Abstract
Background:
Effective health education consequently improves knowledge, attitude, and practices (KAP) leading to better glycemic control and is widely accepted as an integral part of comprehensive diabetes care for affected individuals and their families in primary care settings.
Aims:
To assess the impact of health education on knowledge, attitude, practices, and glycemic control in type 2 diabetes mellitus patients.
Settings and Design:
This case control study was conducted in the department of Medicine of a tertiary care teaching hospital.
Methods:
The study was conducted on 100 diabetic subjects aged more than 40 years comprising of 50 cases and 50 controls. Cases were given education on their disease, drugs, dietary, and lifestyle modifications along with patient education leaflet at baseline and at first follow-up, while controls received neither of these. Subjects were assessed for KAP by administering KAP questionnaire and for glycemic control by measuring glycated hemoglobin (HbA1C) at baseline and at the end of the study.
Results:
In this study, end mean knowledge, attitude, practice, and KAP SUM scores of cases (10.28 ± 1.78, 3.46 ± 0.93, 3.14 ± 0.86, and 16.82 ± 3.40, respectively) showed significant increase from the baseline (3.86 ± 0.93, 1.00 ± 0.83, 0.40 ± 0.64, and 5.26 ± 2.10, respectively) compared to controls, accompanied by significant reduction in HbA1C of cases at the end of the study compared to the controls.
Conclusions:
Effective health education improves knowledge, attitude, and practices, particularly with regard to lifestyle modifications and dietary management, culminating into better glycemic control that can slow down the progression of diabetes and prevent downstream complications.
Keywords: Attitude, glycemic control, health education, knowledge, practices, type 2 diabetes mellitus
Introduction
Diabetes mellitus (DM) leads to alarming clinical, social, financial, and public health issues with devastating long-term effects on the well-being, affecting quality of life including neuropathy, retinopathy, nephropathy, dementia, and cognitive problems.[1,2,3] Self-monitoring of blood sugar and apt self-care with effective metabolic regulation affect hypoglycemia, ketoacidosis, or microvascular and macrovascular complications.[3] DM prevalence has risen dramatically over the past 2 decades, with India being the major contributor. Global burden in 2011 was 8.3% (366.2 millions) compared to 4% in 1995 and is projected to rise to 551.9 million by 2030.[4,5] However, our National Health Policy 2017 envisaged reducing premature mortality from diabetes and other non-communicable diseases to 25% by 2025.[6] There is a need to focus on preventive efforts with research on optimum choice of user-friendly test/s in the first contact care. Although glycated hemoglobin (HbA1C) does not require fasting and may be the best compromise, diagnosis and prognosis cannot be solely relied on HbA1C values that are affected in presence of different physiological and co-morbid conditions.[7,8,9,10] Diabetes education is considered an essential tool as its management largely depends on knowledge, motivation, and ability to pursue self-care in activities of daily living. Therefore, counseling and health education should be given paramount importance by the physicians even in their busy schedule including elaborate advice on lifestyle modifications and diet.[10,11,12,13] Although, evidences suggest that diabetics with more knowledge and motivated self-care help to achieve better glycemic control, there is difference of opinion on effectiveness of methods of health education and educational efforts to improve interventions are key components of effective treatment plan for DM.[14,15,16,17]
Health education is essential in resource poor settings such as ours, wherein DM pose great financial burden and calls for urgent participation of clinicians at all levels especially primary care physicians as they are usually the first care givers and come across known as well as recently detected diabetics. These patients can be imparted health education by primary care physicians to adopt healthy lifestyle practices, remain motivated for regular testing of glycemic status, and be aware of diabetic complications. The consequent changes in knowledge, attitude, and practices of diabetic patients are vital for achieving glycemic control and for preventing the development of complication of diabetes.
This study was undertaken to assess the positive impact of health education on knowledge attitude, and practices with effectively improved patient glycemic control in type 2 DM.
Methods
This case-control study, conducted at the department of Medicine of a tertiary care teaching hospital in north-west India, enrolled 100 diabetics randomized into 50 cases and 50 controls.
Inclusion criteria: Both males and females aged more than 40 years having type 2 DM as per the American Diabetes Association ADA criteria and normal cognition were included in this study.[18]
Exclusion criteria: Patients aged less than 40 years, pregnant women, those having type 1 DM, mental retardation, psychotic disorders, or cognitive decline due to any cause and non-consenters were excluded.
Data collection procedure: The study conformed to the Helsinki Declaration. Approval was sought from the institutional ethics committee. All the participants were explained about the purpose of the study and were ensured strict confidentiality, and that it would be used only for academic purpose. Then, informed consent was taken from each of them before the total procedure. The participants were given the options not to participate in the study if they wanted. All the participants underwent detailed history, clinical examination, and necessary laboratory investigations; baseline levels of knowledge, attitude, and practices regarding DM were assessed. The case group participants received health education on their disease, drugs, dietary, and lifestyle modifications along with the “patient education leaflet” to compliment the verbal counseling at baseline; same was not provided to the control group. After baseline, two follow-ups were made at an interval of 2 months each. At baseline and at each follow-up visit, random plasma glucose (RPG) was measured in all the subjects (cases and controls). HbA1C was measured at baseline and final follow-up. A pre-designed and validated KAP questionnaire [Table 1] was administered at baseline and at final follow-up to assess awareness regarding DM and its management. The questionnaire, in English or regional language was filled in a face-to-face interview, contained questions relating to the socio-demographic information of the participants. The pilot study was carried out among comparable population, following which some of the questions from the interview schedule were modified. Patients taken for the study were treated as per standard treatment guidelines. Patients requiring major treatment modifications during follow-up period were dropped out. Random venous blood samples were taken and were examined in the biochemistry laboratory of the institute.
Table 1.
Knowledge, attitude, and practices questionnaire
| Yes/no | Score | |
|---|---|---|
| Knowledge questions | ||
| Diabetes is a condition in which the body contains higher level of blood sugar than normal | ||
| The major causes of diabetes are hereditary, obesity, and unhealthy eating habits | ||
| The symptoms of diabetes are frequent urination, increased thirst, and hunger | ||
| Diabetes, if not treated, will cause damage to other organs such as heart, eyes, kidneys, and foot ulcers | ||
| The most accurate method of monitoring diabetes is checking blood glucose levels | ||
| In a diabetic patient, high blood pressure can worsen the risk of heart attack, stroke, kidney, and eye problems | ||
| A diabetic patient should measure his or her blood pressure regularly | ||
| The lifestyle modification required for diabetic patients is weight reduction, stopping alcohol consumption, and smoking | ||
| A diabetic patient should have his or her eyes checked every year | ||
| The important factors that help in controlling blood sugar are controlled and planned diet, and medication | ||
| Regular urine tests will help in knowing the amount of proteins in your urine and functional status of kidneys | ||
| A regular exercise regimen will help in blood glucose control | ||
| A well-balanced diet include carbohydrates, proteins, fruits, and fibres | ||
| Diabetes is a curable/non-curable disease | ||
| Attitude questions | ||
| Do you exercise regularly? | ||
| Are you following a controlled and planned diet? | ||
| Do you think missing doses of your diabetic medication will have a negative effect on your disease control? | ||
| Are you aware of your blood sugar levels fall below normal when you are taking drugs? | ||
| Do you think you should keep in touch with your physician? | ||
| Practice questions | ||
| When your blood pressure was last checked? | ||
| When was your last eye examination? | ||
| When was your last urine examination? | ||
| When was your last visit to your physician? | ||
| When was your blood sugars last checked? | ||
| When was your lipids last checked? | ||
| Total | ||
Data analysis: The results were analyzed statistically to assess the impact of health education on knowledge, attitude, practices and glycemic control in diabetic patients. The data collected were entered into Excel spread sheets, and analysis was carried out using IBM SPSS Statistics for Windows, Version 11.0. Armonk, NY SPSS software. The pre-tested closed ended questionnaire was used to assess the impact of health education intervention, where a score of each answer was coded as Yes = 1, No = 0. Mean were used to derive information on knowledge, attitude, and practice aspect of diabetic patients. Paired t test was applied to the pre-test and post-test results of knowledge, attitude, and practice on diabetes to assess the impact of health education intervention, P value <0.05 was considered statistically significant.
Results
Mean age of the cases was 55.50 ± 9.37 years and of controls was 52.02 ± 7.83 years; 22 (44%) males were among cases and 25 (50%) among controls. Among cases, 26 (52%) were literate; in the control group, 30 (60%) were literate. Among cases, 16 (32%) were recently detected to have diabetes, while 34 (68%) were having diabetes for more than 6 months. In the control group, 20 (40%) were recently detected to have diabetes, while 30 (60%) were having diabetes for more than 6 months. In the case group, 27 (54%) were overweight and 23 (46%) were obese; in the control group 32 (64%) were overweight and 18 (36%) were obese. RPG was checked in all the participants at baseline and at each follow-up, showing significant declining trend of RPG in the case group from baseline to first follow-up and subsequently to final follow-up. Similar trend was not observed in the control group [Table 2].
Table 2.
Random plasma glucose-cases and controls
| RPG | Baseline | First follow-up | Final follow-up | |||
|---|---|---|---|---|---|---|
| Case group | Control group | Case group | Control group | Case group | Control group | |
| ≤200 | 0 | 0 | 0 | 0 | 0 | 0 |
| 201-210 | 0 | 0 | 0 | 0 | 0 | 0 |
| 211-220 | 0 | 0 | 0 | 0 | 7 | 0 |
| 221-230 | 0 | 0 | 0 | 0 | 20 | 0 |
| 231-240 | 0 | 0 | 4 | 0 | 13 | 0 |
| 241-250 | 0 | 0 | 1 | 0 | 0 | 0 |
| 251-260 | 0 | 0 | 11 | 0 | 0 | 0 |
| 261-270 | 0 | 0 | 15 | 0 | 0 | 0 |
| 271-280 | 0 | 0 | 8 | 0 | 6 | 0 |
| 281-290 | 0 | 0 | 1 | 0 | 4 | 0 |
| 291-300 | 0 | 0 | 5 | 0 | 0 | 1 |
| 301-310 | 4 | 7 | 3 | 8 | 0 | 6 |
| 311-320 | 0 | 6 | 2 | 5 | 0 | 10 |
| 321-330 | 0 | 2 | 0 | 7 | 0 | 7 |
| 331-340 | 9 | 9 | 0 | 8 | 0 | 6 |
| 341-350 | 7 | 10 | 0 | 6 | 0 | 5 |
| 351-360 | 9 | 0 | 0 | 1 | 0 | 2 |
| 361-370 | 3 | 5 | 0 | 4 | 0 | 6 |
| 371-380 | 3 | 4 | 0 | 4 | 0 | 0 |
| 381-390 | 4 | 0 | 0 | 0 | 0 | 1 |
| 391-400 | 5 | 2 | 0 | 3 | 0 | 3 |
| 401-410 | 4 | 4 | 0 | 3 | 0 | 3 |
| 411-420 | 2 | 1 | 0 | 1 | 0 | 0 |
| 421-430 | 0 | 0 | 0 | 0 | 0 | 0 |
| 431-440 | 0 | 0 | 0 | 0 | 0 | 0 |
| 441-450 | 0 | 0 | 0 | 0 | 0 | 0 |
| ≥451 | 0 | 0 | 0 | 0 | 0 | 0 |
RPG: Random plasma glucose
At baseline, the case group patients had mean knowledge score of 3.86 ± 0.93, and at final follow-up, this score was 10.28 ± 1.78. In the control group, the mean knowledge score was 5.66 ± 1.61 at baseline, and at final follow-up, it was 5.76 ± 1.72. There was a significant increase in mean knowledge score of cases compared to controls at the final follow-up (P = 0.004) [Figure 1].
Figure 1.
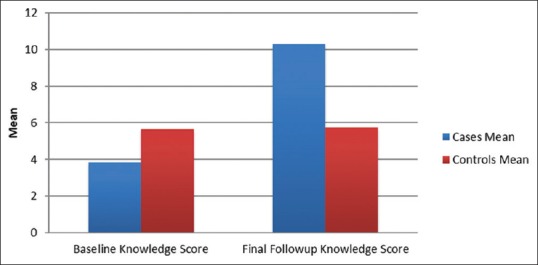
Mean knowledge scores of cases and controls at baseline and at final follow-up
Mean attitude score of the cases at baseline was 1.00 ± 0.83, and at final follow-up, the score rose to 3.46 ± 0.93. The control group had mean attitude scores of 1.78 ± 0.97 at baseline and 1.79 ± 0.48 at final follow-up. The increase in the mean attitude score of cases was statistically significant as compared to the controls (P = 0.003) [Figure 2].
Figure 2.
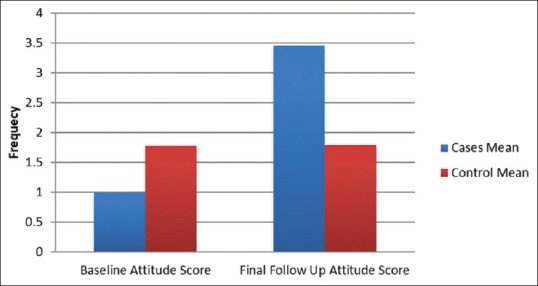
Mean attitude scores of cases and controls at baseline and at final follow-up
The cases had mean practice score of 0.40 ± 0.64 at baseline, and at final follow-up, this score was 3.14 ± 0.86. In the control group, at baseline, the mean practice score was 1.54 ± 0.73, and at final follow-up, it was 1.58 ± 0.86. There was significant increase in the mean practice score of cases as compared to controls at the final follow-up (P = 0.001) [Figure 3].
Figure 3.
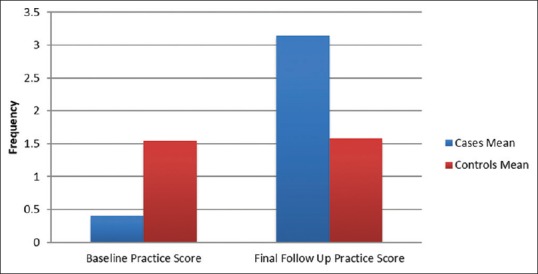
Mean practice scores of cases and controls at baseline and at final follow-up
At baseline, cases had mean KAP SUM score 5.26 ± 2.10, and at final follow-up, this score increased to 16.82 ± 3.40. In the control group, the mean KAP SUM score was 8.98 ± 3.24 at baseline and 9.08 ± 3.36 at final follow-up. Increase in the mean KAP SUM score of cases was statistically significant compared to controls at the final follow-up (P = 0.003) [Figure 4].
Figure 4.
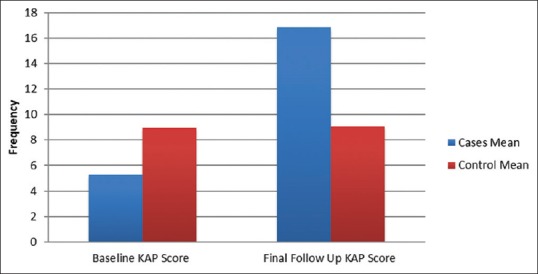
Mean knowledge, attitude, and practice sum scores of cases and controls at baseline and at final follow-up
HbA1c was measured in all the participants at baseline and at final follow-up. At baseline, 22 (44%) cases had HbA1c in the range of 7.1–8%, 17 (34%) had HbA1c between 8.1–9%, and remaining 11 (22%) had HbA1c between 9.1–10%. At final follow-up, 30 (60%) had HbA1c 7%, 11 (22%) had HbA1c in the range of 7.1–8%, and remaining 9 (18%) had HbA1C between 8.1–9%. The reduction in HbA1C of case group patients from baseline to final follow-up was statistically significant (P = 0.01). Among controls, at baseline, 13 (26%) had HbA1C in the range of 7.1–8%, 30 (60%) had HbA1C between 8.1–9%, and remaining 7 (14%) had HbA1C between 9.1–10%. At the final follow-up, 13 (26%) were having HbA1C in the range of 7.1–8%, 30 (60%) had HbA1C ranging between 8.1–9%, and remaining 7 (14%) had HbA1C between 9.1–10%. Thus, there was no reduction in HbA1C of controls at the final follow-up (P = 0.159) [Figure 5].
Figure 5.
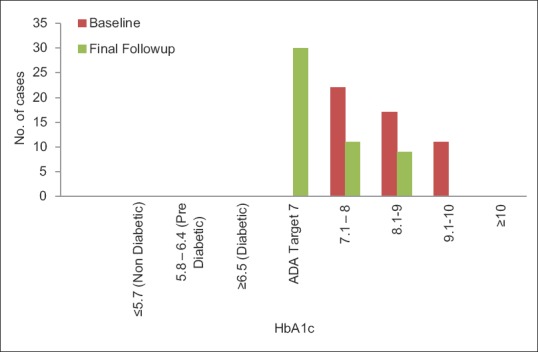
HbA1C of cases at baseline and at final follow-up
Discussion
Health education imparts knowledge on environmental, physical, social, emotional, intellectual, and spiritual health. Sincere health education is able to hone knowledge, attitude, and practices of individuals and can lead to better control of diabetes. It is widely accepted as an integral part of comprehensive diabetes care especially in resource poor settings wherein diabetes poses a great financial burden. The complications of DM have an adverse impact on the quality of life of patients and their families, with a devastating long-term effect on their financial and social well-being. Various studies performed so far suggest positive outcome of health education in terms of slowing the progression of disease and preventing complications.
In this study, a total of 100 diabetics were allocated randomly into 2 groups, 50 cases, and 50 controls (age and sex-matched); 54% were overweight and 46% obese among cases, and in the control group, 64% were overweight and 36% were obese. In a similar study conducted by Fatema et al. in Bangladesh, the mean BMI of subjects was 24.4 ± 4.1 kg/m2.[19]
RPG was checked in all participants at baseline and at each follow-up which showed a declining trend in the case group from baseline to first follow-up and subsequently to final follow-up, which was not observed in the control group. This highlighted the relevance of health education in bringing glycemic control in diabetic patients. Similar results were seen in the study by Shareef et al. who noted a significant decrease in the fasting and post prandial blood glucose levels from baseline on the final follow-up in the intervention group.[20]
In this study, mean knowledge, attitude, practice, and KAP SUM scores of cases measured at the end of the study showed significant increase from the baseline compared to the controls. Thus, imparting health education led to significant improvement in all 3 spheres of diabetes management i.e., knowledge, attitude, and practice. The study conducted by Shareef et al. also found significant increase in overall diabetes knowledge from 18.05% to 25.43% in the intervention group compared to controls. The mean scores of patient's knowledge about diabetes, self-care practices, and knowledge regarding complications of diabetes showed significant improvement in the intervention group patients after they were imparted health education. A significant decrease in the fasting and post prandial blood glucose levels was also observed at final follow-up from the baseline period in the intervention group.[21] Ghazanfari Z. et al. also observed a significant improvement in the knowledge (P < 0.001), attitudes, and practices of the intervention group toward healthy behaviors regarding nutrition, physical activity, and self-care.[22]
In another study similar to ours, the mean knowledge, attitude, and practice scores at baseline were 6.56 ± 4.06, 2.24 ± 1.65, and 1.74 ± 1.26 in the control group, respectively and 6.48 ± 4.49, 2.18 ± 1.36, and 3.1 ± 1.5 in the test group, respectively. Mean KAP scores were 10.46 ± 6.19 and 11.96 ± 6.84 in the control and test groups, respectively at baseline. At final follow-up, the mean knowledge scores were 7.12 ± 3.98 and 12.12 ± 2.12, mean attitude scores were 2.24 ± 1.33 and 4.12 ± 0.87, mean practice scores were 1.92 ± 1.34 and 4.46 ± 1.01, and the mean KAP scores were 11.36 ± 6.12 and 20.78 ± 3.13 in the control and test groups, respectively. Statistically, there was significant difference in knowledge, attitude, practice, and total KAP scores between the test and the control groups at final follow-up.[23]
HbA1C was measured at baseline and at final follow-up; statistically significant reduction in HbA1C was in the cases at final follow-up as compared to baseline HbA1C values. Similar reduction in HbA1C was not observed in the control group. This emphasized the importance of health education in attaining long-term glycemic control in diabetes and preventing its complications. Similar findings were reported in the study by Ahmed et al. wherein the mean levels of FBS and HbA1C had significantly decreased at the second visit compared to the first visit (180.33 ± 34.81; 8.69 ± 0.72 versus 168.04 ± 28.56, 7.50 ± 0.97, respectively). In addition, there was a strong negative correlation between the knowledge attitude (KA) score and HbA1C and between the KA score and fasting blood glucose.[24] However, Islam SMS et al. noted a weak negative association between diabetes knowledge score and HbA1C.[25]
Study by Palaian S et al., resolved with contrasting results. Although knowledge scores in the test group of patients improved with health education compared with those of the control group, the investigators did not observe significant improvement in attitude or practice scores. They concluded that patient counseling improved knowledge scores, but this improved knowledge did not lead to appropriate attitudes or practices.[26]
A study in the north-eastern India pursued to determine the existing knowledge, attitude, practices, and impact of a structured health education intervention regarding diabetes in adults. There was significant improvement in knowledge after intervention regarding (a) risk factors, (b) early symptoms, (c) organs affected, (d) warning signs of hypoglycemia, and (e) personal precautions. In addition, significant improvement of positive attitude was noted (a) to motivate blood sugar testing yearly in family members after 40 years of age, (b) to undergo regular check-up, continue medication, and motivate family members. This study emphasized that there is a dire need of better health information through large scale awareness programs to change the attitude and practices of public regarding diabetes.[14]
Research in Navi Mumbai, Maharashtra, India in their study to assess knowledge, attitude, and self-care activities among type-2 diabetic patients noted that diabetics who were regularly involved in self-care practices (particularly dietary management) attained better glycemic control; there was a significant difference between knowledge toward self-care activities between the glycemic controlled versus uncontrolled cases. In self-care practices, strict diet, and glucose management significantly achieved glycemic control.[23]
Ahmed MM et al. from Department of Family Medicine, Faculty of Medicine, Cairo University, Egypt concluded from their study that educational intervention was a powerful tool to motivate patients’ knowledge and attitude and effectively improved patient glycemic control.[27] Imparting health education through SMS was a feasible and acceptable method for improving glycemic control and self-management behaviors in another Egyptian study.[24] In the study at Xiamen University, Xiamen, Fujian Province, China, the researchers observed that extension of diabetes health education toward self-management support effectively improve the self-care skills of diabetics, reduction of medical costs, and quality of life.[28]
In a U.K study, the British Pakistani women were assessed before and 6 months after intervention by questionnaire and HbA1C blood test for glycemic control. Nearly everyone improved their knowledge scores in the intervention group; illiterate women did not do as well, continuing to score less on knowledge parameters and did not show an improvement in glycemic control.[29] In the 2015 updated position statement of the ADA and the European association for the study of diabetes, it was strongly encouraged that diabetics should adhere to the newer paradigm of the management protocol of hyperglycemia in type 2 diabetes with a patient-centered approach for the best possible outcomes.[13]
Diabetes Canada Clinical Practice Guidelines Expert Committee recommended a variety of education and support programs including group classes and individual counseling sessions, with technology-based strategies (e.g., Internet-based computer programs and mobile phone apps). Diabetics need self-management education and support when first diagnosed, as well as during times when there are changes in treatment, general health, or life circumstances. Diabetics were suggested to adhere to diabetes team with a trusting and collaborative relationship, set goals for caring for disease and health, and identify tailor-made strategies.[16]
Brazilian study stressed on the importance of education and health communication guided dialogical relations and appreciation of popular knowledge, by reorienting the educational practices for self-care, to establish strategies for prevention in their study on knowledge, attitudes, and practices of self-care in individuals with DM.[30] Bangladesh researchers feel that diabetes education improves knowledge and attitudes for self-empowerment regardless of the education program tools (workshop or training package), to promote self-care skills improving the quality of life.[31,32] Australian research group on diabetes recommended education united with behavioral or psychological interventions as the snowball effect on knowledge and physiologic control.[33] Diabetic Association of India conducts Diabetes Education Program every month for all individuals in the field of diabetes whether patients or caregivers.[34]
Above observation and previous literature thus highlighted the positive impact of health education on knowledge, attitude, and practices of diabetic patients which can contribute in achieving desired glycemic control in type 2 DM. This study emphazises the effective role health education can play in reducing severity of disease activity in type 2 DM with regard to glycemic control and progression to complications.
In the era of practicing evidence-based health care, we have forgotten an important truth about putting people's health at the hand of people and how to care for it with a mindset to generate data of our own. The diabetics have to be willing to remove age old ideas from their mindset which is probably the first step to diabetes education. Further, health care providers at all levels have to internalize that with a paradigm shift, we have to consider not only the help of scientific feedback from the teachers and students but also from all the stakeholders of health care delivery system so that patient education should be given due importance for the success of any intervention regarding diagnosis and prognosis. In that direction, we need to overhaul our medical curriculum so that future physicians get trained to effectively communicate with the patients to impart optimum health education.[35]
Strength of the study
Few studies from India focused on impact of health education on diabetes control. This study highlighted the impact of health education on knowledge, attitude, and practices pertaining to diabetics that can be practiced in the primary care settings even in rural areas.
Limitations of the study
This was a single-center study with a small sample size.
Conclusions
In our study, effective health education resulted in improved knowledge, better attitude, and adoption of favorable practices which ultimately lead to better glycemic control in patients with type 2 DM, thus help to slow progression and prevent complications. Non-pharmacological interventions form a cornerstone of diabetes management and require favorable patient knowledge, attitude, and practices. Health education, therefore, is an essential tool in the management of diabetes. Effective patients’ education results in improved knowledge, better attitude, and adoption of right practices which transform into better glycemic control in patients with type 2 diabetes, thus slowing the progression of disease and preventing its complications. Health education is essential in resource poor primary care settings wherein DM pose great financial burden and calls for urgent participation of clinicians and health care workers to inform and motivate diabetic patients and to propagate healthy lifestyle practices vital for achieving glycemic control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Murata GH, Shah JH, Adam KD, Wendel CS, Bokhari SU, Solvas PA, et al. Factors affecting diabetes knowledge in type 2 diabetic veterans. Diabetologia. 2003;46:1170–8. doi: 10.1007/s00125-003-1161-1. [DOI] [PubMed] [Google Scholar]
- 2.Bandyopadhyay A, Mohanta PK, Sarker G, Kumar K, Sarbapalli D, Pal R. Appraisal of cognitive function of diabetics in a rural healthcare teaching institute. Ann Trop Med Public Health. 2016;9:48–55. [Google Scholar]
- 3.Singh M, Pal R, Ranjan R, Sarker G, Bharati DR, Pal S. Diabetes and dementia: Myth and reality. J Krishna Inst Med Sci Univ. 2017;6:12–7. [Google Scholar]
- 4.Makam AN, Nguyen OK. An evidence-based medicine approach to antihyperglycemic therapy in diabetes mellitus to overcome overtreatment. Circulation. 2017;135:180–95. doi: 10.1161/CIRCULATIONAHA.116.022622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buehler AM, Cavalcanti AB, Berwanger O, Figueiro M, Laranjeira LN, Zazula AD, et al. Effect of tight blood glucose control versus conventional control in patients with type 2 diabetes mellitus: A systematic review with meta-analysis of randomized controlled trials. Cardiovasc Ther. 2013;31:147–60. doi: 10.1111/j.1755-5922.2011.00308.x. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S, Singh M, Pal R, Ranjan R, Pal S, Ghosh A. National Health Policy 2017: Can it lead to achievement of sustainable development goals? Al Ameen J Med Sci. 2018;11:4–11. [Google Scholar]
- 7.Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of hbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights. 2016;11:95–104. doi: 10.4137/BMI.S38440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghosh A. Glycated hemoglobin: Diagnostic dilemma. Bengal Physicians J (Bull West Bengal API) 2018;5:35–6. [Google Scholar]
- 9.Ghosh A, Kundu D, Rahman F, Zafar ME, Prasad KR, Baruah HK, et al. Correlation of lipid profile among patients with hypothyroidism and type 2 diabetes mellitus. BLDE Univ J Health Sci. 2018;3:48–53. [Google Scholar]
- 10.Cavagnolli G, Pimentel AL, Freitas PA, Gross JL, Camargo JL. Effect of ethnicity on hbA1c levels in individuals without diabetes: Systematic review and meta-analysis. PLoS One. 2017;12:e0171315. doi: 10.1371/journal.pone.0171315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ezenwaka CE, Offiah NV. Patients’ health education and diabetes control in a developing country. Acta Diabetol. 2003;40:173–5. doi: 10.1007/s00592-003-0107-x. [DOI] [PubMed] [Google Scholar]
- 12.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007;30:2478–83. doi: 10.2337/dc07-0499.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes, 2015: A patient-centred approach. Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2015;58:429–42. doi: 10.1007/s00125-014-3460-0. [DOI] [PubMed] [Google Scholar]
- 14.Pal R, Pal S, Barua A, Ghosh MK. Health education intervention on diabetes in Sikkim. Indian J Endocrinol Metab. 2010;14:3–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherifali D, Berard RN, Gucciardi E, MacDonald B, MacNeill G. Diabetes Canada Clinical Practice Guidelines Expert Committee. Self-Management Education and Support. [Last accessed on 2018 Aug 15]. Available from: http://www.guidelines.diabetes.ca/cpg/chapter7 . [DOI] [PubMed]
- 17.Rheeder P. Type 2 diabetes: The emerging epidemic. SA Fam Pract. 2006;48:20. [Google Scholar]
- 18.American Diabetes Association. Report of the Expert committee on diagnosis and classification of Diabetes Mellitus. Diabetes Care. 2004;27:5–10. [Google Scholar]
- 19.Fatema K, Hossain S, Natasha K, Chowdhury HA, Akter J, Khan T, et al. Knowledge attitude and practice regarding diabetes mellitus among nondiabetic and diabetic study participants in Bangladesh. BMC Public Health. 2017;17:364. doi: 10.1186/s12889-017-4285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luan L, Yang J, He Y, Huang ZX, Liu L, Huang ZS. Impact of diabetes education and self-management support on the 4D series of diabetes patients. Biomed Res. 2017;28:1172–7. [Google Scholar]
- 21.Shareef J, Fernandes J, Samaga L, Bhat M. Effect of pharmacist led educational interventions on disease knowledge and glycemic control in patients with diabetes mellitus in a university hospital. Curr Res Diabetes Obes. 2016;1:555–9. [Google Scholar]
- 22.Ghazanfari Z, Ghofranipour F, Tavafian SS, Ahmadi F, Rajab A. Lifestyle education and diabetes mellitus type 2 – A non-randomized control trial. Iran J Public Health. 2007;36:68–72. [Google Scholar]
- 23.Gupta S, Singla M, Gupta N. A study of impact of patient education of diabetes on his knowledge, attitude and practices. J Med Sci Clin Res. 2017;5:30264–9. [Google Scholar]
- 24.Ahmed MM, Degwy HM, Ali MI, Hegazy NH. The effect of educational intervention on knowledge, attitude and glycemic control in patients with type 2 diabetes mellitus. Int J Community Med Public Health. 2015;2:302–7. [Google Scholar]
- 25.Islam SM, Niessen LW, Seissler J, Ferrari U, Biswas T, Islam A, et al. Diabetes knowledge and glycemic control among patients with type 2 diabetes in Bangladesh. Springerplus. 2015;4:284. doi: 10.1186/s40064-015-1103-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palaian S, Acharaya LD, Rao PG, Nair NP. Knowledge, attitude, and practice outcomes: Evaluating the impact of counselling in hospitalized diabetic patients in India. P T Around World. 2006;31:384. [Google Scholar]
- 27.Kakade AA, Mohanty IR, Rai S. Assessment of knowledge, attitude and self-care activities among type-2 diabetic patients attending a tertiary care teaching hospital. Int J Basic Clin Pharmacol. 2016;5:2458–62. [Google Scholar]
- 28.Abaza H, Marschollek M. SMS education for the promotion of diabetes self-management in low & middle income countries: A pilot randomized controlled trial in Egypt. BMC Public Health. 2017;17:962. doi: 10.1186/s12889-017-4973-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawthorne K. Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Educ Res. 2001;16:373–81. doi: 10.1093/her/16.3.373. [DOI] [PubMed] [Google Scholar]
- 30.Torres HDC, Souza ER, Lima MHM, Bodstein RC. Educational intervention for self-care of individuals with diabetes mellitus. Acta Paul Enferm. 2011;24:514–9. [Google Scholar]
- 31.Saleh F, Afnan F, Ara F, Mumu SJ, Khan AK. Diabetes Education, Knowledge Improvement, Attitudes and Self-Care Activities Among Patients With Type 2 Diabetes in Bangladesh. Jundishapur J Health Sci. 2017;9:36058. [Google Scholar]
- 32.Nabi-Amjad R, Rasouli D, Mohammadpour Y, Jafarizadeh H, Safaei Z, Rokhafrooz D. Comparison of effectiveness of self-empowerment through educational package and workshop in quality of life of diabetic patients. Jundishapur J Chronic Dis Care. 2016;5:3718. [Google Scholar]
- 33.The Rapid Review Team. International Centre for Allied Health Evidence. University of South Australia. Rapid Review of Literature for Health Literacy in People with Diabetes. [Last accessed on 2018 Aug 15]. Available from: https://www.adea.com.au/wp-content/uploads/2013/08/NDSS-Health-Literacy-Final-Report.pdf .
- 34.Diabetic Association of India. [Last accessed on 2018 Aug 15]. Available from: https://www.idf.org/our-network/regions-members/south-east-asia/members/94 india.html .
- 35.Pal R, Kumar R, Pal S, Vidyasagar, Mukherji B, Debabrata S, et al. Medical education: The hot seat. J Family Med Prim Care. 2016;5:20–3. doi: 10.4103/2249-4863.184618. [DOI] [PMC free article] [PubMed] [Google Scholar]


