Abstract
Background and Purpose:
There has been a recent sharp rise in opioid-related deaths in the U.S. Intravenous opioid use can lead to infective endocarditis which can result in stroke. There are scant data on recent trends in this neurological complication of opioid abuse. We hypothesized that increasing opioid abuse has led to a higher incidence of stroke associated with infective endocarditis and opioid use.
Methods:
We used the 1993 to 2015 releases of the National Inpatient Sample and validated International Classification of Diseases, 9th Revision, Clinical Modification codes to identify patients hospitalized with the combination of opioid abuse, infective endocarditis, and stroke (defined as ischemic stroke, intracerebral hemorrhage, or subarachnoid hemorrhage). Survey weights provided by the National Inpatient Sample were used to calculate nationally representative estimates, and population estimates from the U.S. Census were used to calculate annual hospitalization rates per 10 million person-years. Joinpoint regression was used to assess trends.
Results:
From 1993 through 2015, 5,283 patients were hospitalized with stroke associated with infective endocarditis and opioid use. Across this period, the rate of such hospitalizations increased from 2.4 (95% confidence interval [CI], 0.5 to 4.3) to 18.8 (95% CI, 14.4 to 23.3) per 10 million U.S. residents. Joinpoint regression detected two segments: no significant change in the hospitalization rate was apparent from 1993 to 2008 (annual percentage change, 1.9%; 95% CI, −2.2% to 6.1%), and then rates significantly increased from 2008 to 2015 (annual percentage change, 20.3%; 95% CI, 10.5% to 30.9%), most dramatically in non-Hispanic white patients in the Northeastern and Southern U.S.
Conclusions:
U.S. hospitalization rates for stroke associated with infective endocarditis and opioid use were stable for nearly two decades but then sharply increased starting in 2008, coinciding with the emergence of the opioid epidemic.
Keywords: Infective endocarditis, stroke, drug abuse, opioid, Intravenous Drug Use, Infectious endocarditis, cerebrovascular disease/stroke, risk factors
The opioid epidemic in the United States has led to an increasing number of hospitalizations, cardiovascular complications, and deaths.1 In 2016, nearly 11.8 million people reported misusing opioids, including nearly 1 million people who used heroin.2 Emergency department visits and hospitalizations related to opioid abuse have been increasing by 5% annually while opioid-related deaths have quintupled in the past 20 years.3,4 There has also been a demographic shift, with the largest increase in opioid abuse occurring in women, younger patients and non-Hispanic whites.4–6 Similarly, the pattern of drugs associated with opioid-related deaths has changed, with the number of deaths from heroin—usually injected intravenously—having tripled since 2010.4
Infective endocarditis (IE) is a major cardiovascular complication of intravenous opioid use. IE results from endothelial damage related to repetitive injections and introduction of bacteria into the bloodstream via unsterile needles and preparation techniques.7, 8 The incidence of opioid-related IE is increasing, particularly among younger patients.5, 9–11 Stroke is a neurologically devastating complication affecting nearly 20% of IE patients and often leads to long-term disability or death.11–13 There are few data on trends in the occurrence of stroke as a complication of opioid-related IE, particularly in relation to the increasing severity of the opioid epidemic. In our study, we assessed whether increasing opioid use has led to higher rates of stroke associated with IE and opioid use. We hypothesized that the rising incidence of opioid-related IE would be paralleled by an increasing rate of stroke hospitalization in these patients.
Methods
Design
We used inpatient discharge data from the 1993 to 2015 releases of the Healthcare Cost and Utilization Project’s National Inpatient Sample (NIS). The NIS includes data on ~8 million inpatient hospitalizations each year, representing a 20% stratified sample of all nonfederal U.S. hospitals.14 In 2015, the NIS began providing up to 30 diagnosis code positions per hospitalization record; prior to that, 25 diagnosis code positions were available. This study was approved by the Weill Cornell Medicine institutional review board, which waived the need for informed consent. The data used in this study are subject to a data use agreement and thus cannot be shared directly by the authors, but the source data are publicly available via application to the Healthcare Cost and Utilization Project.
Patient Population
We identified all stroke hospitalizations associated with IE and opioid use during our study period. Cases of IE and stroke were identified using previously validated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes (Table 1).9, 15 The ICD-9-CM codes for IE have been used in prior studies and have been shown to have a positive predictive value of 94% and specificity of 99%.9 Stroke was defined as a composite of hemorrhagic (subarachnoid hemorrhage or intracerebral hemorrhage) or ischemic events. Opioid use was identified using ICD-9-CM codes defined in published trend reports by the Healthcare Cost and Utilization Project.6 Patients were only included if all three diagnoses (stroke, opioid use, and IE) were documented during a hospitalization. In order to follow the validated ICD-9-CM algorithms, we did not give any priority to the positioning of codes.
Table 1.
International Classification of Diseases, Ninth Revision, Clinical Modification Codes Used To Ascertain Disease Variables.
| Diagnosis | Code |
|---|---|
| History of opioid abuse | 970.1, 305.90, 305.91, 305.92, 304.00, 304.01, 304.02, 304.70, 304.71, 304.72, 305.50, 305.51, 305.52, 965.00, 965.01, 965.02, 965.09, E850.0, E850.1, E850.2, E935.0, E935.1, E935.2, E940.10 |
| Infective endocarditis | 421.0, 421.1, 421.9, 424.90, 036.42, 098.84, 112.81, 115.04, 115.14, 115.94, 424.91, 424.99 |
| Stroke | Ischemic stroke: 433.x1, 434.x1, 436 Intracerebral hemorrhage: 431 Subarachnoid hemorrhage: 430 (excluding hospitalizations with codes V57, TBI 800-804, 850-854) |
Measurements
To better understand patterns of stroke hospitalizations associated with IE and opioid use, we evaluated demographic factors (age, sex, race) and hospital geographic location. Pre-specified subgroup analyses were performed to evaluate rates by age (<45 versus ≥45 years of age), sex, race/ethnicity (non-Hispanic white versus non-white), and U.S. Census region (Northeast, Midwest, West, and South). We chose these subgroups based on published data indicating increasing opioid abuse among younger patients, women, and non-Hispanic whites.4–6 We included the geographic location of hospitals due to changing regional differences in opioid-related hospitalizations.6
Statistical Analysis
Sampling weights provided by the NIS were used to calculate nationally representative estimates, and population estimates from the U.S. Census were used to calculate hospitalization rates per 10 million person-years. Due to the NIS sample redesign, we used the updated trend weights for 1993-2011 and the original discharge weights for 2012-2015. Results for the year 2015 were normalized for three-quarters of a year since ICD-9-CM was no longer in use after October 2015. We conducted statistical analysis using STATA (version 14.0, College Station, Texas) and Joinpoint Regression Software (version 4.6.0, National Cancer Institute). The joinpoint regression model is composed of a series of continuous regression lines, with the different lines being connected together at the “joinpoints.”16, 17 These joinpoints determine moments in time at which there is an essential change in the trend. In our study, we aimed to examine up to three possible segments (maximum of two joinpoints) in each trend analysis. To determine the number of existing joinpoints, we first tested the hypothesis of no change in trend against the alternative of two joinpoints (our determined maximum number) using log-linear regression models.16 We defined our null hypothesis as no change in the rate of hospitalizations for stroke associated with IE and opioid use throughout the study period. If the null hypothesis was rejected, then the same procedure would be applied to test the null hypothesis of one joinpoint against the alternative of two joinpoints. The test of statistic involved a Monte Carlo permutation model. After the number of joinpoints was selected, the annual percentage change (APC) was determined for each of the detected time segments. While some subgroups had two APCs corresponding to two different segments connected at a joinpoint, other subgroups had only one segment and no joinpoints, meaning the trend remained continuous during the whole study period for that subgroup. The average APC was the weighted average of each individual APC when there was more than one segment. All trends analyses were two-sided tests and statistical significance was defined as P < 0.05.
Results
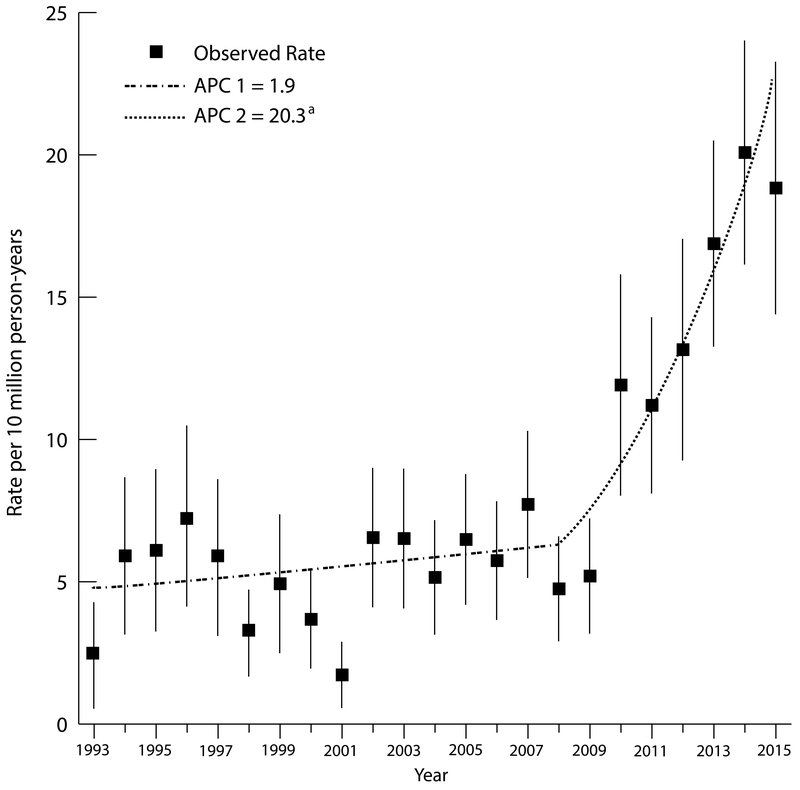
From 1993 to 2015, there were 14,429,338 hospitalizations involving stroke, 12,169,131 involving opioid use, and 815,482 involving IE. During this study period, we identified 5,283 patients hospitalized with stroke associated with IE and opioid use (mean age, 41.2 years; female, 34.2%; non-Hispanic white, 57.6%). Ischemic stroke accounted for 71.5% of hospitalizations and hemorrhagic stroke accounted for 28.5%. Between 1993 and 2015, hospitalizations for stroke associated with IE and opioid use increased from 2.4 (95% confidence interval [CI], 0.5 to 4.3) to 18.8 (95% CI, 14.4 to 23.3) per 10 million U.S. residents per year (Figure 1). Joinpoint analysis detected two segments: no significant change in the hospitalization rate was apparent from 1993 to 2008 (APC, 1.9%; 95% CI, −2.2% to 6.1%), but then rates significantly increased from 2008 to 2015 (APC, 20.3%; 95% CI, 10.5% to 30.9%).
Figure 1. Rates of Hospitalization for Stroke Associated with Infective Endocarditis and Opioid Use, 1993-2015.
Segments indicate log-linear regression estimates for epochs described by different trends as detected by joinpoint regression. APC indicates annual percentage change for each segment. aIndicates that the APC was significantly different from zero. The error bars correspond to 95% confidence intervals for each of the observed annual rates.
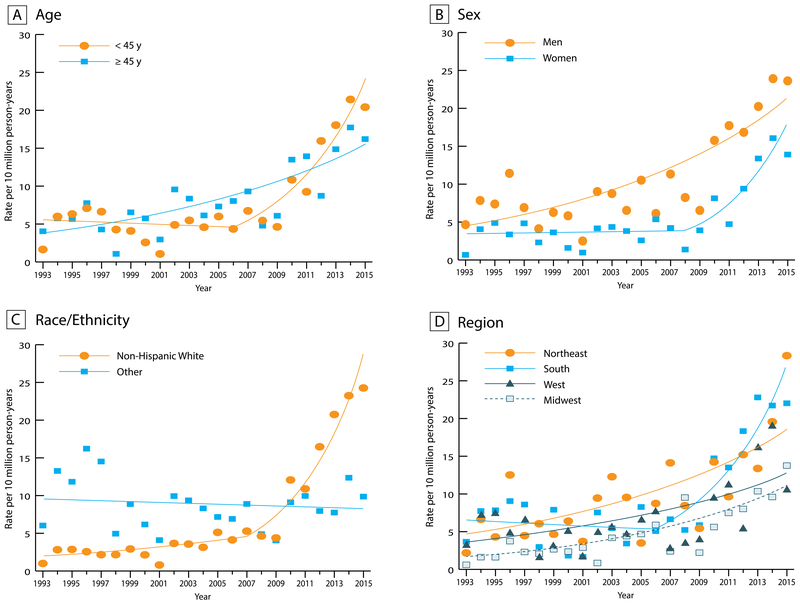
The demographics of patients hospitalized with stroke associated with IE and opioid use changed considerably during the study period (Table 2, Figure 2). After relatively stable trends initially, joinpoint analysis detected a significantly increased rate of stroke hospitalization among patients <45 years old between 2006 and 2015 (Table 3; APC, 20.5%; 95% CI, 12.1% to 29.5%) and women between 2008 and 2015 (APC, 24.4%; 95% CI, 12.1% to 38.1%). In contrast, although there was a significant increase in hospitalization rates among patients ≥45 years and men, rates appeared to continuously increase throughout the study period as joinpoint analysis did not detect changes in either trend.
Table 2.
Characteristics of Patients Hospitalized in the U.S. with Stroke Associated with Infective Endocarditis and Opioid Use.*
|
Women |
Non-Hispanic White‡ |
Ischemic Stroke |
||||||
| Years | Total Number† | Mean age, y | Number | Percent | Number | Percent | Number | Percent |
| 1993-1996 | 578 | 41.2 | 171 | 29.6 | 178 | 35.4 | 406 | 70.3 |
| 1997-2000 | 489 | 42.3 | 175 | 35.7 | 182 | 41.3 | 340 | 69.7 |
| 2001-2004 | 578 | 42.6 | 196 | 34.0 | 227 | 45.9 | 438 | 75.8 |
| 2005-2008 | 740 | 42.7 | 206 | 27.9 | 388 | 60.0 | 559 | 75.6 |
| 2009-2012 | 1284 | 41.0 | 414 | 32.2 | 859 | 73.4 | 924 | 72.0 |
| 2013-2015§ | 1615 | 39.7 | 645 | 39.9 | 1230 | 80.7 | 1110 | 68.7 |
|
U.S. Census Region |
||||||||
|
Northeast |
South |
West |
Midwest |
|||||
| Years | Number | Percent | Number | Percent | Number | Percent | Number | Percent |
| 1993-1996 | 137 | 23.7 | 263 | 45.5 | 130 | 22.4 | 48 | 8.4 |
| 1997-2000 | 115 | 23.5 | 209 | 42.7 | 101 | 20.7 | 64 | 13.1 |
| 2001-2004 | 190 | 32.9 | 186 | 32.1 | 110 | 19.0 | 93 | 16.0 |
| 2005-2008 | 190 | 25.7 | 277 | 37.4 | 141 | 19.0 | 132 | 17.9 |
| 2009-2012 | 249 | 19.4 | 605 | 47.1 | 219 | 17.0 | 212 | 16.5 |
| 2013-2015§ | 305 | 18.9 | 730 | 45.2 | 325 | 20.1 | 255 | 15.8 |
Values in this table are weighted and nationally representative but are not relative to U.S. population estimates as they are meant to characterize hospitalizations documented in the National Inpatient Sample over time.
Column represents the total weighted number of hospitalizations for stroke associated with infective endocarditis and opioid use in the study for each time period.
Percentages were calculated after excluding a small number of patients with missing race/ethnicity data.
Period reflects only 2.75 years of data compared to the other 4-year periods.
Figure 2. Rates of Hospitalization for Stroke Associated with Infective Endocarditis and Opioid Use by (A) Age Group, (B) Sex, (C) Race, and (D) U.S. Region, 1993-2015.
Table 3.
Joinpoint Analysis of Hospitalization Rates per 10 million Population Stratified by Age, Sex, Race/Ethnicity, U.S. Census Region, and Stroke Type
| Trend 1* | Trend 2* | ||||||
|---|---|---|---|---|---|---|---|
| Hospitalization Rate per 10 million |
|||||||
| 1993 | 2015 | Average APC (95% CI)† | Years | APC (95% CI)† | Years | APC (95% CI)† | |
| Overall | 2.4 (0.5 to 4.3) | 18.8 (14.4 to 23.3) | 7.4 (3.6 to 11.3) | 1993-2008 | 1.9 (−2.2 to 6.1) | 2008-2015 | 20.3 (10.5 to 30.9) |
| Age | |||||||
| <45 | 1.6 (0.1 to 3.2) | 20.4 (14.4 to 26.4) | 7.1 (2.5 to 11.8) | 1993-2006 | −1.4 (−7.2 to 4.8) | 2006-2015 | 20.5 (12.1 to 29.5) |
| ≥45 | 4 (−0.8 to 8.9) | 16.2 (10.3 to 22.2) | 6.5 (4.1 to 9.0) | 1993-2015 | 6.5 (4.1 to 9.0) | ||
| Sex | |||||||
| Women | 0.3 (−0.3 to 0.8) | 13.9 (9.1 to 18.7) | 7.7 (2.8 to 12.7) | 1993-2008 | 0.6 (−4.6 to 6.1) | 2008-2015 | 24.4 (12.1 to 38.1) |
| Men | 4.7 (0.9 to 8.5) | 23.6 (16.6 to 30.6) | 7.3 (4.9 to 9.7) | 1993-2015 | 7.3 (4.9 to 9.7) | ||
| Race/Ethnicity | |||||||
| Non-Hispanic White | 1.0 (−0.2 to 2.2) | 24.3 (17.8 to 30.7) | 13.1 (9.2 to 17.3) | 1993-2007 | 6.5 (1.6 to 11.7) | 2007-2015 | 25.7 (17.7 to 34.1) |
| Other | 6.0 (0.2 to 12.2) | 9.4 (4.8 to 14.0) | −0.7 (−3.1 to 1.8) | 1993-2015 | −0.7 (−3.1 to 1.8) | ||
| U.S. Census Region | |||||||
| Northeast | 2.2(−0.9 to 5.3) | 28.4 (14.9 to 41.9) | 6.6 (3.8 to 9.5) | 1993-2015 | 6.6 (3.8 to 9.5) | ||
| South | 3.7 (−0.6 to 7.9) | 22.0 (14.1 to 29.9) | 6.7 (1.2 to 12.6) | 1993-2006 | −1.7 (−9.1 to 6.4) | 2006-2015 | 20.2 (10.7 to 30.4) |
| West | 3.2 (−1.3 to 7.8) | 10.6 (4.1 to 17.0) | 6.0 (2.7 to 9.3) | 1993-2015 | 6.0 (2.7 to 9.3) | ||
| Midwest | 1.6 (−0.6 to 3.9) | 13.8 (6.1 to 21.5) | 9.2 (6.6 to 11.8) | 1993-2015 | 9.2 (6.6 to 11.8) | ||
| Stroke Type | |||||||
| Ischemic | 1.9 (0.2 to 3.6) | 12.8 (9.5 to 16.0) | 7.2 (3.4 to 11.2) | 1993-2008 | 2.7 (−1.5 to 7.0) | 2008-2015 | 17.7 (8.2 to 27.9) |
| Hemorrhagic | 0.5 (−0.1 to 1.0) | 6.1 (3.7 to 8.4) | 6.6 (2.2 to 11.2) | 1993-2005 | −3.1 (−9.5 to 3.8) | 2005-2015 | 19.4 (12.9 to 26.4) |
Abbreviations: APC, Annual Percent Change; CI, Confidence Interval.
Trends are presented as linear segments that are connected at the statistically determined joinpoints. Separate trends are reported only when joinpoint analysis detected points when the slope changed significantly. If no joinpoint was identified for a trend, then there is only one trend and that trend remained continuous for the entire 1993-2015 study period, in which case the average APC is simply the APC for Trend 1. The average APC was not only a function of the starting and ending values of a time series, but was also dependent on the intervening annual estimates and the standard error of each annual estimate. A time series that increased steadily would have a higher average APC than a time series that fluctuated significantly (such as that observed in the Northeast) or a time series with changes in trend (such as that observed in the South). Therefore, regions may have different average APCs despite having similar starting rates in 1993 and ending rates in 2015.
Confidence intervals that do not overlap with 0 represent statistically significant estimates (P < 0.05).
Non-Hispanic whites had the most substantial increase in rates of stroke hospitalization during the study period, with rates increasing from 1.0 (95% CI, −0.2 to 2.2) to 24.3 (95% CI, 17.8 to 30.7) hospitalizations per 10 million U.S. residents between 1993 and 2015. Joinpoint analysis detected a small but significant increase in hospitalization rates among non-Hispanic whites from 1993 to 2007 (APC, 6.5%; 95% CI, 1.6% to 11.7%), followed by a more dramatic increase from 2007 to 2015 (APC, 25.7%; 95% CI, 17.7% to 34.1%). Stroke hospitalization rates began at a much higher level among racial and ethnic minorities compared to non-Hispanic whites in the beginning of the study period, but no significant trend was observed over time.
The Northeast, West, and Midwest regions of the U.S. all experienced significant increases in hospitalization rates for stroke associated with IE and opioid use which were continuous throughout the study period. In the Southern region, rates were stable before sharply increasing from 2006 to 2015 (APC, 20.2%; 95% CI, 10.7% to 30.4%). The Midwest region experienced the greatest relative increase in hospitalization rates, with rates increasing by 9.2% per year. However, the greatest absolute increases were observed in the Northeastern and Southern regions, with rates remaining notably high at the end of the study period (Table 3).
Discussion
In a large, nationally representative sample, we found that U.S. hospitalization rates for stroke associated with IE and opioid use were stable for nearly two decades before rising sharply in 2008, which coincides with known trends in opioid abuse in the U.S. We found that non-Hispanic whites in the Northeastern and Southern U.S. experienced the greatest increases in stroke hospitalization rates over our study period. Additionally, while stroke hospitalizations increased across ages and genders, the greatest increases occurred in women and those <45 years old over the past decade.
Although stroke is a known complication of IE, there are few data on the rate of stroke associated with IE and opioid use. Our study provides new information on the neurological consequences of the opioid epidemic. These novel findings indicate that increasing opioid abuse in the U.S. is not only causing more social/occupational dysfunction, cardiac complications, and premature mortality, but may also be increasing the population burden of permanent functional disability as a result of stroke.
The increased rate of stroke hospitalizations associated with IE and opioid use since 2008 may be a consequence of increased intravenous heroin use over the past decade. Public health concerns over the nonmedical use of prescription opioids has led to implementation of federal and local prevention strategies aimed at reducing the misuse and abuse of prescription opioids.18 While prescription opioid use has been decreasing, there has been a rise in heroin use and overdose-related deaths since 2007, perhaps due to heroin’s lower price and wide availability.2, 4, 19, 20 Unlike prior surges in heroin use, the current opioid epidemic has seen a clear link between nonmedical prescription opioid abuse and heroin use; many current heroin users report abusing prescription opioids prior to starting heroin.21–23 Although only a small percentage of prescription opioid users switch to heroin, prescription opioid use continues to be identified as a strong risk factor for heroin use.22, 23 Heroin is commonly injected intravenously and can cause IE through various mechanisms, including the introduction bacteria into the bloodstream from dirty needles or contaminated syringes, endothelial damage on valves from repetitive drug use, and use of saliva as a diluting agent or as lubrication on injection needles.8, 24, 25 The rise in heroin use combined with these high-risk injection practices may explain why opioid-related IE is becoming more prevalent and leading to complications such as stroke and death.5, 9, 11
Our study should be considered in light of several limitations. First, we used administrative claims data to establish diagnoses which may have resulted in misclassification of diagnoses. We attempted to minimize misclassification by using previously validated diagnosis codes for stroke and IE and validated and standardized diagnosis codes used in surveillance reports on the opioid epidemic.6, 9, 26–29 Second, administrative claims data lack access to granular clinical information related to the stroke (etiology, severity, location) and IE events. Third, given the design of the NIS, there may have been double counting of patients with multiple hospitalizations in a given year. We think it is unlikely that such occurrences would have changed over time and therefore such double-counting should not have significantly affected our trend analyses. Fourth, we may have underestimated absolute rates of strokes from IE since strokes may have occurred after the initial IE hospitalization,30 although the underlying IE diagnosis would most likely have also been documented during the stroke hospitalization. Fifth, our joinpoint analyses may have lacked power to detect changes in trends within specific subgroups. Lastly, underreporting of opioid abuse by patients would have resulted in an underestimation of rates of stroke associated with IE and opioid use.
Conclusion
We found a sharp increase in U.S. hospitalization rates from stroke associated with IE and opioid use beginning in 2008, coinciding with the worsening of the opioid epidemic and known patterns of increased heroin use in the U.S. Non-Hispanic white patients in the Northeastern and Southern U.S. experienced the greatest increases in the rate of hospitalization for stroke associated with IE and opioid use over this time period. These findings add to the urgency of addressing the underlying opioid epidemic in the U.S. and suggest a need for improved awareness of the cerebrovascular complications of opioid abuse.
Acknowledgements:
Sources of Funding: Dr. Salehi Omran is supported by National Institutes of Health StrokeNet grant U24NS107237. Dr. Merkler is supported by American Heart Association grant 18CDA34110419 and the Leon Levy Fellowship in Neuroscience. Dr. Kamel is supported by National Institutes of Health/National Institute of Neurological Disorders and Stroke grants R01NS097443 and U01NS095869 and the Michael Goldberg Research Fund.
Footnotes
Disclosures: None.
References
- 1.Hsu DJ, McCarthy EP, Stevens JP, Mukamal KJ. Hospitalizations, costs and outcomes associated with heroin and prescription opioid overdoses in the united states 2001-12. Addiction. 2017;112:1558–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the united states: Results from the 2016 national survey on drug use and health. Available at: https://www.samhsa.gov/data/.
- 3.Centers for Disease Control and Prevention. Opioid overdose: understanding the epidemic. Available at: www.cdc.gov/drugoverdose/epidemic/index.html.
- 4.Hedegaard H, Warner M, Minino AM. Drug Overdose Deaths in the United States, 1999-2015. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 5.Wurcel AG, Anderson JE, Chui KK, Skinner S, Knox TA, Snydman DR, et al. Increasing Infectious Endocarditis Admissions Among Young People Who Inject Drugs. Open Forum Infect Dis. 2016;3:ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owens P Hospital Inpatient Utilization Related to Opioid Overuse Among Adults, 1993-2012. Available at: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb177-Hospitalizations-for-Opioid-Overuse.jsp. [PubMed]
- 7.Sousa C, Botelho C, Rodrigues D, Azeredo J, Oliveira R. Infective endocarditis in intravenous drug abusers: An update. Eur J Clin Microbiol Infect Dis. 2012;31:2905–2910. [DOI] [PubMed] [Google Scholar]
- 8.Frontera JA, Gradon JD. Right-side endocarditis in injection drug users: review of proposed mechanisms of pathogenesis. Clin Infect Dis. 2000;30:374–379. [DOI] [PubMed] [Google Scholar]
- 9.Toyoda N, Chikwe J, Itagaki S, Gelijns AC, Adams DH, Egorova NN. Trends in Infective Endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartman L, Barnes E, Bachmann L, Schafer K, Lovato J, Files DC. Opiate Injection-associated Infective Endocarditis in the Southeastern United States. Am J Med Sci. 2016;352:603–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Njoroge LW, Al-Kindi SG, Koromia GA, ElAmm CA, Oliveira GH. Changes in the Association of Rising Infective Endocarditis With Mortality in People Who Inject Drugs. JAMA Cardiol. 2018. August 1;3(8)779–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murdoch DR, Corey GR, Hoen B, Miro JM, Fowler VG Jr., Bayer AS, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Cabrera E, Fernandez-Hidalgo N, Almirante B, Ivanova-Georgieva R, Noureddine M, Plata A, et al. Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: A multicenter observational study. Circulation. 2013;127:2272–2284. [DOI] [PubMed] [Google Scholar]
- 14.Healthcare Cost and Utilization Project (HCUP). Overview of the Nationwide Inpatient Sample (NIS). Available at: www.hcup-us.ahrq.gov/nisoverview.jsp.
- 15.Tirschwell DL, Longstreth WT Jr. Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. [DOI] [PubMed] [Google Scholar]
- 16.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. [DOI] [PubMed] [Google Scholar]
- 17.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Statistics in medicine. 2009;28:3670–3682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Department of Health and Human Services. Addressing prescription drug abuse in the United States: current activities and future opportunities. Available at: www.cdc.gov/drugoverdose/pdf/hhs_prescription_drug_abuse_report_09.2013.pdf.
- 19.Unick G, Rosenblum D, Mars S, Ciccarone D. The relationship between us heroin market dynamics and heroin-related overdose, 1992-2008. Addiction. 2014;109:1889–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N Engl J Med. 2016;374:154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lankenau SE, Teti M, Silva K, Jackson Bloom J, Harocopos A, Treese M. Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012;23:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132:95–100. [DOI] [PubMed] [Google Scholar]
- 23.Muhuri PK GJ, Davies MC. Associations of Nonmedical Pain Reliever Use and Initation of Heroin Use in the United States. Available at: www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm.
- 24.Mathew J, Addai T, Anand A, Morrobel A, Maheshwari P, Freels S. Clinical features, site of involvement, bacteriologic findings, and outcome of infective endocarditis in intravenous drug users. Arch Intern Med. 1995;155:1641–1648. [PubMed] [Google Scholar]
- 25.Sande MA LB, Mills J. Endocarditis in Intravenous drug users In: D K, ed. Infective Endocarditis. New York City: Raven Press; 1992:345. [Google Scholar]
- 26.Ellison J, Walley AY, Feldman JA, Bernstein E, Mitchell PM, Koppelman EA, et al. Identifying Patients for Overdose Prevention With ICD -9 Classification in the Emergency Department, Massachusetts, 2013-2014. Public Health Rep. 2016;131:671–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green CA, Perrin NA, Janoff SL, Campbell CI, Chilcoat HD, Coplan PM. Assessing the accuracy of opioid overdose and poisoning codes in diagnostic information from electronic health records, claims data, and death records. Pharmacoepidemiol Drug Saf. 2017;26:509–517. [DOI] [PubMed] [Google Scholar]
- 28.Reardon JM, Harmon KJ, Schult GC, Staton CA, Waller AE. Use of diagnosis codes for detection of clinically significant opioid poisoning in the emergency department: A retrospective analysis of a surveillance case definition. BMC Emerg Med. 2016;16:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss AJ EA, Barrett ML, Steiner CA, Bailey MK, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009-2014. HCUP Statistical Brief #219. [Google Scholar]
- 30.Merkler AE, Chu SY, Lerario MP, Navi BB, Kamel H. Temporal relationship between infective endocarditis and stroke. Neurology. 2015;85:512–516. [DOI] [PMC free article] [PubMed] [Google Scholar]