Abstract
Tuberculosis (TB) is a cause and effect of undernutrition. Patients with active TB in India have a high prevalence of severe undernutrition, an important comorbidity, which increases the risk of mortality, serious adverse effects, relapses after cure and impairs functional status. The World Health Organization and Revised National Tuberculosis Control Programme have now recommended that nutritional assessment, counseling, and support be considered as integral parts of TB care. Nutritional assessment requires calculations of body mass index (BMI) to classify severity of undernutrition at diagnosis and ascertain nutritional recovery at follow-up. We present BMI-based field charts constructed for use by healthcare workers which obviate calculations of BMI and provide weights corresponding to BMI categories, and body weight corresponding to a desirable BMI of 21 kg/m2. These simplified BMI-based field charts will enable appropriate assessment, counseling, and monitoring of undernourished patients with active TB by peripheral health workers in programmatic settings.
Keywords: Body mass index, direct benefit transfer, nutritional assessment, tuberculosis, undernutrition
Introduction
Tuberculosis (TB) is a disease characterized by loss of weight and wasting.[1] In countries like India, malnutrition is a widely prevalent risk factor for TB which is a major driver of the TB epidemic.[2] The nutritional status at diagnosis reflects the worsening of preexisting malnutrition by active TB. In a large cohort of rural patients, the median weights and the body mass indices (BMIs) at diagnosis in adult men and women were 42 kg (16.0 kg/m2) and 34 kg (15.0 kg/m2), respectively.[3] The median weights in men and women reported in the Revised National Tuberculosis Control Programme (RNTCP) were similar, 43 and 38 kg, respectively.[4]
In the absence of nutritional support, the nutritional recovery of Indian patients with TB is incomplete with poor weight gains in the range of 3–4 kg.[3,5] Undernutrition is also a risk factor for mortality during treatment, drug toxicity, drug malabsorption, and relapse after successful cure.[6] The lack of recovery of lean body mass in patients at the end of treatment can impair their return to work. World Health Organization (WHO) recognizes undernutrition as an important comorbidity in patients with TB and recommends that nutritional assessment be an integral part of TB care.[7] RNTCP has also developed and released a guidance document for nutritional care and support of patients with TB in India in 2017.[8] It proposes a system of assessment of nutritional status, counseling, and nutritional support suitable for implementation in Indian settings.[8] Field charts for easy nutritional assessment at diagnosis and follow-up of patients with TB have been developed.[8] This article provides the technical background for these field charts and their use in the program by peripheral health staff.
Need for Simplified Field Charts
Among the available methods for assessment of nutritional status, anthropometric measurements of weight and height are the most widely used tools. WHO has recommended that BMI, which is weight standardized for height; where BMI = (weight in kg)/(height in m)2, be used for classification of nutritional status. It has suggested various categories to classify normal, underweight, overweight, and obesity in adults for nutritional classification. The RNTCP recommends measurement of height and weight at diagnosis and monthly record of weights during follow-up to monitor nutritional improvement.[8] It also recommends a daily intake of calories and proteins based on a target (desirable) body weight, which is based on a desirable BMI of 21 kg/m2.[8] The estimation of BMI by health workers and the calculation of the desirable weight may be difficult due to lack of access to a calculator or performing a calculation involving exponents. The field charts were developed in response to the need for a practical tool for healthcare providers to help classify nutritional status by BMI category at diagnosis, enable estimation of recommended caloric intake, as well as assess adequacy of weight gain during follow-up with reference to a desirable weight according to patient's height.
Construction and Description of the Field Charts
The construction of the chart is based on the height of an adult patient as the basic measurement. For any given height in centimetres (cm), converted to meters (m), the range of body weights consistent with different categories of BMI was calculated. This was done by rearranging the formula of estimation of BMI (mentioned earlier), so that weight = BMI × (height in m)2. This rearranged formula was then used to calculate the weights corresponding to BMI cut-offs for different categories of underweight [Table 1]. For example, the cut-off for defining severe underweight would be a weight corresponding to a BMI of less than 16.0 kg/m2. For a height of 150 cm, this would be 16 × (1.5)2 = 36 kg, while the body weight corresponding to moderate underweight would be a BMI of 17.0 would be 17 × (1.5)2 = 38.3 kg. The weights corresponding to the lower and upper bounds of different BMI categories of underweight were thus calculated. The charts contain an additional cut-off of weights corresponding to a BMI of 14 kg/m2, which signifies extremely severe wasting. This additional cut-off is for logistical reasons. According to the recommendations in the WHO manual for management of severe malnutrition, all adults with a BMI <16 kg/m2 should be admitted for inpatient nutritional care.[9] In a rural cohort of patients with TB in India, nearly 50% of the cohort had a BMI of less than 16 kg/m2 and would thus be eligible for inpatient care, which can be very challenging at programmatic level.[3] The RNTCP guidance document therefore suggests red-flag features warranting admission, which include BMI ≤14 kg/m2 and BMI 14–16 kg/m2 along with the presence of severe anemia or pedal edema, unstable vital signs, and poor performance status.[8]
Table 1.
Simplified body mass index-based field chart to assess nutritional status and weight gain in undernourished patients with active tuberculosis
| Height (cm) | Weights in kg corresponding to cut-offs of different categories of BMI | ||||||
|---|---|---|---|---|---|---|---|
| BMI <14.0 kg/m2 extreme underweight | BMI: 14.0-15.9 kg/m2 severe underweight | BMI: 16.0-16.9 kg/m2 moderate underweight | BMI: 17.0-18.4 kg/m2 mild underweight | BMI: 18.5-24.9 kg/m2 normal | BMI of 21 kg/m2 desirable weight | Suggested caloric intake: 40 kcal/desirable body weight* | |
| 143 | ≤28.4 | 28.5-32.5 | 32.6-34.6 | 34.7-37.6 | 37.7-50.9 | 42.9 | 1700 |
| 144 | ≤28.8 | 28.9-33.0 | 33.1-35.0 | 35.1-38.2 | 38.3-51.6 | 43.6 | 1750 |
| 145 | ≤29.3 | 29.4-33.5 | 33.6-35.6 | 35.7-38.8 | 38.9-52.5 | 44.2 | 1800 |
| 146 | ≤29.8 | 29.9-33.9 | 34.0-36.1 | 36.2-39.2 | 39.3-53.1 | 44.8 | 1800 |
| 147 | ≤30.0 | 30.1-34.4 | 34.5-36.5 | 36.6-39.8 | 39.9-53.8 | 45.4 | 1800 |
| 148 | ≤30.5 | 30.6-34.8 | 34.9-37.0 | 37.1-40.3 | 40.4-54.6 | 46.0 | 1850 |
| 149 | ≤31.0 | 31.1-35.3 | 35.4-37.5 | 37.6-40.9 | 41.0-55.3 | 46.6 | 1850 |
| 150 | ≤31.3 | 31.4-35.8 | 35.9-38.1 | 38.2-41.4 | 41.5-56.1 | 47.3 | 1900 |
| 151 | ≤31.8 | 31.9-36.3 | 36.4-38.6 | 38.7-42.0 | 42.1-56.8 | 47.9 | 1900 |
| 152 | ≤32.1 | 32.2-36.8 | 36.9-39.1 | 39.2-42.5 | 42.6-57.6 | 48.5 | 1950 |
| 153 | ≤32.6 | 32.7-37.3 | 37.4-39.6 | 39.7-43.1 | 43.2-58.3 | 49.2 | 1950 |
| 154 | ≤33.0 | 33.1-37.7 | 37.8-40.1 | 40.2-43.7 | 43.8-59.1 | 49.8 | 2000 |
| 155 | ≤33.4 | 33.5-38.2 | 38.3-40.6 | 40.7-44.2 | 44.3-59.9 | 50.5 | 2000 |
| 156 | ≤33.9 | 34.0-38.7 | 38.8-41.2 | 41.3-44.8 | 44.9-60.6 | 51.1 | 2050 |
| 157 | ≤34.3 | 34.4-39.2 | 39.3-41.7 | 41.8-45.4 | 45.5-61.4 | 51.8 | 2100 |
| 158 | ≤34.7 | 34.9-39.7 | 39.9-42.2 | 42.3-45.9 | 46.0-62.2 | 52.4 | 2100 |
| 159 | ≤35.2 | 35.3-40.2 | 40.3-42.8 | 42.9-46.6 | 46.7-63.0 | 53.1 | 2100 |
| 160 | ≤35.6 | 35.7-40.8 | 40.9-43.3 | 43.4-47.2 | 47.3-63.8 | 53.8 | 2150 |
| 161 | ≤36.1 | 36.2-41.3 | 41.4-43.9 | 44.0-47.8 | 47.9-64.6 | 54.4 | 2200 |
| 162 | ≤36.5 | 36.6-41.8 | 41.9-44.4 | 44.5-48.4 | 48.5-65.4 | 55.1 | 2200 |
| 163 | ≤37.0 | 37.1-42.3 | 42.4-45.0 | 45.1-49.0 | 49.1-66.2 | 55.8 | 2250 |
| 164 | ≤37.5 | 37.6-42.8 | 42.9-45.5 | 45.6-49.6 | 49.7-67.0 | 56.5 | 2250 |
| 165 | ≤37.9 | 38.0-43.3 | 43.4-46.0 | 46.1-50.1 | 50.2-67.9 | 57.2 | 2300 |
| 166 | ≤38.4 | 38.5-43.9 | 44.0-46.6 | 46.7-50.8 | 50.9-68.7 | 57.9 | 2300 |
| 167 | 38.9 | 39.0-44.4 | 44.5-47.2 | 47.3-51.4 | 51.5-69.5 | 58.6 | 2350 |
| 168 | 39.3 | 39.4-45.0 | 45.1-47.8 | 47.9-52.0 | 52.1-70.4 | 59.3 | 2400 |
| 169 | 49.8 | 49.9-45.5 | 45.6-48.4 | 48.5-52.6 | 52.7-71.2 | 60.0 | 2400 |
| 170 | 40.3 | 40.4-46.0 | 46.1-48.8 | 48.9-53.2 | 52.3-72.0 | 60.7 | 2450 |
| 171 | 40.7 | 40.8-46.6 | 46.7-49.5 | 49.6-53.9 | 54.0-72.9 | 61.4 | 2450 |
| 172 | 41.2 | 41.3-47.1 | 47.2-50.1 | 50.2-54.5 | 54.6-73.8 | 62.1 | 2500 |
| 173 | 41.7 | 41.8-47.7 | 47.8-50.7 | 50.8-55.2 | 55.3-74.6 | 62.9 | 2500 |
| 174 | 42.2 | 42.3-48.2 | 48.3-51.3 | 51.4-55.8 | 55.9-75.5 | 63.6 | 2550 |
| 175 | 42.7 | 42.8-48.8 | 48.9-51.9 | 52.0-56.5 | 56.6-76.4 | 64.3 | 2550 |
| 176 | 43.2 | 43.3-49.4 | 49.5-52.4 | 52.5-57.1 | 57.2-77.2 | 65.0 | 2600 |
| 177 | 43.7 | 43.8-49.8 | 50.0-53.2 | 53.3-57.8 | 57.9-78.1 | 65.8 | 2650 |
| 178 | 44.2 | 44.3-50.5 | 50.6-53.7 | 53.8-58.4 | 58.5-79.0 | 66.5 | 2650 |
| 179 | 44.6 | 44.7-51.1 | 51.2-54.3 | 54.4-59.1 | 59.2-79.9 | 67.3 | 2700 |
| 180 | 45.2 | 45.3-51.6 | 51.7-54.9 | 55.0-59.7 | 59.8-80.8 | 68.0 | 2700 |
*Approximate caloric intake assuming patient is sedentary, BMI: Body mass index; desired body weight: Body weight corresponding to BMI of 21 kg/m2
Desirable Body Weight of an Adult Patient with Tuberculosis
For estimation of caloric intake and monitoring of nutritional recovery during treatment, a desirable body weight as one which corresponds to a BMI of 21 kg/m2 is recommended.[8] According to the WHO classification, the bounds of the normal range of BMI are between 18.5 and 24.9 kg/m2. However, targeting a body weight which corresponds to a BMI of 18.5 kg/m2 is less desirable for the following reasons. First, patients often lose weight during resumption of normal work and a patient with a body weight corresponding to a BMI of 18.5 kg/m2 could slip into the category of undernourished with any loss of weight. Second, in developed countries, the Malnutrition Universal Screening Tool (MUST) is a widely accepted and validated tool for nutritional assessment.[10] According to MUST a BMI less than 20 kg/m2 is considered low. Third, according to the report of the expert group on nutrient requirements and recommended dietary intakes for Indians, a reference Indian man is defined as someone between 18 and 29 years of age who weighs 60 kg and has a height of 1.73 m which translates into a BMI of 20.3 kg/m2.[11] Similarly, the Indian reference woman has a height of 1.61 m and a weight of 55 kg which is a BMI of 21.2 kg/m2.[11] If a patient has a height of 1.5 m and weighs 36 kg at the start of treatment, he has a BMI of 16.0 kg/m2. If this patient has to reach desirable BMI of 21 kg/m2 then the corresponding weight will be 21 × 2.25 = 47.2 kg. Thus, a weight gain of 11.2 kg (47.2 -36) is required to reach BMI of 21.0 kg/m2. This type of calculation is difficult at programmatic level and gets simplified with the help of these field charts.
Method of Use of the Field Charts
The field charts are meant to be accessible and can be used by the peripheral-most health worker [Figure 1]. Healthcare personnel should choose the row which corresponds to the measured height of the patient. This row has ranges of body weights corresponding to the recommended BMI cut-offs for various ranges of nutritional status, as well as those for the BMI range considered normal (BMI of 18.5–24.9 kg/m2. Body weight above a cut-off of 23 kg/m2 BMI would categorize a patient as overweight in Asia, while in other regions the range is from 18.5 to 24.9 kg/m2.[12] For adult patients with TB, we have proposed the latter range due to significant coprevalence of undernutrition. If the height is 160 cm and the weight 40 kg, then the healthcare worker can infer that the body weight falls in the red coded column which indicates severe undernutrition category. Furthermore in the same row, the healthcare worker can see the range of BMI considered normal for the patient, a weight of 47.3–63.8 kg while the desirable body weight for this height would be around 54 kg. Thus, this patient needs to gain at least 7 kg to reach a minimum acceptable weight and about 14 kg to reach a desirable body weight corresponding to a BMI of 21 kg/m2. This can guide their assessment of the nutritional status on follow up. On the other hand, if for the same height of 160 cm the weight of the patient is measured to be 34 kg, then this weight falls in the dark red band (corresponding to a BMI <14 kg/m2) and would flag extreme thinness, for which admission to an inpatient facility and nutritional therapy would be strongly recommended. The final column in the field chart also mentions the approximate caloric intake, based on the desirable body weight, to be advised to the patients assuming that he or she is sedentary.
Figure 1.
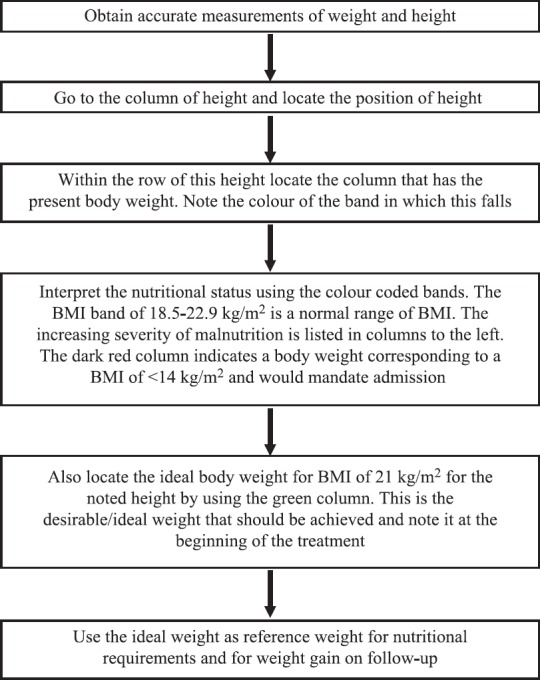
Steps in using body mass index–based field charts
Any weight loss or failure to gain weight during the management of a case of TB requires clinical assessment to rule out resistance, poor adherence, and other comorbidities. The new TB card in the Technical Operational Guidelines has a provision for recording height and monthly weight record.[13] At the same time, no meaningful interpretation is made as BMI is not being calculated at programmatic level. This easy-to-use color-coded field chart will be relevant and useful in interpreting the routine height and weight recording for nutritional assessment and monitoring purposes.
Relevance with End-TB Strategy and Direct Benefit Transfer
The member nations of World Health Assembly have passed a resolution in May 2014 to approve the post-2015 Global TB Strategy. It has laid down important and ambitious targets of reducing the TB deaths by 95% and new cases by 90% by 2035.[14] The resolution puts the patients and their families at the heart of the strategy where pillar 1 focuses on integrated patient-centered care and pillar 2 includes political commitment and addressing social determinants.[14] India in its ambitious response has set goals that are 5 years ahead of the global targets.[15] To address the comorbidity of undernutrition in TB, the Government of India has further adopted a direct benefit transfer (DBT) mechanism for transfer of Rs 500 per month to the bank accounts of all patients with TB during the treatment of TB from April 2018.[16] This is for nutritional support during treatment irrespective of their economic status and geographic location. While this is likely to improve nutrition in the patients, the adequacy of the quantum of support needs to be assessed at programmatic level. The BMI-based field charts can provide a simple assessment and monitoring tool in this regard. Moreover, the gazette notification mentions that the assistance can be cash or kind.[16] This means that there is an opportunity to create an evidence through operational research using these field charts for DBT of both types. Any evidence from our country can contribute in a significant manner toward all the three pillars of End TB Strategy, an integrated patient-centered care, bold policies and supportive systems, and intensified research and innovation.
Usefulness in Primary Care Settings and Family Physicians
The care providers in primary care settings often encounter undernutrition as comorbidity not just in patients with TB but also in other acute and chronic illnesses and first trimester for pregnancy. The simplest and widely used tool to assess nutritional status is the BMI. The field charts make BMI-based nutritional assessment easily accessible to primary care providers, including nonphysicians. The chart also makes available the desirable weight, which would have otherwise required complex calculations.
Conclusion
The simplified BMI-based field charts aid classification of undernutrition in patients with active TB, alert the health worker to a weight which should mandate admission in an inpatient facility, and can also provide information of the range of body weights which would be consistent with the nutritional recovery of the patient. It will allow objective assessment of the progress of the patients toward that target desirable body weight.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Macallan DC. Malnutrition in tuberculosis. Diagn Microbiol Infect Dis. 1999;34:153–7. doi: 10.1016/s0732-8893(99)00007-3. [DOI] [PubMed] [Google Scholar]
- 2.Bhargava A, Benedetti A, Oxlade O, Pai M, Menzies D. Undernutrition and the incidence of tuberculosis in India: National and subnational estimates of the population-attributable fraction related to undernutrition. Natl Med J India. 2014;27:128–33. [PubMed] [Google Scholar]
- 3.Bhargava A, Chatterjee M, Jain Y, Chatterjee B, Kataria A, Bhargava M, et al. Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality. PLoS One. 2013;8:e77979. doi: 10.1371/journal.pone.0077979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Padmapriyadarsini C, Shobana M, Lakshmi M, Beena T, Swaminathan S. Undernutrition & tuberculosis in India: Situation analysis & the way forward. Indian J Med Res. 2016;144:11–20. doi: 10.4103/0971-5916.193278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vasantha M, Gopi PG, Subramani R. Weight gain in patients with tuberculosis treated under directly observed treatment short-course (DOTS) Indian J Tuberc. 2009;56:5–9. [PubMed] [Google Scholar]
- 6.Swaminathan S, Padmapriyadarsini C. Undernutrition and tuberculosis: Strongly linked, but ignored. Natl Med J India. 2014;27:125–7. [PubMed] [Google Scholar]
- 7.World Health Organisation. Geneva: World Health Organisation; 2013. Guideline: Nutritional Care and Support for Patients with Tuberculosis. [PubMed] [Google Scholar]
- 8.Guidance Document on Nutritional Care and Support for Patients with Tuberculosis in India. Central TB Division, Ministry of Health and Family Welfare Government of India. 2017 [Google Scholar]
- 9.Geneva: World Health Organisation; 1999. Management of Severe Malnutrition: A Manual for Physicians and Other Senior Health Workers. [Google Scholar]
- 10.Poulia KA, Yannakoulia M, Karageorgou D, Gamaletsou M, Panagiotakos DB, Sipsas NV, et al. Evaluation of the efficacy of six nutritional screening tools to predict malnutrition in the elderly. Clin Nutr. 2012;31:378–85. doi: 10.1016/j.clnu.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 11.Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2010. Nutrient Requirements and Recommended Dietary Allowances for Indians. [Google Scholar]
- 12.WHO Expert Consultation. Appropriate body-mass index for asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 13.Central TB Division. Revised National TB Control Programme. Technical and Operational Guidelines for Tuberculosis Control in India. 2016. [Last accessed on 2018 Jan 20]. Available from: http://www.health.bih.nic.in/Docs/Guidelines/Guidelines-TB-Control.pdf .
- 14.World Health Organization. Geneva, Switzerland: World Health Organization; 2015. The End TB Strategy. [Google Scholar]
- 15.Central TB Division. Directorate General of Health Services. India TB Report 2018. [Last accessed on 2018 May 15]. Available from: https://www.tbcindia.gov.in/showfile.php?lid=3314 .
- 16.New Delhi: Department of Health and Family Welfare; 2017. Government of India. Guidance tool for Direct Benefit Transfer. National Health Mission. [Google Scholar]


