Abstract
Nephrocalcinosis is a rare condition in clinical practice where there is an increased renal deposition of calcium. Varied causes of this condition have been given in literature, and tuberculosis (TB) has been an important one. Hypercalcemia is a known complication of granulomatous diseases. We report a rare case explicitly showing relationship of extrapulmonary (genitourinary) TB with nephrocalcinosis.
Keywords: Extrapulmonary tuberculosis, hypercalcemia, nephrocalcinosis
Introduction
Nephrocalcinosis is a condition where there is an increased renal parenchymal deposition of calcium which has substantial overlap with hypercalcemia, nephrolithiasis, renal parenchymal damage, and reduced renal function. Nephrocalcinosis most often applies to increased renal calcium content, as opposed to the localized and focal increase in calcium seen in infarct and caseating granulomas in renal tuberculosis (TB). In patients with chronic granulomatous disease such as sarcoidosis,[1] TB,[2] and fungal diseases, excess 1,25 dihydroxy vitamin D synthesis from 25(OH) vitamin D can lead to hypercalcemia and hypercalcuria-related nephrocalcinosis.
Case Report
A 42-year-old female patient, farmer by occupation, resident of Chamba district, presented to our outpatient department with chief complaints of fever for 2 months and right-sided chest pain for the same duration. The patient was apparently well before that when she presented with fever documented up to 102° Fahrenheit with evening rise in temperature and it was associated with night sweats but not associated with any chills and rigor or any rash or skin changes. Her right-sided chest pain was localized to infra-axillary region, nonradiating, sharp, nonexertional, and got aggravated on deep inspiration and coughing. There was no history of cough and shortness of breath. Ten years ago, she took treatment for lymph node (LN) TB but defaulted after 3 months of therapy. She never took any medication for diabetes and hypertension. There was no history suggestive of any contact with TB patient, or high-risk sexual behavior. Family history, menstrual history, and recent treatment history were unremarkable. On examination, the patient had pallor and mild dependent edema. Five LNs were palpable in the right cervical region superior and middle cervical region, the largest being 2.5 cm in diameter, matted, nontender, and not associated with any overlying skin changes not fixed to the underlying structure or skin. On respiratory system examination, the right infra-scapular and infra-axillary region were dull on percussion and breath sounds were decreased with shifting dullness suggestive of right-sided pleural effusion, which was confirmed by chest X-ray. About 5 mL of straw colored fluid was tapped and sent for investigation.
Investigations revealed the following: Hb 8.9 g/dL, total leukocyte count 4970 (neutrophils 76%, lymphocytes 15%, eosinophils 5%, basophils 3%, monocytes 1%), platelet 320,000, serum glutamic oxaloacetic transaminase 44, serum glutamic pyruvate transaminase 34, bilirubin total 0.8, albumin 3.9, alkaline phosphatase 128, urea 96, creatinine 1.9, Na 143, K 4.5, calcium 11.3 mg/dL, phosphorous 4.9, serum and urine electrophoresis was negative, intact parathyroid hormone 20 ng/L (8–51 pg/mL), arterial blood gas showed pH of 7.38, 25(OH) vitamin D 97 ng/mL (30–100 ng/mL), angiotensin converting enzyme level 10 U/L, urine routine and microscopy were normal, and urine for acid fast bacilli was negative. Urinary calcium level was higher than normal (U Ca/Cr = 32). Chloride level was 23 mmol/L. Ultrasonography KUB and noncontrast computed tomography KUB [Figure 1] were suggestive of medullary macro-calcification without any evidences of renal TB. Renal biopsy [Figure 2] was done showing interstitial deposition of calcium without any histological evidences for renal parenchymal TB. Intravenous pyelogram was done and it did not reveal any lesion suggestive of genitourinary TB. LN biopsy revealed caseating granulomatous change with Genexpert (CB-NAAT) positive. Pleural fluid was exudative, and lymphocyte was predominant (95%) with adenosine deaminase level of 67 ng/mL. Hence, a diagnosis of extrapulmonary TB was made.
Figure 1.
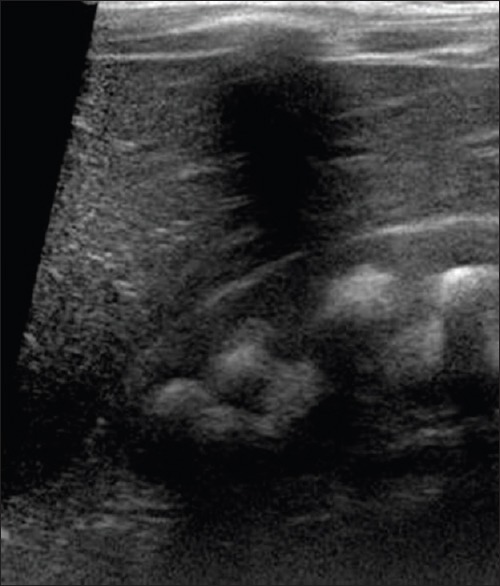
USG showing calcium deposition
Figure 2.
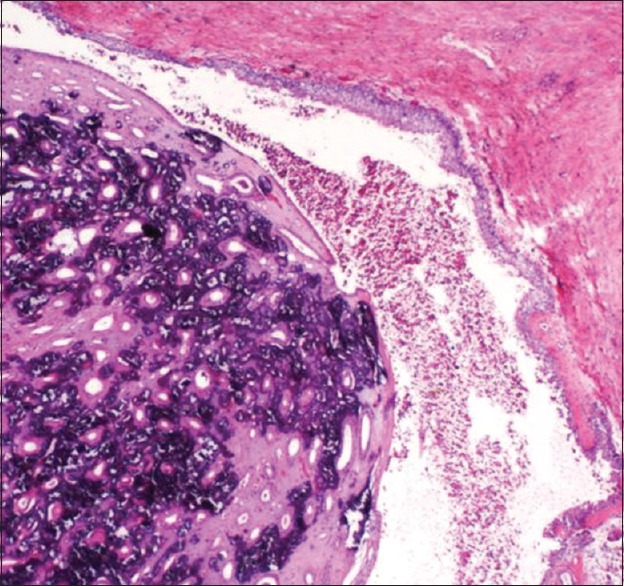
Renal biopsy showing Calcium deposition in medulla
Discussion
TB is one of the most common chronic granulomatous diseases in India though nephrocalcinosis without genitourinary TB is exceedingly rare in practice. Hypercalcemia is known to occur in granulomatous diseases among which sarcoidosis[1] is the most common and the others are TB, fungal infections, berylliosis, and lymphoma. Though infrequent, hypercalcemia is a recognized complication of active TB.[2] The results of various studies from different countries reporting hypercalcemia incidence in TB did not match, probably because of ethnic and racial disturbances, the amount of sun exposure, and difference in vitamin D and calcium intake. In the United States, hypercalcemia is reported in 16%–28% of pulmonary TB, whereas low percentage of hypercalcemia (5.2%) was found in another study from Pakistan.[3] Hematogenous dissemination of Mycobacterium tuberculosis can result in infection of any organ. The commonly affected are the brain, the kidneys, the bones, and the cervical LNs that drain the pulmonary vessel. The most common extrapulmonary cases reported were pleural (16%), LN (40%), bone or joint (10%), genitourinary tract (5%), meningeal (6%), and peritoneal (6%).[4] Renal TB typically presents late with advanced disease because the early stages cause few symptoms and signs.[5] But extrapulmonary TB can lead to hypercalcemia secondary to increased 1,25 dihydroxy vitamin D[6] in a patient with normal vitamin D level, especially people who have adequate sunlight exposure complicating into hypercalcuria and hypercalcemic medullary nephrocalcinosis without any genitourinary TB. This case report is rare as it explains uncommon relationship of TB with nephrocalcinosis. In view of rampant urogenital TB, medullary nephrocalcinosis complicating TB should always be kept as differential diagnosis in a patient presenting to primary care physicians with renal failure and the patient should be evaluated as described above. Since with the treatment of granulomatous conditions such as TB hypercalcemia will be treated and nephrocalcinosis will also recover.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999;160:736–55. doi: 10.1164/ajrccm.160.2.ats4-99. [DOI] [PubMed] [Google Scholar]
- 2.Pruitt B, Onarecker C, Coniglione T. Hypercalcemic crisis in a patient with pulmonary tuberculosis. J Okla State Med Assoc. 1995;88:518–20. [PubMed] [Google Scholar]
- 3.Ijaz A, Mehmood T, Saeed W, Qureshi AH, Dilawar M, Anwar M, et al. Calcium abnormalities in pulmonary tuberculosis. Pakistan J Med Res. 2004;43 [Google Scholar]
- 4.CDC. Reported Tuberculosis in the United States 2010. Atlanta, GA: Department of Health and Human Services; 2011. [Google Scholar]
- 5.Eastwood JB, Corbishley CM, Grange JM. Tuberculosis and the kidney. J Am Soc Nephrol. 2001;12:1307–14. doi: 10.1681/ASN.V1261307. [DOI] [PubMed] [Google Scholar]
- 6.El Maghraoui J, Souilmi FZ, Hbibi M, Houssaini TS, Hida M. Nephrocalcinosis complicating military tuberculosis in an infant. Pan Afr Med J. 2015;20:425. doi: 10.11604/pamj.2015.20.425.6542. [DOI] [PMC free article] [PubMed] [Google Scholar]


