Abstract
In the context of age-related declines in physical activity (PA) and the dramatic increase in ageing populations in many countries, this paper sheds further light on the link between PA and self-perceived health (SPH) by examining whether the magnitude of this relationship is age specific. With a sample of 14,456 Spanish individuals aged 18–69, we estimated three levels of intensity in PA using the International Physical Activity Questionnaire. Individuals who did more PA per week showed higher levels of SPH (β = 0.28; 95% CI 0.24–0.32), and age moderated this relationship, with a positive effect over age 49. People aged 50–59 and 60–69 who practiced PA had higher probabilities of better SPH compared with those aged 40–49 (β = 0.14; 95% CI 0.04–0.24) and (β = 0.32; 95% CI 0.21–0.43), respectively. This association between PA and SPH also depended on the intensity of PA, especially for walking (β = 0.14; 95% CI 0.04–0.24). In particular, in comparison with people age 40–49, a statistically significant relationship with SPH was found among people age 50–59 who walked (β = 0.22; 95% CI 0.07–0.36) and people age 60–69 who did moderate PA (β = 0.38; 95% CI 0.23–0.54). This paper provides a major rationale for the design, organisation and implementation of public policies promoting PA and healthy ageing for different age groups.
Keywords: Physical activity, Age, Self-perceived health, Ageing, Walking, Subjective well-being
Introduction
In the context of the increasing percentage of older adults in many countries (Beard et al. 2012), it is essential to ensure that the population ages healthily and that increased longevity is accompanied by better health-related quality of life (Vagetti et al. 2015). Physical activity (PA) is widely recognised as a key factor in improving health and preventing chronic, non-communicable diseases (World Health Organization [WHO] 2010), which is especially relevant for older people, considering that health decreases with age (i.e. Szende et al. 2014). Preferences for PA evolve and change over an individual’s lifespan. Among young people, motivations such as sensation-seeking and pleasure can be potential sources of engaging in PA, in particular leisure PA, while among people older than 50, concern for health is more relevant (Brunet and Sabiston 2011).
The aim of this paper is to examine the relationship between PA and self-perceived health (SPH), and to test this relationship by age group. This study considers three different ways of being involved in PA in terms of intensity (walking, moderate and vigorous PA), using data from a survey about lifestyles, PA, SPH and use of health services in a sample of Spanish adults aged 18 and older. This research might be useful for assessing the value of PA and for policy interventions to contribute to the development of an active ageing population.
We formulated two research questions. The first concerns the relationship between PA level (including walking) and SPH level, and the role that age plays. We hypothesised that individuals doing PA would show higher levels of SPH and that age moderates this relationship. To justify these hypotheses we argue, primarily, that there is a vast literature extensively confirming the positive relationship between self-reported PA and SPH (e.g. Brown et al. 2004, 2014; Bize et al. 2007; Cohen et al. 2016; Mudrak et al. 2016; Lera-Lopez et al. 2017). Few studies have considered the role played by age in the relationship between PA and SPH. In particular, Brown et al. (2004) and Cimarras-Otal et al. (2014) have shown that associations between these variables tend to be stronger among adults aged 45 and older. In contrast, Cohen et al. (2016) recently showed that for younger adults (i.e. aged 30–59) this relationship is stronger, compared to older adults.
The second research question addresses the extent to which the potential positive association between PA and SPH level depends on the intensity of the PA. The effect of PA by intensity has been neglected in the empirical evidence. Previous evidence is scarce but shows significant differences in the association between PA and health outcomes depending on the intensity of PA. One set of studies has shown a positive relationship between intensity and health outcomes. For example, Meyer et al. (2005) reported that vigorous PA is more closely related to better SPH than moderate PA for adults aged 50 and older in Switzerland. Similar results were found by Casado-Pérez et al. (2015) among the adult working population in Spain, and by Vuillemin et al. (2005) in French adults. Likewise, Heesch et al. (2012), in a sample of women in their 50–80 s, showed that greater amounts of total PA are particularly associated with better health. On the other hand, Vagetti et al. (2015) showed that light walking has a higher impact on different health outcomes than moderate and vigorous intensity, although the study was limited to older adults. Nevertheless, no empirical evidence has been presented about how this relationship might change among different age groups. Considering this evidence, we hypothesise that the role played by age as a moderating variable in the relationship of PA with the level of SPH varies depending on the nature of the PA (i.e. its intensity). In this study, we propose the conceptual model presented in Fig. 1.
Fig. 1.
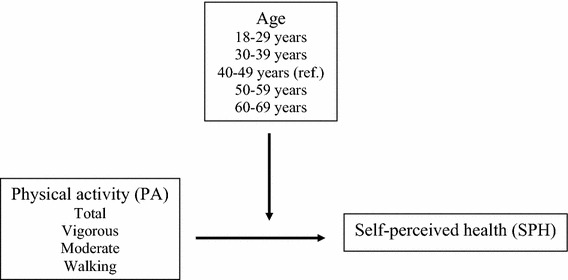
Theoretical model
Methods
Sample
The database used in this study comes from the Spanish National Health Survey (NHS) 2011–2012. This survey is conducted periodically by the Spanish Ministry of Health, Social Services and Equality in collaboration with the Spanish National Statistics Institute (INE 2015). The collection period was from June 2011 to June 2012 and was representative at country and regional levels. The questionnaire was structured in three modules. The first module sought information about the informant’s state of health. The second requested information about healthcare services utilisation and preventative practices. The third collected data about lifestyle features such as the practice of PA, tobacco use and alcohol consumption, some physical characteristics (i.e. height and weight) and demographic variables.
To collect data, each household first was sent a letter from the INE. The letter notified them that they had been selected for the survey and requested collaboration. Data were collected by computer-assisted personal interview (CAPI) and, in exceptional cases, by a personal telephone interview. The initial sample was 21,007 individuals, and the estimated response rate was 89.6%. The final sample, however, decreased by 1990 individuals because of missing values, mainly due to the lack of an answer or an ‘I don’t know’ answer to at least one question in the questionnaire. In addition, people younger than 18 (383 individuals) and aged 70 and older (4178 individuals) were omitted because the short version of the International Physical Activity Questionnaire (IPAQ), applied in the survey to measure PA, has not been validated for people in those age ranges. Consequently, our final sample included 14,456 individuals between age 18 and 69. The sample is representative of the regional distribution of the Spanish population in terms of age, gender and size of urbanisation (INE 2015).
Measures and variables
Self-perceived health (SPH)
SPH is the dependent variable. It is worth noting that the use of self-assessed health status as a measure of health is common in empirical research in different disciplines (Crossley and Kennedy 2002; Simon et al. 2005). Various scales have been developed to quantify SPH, such as health-related quality of life scales (e.g. Brown et al. 2014) and the EuroQol instrument with 5 dimensions (EQ-5D) (e.g. Rabin and Charro 2001). The EQ-5D is a standardised health-related quality of life questionnaire that was developed by the EuroQol Group to provide a simple, generic measure of health for clinical and economic appraisal (EuroQol Group 1990). The EQ-5D has consistently shown excellent metric properties (Chen et al. 2016; Nolan et al. 2016).
In this study, we applied the EQ-5D-5L (Luo et al. 2013; Szende et al. 2014; Cabasés 2015) as a measure of SPH. The EQ-5D-5L is a new version of the EQ-5D (Herdman et al. 2011) in which the current health status of individuals is described through 5 dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each of these dimensions has five possible answers or severity levels: no problem (1), slight problems (2), moderate problems (3), severe problems (4), extreme problems or inability (5). Recently, the EuroQol group has developed a study protocol for obtaining preferences from the results of a series of pilot studies carried out by research teams worldwide to report utilities of health states of the EQ-5D-5L (Devlin et al. 2013). This common protocol already has been applied in Spain to a representative sample of the general population (Ramos-Goñi et al. 2017a), giving a rank of values between 1 and − 0416 (Ramos-Goñi et al. 2017b).
Physical activity
To measure PA and its intensity, we used the short version of the IPAQ developed by Craig et al. (2003) and adapted to the Spanish language by Román Viñas et al. (2013). The IPAQ considers frequency (days per week) and time (minutes) doing PA each day. With the information provided by the IPAQ, we calculated the total minutes of PA per week, widely considered as a measure of the level of PA (Abu-Omar and Rütten 2008; WHO 2010). These estimations were made for the whole PA and for three intensities (vigorous, moderate and walking). In our sample, PA ranged between zero minutes (minimum level) and 3780 min (maximum level) per week. Within levels of intensity, PA was between zero minutes and 1263 min per week. To obtain coefficients in the regression models, we divided minutes by 100.
Age
SPH usually decreases with increasing age (see Szende et al. 2014 for an international study using a sample of 24 countries). We considered age as a moderator between PA and SHP. This variable was measured, following previous literature (Ministry of Health, Social Services and Equality 2014), through the use of five dummy variables that took a value of 1 when the individual had their age indicated in the variable and 0 otherwise. The five age groups were 18–29, 30–39, 40–49, 50–59 and 60–69. In the analysis, only four dummy variables are included, since 40–49 years is the reference category.
Control variables
In line with the previous literature, several control variables were included. Gender was included as a control variable because usually men report higher SPH levels than women (Szende et al. 2014).
There is an increasing awareness of the relationship between body mass index (BMI) and different measures of quality of life, including SPH (for a recent review of the literature, see Cohen et al. 2016). We created four dummy variables reflecting commonly accepted BMI ranges: underweight (< 18.5), normal weight (18.5–25, reference category), overweight (> 25–30) and obese (> 30) (Cohen et al. 2016). In the analysis, only three dummy variables are included, since normal weight is the reference category.
Diseases also were considered. We used the International Classification of Diseases (ICD-10) (http://apps.who.int/classifications/icd10/browse/2016/en) to generate groups of diseases based on international agreement. In particular, we classified these diseases into four categories: metabolic diseases (endocrine, nutritional and metabolic diseases), skeletal and muscular diseases (back pain, thoracic and cervical problems, arthrosis and osteoporosis), cardiovascular and circulatory diseases (hypertensive diseases, ischaemic heart diseases, diseases of arteries, arterioles and capillaries and cerebrovascular diseases) and emotional diseases (recurrent anxiety, depression and other mental problems). These groups of diseases comprise some of the principal diseases in the Spanish adult population, and they generally have been included in previous studies showing that having these diseases is related to lower self-rated health (Heller et al. 2009; Waller et al. 2015; Larsen et al. 2016).
Finally, there are other variables that affect SPH, such as the use of healthcare services (Heller et al. 2009). In our study, we included three variables to consider healthcare service use. The first was the number of times during the preceding 12 months that the interviewed person had used emergency services. The second was the number of days during the preceding year that the interviewed person was admitted to a day hospital. The third was the number of days that the interviewed person was hospitalised overnight during the preceding year.
Table 1 shows the mean values and the frequency distribution of all of the variables included in our analysis for the whole sample as well as for the age groups.
Table 1.
Descriptive statistics, mean and standard deviation (SD), of all variables
| Whole sample | Age 18–29 | Age 30–39 | Age 40–49 | Age 50–59 | Age 60–69 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs: 15,069 | Obs: 2206 | Obs: 3473 | Obs: 3619 | Obs: 3080 | Obs: 2691 | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| SPH (EQ5D5L) | 0.940 | 0.145 | 0.981 | 0.077 | 0.9695 | 0.099 | 0.951 | 0.123 | 0.910 | 0.181 | 0.892 | 0.189 |
| Total PA (min. week) | 615.371 | 598.822 | 665.427 | 618.772 | 614.067 | 619.190 | 588.017 | 587.459 | 604.794 | 592.212 | 624.373 | 575.101 |
| Vigorous PA (min. week) | 75.856 | 219.647 | 129.354 | 265.959 | 95.577 | 240.107 | 71.212 | 213.430 | 55.266 | 197.222 | 36.244 | 164.514 |
| Moderate PA (min. week) | 123.000 | 280.088 | 127.963 | 267.256 | 119.895 | 278.182 | 117.323 | 274.682 | 124.839 | 287.548 | 128.280 | 290.997 |
| Walking PA (min. week) | 416.515 | 419.454 | 408.109 | 421.964 | 398.595 | 431.245 | 399.482 | 414.695 | 424.688 | 415.012 | 459.849 | 410.001 |
| Underweight BMI (< 18.5 kg/m2) | 1.91% | 0.137 | 5.66% | 0.231 | 1.76% | 0.131 | 1.38% | 0.117 | 1.17% | 0.107 | 0.59% | 0.077 |
| Normal BMI (ref.) (18.5–25) | 45.52% | 0.137 | 65.61% | 0.475 | 52.91% | 0.499 | 45.81% | 0.498 | 35.48% | 0.479 | 30.61% | 0.461 |
| Overweight BMI (> 25–30 kg/m2) | 36.08% | 0.480 | 21.57% | 0.411 | 33.13% | 0.471 | 37.52% | 0.484 | 40.99% | 0.492 | 44.24% | 0.497 |
| Obese BM I(> 30 kg/m2) | 16.48% | 0.371 | 7.16% | 0.258 | 12.20% | 0.327 | 15.28% | 0.360 | 22.36% | 0.417 | 24.55% | 0.430 |
| Skeletal-muscular (0–3 diseases) | 0.192 | 0.479 | 0.053 | 0.241 | 0.091 | 0.323 | 0.135 | 0.392 | 0.276 | 0.553 | 0.415 | 0.675 |
| Metabolic (0–3 diseases) | 0.073 | 0.289 | 0.015 | 0.123 | 0.031 | 0.175 | 0.058 | 0.252 | 0.114 | 0.364 | 0.149 | 0.407 |
| Emotional (0–3 diseases) | 0.004 | 0.078 | 0.000 | 0.000 | 0.000 | 0.000 | 0.001 | 0.024 | 0.007 | 0.109 | 0.012 | 0.141 |
| Cardiovascular-respiratory (0–6 diseases) | 0.615 | 0.934 | 0.184 | 0.482 | 0.311 | 0.622 | 0.528 | 0.817 | 0.856 | 1.038 | 1.201 | 1.170 |
| Emergency services | 0.259 | 0.438 | 0.324 | 0.468 | 0.297 | 0.457 | 0.233 | 0.423 | 0.236 | 0.424 | 0.217 | 0.412 |
| Hospitalised | 0.078 | 0.268 | 0.067 | 0.250 | 0.089 | 0.285 | 0.064 | 0.245 | 0.078 | 0.268 | 0.090 | 0.287 |
| Day hospital | 0.075 | 0.263 | 0.058 | 0.233 | 0.064 | 0.245 | 0.068 | 0.252 | 0.092 | 0.289 | 0.090 | 0.287 |
| Male | 0.495 | 0.500 | 0.499 | 0.500 | 0.503 | 0.500 | 0.504 | 0.500 | 0.488 | 0.500 | 0.475 | 0.499 |
Statistical analysis
Given the nature of the dependent variables, ordinary least squares models were estimated to assess the relationship of PA and age with the level of SPH among the Spanish population. We estimated several models using different measures of PA. Firstly, we considered the total PA in minutes per week in all PAs undertaken by the individual, and, secondly, we considered the number of minutes per week by intensity level (walking, moderate and vigorous PA). Moreover, the moderating effect was graphically illustrated as the variation in the slope of the regression line of the dependent variable and the independent variable as a function of the moderator variable.
Regarding reference category, we considered the interval of 40–49 years as the reference group for three reasons. First, middle-aged adults in their 40 s may experience some physiological changes that might affect their physical performance, but health problems have not yet represented a major limiting or impairment problem. Second, previous studies have emphasised how the relationship between PA and SPH seems to be stronger in people in their 40 s (Brown et al. 2004; Meyer et al. 2005; Cimarras-Otal et al. 2014). Third, evidence from Spain has shown that the health expenditure per capita by age group starts increasing after age 40 (Hernández de Cos and Moral-Benito 2011).
It also should be mentioned that, in order to test multicollinearity, condition indices and variance inflation factors were tested and showed values below the usual thresholds of 30 and 5, respectively (Judge et al. 1988), indicating that multicollinearity is not a problem in our models. Statistical analyses were carried out using STATA 14 (StataCorp LLC 2017).
Results
Descriptive statistics
Table 1 presents the mean descriptive statistics of the dependent and independent variables. The number of people in each age group is reasonably well-balanced in the sample and is representative of the Spanish population, as well as the number of males and females. In the sample, 14.6% were aged 18–29, 23.1% were 30–39, 24.0% were 40–49, 20.4% were 50–59, and 17.9% were 60–69. Regarding gender, in the sample, 49.5% were males and 50.5% were females. For the whole sample, we can see that people perceived a good level of SPH; the maximum perception was among the youngest age group and it decreased with age, particularly among those aged 50 and older.
Regarding the practice of PA, Table 1 shows that PA decreased until 49 years of age, and then it started to increase steadily. Consequently, it seems that PA follows a U-shaped curve with two peaks, one occurring among those aged 18–29 and the other at ages 60–69. A similar pattern is followed by the level of moderate PA and walking, although in the case of walking the minimum level is observed among those aged 30–39. Only the level of vigorous PA steadily decreased with age. A lower level of vigorous PA was observed in people aged 60–69, who practice, on average, only 28.0% of the vigorous PA observed in people age 18–29.
Table 2 shows the correlations between the dependent, independent and control variables. The bivariate associations show that, in general, most are in line with expectations. SPH is positively and statistically significantly correlated with PA and is negatively associated with age.
Table 2.
Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. SPH | ||||||||||||||
| 2. Total PA | 0.119*** | |||||||||||||
| 3. Vigorous PA | 0.080*** | 0.473*** | ||||||||||||
| 4. Moderate PA | 0.048*** | 0.610*** | 0.160*** | |||||||||||
| 5. Walking PA | 0.096*** | 0.773*** | 0.046*** | 0.119*** | ||||||||||
| 6. BMI | − 0.144*** | − 0.030*** | − 0.047*** | − 0.004 | − 0.015 | |||||||||
| 7. Skeletal-muscular | − 0.310*** | − 0.045*** | − 0.065*** | − 0.019* | − 0.018* | 0.174*** | ||||||||
| 8. Metabolic | − 0.323*** | − 0.056*** | − 0.049*** | − 0.026** | − 0.038*** | 0.092*** | 0.273*** | |||||||
| 9. Emotional | − 0.154*** | − 0.019** | − 0.017* | − 0.006 | − 0.015 | 0.067*** | 0.207*** | 0.178*** | ||||||
| 10. Cardiovascular-respiratory | − 0.416*** | − 0.066*** | − 0.099*** | − 0.022** | − 0.028*** | 0.224*** | 0.432*** | 0.335*** | 0.164*** | |||||
| 11. Emergency services | − 0.155*** | − 0.028*** | − 0.006 | − 0.022** | − 0.022** | 0.021** | 0.096*** | 0.090*** | 0.024** | 0.113*** | ||||
| 12. Hospitalised | − 0.152*** | − 0.047*** | − 0.033*** | − 0.029*** | − 0.030*** | 0.022** | 0.069*** | 0.098*** | 0.027*** | 0.107*** | 0.275*** | |||
| 13. Day hospital | − 0.160*** | − 0.005 | − 0.019* | − 0.018* | 0.015 | 0.021** | 0.110*** | 0.095*** | 0.028*** | 0.131*** | 0.153*** | 0.148*** | ||
| 14. Male | 0.098*** | 0.112*** | 0.154*** | 0.068*** | 0.034*** | 0.184*** | − 0.056*** | − 0.100*** | − 0.033*** | − 0.155*** | − 0.053*** | − 0.045*** | − 0.025*** | |
| 15. Age | − 0.226*** | − 0.020** | − 0.138*** | 0.001 | 0.043*** | 0.283*** | 0.258*** | 0.165*** | 0.054*** | 0.375*** | − 0.083*** | 0.015 | 0.048*** | − 0.019* |
***p < 0.001, **p < 0.01, *p < 0.05, +p < 0.1
Multivariate analysis
Tables 3 and 4 summarise the results of the regression models of the effect of PA on SPH. In each model estimated we added one group of independent variables to see if the relationship between our interest variables was robust. In the last model, the interactions between PA and age groups also were included.
Table 3.
Models estimating the determinants of self-perceived health (EQ5D5L)
| Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total PA | 0.279*** | 0.019 | 0.266*** | 0.019 | 0.182*** | 0.017 | 0.178*** | 0.017 | 0.187*** | 0.017 | 0.148*** | 0.035 |
| Underweight BMI | 0.290 | 0.771 | − 0.303 | 0.678 | − 0.220 | 0.679 | − 0.998 | 0.755 | − 1.063 | 0.753 | ||
| Normal BMI (ref.) | ||||||||||||
| Overweight BMI | − 1.259*** | 0.254 | 0.180 | 0.225 | 0.069 | 0.231 | 0.416+ | 0.238 | 0.414+ | 0.237 | ||
| Obese BMI | − 5.336*** | 0.330 | − 1.487*** | 0.297 | − 1.588*** | 0.301 | − 1.148*** | 0.307 | − 1.095*** | 0.306 | ||
| Skeletal-muscular | − 3.345*** | 0.240 | − 3.348*** | 0.240 | − 3.104*** | 0.243 | − 3.075*** | 0.242 | ||||
| Metabolic | − 8.431*** | 0.380 | − 8.390*** | 0.380 | − 8.232*** | 0.382 | − 8.081*** | 0.381 | ||||
| Emotional | − 8.937*** | 1.334 | − 8.940*** | 1.334 | − 9.231*** | 1.336 | − 9.030*** | 1.333 | ||||
| Cardiovascular-respiratory | − 4.156*** | 0.126 | − 4.114*** | 0.128 | − 3.791*** | 0.133 | − 3.760*** | 0.133 | ||||
| Emergency services | − 2.090*** | 0.240 | − 2.079*** | 0.240 | − 2.452*** | 0.246 | − 2.435*** | 0.246 | ||||
| Hospitalised | − 3.453*** | 0.396 | − 3.438*** | 0.396 | − 3.444*** | 0.399 | − 3.506*** | 0.398 | ||||
| Day hospital | − 4.027*** | 0.393 | − 4.032*** | 0.393 | − 4.020*** | 0.397 | − 3.974*** | 0.396 | ||||
| Male | 0.452* | 0.211 | 0.444* | 0.215 | 0.470* | 0.214 | ||||||
| Age 18–29 | 1.133*** | 0.345 | 1.958*** | 0.493 | ||||||||
| Age 30–39 | 0.752* | 0.298 | 1.331*** | 0.419 | ||||||||
| Age 40–49 (ref.) | ||||||||||||
| Age 50–59 | − 1.692*** | 0.309 | − 2.553*** | 0.436 | ||||||||
| Age 60–69 | − 1.462*** | 0.331 | − 3.500*** | 0.472 | ||||||||
| Total PA * 18–29 | − 0.115* | 0.055 | ||||||||||
| Total PA * 30–39 | − 0.090+ | 0.049 | ||||||||||
| Total PA * 40–49 (ref.) | ||||||||||||
| Total PA * 50–59 | 0.139** | 0.052 | ||||||||||
| Total PA * 60–69 | 0.321*** | 0.055 | ||||||||||
| Constant | 92.280*** | 0.1677 | 93.816*** | 0.206 | 98.083*** | 0.198 | 97.905*** | 0.215 | 97.762*** | 0.281 | 97.943*** | 0.334 |
| R 2 | 1.41% | 3.02% | 25.15% | 25.17% | 25.84% | 26.24% | ||||||
***p < 0.001, **p < 0.01, *p < 0.05, +p < 0.1
Table 4.
Models estimating the determinants of self-perceived health (EQ5D5L)
| Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | Β-coef | SE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vigorous PA | 0.470*** | 0.054 | 0.433*** | 0.052 | 0.165*** | 0.046 | 0.149*** | 0.047 | 0.103* | 0.048 | 0.090 | 0.099 |
| Moderate PA | 0.130**** | 0.043 | 0.124** | 0.042 | 0.085* | 0.037 | 0.082* | 0.037 | 0.090* | 0.037 | 0.074 | 0.077 |
| Walking PA | 0.310**** | 0.028 | 0.287*** | 0.027 | 0.238*** | 0.024 | 0.237*** | 0.024 | 0.264*** | 0.024 | 0.204*** | 0.050 |
| Underweight BMI | 0.276 | 0.771 | − 0.289 | 0.678 | − 0.196 | 0.679 | − 0.986 | 0.754 | − 1.049 | 0.753 | ||
| Normal BMI (ref.) | ||||||||||||
| Overweight BMI | − 1.233*** | 0.254 | 0.183 | 0.225 | 0.059 | 0.231 | 0.410+ | 0.238 | 0.405+ | 0.237 | ||
| Obese BMI | − 5.292*** | 0.330 | − 1.492*** | 0.297 | − 1.604*** | 0.301 | − 1.163*** | 0.306 | − 1.094*** | 0.306 | ||
| Skeletal-muscular | − 3.351*** | 0.240 | − 3.356*** | 0.240 | − 3.108*** | 0.243 | − 3.071*** | 0.242 | ||||
| Metabolic | − 8.425*** | 0.380 | − 8.380*** | 0.380 | − 8.212*** | 0.381 | − 8.066*** | 0.381 | ||||
| Emotional | − 8.911*** | 1.333 | − 8.910*** | 1.333 | − 9.200*** | 1.336 | − 8.970*** | 1.333 | ||||
| Cardiovascular-respiratory | − 4.157*** | 0.126 | − 4.113*** | 0.128 | − 3.785*** | 0.133 | − 3.758*** | 0.133 | ||||
| Emergency services | − 2.088*** | 0.240 | − 2.074*** | 0.240 | − 2.452*** | 0.246 | − 2.440*** | 0.246 | ||||
| Hospitalised | − 3.458*** | 0.396 | − 3.442*** | 0.396 | − 3.449*** | 0.399 | − 3.489*** | 0.398 | ||||
| Day hospital | − 4.060*** | 0.393 | − 4.067*** | 0.393 | − 4.063*** | 0.397 | − 4.016*** | 0.396 | ||||
| Male | 0.497* | 0.213 | 0.518* | 0.216 | 0.510** | 0.216 | ||||||
| Age 18–29 | 1.186*** | 0.345 | 2.018*** | 0.501 | ||||||||
| Age 30–39 | 0.777** | 0.298 | 1.370*** | 0.426 | ||||||||
| Age 40–49 (ref.) | ||||||||||||
| Age 50–59 | − 1.716*** | 0.309 | − 2.736*** | 0.448 | ||||||||
| Age 60–69 | − 1.528*** | 0.331 | − 3.709*** | 0.487 | ||||||||
| Vigorous PA* 18–29 | − 0.094 | 0.141 | ||||||||||
| Vigorous PA * 30–39 | − 0.006 | 0.133 | ||||||||||
| Vigorous PA * 40-49 (ref.) | ||||||||||||
| Vigorous PA * 50–59 | 0.146 | 0.152 | ||||||||||
| Vigorous PA * 60–69 | 0.187 | 0.177 | ||||||||||
| Moderate PA * 18–29 | − 0.072 | 0.127 | ||||||||||
| Moderate PA * 30–39 | − 0.109 | 0.109 | ||||||||||
| Moderate PA * 40-49 (ref.) | ||||||||||||
| Moderate PA * 50–59 | − 0.005 | 0.111 | ||||||||||
| Moderate PA * 60–69 | 0.253* | 0.114 | ||||||||||
| Walking PA * 18–29 | − 0.142+ | 0.081 | ||||||||||
| Walking PA * 30–39 | − 0.110 | 0.070 | ||||||||||
| Walking PA * 40–49 (ref.) | ||||||||||||
| Walking PA * 50–59 | 0.219** | 0.074 | ||||||||||
| Walking PA * 60–69 | 0.385*** | 0.077 | ||||||||||
| Constant | 92.237*** | 0.172 | 93.759*** | 0.209 | 97.985*** | 0.200 | 97.785*** | 0.218 | 97.594*** | 0.283 | 97.830*** | 0.340 |
| R 2 | 1.55% | 3.14% | 25.20% | 25.23% | 25.94% | 26.33% | ||||||
***p < 0.001, **p < 0.01, *p < 0.05, +p < 0.1
From Table 3, we can conclude that the amount of PA undertaken is, in general, positively associated with SPH and that there is a moderating effect of age in this relationship. In particular, the first hypothesis is confirmed: individuals doing PA show better SPH. This result is consistent among all of the models’ estimates for total PA. The results of the test to determine if age group moderates the relationship between PA and SPH are presented in Table 3, in which the last model shows that although the level of SPH decreases with increasing age, the relationship between PA and SPH becomes stronger with increasing age.
As shown in Fig. 2, people aged 50–69 involved in PA had higher probabilities of having a better SPH compared with individuals age 40–49 involved in PA. Total PA in young people (18–29 years) had a weaker association with SPH. With low and medium values of PA, the younger age group had the best SPH; with higher levels of PA, the older age group had the best SPH. Among middle-aged and older individuals, the positive relationship between SPH and PA is statistically significant compared with the other age groups. In summary, Fig. 2 shows that SPH increases with PA for all age groups, while the association is stronger as the age group is older.
Fig. 2.
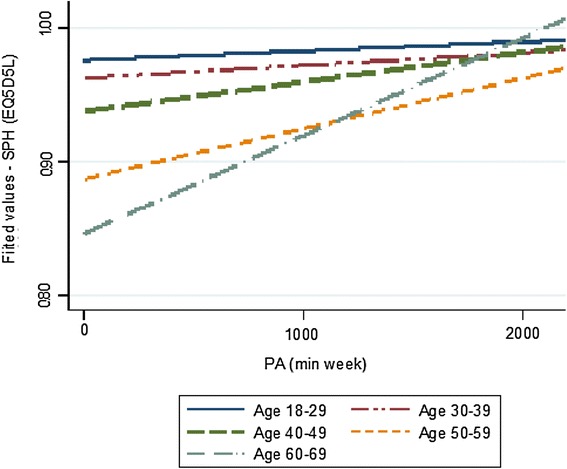
Effects of total physical activity on self-perceived health. Differences by age group. (Estimation by ordinary least squares method)
When we consider the intensity of PA separately (Table 4), some significant results can be highlighted. In the first model estimate, all of the PA intensities are positively related with SPH, although there are differences in terms of statistical significance. Nevertheless, when interactions between age and PA intensity are included (see the last model in Table 4), only walking activity has a positive association with SPH. Moreover, walking seems to have a stronger positive relationship with SPH among people aged 50–69 compared with people aged 40–49. Additionally, practicing moderate PA for those aged 60–69 also has a positive association with SPH compared with the age group of reference.
Figure 3 shows the association of vigorous PA with SPH for all groups and that this relationship is stronger in older age groups. The relationship of vigorous PA with SPH is the strongest for the group aged 60–69, while it is the weakest for the group aged 18–29.
Fig. 3.
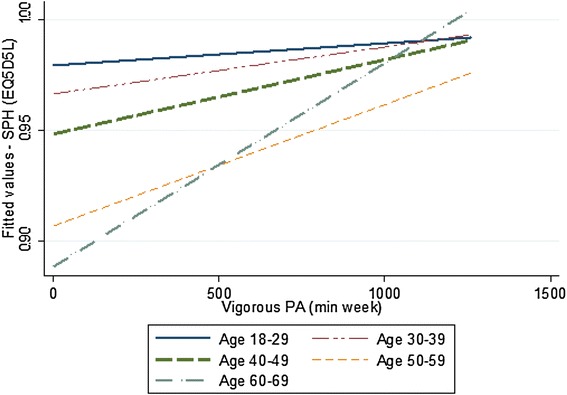
Effects of vigorous physical activity on self-perceived health. Differences by age group. (Estimation by ordinary least squares method)
Regarding the association of moderate PA with SPH, Fig. 4 shows that the relationship is weak for people aged 18–29 and 30–39. This association is a bit stronger for people aged 40–49 and 50–59. The association of moderate PA with SPH is very strong for people aged 60–69. This illustrates that moderate PA has a positive association with SPH and that age moderates this relationship because the effect is greater among the older age group.
Fig. 4.
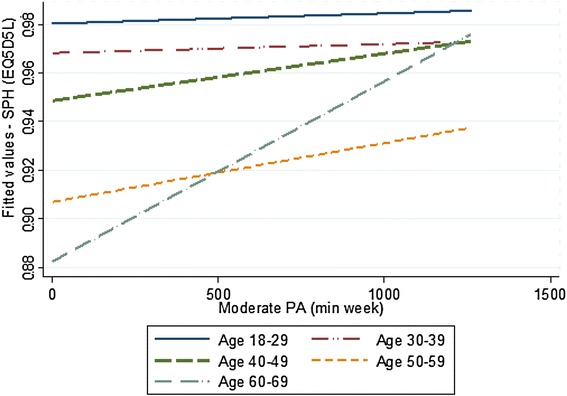
Effects of moderate physical activity on self-perceived health. Differences by age group. (Estimation by ordinary least squares method)
For walking PA, Fig. 5 shows that the association with SPH is weakest for people aged 18–29, while it was strongest for people aged 60–69.
Fig. 5.
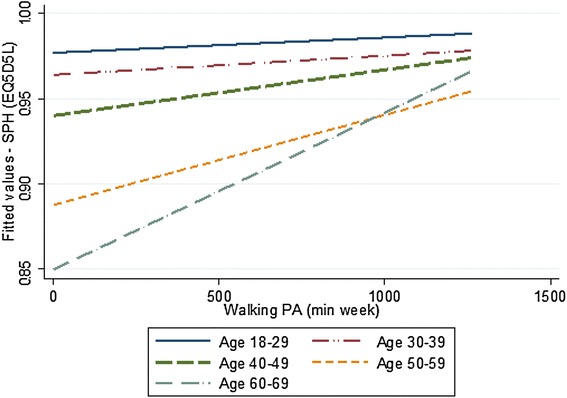
Effects of walking physical activity on self-perceived health. Differences by age group. (Estimation by ordinary least squares method)
Our models are in line with empirical literature about the relationship between PA and SPH. All the previous empirical evidence has demonstrated linear relationships between PA and SPH (Brown et al. 2004; Cimarras-Otal et al. 2014; Cohen et al. 2016). However, we have done additional analyses, in order to test if the effect of PA on SPH was different by gender and also to test if there was a quadratic relationship. Our results showed that gender did not moderate the relationship between PA and SPH (data available upon request).
Discussion and conclusions
The purpose of this article was to shed further light on the link between PA and SPH. Although this relationship has been fairly well established in the literature in recent years, no study has investigated whether the magnitude of this relationship is age specific. Consequently, we wished to test for moderating effects by assessing the extent to which the relationship between PA and SPH is moderated by age. In addition, we considered different types of PA according to intensity, making a distinction between vigorous activity, moderate activity and walking activity, following the guidelines established by the IPAQ and comparable to the recommendations of PA for health made by the WHO. We have included different types of diseases and the use of healthcare services as control variables because these are not personal decisions. On the contrary, personal decisions about engaging in PA might be positively associated with improved SPH.
For the Spanish population aged 18–69, we have shown that PA generally is associated with higher levels of SPH, which is in accordance with previous studies (e.g. Brown et al. 2004; Cohen et al. 2016), and that this positive relationship is moderated by age. In fact, the role played by PA is not homogeneous across all of the age groups under study. Specifically, we observed that only in people aged 50–69 does practicing PA seem to have a stronger positive relationship with the level of SPH, and we observed a weaker relationship in younger ages when compared with people age 40–49 years practicing PA. A potential explanation for the lack of a relationship between PA and SPH for people younger than 40 is that the SPH for these people is generally high, as shown in Table 1 and as has been observed in other studies (Brown et al. 2004; Cohen et al. 2016). Although PA might have positive effects on their health, it does not have a close association to the self-perception of their health status. Also, we could speculate that for this group PA is more associated with emotion, social contacts or pleasure motivations (Brunet and Sabiston 2011). At the same time, among people aged 50–69, PA might be more closely associated with SPH.
We also found that the relationship between PA and SPH varies depending on the intensity with which the PA is undertaken. In particular, we found that PA undertaken in the form of walking had a stronger association with SPH than vigorous and moderate PA, partially confirming the evidence shown by Wicker and Frick (2015). Finally, the role played by age as a moderating variable depended on the intensity of the PA. In particular, PA only had a positive and statistically significant relationship with SPH among people aged 50–69 who engaged in walking and among people aged 60–69 who practiced moderate PA. For the youngest group, compared with people aged 40 and over, the relationship between PA and SPH is significantly weaker, particularly when considering walking. This result might suggest that walking does not improve SPH in all stages of lifespan.
The empirical evidence presented in this study could be helpful in the design of public actions and programmes promoting PA and contributing to a healthier active ageing, although it should be highlighted that more evidence is needed to determine the best policy recommendations. In this respect, it is vital to engage in a debate on possible ways to promote a wider understanding of the relationship between PA and SPH. The results indicate that different strategies should be used to improve SPH through the practice of PA, according to age. Awareness of PA should be emphasised through communication strategies in different domains of an individual’s life in order to promote PA to people older than age 49. Misener and Misener (2016) suggested in a case study at a local level in Canada that cross-sector partnership between different agencies and institutions (e.g. health agencies, firms and social organisation, and non-profit sport organisations) should be encouraged. For example, in terms of the PA conducted at work, firms should create specific measures to increase the level of PA among their workers older than 49, such as using the stairs instead of the elevator, encouraging the sedentary to walk for a few minutes, promoting PA at work and stimulating PA in leisure time. In addition, regional and local authorities might encourage active transportation (i.e. going from one place to another) that avoids the use of cars or public transport. The provision of infrastructure, such as parks and green areas, where the population can easily and comfortably do moderate PA and walking might be recommended.
As Weed (2016) stated, it is necessary to support the promotion of different ways of being physically active, other than sports, to improve physical health. Social institutions and health departments also should emphasise the positive relationship between PA, particularly walking, and SPH, especially for people age 50 and older.
According to the results of this study, for people younger than 40, strategies for promoting PA that emphasise the traditional association between health and PA might have limited results. In these cases, the aim of the campaigns should be different, perhaps emphasising the opportunities in practising PAs for making contact with other people, particularly for PAs developed in leisure time, as has been shown by other studies (Downward and Riordan 2007).
In terms of PA intensity, other implications might be highlighted. First, in terms of health promotion, it generally has been accepted that SPH will be better when the intensity of PA is higher (Meyer et al. 2005; Vuillemin et al. 2005; Casado-Pérez et al. 2015). In the context of this study, however, these statements should be interpreted carefully when we consider the general population and PA as a whole, without making distinctions among domains. Our results show that walking and moderate PA is strongly associated with SPH. Second, this relationship is also moderated by age, and consequently, additional implications might be proposed. People older than 49 might be encouraged to do more moderate PA and walking. Any policy measures to boost PA in this way would contribute to the healthy ageing of the population because these practices are positively related to people’s perceived health.
Some limitations of this study should be mentioned. A first potential limitation is related to the use of self-report measures of health status and PA level. Although all of these measures have been validated in previous studies and countries, these variables might be susceptible to socially desirable responses. Another potential limitation is based on the nature of the data. The cross-sectional nature of the survey precludes us from drawing conclusive causal links among the key variables, and therefore, the causal relationships among them can only be hypothesised. Also, reversed causation might condition the comparisons between the age groups under study. In the future, more evidence is needed; using longitudinal study designs will enable researchers to be more decisive about causality between PA and SPH and the age-specific impact. Further research also should consider including other countries in the sample, to explore the potentially different effect of PA on SPH in different social and cultural contexts.
In summary, this article analyses the relationship between PA and SPH by considering the moderating effect of age in a cross-sectional study in Spain. The results show that the magnitude of this relationship depends on age and that it is stronger as age increases. In terms of PA intensities, the age differences in this relationship are greater when intensity decreases, from vigorous to walking PA.
Acknowledgements
Funding was provided by Ministerio de Educación, Cultura y Deporte (ECO2013-48496-C4-2-R, ECO2017-86305-C4-4-R) and Fundación Caja Navarra (2017).
Footnotes
Responsible editor: D. J. H. Deeg.
References
- Abu-Omar K, Rütten A. Relation of leisure time, occupational, domestic, and commuting physical activity to health indicators in Europe. Prev Med. 2008;47:319–323. doi: 10.1016/j.ypmed.2008.03.012. [DOI] [PubMed] [Google Scholar]
- Beard J, Biggs S, Bloom D, Fried L, Hogan P, Kalache R, Olshansky J (2012) Global population ageing: peril or promise? PGDA Working Paper, 1(89). Retrieved from http://www.hsph.harvard.edu/pgda/working/
- Bize R, Johnson JA, Plotnikoff RC. Physical activity level and health-related quality of life in the general adult population: a systematic review. Prev Med. 2007;45:401–415. doi: 10.1016/j.ypmed.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Brown DW, Brown DR, Heath GW, Balluz L, Giles WH, Ford ES, Mokdad AH. Associations between physical activity dose and health-related quality of life. Med Sci Sports Exerc. 2004;36:890–896. doi: 10.1249/01.MSS.0000126778.77049.76. [DOI] [PubMed] [Google Scholar]
- Brown DR, Carroll DD, Workman LM, Carlson SA, Brown DW. Physical activity and health-related quality of life: US adults with and without limitations. Qual Life Res. 2014;23:2673–2680. doi: 10.1007/s11136-014-0739-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet J, Sabiston CM. Exploring motivation for physical activity across the adult lifespan. Psychol Sport Exerc. 2011;12:99–105. doi: 10.1016/j.psychsport.2010.09.006. [DOI] [Google Scholar]
- Cabasés JM. The EQ-5D as a measure of health outcomes. Gac Sanit. 2015;29:401–403. doi: 10.1016/j.gaceta.2015.08.007. [DOI] [PubMed] [Google Scholar]
- Casado-Pérez C, Hernández-Barrera V, Jiménez-García R, Fernández-de-las-Peñas C, Carrasco-Garrido P, Palacios-Ceña D. Physical activity in adult working population: results from the European National Health Survey for Spain (2009) Aten Prim. 2015;47:563–572. doi: 10.1016/j.aprim.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P, Lin KC, Liing RJ, Wu CY, Chen CL, Chang KC. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual Life Res. 2016;25:1585–1596. doi: 10.1007/s11136-015-1196-z. [DOI] [PubMed] [Google Scholar]
- Cimarras-Otal C, Calderón-Larrañaga A, Poblador-Plou B, González-Rubio F, Gimeno-Feliu LA, Arjol-Serrano JL, Prados-Torres A. Association between physical activity, multimorbidity, self-rated health and functional limitation in the Spanish population. BMC Public Health. 2014;14:1170. doi: 10.1186/1471-2458-14-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A, Baker J, Ardern CI. Association between body mass index, physical activity, and health-related quality of life in Canadian adults. J Aging Phys Act. 2016;24:32–38. doi: 10.1123/japa.2014-0169. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjorstrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Crossley TF, Kennedy S. The reliability of self-assessed health status. J Health Econ. 2002;21:643–658. doi: 10.1016/S0167-6296(02)00007-3. [DOI] [PubMed] [Google Scholar]
- Devlin N, Buckingham K, Shah K, Tsuchiya A, Tilling C, Wilkinson G, van Hout B. A comparison of alternative variants of the lead and lag time TTO. J Health Econ. 2013;22:517–532. doi: 10.1002/hec.2819. [DOI] [PubMed] [Google Scholar]
- Downward P, Riordan J. Social interactions and the demand for sport: an economic analysis. Contemp Econ Policy. 2007;25:518–537. doi: 10.1111/j.1465-7287.2007.00071.x. [DOI] [Google Scholar]
- EuroQol Group EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Heesch KC, Van Uffelen JG, Van Gellecum YR, Brown WJ. Dose–response relationships between physical activity, walking and health-related quality of life in mid-age and older women. J Epidemiol Community Health. 2012;66:670–677. doi: 10.1136/jech-2011-200850. [DOI] [PubMed] [Google Scholar]
- Heller DA, Ahern FM, Pringle KE, Brown TV. Among older adults, the responsiveness of self-rated health to changes in Charlson comorbidity was moderated by age and baseline comorbidity. J Clin Epidemiol. 2009;62:177–187. doi: 10.1016/j.jclinepi.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández de Cos P, Moral-Benito E (2011) Eficiencia y regulación en el gasto sanitario en los países de la OCDE. Documentos ocasionales-Banco de España, nº 1107. (in Spanish)
- INE, Spanish National Institute of Statistics (2015) Spanish National Health Survey 2011–2012 (NHS). Retrieved from http://www.ine.es. Accessed 30 June 2015. (in Spanish)
- Judge GG, Hill RC, Griffiths W, Lutkepohl H, Lee TC. Introduction to the theory and practice of econometrics. 2. New York: Wiley; 1988. [Google Scholar]
- Larsen L, Biering K, Johnsen S, Andersen G, Hjollund N. Self-rated health and return to work after first-time stroke. J Rehabil Med. 2016;48:339–345. doi: 10.2340/16501977-2061. [DOI] [PubMed] [Google Scholar]
- Lera-López F, Garrues-Irisarri MA, Suarez-Fernández MJ. The correlates of physical activity among the population aged 50–70 years. Retos. 2017;31:181–187. [Google Scholar]
- Luo N, Li M, Chevalier J, Lloyd A, Herdman M. A comparison of the scaling properties of the English, Spanish, French, and Chinese EQ-5D descriptive systems. Qual Life Res. 2013;22:2237–2243. doi: 10.1007/s11136-012-0342-0. [DOI] [PubMed] [Google Scholar]
- Meyer K, Rezny L, Breuer C, Lamprecht M, Stamm HP. Physical activity of adults aged 50 years and older in Switzerland. Sozial-und Prävent. 2005;50:218–229. doi: 10.1007/s00038-005-4093-3. [DOI] [PubMed] [Google Scholar]
- Ministry of Health, Social Services and Equality (2014) National Health Survey, Spain 2011/12. Calidad de vida relacionada con la salud en adultos: EQ-5-5L D. Serie Informes monográficos nº 3. Ministry of Health, Social Services and Equality, Madrid. (in Spanish)
- Misener L, Misener KE. Examining the integration of sport and health promotion: partnership or paradox? Int. J Sport Policy Polit. 2016;8:695–712. doi: 10.1080/19406940.2016.1220405. [DOI] [Google Scholar]
- Mudrak J, Stochl J, Slepicka P, Elavsky S. Physical activity, self-efficacy, and quality of life in older Czech adults. Eur J Ageing. 2016;13:5–14. doi: 10.1007/s10433-015-0352-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan CM, Longworth L, Lord J, Canavan JL, Jones SE, Man WD. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71:493–500. doi: 10.1136/thoraxjnl-2015-207782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin R, Charro F. EQ-SD: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Ramos-Goñi JM, Pinto-Prades JL, Oppe M, Cabasés JM, Serrano-Aguilar P, Rivero-Arias O. Valuation and modeling of EQ-5D-5L health states using a hybrid approach. Med Care. 2017;55:e51–e58. doi: 10.1097/MLR.0000000000000283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Goñi JM, Craig BM, Oppe M, Ramallo-FariñaU Pinto-Prades JL, Luo N, Rivero-Arias O. Handling data quality issues to estimate the Spanish EQ-5D-5L value set using a hybrid interval regression approach. Value Health. 2017 doi: 10.1016/j.jval.2017.10.023. [DOI] [PubMed] [Google Scholar]
- Román Viñas B, Ribas Barba L, Ngo J, Serra Majem L. Validity of the international physical activity questionnaire in the Catalan population (Spain) Gac Sanit. 2013;27:254–257. doi: 10.1016/j.gaceta.2012.05.013. [DOI] [PubMed] [Google Scholar]
- Simon J, De Boer J, Joung I, Bosma H, Mackenbach J. How is your health in general? A qualitative study on self-assessed health. Eur J Public Health. 2005;15:200–208. doi: 10.1093/eurpub/cki102. [DOI] [PubMed] [Google Scholar]
- StataCorp LLC (2017). Data analysis and statistical software 14. https://www.stata.com/stata14/. Accessed 22 Nov 2017
- Szende A, Janssen B, Cabasés JM. Self-reported population health: an international perspective based on EQ-5D. London: Springer; 2014. [PubMed] [Google Scholar]
- Vagetti GC, Filho VCB, Moreira NB, de Oliveira V, Mazzardo O, de Campos W. The association between physical activity and quality of life domains among older women. J Aging Phys Act. 2015;23:524–533. doi: 10.1123/japa.2013-0070. [DOI] [PubMed] [Google Scholar]
- Vuillemin A, Boini S, Bertrais S, Tessier S, Oppert J, Hercberg S, Gullimin F, Briancon S. Leisure time physical activity and health-related quality of life. Prev Med. 2005;41:562–569. doi: 10.1016/j.ypmed.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Waller G, Janlert U, Hamberg K, Forssén A. What does age-comparative self-rated health measure? A cross-sectional study from the Northern Sweden MONICA Project. Scand J Public Health. 2015;44:233–239. doi: 10.1177/1403494815618554. [DOI] [PubMed] [Google Scholar]
- Weed M. Should we privilege sport for health? The comparative effectiveness of UK Government investment in sport as a public health intervention. Int J Sport Policy Polit. 2016;8:559–576. doi: 10.1080/19406940.2016.1235600. [DOI] [Google Scholar]
- Wicker P, Frick B. The relationship between intensity and duration of physical activity and subjective well-being. Eur J Public Health. 2015;25:868–872. doi: 10.1093/eurpub/ckv131. [DOI] [PubMed] [Google Scholar]
- WHO, World Health Organization . Global recommendations on physical activity for health. Geneva: WHO; 2010. [PubMed] [Google Scholar]


