Abstract
Context:
The provider-driven disrespect and abuse (DA) of women during childbirth is a marker for quality of maternal care and violation of basic human rights.
Aims:
This study was done to assess prevalence and sociodemographic determinants of DA experienced during facility-based childbirth.
Settings and Design:
This is a cross-sectional, community-based study done in six villages in the district of Aligarh, north India.
Subjects and Methods:
In all, 305 women who underwent facility-based childbirth were interviewed by pretested and structured questionnaire at home between 4 and 6 weeks postpartum period.
Statistical Analysis Used:
Descriptive statistics, Chi-square test, and bivariate regression analysis using SPSS 20.0 were used.
Results:
A total of 257 (84.3%) of 305 women reported any form of DA. Nonconsented services (71.1%) and nonconfidential care (62.3%) were the most common types. Abandonment/neglect during childbirth was reported by 10.2% women, nondignified care by 9.2%, physical abuse by 5.9%, detention in the health facility by 3.3%, and discrimination by 3.9%. Women who had undergone vaginal birth [odds ratio (OR) 3.36; confidence interval (CI) 1.7–6.5], at public health facility (OR 2.65; CI 1.4–5.0), given care by providers other than doctors (OR 2.89; CI 1.5–5.5), who belonged to low socioeconomic status (OR 3.68; CI 1.4–9.7), and who did not decide place of delivery themselves (OR 4.49; CI 2.0–12.1) were more at risk of DA. Out of all females unwilling to attend facility in future, 93.8% reported experiencing DA. The association between any DA and decision to attend the facility in future was statistically significant.
Conclusion:
More than 8 of 10 women experienced any DA during facility-based childbirth. It can be a barrier to utilization of facility for childbirth. Preventing DA is important to improve quality of maternal care and institutional deliveries.
Keywords: Abuse, childbirth, disrespect, facility, maternal care
Introduction
Disrespect and abuse (DA) of women during childbirth in facilities has recently gained recognition not only as a marker for quality of maternal care but also as violation of basic human rights of birthing women.[1] In a 2010 landscape analysis, Bowser and Hill[2] described seven categories of disrespectful and abusive care during childbirth – physical abuse, nonconsensual care, nonconfidential care, nondignified care, discrimination, abandonment of care, and detention in facilities. Various manifestations of DA during childbirth have implications on maternal mortality in ways both direct and indirect – directly by use of inappropriate and excessive (also often not informed and not consented) invasive interventions in vaginal birth, neglect, and delay of care, especially among females with discrimination on the basis of socioeconomic status (SES), HIV status, and marital status[3] and indirectly by becoming a barrier to seeking delivery care.[4] Women experiencing DA during childbirth may not choose the facility for subsequent deliveries[5] and may not recommend it to other women. DA during childbirth not only affects healthcare utilization and maternal mortality but also is a violation of basic human rights of females.[6] Recognizing this emerging public health problem, in 2014, World Health Organization gave a call for preventing and eliminating DA during facility-based childbirth.[7]
Although DA during childbirth has been known to be prevalent around the world from olden times under different names,[8] it has gained recognition and attention during recent years. Respectful Maternity Care (RMC) is the other side of the same coin which has gained momentum as a movement.[9] While RMC primarily emphasizes the absence of DA by healthcare providers and other staff, its definition also advocates positive and supportive staff attitudes and behaviors that increase a woman's satisfaction with her birth experience.
The prevalence of self-reported DA has ranged from 20% in Kenya,[10] 43% in Ethiopia,[11] to 98% in Nigeria.[12] The prevalence varies in various parts of the world and also depends on the time of survey. In a study in rural Tanzania, the proportion of women who reported experiencing any mistreatment during childbirth was 19.5% in the facility exit survey and 28.2% in the follow-up survey 5–10 weeks postpartum.[13] Researchers have also reported higher prevalence of abusive care by direct observation than that reported by women, pointing toward their acceptance of DA as “normal” part of birthing process.[14]
Various sociodemographic factors have been reported to predispose women to DA during childbirth in a facility such as higher parity, lower SES, and HIV-positive status.[2,8] Most of the studies done are qualitative in nature[15,16] with few quantitative studies. There is limited evidence about the prevalence of DA during facility-based childbirth and its type of manifestations in developing country like India and, there is a need to understand its determinants in this setting.
This study was done to assess the prevalence of DA during facility-based childbirth and determine the sociodemographic and obstetrics correlates of the same among recently delivered women of rural north India.
Subjects and Methods
Study design
A community-based cross-sectional study was done among recently delivered females residing in field study areas of Rural Health Training Centre (RHTC) of Department of Community Medicine, J.N. Medical College, Aligarh Muslim University, Aligarh.
Setting
RHTC is located in the Jawan block in the district of Aligarh, Uttar Pradesh, in north India. Six villages are registered under RHTC with a population of 19,000. The data for this cross-sectional study were collected in a period of 1 year, from November 2016 to October 2017.
The nearest facilities available for childbirth in this area include one community health centre, located in the Jawan block, and two private nursing home in village Jawan and village Tejpur. District hospital and Medical College hospital are located at a distance of more than 10 km from this area.
Subject recruitment for study
Identification and registration of newly delivered females was done from the vital records collected and maintained by the medicosocial workers of the Department of Community Medicine. All the females who had undergone facility-based childbirth (either in public or private facility) were visited at home between 4 and 6 weeks postpartum period. All the females who delivered during the 1-year study period and gave consent were included in the study. Those postpartum females who had undergone home delivery or did not give consent or not found at home during two visits were excluded. In total, 305 eligible females were interviewed.
Materials and methods
Ethical clearance was taken from the Institutional Ethical Committee of J.N. Medical College, Aligarh Muslim University. A pilot study was done to test the proforma, and the necessary modifications were made. The proforma consisted of three parts – the first part included sociodemographic information such as age, religion, educational level, occupation of female and her spouse, type of family, and family's per capita income per month. SES of females was assessed using Standard of Living Index, a tool used in National Family Health Survey-2 in India.[17] The second part included information related to childbirth such as parity, place and time and mode of delivery, presence of any family member during childbirth, whether the facility was visited for delivery previously also, and who decided the place of delivery. The third part was regarding perception of any humility at the facility and consisted of detailed history of DA during childbirth described under seven major domains[2] – physical abuse, nonconsented care, nonconfidential care, nondignified care, discrimination based on specific patient attributes, abandonment of care, and detention in facilities for failure to pay. Satisfaction with services in the facility and whether they would revisit the facility for childbirth in future was also enquired about.
Interviews were conducted at home in a confidential and nonjudgemental manner, at least a month after delivery to ensure that females were not distracted by other concerns in the immediate postpartum period (pain in episiotomy or other stitch sites, any breastfeeding problems, etc.). At the same time, only postpartum females up to period of 6 weeks were included to reduce recall bias. Informed verbal consent was taken. Appropriate postnatal care and counseling was provided to mothers and their infants and referral was done if needed.
Statistical analysis
The data were entered in Excel Sheet and checked for correctness and missing data, and then were entered into IBM SPSS 20.0 software for analysis. Descriptive statistics and inferential statistics were computed. Chi-square test and Fisher's exact test were applied for categorical variables. Proportions of different manifestations of DA are reported with their 95% confidence interval (CI). The odds ratio (OR) with 95% CI for sociodemographic and obstetric correlates of DA were calculated. P value less than 0.05 was considered as statistically significant.
Results
Sociodemographic and delivery experience characteristics of study population are shown in Table 1. The majority of females (45.6%) were in 20–25 years age group, were Hindu (75.4%), and belonged to joint-extended family (68.2%). More than half (50.8%) had not attended school and all were home-makers. Most of them belonged to medium SES (46.6%). The majority of females were multipara (62%) and had delivered in a public facility (63.6%), during day time (64.3%), and by vaginal route (78.7%) in the presence of a family member (69.8%). The healthcare provider was other than doctor in a majority of females (55.1%). Only 7.5% of females had decided the place of delivery themselves.
Table 1.
Sociodemographic and delivery experience characteristics of study population (n=305)
| Variable | Categories | n (%) |
|---|---|---|
| Age group (years) | Up to 20 | 39 (12.8) |
| 21-25 | 139 (45.6) | |
| 26-30 | 32 (10.5) | |
| >30 | 32 (10.5) | |
| Religion | Hindu | 230 (75.4) |
| Muslim | 74 (24.3) | |
| Christian | 01 (0.3) | |
| Type of family | Nuclear | 97 (31.8) |
| Joint-extended | 208 (68.2) | |
| Education of female | Did not attend school | 155 (50.8) |
| Primary | 44 (14.4) | |
| Secondary | 46 (15.1) | |
| >Secondary | 60 (19.7) | |
| Occupation of female | Home-maker | 305 (100.0) |
| Husband’s education | Did not attend school | 91 (29.8) |
| Primary | 59 (19.3) | |
| Secondary | 87 (28.5) | |
| >Secondary | 68 (22.3) | |
| Standard of Living Index | Low | 130 (42.6) |
| Medium | 142 (46.6) | |
| High | 33 (10.8) | |
| Parity | Primipara (1) | 97 (31.8) |
| Multipara (2-4) | 189 (62.0) | |
| Grand multipara (≥5) | 19 (6.2) | |
| Place of delivery | Public | 194 (63.6) |
| Private | 111 (36.4) | |
| Time of delivery | Day | 196 (64.3) |
| Night | 109 (35.7) | |
| Mode of delivery | Vaginal | 240 (78.7) |
| Caesarean section | 65 (21.3) | |
| Healthcare provider | Doctor | 137 (44.9) |
| Other (ANM, SN, LHV) | 168 (55.1) | |
| Presence of family members at time of delivery | Yes | 213 (69.8) |
| No | 92 (30.2) | |
| Decision for place of delivery | By woman herself | 23 (7.5) |
| By others | 282 (92.5) |
ANM: Auxiliary nurse midwife; SN: Staff nurse; LHV: Lady Health Visitor
Of 305 recently delivered females, 257, that is, 84.3% (95% CI: 79.7%–87.9%), reported any form of DA. This was defined as presence of any manifestation of disrespect and abuse during the childbirth experience. Figure 1 shows the proportion of various types of DA reported by females. Nonconsented services and nonconfidential care were the most common types of DA, affecting 71.1% (95% CI: 65.8%–75.9%) (n = 217) and 62.3% (95% CI: 56.7%–67.5%) (n = 190) respondents, respectively. Abandonment/neglect during childbirth was reported by 10.2% (95% CI: 7.2%–14.1%) (n = 31) women, nondignified care by 9.2% (95% CI: 6.4%–13.0%) (n = 28), physical abuse by 5.9% (95% CI: 3.7%–9.1%) (n = 18), discrimination by 3.9% (95% CI: 2.2%–6.8%) (n = 12), and detention in the health facility by 3.3% (95% CI: 1.7%–6.0%) (n = 10).
Figure 1.
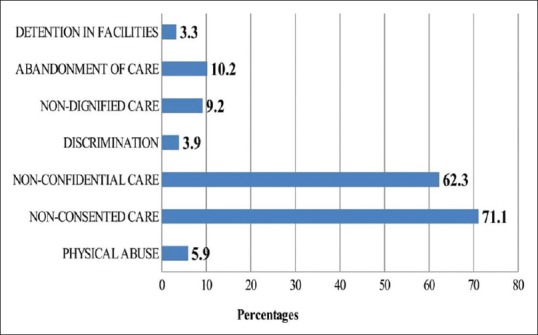
Distribution of different types of disrespect and abuse during facility-based childbirth (N = 305). Note: Women may report more than one type of DA (total may be more than 100%)
The association between DA and sociodemographic factors and association between DA and obstetric factors were assessed by bivariate regression analysis, and are shown in Tables 2 and 3, respectively. Women with nuclear family were 2.26 more at odds to experience DA when compared with those of joint-extended families (OR 2.26; CI 1.1–4.9). Women who had undergone vaginal birth (OR 3.36; CI 1.7–6.5), delivered at public health facility (OR 2.65; CI 1.4–5.0), given care by providers other than doctors (OR 2.89; CI 1.5–5.5), and who belonged to low SES (OR 3.68; CI 1.4–9.7) were more likely to have experienced DA. Age, education, religion and parity of females, time of delivery, and presence of family members at the time of delivery were not found to have significant association with DA. Odds of experiencing DA at facility increased (OR 4.49; CI 2.0–12.1) when the place of delivery was not decided by woman herself.
Table 2.
Sociodemographic determinants of DA during facility-based childbirth (n=305)
| Variable | Any DA, n (%) | Odds ratio | 95% CI | P |
|---|---|---|---|---|
| Age group (years) | ||||
| Up to 20 | 35 (13.6) | - | - | - |
| 21-25 | 112 (43.6) | 0.47 | 0.2-1.4 | 0.190 |
| 26-30 | 80 (31.1) | 0.61 | 0.2-2.0 | 0.408 |
| >30 | 30 (11.7) | 1.71 | 0.3-10.0 | 0.550 |
| Religion | ||||
| Hindu | 190 (82.6) | 0.57 | 0.2-1.3 | 0.181 |
| Muslim | 66 (89.2) | - | - | - |
| Type of family | ||||
| Nuclear | 88 (34.2) | 2.26 | 1.1-4.9 | 0.03 |
| Joint-extended | 169 (65.8) | - | - | - |
| Education of female | ||||
| Did not attend school | 135 (52.5) | 1.68 | 0.8-3.7 | 0.193 |
| Primary | 39 (15.2) | 1.95 | 0.6-6.0 | 0.245 |
| Secondary | 35 (13.6) | 0.79 | 0.3-2.0 | 0.628 |
| >Secondary | 48 (18.7) | - | - | - |
| Husband’s education | ||||
| Did not attend school | 79 (86.8) | 2.19 | 1.0-5.0 | 0.060 |
| Primary | 55 (93.2) | 4.58 | 1.4-14.5 | 0.010 |
| Secondary | 72 (82.8) | 1.60 | 0.7-3.5 | 0.238 |
| >Secondary | 51 (75.0) | - | - | - |
| Standard of Living Index | ||||
| Low | 118 (90.8) | 3.68 | 1.4-9.7 | 0.008 |
| Medium | 115 (81.0) | 1.59 | 0.7-3.8 | 0.293 |
| High | 24 (72.7) | - | - | - |
DA: Disrespect and abuse; CI: Confidence interval. Bold values: *P value<0.05, statistically significant
Table 3.
Obstetric factors as correlates of any DA during facility-based childbirth (n=305)
| Variables | Any DA, n (%) | Odds ratio | 95% CI | P |
|---|---|---|---|---|
| Parity | ||||
| Primi gravida (1) | 79 (81.4) | - | - | - |
| Multigravida (2-4) | 162 (85.7) | 1.37 | 0.7-2.6 | 0.347 |
| Grand multigravida (≥5) | 16 (84.2) | 1.22 | 0.3-4.6 | 0.775 |
| Place of delivery | ||||
| Public | 173 (67.3) | 2.65 | 1.4-5.0 | 0.002 |
| Private | 84 (32.7) | - | - | - |
| Time of delivery | ||||
| Day | 167 (65.0) | 1.2 | 0.6-2.3 | 0.545 |
| Night | 90 (35.0) | - | - | - |
| Mode of delivery | ||||
| Vaginal | 212 (88.3) | 3.36 | 1.7-6.5 | 0.000 |
| Caesarean section | 45 (69.2) | - | - | - |
| Healthcare provider | ||||
| Doctor | 105 (40.9) | - | - | - |
| Other (ANM, SN, LHV) | 152 (59.1) | 2.89 | 1.5-5.5 | 0.001 |
| Presence of family members at time of delivery | ||||
| Yes | 79 (30.7) | - | - | - |
| No | 178 (69.3) | 1.2 | 0.6-2.4 | 0.613 |
| Decision for place of delivery | ||||
| By woman herself | 13 (56.5) | - | - | - |
| By others | 244 (86.5) | 4.49 | 2.0-12.1 | 0.000 |
DA: Disrespect and abuse; CI: Confidence interval; ANM: Auxiliary nurse midwife; SN: Staff nurse. Bold values: *P value<0.05, statistically significant
On being asked whether they were satisfied with the healthcare services at the facility, 86.9% (n = 265) said yes. Among those who were satisfied, 83.8% (222 of 265) had experienced DA, and among those who were unsatisfied, 87.5% (35 of 40) reported it. But the association was not statistically significant (Chi-square = 0.364, df = 1, P > 0.05).
When enquired about their willingness to attend the facility for childbirth in future, 55.1% (n = 168) females were willing, 39.7% (n = 121) were indecisive, and 5.2% (n = 16) said no. Of those females who said no, 93.8% reported experiencing any DA. Of those who were indecisive, 91.7% had experienced the same. The association between any DA and decision to attend the facility in future was found to be statistically significant (Chi-square = 11.188, df = 2, P < 0.05).
Only 9.2% (28 of 305) females responded in yes on being asked about any treatment which they perceived as humiliating, with 89.1% (229 of 257) of females with any DA responding in “no” to this query [Table 4]. The association between DA and perception of any treatment as humiliating was found to be statistically significant (Chi-square = 5.76, df = 1, P < 0.05).
Table 4.
Association between any DA during facility-based childbirth and perception of humiliation by female (n=305)
| Any disrespect and abuse | Total, n (%) | Fisher’s exact test | |||
|---|---|---|---|---|---|
| Absent, n (%) | Present, n (%) | ||||
| Any treatment to make you feel humiliated | No | 48 (100.0) | 229 (89.1) | 277 (90.8) | Chi-square=5.76, df=1, P<0.05 |
| Yes | 0 (0.0) | 28 (10.9) | 28 (9.2) | ||
| Total | 48 (15.7) | 257 (84.3) | 305 (100.0) | ||
DA: Disrespect and abuse
Discussion
This study is a community-based quantitative study done in India which reports DA during childbirth in facility among rural women. More than 8 of 10 women in this study (84.3%) reported experiencing any DA. This prevalence is high and comparable to those reported in Tanzania (70%),[18] Pakistan (97%),[19] and Nigeria (98%)[12] but much higher than that reported in some other developing countries like Brazil (18.3%).[20] Such varied prevalence rates over various parts of world highlight not only the importance of situational analysis at local levels but also the need of standard measurement tools to allow comparability – definition of DA, time of survey to assess the same, observed versus perceived abuse by women, and so on – an issue raised by researchers recently.[21]
In a study done in India among females of urban slums of Lucknow who had delivered in a facility in the past 5 years, more than half of females (54.7%) reported experiencing any mistreatment during delivery in a facility, with verbal abuse being the most common (28.6%) followed by a request for payments or bribes (24.2%).[22]
The higher prevalence of any DA found in this study may be due to the fact that only 4–6 weeks postpartum females were included which greatly reduces reporting bias (inability to recall). The different rates of DA in these two studies may also reflect the urban–rural differentials in health delivery systems of India.
There have been reports of treating disrespectful maternal care as “normal” and part of an age-old process by health providers and also by women undergoing such treatment.[2] In a study done in Pakistan, researchers have reported that objective DA occurred during childbirth for almost all women (99.7%), but only 27.2% reported experiencing the same.[23] Sando et al. have also reported “’normalization” of DA in their study conducted in urban Tanzania.[18] In this study also, “normalization” of DA is evident by the fact that 89.1% of females with any DA did not perceive humiliation even though they had encountered some or other manifestations. Such normalization not only contributes to increased prevalence of the problem but also renders it to “iceberg phenomenon” by way of nonrecognition and underreporting.
In this study, nonconsented care was the most common manifestation of DA (71.1%). A majority of the females reported receiving episiotomy without consent. Although consent for major procedures such as caesarean section is usually taken, minor obstetrical procedures such as episiotomy or application of ventouse/forceps are carried out without patient information or consent as they are assumed to be performed as need arises and in the best interest of the patients. Okafor et al.[12] have also reported nonconsented care to be the most prevalent type of DA among females of Nigeria. Reportedly, interviewees from Latin American countries, sub-Saharan Africa, and Eastern Europe regions have confirmed the lack of routine patient information communication and consent protocols for obstetric procedures in their respective settings, including the widespread practice of episiotomy without patient notification or consent.[2]
DA reported by women did not differ significantly by age group, religion, education, and parity in this study. Similar findings have been reported by another study done in urban slums of Lucknow, India.[24] Okafor et al. have also reported that maternal characteristics such as age, parity, and educational status did not affect prevalence of DA significantly.[12]
Among the various sociodemographic determinants of DA, SES was found to be a significant one, with odds 3.6 times more among females with low SES. Other researchers have reported similarly.[23] Health providers may treat lower SES females poorly as they are less likely to report it or reply back. On the other hand, some authors have found that females belonging to higher wealth quintiles reported more mistreatment.[24] Females of higher SES may have more expectations from facility and are more likely to be sensitive to their needs and behavior meted out to them.
No significant association was found between the time of delivery (daytime or night) and DA in this study. Similar to our finding, Banks et al.[14] found that women who delivered at night were less likely to report DA than those who delivered during day, but the difference was not significant. The risk of DA increased to 4.5 times among the females who did not take decision of birth place themselves. The ability to choose the birthing facility of their choice by the females reflects their empowerment which has been shown to be a significant determinant of DA by many other researchers as well.[19,24]
The risk of reported DA in public health facilities was twice that in private health facilities. At the same time, it was found to be almost three times more likely by health providers like auxiliary nurse midwife (ANM) or staff nurse than by doctors. Similar findings have been reported by Hameed et al.[19] This may be because of higher patient load and unfavorable patient–provider ratio in public hospitals.
Keeping in mind the fact that in India the majority (68.8%) of population is rural,[25] where childbirth care is mostly provided by public health facilities such as primary health centers and community health centres, and health providers are peripheral health workers like ANMs and staff nurse rather than doctors, and where mostly vaginal births are taking place, it becomes apparent that it is the cohort of poor, rural females delivering in public health facilities, undergoing vaginal births at hands of providers other than doctors who are most at risk of experiencing DA. These are also the same females who are more at risk of maternal mortality, which has been shown to be higher among rural area than urban in India. Urban–rural differentials in proportion of deliveries attended by skilled health personnel are also high. In 2013, at all-India level, in rural areas, 84.1% and in urban areas 98.2% of live births were attended by skilled health personnel. In Uttar Pradesh, these same figures were 67.3% in rural and 95.3% in urban areas.[26] DA during childbirth may further these differentials by discouraging uptake of childbirth services. Many studies have reported females citing lack of RMC as a reason for not seeking facility-based childbirth.[15] In this study also, this finding is reciprocated, with more than 90% females among those not wanting to attend facility in future pregnancies reporting any form of DA.
The strengths of the study include that it was conducted in community setting which has more external validity than a hospital-based study. Females may be more inclined to share negative experiences in their own homes rather than on facility grounds.[13] In addition, it was done in 4–6 weeks postpartum females, a time frame which greatly reduces recall bias and at the same time minimizes stress on newly delivered females, who are already overwhelmed by newborn care and their own immediate postpartum problems. Newly discharged mothers are likely to be relieved to have given birth safely and may feel grateful to the facility but they may reevaluate their experience in the subsequent weeks.[18]
This study has limitations in that it does not explore the system-based drivers of DA, perceptions, and limitations from the provider's point of view, which has been shown to be an important link in the framework of occurrence of DA.[27]
To conclude, DA during facility-based childbirth is evidently a major problem in rural India and should be addressed to improve the quality of maternal care, increase rates of utilization of maternal and childbirth services, and realize the rights of every female to RMC. Further mixed-methods studies are required to understand the complex and interactive patient–provider context of DA which may provide ways of reducing and eliminating the same.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors thank all the participants of the study for their co-operation.
References
- 1.Freedman LP, Ramsey K, Abuya T, Bellows B, Ndwiga C, Warren CE, et al. Defining disrespect and abuse of women in childbirth: A research, policy and rights agenda. [Last cited on 2018 Jun 20];Bull World Health Organ [Internet] 2014 92:915–7. doi: 10.2471/BLT.14.137869. Available from: http://www.ncbi. nlm.nih.gov/pubmed/25552776 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth report of a landscape analysis. Harvard Sch Public Heal Univ Res Co, LLC [Internet] 2010. pp. 1–57. Available from: http://www.urc-chs.com/uploads/resourceFiles/Live/RespectfulCareatBirth9-20-101Final.pdf .
- 3.Sen G, Reddy B, Iyer A. Beyond measurement: The drivers of disrespect and abuse in obstetric care? Reproductive Health Matters. 2018:1–13. doi: 10.1080/09688080.2018.1508173. DOI:10.1080/09688080.2018.1508173. [DOI] [PubMed] [Google Scholar]
- 4.Bohren MA, Hunter EC, Munthe-Kaas HM, Souza J, Vogel JP, Gülmezoglu A. Facilitators and barriers to facility-based delivery in low- and middle-income countries: A qualitative evidence synthesis. Reprod Health. 2014;11:71–88. doi: 10.1186/1742-4755-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balde MD, Diallo BA, Bangoura A, Sall O, Soumah AM, Vogel JP, et al. Perceptions and experiences of the mistreatment of women during childbirth in health facilities in Guinea: A qualitative study with women and service providers. Reprod Health [Internet] 2017. pp. 1–13. Available from: http://dx.doi.org/10.1186/s12978-016-0266-1 . [DOI] [PMC free article] [PubMed]
- 6.Khosla R, Zampas C, Vogel JP, Bohren MA, Roseman M, Erdman JN. International Human Rights and the Mistreatment of Women During Childbirth. [Last accessed on 2018 Oct 27];Health Hum Rights. 2016 18:131–43. [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. WHO | Prevention and elimination of disrespect and abuse during childbirth [Internet] 2017. [[cited 2018 Jun 27]]. Available from: http://www.who.int/reproductivehealth/topics/maternal_perinatal/statement-childbirth/en/
- 8.Diniz SG, Salgado HO, Andrezzo HFA, Carvalho PGC, Carvalho PCA, Aguiar CA, et al. Abuse and disrespect in childbirth care as a public health issue in Brazil: Origins, definitions, impacts on maternal health, and proposals for its prevention. J Hum Growth Dev. 2015;25:377–84. [Google Scholar]
- 9.White Ribbon Alliance; 2011. Respectful Maternity Care: The Universal Rights of Childbearing Women. [Google Scholar]
- 10.Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One. 2015;10:1–13. doi: 10.1371/journal.pone.0123606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women's intent to use maternity service in Bahir Dar, Ethiopia. [[cited 2018 Sep 29]];BMC Pregnancy Childbirth [Internet] 2018 18:1–9. doi: 10.1186/s12884-018-1909-8. Available from: https://bmcpregnancychildbirth.biomedcentral.com/track/pdf/10.1186/s12884-018-1909-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okafor II, Ugwu EO, Obi SN. Disrespect and abuse during facility-based childbirth in a low-income country. Int J Gynecol Obstet [Internet] 2015;128:110–3. doi: 10.1016/j.ijgo.2014.08.015. Available from: http://dx.doi.org/10.1016/j.ijgo. 2014.08.015 . [DOI] [PubMed] [Google Scholar]
- 13.Kruk ME, Kujawski S, Mbaruku G, Ramsey K, Moyo W, Freedman LP. Disrespectful and abusive treatment during facility delivery in Tanzania: A facility and community survey. 2018;33:e26–33. doi: 10.1093/heapol/czu079. [DOI] [PubMed] [Google Scholar]
- 14.Banks KP, Karim AM, Ratcliffe HL, Betemariam W, Langer A. Jeopardizing quality at the frontline of healthcare: Prevalence and risk factors for disrespect and abuse during facility-based childbirth in Ethiopia. Health Policy Plan. 2018;33:317–27. doi: 10.1093/heapol/czx180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moyer CA, Adongo PB, Aborigo RA, Hodgson A, Engmann CM. “They treat you like you are not a human being”: Maltreatment during labour and delivery in rural northern Ghana. Midwifery [Internet] 2014;30:262–8. doi: 10.1016/j.midw.2013.05.006. Available from: http://dx.doi.org/10.1016/j.midw. 2013.05.006 . [DOI] [PubMed] [Google Scholar]
- 16.Chattopadhyay S, Mishra A, Jacob S. “Safe”, yet violent ? Women's experiences with obstetric violence during hospital births in rural Northeast India. Cult Health Sex [Internet] 2018;20:815–29. doi: 10.1080/13691058.2017.1384572. Available from: http://doi.org/10.1080/13691058.2017.1384572 . [DOI] [PubMed] [Google Scholar]
- 17.Mumbai: International Institute of Population Sciences; 2000. IIPS and Macro International. National Family Health Survey (NFHS-2), 1998-99: India. [Google Scholar]
- 18.Sando D, Ratcliffe H, McDonald K, Spiegelman D, Lyatuu G, Mwanyika-Sando M, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth [Internet] 2016. pp. 1–10. Available from: http://dx.doi.org/10.1186/s12884-016-1019-4 . [DOI] [PMC free article] [PubMed]
- 19.Hameed W, Avan BI. Women's experiences of mistreatment during childbirth: A comparative view of home- and facility-based births in Pakistan. PLOS One. 2018:1–17. doi: 10.1371/journal.pone.0194601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mesenburg MA, Victora CG, Jacob Serruya S, Ponce de León R, Damaso AH, Domingues MR, et al. Disrespect and abuse of women during the process of childbirth in the 2015 Pelotas birth cohort. [[cited 2018 Sep 17]];Reprod Health [Internet] 2018 Dec 27;15:54. doi: 10.1186/s12978-018-0495-6. Available from: https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-018-0495-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sando D, Abuya T, Asefa A, Banks KP, Freedman LP, Kujawski S, et al. Methods used in prevalence studies of disrespect and abuse during facility based childbirth: Lessons learned. Reprod Health. 2017;14:1–18. doi: 10.1186/s12978-017-0389-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sudhinaraset M, Treleaven E, Melo J, Singh K, Diamond-smith N. Women's status and experiences of mistreatment during childbirth in Uttar Pradesh: A mixed methods study using cultural health capital theory. BMC Pregnancy Childbirth [Internet] 2016. Available from: http://dx.doi.org/10.1186/s12884-016-1124-4 . [DOI] [PMC free article] [PubMed]
- 23.Azhar Z, Oyebode O, Masud H. Disrespect and abuse during childbirth in district Gujrat, Pakistan: A quest for respectful maternity care. Ann Glob Heal [Internet] 2017;83:108. doi: 10.1371/journal.pone.0200318. Available from: http://dx.doi.org/10.1016/j.aogh. 2017.03.240 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diamond-Smith N, Treleaven E, Murthy N, Sudhinaraset M. Women's empowerment and experiences of mistreatment during childbirth in facilities in Lucknow, India: Results from a cross-sectional study. 2017;17(Suppl 2) doi: 10.1186/s12884-017-1501-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Census of India 2011 [Internet] [cited 2018 Jun 27]. Available from: http://censusindia.gov.in/2011-prov-results/paper2/data_files/india/Rural_Urban_2011.pdf .
- 26.National Institute of Public Cooperation and, Child Development, New Delhi. An analysis of levels and trends in maternal health and maternal mortality ratio in India [Internet] New Delhi: 2015. [[cited 2018 Jun 20]]. Available from: http://nipccd.nic.in/reports/mhmm.pdf . [Google Scholar]
- 27.Freedman LP, Ramsey K, Abuya T, Bellows B, Ndwiga C, Warren CE, et al. Defining disrespect and abuse of women in childbirth: A research, policy and rights agenda. 2014:915–7. doi: 10.2471/BLT.14.137869. March. [DOI] [PMC free article] [PubMed] [Google Scholar]


