Abstract
Maternal obesity and associated metabolic disease contribute to adverse outcomes in women and their offspring, and many of these outcomes have significant acute and chronic implications for both mother and neonate. Targeted movement (ie, physical activity or exercise training) during pregnancy has been shown to be safe and effective for improving many of these outcomes in women at a healthy weight and women who are obese. However, movement prescription and advice during pregnancy are often not addressed by health care providers; this situation creates a unique opportunity for physical therapists to use their expertise in movement with patients who are pregnant. The objective of this article is to briefly review the adverse maternal and neonatal outcomes associated with maternal obesity, the benefits of intentional maternal movement during pregnancy for women who are obese, the evidence-based guidelines for prescribing intentional movement during pregnancy for women who are obese, and the potential for physical therapists to become the driving force behind a necessary increase in movement levels in women who are pregnant. Physical therapists can play a significant role in encouraging movement in women who are healthy and women who have metabolic challenges during pregnancy and thus assist in combating the vicious cycle of obesity by improving maternal and offspring health.
The high prevalence of obesity continues to be an international public health crisis. Concurrent with record rates of obesity in the general population is the increasing prevalence of maternal obesity.1 Obesity before and during pregnancy is associated with higher risks of several obstetric and metabolic complications in women and their offspring.2 Moderate- to high-intensity movement (ie, physical activity or exercise training) during pregnancy has been shown to be safe and effective in improving maternal and neonatal outcomes in populations that are healthy, overweight, or obese,3 yet the number of women who exercise during pregnancy remains low. Specifically, only 23% of women who are pregnant report meeting the guidelines for physical activity described by the American Congress of Obstetricians and Gynecologists (ACOG),4 and the percentage is even lower for women who are pregnant and overweight or obese.5 Many women who are pregnant have not been educated on the benefits of physical activity during pregnancy, the truth about many common misconceptions regarding exercise during pregnancy, and what constitutes a safe and effective exercise program during pregnancy. As movement experts, physical therapists—along with other women's health care professionals—should serve as catalysts for encouraging and increasing safe exercise regimens for women who are pregnant and at all body weights. Obesity prevention must start with women of childbearing age,6 and it is vitally important that physical therapists become a more essential part of the process of combating and preventing obesity. The objective of this article is to briefly review the risks associated with maternal obesity, the benefits of maternal physical activity during pregnancy in women who are pregnant and obese, the evidence-based guidelines for prescribing physical activity during pregnancy in women who are pregnant and obese, and the opportunity for physical therapists to play a major role in a necessary increase in physical activity levels in women who are pregnant.
Obesity During Pregnancy
Maternal obesity has increased dramatically in the United States, with nearly 1 in 3 women now entering pregnancy obese.7 Maternal obesity adversely contributes to gestational weight gain (GWG) and postpartum weight retention and induces many physiological consequences that may increase the risk of altered maternal and neonatal metabolic health.8 Physical inactivity in combination with excess maternal adiposity can alter the intrauterine metabolic environment, contribute to adverse fetal programming, and lead to unfavorable neonatal outcomes with long-term health implications.9,10 The primary hypothesis attempting to explain the well-established connection between alterations in maternal health during pregnancy and neonatal outcomes is termed the “fetal origins hypothesis.”11 The seriousness of the issue has been highlighted by researchers and physicians who suggest that obesity may be the most common health risk for the developing fetus.10
Maternal Risks of Obesity During Pregnancy
Maternal obesity increases the risks of excessive GWG, gestational diabetes mellitus, preeclampsia, and other hypertensive disorders. It also has been associated with higher levels of maternal inflammation and oxidative stress, disrupted maternal lipid metabolism, labor and delivery complications, and the delivery of neonates with undetected anomalies and elevated risks for cognitive or emotional disorders, excess adiposity, and long-term development of obesity, diabetes, and hypertension.2
Excessive GWG.
One of the most well-documented risks of prepregnancy obesity is the risk of excessive GWG.12 Specifically, women who are overweight or obese are 2 to 6 times more likely to exceed the guidelines for appropriate weight gain in pregnancy recommended by the Institute of Medicine in 2009.12,13 Excessive GWG is the strongest risk factor for maternal postpartum overweight and obesity and, similar to prepregnancy obesity, is related to many adverse maternal and neonatal outcomes, including excess adiposity and its associated comorbidities.14,15
Gestational diabetes mellitus.
Gestational diabetes mellitus is defined as glucose intolerance with onset or first recognition during pregnancy. Women who develop gestational diabetes have increased risks of adverse perinatal, maternal, and neonatal outcomes; recurrence of gestational diabetes in subsequent pregnancies; and development of type 2 diabetes postpartum.16 Women who are nongravid and obese have lower insulin sensitivity that is exaggerated during pregnancy.17 Women who are pregnant and obese or morbidly obese are 3.5 or 8.5 times more likely to develop gestational diabetes, respectively.18
Preeclampsia and hypertensive disorders.
Preeclampsia, the most common hypertensive disorder during pregnancy, can be life-threatening for both women who are pregnant and their fetuses; 10% to 15% of all maternal deaths are related to preeclampsia and eclampsia.19 Maternal preeclampsia may lead to premature cardiovascular disease, chronic hypertension, ischemic heart disease, and stroke. Offspring of women who had preeclampsia during their pregnancy have increased risks of stroke, heart disease, and metabolic syndrome in adulthood.20,21 A systematic review by O'Brien et al22 that included 1.4 million women revealed that the risk of preeclampsia doubled for every 6-unit increase in prepregnancy body mass index (BMI); these data highlighted the substantial impact of obesity on the development of preeclampsia.
Labor and delivery complications.
Women who are obese are at least 2 times more likely to give birth to infants who are large for their gestational age; this scenario potentially increases the risk for other short-term complications at delivery, such as shoulder dystocia, prolonged labor, emergency cesarean section, postpartum hemorrhage, or third-degree perineal trauma.23,24 Women who are obese are also more likely to require a medically necessary cesarean section, which is associated with numerous other comorbidities and complications, including infection and prolonged recovery.25 Minsart et al26 evaluated data from 38,675 births and demonstrated that women who were pregnant and obese were 38% more likely than their counterparts at a healthy weight to require care in an intensive care unit as a result of labor and delivery complications.
Inflammation, oxidative stress, and disrupted lipid metabolism.
Like physiological function in women who are nongravid, physiological function in women who are pregnant and obese is altered compared with that in women who are pregnant and at a healthy body weight. Women who are pregnant and obese have higher plasma levels of oxidative stress27 and inflammation,28 both of which can extend into the placenta,29 thus adversely affecting neonatal and maternal health. Similarly, women who are pregnant and obese have exaggerated hyperlipidemia and higher free fatty acid concentrations because of the inability of insulin to suppress the rate of lipolysis.10,17
Neonatal Risks of Maternal Obesity During Pregnancy
Offspring of women who are obese face many short- and long-term health-related complications. Prepregnancy obesity puts infants at a higher risk for cardiac anomalies,30 including undetected malformations, because of adiposity-related insensitivity on fetal ultrasound studies.31 Neonates born to women who are obese also have greater risks of autism spectrum disorders, developmental delays, attention deficit disorders, and difficulty regulating emotions.32,33
Maternal obesity also increases the risk of giving birth to infants with excess adiposity.10 Overweight in infancy is believed to persist through childhood years.34 Because childhood obesity is a strong predictor of adult obesity,35 the effects of maternal obesity on offspring health clearly have a lifelong impact on children by perpetuating the cycle of obesity.
In addition to the increased risk of obesity into childhood and adulthood, offspring of women with maternal obesity also have elevated risks of hypertension, insulin resistance, dyslipidemia, and cardiovascular disease.36,37 For example, infants born to women who are obese are more insulin resistant, as measured with a homeostatic model assessment of insulin resistance,38 and this insulin resistance persists into childhood.37 Taken together, these data support the fetal origins hypothesis in suggesting that the obesity epidemic and the subsequent risk of metabolic syndrome may begin in utero.9 An abnormal maternal metabolic environment in women who are pregnant and obese may lead to permanent changes in fetal genetics and epigenetics that underlie the programming of offspring obesity and disease.10
Fetal programming of metabolic function induced by obesity may perpetuate obesity in the next generation.39 To break this vicious cycle and avoid serious consequences for women and their offspring, the prevention and management of maternal obesity during pregnancy through evidence-based interventions are critical.39 Currently, physical activity/exercise (ie, movement) appears to be an efficacious and feasible treatment for this public health problem. As movement experts, physical therapists are well suited to playing a significant role in the prevention and treatment of adverse maternal and neonatal health for both women who are at a healthy weight and women who are overweight or obese.
Physical Activity During Pregnancy
Women who are pregnant are far less active than their counterparts who are not pregnant,40 with only 23% of women who are pregnant reporting that they are exercising in accordance with the guidelines set by the ACOG4; the percentage is even lower for women who are pregnant and obese.5 These low percentages of exercise occur despite strong scientific evidence supporting the physiological benefits and minimal risks of exercise for the mother and her fetus/neonate. Even with the profound anatomical and physiological changes that occur during pregnancy, physical activity has been shown to be safe and effective in women who are pregnant and at all body weights.41 To improve short- and long-term maternal and neonatal health, it is important for both patients and physical therapists to understand all of the benefits (and risks) associated with being physically active during pregnancy.
Maternal Benefits of Physical Activity During Pregnancy in Women Who Are Pregnant and Obese
Physical fitness and physiologic adaptations.
In general, women who are pregnant undergo similar adaptations to exercise training as women who are not pregnant. Women who are pregnant and active perceive improvements in physical health, stamina, muscular strength, energy level, body build, mood, and self-image.42 Concurrent with their perceptions, physical activity in pregnancy leads to significant improvements in maternal aerobic capacity, exercise performance, cardiovascular function (blood pressure, heart rate, and cardiac output), well-being, and mental or emotional health.43–45 In addition, women who are pregnant and active experience fewer adverse pregnancy symptoms, such as insomnia, anxiety, nausea, heartburn, leg cramps, ligament pain, and low back pain46,47; the greatest relief is seen in those who remain active during the entire pregnancy.46 Although these findings were not exclusive to women who were pregnant and obese, many of the cohorts in these studies included women who were overweight or obese. Endurance exercise training has been shown to increase submaximal exercise capacity48 and improve heart rate variability45 exclusively in women who are pregnant and overweight or obese. Taken together, the fitness benefits and physiological adaptations that result from exercise during pregnancy appear to occur in women in all BMI ranges (similar to data for women who are nongravid49).
Labor and delivery outcomes.
Women who are physically active during pregnancy have a lower incidence of abdominal (cesarean) and operative vaginal deliveries, spend less total time in labor, and have a lower risk of acute stress at delivery.50–52 Additionally, women who are physically active during pregnancy are able to recover faster (ie, return to their predelivery activities of daily living faster) after a vaginal delivery than women who are not active during pregnancy.50 Unfortunately, the impact of exercise on labor and delivery outcomes exclusively in women who are pregnant and obese has not been well studied. Some studies have shown no difference in rates of cesarean deliveries between women who are obese and exercise and women who are obese and do not exercise.53–55 One study demonstrated that women who were obese and physically active spent less total time in labor than their counterparts who were not active.54 Although the evidence supporting the benefits of physical activity for labor and delivery outcomes is limited, to date, no studies have demonstrated a harmful effect of physical activity on obstetric outcomes in women who are obese. Therefore, physical activity during pregnancy in women who are obese may improve obstetric outcomes without imposing any harm; however, more research is needed.
GWG and postpartum weight retention.
Similar to the impact of physical activity–associated effects on the weight of women who are nongravid,56 physical activity limits GWG during pregnancy. Women who are physically active during pregnancy gain less weight,43 and the effect of physical activity on GWG also has been shown exclusively in women who are pregnant and obese.53 In a systematic review, women who were obese and were provided with a supervised exercise program gained significantly less weight during pregnancy than women who were obese and were not provided with the program.57 Considering that excessive GWG is the strongest risk factor for maternal overweight and obesity postpartum and is related to many adverse maternal and neonatal outcomes,14,15 the role of maternal exercise in maintaining a healthy pregnancy in women who are obese is substantial.
Preeclampsia.
Physical activity during pregnancy decreases the risk of preeclampsia and other hypertensive disorders.58 These findings extend to women who are pregnant and overweight or obese, as physical activity attenuates the increase in blood pressure and the loss of parasympathetic tone associated with pregnancy in women who are pregnant and overweight or obese.45 With hypertensive disorders being a significant health concern in women who are pregnant and obese, physical activity may be an important way in which these women can decrease the risk of developing preeclampsia.
Insulin resistance and inflammation.
Maternal physical activity during pregnancy improves insulin resistance and inflammation in women who are pregnant and at a healthy weight,59,60 and similar results have been obtained in women who are pregnant and overweight or obese. Relative to women who are pregnant, overweight or obese, and not active, women who are pregnant, overweight or obese, and physically active have a lower level of insulin resistance61 and women who are pregnant, obese, and physically active have a lower level of systemic inflammation.62
Neonatal Benefits of Physical Activity During Pregnancy
The benefits of maternal exercise during pregnancy extend well beyond the mother; the neonate experiences many benefits as well. The benefits begin in utero, as weight-bearing exercise positively correlates with placental growth and volume.63 At the time of delivery, neonates born to women who are physically active have significantly higher 1-minute Apgar scores51 and a lower incidence of acute neonatal stress.50 The effects of maternal physical activity on fetal and neonatal outcomes have not been well studied exclusively in women who are pregnant and obese. Because the risks of issues with fetal growth and complications at delivery are increased in women who are pregnant and obese,23,24 the potential for physical activity to improve these outcomes is an important direction of future study.
Another well-established neonatal benefit of maternal physical activity during pregnancy is healthier infant birth weight. Participation in moderate- to high-intensity exercise throughout pregnancy may contribute to smaller (within a healthy range) and leaner babies in women who are pregnant and at a healthy weight.64 This finding may translate to women who are pregnant and obese, as neonatal abdominal circumference (a measure of body fatness) is inversely associated with physical activity levels in women who are obese.65 However, some studies53,55,62 showed no difference in infant birth weight between women who are pregnant, obese, and active and women who are pregnant, obese, and not active. Therefore, it is possible that maternal physical activity decreases infant birth adiposity but not birth weight. However, more research is needed to confirm this notion.
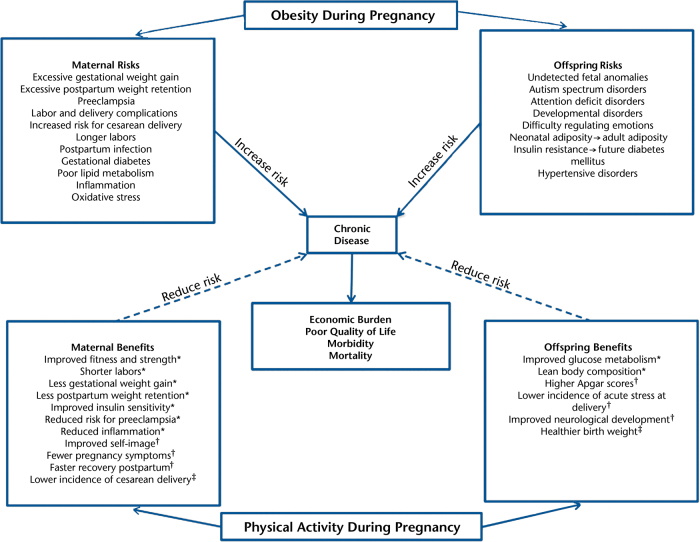
Importantly, the impact of maternal physical activity on neonatal body composition appears to extend into childhood. Higher physical activity levels during pregnancy are associated with lower toddler weights, lower weight-to-height ratios,66 and lower levels of offspring obesity at 8 years of age.67 These data may have serious future ramifications for offspring, as obesity in childhood is a strong predictor of adult adiposity.35 With obesity and its subsequent associated disease states being significant public health concerns, maternal physical activity during pregnancy may play a critical role in the long-term metabolic health of the offspring by reducing the risk of obesity and diabetes later in life. Further support for the impact of maternal physical activity on the metabolic health of neonates for women who are obese is that infants born to women who are obese and exercise during pregnancy are less likely to have hypoglycemia shortly after delivery than those born to women who are obese but do not exercise during pregnancy.53 In addition to the long-term risks of obesity and metabolic disease, evidence from women at a healthy weight has suggested that maternal physical activity can improve offspring neurodevelopment during the first 4 years of life68; however, this notion has not been studied exclusively in women who are pregnant and obese. The Figure summarizes the risks associated with maternal obesity and the benefits of maternal physical activity.
Figure.
Impact of obesity and physical activity on maternal and offspring short-and long-term health. *The benefit has been shown to occur in obese pregnant populations. †The benefit has not been well-studied in exclusively obese pregnant populations. ‡The benefit has been shown to not occur in obese pregnant populations.
Risks of Physical Activity During Pregnancy for Women in All BMI Ranges
The most commonly reported barrier to maternal physical activity participation during pregnancy is concern about the safety of the unborn baby.69 Therefore, women who are pregnant and their health care providers should understand the risks (or lack thereof) of physical activity during pregnancy. Here, we address many common misconceptions about maternal and neonatal risks associated with physical activity during pregnancy for women in all BMI ranges.
Blood flow distribution and fetal heart rate.
Women and their health care providers want to ensure that the uterus, placenta, and fetus are receiving adequate blood flow, oxygen, and nutrients—a reasonable concern considering that blood flow is shunted to skeletal muscle, heart, and skin during exercise.70 During maximal exercise, the reduction in uterine blood flow has been reported to be approximately 20%.71 However, despite a reduction in uterine blood flow, uterine oxygen uptake remains unaltered because of compensatory mechanisms that prevent fetuses from being affected or harmed by changes in uterine blood flow.71,72 Furthermore, maternal exercise during pregnancy is not associated with a decrease in fetal oxygen supply.72 Additional support for the safety of exercise during pregnancy is provided by the fact that after strenuous maximal-effort exercise in the third trimester of pregnancy, umbilical and uterine artery Doppler imaging is unaffected.73 In addition to changes in blood flow, subtle changes in fetal heart rate (typically, an increase in fetal heart rate74) during strenuous exercise have been observed; however, they are mild, transient, and not associated with adverse fetal outcomes.73 Blood flow distribution and fetal heart rate during exercise have not been studied exclusively in women who are pregnant and obese.
Exercise-induced hyperthermia.
Exercise-induced hyperthermia is a common concern for exercising during pregnancy, as animal models have suggested that it may be related to congenital abnormalities.75 However, there is no evidence to support this idea in humans.70 Fetal body temperature does increase with that of the mother by approximately 2°C during high-intensity or maximal exercise71; however, women who are pregnant possess physiologic compensatory mechanisms to protect the fetus.76 There is no evidence that an increase in body temperature during exercise sessions in pregnancy is teratogenic.76 However, maternal and fetal body temperatures during exercise have not been studied in women who are pregnant and obese. In women who are nongravid, the change in core body temperature during exercise is higher in those who are obese than in those who are lean77; therefore, it is reasonable to suggest that body temperature may be elevated at similar exercise intensities in women who are pregnant and obese. Understanding the impact of obesity on body temperature during exercise in women who are pregnant is an important direction of future study.
Pregnancy loss or preterm delivery.
Maternal exercise during pregnancy does not increase the risk of pregnancy loss or placental abruption.78,79 In women who are pregnant and obese (who have a higher risk of pregnancy loss), physical activity during pregnancy does not increase the incidence of miscarriage.53 Furthermore, maternal exercise throughout pregnancy does not cause preterm delivery in women who are pregnant and at a healthy weight80 or obese.53
Risks specific to women who are pregnant and obese.
Many women who are pregnant and obese are considered to be at high risk because of several other factors, including preeclampsia22 and gestational diabetes.18 Therefore, the risks associated with maternal physical activity in women who are pregnant and obese may differ from those in women who are pregnant and at a healthy weight, as their specific conditions would indicate. In most situations, it would be valuable for the physical therapist to calculate a risk-to-benefit ratio to determine whether the potential benefits of physical activity would outweigh the risks. The reality is that women who are pregnant and obese likely have even more to gain from a physically active lifestyle, and this gain may outweigh the potential risks. Although these women may require careful preexercise screening and more vigilant supervision, maternal physical activity should be encouraged. Fortunately, the literature regarding physical activity during pregnancy exclusively in women who are obese indicates that exercise during pregnancy does not appear to be associated with increased harm.41,53,57,62
Exercise Prescription
For women who are nongravid, those who are obese are encouraged to exercise according to the guidelines given by the American College of Sports Medicine but to modify exercise for comorbidities (eg, hypertension, orthopedic limitations, and insulin resistance) and to start with lower intensities and durations until they are able to safely increase those.81 Similarly, women who are pregnant and obese should be encouraged to participate in physical activity during pregnancy.41 The ACOG recommends that women who are obese should modify the current exercise recommendations as necessary and that lower-intensity, shorter-duration, and progressive exercise regimens should be encouraged.41 Although there are no published guidelines for physical activity specific to women who are pregnant and obese, here we discuss the frequencies, durations, intensities, and modes that are recommended by the ACOG for all women who are pregnant, as well as those that have been studied in randomized controlled clinical trials exclusively for women who are overweight or obese.
Frequency and Duration
The ACOG recommends that women who are pregnant participate in 20 to 30 minutes of moderate-intensity aerobic exercise on all or most days of the week.41 Clapp82 also recommended that women who were previously sedentary (eg, women who were pregnant and obese) walk briskly for 20 to 30 minutes on 3 to 5 days per week; exercising for approximately 20 to 30 minutes on 3 to 5 days per week is consistent with exercise interventions safely implemented in women who are pregnant and overweight or obese.45,48,53,55,62,83–85
Intensity
The ACOG suggests using ratings of perceived exertion as an effective means of monitoring exercise intensity because of known heart rate response alterations during pregnancy.41 The ACOG recommends moderate intensity during pregnancy; therefore, on a Borg scale of 6 to 20, a rating of 13 or 14 (somewhat hard) appears to be most appropriate.41 Most exercise recommendations are likely conservative, as high-intensity exercise does not appear to be associated with adverse outcomes.51,71,73 Lotgering concluded that “strenuous exercise in healthy women who are pregnant does not harm the fetus. Thus, the millennia-old perspective has changed.”71(p109) Although most guidelines for exercise intensity can be used in women who are pregnant and obese, the results from several randomized controlled trials suggested that light- to moderate-intensity activity may be best for women who are pregnant and obese86 and that women who are obese and beginning an exercise routine should start at a low intensity and increase as they are able.41
Mode
The ACOG provided a list of recommended physical activities that might be used during pregnancy: walking, swimming, stationary cycling, low-impact aerobics, modified yoga (avoiding positions resulting in decreased venous return), Pilates, running or jogging (if women ran or jogged before pregnancy), racquet sports, and strength training. Petersen et al87 found that walking was, by far, the most common mode of exercise during pregnancy across all BMI categories, followed by aerobics and swimming; these findings are consistent with those of studies exclusively of women who were pregnant and obese.42,49,81 The ACOG also provided a list of several activities that should be avoided, as well as warning signs that exercise during pregnancy should be terminated.41 Regardless of body weight, all women who are pregnant and their health care providers should be aware of these activities and warning signs.
In women who are pregnant and overweight or obese, a variety of exercise programs or modes have been implemented (in short- and long-term studies) and proven safe and effective. These programs or modes include resistance training,83,84 stationary cycling,62,85 aerobics classes,48 and walking.45,53,55 Of note, a meta-analysis of prenatal exercise interventions determined that in women who are pregnant and overweight or obese, supervised physical activity programs with personalized prescriptions or goals are needed to elicit results; therefore, advice from a health care provider may not be enough to improve outcomes in this at-risk population.86 This situation provides a unique opportunity for a movement expert (ie, a physical therapist) to play a crucial role in designing and implementing exercise plans for women who are pregnant and obese. Overall, women who are pregnant and obese should be encouraged to pursue a healthy lifestyle including regular physical activity.41
Exercise Precautions
Although exercising, even at high intensities,71 appears to be safe in healthy pregnancies, numerous precautions should still be taken. A thorough clinical evaluation should be performed before a woman begins any type of exercise during pregnancy.41 The ACOG has produced a list of absolute and relative contraindications to exercise during pregnancy; this list should be considered before the implementation of any type of exercise program during pregnancy. In addition, there are a few other important exercise considerations (ie, avoid end-range-of-motion activities, the Valsalva maneuver, and supine activities).41 In women who are pregnant and obese, there is an increased likelihood of the presence of comorbidities; therefore, careful screening and supervision may be required to ensure safety.
Role of the Physical Therapist in Prescribing Movement During Pregnancy
Movement prescription and advice are inconsistently managed during pregnancy88; to improve maternal and neonatal health outcomes, health care providers need to improve the management of maternal exercise during pregnancy. Physical therapists are considered movement experts89; however, their expertise regarding safe and effective exercise during the prenatal period is often not used. Women who are pregnant appear to obtain their movement advice (if any) from physicians, family, friends, printed materials, the internet, and the media instead of from physical therapists.90 Unfortunately, even physicians may not be well prepared to assist women who are pregnant and could benefit from exercise, as a review of medical schools demonstrated that most US institutions did not offer any courses on physical activity.91 Therefore, physical therapists are the ideal health care professionals for evaluating and prescribing movement to women during pregnancy because their knowledge of biomechanics, pathophysiology, exercise physiology, and pharmacology can result in safe and effective movement prescriptions. In addition to the treatment of pregnancy-related pain and musculoskeletal dysfunction, physical therapist services for women who are pregnant should include safe and targeted movement (ie, physical activity or exercise training) prescriptions.92 Given the growing number of women who are pregnant and have obesity, metabolic disease, or both and the enormous potential for movement therapy to improve outcomes across all BMI categories, the potential for physical therapists to be catalysts for change is significant.
The potential transition of exercise advice and prescription during pregnancy from the current paradigm to a model that includes physical therapists has challenges. Physical therapists are not routinely located in obstetric clinics; therefore, a system for incentivizing and encouraging women to seek care from physical therapists would be necessary. Many states do not require a physician's referral for a physical therapist to begin treatment, although the laws vary by state. In addition, most physical therapist services are covered under medical insurance plans without large out-of-pocket expenses. In states that do not require a physician's referral, simply educating women who are pregnant and their health care team on all of the services that a physical therapist can provide during pregnancy (ie, not just treatment of pain, but tailored exercise prescriptions) might be sufficient stimulus to induce a change in the involvement of physical therapists in the care of women who are pregnant and at all body weights. In states with restrictions, a referral from a physician would be necessary to allow women to seek care from a physical therapist; this situation provides a rationale for the importance of involving the entire obstetric health care team in the management of exercise plans for women who are pregnant. This goal could be facilitated by employing a physical therapist as part of the obstetric health care team—an adaptation of the medical home primary care model.93
Hypothetically, consultation with a physical therapist during pregnancy might result in a reduction in future health care costs (eg, a reduction in the development of maternal and infant morbidity); however, to our knowledge, this notion has not been studied. Data demonstrated the efficacy of physical therapy during the prenatal and postnatal periods for low back or pelvic pain94 and urinary and fetal incontinence95; however, cost analyses associated with these improvements were not conducted. We envision physical therapy playing a holistic role throughout pregnancy not only in educating patients about pain-related issues (eg, low back or pelvic pain prevention or care) and pelvic floor exercises to reduce or prevent postpartum incontinence but also—and most importantly—in providing prenatal exercise to minimize gestational weight gain and to promote maternal and offspring metabolic health.
In conclusion, we believe that physical therapists are ideally suited to work with obstetricians in developing safe, effective movement-based programs for women who are pregnant. Strong evidence supporting the role of obesity in adverse maternal and neonatal outcomes and emerging evidence for the benefits of movement during pregnancy can aid in the empowerment of physical therapists to fulfill and expand their scope of practice into the movement-based treatment of obesity and metabolic disease during pregnancy. With one-third of all women entering pregnancy obese,7 physical therapist involvement in implementing evidence-based exercise interventions is crucial. It is clear that movement-based interventions during pregnancy are safe, feasible, and effective options for improving maternal and neonatal health for women at all body weights. Physical therapists should use their exercise expertise and become more involved in managing movement-based interventions in women who are pregnant and at all body weights, especially those who are overweight or obese. Physical therapists have the ability to improve outcomes for women and their infants by encouraging and prescribing movement during the prenatal period, and their future involvement in prenatal care is critical to combating the vicious cycle of obesity and metabolic disease.
References
- 1. Kim SY, Dietz PM, England L et al. Trends in pre-pregnancy obesity in nine states, 1993–2003. Obesity (Silver Spring). 2007;15:986–993. [DOI] [PubMed] [Google Scholar]
- 2. Yogev Y, Catalano PM. Pregnancy and obesity. Obstet Gynecol Clin North Am. 2009;36:285–300, viii. [DOI] [PubMed] [Google Scholar]
- 3. Sui Z, Dodd JM. Exercise in obese pregnant women: positive impacts and current perceptions. Int J Womens Health. 2013;5:389–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010;50:123–128. [DOI] [PubMed] [Google Scholar]
- 5. Renault K, Norgaard K, Andreasen KR et al. Physical activity during pregnancy in obese and normal-weight women as assessed by pedometer. Acta Obstet Gynecol Scand. 2010;89:956–961. [DOI] [PubMed] [Google Scholar]
- 6. Zylke JW, Bauchner H. The unrelenting challenge of obesity. JAMA. 2016;315:2277–2278. [DOI] [PubMed] [Google Scholar]
- 7. King JC. Maternal obesity, metabolism, and pregnancy outcomes. Annu Rev Nutr. 2006;26:271–291. [DOI] [PubMed] [Google Scholar]
- 8. Catalano PM, McIntyre HD, Cruickshank JK et al. The Hyperglycemia and Adverse Pregnancy Outcome Study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35:780–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barker DJ. The developmental origins of chronic adult disease. Acta Paediatr Suppl. 2004;93:26–33. [DOI] [PubMed] [Google Scholar]
- 10. Heerwagen MJ, Miller MR, Barbour LA, Friedman JE. Maternal obesity and fetal metabolic programming: a fertile epigenetic soil. Am J Physiol Regul Integr Comp Physiol. 2010;299:R711–R722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Almond D, Currie J. Killing me softly: the fetal origins hypothesis. J Econ Perspect. 2011;25:153–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chasan-Taber L, Schmidt MD, Pekow P et al. Predictors of excessive and inadequate gestational weight gain in Hispanic women. Obesity (Silver Spring). 2008;16:1657–1666. [DOI] [PubMed] [Google Scholar]
- 13. Rasmussen KM, Catalano PM, Yaktine AL. New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol. 2009;21:521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Vinter CA, Jensen DM, Ovesen P et al. The LiP (Lifestyle in Pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care. 2011;34:2502–2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Claesson IM, Sydsjo G, Brynhildsen J et al. Weight gain restriction for obese pregnant women: a case-control intervention study. BJOG. 2008;115:44–50. [DOI] [PubMed] [Google Scholar]
- 16. Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–1779. [DOI] [PubMed] [Google Scholar]
- 17. O'Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9–16. [DOI] [PubMed] [Google Scholar]
- 18. Chu SY, Callaghan WM, Kim SY et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care. 2007;30:2070–2076. [DOI] [PubMed] [Google Scholar]
- 19. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33:130–137. [DOI] [PubMed] [Google Scholar]
- 20. Eriksson JG, Forsen T, Tuomilehto J et al. Early growth and coronary heart disease in later life: longitudinal study. BMJ. 2001;322:949–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Osmond C, Kajantie E, Forsén TJ et al. Infant growth and stroke in adult life: the Helsinki birth cohort study. Stroke. 2007;38:264–270. [DOI] [PubMed] [Google Scholar]
- 22. O'Brien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology. 2003;14:368–374. [DOI] [PubMed] [Google Scholar]
- 23. Hilliard AM, Chauhan SP, Zhao Y, Rankins NC. Effect of obesity on length of labor in nulliparous women. Am J Perinatol. 2012;29:127–132. [DOI] [PubMed] [Google Scholar]
- 24. Sebire NJ, Jolly M, Harris JP et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175–1182. [DOI] [PubMed] [Google Scholar]
- 25. Conner SN, Verticchio JC, Tuuli MG et al. Maternal obesity and risk of postcesarean wound complications. Am J Perinatol. 2014;31:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Minsart AF, Buekens P, De Spiegelaere M, Englert Y. Neonatal outcomes in obese mothers: a population-based analysis. BMC Pregnancy Childbirth. 2013;13:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rkhzay-Jaf J, O'Dowd JF, Stocker CJ. Maternal obesity and the fetal origins of the metabolic syndrome. Curr Cardiovasc Risk Rep. 2012;6:487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Basu S, Haghiac M, Surace P et al. Pregravid obesity associates with increased maternal endotoxemia and metabolic inflammation. Obesity (Silver Spring). 2011;19:476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Challier JC, Basu S, Bintein T et al. Obesity in pregnancy stimulates macrophage accumulation and inflammation in the placenta. Placenta. 2008;29:274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cedergren MI, Kallen BA. Maternal obesity and infant heart defects. Obes Res. 2003;11:1065–1071. [DOI] [PubMed] [Google Scholar]
- 31. Hendler I, Blackwell SC, Treadwell MC et al. Does advanced ultrasound equipment improve the adequacy of ultrasound visualization of fetal cardiac structures in the obese gravid woman? Am J Obstet Gynecol. 2004;190:1616–1619. [DOI] [PubMed] [Google Scholar]
- 32. Rodriguez A, Miettunen J, Henriksen TB et al. Maternal adiposity prior to pregnancy is associated with ADHD symptoms in offspring: evidence from three prospective pregnancy cohorts. Int J Obes (Lond). 2008;32:550–557. [DOI] [PubMed] [Google Scholar]
- 33. Krakowiak P, Walker CK, Bremer AA et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 2012;129:e1121–e1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mei Z, Grummer-Strawn LM, Scanlon KS. Does overweight in infancy persist through the preschool years? An analysis of CDC Pediatric Nutrition Surveillance System data. Soz Praventivmed. 2003;48:161–167. [DOI] [PubMed] [Google Scholar]
- 35. Danielzik S, Langnäse K, Mast M et al. Impact of parental BMI on the manifestation of overweight 5–7 year old children. Eur J Nutr. 2002;41:132–138. [DOI] [PubMed] [Google Scholar]
- 36. Catalano PM, Ehrenberg HM. The short- and long-term implications of maternal obesity on the mother and her offspring. BJOG. 2006;113:1126–1133. [DOI] [PubMed] [Google Scholar]
- 37. Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115:e290–e296. [DOI] [PubMed] [Google Scholar]
- 38. HAPO Study Cooperative Research Group, Metzger BE, Lowe LP et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. [DOI] [PubMed] [Google Scholar]
- 39. Galliano D, Bellver J. Female obesity: short- and long-term consequences on the offspring. Gynecol Endocrinol. 2013;29:626–631. [DOI] [PubMed] [Google Scholar]
- 40. Gaston A, Cramp A. Exercise during pregnancy: a review of patterns and determinants. J Sci Med Sport. 2011;14:299–305. [DOI] [PubMed] [Google Scholar]
- 41. ACOG Committee Opinion No. 650: Physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126:e135–e142. [DOI] [PubMed] [Google Scholar]
- 42. Marquez-Sterling S, Perry AC, Kaplan TA et al. Physical and psychological changes with vigorous exercise in sedentary primigravidae. Med Sci Sports Exerc. 2000;32:58–62. [DOI] [PubMed] [Google Scholar]
- 43. Clapp JF., III Exercise during pregnancy: a clinical update. Clin Sports Med. 2000;19:273–286. [DOI] [PubMed] [Google Scholar]
- 44. Shivakumar G. Exercise improves depressive symptoms during pregnancy. BJOG. 2015;122:63. [DOI] [PubMed] [Google Scholar]
- 45. Stutzman SS, Brown CA, Hains SM et al. The effects of exercise conditioning in normal and overweight pregnant women on blood pressure and heart rate variability. Biol Res Nurs. 2010;12:137–148. [DOI] [PubMed] [Google Scholar]
- 46. Sternfeld B, Quesenberry CP Jr, Eskenazi B, Newman LA. Exercise during pregnancy and pregnancy outcome. Med Sci Sports Exerc. 1995;27:634–640. [PubMed] [Google Scholar]
- 47. Goodwin A, Astbury J, McMeeken J. Body image and psychological well-being in pregnancy: a comparison of exercisers and non-exercisers. Aust NZ J Obstet Gynaecol. 2000;40:442–447. [DOI] [PubMed] [Google Scholar]
- 48. Santos IA, Stein R, Fuchs SC et al. Aerobic exercise and submaximal functional capacity in overweight pregnant women: a randomized trial. Obstet Gynecol. 2005;106:243–249. [DOI] [PubMed] [Google Scholar]
- 49. DiPietro L, Stachenfeld NS. Exercise treatment of obesity. In: De Groot LJ, Beck-Peccoz P, Chrousos G et al., eds. Endotext [internet] South Dartmouth, MA: MDTest.com, Inc; 2000:chap 19. [Google Scholar]
- 50. Price BB, Amini SB, Kappeler K. Exercise in pregnancy: effect on fitness and obstetric outcomes—a randomized trial. Med Sci Sports Exerc. 2012;44:2263–2269. [DOI] [PubMed] [Google Scholar]
- 51. Clapp JF., III The course of labor after endurance exercise during pregnancy. Am J Obstet Gynecol. 1990;163:1799–1805. [DOI] [PubMed] [Google Scholar]
- 52. Melzer K, Schutz Y, Soehnchen N et al. Effects of recommended levels of physical activity on pregnancy outcomes. Am J Obstet Gynecol. 2010;202:266.e1–266.e6. [DOI] [PubMed] [Google Scholar]
- 53. Poston L, Bell R, Croker H et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3:767–777. [DOI] [PubMed] [Google Scholar]
- 54. Tinius R, Cahill AG, Cade WT. Impact of physical activity during pregnancy on obstetric outcomes in obese women. J Sports Med Phys Fitness. 2015November12[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Renault KM, Nørgaard K, Nilas L et al. The Treatment of Obese Pregnant Women (TOP) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol. 2014;210:134.e1–134.e9. [DOI] [PubMed] [Google Scholar]
- 56. Jakicic JM, Clark K, Coleman E et al. American College of Sports Medicine position stand: appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2001;33:2145–2156. [DOI] [PubMed] [Google Scholar]
- 57. Sui Z, Moran LJ, Dodd JM. Physical activity levels during pregnancy and gestational weight gain among women who are overweight or obese. Health Promot J Austr. 2013;24:206–213. [DOI] [PubMed] [Google Scholar]
- 58. Meher S, Duley L. Exercise or other physical activity for preventing pre-eclampsia and its complications. Cochrane Database Syst Rev. 2006;2:CD005942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hawkins M, Pekow P, Chasan-Taber L. Physical activity, sedentary behavior, and C-reactive protein in pregnancy. Med Sci Sports Exerc. 2014;46:284–292. [DOI] [PubMed] [Google Scholar]
- 60. Damm P, Breitowicz B, Hegaard H. Exercise, pregnancy, and insulin sensitivity: what is new? Appl Physiol Nutr Metab. 2007;32:537–540. [DOI] [PubMed] [Google Scholar]
- 61. van Poppel MN, Oostdam N, Eekhoff ME et al. Longitudinal relationship of physical activity with insulin sensitivity in overweight and obese pregnant women. J Clin Endocrinol Metab. 2013;98:2929–2935. [DOI] [PubMed] [Google Scholar]
- 62. Tinius RA, Cahill AG, Strand EA, Cade WT. Maternal inflammation during late pregnancy is lower in physically active compared with inactive obese women. Appl Physiol Nutr Metab. 2016;41:191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Clapp JF III, Kim H, Burciu B, Lopez B. Beginning regular exercise in early pregnancy: effect on fetoplacental growth. Am J Obstet Gynecol. 2000;183:1484–1488. [DOI] [PubMed] [Google Scholar]
- 64. Clapp JF III, Capeless EL. Neonatal morphometrics after endurance exercise during pregnancy. Am J Obstet Gynecol. 1990;163:1805–1811. [DOI] [PubMed] [Google Scholar]
- 65. Hayes L, Bell R, Robson S et al. Association between physical activity in obese pregnant women and pregnancy outcomes: the UPBEAT pilot study. Ann Nutr Metab. 2014;64:239–246. [DOI] [PubMed] [Google Scholar]
- 66. Mattran K, Mudd LM, Rudey RA, Kelly JS. Leisure-time physical activity during pregnancy and offspring size at 18 to 24 months. J Phys Act Health. 2011;8:655–662. [DOI] [PubMed] [Google Scholar]
- 67. Mourtakos SP, Tambalis KD, Panagiotakos DB et al. Maternal lifestyle characteristics during pregnancy, and the risk of obesity in the offspring: a study of 5,125 children. BMC Pregnancy Childbirth. 2015;15:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Domingues MR, Matijasevich A, Barros AJ et al. Physical activity during pregnancy and offspring neurodevelopment and IQ in the first 4 years of life. PLoS One. 2014;9:e110050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sui Z, Turnbull D, Dodd J. Enablers of and barriers to making healthy change during pregnancy in overweight and obese women. Australas Med J. 2013;6:565–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Morris SN, Johnson NR. Exercise during pregnancy: a critical appraisal of the literature. J Reprod Med. 2005;50:181–188. [PubMed] [Google Scholar]
- 71. Lotgering FK. 30(+) years of exercise in pregnancy. Adv Exp Med Biol. 2014;814:109–116. [DOI] [PubMed] [Google Scholar]
- 72. Clapp JF., III The effects of maternal exercise on fetal oxygenation and feto-placental growth. Eur J Obstet Gynecol Reprod Biol. 2003;110(suppl 1):S80–S85. [DOI] [PubMed] [Google Scholar]
- 73. Szymanski LM, Satin AJ. Strenuous exercise during pregnancy: is there a limit? Am J Obstet Gynecol. 2012;207:179.e1–179.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Clapp JF III, Little KD, Capeless EL. Fetal heart rate response to sustained recreational exercise. Am J Obstet Gynecol. 1993;168:198–206. [DOI] [PubMed] [Google Scholar]
- 75. Edwards MJ, Walsh DA, Webster WS, Lipson AH. Hyperthermia: is it a “direct” embryonic teratogen? Teratology. 1986;33:375–378. [DOI] [PubMed] [Google Scholar]
- 76. Clapp JF., III The changing thermal response to endurance exercise during pregnancy. Am J Obstet Gynecol. 1991;165:1684–1689. [DOI] [PubMed] [Google Scholar]
- 77. Eijsvogels TM, Veltmeijer MT, Schreuder TH et al. The impact of obesity on physiological responses during prolonged exercise. Int J Obes (Lond). 2011;35:1404–1412. [DOI] [PubMed] [Google Scholar]
- 78. Committee on Obstetric Practice. ACOG committee opinion: exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002;77:79–81. [DOI] [PubMed] [Google Scholar]
- 79. Clapp JF., III The effects of maternal exercise on early pregnancy outcome. Am J Obstet Gynecol. 1989;161:1453–1457. [DOI] [PubMed] [Google Scholar]
- 80. Barakat R, Pelaez M, Montejo R et al. Exercise throughout pregnancy does not cause preterm delivery: a randomized, controlled trial. J Phys Act Health. 2014;11:1012–1017. [DOI] [PubMed] [Google Scholar]
- 81. McQueen MA. Exercise aspects of obesity treatment. Ochsner J. 2009;9:140–143. [PMC free article] [PubMed] [Google Scholar]
- 82. Clapp JF., III A clinical approach to exercise during pregnancy. Clin Sports Med. 1994;13:443–458. [PubMed] [Google Scholar]
- 83. Brankston GN, Mitchell BF, Ryan EA, Okun NB. Resistance exercise decreases the need for insulin in overweight women with gestational diabetes mellitus. Am J Obstet Gynecol. 2004;190:188–193. [DOI] [PubMed] [Google Scholar]
- 84. Barakat R, Lucia A, Ruiz JR. Resistance exercise training during pregnancy and newborn's birth size: a randomised controlled trial. Int J Obes (Lond). 2009;33:1048–1057. [DOI] [PubMed] [Google Scholar]
- 85. Ong MJ, Guelfi KJ, Hunter T et al. Supervised home-based exercise may attenuate the decline of glucose tolerance in obese pregnant women. Diabetes Metab. 2009;35:418–421. [DOI] [PubMed] [Google Scholar]
- 86. Choi J, Fukuoka Y, Lee JH. The effects of physical activity and physical activity plus diet interventions on body weight in overweight or obese women who are pregnant or in postpartum: a systematic review and meta-analysis of randomized controlled trials. Prev Med. 2013;56:351–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Petersen AM, Leet TL, Brownson RC. Correlates of physical activity among pregnant women in the United States. Med Sci Sports Exerc. 2005;37:1748–1753. [DOI] [PubMed] [Google Scholar]
- 88. Lewis E. Exercise in pregnancy. Aust Fam Physician. 2014;43:541–542. [PubMed] [Google Scholar]
- 89. Sahrmann SA. The human movement system: our professional identity. Phys Ther. 2014;94:1034–1042. [DOI] [PubMed] [Google Scholar]
- 90. Evenson KR, Bradley CB. Beliefs about exercise and physical activity among pregnant women. Patient Educ Couns. 2010;79:124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Cardinal BJ, Park EA, Kim M, Cardinal MK. If exercise is medicine, where is exercise in medicine? Review of U.S. medical education curricula for physical activity-related content. J Phys Act Health. 2015;12:1336–1343. [DOI] [PubMed] [Google Scholar]
- 92. Gleeson PB, Pauls JA. Obstetrical physical therapy: review of the literature. Phys Ther. 1988;68:1699–1702. [DOI] [PubMed] [Google Scholar]
- 93. Epperly T. The patient-centred medical home in the USA. J Eval Clin Pract. 2011;17:373–375. [DOI] [PubMed] [Google Scholar]
- 94. van Benten E, Pool J, Mens J, Pool-Goudzwaard A. Recommendations for physical therapists on the treatment of lumbopelvic pain during pregnancy: a systematic review. J Orthop Sports Phys Ther. 2014;44:464–473, A1–A15. [DOI] [PubMed] [Google Scholar]
- 95. Boyle R, Hay-Smith EJ, Cody JD, Mørkved S. Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women: a short version Cochrane review. Neurourol Urodyn. 2014;33:269–276. [DOI] [PubMed] [Google Scholar]