Abstract
Background
Luteinized thecoma with sclerosing peritonitis (LTSP) is a very rare condition, and its clinical management is not evidence-based. Here we describe a case of long-term disease control achieved with leuprorelin and tamoxifen therapy.
Case presentation
A 18-year-old woman with acute abdomen underwent surgical removal of an ovarian mass and received diagnosis of LTSP. Treatment plan consisted of leuprorelin and tamoxifen, followed by a good instrumental response. After 5 years, leuprorelin was stopped, and the patient continued tamoxifen alone. Ten years after diagnosis, she is still disease free.
Conclusion
Even in the absence of solid evidence, the combination of leuprorelin and tamoxifen could be considered as a possible medical treatment of LTSP. Considering the limitations related to the rarity of disease, further studies are needed to improve its management.
Keywords: Thecoma, Sclerosing, Peritonitis, Hormonal, Therapy, Ovary
Highlights
-
•
Luteinized thecoma with sclerosing peritonitis (LTSP) is a rare condition characterized by a very hard management.
-
•
Few cases are described in literature and no evidences about the best treatment of this condition are available.
-
•
We present a case of a very long control (ten year) of LTSP with tamoxifen and leuprorelin treatment.
-
•
Based on the lack of evidences, this approach could be considered as treatment of LTSP.
1. Introduction
Thecoma is a very uncommon cancer, originated by ovarian theca cells, that represents less of 5% of all ovarian cancers (Chechia et al., 2008). It arises normally in young and midlife women, presenting as a single round mass in the abdomen. An even rarer variant of thecoma is luteinized thecoma with sclerosing peritonitis (LTSP). This entity was originally described in 1994 and represents less than 0.01% of all ovarian cancers (Clement et al., 1994). Sclerosing peritonitis, that is a complication of this kind of cancer, consists of an abnormal proliferation of fibroblasts below the mesothelium, resulting in the growth of a mass of fibrous tissue that incorporates abdominal organs (Iwasa et al., 1996). The consequence is the progressive incarceration of intestinal loops, followed by clinically relevant gut obstruction. Nowadays, the pathogenesis of LTSP is still unknown; an association between this condition and antiepileptic drugs administration was proposed based on clinical observations (Levavi et al., 2009). Currently, there are no clear guidelines about the management of LTSP, and the few available evidences are mostly based on the description of single cases. Surgery is burdened by a high mortality rate; therefore, it is normally reserved to the emergency treatment of intestinal obstruction. Regarding the pharmacological therapy, a single case of objective response to hormonal therapy has been reported in literature: after surgical resection of thecoma, a 39-year-old patient was treated with toremifene and leuprorelin, achieving the complete regression of peritoneal lesions after 3 months of therapy (Bianco et al., 2005). Another case report showed a similar therapeutic result with the combination of corticosteroid and leuprorelin in a 25-year-old patient with LTSP (Schonman et al., 2008). Here we report the very long follow-up (10 years) of an 18-year-old woman affected by LTSP, treated with leuprorelin and tamoxifen.
2. Case presentation
An 18-year-old woman was admitted to the emergency room in February 2008 because of the progressive onset of severe abdominal pain. An exploratory laparotomy was performed, showing appendicitis, and a right ovarian mass. The patient underwent appendicectomy and left salpingo-oophorectomy, and a biopsy of the ovarian mass was performed, without removing the mass. The histological exam showed only cells of ovarian fibroma with hemorrhagic infarction. One month later, due to the occurrence of a partial bowel obstruction, the patient was again referred to the surgeons. Another laparotomy was performed and the ovarian mass in the right ovary was completely removed, as well as a portion of peritoneum. The histological examination showed cells of luteinized thecoma (Fig. 1), associated with follicular cysts and granulosa-cells hyperplasia, and sclerosing peritonitis with foreign-body giant cells (Fig. 2). Expression of estrogen-receptors (Fig. 3) and progesterone-receptors (Fig. 4) was detected by immunohistochemistry on thecoma cells. No assumption of antiepileptic drugs was reported by the patient. The case was initially assessed by gynecologist and hormonal therapy with the aromatase inhibitor letrozole, 2.5 mg/day was suggested. Because of the extreme rarity of the disease, the patient was collectively evaluated by a multidisciplinary team of gynecologists and oncologists, in June 2008. A treatment with leuprorelin 3.75 mg/month and tamoxifen 20 mg/day was started and the hormonal therapy with letrozole was suspended. In the next two months, the patient experienced a relevant clinical improvement, moving to a regular function of bowel and she regularly restarted oral intake of food. A single episode of severe vomiting occurred in May 2008, and the patient underwent a CT scan that showed a thickening of intestinal loops, compatible with sclerosing peritonitis, and a mild amount of peritoneal effusion. However, this episode resolved spontaneously, and the patient continued the hormonal treatment with leuprorelin and tamoxifen. In December 2009, after 18 months of disease stabilization and progressive resorption of peritoneal effusion, as showed in two follow-up CT scans, the patient had a new episode of partial bowel obstruction. At that time, an MRI of abdomen was conducted, showing that the sclerosing peritonitis was substantially unchanged. During next four years, the patient did not develop any other episode of complete or partial bowel obstruction, but a bone densitometry showed a condition of osteoporosis (T-score of femoral neck: −2.1), and a therapy with zoledronic acid (a single intravenous infusion of 5 mg, administered once a year) was initiated. Because of the complete absence of symptoms, no radiological re-assessments were conducted until October 2013, when a new CT scan showed the complete regression of peritoneal lesions. Based on this favorable CT findings, and considering the time elapsed from diagnosis, after multidisciplinary re-assessment, therapy with leuprorelin was stopped, while continuing tamoxifen. In February 2014, after five years, also the treatment with zoledronic acid was suspended. In April 2014, the patient underwent a further CT scan, that confirmed the absence of the relapse of the disease. Nowadays, the patient is continuing her follow-up, and since the last CT scan, she did not show any sign or symptom related to the relapse of the disease. In April 2018, within multidisciplinary re-assessment, considering the time of ten years elapsed from starting of hormonal treatment with leuprorelin and tamoxifen, the decision to stop tamoxifen was taken.
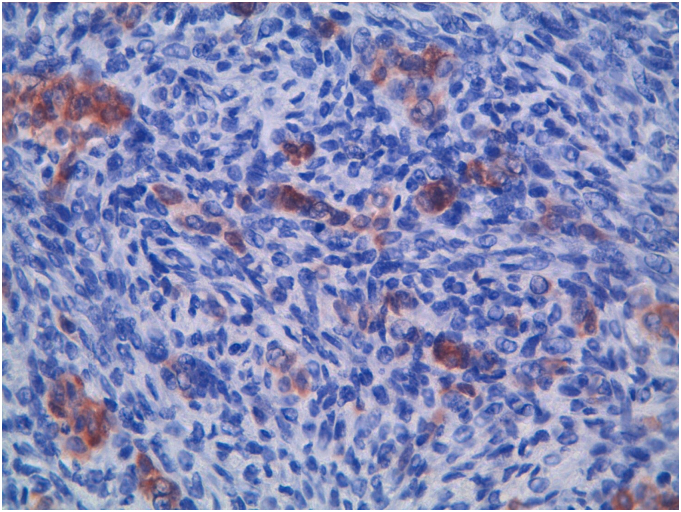
Fig. 1.
Cells of thecoma, immunohistochemistry positive for inhibin (40×).
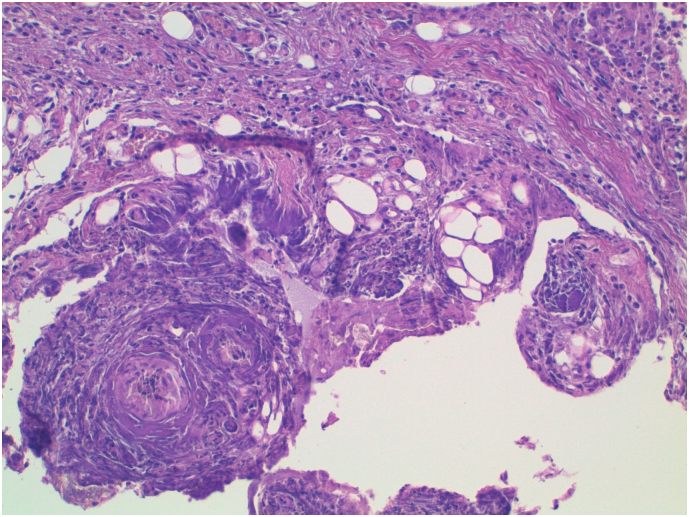
Fig. 2.
Sclerosing peritonitis with granulomas and foreign-body giant cells (20×).
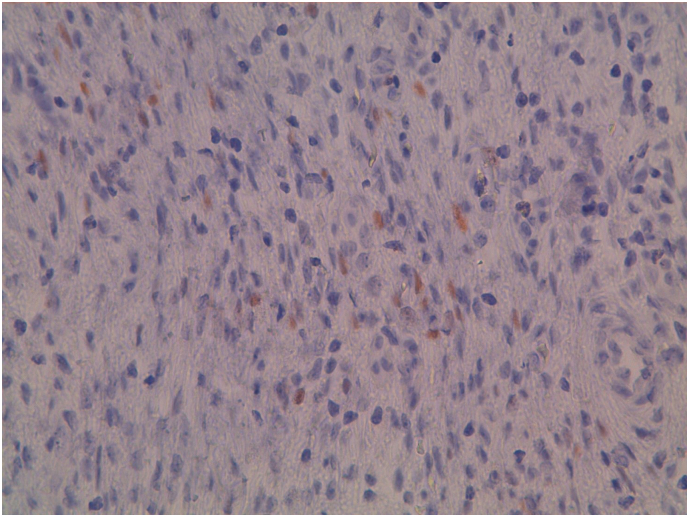
Fig. 3.
Immunohistochemical expression of estrogen-receptors (40×).
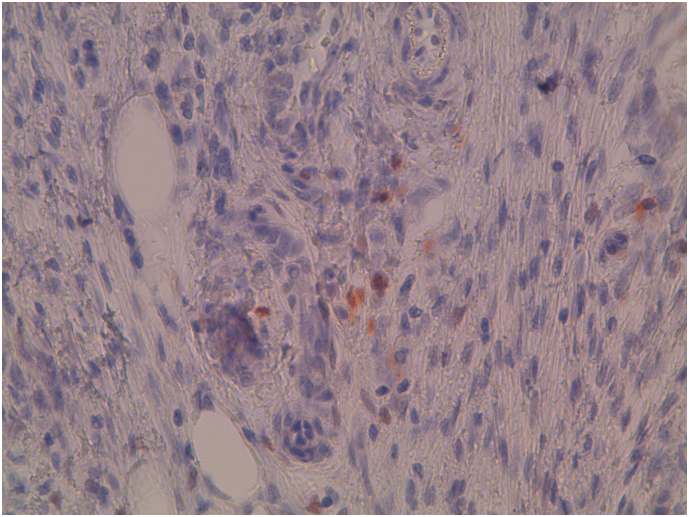
Fig. 4.
Immunohistochemical expression of progesterone-receptors (40×).
3. Discussion
To our knowledge, this case represents the first experience of a long-term disease control in a patient with LTSP treated with leuprorelin for 5 years and tamoxifen for 10 years. LTSP is a very uncommon disease, with a few cases reported in literature and scanty evidence about effective treatments. The first attempts of a systemic treatment for this disease were based on the hypothesis that hormonal stimulation could drive the growth of this neoplasm, even triggering the formation of fibrous tissue in the peritoneum. At the same time, tamoxifen had already shown activity in the treatment of fibrosis associated with peritoneal dialysis, a clinical-radiological condition similar to thecoma-related sclerosing peritonitis (Bajo et al., 2003). In the present case, a hormonal therapeutic approach with an aromatase inhibitor, not justified by the existing evidence, was initially attempted, but shortly interrupted thereafter in favor of a treatment with leuprorelin plus tamoxifen, based on the already mentioned case report that, at the time of diagnosis, represented the only treatment experience that had demonstrated activity (Bianco et al., 2005). However, the management of the disease was not without complications. First of all, the clinical history was characterized, mainly in the first years, by repeated episodes of partial bowel obstruction caused by the develop of abdominal adhesions, which was followed by a progressive impairment of food oral intake and weight loss, as well as therapy discontinuation. Secondly, the effect of bone depletion induced by leuprorelin prevailed over the bone protective effect of tamoxifen, causing osteoporosis that required bisphosphonate therapy. However, hormonal therapy has been successful and the patient now, disease-free ten years after diagnosis, could be considered potentially healed. Nowadays, despite the time elapsed, the evidence about the treatment of this disease is substantially unchanged. In 2008, a review of 27 cases of LTSP was published, in which the immunohistochemical profile of the primary ovarian lesion was evaluated, reporting that a subgroup of patients had tumor cells expressing estrogen (ER) and progesterone (PgR) receptors (Staats et al., 2008). This receptor status would justify the successes obtained with hormonal therapy, but at the same time it suggests that patients benefiting from this approach could represent only a subgroup of the overall group of patients with a diagnosis of thecoma. In the future, patients with thecoma should be investigated for the immunohistochemical positivity of ER and PgR receptors, which could help to select the patients who would most likely benefit from hormonal treatment. However, the rarity of the disease makes hard to adequately describe the interaction between the efficacy of treatments and potential predictive factors. Generally, the rarity of the disease makes unrealistic any attempt to perform randomized clinical trials and produce solid evidence-based treatment guidelines. Therefore, reporting the clinical experience of individual cases or collecting retrospective series represent a potentially useful way to accumulate novel data, that over time could potentially improve the management of this rare disease.
Author contribution
All authors contributed equally to the paper.
Conflict of interest statement
All authors declare to have no conflict of interest.
Contributor Information
L. Muratori, Email: leonardo.muratori@unito.it.
G. Gorzegno, Email: g.gorzegno@sanluigi.piemonte.it.
A. Andreozzi, Email: a.andreozzi@sanluigi.piemonte.it.
M. Di Maio, Email: massimo.dimaio@unito.it.
G.V. Scagliotti, Email: giorgio.scagliotti@unito.it.
References
- Bajo M.A. Advances in Peritoneal Dialysis. Conference on Peritoneal Dialysis. vol. 19. 2003. Clinical experience with tamoxifen in peritoneal fibrosing syndromes. [PubMed] [Google Scholar]
- Bianco R. Ovarian luteinized thecoma with sclerosing peritonitis in an adult woman treated with leuprolide and toremifene in complete remission at 5 years. Gynecol. Oncol. 2005;96(3):846–849. doi: 10.1016/j.ygyno.2004.10.044. [DOI] [PubMed] [Google Scholar]
- Chechia A. Incidence, clinical analysis, and management of ovarian fibromas and fibrothecomas. Am. J. Obstet. Gynecol. 2008;199(5):473–e1. doi: 10.1016/j.ajog.2008.03.053. [DOI] [PubMed] [Google Scholar]
- Clement P.B. Sclerosing peritonitis associated with luteinized Thecomas of the ovary: a clinicopathological analysis of six cases. Am. J. Surg. Pathol. 1994;18(1):1–13. doi: 10.1097/00000478-199401000-00001. [DOI] [PubMed] [Google Scholar]
- Iwasa Y. Sclerosing peritonitis associated with luteinized thecoma of the ovary. Pathol. Int. 1996;46(7):510–514. doi: 10.1111/j.1440-1827.1996.tb03646.x. [DOI] [PubMed] [Google Scholar]
- Levavi H. Sclerosing peritonitis associated with bilateral luteinized thecoma, linked to anticonvulsant therapy. Eur. J. Gynaecol. Oncol. 2009;30(6):695–700. [PubMed] [Google Scholar]
- Schonman R. Luteinized thecoma associated with sclerosing peritonitis—conservative surgical approach followed by corticosteroid and GnRH agonist treatment—a case report. Gynecol. Oncol. 2008;111(3):540–543. doi: 10.1016/j.ygyno.2008.04.014. [DOI] [PubMed] [Google Scholar]
- Staats P.N. Luteinized thecomas (thecomatosis) of the type typically associated with sclerosing peritonitis: a clinical, histopathologic, and immunohistochemical analysis of 27 cases. Am. J. Surg. Pathol. 2008;32(9):1273–1290. doi: 10.1097/PAS.0b013e3181666a5f. [DOI] [PubMed] [Google Scholar]