Abstract
Severe malaria is a concerning problem in developing country and is mostly due to Plasmodium Falciparum. Common organs involved are liver, central nervous system, lungs, kidneys, and vasculature. Cardiac involvement is very rare and is mostly underestimated. Cardiac involvement occurs in the form of myocardial dysfunction, arrhythmia, and ventricular systolic dysfunction. This is the rare case of acute pericarditis due to plasmodium falciparum mimicking as inferolateral ST elevation myocardial infarction (STEMI) due to suggestive electrocardiography (ECG) findings.
Keywords: Falciparum malaria, myocardial infarction, pericarditis
Case Description
A 40-year-old male presented with the complaint of intermittent high-grade fever since 4 days and diffuse chest pain for 3 hours. The pain was moderate in intensity and was radiating to the nape of neck. There was no history of hypertension, diabetes, dyslipidemia, and smoking. There was no history of cough, burning micturition, diarrhea, and vomiting. On examination, the patient was afebrile, and blood pressure was 130/80 mmHg with a pulse rate of 100 bpm. Chest examination was normal. Patient was admitted for further workup. Blood investigations were sent and results were pending. ECG showed ST elevation in II, I, aVL, V5, V6 [Figure 1]. Diagnosis of acute inferolateral wall STEMI was made. Patient was taken to the Cath. lab for primary angioplasty within an hour of admission. To our surprise, angiography came out be normal. Results of blood investigation showed white blood cell count was 7,000/mm3, platelet count was 60,000/mm3 indicating thrombocytopenia, hemoglobin was 10 g/dL, and blood glucose was 120 mg/dL. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were raised. Liver function tests revealed a Gamma Glutamine Transferase (GGT) of 90 IU/L, Serum glutamic oxaloacetic transaminase (SGOT) of 110 IU/L, serum glutamic pyruvate transaminase (SGPT) of 126 IU/L, and LDH of 356 IU/L. Renal function tests showed a blood urea of 56 mg/dL and a serum creatinine of 1.5 g/dL. Blood smear was positive for plasmodium falciparum. Cardiac troponin was 0.05 ng/dL. Thorough history and examination of the patient was done after the procedure. It was revealed that the patient had history of chest pain that increased on breathing and decreased on leaning forward with radiation of chest pain to the nape of the neck. Also, examination revealed faint pericardial rub and moderately enlarged spleen on abdominal examination. History and examination findings with ECG changes were suggestive of pericarditis. Moreover, on careful reading of ECG, it was noticed that ST segment elevations were concave upward and there was PR segment elevation in aVR and PR segment depression in other leads characteristic of acute pericarditis. Further, echocardiography was done and mild pericardial effusion was seen. There were no regional wall motion abnormalities and left ventricular ejection fraction was normal on echocardiography. Thereafter, pertaining to the clinical picture, it was assumed that the pericarditis was the result of involvement of heart due to severe falciparum malaria. The patient was treated with an Artemisinin combination therapy for 3 days. The patient was treated for pericarditis with ibuprofen 600 mg every 8 hours for a week and then twice a day for another week. Serial ECG was done and no dynamic changes were noticed. The patient's symptoms improved after a week. Repeat blood smear at the end of antimalarial therapy showed no evidence of malarial parasites. Patient was discharged. ECG remained same on discharge and returned to normal during follow-up after 15 days.
Figure 1.
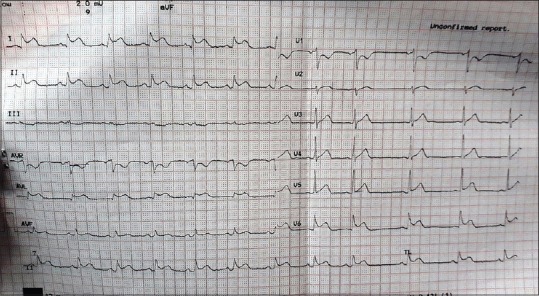
ECG showing ST elevation in II, I, aVL, V5, V6 with concavity upward and PR segment elevation in aVR and PR segment depression in other leads
Discussion
Although mortality and morbidity caused by malaria have decreased globally,[1] it is still a concerning issue in developing countries. Progression to fatal or severe malaria is largely due to Plasmodium falciparum. WHO definition for severe malaria includes multiorgan involvement with high level of parasitemia. It can present with impaired consciousness, acidosis, acute kidney injury, jaundice, pulmonary edema, significant bleeding, or shock.[2] Cardiac involvement is unrecognised and underestimated in cases of severe malaria. Cardiac involvement can occur in the form of circulatory failure due to decrease cardiac output as a result of myocardial dysfunction, arrhythmias, and congestive heart failure.[3] Nayak et al. studied cardiovascular involvement in 100 cases of acute malaria by performing clinical examination, chest X-ray, ECG, echocardiography, and measuring cardiac enzymes. They found cardiac involvement in 17% patients in the form of circulatory failure (11%), congestive cardiac failure (7%), and pulmonary edema (2%). They found nonspecific ST changes in eight patients and raised cardiac markers in seven patients suggestive of myocarditis.[4] On reviewing the literature, it was revealed that pericarditis is rare complication of acute malaria and is mostly asymptomatic and unrecognized.[5,6] However, our patient presented with typical, suggestive symptoms of pericarditis. The pathophysiology behind the pericardial involvement in acute malaria is still unclear. One possible explanation could be the direct toxic effects of proteins released by parasites and excessive production of inflammatory cytokines and immune mediators causing the inflammation and effusion.[7]
Myocardial infarction (MI) and pericarditis can be differentiated basis on thorough history, clinical examination, and ECG findings. Measurement of cardiac enzymes, basic metabolic panel, and echocardiography findings are important to confirm the diagnosis. Classic electrocardiographic changes in acute pericarditis include widespread concave upward ST-segment elevation and PR segment depression.[8] However, in some clinical scenarios, it is difficult to differentiate the two only on the basis of ECG especially in case of regional pericarditis.[9] There are three important points that has to be stressed upon that were missed in this case during the evaluation. First, inferolateral MI was suspected based on ECG changes, but ECG did not show typical contiguous lead involvement. Only lead II out of all inferior leads showed ST elevation. Also, classic ECG changes found in acute pericarditis were missed. Such ECG should have high index of suspicion for pericarditis. Second, while results of cardiac markers were awaited, it was crucial to go for angioplasty immediately to prevent the delay in reperfusion when inferolateral MI was suspected. At the same time, it is to be reinforced that echocardiography should be done before primary angioplasty as a protocol, which was not done in this case. Third, thorough history and physical examination plays an important role in early diagnosis and treatment. The chest pain in acute pericarditis is sharp retrosternal chest pain that might radiate to neck, jaw, and arms. Unlike chest pain in MI, this pain increases on inspiration and coughing and the pericardial friction rub is present in up to 85% of patients with acute pericarditis.[10] The faint pericardial rub was later detected in our case after the procedure.
It is important to keep the suspicion high for acute pericarditis when the patient presents with characteristic chest pain and ST segment changes in case of severe falciparum malaria.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.CDC - Malaria - Malaria Worldwide - Impact of Malaria [Internet]. Centres for Disease Control and Prevention. [Last cited on 2018 Jul 19]. Available from: https://www.cdc.gov/malaria/malaria_worldwide/impact.html .
- 2.CDC - Malaria - Malaria Worldwide - Impact of Malaria [Internet]. Centres for Disease Control and Prevention. [Last cited on 2018 Jul 19]. Available from: https://www.cdc.gov/malaria/malaria_worldwide/impact.html .
- 3.Ray HN, Doshi D, Rajan A, Singh AK, Singh SB, Das MK. Cardiovascular involvement in severe malaria: A prospective study in Ranchi, Jharkhand. J Vector Borne Dis. 2017;54:177–82. [PubMed] [Google Scholar]
- 4.Nayak KC, Meena SL, Gupta BK, Kumar S, Pareek V. Cardiovascular involvement in severe vivax and falciparum malaria. J Vector Borne Dis. 2013;50:285–91. [PubMed] [Google Scholar]
- 5.Colomba C, Trizzino M, Gioè C, Coelho F, Lopo I, Pinheiro P, et al. Malaria and the heart: Two rare case reports of Plasmodium falciparum associated pericarditis. J Vector Borne Dis. 2017;54:372–74. doi: 10.4103/0972-9062.225845. [DOI] [PubMed] [Google Scholar]
- 6.Franzen D, Curtius JM, Heitz W, Höpp HW, Diehl V, Hilger HH. Cardiac involvement during and after malaria. Clin Investig. 1992;70:670–73. doi: 10.1007/BF00180283. [DOI] [PubMed] [Google Scholar]
- 7.Mishra SK, Behera PK, Satpathi S. Cardiac involvement in malaria: An overlooked important complication. J Vector Borne Dis. 2013;50:232–35. [PubMed] [Google Scholar]
- 8.Tonini M, Melo DTP de, Fernandes F. Acute pericarditis. Rev Assoc Med Bras. 2015;61:184–90. doi: 10.1590/1806-9282.61.02.184. [DOI] [PubMed] [Google Scholar]
- 9.Barnes AR, Burchell HB. Acute pericarditis simulating acute coronary occlusion: A report of fourteen cases. Am Heart J. 1942;23:247–68. [Google Scholar]
- 10.Snyder MJ, Bepko J, White M. Acute pericarditis: Diagnosis and management. Am Fam Physician. 2014;89:553–60. [PubMed] [Google Scholar]


