stasis and kill endpoints.
The doses necessary to produce a net bacteriostatic effect, a 1-log10 kill, and 2-log10 kill are shown in Table 2 for both S. aureus and S. pneumoniae. The corresponding 24-h AUC/MIC values for these doses are also presented utilizing both plasma and ELF pharmacokinetic data. For S. aureus, the doses needed for static, 1-log10 kill, and 2-log10 kill endpoints were 1.37 mg/kg/24 h, 3.03 mg/kg/24 h, and 7.52 mg/kg/24 h, respectively. The corresponding free drug plasma 24-h AUC/MIC values were 1.13, 2.59, and 7.16. The corresponding ELF 24-h AUC/MIC values were 2.01, 4.22, and 8.37. Doses required to achieve the same endpoints for S. pneumoniae were much lower than for S. aureus; however, one would expect this based on the significantly lower KBP-128 7072 MIC for this group. For S. pneumoniae, the doses needed for static, 1-log10 kill, and 2-log10 kill endpoints were 0.09 mg/kg/24 h, 0.39 mg/kg/24 h, and 2.04 mg/kg/24 h, respectively. The corresponding free plasma 24 h AUC/MIC values were 1.41, 5.67, and 31.14. The corresponding ELF 24-h AUC/MIC values were 2.50, 10.08, and 42.92.
TABLE 2.
Pharmacodynamic targets associated with net stasis, 1-log kill, and 2-log kill in the neutropenic murine pneumonia infection model for S. aureus and S. pneumoniaea
| Species | Strain | Stasis |
1-log kill |
2-log kill |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 24-h dose (mg/kg) | 24-h plasma tAUC/MIC | 24-h plasma fAUC/MIC | 24-h ELF AUC/MIC | 24-h dose (mg/kg) | 24-h plasma tAUC/MIC | 24-h plasma fAUC/MIC | 24-h ELF AUC/MIC | 24-h dose (mg/kg) | 24-h plasma tAUC/MIC | 24-h plasma fAUC/MIC | 24-h ELF AUC/MIC | ||
| S. aureus | ATCC 33591 | 1.78 | 6.54 | 1.47 | 2.62 | 5.54 | 22.21 | 5.00 | 6.97 | 18.17 | 80.25 | 18.06 | 17.91 |
| ATCC 25923 | 1.05 | 3.84 | 0.86 | 1.54 | 1.59 | 5.84 | 1.31 | 2.34 | 2.38 | 8.74 | 1.97 | 3.49 | |
| ATCC 29213 | 1.17 | 4.31 | 0.97 | 1.72 | 3.22 | 11.81 | 2.66 | 4.72 | 7.86 | 33.61 | 7.56 | 8.64 | |
| MW2 | 1.09 | 3.99 | 0.90 | 1.60 | 1.79 | 6.56 | 1.48 | 2.63 | 2.91 | 10.67 | 2.40 | 4.27 | |
| R2527 | 1.77 | 6.49 | 1.46 | 2.60 | 3.01 | 11.04 | 2.48 | 4.41 | 6.28 | 25.84 | 5.81 | 7.51 | |
| Mean | 1.37 | 5.04 | 1.13 | 2.01 | 3.03 | 11.49 | 2.59 | 4.22 | 7.52 | 31.82 | 7.16 | 8.37 | |
| Median | 1.17 | 4.31 | 0.97 | 1.72 | 3.01 | 11.04 | 2.48 | 4.41 | 6.28 | 25.84 | 5.81 | 7.51 | |
| SD | 0.37 | 1.36 | 0.31 | 0.55 | 1.58 | 6.54 | 1.47 | 1.87 | 6.38 | 29.00 | 6.53 | 5.75 | |
| S. pneumoniae | ATCC 10813 | 0.11 | 6.28 | 1.41 | 2.51 | 0.30 | 16.96 | 3.82 | 6.78 | 0.81 | 46.50 | 10.46 | 18.60 |
| 1293 | 0.06 | 3.54 | 0.80 | 1.42 | 0.21 | 12.31 | 2.77 | 4.92 | 0.70 | 40.05 | 9.01 | 16.02 | |
| 1199 | 0.19 | 11.09 | 2.50 | 4.44 | 1.04 | 59.87 | 13.47 | 23.95 | 7.84 | 523.67 | 117.83 | 134.83 | |
| 140 | 0.04 | 2.46 | 0.55 | 0.98 | 0.18 | 10.46 | 2.35 | 4.18 | 0.73 | 42.08 | 9.47 | 16.83 | |
| 673 | 0.09 | 10.50 | 2.36 | 4.20 | 0.31 | 35.85 | 8.07 | 14.34 | 0.95 | 108.45 | 24.40 | 43.38 | |
| 1285 | 0.06 | 3.65 | 0.82 | 1.46 | 0.27 | 15.73 | 3.54 | 6.29 | 1.21 | 69.62 | 15.67 | 27.85 | |
| Mean | 0.09 | 6.25 | 1.41 | 2.50 | 0.39 | 25.20 | 5.67 | 10.08 | 2.04 | 138.40 | 31.14 | 42.92 | |
| Median | 0.08 | 4.97 | 1.12 | 1.99 | 0.28 | 16.34 | 3.68 | 6.54 | 0.88 | 58.06 | 13.06 | 23.22 | |
| SD | 0.05 | 3.74 | 0.84 | 1.50 | 0.33 | 19.27 | 4.34 | 7.71 | 2.85 | 190.50 | 42.86 | 46.20 | |
tAUC, total drug AUC; fAUC, free drug AUC; ELF, epithelial lining fluid. Means, medians, and SDs are in bold.
DISCUSSION
Tetracycline antibiotics have been in clinical use for almost seven decades and are generally regarded to be safe and effective medicines (5). However, the increasing incidence of bacterial resistance has relegated older tetracyclines to a limited role for treating common infectious diseases (5, 6). Advances in synthetic chemistry have yielded the promising development of new generations of tetracycline with activity against drug-resistant organisms, such as tigecycline (7), eravacycline (8), omadacycline (9), and KBP-7072, which is the focus of present study.
KBP-7072 is a novel aminomethylcycline exhibiting broad-spectrum activity against multidrug-resistant bacteria and is under development for the treatment of community-acquired bacterial pneumonia. PK/PD evaluation in animal infection models plays an essential role in preclinical assessments of new antibiotics. This includes examining drug exposure related to microbiological effect to elucidate the optimal dosing regimen design for clinical trials and setting susceptibility breakpoints (10–12). We present here the pharmacodynamic characteristics of KBP-7072 in a preclinical animal model of S. aureus and S. pneumoniae pneumonia. KBP-7072 demonstrated in vitro and in vivo potency against a diverse group of S. aureus and S. pneumoniae strains, including those resistant to other antibiotics such as methicillin, penicillin, and earlier generations of the tetracycline class. We observed extensive bacterial killing, with a ≥4-log10 kill in three of five S. aureus strains tested and five of six S. pneumoniae strains tested, and the shapes of the exposure-response curves were very steep, with small increases in drug exposure resulting in large increases in cidal activity. We also examined the drug exposures associated with efficacy in terms of plasma pharmacokinetic and ELF pharmacokinetic exposures. It is plausible that the potent activity we observed in the murine pneumonia model is partly explained by high penetration ratios (82% to 238%) of KBP-7072 into ELF.
Previous studies have demonstrated that AUC/MIC is the PK/PD index linked to in vivo activity of tetracycline class (4, 13–16). We therefore used this parameter in the present study for PK/PD target analysis. While this is the first PK/PD study in an animal model for KBP-7072, similar animal model PK/PD target studies have been performed for doxycycline (17), tigecycline (18–20), eravacycline (16), and omadacycline (4) against a variety of pathogens, such as S. aureus, S. pneumoniae, Escherichia coli, and Klebsiella pneumoniae.
For comparison, a study examining the PK/PD relationships of tigecycline in an S. aureus murine pneumonia model found that an AUC for the free, unbound fraction (fAUC)/MIC target of 1.88 was associated with net stasis (19), which is quite comparable to that found in this study with KBP-7072. A more recent evaluation of another aminomethylcycline, omadacycline, in the murine pneumonia model demonstrated a stasis total drug AUC/MIC target of about 8 against S. pneumoniae (4), similar to that found in this study. Importantly, in the case of tigecycline, clinical PK/PD analysis in patients with skin and skin structure infection, complicated intra-abdominal infections, and community-acquired pneumonia have confirmed the relevance of the PK/PD targets identified in preclinical models on treatment outcome (15, 21, 22). A limitation of the current study was the relatively narrow MIC range for strains utilized. Further studies with a wider range of MICs as well as against other drug-resistant pathogens, including Gram-negative organisms, is warranted.
In conclusion, KBP-7072 exhibited potent in vitro and in vivo efficacy against S. aureus and S. pneumoniae, including strains resistant to methicillin, penicillin, and tetracyclines. Both net stasis and bactericidal endpoints were achieved in a clinically relevant animal infection model. The PD targets identified in this study will be useful in guiding appropriate dosing regimen design for future clinical studies in the context of human pharmacokinetic exposures and MIC distribution and in the development of susceptibility breakpoints.
MATERIALS AND METHODS
Organisms, media, and antibiotic.
Five S. aureus and six S. pneumoniae strains were used in the studies and are listed in Table 1. Strains were chosen that varied in phenotypic resistance patterns to a number of relevant antimicrobials, including penicillin, methicillin, and minocycline. All organisms were grown, subcultured, and quantified using Mueller-Hinton agar for S. aureus and sheep blood agar for S. pneumoniae (Remel, Milwaukee, WI). The drug compounds used for in vitro and in vivo studies were supplied by KBP Biosciences USA Inc.
In vitro susceptibility studies.
The MICs of KBP-7072 and comparator agents against each strain were determined using Clinical and Laboratory Standards Institute microdilution methods (23). All MIC assays were performed in duplicate on three separate occasions. The median MIC of replicate assays is reported and was utilized in PK/PD analysis.
Murine model.
Animals were maintained in accordance with the Association for Assessment and Accreditation of Laboratory Animal Care International (24). All animal studies were approved by the Animal Research Committees of the William S. Middleton Memorial VA Hospital and the University of Wisconsin. Six-week-old, specific-pathogen-free, female ICR/Swiss mice weighing 24 to 27 g were used for all studies (Harlan Sprague-Dawley, Indianapolis, IN). Mice were rendered neutropenic (neutrophils < 100/mm3) by injecting cyclophosphamide (Mead Johnson Pharmaceuticals, Evansville, IN) subcutaneously 4 days (150 mg/kg) and 1 day (100 mg/kg) before lung infection. S. aureus and S. pneumoniae strains were grown overnight on Mueller-Hinton agar and sheep blood agar, respectively. A sterile loop was then used to transfer organism to sterile saline and absorbance was adjusted to 0.3 at 580 nm using a Spectronic 88 spectrophotometer (Bausch and Lomb, Rochester, NY). After a 1:10 dilution, bacterial counts of the inoculum ranged from 107.9 to 108.9 CFU/ml. Lung infections with each of the strains were produced by the administration of 50 μl of inoculum into the nares of isoflurane-anesthetized mice. Mice were then held upright to allow for aspiration into the lungs. Therapy with KBP-7072 was initiated 2 h after induction of infection. Mice were sacrificed at 24 h after dosing. No treatment controls at the start and end of study period were included in all experiments. Organism burden was quantified by CFU counts from dilutions of whole-organ homogenates.
Drug pharmacokinetics.
Single-dose plasma pharmacokinetics of KBP-7072 were determined for mice. Dose levels of 1, 4, 16, 64, and 256 mg/kg were administered subcutaneously. Groups of three mice were sampled for drug concentration determination at 1, 3, 6, 8, 12, 18, and 24 h. Both plasma and bronchoalveolar lavage (BAL) fluid were obtained for pharmacokinetic analysis. Plasma was obtained from each animal by centrifugation of anticoagulated blood obtained by cardiac puncture. BAL fluid was obtained by instillation of 1 ml of sterile saline into the lungs of each animal, followed by immediate removal. The BAL fluid was centrifuged to remove blood and cellular debris, and the supernatant was collected. Plasma and BAL supernatant was stored at −80°C. All drug concentrations were determined by liquid chromatography-tandem mass spectrometry methods by the sponsor. ELF concentrations were calculated from BAL fluid concentrations by urea correction methodology according to the following formula (4): [drug]ELF = [drug]BAL × ([urea]plasma/[urea]BAL). Pharmacokinetic parameters (mean ± the standard deviation), including the elimination half-life (t1/2), AUC0–∞, and Cmax, were calculated using a noncompartmental model with mean concentration values from each group of mice. The half-life was determined by linear least-squares regression. The AUC was calculated from the mean concentrations using the trapezoidal rule. Pharmacokinetic estimates for dose levels that were not directly measured were calculated using linear interpolation for dose levels between those with measured kinetics and linear extrapolation for dose levels above or below the highest and lowest dose levels with kinetic measurements. Protein binding of KBP-7072 in murine plasma is 77.5% as provided by sponsor (KBP Biosciences USA Inc.) and was used to calculate free drug concentrations for analysis. The penetration ratio of KBP-7072 was calculated according to the following formula: penetration ratio = [drug]ELF/{[drug]plasma × (1 − murine protein binding)}. Protein binding was not applied to ELF drug concentrations.
Relationship between PK/PD parameter AUC/MIC and efficacy.
AUC/MIC was chosen as the pharmacodynamic parameter for KBP-7072 based on previous studies demonstrating this PK/PD index to be predictive of treatment efficacy for the tetracycline class (4, 13, 16, 25). In vivo treatment studies were performed in the murine pneumonia model for each strain. Groups of three mice per dosing regimen and control group were utilized. Dose-response studies consisted of 4-fold-increasing doses (ranges, 0.25 to 64 mg/kg/6 h for S. aureus and 0.0625 to 16 mg/kg/6 h for S. pneumoniae) administered subcutaneously. The dose-response effect was determined as described above by measurement of CFU in lung homogenates. The correlation between efficacy and the PK/PD parameter AUC/MIC was determined by nonlinear least-squares multivariate regression (SigmaPlot version 13; Systat Software, San Jose, CA). The mathematical model used was derived from the Hill equation, E = (Emax × DN)/(ED50N – DN), where E is the effector, in this case, the log change in CFU per lung between treated mice and untreated controls after the 24-h period of study, Emax is the maximum effect, D is the 24-h total AUC/MIC, ED50 is the AUC/MIC required to achieve 50% of the Emax, and N is the slope of the dose-effect curve. The values for the indices Emax, ED50, and N were calculated using nonlinear least-squares regression. The coefficient of determination (R2) was used to estimate the variance that might be due to regression with the PK/PD parameter AUC/MIC.
AUC/MIC magnitude associated with stasis and kill endpoints.
Using the sigmoid Emax model described above, the dose required to produce net static effect (static dose) and the 1- and 2-log10 kills compared to the start of therapy were calculated for each drug-organism combination. The plasma and ELF pharmacokinetic results were then used to estimate the AUC/MIC exposure associated with each of the endpoints for each organism. The associated 24-h total and free plasma drug AUC/MIC targets and ELF AUC/MIC targets (mean, median, and standard deviation) were calculated for each species group.
ACKNOWLEDGMENT
This study was funded by KBP Biosciences Co., Ltd.
REFERENCES
- 1.Wang Y, Q L, Zhang B. 2016. Antibacterial activity of KBP-7072 against clinical isolates of drug-resistant bacteria, abstr Monday-565 ASM Microbe. American Society for Microbiology, Washington, DC. [Google Scholar]
- 2.Zhang B, Wang Y, Chen Y, Yang F. 2016. Single ascending dose safety, tolerability, and pharmacokinetics of KBP-7072, a novel third generation tetracycline. Open Forum Infect Dis 3:S515. doi: 10.1093/ofid/ofw172.1544. [DOI] [Google Scholar]
- 3.Yang F, Yanli W, Wang P, Hong M, Benn V. 2017. Multiple ascending dose safety, tolerability, and pharmacokinetics of KBP-7072, a novel third generation tetracycline. Open Forum Infect Dis 4:S291. doi: 10.1093/ofid/ofx163.662. [DOI] [Google Scholar]
- 4.Lepak AJ, Zhao M, Marchillo K, VanHecker J, Andes DR. 2017. In vivo pharmacodynamic evaluation of omadacycline (PTK 0796) against Streptococcus pneumoniae in the murine pneumonia model. Antimicrob Agents Chemother 61:e02368-16. doi: 10.1128/AAC.02368-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen F, Starosta AL, Arenz S, Sohmen D, Donhofer A, Wilson DN. 2014. Tetracycline antibiotics and resistance mechanisms. Biol Chem 395:559–575. doi: 10.1515/hsz-2013-0292. [DOI] [PubMed] [Google Scholar]
- 6.Grossman TH. 2016. Tetracycline antibiotics and resistance. Cold Spring Harb Perspect Med 6:a025387. doi: 10.1101/cshperspect.a025387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen F, Han Q, Xie D, Fang M, Zeng H, Deng Y. 2015. Efficacy and safety of tigecycline for the treatment of severe infectious diseases: an updated meta-analysis of RCTs. Int J Infect Dis 39:25–33. doi: 10.1016/j.ijid.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Zhanel GG, Cheung D, Adam H, Zelenitsky S, Golden A, Schweizer F, Gorityala B, Lagace-Wiens PR, Walkty A, Gin AS, Hoban DJ, Karlowsky JA. 2016. Review of eravacycline, a novel fluorocycline antibacterial agent. Drugs 76:567–588. doi: 10.1007/s40265-016-0545-8. [DOI] [PubMed] [Google Scholar]
- 9.Villano S, Steenbergen J, Loh E. 2016. Omadacycline: development of a novel aminomethylcycline antibiotic for treating drug-resistant bacterial infections. Future Microbiol 11:1421–1434. doi: 10.2217/fmb-2016-0100. [DOI] [PubMed] [Google Scholar]
- 10.Andes DR, Lepak AJ. 2017. In vivo infection models in the pre-clinical pharmacokinetic/pharmacodynamic evaluation of antimicrobial agents. Curr Opin Pharmacol 36:94–99. doi: 10.1016/j.coph.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 11.Zhao M, Lepak AJ, Andes DR. 2016. Animal models in the pharmacokinetic/pharmacodynamic evaluation of antimicrobial agents. Bioorg Med Chem 24:6390–6400. doi: 10.1016/j.bmc.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Craig WA. 1998. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 26:1–10; quiz, 11–12. doi: 10.1086/516284. [DOI] [PubMed] [Google Scholar]
- 13.van Ogtrop ML, Andes D, Stamstad TJ, Conklin B, Weiss WJ, Craig WA, Vesga O. 2000. In vivo pharmacodynamic activities of two glycylcyclines (GAR-936 and WAY 152,288) against various gram-positive and gram-negative bacteria. Antimicrob Agents Chemother 44:943–949. doi: 10.1128/AAC.44.4.943-949.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meagher AK, Ambrose PG, Grasela TH, Ellis-Grosse EJ. 2005. The pharmacokinetic and pharmacodynamic profile of tigecycline. Clin Infect Dis 41:S333–S340. doi: 10.1086/431674. [DOI] [PubMed] [Google Scholar]
- 15.Passarell JA, Meagher AK, Liolios K, Cirincione BB, Van Wart SA, Babinchak T, Ellis-Grosse EJ, Ambrose PG. 2008. Exposure-response analyses of tigecycline efficacy in patients with complicated intra-abdominal infections. Antimicrob Agents Chemother 52:204–210. doi: 10.1128/AAC.00813-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao M, Lepak AJ, Marchillo K, VanHecker J, Andes DR. 2017. In vivo pharmacodynamic target assessment of eravacycline against Escherichia coli in a murine thigh infection model. Antimicrob Agents Chemother 61:e00250-17. doi: 10.1128/AAC.00250-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christianson J, Andes D, Craig W. 2001. Magnitude of the 24-h AUC/MIC required for efficacy of doxycycline (doxy) against Streptococcus pneumoniae (SP) in a murine thigh-infection model, abstr 475. 39th Infect Dis Soc Am Annu Meet. Infectious Diseases Society of America, San Francisco, CA. [Google Scholar]
- 18.Crandon JL, Banevicius MA, Nicolau DP. 2009. Pharmacodynamics of tigecycline against phenotypically diverse Staphylococcus aureus isolates in a murine thigh model. Antimicrob Agents Chemother 53:1165–1169. doi: 10.1128/AAC.00647-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koomanachai P, Crandon JL, Banevicius MA, Peng L, Nicolau DP. 2009. Pharmacodynamic profile of tigecycline against methicillin-resistant Staphylococcus aureus in an experimental pneumonia model. Antimicrob Agents Chemother 53:5060–5063. doi: 10.1128/AAC.00985-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicasio AM, Crandon JL, Nicolau DP. 2009. In vivo pharmacodynamic profile of tigecycline against phenotypically diverse Escherichia coli and Klebsiella pneumoniae isolates. Antimicrob Agents Chemother 53:2756–2761. doi: 10.1128/AAC.01678-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meagher AK, Passarell JA, Cirincione BB, Van Wart SA, Liolios K, Babinchak T, Ellis-Grosse EJ, Ambrose PG. 2007. Exposure-response analyses of tigecycline efficacy in patients with complicated skin and skin-structure infections. Antimicrob Agents Chemother 51:1939–1945. doi: 10.1128/AAC.01084-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubino CM, Bhavnani SM, Forrest A, Dukart G, Dartois N, Cooper A, Korth-Bradley J, Ambrose PG. 2012. Pharmacokinetics-pharmacodynamics of tigecycline in patients with community-acquired pneumonia. Antimicrob Agents Chemother 56:130–136. doi: 10.1128/AAC.00277-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clinical and Laboratory Standards Institute. 2015. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, 10th ed CLSI document M07-A10. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 24.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academies Press, Washington, DC. [Google Scholar]
- 25.Agwuh KN, MacGowan A. 2006. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother 58:256–265. doi: 10.1093/jac/dkl224. [DOI] [PubMed] [Google Scholar]