Abstract
Cancer has become the number one killer. The most difficult part of cancer treatment is the treatment of metastasis, particularly the peritoneal metastasis, generally referred to as peritoneal carcinomatosis (PC). Internationally, the integrated treatment strategy of cytoreductive surgery (CRS) plus hyperthermic intraperitoneal chemotherapy (HIPEC) has been developed to be the standard treatment for PC. Although the development in this field has been relatively slow, as a result of the hard work put in over the last 20 years, there has been outstanding progress and gratifying achievements in both the diagnosis and treatment of PC in China. Our center (Department of Peritoneal Cancer Surgery, Beijing Shijitan Hospital, Capital Medical University) focuses on the research in diagnostic methods for PC, CRS+HIPEC, and management of perioperative adverse events. Based on these, “Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal malignancies” is developed. Our center that is the pioneering center for this treatment in China has accumulated a wealth of experiences and achievements with more than 1000 cases of CRS+HIPEC. Additionally, our center establishes a nationwide professional training program to promote and standardize the practice of CRS+HIPEC gradually.
Keywords: Peritoneal carcinomatosis, History of research, Experiences and achievements, Professional training
As a developing country, China is striving to build a national health service with high quality, high efficiency, and Chinese characteristics. Currently, China’s nationwide health service system is divided into three management levels. The first level is the community-based medical facilities, the second level is the county-based or prefecture-based general hospitals, and the third level is the provincial or municipal comprehensive or specialty medical institutions. Such three-level medical service system forms a disease-grading pattern, so that differential health services are delivered according to the priority of the disease and the difficulty of treatment. Cancer has become the number one killer disease in China, and China has a three-level referral system for cancer treatment. The most difficult part of cancer treatment is the metastasis, particularly the peritoneal metastasis, generally referred to as peritoneal carcinomatosis (PC).
PC represents a group of malignancies that occur and/or develop on the surface of peritoneum, including both primary and secondary. The commonest primary peritoneal tumors are primary peritoneal carcinoma and peritoneal malignant mesothelioma. Peritoneal metastases are secondary to various tumors, such as gastrointestinal and gynecological tumors and are the typical examples of the latter [1]. For a long time, PC is generally regarded as a form of systemic and widespread metastasis and the terminal stage of disease that deserves only palliative care. Even if there is a surgical intervention, it is only for palliative reasons. Active treatment is not advocated.
With research into tumor biology and advances in cancer treatment technology, revolutionary changes have taken place in understanding PC, which is currently regarded as a kind of locoregional cancer progression, not a widespread terminal-stage cancer metastasis. Accordingly, an integrated treatment strategy of cytoreductive surgery (CRS) plus hyperthermic intraperitoneal chemotherapy (HIPEC) has been developed by pioneering oncologists, with proven efficacy and safety in selected PC patients.
PC remains one of the most difficult challenges for China’s anti-cancer campaign. Although the development in this field has been relatively slow, as a result of the hard work put in over the last 20 years, there have been outstanding progresses and gratifying achievements in both the diagnosis and treatment of PC. Gradually, standard CRS+HIPEC has been established and promoted in many cancer centers in China.
History of Research on Peritoneal Surface Oncology in China
In 2001, Chen et al. [2] performed radical gastrectomy and peritoneal lavage for 10 min with 400 ml of double distilled water at 43 °C on the patients with gastric cancer of stages II and IIIA. They found that the 5-year survival rate was 63.8% in the lavage group and 51.2% in the control group (P < 0.01), and the clinical efficacy was significant. In 2003, Liang et al. [3] treated and prevented advanced gastric cancer patients at stages III and IV with intraperitoneal chemotherapy of mitomycin C bound to activated carbon particles. They found that the 3-year and 5-year survival rate was improved by 43.1% and 30.1% respectively comparing with the control group (P < 0.01). In 2006, Zhu et al. [4] conducted a preventive and therapeutic study on intraoperative hyperthermic chemotherapy (IPHC) for advanced gastric cancer with cisplatin and mitomycin C. In the preventive group, the average survival was statistically longer comparing IPHC with surgery alone (43.4 ± 2.6 months vs. 41.8 ± 3.8 months, P < 0.05). Similarly, in the therapeutic group, the median survival of IPHC patients was significantly better than those in the surgery alone group (10 months vs. 5 months, P < 0.05). The Cox regression model revealed that IPHC procedure was an independent prognostic factor of advanced gastric cancer.
Since 2003, our center (Department of Peritoneal Cancer Surgery, Beijing Shijitan Hospital, Capital Medical University) has been focusing on the diagnosis and treatment of PC. The diagnostic system for PC consisted of serum tumor markers detection including carcino-embryonic antigen (CEA), cancer antigen 199 (CA199), and cancer antigen 125 (CA125) and medical imaging studies including contrast-enhanced multi-detector row computed tomography (MDCT) and three-dimensional reconstruction, oral gastrografin radiography [5–7]. These techniques could help diagnose clinical stage PC with acceptable sensitivity and specificity. In brief, CEA could help evaluate the extent of tumor invasion, CA199 could help evaluate the proliferative activity of tumor cells in ascites and primary tumor, and CA125 could help evaluate the ascites and peritoneal tumor burden. Preoperative CT-PCI score could be estimated by MDCT according to the typical imaging signs and lesion size, so as to determine the extent of PC. The oral gastrografin radiography of the whole digestive tract could be used to observe the intestinal peristalsis, distribution status, and the duration of the contrast medium to pass through the small intestine, so as to evaluate gastrointestinal motility, intestinal obstruction, and mesenteric contracture.
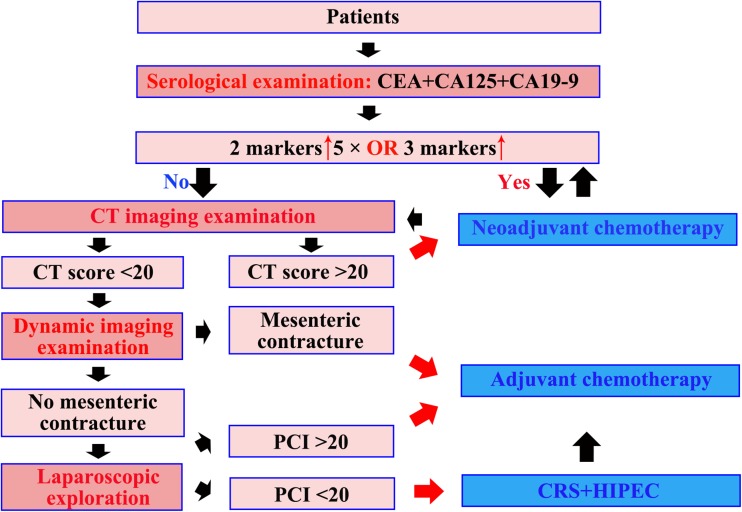
And clinical pathway has been built based on these diagnostic techniques (Fig. 1). The PC patients first receive the serological examination (CEA, CA125, CA199), CT imaging examination (contrast-enhanced MDCT and three-dimensional reconstruction), and dynamic imaging examination (oral gastrografin radiography). If CRS+HIPEC is feasible based on the three examinations, laparoscopic exploration is performed on the PC patients. Based on this clinical pathway, optimal treatments are chosen for the PC patients, so as to obtain max survival benefit and safety. There are four important risk criteria: (1) Any 2 of 3 tumor markers are more than 5 times higher than the normal, or all 3 tumor markers are higher than normal; (2) PCI score by CT > 20; (3) mesenteric contracture; and (4) PCI score in laparoscopic exploration > 20. Neoadjuvant chemotherapy is chosen, when the PC patients have the criterion (1) or (2), without (3) and (4). After every two-cycle neoadjuvant chemotherapy, the patients are re-evaluated by the clinical pathway. Palliative adjuvant chemotherapy is chosen, as long as the PC patients meet criterion (3), or meet (4) without (1), (2), and (3). Adjuvant chemotherapy is also delivered for all patients after CRS+HIPEC. CRS+HIPEC is chosen, when the PC patients have none of these four important risk criteria.
Fig. 1.
Clinical pathway for treatment of peritoneal carcinomatosis (PC) based on diagnosis systems
In the same time, the study of PC animal model [8, 9] is carried out, which illustrates the efficacy of HIPEC in prolonging PC survival.
In 2011, a phase III randomized clinical trial [10] was completed at our center to evaluate the efficacy and safety of CRS+HIPEC for the treatment of PC from gastric cancer. The median survival was 6.5 months (95% confidence interval, 4.8–8.2 months) for the CRS group, and 11.0 months (95% CI, 10.0–11.9 months) for the CRS+HIPEC group (P < 0.05). Moreover, the median survival of the patients with synchronous PC was statistically much better than the surgery alone group (12.0 months vs. 6.5 months, P < 0.05). And the multivariate analysis found that CRS+HIPEC and synchronous PC were major independent predictors for better survival. Therefore, the integrated diagnostic and treatment strategy of CRS+HIPEC for PC was developed based on the high-level consultation on medical evidence. In 2015, “Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal malignancies” [11] was developed with our center being the leading institution, and gradually promoted throughout the country. In 2017, an effective perioperative treatment system was summarized and standardized for management of adverse events after CRS+HIPEC. This was based on the results of a clinical study and includes clinical pathways for prevention of postoperative venous thromboembolism (VTE) [12, 13], the treatment for postoperative gastrointestinal fistula [14], and the treatment of postoperative hypermyoglobinemia [15]. In 2018, as the Beijing International Cooperation Center of Peritoneal Cancer Research and Treatment, under the Beijing Municipal Bureau of Science and Technology, our center performed the study of new surgical navigation technology based on fluorescence imaging in situ, cooperating with professor Yonemura from Japanese National Peritoneal Oncology to Support Peritoneal Surface Malignancy Treatment that opened the era of precision treatment for PC.
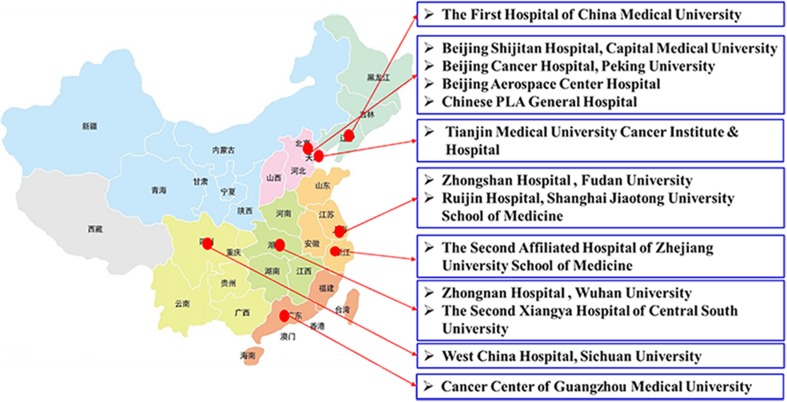
Chinese Centers of the Diagnosis and Treatment for PC
At present, there are 16 centers for the diagnosis and treatment for PC in China that are equipped to carry out standardized integrated diagnosis of PC and the treatment strategy of CRS+HIPEC. All these centers are distributed in first-level cities in the central and eastern regions (Fig. 2) of the country, including (1) Beijing Shijitan Hospital, Capital Medical University; (2) Beijing Aerospace Central Hospital; (3) Chinese PLA General Hospital; (4) Cancer Center of Guangzhou Medical University; (5) Zhongnan Hospital of Wuhan University; (6) Tianjin Medical University Cancer Institute and Hospital; (7) Zhongshan Hospital affiliated to Fudan University; (8) Ruijin Hospital affiliated to Shanghai Jiaotong University; (9) Beijing Cancer Hospital, Peking University; (10) The First Hospital of China Medical University; (11) Cancer Hospital of Chinese Academy of Medical Sciences; (12) Beijing Hospital affiliated to Ministry of National Health; (13) The Second Xiangya Hospital of Central South University; (14) Peking University People’s Hospital; (15) The Second Affiliated Hospital of Zhejiang University School of Medicine; and (16) West China Hospital, Sichuan University.
Fig. 2.
Geographical distribution of Chinese centers of the diagnosis and treatment for PC
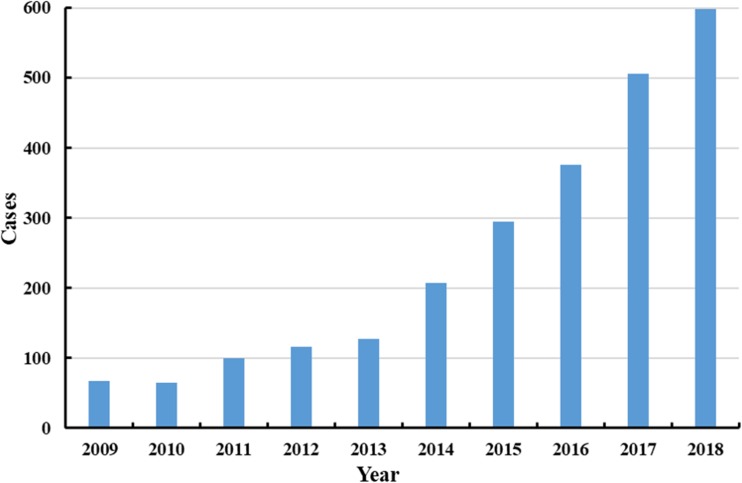
Over the past 10 years, with the continuous promotion of standardized integrated diagnostic and treatment strategy of CRS+HIPEC for PC, the annual operation volume of CRS+HIPEC in the main Chinese centers of the diagnosis and treatment for PC has been increasing considerably. In 2017, the annual operation volume was more than 500 cases, and almost 600 cases by the end of 2018 (Fig. 3).
Fig. 3.
The annual operation volume of the Chinese main centers of the diagnosis and treatment for PC in the past 10 years
Experience and Achievements of Beijing Shijitan Hospital, Capital Medical University
Our center (Beijing Shijitan Hospital, Capital Medical University) is the only professional center in China dedicated to the research, diagnosis, and treatment of PC in China. Our institution is also the Chinese Center recognized by the Peritoneal Surface Oncology Group International (PSOGI), the European Society of Surgical Oncology, and European School of Peritoneal Surface Oncology as a center of expertise in peritoneal surface oncology. At country level, our center is the Beijing Municipal Training Center of Cancer Hyperthermia Treatment (Beijing Municipal Commission of Health and Family Planning), Beijing Municipal Medical Talents Group on Peritoneal Surface Oncology (Beijing Committee of the Communist Party of China), and International Technology Cooperation Demonstration Center of Integrated Diagnosis and Treatment Strategy for PC (Beijing Municipal Science and Technology Commission).
Through effort of over 15 years, our center has established a demonstrational diagnosis and treatment technology system of PC and accumulates more than 1000 cases of CRS+HIPEC. The patient distribution is from all over the country, and even from Japan, Egypt, Vietnam, and Canada (Fig. 4).
Fig. 4.
Geographical distribution of patients at our center
As a comprehensive center of PC, patients with a series of pathological types come to our center for expert treatment. These patients include gastric cancer PC 147 cases (14.7%), colorectal cancer PC 211 cases (21.1%), pseudomyxoma peritonei (PMP) 225 cases (22.5%), ovarian cancer PC 144 cases (14.4%), malignant peritoneal mesothelioma (MPM) 53 cases (5.3%), primary peritoneal carcinomatosis 44 cases (4.4%), and retroperitoneal sarcoma (liposarcoma, leiomyosarcoma, synovial sarcoma) 68 cases (6.8%). A total of 38 pathological types are involved. Median peritoneal cancer index (PCI) is up to 21, and 52.6% of the patients have a PCI ≥ 20. There are 58.6% patients who have a complete cytoreduction (CC 0–1) (Table 1). Perioperative mortality rate is 1.5% within 30 days after CRS+HIPEC, and morbidity of serious adverse event (SAE, III-IV grade) is 12.4%. The main SAE includes anastomotic fistula, gastrointestinal fistula, biliary fistula, pancreatic fistula, intestinal obstruction, myelosuppression, acute renal insufficiency, ureteral fistula, hemorrhage, pleural effusion, pulmonary infection, acute cardiac insufficiency, abdominal infection, incision infection, SAE related central venous catheter, and VTE.
Table 1.
Clinical characteristics of 1000 PC patients treated at our center
| Characteristic | Value (%) |
|---|---|
| Age (year) | |
| Median (range) | 55 (10–87) |
| Gender | |
| Male/female | 392/608 |
| Primary disease | |
| Gastric cancer | 147 (14.7) |
| Colorectal cancer | 211 (21.1) |
| Pseudomyxoma peritonei | 225 (22.5) |
| Ovarian cancer | 144 (14.4) |
| Mesothelioma | 53 (5.3) |
| Primary peritoneal carcinomatosis | 44 (4.4) |
| Retroperitoneal sarcoma | 68 (6.8) |
| Others# | 108 (10.8) |
| PCI | |
| Median | 21 |
| < 20 | 474 (47.4) |
| ≥ 20 | 526 (52.6) |
| CC | |
| 0–1 | 586 (58.6) |
| 2–3 | 414 (41.4) |
#Liver cancer, endometrial cancer, breast cancer, lung cancer, and so on. PCI, peritoneal cancer index; CC, completeness of cytoreduction
According to the research on the learning curve internationally, our center has reached the technical proficiency of CRS+HIPEC, achieving better operative and oncologic outcomes with acceptable mortality and morbidity. The patients with PC have survival benefit without significantly increasing the economic pressure, because of the nationwide healthcare system. The government has established a comprehensive medical insurance system in China. Therefore, a patient with PC would cost about 25,000 dollars on the operation of CRS+HIPEC and the systems of care perioperatively, about 75% of which would be reimbursed from the medical insurance fund of Chinese government.
Professional Training System
As a first professional diagnosis and treatment center of PC, our center (Beijing Shijitan Hospital, Capital Medical University) is designated as the only “Beijing Municipal Training Center of Cancer Hyperthermia Treatment” by Beijing Municipal Commission of Health and Family Planning. Our nationwide training program covers both the theoretical study and clinical practice, including lectures of theory, case discussions, expert instruction, and hand-on surgery. Our center provides more learning opportunities for trainees by conducting several continuing education projects and helping them to attend academic conferences at home and abroad.
Admission Requirements for the Course
(1) The qualification certificate and practice license of medical practitioner; (2) above master degree in surgery and/or oncology; (3) resident doctor beyond 3 years or attending doctor beyond 1 year; (4) engaged in the specialty related to tumor hyperthermic technology.
Training Time
One year for comprehensive study type, 3 months for surgical technique improvement type, and 7 days for clinical experience type.
Training Content
For the comprehensive study type, the training program covers (1) theoretical study over 20 classes; (2) performing 100 CRS+HIPEC procedures consecutively for concentrated surgical skill training; (3) the diagnosis and treatment, overall management of more than 100 patients with PC treated by CRS+HIPEC, including writing medical records, preoperative evaluation, CRS+HIPEC procedure, perioperative management, adverse event management, follow-up, and so on; (4) construction and analysis of clinical research database; (5) writing monthly work summary reports for a total of 12 reports; (6) attending at least one national or international academic conference on peritoneal cancer; (7) Writing at least one research paper on peritoneal cancer treatment.
Training Appraisal
One week before the end of training, both theory knowledge examination and operation assessment are conducted under the supervision of the medical education center. The final training outcome is composed of the assessment examination results (90% of the total score) and the attendance rate (10% of the total score). A candidate is deemed qualified only if the examination score > 80, the certificate of completion shall be issued, and the training, examination, and assessment files would be established.
Looking into the Future
As two developing countries with the largest population, China and India share a lot in common in the field of clinical oncology, particularly in developing and promoting practical strategies to treat peritoneal carcinomatosis. China’s experiences of PC diagnosis and treatment have demonstrated the importance of professional training, and multicenter collaboration. In the future development, China should step up international co-operations, both with the developed and developing countries. We are willing and eager to share with and to learn from our Indian colleagues.
Funding Information
This study was supported by the Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20180701), Special Fund for the Capital Characteristic Clinical Medicine Development Project (Z161100000516077), Beijing Municipal Grant for Medical Talents Group on Peritoneal Surface Oncology (2017400003235J007), Key Discipline Development Fund of Beijing Shijitan Hospital affiliated to the Capital Medical University (2016fmzlwk), and Beijing Natural Science Foundation (7172108).
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li Y. My views on peritoneal carcinomatosis research. Chin J Clin Oncol. 2012;39(22):1685–1686. [Google Scholar]
- 2.Chen JQ, Wang SB, Xu HM, et al. Curative effect of radical gastrectomy combined with peritoneal lavage with thermal hypoosmotic solution in treatment of gastric cancer. Nat Med J China. 2001;81(12):730–732. [PubMed] [Google Scholar]
- 3.Liang H, Wang P, Wang XN, et al. Prospective randomized trial of prophylaxis of postoperative peritoneal carcinomatosis of advanced gastric cancer: intraperitoneal chemotherapy with mitomycin C bound to activated carbon particles. Chin J Surg. 2003;41(4):274–277. [PubMed] [Google Scholar]
- 4.Zhu ZG, Tang R, Yan M, et al. Clinical effect of intraoperative peritoneal hyperthermic chemotherapy for advanced gastric cancer. Chin J Gastrointes Surg. 2006;9(1):26–30. [PubMed] [Google Scholar]
- 5.Yang XQ, Li Y, Chen C, et al. Preoperative serum carbohydrate antigen 125 level is an independent negative prognostic marker for overall survival in colorectal cancer. Med Oncol. 2011;28(3):789–795. doi: 10.1007/s12032-010-9518-z. [DOI] [PubMed] [Google Scholar]
- 6.Mei LJ, Wang LW, Zhou YF, et al. Role of contrast-enhanced multi-detector row computed tomography and multiplanar reconstruction in diagnosing peritoneal carcinomatosis. Chin J Clin Oncol. 2012;39(22):1745–1749. [Google Scholar]
- 7.Mei LJ, Wang LW, Huang CQ, et al. Oral gastrografin radiography for the evaluation of the functional impact of peritoneal carcinomatosis: correlation with clinicopathological findings. Mol Clin Oncol. 2015;3(5):979–986. doi: 10.3892/mco.2015.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li PC, Chen LD, Zheng F, et al. Intraperitoneal chemotherapy with hydroxycamptothecin reduces peritoneal carcinomatosis: results of an experimental study. J Cancer Res Clin Oncol. 2008;134(1):37–44. doi: 10.1007/s00432-007-0242-9. [DOI] [PubMed] [Google Scholar]
- 9.Tang L, Mei LJ, Yang XJ, et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy improves survival of gastric cancer with peritoneal carcinomatosis: evidence from an experimental study. J Transl Med. 2011;9:53. doi: 10.1186/1479-5876-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang XJ, Huang CQ, Suo T, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol. 2011;18(6):1575–1581. doi: 10.1245/s10434-011-1631-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Zhou YF, Liang H, et al. Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal malignancies. World J Gastroenterol. 2016;22(30):6906–6916. doi: 10.3748/wjg.v22.i30.6906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peng KW, Zhang Q, Liu JY, et al. Venous thromboembolism prevention for peritoneal carcinomatosis patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Chin J Clin Oncol. 2017;44(8):384–389. [Google Scholar]
- 13.Liu G, Li XB, Ji ZH, et al. Diagnostic value of combined detection of D-dimer and thrombin time for exclusion of lower extremity deep vein thrombosis in patients with peritoneal carcinomatosis. Chin J Gen Surg. 2018;27(6):740–746. [Google Scholar]
- 14.Zhang YB, Ji ZH, Liu G, et al. A double-catheter washing and aspiration system for the treatment of gastrointestinocutaneous fistula after peritoneal cancer resection. Chin J Gen Surg. 2017;6(32):505–508. [Google Scholar]
- 15.Liu G, Ji ZH, Yu Y, et al. Treatment of hypermyoglobinemia after CRS + HIPEC for patients with peritoneal carcinomatosis: a retrospective comparative study. Medicine (Baltimore) 2017;96(45):e8573. doi: 10.1097/MD.0000000000008573. [DOI] [PMC free article] [PubMed] [Google Scholar]