Key Points
Question
Does an association exist between objectively measured age-related hearing loss and depression in Hispanic adults?
Findings
In this cross-sectional study of 5328 Hispanic adults 50 years or older from 4 US communities, audiometric hearing loss was associated with clinically relevant depressive symptoms as assessed using the Center for Epidemiologic Studies Depression Scale, 10-item version, adjusting for hearing aid use, age, sex, educational level, study site, geographic background, cardiovascular disease, and antidepressant use. The odds of having clinically significant depressive symptoms increased approximately 45% for every 20-dB increase in hearing loss.
Meaning
Objectively measured hearing loss appears to be independently associated with clinically significant depressive symptoms in older Hispanic individuals.
Abstract
Importance
Age-related hearing loss is highly prevalent and has recently been associated with numerous morbid conditions of aging. Late-life depression is also prevalent and can be resistant to available treatments. Preliminary studies examining the association between hearing loss and late-life depression have been limited by subjective hearing measures, small sample sizes, and primarily white populations.
Objective
To assess whether a cross-sectional association exists between objective audiometric hearing loss and depressive symptoms in older Hispanic adults.
Design, Setting, and Participants
This cross-sectional study uses 2008-2011 Hispanic Community Health Study/Study of Latinos data collected in Miami, Florida, San Diego, California, Chicago, Illinois, or the Bronx, New York, from 5328 Hispanic adults 50 years or older who had exposure, outcome, and covariate data. Data analyses were conducted from March 2018 to September 2018.
Exposure
Audiometric hearing loss (pure-tone average).
Main Outcomes and Measures
Center for Epidemiologic Studies Depression Scale, 10-item version (CESD-10) score of 10 or higher, which indicates clinically significant depressive symptoms.
Results
The median age (interquartile range) of the 5328 participants was 58 (53-63) years, and 3283 participants (61.6%) were female. The mean (SD) CESD-10 score was 7.7 (6.4). Of the 5328 included participants, 1751 (32.9%) had clinically significant depressive symptoms. The odds of having these symptoms increased 1.44 (95% CI, 1.27-1.63) times for every 20 dB of hearing loss, adjusting for hearing aid use, age, sex, educational level, study site, geographic background, cardiovascular disease, and antidepressant use. Compared with those for individuals with normal hearing (0 dB), the odds of having clinically significant depressive symptoms was 1.81 (95% CI, 1.48-2.22) times as high in individuals with mild hearing loss (median threshold, 32.5 dB), 2.38 (95% CI, 1.77-3.20) times as high in individuals with moderate hearing loss (median threshold, 47.5 dB), and 4.30 (95% CI, 2.61-7.09) times as high in individuals with severe hearing loss (median threshold, 80 dB).
Conclusions and Relevance
Objective hearing loss appears to be associated with clinically significant depressive symptoms in older Hispanic people, with greater hearing loss seemingly associated with greater odds of having depressive symptoms. Given the high prevalence of untreated hearing loss in older adults, hearing loss may be a potentially modifiable risk factor for late-life depression.
This multicenter, cross-sectional study uses Community Health Study/Study of Latinos data collected from 4 US communities to assess whether an association exists between age-related, audiometrically measured hearing loss and clinically relevant depressive symptoms in Hispanic adults 50 years or older.
Introduction
Age-related hearing loss (HL) has historically been considered a clinically inconsequential result of aging. At worst a quality of life issue, age-related HL had no strong evidence linking it with more concerning health conditions. However, in the last decade, mounting evidence has suggested that hearing may have broader implications, including for mental1,2,3,4 and neurocognitive health.5,6 Although causation between HL and neuropsychiatric outcomes has yet to be proven, there is early mechanistic evidence, including accelerated brain volume decrease, in those with HL.7 A recent article predicted that preventing or treating HL may result in the single largest percentage rate reduction in dementia prevalence of any known risk factor.8 This is based on the very high prevalence of age-related HL, which affects two-thirds of those older than 70 years, or 38 million Americans overall.9
Data suggesting a link between HL and depression have been more variable.10 Some, but not all, existing studies have shown associations between these conditions, but even those studies showing an association rely largely on subjectively determined (ie, self-reported) HL,11,12 which is a suboptimal measure.13 For example, many of these studies evaluated responses having a simple yes or no answer to the question of whether an individual noticed HL. More recent studies implementing audiometric testing have shown inconsistent results1,2,3,4 and have been limited to largely white cohorts.
Elucidating risk factors for late-life depression is important because it is prevalent and disabling in older adults. Late-life depression is also frequently resistant to empirical administration of medications (ie, antidepressants) that are not tailored to a specific cause in a given patient. Because HL is readily measurable, modifiable (via hearing aids or cochlear implants), and highly prevalent in later life, demonstrating a link between HL and late-life depression may provide a therapeutically actionable strategy to alleviate depression in the subgroup of patients with comorbid HL.9
In the present study, we examined whether an association exists between audiometrically measured HL and clinically significant depressive symptoms using data from the Hispanic Community Health Study/Study of Latinos (HCHS). We were particularly interested in evaluating whether this association exists in a racial/ethnic minority because few Hispanic people14 have been evaluated for this association to date.14,15 Depression prevalence has also been reported to be higher in Hispanic people than in other ethnic/racial groups (eg, 26.1% in Hispanic participants compared with 21.5% in non-Hispanic white participants by 1 estimate).16,17,18 Furthermore, depression may be underdiagnosed in Hispanic individuals owing to language, cultural, and health literacy barriers as well as to different (eg, more somatic) presentations.19 We hypothesized that HL in Hispanic individuals would be associated with higher odds of having depressive symptoms.1
Methods
Participants and Data Source
The HCHS is a multicenter, prospective, community-based cohort study conducted in the United States. The HCHS has a uniquely large sample of Hispanic people with audiometric hearing data (n = 16 415 before exclusions) and is the largest study to date (by a factor of 4; n = 5328 after exclusions vs n = 1332 in the previously largest study11) to examine associations between HL and depression. The HCHS data set includes data from interviews, physical examinations, and specialty tests (eg, neuropsychological testing, electrocardiogram, laboratory blood workup, and actigraph recording results). Audiometry is included for all participants. Currently, only 1 wave of data, collected from 2008 to 2011, are publicly available, enabling cross-sectional analysis. The present study using the HCHS data was approved by the Columbia University Institutional Review Board, New York, New York, which also waived the need for obtaining informed patient consent because these data are publicly available.
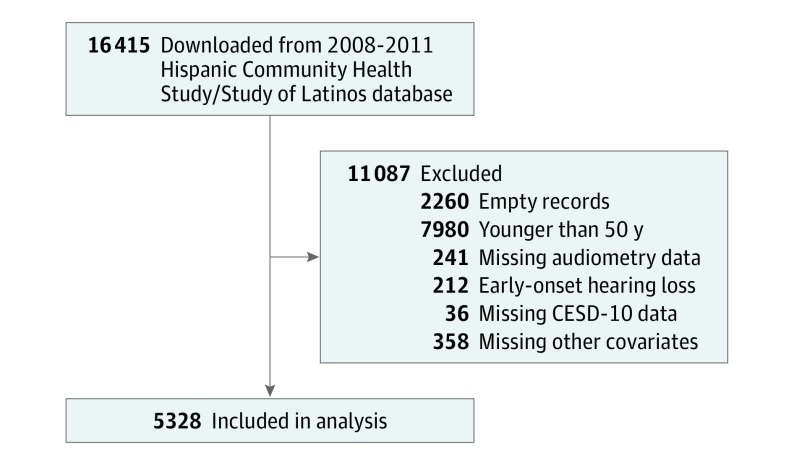
The Figure is a flowchart showing participant data screening and exclusions. In total, 16 415 participants were included in the downloaded data set. Of those, 2260 participants were eliminated because their records were empty. In addition, 7980 participants younger than 50 years as well as 212 participants with early-onset HL were excluded to restrict the analysis to age-related HL. Participants with missing audiometry results, Center for Epidemiologic Studies Depression Scale, 10-item version (CESD-10) scores, or covariate data were also excluded. Thus, 5328 participants were included in the final analysis.
Figure. Flowchart of Enrollment and Inclusion for Analysis.
CESD-10 indicates Center for Epidemiologic Studies Depression Scale, 10-item version.
Exposure
Pure-tone audiometry across frequencies 500 Hz to 8000 Hz was performed in dedicated sound-isolated rooms by trained examiners.20 The 4 frequency pure-tone average (PTA) was calculated for each ear from the decibel hearing level threshold at 500, 1000, 2000, and 4000 Hz. The HL was based on the PTA of the better hearing ear and unilateral HL was excluded.
For regression modeling, HL was used as a continuous variable. However, for clinical purposes, HL is often described categorically. For this reason, model-based odds ratios (ORs) are presented for comparing specific categories of HL. The severity of HL was categorized as follows21: absent or normal, 0 to 25 dB; mild, 26 to 40 dB; moderate, 41 to 55 dB; moderately severe, 56 to 70 dB; severe 71 to 90 dB; and profound, 91 dB or worse. Because there were few participants with severe or profound HL, those categories were aggregated with the moderately severe HL category.
Outcomes
Depressive symptoms were measured with the CESD-10 instrument. Regression analysis primarily used a binarized CESD-10 score. Clinically significant depressive symptoms were defined using a CESD-10 score cut point of 10 or higher, which has been associated with greater disability and adverse health outcomes in older adults.22,23 Those scores have also been shown to have good predictive accuracy compared with the standard CESD-20 cut point of 16 or higher.24 Alternative outcomes were used as part of sensitivity analyses, which included defining depressive symptoms with a CESD-10 cut point of 16 or higher25 as well as defining depressive symptoms as use of antidepressants.
Covariates
In the multivariable models, we adjusted for covariates that might alter or confound the association between HL and depression. This included hearing aid use, demographics (age, sex, educational level in years, study site, and geographic background), and cardiovascular disease. Cardiovascular disease is a potential confounder because it may cause both HL26 and depression.27 A composite cardiovascular disease variable was created to address possible multicollinearity of risk factors, as previously described.28 One point was assigned for each of the following 3 individual cardiovascular disease variables if present: coronary artery disease (any of prior electrocardiogram reports of old or possible old myocardial infarction, history of angina, history of heart attack, angioplasty, or cardiac surgery), measured hypertension, or self-reported stroke. An additional 1 or 2 points were added for laboratory-defined diabetes (1 point for impaired glucose tolerance and 2 points for diabetes). In the final model, we also adjusted for antidepressant use (yes or no by documented prescription of any antidepressant class plus self-declared use in the previous 4 weeks).
The likelihood of HL differs across race/ethnic groups.29 However, data about race/ethnicity were missing in more than a third of study participants. For this reason, we did not consider race/ethnicity in the primary analysis. For participants in whom race/ethnic data were available (Asian, Hawaiian Native or Pacific Islander, black, white, or multiracial), we included race/ethnic group as an additional covariate in part of the sensitivity analysis.
Statistical Analysis
The Shapiro-Wilk test was used to assess normality of the continuous variables. Spearman correlation was used to examine the association between continuous CESD-10 scores and hearing.
Regression modeling was used to assess associations between predictors and depression status. Logistic regression was used because outcomes of interest were binary and because the existing literature examining the association between HL and depression overwhelmingly uses logistic regression,1,2,3,4 enabling comparisons with results from previous studies. A univariable model with HL as the predictor was created first, followed by multivariable analysis.
Because logistic regression analysis does not directly estimate prevalence ratios, and the odds ratio does not approximate the prevalence ratio when the outcome is common (as in our sample), we additionally fit log-linear regression models using the same outcome and predictors as the logistic models described above. Model-based prevalence ratios and their corresponding 95% CIs are reported in an additional analysis.
Hearing loss was included in each model as a continuous predictor. An initial Loess fit (binary depression status vs HL) was used to obtain empirical logits, which were plotted against PTA hearing to reveal an approximately linear relationship. Hence, PTA hearing was assumed to have a linear association with the log odds of depression in all logistic models.
Unless otherwise indicated, all estimates are presented with 95% CIs. Data analysis was performed from March 2018 to September 2018 using R, version 3.4.3 (R Foundation for Statistical Computing) with RStudio, version 1.1.423 (RStudio, Inc). No external packages were used for the main analysis. Log-linear models were performed using the core Stats package (glm function, with Poisson family and log link).
Results
Sample Characteristics
Baseline participant characteristics stratified by HL category are given in Table 1. The median (interquartile range) age of participants was 58 (53-63) years old. Most participants (3283 [61.6%]) were women, a reflection of enrollment patterns in HCHS. The majority of participants (4387 [82.3%]) had no HL, 749 (14.1%) had mild HL, 143 (2.7%) had moderate HL, and 49 (0.9%) had moderately severe or worse HL. The mean (SD) CESD-10 score was 7.7 (6.4). Clinically significant depressive symptoms (CESD-10 score ≥10) were present in 1405 (32.0%) of those without HL, 254 (33.9%) of those with mild HL, 64 (44.8%) of those with moderate HL, and 28 (57.1%) of those with moderately severe or worse HL.
Table 1. Participant Characteristics by Hearing Loss Category.
| Characteristic | Total | No HL (0-25 dB) | Mild HL (26-40 dB) | Moderate HL (41-55 dB) | Moderately Severe or Worse HL (>55 dB) |
|---|---|---|---|---|---|
| No. | 5328 | 4387 | 749 | 143 | 49 |
| Hearing aid use | |||||
| No. (%) | 47 (0.9) | 9 (0.2) | 8 (1.1) | 18 (12.6) | 12 (24.5) |
| OR vs no HL (98.3% CI)a | … | 1 [Reference] | 5.2 (1.4-19.2) | 69.7 (24.5-222.4) | 155.3 (46.0-565.9) |
| Age | |||||
| Mean (SD) | 58.5 (6.3) | 57.7 (5.9) | 61.8 (6.6) | 63.6 (7.3) | 63.6 (6.1) |
| Difference vs no HL (98.3% CI) | … | 1 [Reference] | 4.1 (3.5-4.7) | 5.9 (4.4-7.4) | 5.9 (3.7-8.1) |
| Male | |||||
| No. (%) | 2045 (38.4) | 1546 (35.2) | 402 (53.7) | 74 (51.7) | 23 (46.9) |
| OR vs no HL (98.3% CI) | … | 1 [Reference] | 2.1 (1.8-2.6) | 2.0 (1.3-3.0) | 1.6 (0.8-3.2) |
| Study site, No. (%) | |||||
| Bronx, NY | 1296 (24.3) | 1054 (24.0) | 188 (25.1) | 31 (21.7) | 23 (46.9) |
| Chicago, IL | 1169 (21.9) | 968 (22.1) | 161 (21.5) | 31 (21.7) | 9 (18.4) |
| Miami, FL | 1638 (30.7) | 1346 (30.7) | 240 (32.0) | 41 (28.7) | 11 (22.4) |
| San Diego, CA | 1225 (23.0) | 1019 (23.2) | 160 (21.4) | 40 (28.0) | 6 (12.2) |
| Study site, OR vs Bronx (in HL vs no HL) (98.3% CI) | |||||
| Bronx | … | … | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Chicago | … | … | 0.9 (0.7-1.2) | 1.1 (0.6-2.0) | 0.4 (0.2-1.1) |
| Miami | … | … | 1.0 (0.8-1.3) | 1.0 (0.6-1.8) | 0.4 (0.2-0.9) |
| San Diego | … | 1 [Reference] | 0.9 (0.7-1.2) | 1.3 (0.7-2.4) | 0.3 (0.1-0.8) |
| Geographic background, No. (%) | |||||
| Dominican Republic | 469 (8.8) | 400 (9.1) | 62 (8.6) | 3 (2.1) | 4 (8.2) |
| Central or South America | 905 (17.0) | 773 (17.6) | 110 (14.7) | 16 (11.2) | 6 (12.2) |
| Cuba | 1044 (19.6) | 837 (19.1) | 170 (22.7) | 28 (19.6) | 9 (18.4) |
| Mexico | 1780 (33.4) | 1481 (33.8) | 229 (30.6) | 60 (42.0) | 10 (20.4) |
| Puerto Rico | 1029 (19.3) | 815 (18.6) | 163 (21.8) | 33 (23.1) | 18 (36.7) |
| Other or multiple | 101 (1.9) | 81 (1.8) | 15 (2.0) | 3 (2.1) | 2 (4.1) |
| Geographic background, OR vs Dominican Republic (in HL vs no HL) (98.3% CI) | |||||
| Dominican Republic | … | … | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Central or South America | … | … | 0.9 (0.6-1.4) | 2.8 (0.6-22.7) | 0.8 (0.1-5.4) |
| Cuba | … | … | 1.3 (0.9-2.0) | 4.5 (1.1-35.1) | 1.1 (0.2-6.8) |
| Mexico | … | … | 1.0 (0.7-1.5) | 5.4 (1.5-41.1) | 0.7 (0.2-4.2) |
| Puerto Rico | … | … | 1.3 (0.9-1.9) | 5.4 (1.4-42.1) | 2.2 (0.6-12.7) |
| Other or multiple | … | 1 [Reference] | 1.2 (0.5-2.6) | 4.9 (0.4-58.1) | 2.5 (0.1-25.5) |
| Educational level, y | |||||
| Mean (SD) | 10.4 (4.7) | 10.7 (4.7) | 9.4 (4.6) | 8.6 (4.4) | 8.5 (4.6) |
| Difference vs no HL (98.3% CI) | … | 1 [Reference] | −1.2 (−0.8 to −1.7) | −2.1 (−1.2 to −3.0) | −2.2 (−0.6 to −3.8) |
| Antidepressant use | |||||
| No. (%) | 533 (10.0) | 424 (9.7) | 88 (11.7) | 15 (10.5) | 6 (12.2) |
| OR vs no HL (98.3% CI) | … | 1 [Reference] | 1.2 (0.9-1.7) | 1.1 (0.5-2.1) | 1.3 (0.3-3.6) |
| Cardiovascular disease scoreb | |||||
| Mean (SD) | 1.7 (1.1) | 1.6 (1.1) | 1.9 (1.1) | 2.0 (1.1) | 2.2 (1.2) |
| Difference vs no HL (98.3% CI) | … | 1 [Reference] | 0.3 (0.2-0.4) | 0.4 (0.2-0.6) | 0.5 (0.1-1.0) |
| Cardiovascular disease score components, No. (%) | |||||
| Coronary artery disease | 616 (11.6) | 465 (10.6) | 111 (14.8) | 26 (18.2) | 14 (28.6) |
| Hypertension | 2558 (48.0) | 2032 (46.3) | 412 (55.0) | 84 (58.7) | 30 (61.2) |
| Stroke | 138 (2.6) | 100 (2.3) | 29 (3.9) | 5 (3.5) | 4 (8.2) |
| Diabetes | … | … | … | … | … |
| Impaired glucose tolerance | 2649 (49.7) | 2195 (50.0) | 365 (48.7) | 67 (46.9) | 22 (44.9) |
| Diabetes | 1481 (27.8) | 1158 (26.4) | 250 (33.4) | 55 (38.5) | 18 (36.7) |
| Cardiovascular disease score components, OR vs Reference (98.3% CI)b | |||||
| Coronary artery disease | … | 1 [Reference] | 1.5 (1.1-1.9) | 1.9 (1.1-3.2) | 3.4 (1.6-7.3) |
| Hypertension | … | 1 [Reference] | 1.4 (1.2-1.7) | 1.7 (1.1-2.5) | 1.8 (0.9-3.7) |
| Stroke | … | 1 [Reference] | 1.7 (1.0-2.9) | 1.6 (0.4-4.5) | 3.8 (0.7-12.8) |
| Diabetes, OR vs not impaired (in HL vs no HL) (98.3% CI) | 1 [Reference] | ||||
| Impaired glucose tolerance | … | … | 1.3 (1.0-1.7) | 1.5 (0.8-2.8) | 1.2 (0.4-3.0) |
| Diabetes | … | … | 1.7 (1.3-2.2) | 2.3 (1.3-4.4) | 1.8 (0.7-4.8) |
| CESD-10 score | |||||
| Mean (SD) | 7.7 (6.4) | 7.7 (6.4) | 7.8 (6.5) | 8.6 (6.7) | 10.5 (7.2) |
| Difference vs no HL (98.3% CI) | … | 1 [Reference] | 0.1 (−0.5 to 0.7) | 1.0 (−0.4 to 2.3) | 2.9 (0.3-5.4) |
| Clinically significant depressive symptoms | |||||
| CESD-10 score ≥10 | |||||
| No. (%) | 1751 (32.9) | 1405 (32.0) | 254 (33.9) | 64 (44.8) | 28 (57.1) |
| OR vs no HL (98.3% CI) | … | 1 [Reference] | 1.1 (0.9-1.3) | 1.7 (1.1-2.6) | 2.8 (1.4-5.7) |
| CESD-10 score ≥16 | |||||
| No. (%) | 690 (13.0) | 557 (12.7) | 102 (13.6) | 19 (13.3) | 12 (24.5) |
| OR vs no HL (98.3% CI) | … | 1 [Reference] | 1.1 (0.8-1.4) | 1.1 (0.6-1.9) | 2.2 (1.0-5.0) |
Abbreviations: CESD-10, Center for Epidemiologic Studies Depression Scale, 10-item version; HL, hearing loss; OR, odds ratio; …, not applicable.
All 98.3% CIs correspond to a conservative Bonferroni adjustment for 3 comparisons.
Cardiovascular disease score ranges from 0 (lowest) to 5 (highest). Points were assigned for each prevalent component (1 point each for coronary artery disease, hypertension, stroke, or impaired glucose tolerance and 2 points for diabetes).
Univariable Model
In the univariable model, the odds of clinically significant depressive symptoms (defined as CESD-10 score ≥10) were 1.27 (95% CI, 1.14-1.41) times as high per 20 dB of HL (Table 2).30 An increase in 20-dB HL is approximately equivalent to a 1-category worsening (ie, across categories of normal, mild, moderate, moderately severe, severe, and profound).
Table 2. Data From Logistic Regression Models for Clinically Significant Depressive Symptoms Among 5328 Older Hispanic Adultsa.
| Model | OR per 20-dB Hearing Loss (95% CI)b |
|---|---|
| 1. Hearing lossc | 1.27 (1.14-1.41) |
| 2. Above + hearing aidd | 1.29 (1.16-1.44) |
| 3. Above + demographicse | 1.47 (1.30-1.66) |
| 4. Above + cardiovascular risk factorsf | 1.46 (1.29-1.65) |
| 5. Above + antidepressant use (fully adjusted model) | 1.44 (1.27-1.63) |
Abbreviation: OR, odds ratio.
Assessed as Center for Epidemiologic Studies Depression Scale, 10-item version, score of 10 or higher.
A 20-dB increase in hearing loss is approximately equivalent to a 1-category worsening (categories are: normal, mild, moderate, moderately severe, severe, profound).
Based on magnitude of pure-tone average in better-hearing ear.
Hearing aid use in the previous year (yes or no).
Demographics include age, sex, educational level, study site, and geographic background.
Includes coronary artery disease (test defined), hypertension (measured), stroke (self-reported), diabetes (laboratory defined).
Multivariable Model
Adjusting for hearing aid use, the odds of clinically significant depressive symptoms (defined as a CESD-10 score ≥10) were 1.29 (95% CI, 1.16-1.44) per 20 dB of HL. In addition, adjusting for demographic factors, including age, sex, educational level, study site, and geographic background, increased the OR to 1.47 (95% CI, 1.30-1.66). Adding cardiovascular risk factors to this model had a negligible effect. Finally, adding antidepressant use to the model slightly decreased the clinically significant depressive symptoms OR to 1.44 (95% CI, 1.27-1.63). This latter model is referred to as the fully adjusted model (Table 2). In summary, the odds of clinically significant depressive symptoms increased 1.44 (95% CI, 1.27-1.63) times for every 20-dB increase in HL, adjusting for hearing aid use, numerous demographic factors, cardiovascular disease, and antidepressant use.
The fully adjusted model was then used to calculate the odds of clinically significant depressive symptoms for each category of HL (the median within-category value was chosen) compared with normal hearing (0 dB). The odds of clinically significant depressive symptoms were 1.81 (95% CI, 1.48-2.22) times as high for mild HL (32.5 dB), 2.38 (95% CI, 1.77-3.20) times as high for moderate HL (47.5 dB), 3.12 (95% CI, 2.12-4.62) times as high for moderately severe HL (62.5 dB), and 4.30 (95% CI, 2.61-7.09) times as high for severe HL (80 dB).
We included the interaction between HL and sex in the fully adjusted model to assess whether the association between HL and depression status was modified by sex but found no evidence of an interaction (interaction coefficient OR, 1.00; 95% CI, 0.99-1.02). Similarly, we found no evidence of an interaction between HL and antidepressant use (interaction coefficient OR, 0.99; 95% CI, 0.99-1.01). When stratified by antidepressant use, the odds of clinically significant depressive symptoms were 1.43 (95% CI, 1.25-1.63) times as high per 20 dB of HL in those who were not using antidepressants. By comparison, the odds were 1.59 (95% CI, 1.05-2.48) times as high for those who were using antidepressants.
We examined alternative outcomes as part of a sensitivity analysis. When antidepressant use was included as a surrogate outcome of depression, an association with HL was still observed. In the fully adjusted model with antidepressant use as the outcome (instead of a covariate), the odds of antidepressant use were 1.21 (95% CI, 1.01-1.44) times as high per 20 dB of HL (eTable 1 in the Supplement). When a CESD-10 cut-point score of 16 (instead of 10) was used as an alternative outcome, an even higher OR of 1.49 (95% CI, 1.27-1.75) was found, adjusting for the same covariates as the fully adjusted model (eTable 2 in the Supplement).
We also examined race/ethnicity as a covariate as part of the sensitivity analysis. We found no significant association between HL and race for either the univariable regression or the multivariable regression adjusting for demographic characteristics. Race/ethnicity was omitted from the main models because more than one-third of participants lacked race/ethnic data. In the fully adjusted model restricted to 3511 participants with available race/ethnic data, adding race/ethnicity as a covariate had no effect on the association between HL and depressive symptoms (before and after adding race/ethnicity OR, 1.48; 95% CI, 1.26-1.73).
Few participants (47 [0.9%]) used a hearing aid. Restricting the full model to the 5281 participants without hearing aids had virtually no effect on the association between HL and depressive symptoms (excluding hearing aid participants OR, 1.43; 95% CI, 1.26-1.62 vs with all participants OR, 1.44; 95% CI, 1.27-1.63).
Finally, log-linear regression was performed to directly estimate prevalence ratios. In the fully adjusted model, the prevalence of clinically significant depressive symptoms increased 1.23 (95% CI, 1.12-1.34) times for every 20-dB increase in HL, adjusting for hearing aid use, demographics, cardiovascular disease, and antidepressant use (eTable 3 in the Supplement).
Discussion
Age-related HL loss has been recognized as a risk factor for many conditions of public health concern, most notably cognitive impairment and dementia.5,6,31 The association between HL and depression, 2 common conditions of older life, has remained less rigorously defined. We found a strong and robust association between audiometric HL and clinically significant depressive symptoms as defined by a CESD-10 score of 10 or higher.24
In the fully adjusted model, accounting for hearing aid use, age, sex, educational level, study site, geographic background, cardiovascular disease, and antidepressant use, the odds of clinically significant depressive symptoms increased nearly 1.5 times for every 20 dB of HL. This 20-dB change is approximately the difference between categories of HL, for example, mild vs normal, or moderate vs mild. An individual with mild HL (32.5 dB median threshold) had nearly twice the odds of having clinically significant depressive symptoms compared with someone with normal hearing (0-dB threshold). An individual with moderate HL had nearly 2.5 times the odds of having clinically significant depressive symptoms, whereas an individual with severe HL had more than 4 times the odds.
Hearing loss may be associated with depression through the mediating effect of socialization. Hearing loss may lead to social isolation32 and loneliness,33,34 which, in turn, could result in depression. This pathway may be modifiable because loneliness has been shown to improve with certain treatments for HL.34,35 Furthermore, in an early randomized clinical trial, HL treatment with hearing aids improved both social function and depressive symptoms.36
Previous studies on the association between HL and depression have largely relied on nonaudiometric subjective HL assessments.11,12 Although associations were found, subjective HL is not an ideal measure.13 Particularly in studies of depression, subjective HL may be exaggerated owing to reverse causation, whereby depressed individuals may have a worse subjective perception of their abilities.
Other studies that have examined objective audiometric HL have found weak1 or absent3,4 associations. A recent study by our group in a smaller, non-Hispanic cohort did find an association between audiometric HL and depressive symptoms.14 The present study provides a more robust statistical analysis, including adjustments for numerous confounders. One study in Chinese individuals also showed associations between audiometric HL and depression. However, sample sizes were smaller and variables were not analyzed as continuous, which limited the analysis.2 To our knowledge, the sample size in the present study is the largest to date for studies examining HL and depression, by a factor of 4.11 The present study also extends the earlier findings in Chinese2 and largely white14 individuals to a different ethnic group (Hispanic people). These data suggest that the association between HL and depression may be generalizable across multiple races/ethnicities.
It is important to study the association between HL and depression in the Hispanic population, the fastest growing ethnicity in the United States. Hispanic people have accounted for half of all US population growth since 2000.37 Depression may also be more prevalent in Hispanic people compared with other ethnic/racial groups.16,17 Indeed, we found a relatively high prevalence of depressive symptoms in our Hispanic cohort. Finally, identifying potentially modifiable risk factors for depression in Hispanic individuals is important, particularly given increased challenges with pharmacotherapy. Latino individuals, for example, are half as likely as white individuals to start antidepressant therapy and are also more likely to discontinue such therapy within the first 30 days of treatment. This observation holds even when adjusting for increasing age.38,39
Depression is a multifactorial disorder with numerous risk factors. Despite the strong association observed in the present study between HL and depressive symptoms, the correlation coefficient between our measures of HL and depressive symptoms was very modest. This indicates that only a small fraction of the overall variability in the CESD-10 scores is explained by HL. However, any association between HL and depression is important given the high prevalence of HL (80% in those older than 80 years)9 and low treatment levels (<20% use hearing aids or cochlear implants). This high prevalence and low treatment level could result in a high proportion of late-life depression being attributable to HL.40
Limitations and Strengths
The present study has some limitations. Because of the cross-sectional design, the temporal order of the exposure and outcome cannot be determined. Thus, reverse causation, whereby depression causes HL, cannot be ruled out. This scenario could be imagined if participants with depression were exposed to known risk factors for HL, such as unprotected noise exposure. Although this is theoretically possible, noise-induced HL typically causes HL centered at 4000 Hz, which was rarely observed in the present study. It is also plausible that participants with depression may have showed worse outcomes on the hearing test because of lack of effort or attention. Although this cannot be entirely ruled out, the examiners were certified in conducting audiometric protocols, which included probing for reliability and consistency. The test-retest reliability of audiometry also approaches 99%.41
There were several other unavoidable limitations. We attempted to control for confounders between hearing and depression. However, it is also possible that residual confounding could be present. A randomized controlled trial would be needed to eliminate confounding. The oldest participants were 76 years, which does not fully capture the upper age range affected by age-related HL. However, large clinical studies often aggregate all ages over 80 years into a single group to protect anonymity.42 Thus, from an analytic standpoint, the upper age range in the present study was about as high as can be practically used. Finally, while the HCHS is a longitudinal study, prospective data collection has only recently begun and only the first wave is currently available. Thus, the current study is limited to cross-sectional analyses. Future studies should study longitudinal data.
This study also has several strengths. With more than 14 000 participants total, the HCHS is one of the largest data sets that contains objective audiometric data. This increased power facilitated finding associations that appear to be generalizable to the US population. Finally, the results remained robust in sensitivity analyses, such as including a CESD-10 cut-point score of 16 and antidepressant use, and in alternative model techniques, including log-linear regression.
Conclusions
We found an association between audiometric age-related HL and clinically significant depressive symptoms as assessed using the CESD-10 in older Hispanic adults. This association remained when adjusting for potentially confounding covariates. Future studies should examine longitudinal relationships and whether treating HL reduces the risk of late-life depression. This is particularly significant in light of the near-universal prevalence of age-related HL and low levels of treatment.
eTable 1. Logistic Regression Models for Antidepressant Use Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328
eTable 2. Logistic Regression Models for Clinically Significant Depressive Symptoms (CESD-10 Score ≥16) Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328
eTable 3. Log-Linear Regression Models for Clinically Significant Depressive Symptoms (CESD-10 Score ≥10) Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328
References
- 1.Gopinath B, Wang JJ, Schneider J, et al. . Depressive symptoms in older adults with hearing impairments: the Blue Mountains Study. J Am Geriatr Soc. 2009;57(7):1306-1308. doi: 10.1111/j.1532-5415.2009.02317.x [DOI] [PubMed] [Google Scholar]
- 2.Lee AT, Tong MC, Yuen KC, Tang PS, Vanhasselt CA. Hearing impairment and depressive symptoms in an older Chinese population. J Otolaryngol Head Neck Surg. 2010;39(5):498-503. [PubMed] [Google Scholar]
- 3.Mener DJ, Betz J, Genther DJ, Chen D, Lin FR. Hearing loss and depression in older adults. J Am Geriatr Soc. 2013;61(9):1627-1629. doi: 10.1111/jgs.12429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Contrera KJ, Betz J, Deal JA, et al. ; Health ABC Study . Association of hearing impairment and emotional vitality in older adults. J Gerontol B Psychol Sci Soc Sci. 2016;71(3):400-404. doi: 10.1093/geronb/gbw005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deal JA, Betz J, Yaffe K, et al. ; Health ABC Study Group . Hearing impairment and incident dementia and cognitive decline in older adults: the Health ABC study. J Gerontol A Biol Sci Med Sci. 2017;72(5):703-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Golub JS. Brain changes associated with age-related hearing loss. Curr Opin Otolaryngol Head Neck Surg. 2017;25(5):347-352. doi: 10.1097/MOO.0000000000000387 [DOI] [PubMed] [Google Scholar]
- 7.Lin FR, Ferrucci L, An Y, et al. . Association of hearing impairment with brain volume changes in older adults. Neuroimage. 2014;90:84-92. doi: 10.1016/j.neuroimage.2013.12.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Livingston G, Sommerlad A, Orgeta V, et al. . Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673-2734. doi: 10.1016/S0140-6736(17)31363-6 [DOI] [PubMed] [Google Scholar]
- 9.Goman AM, Lin FR. Prevalence of hearing loss by severity in the United States. Am J Public Health. 2016;106(10):1820-1822. doi: 10.2105/AJPH.2016.303299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rutherford BR, Brewster K, Golub JS, Kim AH, Roose SP. Sensation and psychiatry: linking age-related hearing loss to late-life depression and cognitive decline. Am J Psychiatry. 2018;175(3):215-224. doi: 10.1176/appi.ajp.2017.17040423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cacciatore F, Napoli C, Abete P, Marciano E, Triassi M, Rengo F. Quality of life determinants and hearing function in an elderly population: Osservatorio Geriatrico Campano Study Group. Gerontology. 1999;45(6):323-328. doi: 10.1159/000022113 [DOI] [PubMed] [Google Scholar]
- 12.Huang CQ, Dong BR, Lu ZC, Yue JR, Liu QX. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Res Rev. 2010;9(2):131-141. doi: 10.1016/j.arr.2009.05.005 [DOI] [PubMed] [Google Scholar]
- 13.Choi JS, Betz J, Deal J, et al. . A comparison of self-report and audiometric measures of hearing and their associations with functional outcomes in older adults. J Aging Health. 2016;28(5):890-910. doi: 10.1177/0898264315614006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brewster KK, Ciarleglio A, Brown PJ, et al. . Age-related hearing loss and its association with depression in later life. Am J Geriatr Psychiatry. 2018;26(7):788-796. doi: 10.1016/j.jagp.2018.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golub JS, Luchsinger JA, Manly JJ, Stern Y, Mayeux R, Schupf N. Observed hearing loss and incident dementia in a multiethnic cohort. J Am Geriatr Soc. 2017;65(8):1691-1697. doi: 10.1111/jgs.14848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swenson CJ, Baxter J, Shetterly SM, Scarbro SL, Hamman RF. Depressive symptoms in Hispanic and non-Hispanic White rural elderly: the San Luis Valley Health and Aging Study. Am J Epidemiol. 2000;152(11):1048-1055. doi: 10.1093/aje/152.11.1048 [DOI] [PubMed] [Google Scholar]
- 17.Dunlop DD, Song J, Lyons JS, Manheim LM, Chang RW. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93(11):1945-1952. doi: 10.2105/AJPH.93.11.1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Depression in the US household population, 2009-2012. NCHS data brief No. 172. https://www.cdc.gov/nchs/data/databriefs/db172.htm. Published December 2014. Accessed July 1, 2018.
- 19.Lewis-Fernández R, Das AK, Alfonso C, Weissman MM, Olfson M. Depression in US Hispanics: diagnostic and management considerations in family practice. J Am Board Fam Pract. 2005;18(4):282-296. doi: 10.3122/jabfm.18.4.282 [DOI] [PubMed] [Google Scholar]
- 20.Hispanic Community Health Study: Study of Latinos. Manual 8: audiometry exam version 1.0. 2008. https://sites.cscc.unc.edu/hchs/manuals-forms. Published January 31, 2008. Accessed October 15, 2018.
- 21.Pasha R, Golub JS, eds. Otolaryngology-Head & Neck Surgery: Clinical Reference Guide. 5th ed San Diego, CA: Plural Publishing; 2018:355. [Google Scholar]
- 22.Brown PJ, Roose SP, Fieo R, et al. . Frailty and depression in older adults: a high-risk clinical population. Am J Geriatr Psychiatry. 2014;22(11):1083-1095. doi: 10.1016/j.jagp.2013.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129(1-3):126-142. doi: 10.1016/j.jad.2010.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77-84. doi: 10.1016/S0749-3797(18)30622-6 [DOI] [PubMed] [Google Scholar]
- 25.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429-436. doi: 10.1177/1073191113481998 [DOI] [PubMed] [Google Scholar]
- 26.Oron Y, Elgart K, Marom T, Roth Y. Cardiovascular risk factors as causes for hearing impairment. Audiol Neurootol. 2014;19(4):256-260. doi: 10.1159/000363215 [DOI] [PubMed] [Google Scholar]
- 27.Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365-1372. doi: 10.1093/eurheartj/eht462 [DOI] [PubMed] [Google Scholar]
- 28.Luchsinger JA, Reitz C, Honig LS, Tang MX, Shea S, Mayeux R. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology. 2005;65(4):545-551. doi: 10.1212/01.wnl.0000172914.08967.dc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin BM, Li WQ, Curhan SG, Stankovic KM, Qureshi AA, Curhan GC. Skin pigmentation and risk of hearing loss in women. Am J Epidemiol. 2017;186(1):1-10. doi: 10.1093/aje/kwx024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. Grades of hearing impairment. http://www.who.int/pbd/deafness/hearing_impairment_grades/en/. Accessed March 29, 2017.
- 31.Thomson RS, Auduong P, Miller AT, Gurgel RK. Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope Investig Otolaryngol. 2017;2(2):69-79. doi: 10.1002/lio2.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Resnick HE, Fries BE, Verbrugge LM. Windows to their world: the effect of sensory impairments on social engagement and activity time in nursing home residents. J Gerontol B Psychol Sci Soc Sci. 1997;52(3):S135-S144. doi: 10.1093/geronb/52B.3.S135 [DOI] [PubMed] [Google Scholar]
- 33.Sung YK, Li L, Blake C, Betz J, Lin FR. Association of hearing loss and loneliness in older adults. J Aging Health. 2016;28(6):979-994. doi: 10.1177/0898264315614570 [DOI] [PubMed] [Google Scholar]
- 34.Contrera KJ, Sung YK, Betz J, Li L, Lin FR. Change in loneliness after intervention with cochlear implants or hearing aids. Laryngoscope. 2017;127(8):1885-1889. doi: 10.1002/lary.26424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weinstein BE, Sirow LW, Moser S. Relating hearing aid use to social and emotional loneliness in older adults. Am J Audiol. 2016;25(1):54-61. doi: 10.1044/2015_AJA-15-0055 [DOI] [PubMed] [Google Scholar]
- 36.Mulrow CD, Aguilar C, Endicott JE, et al. . Quality-of-life changes and hearing impairment: a randomized trial. Ann Intern Med. 1990;113(3):188-194. doi: 10.7326/0003-4819-113-3-188 [DOI] [PubMed] [Google Scholar]
- 37.Pew Research Center. Factank: how the US Hispanic population is changing. http://www.pewresearch.org/fact-tank/2017/09/18/how-the-u-s-hispanic-population-is-changing/. Published September 18, 2017. Accessed May 8, 2018.
- 38.Vargas SM, Cabassa LJ, Nicasio A, et al. . Toward a cultural adaptation of pharmacotherapy: Latino views of depression and antidepressant therapy. Transcult Psychiatry. 2015;52(2):244-273. doi: 10.1177/1363461515574159 [DOI] [PubMed] [Google Scholar]
- 39.Lanouette NM, Folsom DP, Sciolla A, Jeste DV. Psychotropic medication nonadherence among United States Latinos: a comprehensive literature review. Psychiatr Serv. 2009;60(2):157-174. doi: 10.1176/ps.2009.60.2.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chien W, Lin FR. Prevalence of hearing aid use among older adults in the United States. Arch Intern Med. 2012;172(3):292-293. doi: 10.1001/archinternmed.2011.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmuziger N, Probst R, Smurzynski J. Test-retest reliability of pure-tone thresholds from 0.5 to 16 kHz using Sennheiser HDA 200 and Etymotic Research ER-2 earphones. Ear Hear. 2004;25(2):127-132. doi: 10.1097/01.AUD.0000120361.87401.C8 [DOI] [PubMed] [Google Scholar]
- 42.Golub JS, Lin FR, Lustig LR, Lalwani AK. Prevalence of adult unilateral hearing loss and hearing aid use in the United States. Laryngoscope. 2018;128(7):1681-1686. doi: 10.1002/lary.27017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Logistic Regression Models for Antidepressant Use Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328
eTable 2. Logistic Regression Models for Clinically Significant Depressive Symptoms (CESD-10 Score ≥16) Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328
eTable 3. Log-Linear Regression Models for Clinically Significant Depressive Symptoms (CESD-10 Score ≥10) Based on Hearing Loss. Hispanic Community Health Study (HCHS), age ≥50 years, n = 5328