Abstract
With the increasing push to legalize cannabis in Western nations, there is a need to gauge the potential impact of this policy change on vulnerable populations, such as those with mental illness, including schizophrenia, mood and anxiety disorders. This is particularly important as there are strong motives in these individuals to seek short-term reward (e.g., “getting high”). Nonetheless, data to support the beneficial effects of cannabis use in psychiatric populations are limited, and potential harms in patients with psychotic and mood disorders have been increasingly documented. This article reviews the effects of cannabis in people with mental illness. Then, we provide a reconciliation of the addiction vulnerability and allostatic hypotheses to explain addiction co-morbidity in mentally ill cannabis users, as well as to further aid in developing a rational framework for assessment and treatment of problematic cannabis use in these patients.
Keywords: Cannabis, Addiction, Therapeutics, Harms, Schizophrenia, Mood Disorders, Anxiety Disorders, Posttraumatic Stress Disorder, Legalization
Introduction
In recent years, there has been a shift surrounding societal and legal perspectives on cannabis. In 2017, past-year rates of cannabis use in Canada were approximately 43% in individuals 16–24 years [125], and 18% in individuals over 25 years [19]. Moreover, there has been increasing legalization of cannabis throughout the United States, as well as nationwide legalizaiton in Canada as of October 17, 2018. The trend in legalization coincides with heightened acceptance, reduced perception of risk, and an increase in cannabis use in both adults and adolescents [23, 114, 132]. Based on the experience from commercial tobacco and the few examples of legalized recreational cannabis use (e.g. American states, such as Colorado and Washington, and in Uruguay), there is strong evidence that cannabis prevalence may increase [67, 123], which would have a disproportionate burden on those with mental illness [59]. Moreover, there will be clear societal benefits of cannabis legalization, such as shifting law enforcement away from minor crimes such as possession, which will benefit people with mental illness. Thus, from both a policy and clinical perspective, it is vital to examine the epidemiological and scientific trends of cannabis use alongside a projected growing user population.
Cannabis contains various cannabinoids that compose the Cannabis Sativa or Indica plant, such as cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC), which have been a primary clinical focus for research and clinical interests. CBD and THC both induce clinical effects through their influence on the endogenous endocannabinoid system; however, the observable impact of these pharmacological components differs significantly. The psychoactive component of cannabis involves effects produced primarily by THC’s partial agonistic effects on cannabinoid-1 receptors (CB1R’s), which generates the “high” that users feel. In contrast, CBD has been shown in early studies to exhibit potential therapeutic effects (e.g. antipsychotic, anxiolytic, anti-craving pro-cognitive and neuroprotective effects), as it appears to have differential, and somewhat opposing, pharmacological effects compared to THC [29]. Recreational cannabis, both unregulated and regulated, is prepared with various combinations of THC and CBD. Overtime, however, the most common cannabis preparations have come to consist of high THC and lower CBD potency [48]. Due to the complex pharmacological makeup of cannabis products, as well as the diffuse distribution of cannabinoid receptors throughout the brain that influence a variety of neurotransmitters, the clinical effects range from euphoria and relaxation to panic anxiety and psychosis.
Problematic cannabis use (e.g. cannabis use disorder (CUD)) is much higher in individuals with mental illness, including schizophrenia, mood and anxiety disorders, personality disorders and post-traumatic stress disorder, compared to the general population [14, 17, 22, 68, 92]. Psychiatric symptoms have been shown to predict not only problematic cannabis use, but also the perception of cannabis as harmless [11, 133]. Additionally, as cannabis use becomes more clinically severe, a stronger correlation has been described between a diagnosis of CUD and concurrent psychiatric disorder [68]. Despite this high prevalence, well-controlled studies have suggested more harms than therapeutic benefits from recreational cannabis use in these populations; however, further research is needed.
This review will examine the paradox between the high prevalence of cannabis use in mentally ill populations and evidence for the therapeutic potential of cannabis. In order to understand this paradox, the addiction vulnerability [21] and self-medication [85] hypotheses will be used as pillars to guide the analysis in determining whether cannabis (and its constituents) has true therapeutic potential versus whether its effects are more harmful.
A Review of the Effects of Cannabis in Mental Illness
There are several lines of evidence suggesting either therapeutic potential or harmful effects associated with cannabis use in psychiatric populations. In this section, we provide an overview of the current scientific literature on the effects of cannabis across schizophrenia, mood disorders, anxiety disorders and post-traumatic stress disorder (PTSD). A recent report by the National Academies of Sciences [109] assessed the potential therapeutic effects and harms of cannabis in detail, concluding that there are many gaps of which remain across the scientific literature. In order to understand what the evidence currently suggests about both the acute and long-term effects of cannabis in mental illness, high-quality studies (see Table 1) will be discussed. Search strategies for this review included PubMED and PSYCHinfo to select appropriate studies for the analysis.
Table 1.
Evidence Ratings for Therapeutic Benefits versus Harms of Cannabis
| Diagnosis | Therapeutic Benefits | Refs. | Harms | Refs. | Future Research |
|---|---|---|---|---|---|
| SZ | There is minimal and equivocal evidence supporting a therapeutic role for cannabis, specifically CBD, in SZ. | [9, 76, 93, 101] | Cannabis use has been shown to have a strong correlation (dose- dependent) to poorer outcomes in and increased risk of psychosis. | [2, 33, 54, 100, 107, 113,116, 117,128, 145] | Further randomized, controlled trials are needed to determine CBD effects across heterogeneous populations of SZ. Additionally, further randomized, controlled studies looking at combined effects of CBD and THC are needed. |
| MDD | There is no clear evidence for a positive influence of cannabis in depression (only studies that show lack of association). | [34, 50] [111] | Evidence suggests more of a harmful influence of cannabis on the course of depression, specifically associated with adolescent onset of use. | [4, 5, 75, 106, 120, 129] | Longitudinal, prospective and controlled trials to investigate what preparation(s) of cannabis as well as what frequency and onset of use is associated with harms. |
| BD | There is no evidence of any therapeutic effect with cannabis use, besides acute relief shortly after use. | [121] [73, 126] | Cannabis use has been associated with harms, including increased risk of and outcomes in BD; however, there are equal findings with statistically insignificant associations. | [27, 86, 111, 144, 155] | Longitudinal, prospective and controlled trials to investigate what preparation(s) of cannabis as well as what frequency and onset of use is associated with harms. |
| PTSD | There is minimal evidence of any therapeutic effect with cannabis use. Benefits for have been reported mainly for sleep-related dysfunctions. | [18, 56, 78, 124] | There is minimal evidence of reported harms with cannabis use. Long-term effects of cannabis on PTSD are still unclear. | [45, 98, 141, 153] | Randomized, controlled trials with larger sample sizes are needed to understand potential therapeutic effects. Longitudinal, prospective trials are needed to understand potential harms. |
| GAD | There is no clear evidence for the therapeutic benefit of cannabis across anxiety disorders, despite self-reported claims. | [7, 19] | There is equivocal evidence suggesting either positive or lack of statistically significant associations between cannabis use and anxiety disorder or anxiety symptoms. | [27, 34, 37, 50, 66, 69, 130, 144] | Randomized, controlled trials and longitudinal, prospective studies are needed to associate specific preparations of cannabis with anxiety outcomes and risk for anxiety development. |
| Evidence Ratings | |||||
|
Rating 1: Minimal Evidence Case Reports & Retrospective Studies |
Rating 2: Equivocal Evidence Case-Controls & Cross-Sectional Studies |
Rating 3: Strong Evidence Randomized Controlled Trials |
|||
SZ, Schizophrenia; MDD, Major Depressive Disorder; BD, Bipolar Disorder, PTSD: Posttraumatic Stress Disorder; GAD, Generalized Anxiety Disorder.
Schizophrenia
Cannabis use has been described as one of many environmental influences associated with an individual’s increased vulnerability towards the development of psychotic illness [13, 35, 38, 61], with approximately one in every four individuals in this population presenting with a concurrent CUD diagnosis [89]. Several studies have demonstrated negative effects of cannabis use in patients with schizophrenia. Specifically, THC in cannabis has been associated with an increased risk of psychosis in a dose-dependent manner: regular cannabis users and heavy cannabis users are 2- and 4-times more likely to develop psychosis, respectively [39, 100]. Furthermore, increased risk for earlier psychotic symptom presentation has been observed in conjunction with cannabis use in the general population [70, 81]. Results from one of the largest longitudinal studies involving over 50,000 male participants indicates that those who smoked cannabis by the age of 18 had twice the risk for receiving a diagnosis of schizophrenia, while those who used chronically were at six times the risk compared to non-users [2]. Notably, the administration of intravenous THC in healthy individuals has been shown to directly induce psychotic symptoms, both self-reported and assessed by the Positive and Negatve Symptom Scale (PANSS) [32, 107]. Across multiple studies, cannabis use has been correlated with earlier onset of psychosis, increased symptom severity, higher rates of relapse and longer hospitalization time, as well as overall poorer illness and quality-of-life outcomes [33, 40, 54, 58, 79, 90, 99, 113, 145]. In one study, continued cannabis use following psychosis onset, when compared to discontinued use, was associated with higher rates of relapse, longer hospital admissions, enhanced positive and negative symptoms, as well as a variety of negative impacts on daily functioning [128]. Importantly, cannabis abstinence has been shown to ameliorate cognitive impairments related to cannabis use, such as verbal memory and learning, as well as specific symptomology (e.g. depression), suggesting that cannabis may contribute to symptom exacerbation in schizophrenia [116–118]. Interestingly, however, a recent trial by McGuire and colleagues suggests the potential of administering 1000 mg of cannabidiol (CBD) daily for 6 weeks alongside current antipsychotics for reducing positive symptoms as rated by the PANSS, as well as for improving self-reported and clinician-reported functional outcomes in schizophrenia compared to placebo [102]. Moreover, a study by Leweke and colleagues compared the efficacy of CBD to a potent antipsychotic, amisulpride, in acute schizophrenia, describing similar efficacy in clinical symptomatic improvement as well as superior side effects, such as increased anandamide serum levels that were significantly associated with clinical improvements [93]. In a trial similar to McGuire et al.’s, conducted by Boggs and colleagues, 600 mg of CBD was administered daily for 6 weeks and, despite being well tolerated, was not associated with any improvement with symptoms using the PANSS, or with cognition compared to placebo in stable, treated patients with schizophrenia [9]. A systematic review of the therapeutic potential of CBD and higher CBD cannabis preparations for psychosis and schizophrenia describes a promising future with effective and tolerable results thus far [76]. Moreover, published on the ClinicalTrials.gov database, there are currently two active, but not yet recruiting, clinical trials that will assess CBD in acute schizophrenia (NCT02088060), as well as in early psychosis (NCT02504151). There are also two completed trials that have assessed CBD in acute psychosis (NCT00628290) and in schizophrenia or schizophreniform disorder (NCT00309413), but have no published results. Randomized mulit-site clinical trials are needed to substantiate the external validity of these trials.
Major Depressive Disorder (MDD) and Bipolar Disorder (BD)
In MDD, much of the evidence suggests harmful consequences of cannabis use. In a 40-year study that analyzed a cohort of over 400 individuals across several time points, cannabis use was correlated with an increased risk of receiving a MDD diagnosis, and earlier onset of cannabis use was correlated with a shorter time to MDD presentation [129]. Other studies have shown similar results, demonstrating a positive correlation between cannabis use and depression, of which chronic use further strengthens this association [75, 120]. One study found the association between MDD and cannabis only in those with CUD, rather than those who occasionally use cannabis, while other studies describe weekly cannabis use being sufficient [4, 75]. This warrants a deeper investigation towards the extent of cannabis use (e.g. frequency and CBD/THC potency) that is necessary to better understand this association. Not only has cannabis use been shown to potentially predict risk of developing MDD, but it has also been shown to promote depressive symptom progression [5, 106]. Despite a substantial collection for the harmful implications of cannabis on depressive outcomes, there are other studies that have found no correlation between cannabis use and later MDD diagnosis or symptom severity after controlling for multiple confounding factors, including other illicit drug use, education and childhood upbringing [34, 51, 111]. Nonetheless, there have been no randomized, clinical trials for the use of cannabinoids in depression. There are, however, studies that have analyzed depression symptoms as secondary outcome measurements in participants with other disorders, such as chronic pain, but no significant therapeutic benefit has been found in association with the administered cannabinoids, including nabiximols and dronabinol [109]. Thus far, the literature suggests more evidence for harms, rather than therapeutic effects, of cannabis in MDD (Table 1); research gaps need to be addressed in future research with prospective, controlled study designs.
Similarly, the majority of evidence suggests harmful effects of cannabis use in bipolar disorder (BD), another common mood disorder associated with CUD [97]. Using a nationally representative sample of over 40,000 individuals, cannabis use has been associated with a greater risk of BD onset [27]. This association has been found by others, with higher frequency cannabis use further potentiating the risk for developing BD and worsening BD symptomology, including sucide risk [111, 144]. One study highlights a positive association between BD and cannabis use, but with interactive effects of cannabis use and BD measures on gender and medication type [86], while other studies describe cannabis use as predictive of longer affective episode duration, more frequent rapid cycling between mood states, as well as lower remission rates and lower clinical and functional recovery [137, 155]. In contrast, another study suggests an improvement in BD symptoms 4 hours following cannabis use [126]; however, this only reflects an acute profile of cannabis use in BD. There are additional studies that suggest no statistically significant relationship between cannabis and BD outcomes [73, 121]. Moreover, there have been no studies to investigate any therapeutic relationship between cannabinoids and BD. Further research is necessary to better understand the nature of the relationship between cannabis and BD, but thus far the current literature indicates that there are more harmful consequences compared to benefits associated with long-term cannabis use in BD symptomatology and disease progression.
Anxiety Disorders
About 50% of respondents in a 2017 Canadian cannabis survey claimed that cannabis had a positive effect on anxiety [19]. Despite this claim, much of the research to date suggests otherwise. For example, there is significant evidence for an association between cannabis use, agoraphobia and social anxiety disorder (SAD) [27, 140]; in a nationally representative study, a clear, statistically significant association was observed between daily cannabis use and SAD [50]. However, findings on this co-morbidity across disorders of anxiety remain mixed. For instance, regarding generalized anxiety disorder (GAD), research ranges from a two-fold increased risk of anxiety symptoms with cannabis use to no significant association between the two factors [37, 144]. One study supports the relationship between cannabis use and GAD, but not between cannabis use and SAD, further complicating the results [66], while others describe persistent reports of heightened anxiety symptoms in cannabis users compared to non-users [42]. Some studies have investigated the effects of cannabis use in early childhood and adolescent stages, demonstrating an increased risk of developing anxiety symptoms and anxiety disorder, which was strengthened with earlier onset of cannabis use [25, 36, 69]. Again, there are also studies that describe a lack of any significant correlation after controlling for significant confounds, such as cigarette use and childhood factors [34, 57, 130, 156]. A systematic review by Whiting et al. on the medical use of cannabinoids describes only one clinical trial conducted by Bergamaschi and colleagues in which a single 600 mg dose of CBD in individuals with SAD was associated with improved scores on a visual analogue scale after a simulated public speaking test in comparison to placebo; however, the authors note how this study holds high potential bias [7, 152]. Any other study assessing benefits of cannabis on anxiety are, however, only secondary analyses within pain populations [55, 108, 135, 152]. Nonetheless, the current literature does not suggest any robust therapeutic benefits of cannabis for anxiety, and therefore is inconsistent with claims of self-medication. Further research should focus on prospective designs that allow researchers to understand the directionality of the association between cannabis and anxiety.
Post-Traumatic Stress Disorder (PTSD)
Cannabis use has become increasingly common amongst patients with PTSD [83]. Although there is mixed data regarding the use of cannabis as a treatment for PTSD, current research has shown a strong positive association between PTSD symptom severity and daily cannabis use [43]. There is evidence that supports the notion that individuals with PTSD use cannabis as a means for coping with symptoms, primarily involving insomnia in contrast to anxiety-related symptoms [10, 56]. This finding, however, has been challenged as Metrik and colleagues found that, while individuals with PTSD report using cannabis to cope with sleep disturbances, patients later report significantly poorer sleep quality and physical health [105]. In terms of PTSD symptom severity, most data supports the association of cannabis users having a higher likelihood of presenting with PTSD symptoms, experiencing heightened negative affect, and showing improvements in symptoms following cannabis abstinence [91, 98, 141, 153]. Moreover, when an individual meets PTSD criteria and concurrently uses cannabis, they typically experience increased withdrawal and craving [8]. Other studies either show mixed support for both the potential harms [26, 62, 104, 148], the therapeutic benefits, of which mostly involves improvements in sleep-related outcomes [18, 45, 64, 124], or show lack of association between PTSD outcomes and cannabis use [80]. There is mixed data for the use of cannabis as a therapeutic treatment for PTSD. A randomized, double-blind, cross-over study describes therapeutic effects of nabilone (target dose of 3 mg daily for 7 weeks), a synthetic cannabinoid that mimics the effects of THC, for nightmares, global functioning and overall well-being in comparison to placebo [78]. Another study showed similar improvements following nabilone administration; however, this was a retrospective design [18]. Another study examined the administration of THC in patients with PTSD, describing favourable results in a sample of 10 participants [124]. To note, nearly half of the studies that assess cannabis use in PTSD, as well as its potential therapeutic effects, were conducted in U.S. military veterans, who exhibit high comorbidities of cannabis use and CUD, commonly reporting the use of cannabis to cope with one’s traumatic experiences [8, 45, 62, 78, 80, 98, 104, 105, 153]. This population may be the most benefited by research in this area based on the high prevalence of cannabis use, which may have positive or negative effects on recovery. Despite no association between cannabis use and PTSD development, there are reported harmful effects from cannabis use on psychiatric outcomes in PTSD. There are also, however, non-significant associations that have been concluded between cannabis use and PTSD symptomatology. Additionally, reported benefits are minimal and involve mixed findings across studies. Accordingly, further research is required using prospective, controlled clinical designs to understand the relationship between cannabis and PTSD.
Self-Report vs. Scientific Evidence
The majority of the empirical literature supports the argument that cannabis produces more harm than benefits insofar as psychiatric illness severity and progression (Table 1). Despite the current gaps that exist in research surrounding this topic, there seems to be a discrepancy that remains between evidence for cannabis’ therapeutic potential and self-reported motivation underlying cannabis use. For example, in a cross-sectional study across 1,429 participants from 18 different countries, individuals reported using cannabis “medically” rather than “recreationally”, and users described pain (61.2%), anxiety (58.1%) and depression (50.3%) as top reasons for using cannabis [133]. Other studies have found similar results, with sleep, pain and anxiety among the most common reasons for use [11, 50, 122, 151]. Individuals are also directly reporting the use of cannabis to self-medicate specific mental illnesses, such as anxiety and PTSD [26, 50, 142]. Additionally, some clinicians are directly prescribing cannabis for anxiety and depression [110, 122]. However, it is clear that there is limited evidence to make any strong conclusions about therapeutic effects of cannabis [109]. Due to the anticipated increase in cannabis availability with legalization, and subsequent increased prevalence, it is important to resolve the paradox surrounding why cannabis users report self-medication for psychiatric symptoms when the science, to date, does not support this account.
Methodological Shortcomings in the Current Literature
In order to understand the discrepancy between self-reported reasons for cannabis use and the scientific evidence that currently exists, there are many areas of research that must be addressed, see Table 1. For schizophrenia, while initial results have been promising, more rigorous, controlled trials, as well as multi-site clinical trials, are necessary to confirm CBD’s therapeutic potential. The evidence, however, is strong surrounding the harms of recreational cannabis use in schizophrenia. Although, additional longitudinal, prospective studies are necessary in understanding what exact preparations of cannabis, frequency of cannabis use and age of onset of use promote this association. For MDD, there are only secondary analyses of cannabinoids benefiting depressive symptoms. Future research addressing the direct relationship between specific cannabinoids and MDD using appropriate measures are necessary. Moreover, longitudinal, prospective designs as well as controlled, clinical trials must assess the relationship between cannabis use and potential harms, such as risk of MDD and worsening of depression symptoms and outcomes. There is only minimal evidence in BD suggesting the harms of cannabis use, therefore, future controlled, prospective designs are necessary in furthering these primary findings. Considering anxiety disorders, additional longitudinal, prospective studies as well as controlled, clinical trials are necessary for determining any therapeutic potential of cannabinoids. Moreover, similarly as described in MDD and BD, future research is required to determine the specific harms that cannabis can induce in anxiety, as findings are currently mixed. Finally in PTSD, current trials reporting benefits of cannabis involve specific populations, such as exclusively male participants or military veterans, and very small sample sizes. Future controlled studies addressing these limitations are warranted. To better understand potential cannabis harms, longitudinal, prospective studies must be conducted to determine the exact association between cannabis use overtime in PTSD of which also addresses frequency, preparation and onset of cannabis use.
Physical Harms of Cannabis
Apart from the current evidence that suggests both short- and long-term risks in psychiatric illness, cannabis involves other adverse effects that must not be overlooked. Cognition can be impaired with both acute use of cannabis as well as overtime in chronic users. This includes impaired short-term memory, motor coordination and control, executive functioning, as well as altered judgement [12, 28, 103, 136]. These deficits can put individuals at higher risk for injury and disease, for example, from motor vehicle accidents due to impaired motor control or from sexually transmitted disease due to impaired judgement in sexual encounters [149]. Additionally, short-term cannabis use, if consumed at high doses and with high THC potency, can induce paranoia and even psychosis, as described in the ‘schizophrenia’ section [31, 149]. With respect to long-term effects, a major risk involved with cannabis use is addiction; roughly 8.9% of individuals who use cannabis develop an addiction following lifetime exposure [95]. Moreover, almost half of chronic users experience robust withdrawal symptoms after cessation, which can include characteristics that range from sleep problems and nightmares to dysphoria and nausea [16]. Of note, cannabis use has also been associated with progression to other illicit drug use, which becomes strengthened with increased frequency and earlier onset of use [52], therefore placing individuals at risk for other substance use disorders and drug-related harms. A second long-term adverse effect that has been substantiated is risk of smoking cannabis is risk of developing symptoms of chronic bronchitis due to airway and lung inflammation [149]. Other adverse effects that are more strongly associated with cannabis use onset specifically in adolescence involves poorer education outcomes, cognitive impairment and hindrance to one’s overall success [31, 96, 149]. Finally, other forms of cannabis consumption can be associated with additional harms towards the user. Apart from smoking cannabis via joints, pipes, blunts or bongs, other methods for administering cannabinoids include butane hash oil (“dabs”) and oral consumption (“edibles”), which pose risks that are associated with stronger and slower delivery, respectively, as well as with the inaccuracy in product labelling [6, 94, 147]. Alternatively, one form of consumption that may pose less risk for users in comparison to smoking involves the method of vaporizing cannabis, which is associated with fewer respiratory problems [44, 46, 60]. Depending on the route of administration, physical harms may differ slightly; however, these outcomes must be acknowledged regardless of the focus (i.e. therpauetic benefits or potential harms) in discussions of cannabis and mental illness.
Conceptualizing Problematic Cannabis Use in Mental Illness: Addiction Vulnerability versus Self-Medication Hypothesis
To understand why an individual describes self-medicating with cannabis to cope with clinical symptoms of mental illness, a framework highlighting the developmental process of CUD needs explanation. The sensations experienced during an acute intoxication, or “high”, from cannabis facilitate positive reinforcement through the temporary escape from psychiatric symptomolgy, which is followed by craving and further use. This is consistent with theories of addiction vulnerability, which predisposes an individual to not only using cannabis, but developing CUD. Repeated drug use can lead to neurobiological transitioning into an allostatic state [87], which produces an affective deficit over time that coincides with persistent cannabis use.
Cannabis Use: Reinforcement and Addiction Vulnerability
What initially primes an addictive disorder is not necessarily what maintains the disorder. Addiction is, in principle, behavioural, with positive reinforcement from neurochemical effects (e.g. a dopaminergic surge following reward) that are linked to drug-contingent memories driving pervasive drug craving and dysphoria [154]. Most individuals report using cannabis to get “stoned” or “high”, which involves sensations including general euphoria, heightened awareness, relaxation and pleasure [30, 63]. Biologically, cannabis stimulates CB1Rs, which alters dopamine function, of which is associated with one’s positive hedonic experience [112]. Because of these intoxication characteristics, the user’s psychological state becomes associated with the drug and context of use, priming a cycle of positive reinforcement and incentive salience [88]. These neurobiological and psychological changes mark the initial process in drug use and addiction, with mesocorticolimbic dopamine transmission playing a key role alongside other neurotransmitter activations in regions including the ventral tegmental area, nucleus accumbens and frontal cortex [88]. The reported “high” induced by cannabis may explain what primes this addiction.
Several factors may predispose individuals to developing CUD. Additionally, these same individuals may have an equal predisposition to developing a comorbid mental illness [119, 150]. The addiction vulnerability hypothesis outlines pre-existing vulnerabilities that one may have to developing an addiction. There are factors, including impulsivity, genetic predisposition, epigenetic states, and overlapping neurobiology that bias an individual to not only mental illness, but also to developing SUDs, including CUD [21, 115, 139, 146]. For example, genetic studies have confirmed vulnerability models in which there are shared genetic predispositions to CUD and, for example, major depression [20, 74, 134]. It is known that CUD and mental illness are highly prevalent together. For example, one study has described how those who are addicted to cannabis, compared to non-addicted users, report mental health problems, including anxiety and depression, further emphasizing the potential comorbid vulnerability model [143]. Not only are there shared vulnerabilities, but the presence of a mental illness itself is a vulnerability factor for addiction, despite the heterogeneity across comorbidities [24, 82, 131, 138]. For example, depression and anxiety have been described as a strong predictors of whether regular cannabis use will transition to a CUD [53]. Nevertheless, individuals who have a mental illness are at a heightened risk for developing CUD.
The Perception of Self-Medication
The self-medication hypothesis is based on the notion that individuals use substances due to dysfunctional self-regulatory abilities and affect states [84, 85]. Individuals medicate the distress and pain associated with difficulties surrounding general self-care, emotion regulation, self-esteem and interpersonal difficulties, all of which are classified under ‘self-regulation’ [84]. When an individual becomes distressed, substances are more likely to be used to attenuate these feelings due to lack of coping skills, which are necessary in addressing emotional dysregulation [85]. Interestingly, a review that analyzes neuroimaging studies in addicted individuals describes decreases in grey matter within regions associated with self-regulation and introspection [49]. Moreover, individuals who use cannabis are likely to report dysfunctional coping as a primary motivation for substance use [11]. For example, individuals with SAD have been shown as more likely to crave cannabis in social interactions as their (dysfunctional) coping mechanism [15].
As previously noted, many individuals tend to describe using cannabis to self-medicate the symptoms of mental illness. In using the term “self-medication”, one assumes that the substance is helping to treat the specific illness; however, cannabis only provides momentary relief. There is an acute reduction that one may perceive in their symptom severity that is masked by the “high” that they feel. This subjective feeling may temporarily hide the reality of their illness presentation, substituting distressing symptoms of their illness with acutely pleasurable ones. For example, acute use of cannabis in people with BD is associated with symptom alleviation, including symptoms of depression, mania, anger and tension [126]. The relief, however, is not a true therapeutic effect, but rather a temporary and immediate relief that would not be found through their absent self-regulatory processes. Additionally, this perception may be more of an initial reason for use, illustrating the addiction vulnerability in this population (Figure 1). In fact, roughly half of individuals who initially use cannabis for anxiety, depression, and insomnia do not report these same reasons for continued use cannabis [11].
Figure 1. Addiction Vulnerability and Allostasis Models Conceptualized for Cannabis Users with Mental Illness.
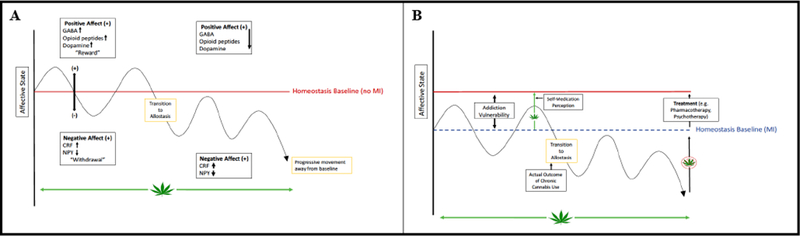
Individuals without mental illness (MI) (A) who use cannabis transition to an allostatic state, leading to neurobiological changes that induce a continuous reduction in positive affect that is associated with further use in attempts to regain original homeostatic levels. Individuals with MI (B) already have a lowered set point for positive and negative hedonic homeostasis, promoting addiction vulnerability, as substances are used in attempts to normalize an already altered (reduced) set point. Addiction in psychiatric patients is associated with a similar transition to an allostatic state but with an even lower homeostatic baseline (see dashed line in Panel B), with cannabis use continuing in attempts to regain the original positive affect experienced prior to substance use.
Nonetheless, it is understandable why the self-medication hypothesis has stood the test of time. Emotion dysregulation, common in mental illnesses, and lack of protective coping mechanisms, illustrated by Khantzian [84] who initially described this hypothesis, make this population vulnerable, which primarily drives one to using a substance. Moreover, cannabis users have been described to have prominent affective dysregulation, such as higher levels of anhedonia, placing this population at even further risk [41]. The perception of cannabis’ ability for self-medication contributes to this notion, as these individuals rely on a substance to replace social and neuropsychological mediators. For example, in a study of veterans using cannabis, as symptoms of PTSD increased, heightened use of cannabis and expectations for cannabis to aid symptom severity followed [45]. The belief that cannabis can be used to medicate symptoms of mental illness combined with acute withdrawal relief, including the relief of symptoms not limited to anhedonia-like reports, anxiety and headaches, together primes reinforcement for further drug use [1, 84, 87]. This perception may place individuals with mental illness at higher addiction risk.
Chasing the “high”
After chronic and frequent cannabis use, the trajectory for developing CUD progresses. Addiction encompasses the adverse consequences of repeated drug misuse, which leads to neurobiological changes that further influence the neural circuitry involved in emotion, sensation, and higher order cognition [87]. Allostasis results from system neuroadaptations that change one’s homeostatic set-point in order to compensate for substance-induced changes in the brain. Neurotransmission and hormonal signalling adapt to accommodate the continual influence on reward circuitry by altering one’s set-point to maintain hedonic homeostasis. Consequentially, the cannabis user’s affective state, which is a combination of positive mood state processes and negative, anti-reward processes, becomes altered [87]. Dysfunctional reward neurotransmission (e.g. dopaminergic reward circuitry) results due to the consistent activations by, in this case, cannabis, as well as the anti-reward systems being developed and heightened [154]. This is due to the surge in reward activation followed by substance use, which then becomes downregulated to maintain allostasis, leading to chronic hypofunctioning of positive reinforcement circuitry and increased stress activation, such as hypothalamic-pituitary adrenal axis and corticotrophin releasing factor (CRF) stimulation [87]. Cannabis may blunt dopamine production and signalling with chronic use [127], which further supports the allostasis model. Hill describes this phenomenon in the context of anxiety as the “rebound effect” such that individuals will experience anxiety and proceed to use cannabis to temporarily alleviate these symptoms. Overtime, and once the acute effects of cannabis dissipate, however, one’s affective state becomes further exacerbated due to the long-term effects of the substance [71]. The question remains as to why the perception remains that cannabis has therapeutic effects towards mental illness when the relief may be only acute during the time of intoxication and, ultimately, lead to a reduction in affect through allostasis production (Figure 1).
When an individual experiences withdrawal, there are two outcomes: a negative affective state common among many substances, described as the “rebound effect” or allostatic phenomenon, as well as drug-specific withdrawal symptoms. An allostasis deficit occurs due to physiological changes, including decreased dopamine, endogenous opioid peptides, serotonin and increased dynorphin, leading to symptoms, such as depression, dysphoria and pain, as well as decreased gamma-aminobutyric acid (GABA), neuropeptide-Y and increased corticotrophin releasing factor (CRF) leading to symptoms, such as anxiety, stress and panic attacks [87]. Koob has conceptualized addiction into a theory that involves a binge and intoxication stage, a withdrawal and negative affect stage, and a preoccupation and anticipation stage, all of which are fueled by negative reinforcement [154]. Negative reinforcement involves the removal of an aversive stimulus by cannabis use, therefore maintaining the behaviour. This can explain how cannabis may be used as a form of “self-medication” in maintaining addiction, in that individuals go through withdrawal in-between use and, to alleviate these symptoms, use cannabis. Negative reinforcement, or the reversal of withdrawal symptoms due to the deficit produced in the allostatic state, maintains the perception of self-medication. In reality, however, the user is only medicating one’s abnormally low affective baseline due to the neurobiological changes mediating allostasis that is observed in addiction. Moreover, based on the dual process model of addiction [146], an individual’s automatic processes, also described as one’s impulsive behavior, overshadows more executive, controlling cognition, which also maintains addictive behavior.
Many of cannabis’ withdrawal symptoms mimic symptoms of psychiatric disorders, further creating the façade of treating one’s disorder. Symptoms upon abstaining from cannabis include anxiety, irritability, craving, dysphoria and insomnia, of which coincide with many symptoms of mood and anxiety disorders, as well as schizophrenia and PTSD [3, 68].
Addiction Vulnerability Hypothesis Reconceived: Reconciliation with the Allostasis Model
Addiction vulnerability is described as the genetic, neurobiological and environmental factors that predispose an individual to develop substance use disorder. In individuals with comorbid mental illness and CUD, there is some evidence for a shared vulnerability. Mental illness, however, may also be a vulnerability factor itself, as it primes an individual to seek self-medication (Figure 1). Specifically, when an individual lacks protective self-regulatory abilities to deal with emotional dysfunction, cannabis use may be used as a substitute in order to cope with one’s mental illness. Initial relief of one’s affective state may positively reinforce the behaviour, eventually leading to an allostatic state in which a neurobiological affect deficit is produced. This deficit leads to reward circuitry hypofunction and the aggravation of affective symptoms observed during withdrawal. Continued cannabis use influences negative reinforcement by temporarily relieving the distress caused by withdrawal symptoms and the neurobiological deficit. Moreover, the cannabis user is unaware of these processes, perceiving cannabis as a mode to attenuate symptoms. In other words, mental illness makes an individual vulnerable to potential reliance on cannabis as a coping strategy to manage clinical symptoms. This further places an individual at risk to CUD, which leads to an allostatic state that progresses to addiction. Throughout the transition from cannabis use to CUD, the perception that cannabis improves mental illness highlights this paradox.
Societal Implications of Cannabis Legalization
It is clear that there are many impediments to properly informing policy and public education of which are necessary to address in the current landscape of increasing cannabis legalization and prevalence. Two of the main, overarching barriers include 1) the perception that cannabis is a single drug with “only good” or “only bad” outcomes and 2) the notion that cannabis is a form of alternative medicine. This manuscript does not aim to discredit or discount the therapeutic potential that cannabis may have; however, most studies that describe these benefits are analyzing distinct, isolated compounds, such as pure CBD, for example, as well as specific dosing schedules and routes of administration. The current evidence suggests more harms associated with cannabis use in mental illness than benefits; however, these studies are mostly observational and reflect recreational cannabis, which contains increasingly higher THC potency and lower CBD concentrations [47]. With this said, cannabis is a drug of many constituents with differential effects, which can be combined and prepared in various forms, placing it in what Hill describes as a ‘gray zone’ that is not entirely good or bad [72]. There must, therefore, be a shift in the current public conceptualization of cannabis as being “only good” and a form of “alternative medicine” or “purely harmful”. High THC-potent cannabis may be mostly harmful, specifically in mental illness; however, pure CBD may promote therapeutic relief. Recognizing that cannabis exists in this ‘gray zone’ will ultimately aid in accurately filling the scientific gaps that remain, as well as in properly addressing policy implementation and social education.
Conclusions and Future Directions
Individuals may be predisposed to developing an addictive disorder due to various biological and sociological factors. This may support vulnerability towards initial use as well as both the positive and negative reinforcement that follows. Having a comorbid psychiatric disorder further complicates this, as the initial positive reinforcement received and the later withdrawal alleviation may mask itself as ‘self-medication’. The reality, however, is that the perception of self-medicating one’s mental illness with cannabis is common in mentally ill patients. The evidence thus far supports more harmful effects of recreational cannabis use on mental illness, rather than therapeutic. The high prevalence of cannabis users self-reported therapeutic effects, however, creates a paradox that has negatively influenced societal and political perspectives, as well as contributed to polarized views on cannabis. Collection and analysis of prospective data is vital in order to disseminate accurate information to the public so that individuals can make informed choices, and evidence-based policies can be implemented.
Footnotes
Disclosures
Ms. Lowe, Ms. Coles and Ms. Sasiadek have no conflicts of interest in relation to this manuscript. Dr. George has been a consultant to NIH and the Canadian Centre for Substance Abuse, and has grant support from the Canadian Institute of Health Research (MOP-115145) and the National Insisute on Drug Abuse (R21-DA-043949).
References
- 1.Agrawal A, Pergadia ML, Lynskey MT (2008) Is there evidence for symptoms of cannabis withdrawal in the national epidemiologic survey of alcohol and related conditions? The American journal on addictions 17:199–208 [DOI] [PubMed] [Google Scholar]
- 2.Andréasson S, Engström A, Allebeck P, Rydberg U (1987) Cannabis and schizophrenia a longitudinal study of swedish conscripts. The Lancet 330:1483–1486 [DOI] [PubMed] [Google Scholar]
- 3.APA (2013) Diagnostic and statistical manual of mental disorders Washington, DC [Google Scholar]
- 4.Baggio S, N’goran AA, Deline S, Studer J, Dupuis M, Henchoz Y, Mohler‐Kuo M, Daeppen JB, Gmel G (2014) Patterns of cannabis use and prospective associations with health issues among young males. Addiction 109:937–945 [DOI] [PubMed] [Google Scholar]
- 5.Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD (2017) Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. Journal of affective disorders 213:168–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrus DG, Capogrossi KL, Cates SC, Gourdet CK, Peiper NC, Novak SP, Lefever TW, Wiley JL (2016) Tasty thc: Promises and challenges of cannabis edibles. Methods report (RTI Press) 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bergamaschi MM, Queiroz RHC, Chagas MHN, De Oliveira DCG, De Martinis BS, Kapczinski F, Quevedo J, Roesler R, Schröder N, Nardi AE (2011) Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology 36:1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boden MT, Babson KA, Vujanovic AA, Short NA, Bonn‐Miller MO (2013) Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. The American Journal on Addictions 22:277–284 [DOI] [PubMed] [Google Scholar]
- 9.Boggs DL, Surti T, Gupta A, Gupta S, Niciu M, Pittman B, Martin AMS, Thurnauer H, Davies A, D’Souza DC (2018) The effects of cannabidiol (cbd) on cognition and symptoms in outpatients with chronic schizophrenia a randomized placebo controlled trial. Psychopharmacology:1–10 [DOI] [PubMed] [Google Scholar]
- 10.Bonn-Miller MO, Babson KA, Vandrey R (2014) Using cannabis to help you sleep: Heightened frequency of medical cannabis use among those with ptsd. Drug and alcohol dependence 136:162–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonn-Miller MO, Boden MT, Bucossi MM, Babson KA (2014) Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. The American journal of drug and alcohol abuse 40:23–30 [DOI] [PubMed] [Google Scholar]
- 12.Bossong MG, Jansma JM, van Hell HH, Jager G, Oudman E, Saliasi E, Kahn RS, Ramsey NF (2012) Effects of δ9-tetrahydrocannabinol on human working memory function. Biological psychiatry 71:693–699 [DOI] [PubMed] [Google Scholar]
- 13.Brown AS, Lau FS (2016) A review of the epidemiology of schizophrenia. Modeling the psychopathological dimensions of schizophrenia: From molecules to behavior:17–30 [Google Scholar]
- 14.Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM (2008) Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of psychiatric research 42:230–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buckner JD, Zvolensky MJ, Ecker AH, Jeffries ER (2016) Cannabis craving in response to laboratory-induced social stress among racially diverse cannabis users: The impact of social anxiety disorder. Journal of Psychopharmacology 30:363–369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Budney AJ, Hughes JR, Moore BA, Vandrey R (2004) Review of the validity and significance of cannabis withdrawal syndrome. American journal of Psychiatry 161:1967–1977 [DOI] [PubMed] [Google Scholar]
- 17.Bujarski SJ, Galang JN, Short NA, Trafton JA, Gifford EV, Kimerling R, Vujanovic AA, McKee LG, Bonn-Miller MO (2016) Cannabis use disorder treatment barriers and facilitators among veterans with ptsd. Psychology of Addictive Behaviors 30:73. [DOI] [PubMed] [Google Scholar]
- 18.Cameron C, Watson D, Robinson J (2014) Use of a synthetic cannabinoid in a correctional population for posttraumatic stress disorder–related insomnia and nightmares, chronic pain, harm reduction, and other indications: A retrospective evaluation. Journal of clinical psychopharmacology 34:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Go Canada (2017) Canadian cannabis survey 2017 - summary In:
- 20.Carey CE, Agrawal A, Bucholz KK, Hartz SM, Lynskey MT, Nelson EC, Bierut LJ, Bogdan R (2016) Associations between polygenic risk for psychiatric disorders and substance involvement. Frontiers in genetics 7:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chambers RA, Krystal JH, Self DW (2001) A neurobiological basis for substance abuse comorbidity in schizophrenia. Biological psychiatry 50:71–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Charilaou P, Agnihotri K, Garcia P, Badheka A, Frenia D, Yegneswaran B (2017) Trends of cannabis use disorder in the inpatient: 2002 to 2011. The American journal of medicine 130:678–687. e677 [DOI] [PubMed] [Google Scholar]
- 23.Compton WM, Han B, Jones CM, Blanco C, Hughes A (2016) Marijuana use and use disorders in adults in the USA, 2002–14: Analysis of annual cross-sectional surveys. The Lancet Psychiatry 3:954–964 [DOI] [PubMed] [Google Scholar]
- 24.Conway KP, Swendsen J, Husky MM, He J-P, Merikangas KR (2016) Association of lifetime mental disorders and subsequent alcohol and illicit drug use: Results from the national comorbidity survey–adolescent supplement. Journal of the American Academy of Child & Adolescent Psychiatry 55:280–288 [DOI] [PubMed] [Google Scholar]
- 25.Copeland J, Rooke S, Swift W (2013) Changes in cannabis use among young people: Impact on mental health. Current opinion in psychiatry 26:325–329 [DOI] [PubMed] [Google Scholar]
- 26.Cougle JR, Bonn-Miller MO, Vujanovic AA, Zvolensky MJ, Hawkins KA (2011) Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychology of Addictive Behaviors 25:554. [DOI] [PubMed] [Google Scholar]
- 27.Cougle JR, Hakes JK, Macatee RJ, Chavarria J, Zvolensky MJ (2015) Quality of life and risk of psychiatric disorders among regular users of alcohol, nicotine, and cannabis: An analysis of the national epidemiological survey on alcohol and related conditions (nesarc). Journal of psychiatric research 66:135–141 [DOI] [PubMed] [Google Scholar]
- 28.Crean RD, Crane NA, Mason BJ (2011) An evidence based review of acute and longterm effects of cannabis use on executive cognitive functions. Journal of addiction medicine 5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crippa JA, Guimarães FS, Campos AC, Zuardi AW (2018) Translational investigation of the therapeutic potential of cannabidiol (cbd): Toward a new age. Frontiers in immunology 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curran H, Morgan C (2014) Desired and undesired effects of cannabis on the human mind and psychological well-being Handbook of Cannabis Oxford, UK: Oxford University Press UK:647–660 [Google Scholar]
- 31.Curran HV, Freeman TP, Mokrysz C, Lewis DA, Morgan CJ, Parsons LH (2016) Keep off the grass? Cannabis, cognition and addiction. Nature Reviews Neuroscience 17:293. [DOI] [PubMed] [Google Scholar]
- 32.D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Braley G, Gueorguieva R, Krystal JH (2004) The psychotomimetic effects of intravenous delta-9tetrahydrocannabinol in healthy individuals: Implications for psychosis. Neuropsychopharmacology 29:1558. [DOI] [PubMed] [Google Scholar]
- 33.D’Souza DC, Abi-Saab WM, Madonick S, Forselius-Bielen K, Doersch A, Braley G, Gueorguieva R, Cooper TB, Krystal JH (2005) Delta-9-tetrahydrocannabinol effects in schizophrenia: Implications for cognition, psychosis, and addiction. Biological psychiatry 57:594–608 [DOI] [PubMed] [Google Scholar]
- 34.Danielsson A-K, Lundin A, Agardh E, Allebeck P, Forsell Y (2016) Cannabis use, depression and anxiety: A 3-year prospective population-based study. Journal of affective disorders 193:103–108 [DOI] [PubMed] [Google Scholar]
- 35.Davis GP, Compton MT, Wang S, Levin FR, Blanco C (2013) Association between cannabis use, psychosis, and schizotypal personality disorder: Findings from the national epidemiologic survey on alcohol and related conditions. Schizophrenia research 151:197–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Degenhardt L, Coffey C, Romaniuk H, Swift W, Carlin JB, Hall WD, Patton GC (2013) The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction 108:124–133 [DOI] [PubMed] [Google Scholar]
- 37.Degenhardt L, Hall W, Lynskey M (2001) The relationship between cannabis use, depression and anxiety among australian adults: Findings from the national survey of mental health and well-being. Social psychiatry and psychiatric epidemiology 36:219–227 [DOI] [PubMed] [Google Scholar]
- 38.Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, Bianconi F, GardnerSood P, O’Connor J, Russo M (2015) Proportion of patients in south london with firstepisode psychosis attributable to use of high potency cannabis: A case-control study. The Lancet Psychiatry 2:233–238 [DOI] [PubMed] [Google Scholar]
- 39.Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, Russo M, Paparelli A (2009) High-potency cannabis and the risk of psychosis. The British Journal of Psychiatry 195:488–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, Marconi A, La Cascia C, Reis Marques T, Pariante C (2013) Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophrenia bulletin 40:1509–1517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dorard G, Berthoz S, Phan O, Corcos M, Bungener C (2008) Affect dysregulation in cannabis abusers. European child & adolescent psychiatry 17:274–282 [DOI] [PubMed] [Google Scholar]
- 42.Duperrouzel J, Hawes SW, Lopez-Quintero C, Pacheco-Colón I, Comer J, Gonzalez R (2018) The association between adolescent cannabis use and anxiety: A parallel process analysis. Addictive behaviors 78:107–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dworkin ER, Kaysen D, Bedard-Gilligan M, Rhew IC, Lee CM (2017) Daily-level associations between ptsd and cannabis use among young sexual minority women. Addictive behaviors 74:118–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Earleywine M, Barnwell SS (2007) Decreased respiratory symptoms in cannabis users who vaporize. Harm Reduction Journal 4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Earleywine M, Bolles JR (2014) Marijuana, expectancies, and post-traumatic stress symptoms: A preliminary investigation. Journal of psychoactive drugs 46:171–177 [DOI] [PubMed] [Google Scholar]
- 46.Earleywine M, Van Dam NT (2010) Case studies in cannabis vaporization. Addiction Research & Theory 18:243–249 [Google Scholar]
- 47.ElSohly M (2014) Potency monitoring program quarterly report no. 123—reporting period: 09. In:16/2013–12/15/2013
- 48.ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC (2016) Changes in cannabis potency over the last 2 decades (1995–2014): Analysis of current data in the united states. Biological psychiatry 79:613–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ersche KD, Williams GB, Robbins TW, Bullmore ET (2013) Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Current opinion in neurobiology 23:615–624 [DOI] [PubMed] [Google Scholar]
- 50.Feingold D, Weiser M, Rehm J, Lev-Ran S (2016) The association between cannabis use and anxiety disorders: Results from a population-based representative sample. European Neuropsychopharmacology 26:493–505 [DOI] [PubMed] [Google Scholar]
- 51.Feingold D, Weiser M, Rehm J, Lev-Ran S (2015) The association between cannabis use and mood disorders: A longitudinal study. Journal of affective disorders 172:211–218 [DOI] [PubMed] [Google Scholar]
- 52.Fergusson DM, Boden JM, Horwood LJ (2006) Cannabis use and other illicit drug use: Testing the cannabis gateway hypothesis. Addiction 101:556–569 [DOI] [PubMed] [Google Scholar]
- 53.Flórez-Salamanca L, Secades-Villa R, Budney AJ, García-Rodríguez O, Wang S, Blanco C (2013) Probability and predictors of cannabis use disorders relapse: Results of the national epidemiologic survey on alcohol and related conditions (nesarc). Drug and alcohol dependence 132:127–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Foti DJ, Kotov R, Guey LT, Bromet EJ (2010) Cannabis use and the course of schizophrenia: 10-year follow-up after first hospitalization. American Journal of Psychiatry 167:987–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Frank B, Serpell M, Hughes J, Matthews J, Kapur D (2008) Comparison of analgesic effects and patient tolerability of nabilone and dihydrocodeine for chronic neuropathic pain: Randomised, crossover, double blind study. Bmj 336:199–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fraser GA (2009) The use of a synthetic cannabinoid in the management of treatment‐resistant nightmares in posttraumatic stress disorder (ptsd). CNS neuroscience & therapeutics 15:84–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gage SH, Hickman M, Heron J, Munafò MR, Lewis G, Macleod J, Zammit S (2015) Associations of cannabis and cigarette use with depression and anxiety at age 18: Findings from the avon longitudinal study of parents and children. PloS one 10:e0122896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Galvez-Buccollini JA, Proal AC, Tomaselli V, Trachtenberg M, Coconcea C, Chun J, Manschreck T, Fleming J, Delisi LE (2012) Association between age at onset of psychosis and age at onset of cannabis use in non-affective psychosis. Schizophrenia research 139:157–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.George TP, Hill KP, Vaccarino FJ (2018) Cannabis legalization and psychiatric disorders: Caveat “hemp-tor”. The Canadian Journal of Psychiatry:0706743718762387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gieringer D, St. Laurent J, Goodrich S (2004) Cannabis vaporizer combines efficient delivery of thc with effective suppression of pyrolytic compounds. Journal of Cannabis Therapeutics 4:7–27 [Google Scholar]
- 61.Giordano GN, Ohlsson H, Sundquist K, Sundquist J, Kendler K (2015) The association between cannabis abuse and subsequent schizophrenia: A swedish national co-relative control study. Psychological medicine 45:407–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grant S, Pedersen ER, Neighbors C (2016) Associations of posttraumatic stress disorder symptoms with marijuana and synthetic cannabis use among young adult us veterans: A pilot investigation. Journal of studies on alcohol and drugs 77:509–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Green B, Kavanagh D, Young R (2003) Being stoned: A review of self‐reported cannabis effects. Drug and alcohol review 22:453–460 [DOI] [PubMed] [Google Scholar]
- 64.Greer GR, Grob CS, Halberstadt AL (2014) Ptsd symptom reports of patients evaluated for the new mexico medical cannabis program. Journal of Psychoactive Drugs 46:73–77 [DOI] [PubMed] [Google Scholar]
- 65.Grotenhermen F (2004) Pharmacology of cannabinoids. Neuroendocrinology letters 25:14–23 [PubMed] [Google Scholar]
- 66.Guttmannova K, Kosterman R, White HR, Bailey JA, Lee JO, Epstein M, Jones TM, Hawkins JD (2017) The association between regular marijuana use and adult mental health outcomes. Drug and alcohol dependence 179:109–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hall W, Weier M (2015) Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clinical pharmacology & therapeutics 97:607–615 [DOI] [PubMed] [Google Scholar]
- 68.Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, Grant BF (2016) Prevalence and correlates of dsm-5 cannabis use disorder, 2012–2013: Findings from the national epidemiologic survey on alcohol and related conditions–iii. American Journal of Psychiatry 173:588–599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W (2007) Cannabis and anxiety and depression in young adults: A large prospective study. Journal of the American Academy of Child & Adolescent Psychiatry 46:408–417 [DOI] [PubMed] [Google Scholar]
- 70.Helle S, Ringen PA, Melle I, Larsen T-K, Gjestad R, Johnsen E, Lagerberg TV, Andreassen OA, Kroken RA, Joa I (2016) Cannabis use is associated with 3 years earlier onset of schizophrenia spectrum disorder in a naturalistic, multi-site sample (n= 1119). Schizophrenia research 170:217–221 [DOI] [PubMed] [Google Scholar]
- 71.Hill KP (2015) Marijuana: The unbiased truth about the world’s most popular weed. Simon and Schuster [Google Scholar]
- 72.Hill KP (2015) Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: A clinical review. JAMA 313:2474–2483 [DOI] [PubMed] [Google Scholar]
- 73.Hjorthøj C, Østergaard MLD, Benros ME, Toftdahl NG, Erlangsen A, Andersen JT, Nordentoft M (2015) Association between alcohol and substance use disorders and allcause and cause-specific mortality in schizophrenia, bipolar disorder, and unipolar depression: A nationwide, prospective, register-based study. The Lancet Psychiatry 2:801–808 [DOI] [PubMed] [Google Scholar]
- 74.Hodgson K, Almasy L, Knowles EE, Kent JW, Curran JE, Dyer TD, Göring HH, Olvera RL, Woolsey MD, Duggirala R (2017) The genetic basis of the comorbidity between cannabis use and major depression. Addiction 112:113–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Horwood LJ, Fergusson DM, Coffey C, Patton GC, Tait R, Smart D, Letcher P, Silins E, Hutchinson DM (2012) Cannabis and depression: An integrative data analysis of four australasian cohorts. Drug and alcohol dependence 126:369–378 [DOI] [PubMed] [Google Scholar]
- 76.Iseger TA, Bossong MG (2015) A systematic review of the antipsychotic properties of cannabidiol in humans. Schizophrenia research 162:153–161 [DOI] [PubMed] [Google Scholar]
- 77.Quickfall Jeremy MD, F.R.C.P. Crockford David MD, F.R.C.P., (2006) Brain neuroimaging in cannabis use: A review. The Journal of Neuropsychiatry and Clinical Neurosciences 18:318–332 [DOI] [PubMed] [Google Scholar]
- 78.Jetly R, Heber A, Fraser G, Boisvert D (2015) The efficacy of nabilone, a synthetic cannabinoid, in the treatment of ptsd-associated nightmares: A preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology 51:585–588 [DOI] [PubMed] [Google Scholar]
- 79.Johns A (2001) Psychiatric effects of cannabis. The British Journal of Psychiatry 178:116–122 [DOI] [PubMed] [Google Scholar]
- 80.Johnson MJ, Pierce JD, Mavandadi S, Klaus J, Defelice D, Ingram E, Oslin DW (2016) Mental health symptom severity in cannabis using and non-using veterans with probable ptsd. Journal of affective disorders 190:439–442 [DOI] [PubMed] [Google Scholar]
- 81.Kelley ME, Wan CR, Broussard B, Crisafio A, Cristofaro S, Johnson S, Reed TA, Amar P, Kaslow NJ, Walker EF (2016) Marijuana use in the immediate 5-year premorbid period is associated with increased risk of onset of schizophrenia and related psychotic disorders. Schizophrenia research 171:62–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kessler RC (2004) The epidemiology of dual diagnosis. Biological psychiatry 56:730737. [DOI] [PubMed] [Google Scholar]
- 83.Kevorkian S, Bonn-Miller MO, Belendiuk K, Carney DM, Roberson-Nay R, Berenz EC (2015) Associations among trauma, posttraumatic stress disorder, cannabis use, and cannabis use disorder in a nationally representative epidemiologic sample. Psychology of Addictive Behaviors 29:633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Khantzian EJ (2012) Reflections on treating addictive disorders: A psychodynamic perspective. The American journal on addictions 21:274–279 [DOI] [PubMed] [Google Scholar]
- 85.Khantzian EJ (1997) The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard review of psychiatry 4:231–244 [DOI] [PubMed] [Google Scholar]
- 86.Kim S-W, Dodd S, Berk L, Kulkarni J, de Castella A, Fitzgerald PB, Kim J-M, Yoon J-S, Berk M (2015) Impact of cannabis use on long-term remission in bipolar i and schizoaffective disorder. Psychiatry investigation 12:349–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Koob GF, Le Moal M (2001) Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 24:97. [DOI] [PubMed] [Google Scholar]
- 88.Koob GF, Volkow ND (2016) Neurobiology of addiction: A neurocircuitry analysis. The Lancet Psychiatry 3:760–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Koskinen J, Löhönen J, Koponen H, Isohanni M, Miettunen J (2009) Rate of cannabis use disorders in clinical samples of patients with schizophrenia: A meta-analysis. Schizophrenia bulletin 36:1115–1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Large M, Sharma S, Compton MT, Slade T, Nielssen O (2011) Cannabis use and earlier onset of psychosis: A systematic meta-analysis. Archives of general psychiatry 68:555–561 [DOI] [PubMed] [Google Scholar]
- 91.Lee JY, Brook JS, Finch SJ, Brook DW (2018) Trajectories of cannabis use beginning in adolescence associated with symptoms of posttraumatic stress disorder in the midthirties. Substance abuse 39:39–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lev-Ran S, Le Foll B, McKenzie K, George TP, Rehm J (2013) Cannabis use and cannabis use disorders among individuals with mental illness. Comprehensive psychiatry 54:589–598 [DOI] [PubMed] [Google Scholar]
- 93.Leweke F, Piomelli D, Pahlisch F, Muhl D, Gerth C, Hoyer C, Klosterkötter J, Hellmich M, Koethe D (2012) Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Translational psychiatry 2:e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Loflin M, Earleywine M (2014) A new method of cannabis ingestion: The dangers of dabs? Addictive behaviors 39:1430–1433 [DOI] [PubMed] [Google Scholar]
- 95.Lopez-Quintero C, de los Cobos JP, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C (2011) Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the national epidemiologic survey on alcohol and related conditions (nesarc). Drug and alcohol dependence 115:120–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lynskey M, Hall W (2000) The effects of adolescent cannabis use on educational attainment: A review. Addiction 95:1621–1630 [DOI] [PubMed] [Google Scholar]
- 97.Ma M, Coles AS, George TP (2018) Understanding and treating co-occurring bipolar disorder and substance use disorders. Psychiatric Times 35: p. 8–9.:8–9. [Google Scholar]
- 98.Manhapra A, Stefanovics E, Rosenheck R (2015) Treatment outcomes for veterans with ptsd and substance use: Impact of specific substances and achievement of abstinence. Drug and alcohol dependence 156:70–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Andreasson S, Allebeck P (2014) Prognosis of schizophrenia in persons with and without a history of cannabis use. Psychological medicine 44:2513–2521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E (2016) Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophrenia bulletin 42:1262–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.McGuire P, Robson P, Cubala WJ, Vasile D, Morrison PD, Barron R, Taylor A, Wright S (2017) Cannabidiol (cbd) as an adjunctive therapy in schizophrenia: A multicenter randomized controlled trial. American Journal of Psychiatry 175:225–231 [DOI] [PubMed] [Google Scholar]
- 102.McGuire P, Robson P, Cubala WJ, Vasile D, Morrison PD et al. (2018) Cannabidiol (cbd) as an adjunctive therapy in schizophrenia: A multicenter randomized controlled trial. Am J Psychiatry 175:225–231. [DOI] [PubMed] [Google Scholar]
- 103.Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, McDonald K, Ward A, Poulton R, Moffitt TE (2012) Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences:201206820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Metrik J, Bassett SS, Aston ER, Jackson KM, Borsari B (2018) Medicinal versus recreational cannabis use among returning veterans. Translational Issues in Psychological Science 4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, Borsari B (2016) The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with ptsd and mdd. Psychology of Addictive Behaviors 30:743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moitra E, Anderson BJ, Stein MD (2016) Reductions in cannabis use are associated with mood improvement in female emerging adults. Depression and anxiety 33:332–338 [DOI] [PubMed] [Google Scholar]
- 107.Morrison P, Zois V, McKeown D, Lee T, Holt D, Powell J, Kapur S, Murray R (2009) The acute effects of synthetic intravenous δ9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychological medicine 39:1607–1616 [DOI] [PubMed] [Google Scholar]
- 108.Narang S, Gibson D, Wasan AD, Ross EL, Michna E, Nedeljkovic SS, Jamison RN (2008) Efficacy of dronabinol as an adjuvant treatment for chronic pain patients on opioid therapy. The Journal of Pain 9:254–264 [DOI] [PubMed] [Google Scholar]
- 109.National Academies of Sciences E, Medicine (2017) The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. National Academies Press; [PubMed] [Google Scholar]
- 110.Nunberg H, Kilmer B, Pacula RL, Burgdorf JR (2011) An analysis of applicants presenting to a medical marijuana specialty practice in california. Journal of drug policy analysis 4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Østergaard ML, Nordentoft M, Hjorthøj C (2017) Associations between substance use disorders and suicide or suicide attempts in people with mental illness: A danish nation‐wide, prospective, register‐based study of patients diagnosed with schizophrenia, bipolar disorder, unipolar depression or personality disorder. Addiction 112:1250–1259 [DOI] [PubMed] [Google Scholar]
- 112.arsons LH, Hurd YL (2015) Endocannabinoid signalling in reward and addiction. Nature Reviews Neuroscience 16:579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Patel R, Wilson R, Jackson R, Ball M, Shetty H, Broadbent M, Stewart R, McGuire P, Bhattacharyya S (2015) Cannabis use and treatment resistance in first episode psychosis: A natural language processing study. The Lancet 385:S79. [DOI] [PubMed] [Google Scholar]
- 114.Piontek D, Kraus L, Bjarnason T, Demetrovics Z, Ramstedt M (2013) Individual and country-level effects of cannabis-related perceptions on cannabis use. A multilevel study among adolescents in 32 european countries. Journal of Adolescent Health 52:473–479 [DOI] [PubMed] [Google Scholar]
- 115.Quello SB, Brady KT, Sonne SC (2005) Mood disorders and substance use disorder: A complex comorbidity. Science & Practice Perspectives 3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rabin RA, Barr MS, Goodman MS, Herman Y, Zakzanis KK, Kish SJ, Kiang M, Remington G, George TP (2017) Effects of extended cannabis abstinence on cognitive outcomes in cannabis dependent patients with schizophrenia vs non-psychiatric controls. Neuropsychopharmacology [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rabin RA, Kozak K, Zakzanis KK, Remington G, George TP (2018) Effects of extended cannabis abstinence on clinical symptoms in cannabis dependent schizophrenia patients versus non-psychiatric controls. Schizophrenia research 194:55–61 [DOI] [PubMed] [Google Scholar]
- 118.Rabin RA, Zakzanis KK, Daskalakis ZJ, George TP (2013) Effects of cannabis use status on cognitive function, in males with schizophrenia. Psychiatry research 206:158–165 [DOI] [PubMed] [Google Scholar]
- 119.RachBeisel J, Scott J, Dixon L (1999) Co-occurring severe mental illness and substance use disorders: A review of recent research. Psychiatric services 50:1427–1434 [DOI] [PubMed] [Google Scholar]
- 120.Rasic D, Weerasinghe S, Asbridge M, Langille DB (2013) Longitudinal associations of cannabis and illicit drug use with depression, suicidal ideation and suicidal attempts among nova scotia high school students. Drug and alcohol dependence 129:49–53 [DOI] [PubMed] [Google Scholar]
- 121.Ratheesh A, Cotton SM, Betts JK, Chanen A, Nelson B, Davey CG, McGorry PD, Berk M, Bechdolf A (2015) Prospective progression from high-prevalence disorders to bipolar disorder: Exploring characteristics of pre-illness stages. Journal of affective disorders 183:45–48 [DOI] [PubMed] [Google Scholar]
- 122.Reinarman C, Nunberg H, Lanthier F, Heddleston T (2011) Who are medical marijuana patients? Population characteristics from nine california assessment clinics. Journal of psychoactive drugs 43:128–135 [DOI] [PubMed] [Google Scholar]
- 123.Richter KP, Levy S (2014) Big marijuana—lessons from big tobacco. N Engl J Med 371:399–401 [DOI] [PubMed] [Google Scholar]
- 124.Roitman P, Mechoulam R, Cooper-Kazaz R, Shalev A (2014) Preliminary, open-label, pilot study of add-on oral δ 9-tetrahydrocannabinol in chronic post-traumatic stress disorder. Clinical drug investigation 34:587–591 [DOI] [PubMed] [Google Scholar]
- 125.Rotermann M, Langlois K (2015) Prevalence and correlates of marijuana use in canada, 2012. In:Statistics Canada Ottawa, Ontario: [PubMed] [Google Scholar]
- 126.Sagar KA, Dahlgren MK, Racine MT, Dreman MW, Olson DP, Gruber SA (2016) Joint effects: A pilot investigation of the impact of bipolar disorder and marijuana use on cognitive function and mood. PloS one 11:e0157060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sami MB, Rabiner EA, Bhattacharyya S (2015) Does cannabis affect dopaminergic signaling in the human brain? A systematic review of evidence to date. European Neuropsychopharmacology 25:1201–1224 [DOI] [PubMed] [Google Scholar]
- 128.Schoeler T, Monk A, Sami MB, Klamerus E, Foglia E, Brown R, Camuri G, Altamura AC, Murray R, Bhattacharyya S (2016) Continued versus discontinued cannabis use in patients with psychosis: A systematic review and meta-analysis. The Lancet Psychiatry 3:215–225 [DOI] [PubMed] [Google Scholar]
- 129.Schoeler T, Theobald D, Pingault J-B, Farrington DP, Coid JW, Bhattacharyya S (2018) Developmental sensitivity to cannabis use patterns and risk for major depressive disorder in mid-life: Findings from 40 years of follow-up. Psychological medicine:1–8 [DOI] [PubMed] [Google Scholar]
- 130.Scholes-Balog KE, Hemphill SA, Evans-Whipp TJ, Toumbourou JW, Patton GC (2016) Developmental trajectories of adolescent cannabis use and their relationship to young adult social and behavioural adjustment: A longitudinal study of australian youth. Addictive behaviors 53:11–18 [DOI] [PubMed] [Google Scholar]
- 131.Schuckit MA (2006) Comorbidity between substance use disorders and psychiatric conditions. Addiction 101:76–88 [DOI] [PubMed] [Google Scholar]
- 132.Schuermeyer J, Salomonsen-Sautel S, Price RK, Balan S, Thurstone C, Min S-J, Sakai JT (2014) Temporal trends in marijuana attitudes, availability and use in colorado compared to non-medical marijuana states: 2003–11. Drug & Alcohol Dependence 140:145–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sexton M, Cuttler C, Finnell JS, Mischley LK (2016) A cross-sectional survey of medical cannabis users: Patterns of use and perceived efficacy. Cannabis and cannabinoid research 1:131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sherva R, Wang Q, Kranzler H, Zhao H, Koesterer R, Herman A, Farrer LA, Gelernter J (2016) Genome-wide association study of cannabis dependence severity, novel risk variants, and shared genetic risks. JAMA psychiatry 73:472–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Skrabek RQ, Galimova L, Ethans K, Perry D (2008) Nabilone for the treatment of pain in fibromyalgia. The Journal of Pain 9:164–173 [DOI] [PubMed] [Google Scholar]
- 136.Solowij N, Stephens RS, Roffman RA, Babor T, Kadden R, Miller M, Christiansen K, McRee B, Vendetti J (2002) Cognitive functioning of long-term heavy cannabis users seeking treatment. Jama 287:1123–1131 [DOI] [PubMed] [Google Scholar]
- 137.Strakowski SM, DelBello MP, Fleck DE, Adler CM, Anthenelli RM, Keck PE, Arnold LM, Amicone J (2007) Effects of co-occurring cannabis use disorders on the course of bipolar disorder after a first hospitalization for mania. Archives of general psychiatry 64:57–64 [DOI] [PubMed] [Google Scholar]
- 138.Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas KR, Sampson N, Kessler RC (2010) Mental disorders as risk factors for substance use, abuse and dependence: Results from the 10‐year follow‐up of the national comorbidity survey. Addiction 105:1117–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Swendsen JD, Merikangas KR (2000) The comorbidity of depression and substance use disorders. Clinical psychology review 20:173–189 [DOI] [PubMed] [Google Scholar]
- 140.Tournier M, Sorbara F, Gindre C, Swendsen JD, Verdoux H (2003) Cannabis use and anxiety in daily life: A naturalistic investigation in a non-clinical population. Psychiatry research 118:1–8 [DOI] [PubMed] [Google Scholar]
- 141.Tull MT, McDermott MJ, Gratz KL (2016) Marijuana dependence moderates the effect of posttraumatic stress disorder on trauma cue reactivity in substance dependent patients. Drug and alcohol dependence 159:219–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Van Dam NT, Bedi G, Earleywine M (2012) Characteristics of clinically anxious versus non-anxious regular, heavy marijuana users. Addictive behaviors 37:1217–1223 [DOI] [PubMed] [Google Scholar]
- 143.van der Pol P, Liebregts N, de Graaf R, ten Have M, Korf DJ, van den Brink W, van Laar M (2013) Mental health differences between frequent cannabis users with and without dependence and the general population. Addiction 108:1459–1469 [DOI] [PubMed] [Google Scholar]
- 144.Van Laar M, Van Dorsselaer S, Monshouwer K, De Graaf R (2007) Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population? Addiction 102:1251–1260 [DOI] [PubMed] [Google Scholar]
- 145.Van Os J, Bak M, Hanssen M, Bijl R, De Graaf R, Verdoux H (2002) Cannabis use and psychosis: A longitudinal population-based study. American journal of epidemiology 156:319–327 [DOI] [PubMed] [Google Scholar]
- 146.Vandermeeren R, Hebbrecht M (2012) The dual process model of addiction. Towards an integrated model? Tijdschrift voor psychiatrie 54:731–740 [PubMed] [Google Scholar]
- 147.Vandrey R, Raber JC, Raber ME, Douglass B, Miller C, Bonn-Miller MO (2015) Cannabinoid dose and label accuracy in edible medical cannabis products. Jama 313:2491–2493 [DOI] [PubMed] [Google Scholar]
- 148.Villagonzalo K-A, Dodd S, Ng F, Mihaly S, Langbein A, Berk M (2011) The relationship between substance use and posttraumatic stress disorder in a methadone maintenance treatment program. Comprehensive psychiatry 52:562–566 [DOI] [PubMed] [Google Scholar]
- 149.Volkow ND, Baler RD, Compton WM, Weiss SR (2014) Adverse health effects of marijuana use. New England Journal of Medicine 370:2219–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Volkow ND, Li T-K (2004) Drug addiction: The neurobiology of behaviour gone awry. Nature Reviews Neuroscience 5:963. [DOI] [PubMed] [Google Scholar]
- 151.Walsh Z, Callaway R, Belle-Isle L, Capler R, Kay R, Lucas P, Holtzman S (2013) Cannabis for therapeutic purposes: Patient characteristics, access, and reasons for use. International Journal of Drug Policy 24:511–516 [DOI] [PubMed] [Google Scholar]
- 152.Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, Misso K, Ryder S (2015) Cannabinoids for medical use: A systematic review and meta-analysis. Jama 313:2456–2473 [DOI] [PubMed] [Google Scholar]
- 153.Wilkinson ST, Stefanovics E, Rosenheck RA (2015) Marijuana use is associated with worse outcomes in symptom severity and violent behavior in patients with posttraumatic stress disorder. The Journal of clinical psychiatry 76:1174–1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Wise RA, Koob GF (2014) The development and maintenance of drug addiction. Neuropsychopharmacology 39:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zorrilla I, Aguado J, Haro J, Barbeito S, Lopez Zurbano S, Ortiz A, Lopez P, Gonzalez‐Pinto A (2015) Cannabis and bipolar disorder: Does quitting cannabis use during manic/mixed episode improve clinical/functional outcomes? Acta Psychiatrica Scandinavica 131:100–110 [DOI] [PubMed] [Google Scholar]
- 156.Zvolensky MJ, Lewinsohn P, Bernstein A, Schmidt NB, Buckner JD, Seeley J, BonnMiller MO (2008) Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. Journal of psychiatric research 42:1017–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]


