Abstract
Objectives:
(1) To determine the prevalence of chronic pain of musculoskeletal origin at different body sites among elderly (≥60 years). (2) To study the determinants of chronic pain and the healthcare seeking behavior among elderly with chronic pain. (3) To explore the perceptions of chronic pain among elderly.
Materials and Methods:
This study was done in 55 field practice villages of the Rural Health Training Centre (RHTC) of the Department of Community Medicine, SMVMCH, Puducherry. An Exploratory Mixed-Method study design, where a qualitative phase (in-depth interviews [IDI]) followed the quantitative phase (Survey). A representative sample of 850 respondents was selected by two-stage cluster sampling. A trained investigator did a house-to-house visit and interviewed selected elderly respondents by using predesigned and pretested questionnaire. The intensity of chronic pain was measured using the Functional Rating Scale and Numeric Rating Scale. The manual content analysis was done for qualitative data. Multiple logistic regression was performed on quantitative data.
Results:
Qualitative data were described under two broad themes: (1) perceptions of elderly people about chronic pain and 2) healthcare seeking and coping mechanisms. Prevalence of chronic pain among the elderly respondents was found to be 47.6%. Most common site for chronic pain was knee joint (64.5%) followed by a low backache (21.7%). Most of the older people with chronic pain had mild-to-moderate and tolerable pain. Two predictors for chronic pain were the age of the respondent (adjusted OR -1.03, 95% CI = 1.01–1.05) and the presence of at least one chronic morbidity (adjusted OR -1.37, 95% CI = 1.03–1.82).
Conclusions and Recommendations:
Since the chronic pain was found to be associated with aging and the presence of at least one of the chronic morbidities, it is crucial for treating community physicians to consider the comorbid conditions while managing chronic pain in elderly. Considering the complex nature of chronic pain in old age, the primary care physician should be trained in drug and context-specific nondrug interventions to address the biomedical causes and other cognitive-behavior factors, respectively, through active support from their family and neighborhood.
Keywords: Chronic pain, India, old age, pain assessment, rural
Introduction
Chronic pain is defined as a painful experience that continues for more than a period of 6 months. Studies in the west found its prevalence to range from 50% to 75% among elderly[1] The elderly population tends to differ with a younger population with respect to physiological, psychological, and socioeconomical characteristics. The high prevalence of other comorbid conditions among elderly further increases the challenges in pain management. Hence, they require a different pain management approach.[2] Studies in the west have shown that it is important to study chronic pain experience among older people and explore their coping strategies for its effective pharmacological and nonpharmacological management.[3]
The impact of chronic pain among elderly is considerable because it constitutes a health burden to patients and their economically active family members. It often leads to loss of function, independence, dignity and mobilization for the elders who experiences chronic pain.[3] Being a neglected area of research in India, there is no systematic community-based study on chronic pain of musculoskeletal origin among old people. The findings of such study would help in planning services in primary health care settings. The high frequency of chronic pain as a presentation in primary care and the majority of the patients with chronic pain are managed in primary care that drastically reduces the patients. Out-of-pocket expenditure for consultation, medicine, and travel comparing with tertiary care facility.
Hence, this study was done to (1) determine the prevalence of chronic pain of musculoskeletal origin at different body sites among elderly (≥60 years), (2) study the determinants of chronic pain and the healthcare seeking behavior among elderly with chronic pain, and (3) explore the perceptions of chronic pain among elderly.
Materials and Methods
Study area and setting: This study was undertaken in the field practice area of the Rural Health Training Centre (RHTC) of the Department of Community Medicine, Sri Manakula Vinayagar Medical College and Hospital (SMVMCH), Pondicherry. It consists of 55 villages of three Primary Health Centers (Thiruvenainallur, Iruvalpattu, and Sirumadurai) in Villupuram district in Tamil Nadu, which is 200 km southwest of state capital Chennai. The area has a total population of 90,794 in 27,177 households. Overall, life expectancy in Tamil Nadu is 68.9 years. In Villupuram district, the overall adult literacy rate in rural areas of Villupuram district is 69.59% and 91.79% of the population are Hindu as per census data 2011. The main occupations of the people of the Villupuram district are agriculture, laborers, and household workers.[4]
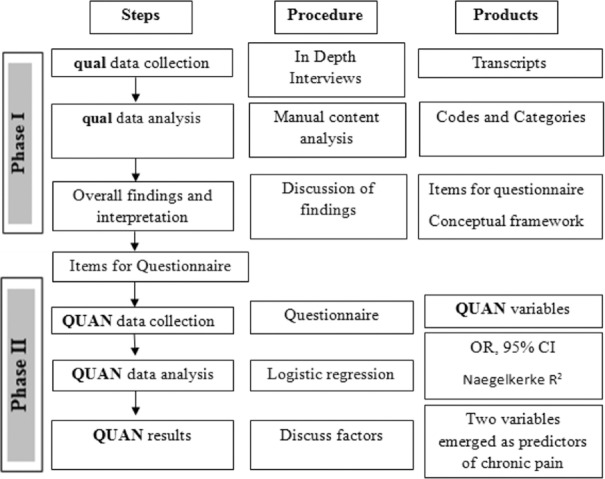
Study design: This study was an Exploratory Mixed-Method study design [Figure 1], where a qualitative phase (in-depth interviews [IDIs]) followed the quantitative phase (Survey) was used.[5]
Figure 1.
Visual diagram of the study design
Phase-I: Presurvey qualitative research (qual)
Presurvey, IDIs were undertaken with a purposively selected sample of 10 vocal and willing elders (>60 years) who were currently experiencing chronic pain (>6 months duration). The elders were identified from the Out Patient Department of RHTC and Thirubhuvanai Primary Health Centre.
The purpose of the IDIs was to explore the perceptions of the elders on chronic pain and their treatment seeking behavior. The findings from IDIs were expected to benefit in the survey instrument development for this study.
After obtaining informed consent, interviews were conducted at their home at a time convenient to the participants. A male investigator trained in qualitative research techniques conducted the interviews by using a semistructured guideline using broad open-ended questions. Interviews were conducted in the local regional language Tamil. Interviews were started by “briefing” the participant about the purpose of the study. The interviews lasted for approximately 45–60 min. Out of 10 interviews, two interviews were done in two meetings. At the end, the participant was “debriefed”on the recorded information to ensure participant validation. After completion of the discussions, the respondents were provided with the refreshments.
Observations were recorded as field notes. Interviews were audio-recorded and transcribed as Verbatim at the earliest. Since it was a “theoretically driven” sample, the transcript of the previously done interview was reviewed before planning the next interview. IDIs were undertaken until the point of saturation, i.e., until they stopped yielding any new information.[6]
Phase-II: Quantitative research – Survey (QUAN)
Sample size: An estimate of the proportion of elderly suffering from chronic pain was taken as 0.5 (as no previous study was available). Thus, considering p-0.5, design effect-2, the relative error in the estimated prevalence as 10%, the sample size 769 (Calculated by Epi_Info version 6.04d) was required. It was further inflated by 10% to cover nonresponse rate. Thus, the final sample size was 850 elderly people (>60 years).
Study population and duration: The respondents who participated in the study were the elders (≥60 years). The data were collected between the months of July 2014 and March 2015.
Sampling: Two-stage cluster sampling technique was adapted to select the required sample for the study. At the first stage, 30 clusters were selected by population proportional to size method from the list of villages (55), after calculating the cluster interval (2,131), a random number (1,082) was generated by using a random number generator in Epi_Info software.
At the second stage, 29 elders (>60 years) were identified from each selected cluster by “random walk” method. The random walk method was done in two steps, the first step was to select the starting point from the village and it was done after identifying the center of the village from there by rotating a pen and followed the direction shown by the tip of the pen. The second step was done to select the house that was performed by writing the house number on pieces of paper and randomly drawing one piece of paper for selecting the first house and the following houses were subsequently selected in clockwise direction till the desired sample is achieved.[7] In case, two or more elders were present in a particular household the eldest person was selected for this study.
Data collection and measurements: Based on the findings from qualitative data, a locally relevant questionnaire was developed. The questionnaire included information on sociodemographic details, chronic pain sites, healthcare seeking, preferred treatment, and home remedies. The draft questionnaire was pilot tested on a convenient sample of 30 elderly respondents in the area other than the study site by using a “conventional pilot testing technique.” It was then revised to improve the comprehension of questions, response options, order. and wordings in the questions.
The data were collected by the trained male investigator (Postgraduate) in Community Medicine who has been certified in a course called as “Essentials of Palliative Care” offered by Indian Association of Palliative Care (IAPC). The investigator paid house-to-house visit and interviewed the selected respondent.
After obtaining the informed consent, interviewer collected the information using the predesigned and pretested questionnaire. A survey was done in the evening hours when most of the elders and their caregivers were available. To begin with, respondents were asked about their sociodemographic details, such as age, gender, education, occupation, socioeconomical status, marital status, living arrangements, and membership in self-help groups and benefits of other social security schemes. Respondents were enquired if they had any chronic musculoskeletal pain of more than 6-month duration.
Later, respondents, who reported having a chronic pain at the time of the survey, were asked to identify the sites of their pain from the front and back view of human body pictures provided in the questionnaire. Information on aggravating, relieving factors, and current healthcare seeking for chronic pain was collected. Later, among those who had a chronic pain, the functionality and intensity of pain for each of the reported site was assessed by using functional rating scale (FRS) and numeric rating scale (NRS), respectively, having sensitivity and specificity of 80% each.[8]
The effect of pain on the restriction of day-to-day activities was assessed by using FRS. Respondents’ were instructed to grade the level of restriction of their daily activities on a scale of 0–5 [0 = no pain, 1 = tolerable (and does not prevent any activities), 2 = tolerable (but does prevent some activities), 3 = intolerable (but can use telephone, watch TV or read), 4 = intolerable (but cannot use the telephone, watch TV, or read because of pain), 5 = intolerable (and unable to verbally communicate because of pain)].
While administering NRS, the respondents’ understanding of the digit from 0 to 10 was checked by the interviewer. The tool was administered verbally, where respondents were instructed in their local language that the number 0 corresponded to no pain and 10 corresponded to the worst pain they had experienced before. Then, the respondent was asked to indicate the numeric value on the scale that best described their pain intensity.
The old people with chronic pain were asked about their health care seeking and coping mechanisms. Healthcare seeking is defined as any attempt by the elder to obtain an expert opinion from a biomedical health care provider outside the home, such as government health care facilities, private healthcare providers, and practitioners of Indian System of Medicine. Coping mechanisms were patients’ own initiatives to reduce the pain.[2]
Ethical issues: Ethical principles such as respect for the persons, beneficence, and justice were adhered. This study was cleared by the Research Committee of SMVMCH and the Institutional Ethics Committee of SMVMCH, Pondicherry.
Analysis of qualitative and qualitative data and reporting: Manual content analysis of qualitative data was done. The analysis was done at textual level analysis and it included both the inductive and deductive codes derived from the transcripts. Later, similar codes were merged together to form the categories, then the related categories were grouped into themes. Content analysis was done by two researchers to increase the “trustworthiness” of the results. Any discrepancy between the two was resolved by mutual discussion.[9] Text lines written in Italic font in the results signifies direct quotation from the participants and the text lines in square brackets are the authors’ words. Names used in this manuscript for respondent's direct quotation are fictitious.
The quantitative data were entered and analyzed using SPSS 12.0.1 software (SPSS Inc., Chicago, IL, USA) package. Chi-square (χ2) test was applied to proportions to test the level of significance. The intensity of pain was classified as mild pain (1, 2, and 3), moderate pain (4, 5, 6, and 7) and server pain (8, 9, and 10) in NRS. Multiple logistic regression was done to identify the combinations of variables that the best predicts the risk of the development of chronic pain. Twelve predictors were entered the model using the “Enter” selection method. The multiple coefficients of determination (R2) was used as the goodness-of-fit statistic for the model. The level of significance was fixed at 0.05. The guidelines for reporting mixed methods studies were followed for reporting of this study.[10]
Results
Ten elderly respondents (five male and five female) with chronic pain were purposively chosen for IDI. All respondents were >60 years, four respondents were from the service area of Thirubuvanai Primary Health Centre, Puducherry, and six were from Rural Health Training Centre service area at Thiruvennainallur, Villupuram District, Tamil Nadu. The highest educational level of the participants was up to elementary school (8th standard). Agriculture and animal rearing were their major occupations.
The result of the 10 IDIs was described under two key themes: (1) perceptions of older people about pain and (2) healthcare seeking. There were five categories under the theme of “perceptions of chronic pain.” These were (1) meaning for chronic pain, (2) perceived reasons for chronic pain, (3) perceived aggravating, (4) relieving activities, and (5) effect of chronic pain in their life. There were four categories under the theme of “healthcare seeking practices.” These categories were about various treatment options commonly used by them, such as (1) Home remedies; (2) Allopathic medicine; (3) Ayurveda, Yoga, Unani, Siddha, and Homeopathy (AYUSH); and 4) Physiotherapy.
Theme-1: Perceptions of chronic pain: The respondents’ perception of chronic pain was grouped broadly under following five categories.
Category 1: Meaning of chronic pain
They felt it as a sense of discomfort and an indicator of their health status. Some of them mentioned the pain as unpleasant feelings, heavy burden on their life, and an experience that reminds the most sorrowful part of their life. Some of them felt that it is an indicator of their poor physical and psychological health. Mr. Ramarajan, a 80-year-old man, described it in his words as, “Pain is a trouble for me. Pain is a bad feeling which is felt in my body. It's connected with both mind and body. It is the most painful part of my life.”
Category 2: Perceived reasons for chronic pain
2.1 Subcategory: Senility
Almost all the participants perceived that their old age is responsible for their pain due to a progressive decline in stamina and strength. Mrs. Punitha, a 62-year-old female patient, explained as, “My bones have eroded well because of my old age. This is the main reason that I have pain all over my body.”
2.2 Subcategory: Presence of comorbidities
Few pointed out that the presence of comorbidities, such as diabetes, hypertension, and bone illness were responsible for chronic pain. Mr. Krishna, a 63-year-old man, told that “I am diabetic and hypertensive. I was under regular treatment. But whenever my blood pressure shoots up I feel more pain in my neck.”
2.3 Subcategory: Social and spiritual causes
Respondent attributed the cause of their pain to their sins in their past life and even in the current life. Mr. Ramarajan, an 80-year-old man, described it in his words as, “Reason for my pain, many people says it is because of old age, but I believe that it could be due to my sins which I did in my young age. I betrayed my wife when I was young. I feel that is responsible for the suffering that I have now.”
Category 3: Chronic pain aggravating activities
Factors that aggravate their chronic pain were physical activities and environmental influences.
3.1 Subcategory: Physical activity and environmental factors
Strenuous and more physical activities, long walks and indulgence in sexual activities were said to aggravate the chronic pain. Noisy environment, winter season, sunny weather was perceived to contribute to pain.
Category 4: Chronic pain-relieving activities
Factors that relieve their chronic pain were medications, diet, and family support, intimacy with a neighbor.
4.1 Subcategory: Medications and diet
Pain reducing tablets, injections, regular intake of prescribed medication was found to be useful in reducing their pain. According to some respondents, proper meals reduce the pain and fasting increase the intensity of pain. Some of them reported avoiding potato, yam and other roots and tubers that grow under the earth's surface. One of the respondents said, “I used to drink kasayam [Home made syrup prepared from herbal plants] and avoid all roots and tubers like a potato when the pain was severe.”
4.2 Subcategory: Family and neighborhood support
Family and neighborhood support was useful to help them to cope up with chronic pain. “Sharing with my neighbours and chatting with them keeps me not to think about my pain.”
Category 5: Effects of chronic pain
The majority of them told their physical movements were restricted and they were dependent on others. This led to their less involvement in family programs, festivals, and recreational activities. Mrs. Poongothai, a 62-year-old lady, describes it as, “Any work which involves my knee is painful to me. Find difficult to be in Squatting position, kneeling down to clean utensils and to wash clothes. Sometimes I expect support from my family members.”
Theme 2: Health care seeking
Category 6: Home remedies
Respondents reported using home remedies at some point of time in their life for chronic pain. Turmeric powder with Elavan Thanzhai(Acalypha indicia), Neem oil mixed with coconut oil application was commonly used home remedies.
Category 7: Allopathic medicine
Many of the participants were using Allopathic medicine. They narrated that allopathic drugs relieve the pain completely though these are expensive and produces some side effects. They preferred analgesic injections over tablets as it offers quick pain relief. They prefer hospital with simple buildings and avoid multistoried buildings with staircases, lifts, and complex referral systems. Mr. Mannar, a 60-year-old man, said that.
“If I go private hospitals they ask us to go, here and there to put seat [registration] and finding the room in that huge building is another problem. They will also ask us to stay in the hospital. So it will take my entire time and my half-day will be spent in that hospital”.
Category 8: AYUSH
The majority of the participants could not distinguish between Siddha and Ayurveda system and very few told that they knew about the homeopathic system of medicine. Very few of them were taking AYUSH system of medicine for their pain management. They were doubtful of its credibility and availability of the genuine AYUSH practitioner.
Category 9: Physiotherapy
The main reason for practicing physiotherapy it is a non-pharmacological therapy. But, the lack of trained physiotherapist and electric power is the major limitation of it in rural areas.
“I went to take current treatment once it was really pain relieving to me, they asked me to come another day. But I was waiting for a few hours due to loss of power supply so I couldn’t able to continue that treatment”.
Results of the Quantitative Survey
Out of 850 respondents, 405 (47.6%) reported to have chronic pain of more than 6 months, among them, 178 (46.3%) were males and 227 (48.7%) were females. There was no significant sex difference seen.
As seen Table 1, out of 850 respondents, 384 (45.2%) were male and remaining 466 (54.8%) were female. The mean age of the respondents was 66.99 (±7.01) years, where the mean age of the male 67.85 (±7.08) years and for female respondents 66.29 (±6.89) years. About 447 (52.6%) were “below the poverty line.” Noteworthy, 392 (46.1%) respondents had a health insurance, which was significantly higher among male (54.2%) than female (45.8%) (P = 0.001). About 586 (68.9%) respondents were married, 219 (25.8%) were widowed. Female 182 (39.1%) were significantly more than male 37 (9.7%) in those widowed (P = 0.001). Among the total respondents, 425 (50%) lived with family and 92 (10.2) lived alone. Considering the above, male (60.4%) respondents living with the family was significantly more than female (41.4%) (P = 0.001). Significantly more female (14.4%) lived alone than male (6.5%) (P = 0.001). Around 378 (44.5%) were illiterate, female (56.4%) was significantly more than male (29.9%) (P = 0.001). From the total respondents, 280 (33%) were doing agricultural work and 230 (27.1%) were not working. Significantly more male (38.1%) were doing agricultural works than female (12.7%) (P < 0.001). Among the total respondents, 773 (90.9%) were Hindus, 57 (6.7%) were Muslims, and 20 (2.4%) belonged to Christianity. About 106 (12.5%) elderly were receiving a pension at the time survey. Nearly, 19 (2.1%) respondents had membership in self-help groups. Out of 850 respondents, 336 (39.5%) reported to be addicted to tobacco and 87 (10.2%) reported they are addicted to alcohol. Significantly more male was addicted to tobacco and alcohol consumption compared to females. (P < 0.05).
Table 1.
Background characteristics of the respondents
| Characteristics | Male (384) | Female (466) | Total (850) |
|---|---|---|---|
| Average age of respondents (mean±SD) | 67.85±7.08 | 66.29±6.89 | 66.99±7.01 |
| Ration card | |||
| Below poverty line | 201 (52.3) | 246 (52.8) | 447 (52.6) |
| Health insurance | |||
| Yes | 208 (54.2) | 184 (45.8) | 392 (46.1) |
| Marital status | |||
| Married* | 324 (84.6) | 260 (55.9) | 586 (68.9) |
| Widowed* | 37 (9.7) | 182 (39.1) | 219 (25.8) |
| Living with | |||
| Family* | 232 (60.4) | 193 (41.4) | 425 (50) |
| Living alone* | 25 (6.5) | 67 (14.4) | 92 (10.8) |
| Years of education | |||
| Illiterate* | 115 (29.9) | 263 (56.4) | 378 (44.5) |
| Occupation | |||
| Agricultural work* | 146 (38.1) | 59 (12.7) | 205 (24.1) |
| Not working | 96 (25.1) | 134 (28.8) | 231 (27.1) |
| Religion | |||
| Hindu | 346 (90.1) | 427 (91.6) | 773 (90.9) |
| Muslim | 25 (6.5) | 32 (6.9) | 57 (6.7) |
| Christian | 13 (3.4) | 7 (1.5) | 20 (2.4) |
| Pension | |||
| Yes | 44 (11.5) | 62 (13.3) | 106 (12.5) |
| Membership in self-help groups | |||
| Yes | 8 (2.1) | 10 (2.2) | 19 (2.1) |
| Addictions | |||
| Tobacco products* | 167 (43.5) | 169 (36.3) | 336 (39.5) |
| Alcohol* | 81 (21.1) | 6 (1.3) | 87 (10.2) |
SD: Standard deviation. Figures in parenthesis are percentages. *P<0.05
As seen in Table 2, out of 405 respondents who reported to have chronic pain, 10 (2.3%) had headache, 28 (6.6%) had neck pain, 32 (7.5%) had shoulder pain, 8 (1.9%) had chest pain, 73 (17.1%) had hip joint pain, 92 (21.7%) had low back ache, 7 (1.7%) had hand pain, 13 (3.1%) had thigh pain, 274 (64.5%) had knee pain, 5 (1.2%) had calf muscle pain, 8 (1.9%) had ankle pain, and 10 (2.4%) had foot pain. Significantly more female 61 (25.4%) had low backache than male 31 (16.8%) (P = 0.024).
Table 2.
Sites of chronic pain among male and female respondents (multiple responses)
| Sites | Male (178) | Female (227) | Total (405) |
|---|---|---|---|
| Head | 2 (1.1) | 8 (3.3) | 10 (2.3) |
| Neck | 8 (4.3) | 20 (8.4) | 28 (6.6) |
| Shoulder | 14 (7.6) | 18 (7.5) | 32 (7.5) |
| Chest | 3 (1.6) | 5 (2.1) | 8 (1.9) |
| Hip | 28 (15.1) | 45 (18.6) | 73 (17.1) |
| Low back* | 31 (16.8) | 61 (25.4) | 92 (21.7) |
| Hand | 2 (1.1) | 5 (2.1) | 7 (1.7) |
| Thigh | 7 (3.8) | 6 (2.5) | 13 (3.1) |
| Knee | 128 (69.6) | 146 (60.6) | 274 (64.5) |
| Calf muscle | 2 (1.1) | 3 (1.2) | 5 (1.2) |
| Ankle | 3 (1.6) | 5 (2.1) | 8 (1.9) |
| Foot | 4 (2.2) | 6 (2.5) | 10 (2.4) |
Figures in parenthesis are percentages. *P<0.05
The major pain aggravating factors were mild activities 110 (25.8%), heavy work 369 (86.4%), and depression 250 (58.5%). The other aggravating factors were loss of family support (7.3%) and inadequate sleep (6.1%). Significantly more female than male perceived pain during the depression and loss of family support. The major pain-relieving factors were medication 383 (89.7%), exercise 156 (36.5%), and rest 250 (58.5%). Significantly more male than women reported cold and rest as pain relieving factors (P = 0.014) [Table 3].
Table 3.
Frequency of aggravating and relieving factors for chronic pain (multiple responses)
| Male (178) | Female (227) | Total (405) | |
|---|---|---|---|
| Aggravating factors | |||
| Mild activity | 48 (25.9) | 62 (25.6) | 110 (25.8) |
| Heavy activity | 162 (87.6) | 207 (85.5) | 369 (86.4) |
| Cough | 3 (1.6) | 7 (2.9) | 10 (2.3) |
| Winter season* | 7 (3.8) | 1 (0.4) | 8 (1.9) |
| Hot weather | 4 (2.2) | 4 (1.7) | 8 (1.9) |
| Anxiety | 12 (6.5) | 12 (5) | 24 (5.6) |
| Depression* | 98 (53) | 152 (62.8) | 250 (58.5) |
| Loss of family support* | 8 (4.3) | 23 (9.5) | 31 (7.3) |
| Inadequate sleep | 9 (4.9) | 17 (7) | 26 (6.1) |
| Relieving factors | |||
| Medications | 167 (90.3) | 216 (89.3) | 383 (89.7) |
| Exercise | 75 (40.5) | 81 (33.5) | 156 (36.5) |
| Massage | 32 (17.3) | 45 (18.6) | 77 (18) |
| Cold (ice packs)* | 7 (3.8) | 1 (0.4) | 8 (1.9) |
| Heat compression | 6 (3.2) | 4 (1.7) | 10 (2.3) |
| Health tonics | 9 (4.9) | 10 (4.1) | 19 (4.4) |
| Rest * | 98 (53) | 152 (62.8) | 250 (58.5) |
| Consumption of Alcohol | 4 (2.2) | 2 (0.8) | 6 (1.4) |
| Chewing tobacco | 1 (0.5) | 1 (0.4) | 2 (0.5) |
Figures in parenthesis are percentages. *P<0.05
As seen in Table 4, describes the perceived intensity of chronic pain among male and female across different sites of chronic pain. Among those who had hip pain, according to the functional rating scale, 18 (9.9%) male and 32 (13.3%) female had tolerable hip pain which did not prevent any activities, 9 (4.9%) male and 13 (5.4%) female had tolerable hip pain, but had prevented some activities, One male and female each had intolerable hip pain but could make a movement to use telephone, watch TV, or read. The median score for hip pain on a numeric rating scale was 2 for both male and female. Regarding knee pain, according to the functional rating scale, 96 (51.9%) male and 104 (43.2%) female had tolerable knee pain which did not prevent any activities; 25 (13.5%) male and 39 (16.2%) female had tolerable knee pain but had prevented some activities; 5 (2.7%) male and 3 (1.2%) female had intolerable knee pain but could make a movement to use telephone, watch TV, or read; and only 2 male respondents had intolerable knee pain who could not make a movement to use cannot use telephone, watch TV, or read. The median score for knee pain on a numeric rating scale was 2 for both male and female. About 23 (12.5%) male and 41 (17.2%) female had tolerable low back pain, which did not prevent any activities; 8 (4.3%) male and 20 (8.4%) female had tolerable low back pain, which had prevented some activities. The median score for low back pain on a numeric rating scale was 2 for both male and female.
Table 4.
Comparison of chronic pain perceived intensity at different body sites using functional pain scale and numeric rating scale
| Body sites | Male (n=178) | Female (n=227) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional pain scale* | Numeric rating scale Median |
Total n |
Functional pain scale* | Numeric rating scale Median |
Total n |
||||||
| 1 | 2 | 3 | 4 | 1 | 2 | 3 | |||||
| Front side | |||||||||||
| Head | 2 (1.1) | 0 | 0 | 0 | 1 | 2 | 7 (2.9) | 0 | 0 | 2 | 7 |
| Shoulder | 9 (4.9) | 0 | 0 | 0 | 2 | 9 | 12 (5) | 0 | 0 | 2 | 12 |
| Chest | 1 (0.5) | 2 (1.1) | 0 | 0 | 3 | 3 | 4 (1.7) | 1 (0.4) | 0 | 3 | 5 |
| Hip | 18 (9.9) | 9 (4.9) | 1 (0.5) | 0 | 2 | 28 | 32 (13.3) | 13 (5.4) | 1 (0.4) | 2 | 46 |
| Hand | 2 (1.1) | 0 | 0 | 0 | 2 | 2 | 5 (2.1) | 0 | 0 | 2 | 5 |
| Thigh | 3 (1.6) | 1 (0.5) | 2 (1.1) | 1 (0.5) | 2 | 7 | 6 (2.5) | 0 | 0 | 2 | 6 |
| Knee | 96 (51.9) | 25 (13.5) | 5 (2.7) | 2 (1.1) | 2 | 128 | 104 (43.2) | 39 (16.2) | 3 (1.2) | 2 | 146 |
| Calf muscle | 1 (0.5) | 1 (0.5) | 0 | 0 | 1.5 | 2 | 3 (1.3) | 0 | 0 | 2 | 3 |
| Ankle | 1 (0.5) | 2 (1.1) | 0 | 0 | 2 | 3 | 1 (1.3) | 2 (0.8) | 0 | 2 | 3 |
| Foot | 4 (2.2) | 0 | 0 | 0 | 1.5 | 4 | 4 (1.7) | 2 (0.8) | 0 | 2 | 6 |
| Backside of the body sites | |||||||||||
| Neck | 7 (3.8) | 1 (0.5) | 0 | 0 | 1.5 | 8 | 11 (4.6) | 8 (3.3) | 1 (0.4) | 2 | 20 |
| Low back | 23 (12.5) | 8 (4.3) | 0 | 0 | 2 | 31 | 41 (17.2) | 20 (8.4) | 0 | 2 | 61 |
As seen in the Table 5, out of 391 respondents who were on medications for chronic pain management, 218 (55.7%) were taking treatment from government health care facilities, 138 (35.2%) were taking treatment from private healthcare facilities, and 35 (8.9%) were taking medicines over the counter.
Table 5.
Healthcare seeking for chronic pain
| Health care facilities | Male (169) | Female (222) | Total (391) |
|---|---|---|---|
| Government healthcare facilities | 93 (55) | 125 (56.3) | 218 (55.7) |
| Private healthcare facilities | 60 (35.5) | 78 (35.1) | 138 (35.2) |
| Over the counter | 16 (9.4) | 19 (8.5) | 35 (8.9) |
Figures in parenthesis are percentages
As seen in Table 6, out 405 respondents who had chronic pain, 365 (90.1%) were seeking Allopathic treatment, 4 (1%) were using Ayurveda. 4 (1%) were taking Siddha, 19 (4.7%) were receiving physiotherapy, and 115 (28.5%) were following some home-based remedies.
Table 6.
Types of medication used for management of chronic pain (multiple responses)
| Types | Male (178) | Female (227) | Total (405) |
|---|---|---|---|
| Allopathy | 160 (89.9) | 205 (90.3) | 365 (90.1) |
| Ayurveda | 3 (1.7) | 1 (0.4) | 4 (1.0) |
| Siddha | 1 (0.6) | 3 (1.3) | 4 (1.0) |
| Physiotherapy | 10 (5.6) | 9 (3.9) | 19 (4.7) |
| Home based remedies | 49 (27.7) | 66 (29.2) | 115 (28.5) |
Figures in parenthesis are percentages
In multivariate analysis, two variables emerged as significant predictors of the risk of developing chronic pain. The risk of developing chronic pain among respondents increased about 1.03 times (CI: 1.01–1.05) for a unit increase in age (P = 0.007). Those with at least one chronic morbidity were 1.37 times (CI: 1.03–1.82) at risk of developing chronic pain compared with those without chronic morbidity (P = 0.029). The Nagelkerke pseudo-R2 value for the final model was 0.032 [Table 7].
Table 7.
Final Model: Multivariate logistic regression for determinants of chronic pain
| Characters | Total (n=850) | Chronic pain (n=405) | Adjusted OR (95%CI) | P |
|---|---|---|---|---|
| Age* (Continuous variable) | ||||
| ≥60 years | 850 | 405 (47.6) | 1.03 (1.01-1.05) | 0.007 |
| Chronic morbidity* | ||||
| No chronic morbidity | 464 | 206 (48.4) | 1 (1) | 0.029 |
| At least one chronic morbidity | 386 | 199 (51.5) | 1.37 (1.03-1.82) |
Figures in parenthesis are percentages. *P<0.05
Discussions
Overall, this study explored the elders’ perceptions of chronic pain, healthcare seeking, and their coping mechanism. The prevalence of chronic pain among the respondents (elderly ≥60 years) was found to be 47.6% in this study. The knee joint (64.5%) was the most commonly reported site for chronic pain among the elderly. The low back ache was significantly high among females. Heavy activities (86.4%), such as lifting heavy objects, washing clothes, climbing stairs, etc., were commonly found to aggravate their pain. A majority reported medications (89.7%) as a relieving factor. In multivariate analysis, only two variables emerged as the predictors of chronic pain. These were the age of the respondent (adjusted OR -1.03, 95% CI: 1.01–1.05) and the presence of at least one chronic morbidity (adjusted OR -1.37, 95% CI: 1.03–1.82).
In qualitative exploration, elderly with perceived chronic pain as a sign of their poor [deteriorating] health and they had an unpleasant feeling of sadness and burden [on their caregivers]. They attributed this pain to their old age, other health problems and sins in their past and current life. This finding shows the relevance of the cognitive-behavioral model of pain to older persons with chronic pain, which emphasizes that the chronic pain, in old age is a complex sensory and emotional experience.[2] Hence, to effectively manage the old person's chronic pain, the physician must carry out the comprehensive pain assessment and explore the various cognitive and behavioral influences. The qualitative research explores some pain coping methods adopted by older people to deal with or minimize their pain, which was subsequently quantified in the survey phase of research. This information is crucial for cognitive-behavior intervention, where the cognitive therapy focuses on challenges how patients perceive the pain and help them divert their thoughts away from pain and behavior therapy modify pain behavior and encourages wellness behaviors through active involvement of family caregivers and neighborhood support. The respondents expressed the need of an elderly-friendly hospital building for easy physical access and emphasized the role of family and neighborhood support in pain relief.
In this study, the prevalence of chronic pain was found to 47.6% among elderly. Pereira et al. did a population-based study in Goiania state, Brazil, reported 52.8% prevalence of chronic pain among elderly.[11] We could get two studies on pain done in India. However, these studies were done on adult population for acute pain. Majumdar et al. did a study in rural Puducherry, India, on adults (≥20 years of age) with a reference period of 7 days prior to the survey and one year.[12] Chopra et al. did a study in Pune, India, on adults (defined as 15 years of age and over) with a reference period of 7 days prior to the survey.[13]
In this study, 85.9% respondents with chronic pain reported mild pain and the rest 14.07% reported moderate pain. The majority of them had tolerable pain, indicating that this can be managed at the primary care level. Pereira et al. in Brazil found that 19.4% respondents had mild pain, 25.9% respondents had moderate pain, and 42.1% reported severe pain and 12.6% considered it as worst pain possible pain. The difference in perception of pain intensity could be due to the difference in the age structure of the selected sample, racial\cultural origin, and urban vs rural background of the sample in two these studies. According to the literature, Asian and North European patients are less expressive of their pain, while Hispanic, Middle Eastern, and Mediterranean are more likely to verbalize their expressions of pain.[14]
As found in this study, the commonly reported pain sites in the body were knee (64.5%), low back pain (21.7%), shoulder (7.5%), and neck pain in 6.6 percent. According to Pereira et al. study knee 34.5%, low back pain 29.5%, shoulder 10%, and neck 6.6%.[12] This variation of could be due to differences in the age group selection, occupation, diet, and lifestyle. In the present study, we found that 64.5% of the elders reported having chronic pain in the knee joint with no sex differentials. Another community-based study in rural Tamil Nadu found it as high as 61.3%. However, a survey in neighboring Kerala state found it relatively lower (37.5%) among old people.[15] However, the reasons for this difference need to be explored in the future studies.
In this study, the relieving factors for chronic pain were medications (89.7%), taking a rest (58.5%), mild exercises (36.5%), and massages (18%). Podichetty in Florida found that massage, ultrasound, heat compression, ice packs, compression and supplement diet, such as glucosamine-rich food items.[16] Little is known about the effectiveness of such nondrug intervention in pain management, but it was observed to help the patient to divert his mind from the pain. The relieving and aggravating factors also depend on the cause of pain.[2] This understanding of aggravating and relieving factors of chronic pain would also help us to prepare locally relevant pain education material and counselling guides for both the patients and their caregivers.
We found that the health care seeking for chronic pain was more toward the public health facilities (55.7%) followed by private health facilities (35.2%) and over the counter (8.9%). Use of allopathic medicine was universal with only one percent using the Indian System of Medicines, such as Ayurveda, Siddha, and one-third reported to use some home remedies. India's National Policy for Senior Citizens of India has recommended mainstreaming AYUSH in the healthcare system.[17]
We found that the age of the respondent (adjusted OR -1.03, 95% CI: 1.01–1.05) and the presence of at least one chronic morbidity (adjusted OR -1.37, 95% CI: 1.03–1.82) as a predictor of chronic pain among elderly. Thus, the physician managing the chronic pain must consider the other comorbid conditions while managing the chronic pain among elderly.
The Primary Care physicians play the vital role in caring for patients with chronic pain especially among elderly. Pain management is often an inadequately taught in medical course. Based on the study outcome the pain severity lies between mild-to-moderate nonmalignant chronic pain which can be managed in primary care using WHO analgesic ladder. The Primary Care Community Health-based model of service delivery includes patient-centered care delivery strategies that can improve clinical outcomes, cost, and patient and primary care provider satisfaction with services.[18] Implementing pain management approach in Primary Care setting, potentially providing a more effective, safe, and more satisfactory alternative to opioid-based chronic pain treatment.[19]
According to the best of our knowledge, this study has been first community-based mixed methods study on the prevalence of chronic pain and its determinants on a larger representative sample in a wider geographical area in a rural setting. Qualitative results reinforced the quantitative survey. Valid pain assessment tools such as FPS and NRS were used to assess the pain intensity. However, being a community-based mixed methods research of sequential type, it was a time demanding and lengthy research process. We did not explore the biomedical causes of the pain.
In conclusion, the prevalence of chronic pain among the elderly was found high. The majority of the old people had a mild type of chronic pain without much affecting their daily functional activities; hence, it can be managed in a primary care setting. The chronic pain was found to be associated with aging and the presence of at least one of the chronic morbidities; it is crucial for treating community physicians to consider the comorbid conditions in pain management among elderly. The readiness of primary care facilities in the form of drug availability, physiotherapy unit, and its elder-friendly design for ease of physical access is important. Considering the complex nature of chronic pain in old age, the primary care physician should be trained in drug and context-specific nondrug interventions to address the biomedical causes and other cognitive-behaviur factors, respectively, through active support from their family and neighborhood.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rastogi R, Meek BD. Management of chronic pain in elderly, frail patients: Finding a suitable, personalized method of control. Clin Interv Aging. 2013;8:37–46. doi: 10.2147/CIA.S30165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrel BR, Ferrell BA, editors. Seattle (USA): International Association for the Study of Pain; 1996. Pain in the Elderly: Task Force on Pain in the Elderly. [Google Scholar]
- 3.Herr AK, Garand L. Assessment and measurement of pain in older adults. Clin Geriatric Med. 2001;17:457. doi: 10.1016/s0749-0690(05)70080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.District profile format. [Online] [Last accessed on 2016 May 31]. Available from: http://shodhganga.inflibnet.ac.in/bitstream/10603/26772/7/07_chapter%202.pdf .
- 5.Bergman MM, editor. London: SAGE publications Ltd; 2009. Advances in Mixed Methods Research: Theories and Applications. [Google Scholar]
- 6.Hudleson PM. Geneva: World Health Organisation; 1994. Qualitative Research for Health Programmes. [Google Scholar]
- 7.Chromy JR. Probability Proportional to Size (PPS) sampling. SAGE research methods. 2008. [Last accessed on 2016 May 20]. [Online] Available from: https://srmo.sagepub.com/view/encyclopedia-of-survey-research-methods/n405.xml .
- 8.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain. American college of rheumatology. Arthritis Care Res. 2011;63:240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh HF. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 10.Creswell JW, Vicki L, Clark P. 2nd ed. New Delhi: Sage Publications; 2011. Designing, and Conducting Mixed Methods Research; p. 63. [Google Scholar]
- 11.Pereira LV, Vasconcelos PP, Souza LA, Pereira GD, Nakatani AY, Bachion MM. Prevalence and intensity of chronic pain and self-perceived health among elderly people: A population-based study. Rev Lat Am Enfermagem. 2014;22:662–9. doi: 10.1590/0104-1169.3591.2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majumdar A, Kumar G, Nair D, Sujiv A. Musculoskeletal complaints and predictors of Musculoskeletal pain among adults in Rural Puducherry. Indian J Palliat Care. 2015;21:121–3. doi: 10.4103/0973-1075.150206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chopra A, Saluja M, Patil J, Tandale HS. Pain and disability, perceptions and beliefs of a rural Indian population: A WHO-ILAR COPCORD study. J Rheumatol. 2002;29:614–21. [PubMed] [Google Scholar]
- 14.Campbell CM, Edwards RR. Ethnic differences in pain and pain management. Pain Manage. 2012;2:219–30. doi: 10.2217/pmt.12.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dongre AR, Rajendran KP, Kumar S, Deshmukh PR. The effect of community managed palliative care program on quality of life in the elderly in rural Tamil Nadu, India. Indian J Palliat Care. 2012;18:219–25. doi: 10.4103/0973-1075.105694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Podichetty VK, Mazanec DJ, Biscup RS. Chronic non- malignant musculoskeletal pain in older adults: Clinical issues and opioid intervention. Postgrad Med J. 2003;79:627–33. doi: 10.1136/pmj.79.937.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The government of India [Online] National Policy for Senior Citizens. Ministry of Social Justice and Empowerment. 2011. [Last accessed on 2016 May 31]. Available from: http://socialjustice.nic.in/pdf/dnpsc.pdf .
- 18.Sandoval BE, Bell J, Khatri P, Robinson PJ. Toward a unified integration approach: Uniting diverse primary care strategies under the Primary Care Behavioral Health (PCBH) Model. J Clin Psychol Med Settings. 2018;25:187–196. doi: 10.1007/s10880-017-9516-9. [DOI] [PubMed] [Google Scholar]
- 19.DeBar L, Benes L, Bonifay A, Deyo RA, Elder CR, Keefe FJ, et al. Interdisciplinary team-based care for patients with chronic pain on long-term opioid treatment in primary care (PPACT)-Protocol for a pragmatic cluster randomized trial. Contemp Clin Trials. 2018;67:91–9. doi: 10.1016/j.cct.2018.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]