Abstract
Objectives
This multicentre study aimed to investigate the overall mortality of combined pulmonary fibrosis and emphysema (CPFE) in systemic sclerosis (SSc) and to compare CPFE-SSc characteristics with those of other SSc subtypes (with interstitial lung disease—ILD, emphysema or neither).
Methods
Chest CTs, anamnestic data, immunological profile and pulmonary function tests of patients with SSc were retrospectively collected. Each chest CT underwent a semiquantitative assessment blindly performed by three radiologists. Patients were clustered in four groups: SSc-CPFE, SSc-ILD, SSc-emphysema and other-SSc (without ILD nor emphysema). The overall mortality of these groups was calculated by Kaplan-Meier method and compared with the stratified log-rank test; Kruskal-Wallis test, t-Student test and χ² test assessed the differences between groups. P<0.05 was considered statistically significant.
Results
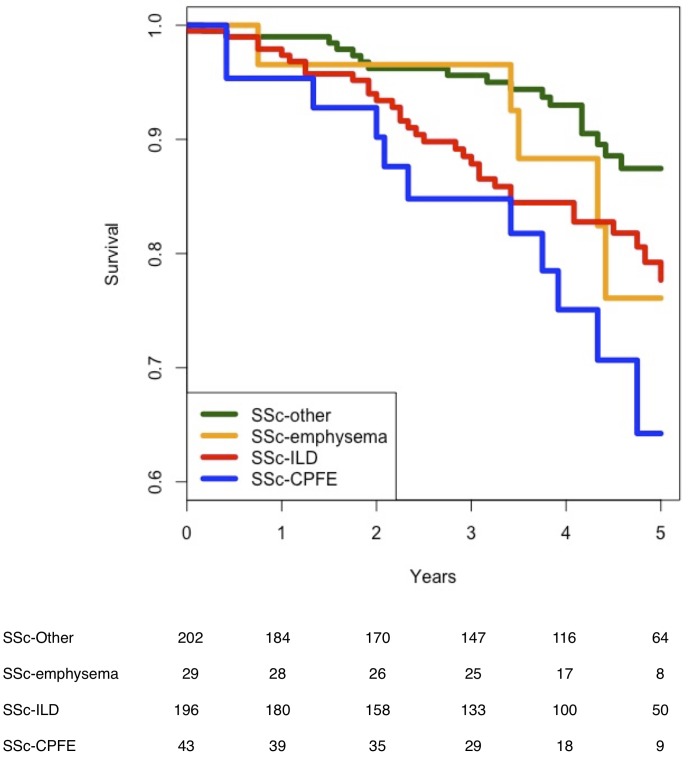
We enrolled 470 patients (1959 patient-year); 15.5 % (73/470) died during the follow-up. Compared with the SSc-ILD and other-SSc, in SSc-CPFE there was a higher prevalence of males, lower anticentromere antibodies prevalence and a more reduced pulmonary function (p<0.05). The Kaplan-Meier survival analysis demonstrates a significantly worse survival in patients with SSc-CPFE (HR vs SSc-ILD, vs SSc-emphysema and vs other-SSc, respectively 1.6 (CI 0.5 to 5.2), 1.6 (CI 0.7 to 3.8) and 2.8 (CI 1.2 to 6.6).
Conclusions
CPFE increases the mortality risk in SSc along with a highly impaired lung function. These findings strengthen the importance to take into account emphysema in patients with SSc with ILD.
Keywords: pulmonary fibrosis, combined pulmonary fibrosis and emphysema, systemic sclerosis, semiquantitative chest CT
Key messages.
What is already known about this subject?
Combined pulmonary fibrosis and emphysema (CPFE) was observed in short-survival IPF patients and in SSc subjects with a relevant decrease in FVC and a DLco.
What does this study add?
This is the first study describing a more reduced survival in SSc-CPFE compared with other SSc subgroups.
How might this impact on clinical practice?
CPFE is a radiological pattern that should always be considered in SSc chest CT assessment
CPFE detection can be useful in order to select patients with a more severe SSc.
Introduction
As interstitial lung disease (ILD) increases the mortality in systemic sclerosis (SSc),1 many studies are focusing on predictive factors of survival. Pulmonary function tests (forced vital capacity—FVC and diffusion lung capacity of CO—DLco) and semiquantitative assessment of ILD extension detectable in chest CT (sQCT), are the most important.2 In particular, FVC and DLco are quite diffused and they play a pivotal role in the diagnostic and therapeutic decision making process.
Combined pulmonary fibrosis and emphysema (CPFE) is a lung affection characterised by the presence of ILD and emphysema. CPFE was observed in short-survival IPF patients, even non-smokers.3 Other following studies supported the hypothesis that emphysema is an independent mortality risk factor in ILD.4
Cottin et al. reported 34 cases of CPFE in connective tissue disease for the first time.5 In the next years, some authors presented cases of SSc-ILD affected by severe emphysema.6 Recently, Antoniou et al described the characteristics of a cohort of SSc-CPFE.7 These patients had almost normal FVC and a DLco considerably decreased. These findings arise a discussion on the possible bias that FVC assessment and lack of pulmonary hypertension measurement could generate in this subgroup of SSc-ILD but were inconclusive about CPFE role in SSc.8 Especially, it remains not clear if CPFE is associated with a decreased survival in SSc.
The main aim of this study was to investigate the overall mortality of CPFE in patients with SSc. The secondary objective was to compare SSc-CPFE characteristics versus those of patients with SSc affected by ILD (SSc-ILD), emphysema (SSc-emphysema) or neither of them (other-SSc).
Methods
This study was conducted according to the Declaration of Helsinki. The Institutional Review Boards approved the study protocol; all patients provided informed consent.
Patients
Four-hundred and seventy (470) consecutive patients fulfilling the ACR/EULAR classification criteria9 for SSc were enrolled. Exclusion criteria were age <18 years and follow-up data available. The survival time was considered the time interval between the CT date and the death or the last clinic visit.
Pulmonary function tests
FVC and DLco performed within 6 months from CT were recorded. All centres performed PFTs according to the ATS/ERS standards.
sQCT assessments
Three thoracic radiologists scored the CT images as previously proposed.7 On the basis of the sQCT, four subgroups were identifies: (1) SSc-other (neither ILD nor emphysema); (2) SSc-emphysema (exclusive presence of emphysema); (3) SSc-ILD (exclusive presence of ILD); (4) CPFE (presence of ILD and emphysema).
Statistical analysis
Statistical analysis was performed using R (http://www.r-project.org, V.3.3.3). Kaplan-Meier survival analysis and log-rank test verified the difference between the four subgroups. The HR with 95% CI was calculated according to Klein & Moeschberger method. P<0.05 was considered statistically significant.
More information are in the online supplementary file 1.
rmdopen-2018-000820supp001.pdf (354.9KB, pdf)
Results
This study included 1959 patient-year with a median follow-up of 4.2 (CI 3.9 to 4.3) years; 15% of patients (72/470) died. Patients’ characteristics are listed in table 1.
Table 1.
Patients characteristics
| Total | Other-SSc | SSc-emphysema | SSc-ILD | SSc-CPFE | P value | |
| n (%) | 470 (100) | 202 (43) | 29 (6) | 196 (42) | 43 (9) | – |
| Age, mean (year) (95% CI) |
59.2 (57.2 to 60.5) |
59.3 (57.3 to 61.3) |
59.8 (54.8 to 64.9) |
59.4 (57.4 to 61.3) |
57.7 (53.3 to 62.1) |
nss |
| Sex (M:F) | 90:380 | 30:172 | 8:21 | 36:160 | 16:27 | (CPFE vs SSc-ILD)** (CPFE vs Other-SSc)*** |
| Disease duration, mean (year) (95% CI) | 8.2 (7.4 to 8.9) |
7.8 (6.6 to 9.0) |
8.4 (5.3 to 11.5) |
8.4 (7.4 to 9.5) |
8.6 (6.1 to 11) |
nss |
| Smoke habit‡ (none:former:current) | 351:57:52 | 165:17:19 | 17:5:6 | 146:28:18 | 25:7:9 | (CPFE vs Other-SSc)** (SSc-Emphysema vs Other-SSc)* |
| ACA prevalence (n) | 160 | 107 | 21 | 27 | 5 | (CPFE vs SSc-Other)§ (CPFE vs SSc-Emphysema)§ (SSc-ILD vs SSc-Emphysema)§ (SSc-Other vs SSc-Emphysema)* (Other-SSc vs SSc-ILD)§ |
| anti Scl70 prevalence (n) | 154 | 23 | 0 | 113 | 18 | (CPFE vs SSc-Emphysema)*** (CPFE vs Other-SSc)§ (SSc-ILD vs SSc-Emphysema)§ (SSc-ILD vs Other-SSc)§ |
| FVC-predicted, mean (95% CI) | 99% (97 to 102) |
109% (105 to 113) |
103% (92 to 114) |
91% (88 to 95) |
88% (80 to 95) |
(CPFE vs Other-SSc)† (CPFE vs SSc-Emphysema)** (Other-SSc vs SSc-ILD)† (SSc-ILD vs SSc-Emphysema)* |
| TLC-predicted, mean (95% CI) | 93% (90 to 95) |
99% (96 to 103) |
104% (93 to 116) |
85% (81 to 89) |
82% (76 to 88) |
(CPFE vs Other-SSc)† (CPFE vs SSc-Emphysema)† (SSc-ILD vs SSc-Emphysema)† (Other-SSc vs SSc-ILD)† |
| DLco-predicted, mean (95% CI) | 65% (63 to 67) |
73% (70 to 75) |
63% (55 to 65) |
61% (58 to 64) |
48% (42 to 55) |
(CPFE vs Other-SSc)† (CPFE vs SSc-ILD)† (CPFE vs SSc-Emphysema)** (SSc-Other vs SSc-Emphysema)* (Other-SSc vs SSc-ILD)*** |
| DLco/VA-predicted, mean (95% CI) | 82% (80 to 85) |
85% (81 to 88) |
83% (75 to 91) |
85% (81 to 89) |
59% (52 to 67) |
(CPFE vs SSc-ILD)† (CPFE vs Other-SSc)† (CPFE vs SSc-Emphysema)† |
| ILD extent >20%, n (%) | 95 (20) | 0 (0) | 0 (0) | 74 (38) | 21 (49) | (CPFE vs Other-SSc)§ (CPFE vs SSc-Emphysema)§ (SSc-ILD vs SSc-Emphysema)§ (Other-SSc vs SSc-ILD)§ |
| sQCT of ILD, median (95% CI) | 1% (0 to 3) |
0 | 0 | 15% (13 to 17) |
20% (18 to 26) |
(CPFE vs Other-SSc)† (CPFE vs SSc-ILD)** (CPFE vs SSc-Emphysema)† (SSc-ILD vs SSc-Emphysema)† (Other-SSc vs SSc-ILD)*** |
| sQCT of emphysema, median (95% CI) | 0 | 0 | 4% (2 to 10) |
0 | 4% (2 to 7) |
(CPFE vs SSc-ILD)† (CPFE vs Other-SSc)† (SSc-Emphysema vs SSc-ILD)† (SSc-Emphysema vs Other-SSc)† |
A graphical presentation of key findings is in the online supplementary file 1.
*<0.05; **<0.01; ***<0.001.
†<0.005.
‡Ten patients had an unknown smoke habit.
§<0.0001.
ACA, anticentromere antibodies; CPFE, combined pulmonary fibrosis and emphysema; DLco, diffusion lung capacity of CO; FVC, forced vital capacity; ILD, interstitial lung disease; IPF, Idiopathic pulmonary fibrosis; SSc, systemic sclerosis; TLC, Total lung capacity; VA, alveolar volume.
CPFE prevalence was 18% in patients with ILD and 7% in never smokers. Patients with CPFE had the highest male prevalence and the lowest DLco (p<0.05). CPFE and SSc-ILD had a similar autoimmune profile, which was different from patients with SSc-emphysema and other SSc (p<0.0005). In CPFE, there was a more relevant lung impairment (fibrosis extent and pulmonary function decrease) than in the other three subgroups (p<0.01). In SSc-emphysema, we observed the highest anticentromere antibodies prevalence (p<0.05) and a DLco decrease (similar to SSc-ILD, lower than in other-SSc and higher than in SSc-CPFE), while FVC was normal (higher than in SSc-CPFE and SSc-ILD). The extent of emphysema was similar in the SSc-CPFE and SSc-emphysema subgroups.
The Kaplan-Meier survival analysis demonstrated a worse survival in SSc-CPFE compared with other-SSc (p<0.01) and SSc-ILD or SSc-emphysema (p=0.1) (figure 1). The HR was, respectively, 2.8 (CI 1.2 to 6.6), 1.6 (CI 0.7 to 3.8) and 1.6 (IC 0.5–5.2).
Figure 1.
Survival in SSc-CPFE, SSc-ILD, SSc-emphysema and other-SSc. CPFE, combined pulmonary fibrosis and emphysema; ILD, interstitial lung disease; SSc, systemic sclerosis.
Discussion
This is the largest population of CPFE related to SSc ever described. Our observations about pulmonary function impairment, disease duration and smoke habit are similar to those of previous studies.5–7 We confirm that CPFE decreases gas exchange more than ILD or emphysema alone; on the other hand, pulmonary static volumes are little or not affected.
Lung impairment (ILD, emphysema or both of them) appears to be related to a higher risk of death and a decrease of pulmonary function. ILD is a predictor of mortality,1 while emphysema presence was never taken into account. The detection of emphysema in never smokers was so far neglected, yet we showed that it deserves clinical attention.
Our findings confirm previous hypothesis about the role of emphysema in patients with SSc with pulmonary fibrosis that namely it is a synergistic risk factor.5 So, emphysema combined with pulmonary fibrosis is a radiological pattern that should be considered in chest CT assessment. CPFE detection can be useful in order to select patients with an increased risk of mortality related to more severe SSc.
This study has the limitations of a retrospective design. In particular, there was not a control group of IPF-CPFE subjects, only two antibody patterns were recorded as far as the smoke habit duration (that is likely to have been a risk factor for emphysema onset). Moreover, the definition of CPFE is not clear. In the first studies, CPFE diagnosis was based on imaging features.5 We classified CPFE if sQCT of ILD and emphysema was ≧1%, as Antoniou et al proposed.7 However, this approach does not take into account the emphysema type, distribution and proximity to fibrotic lesions. Walsh et al 10 showed that traction bronchiectasis are strongly associated with mortality in ILD related to connective tissue disease. So it is impossible to exclude that emphysema-like lesions near to fibrosis are an expression of ILD severity.
In conclusion, CPFE increases the risk of mortality and it should always be sought in order to better outline the prognosis in patients with SSc.
Acknowledgments
We want to thank Antonio Michele Ghislieri for his valuable networking support.
Footnotes
Presented at: An abstract of this study was submitted to and accepted as oral presentation for the Congress of Italian Society of Rheumatology (Rimini, 27 November 2017).
Contributors: All authors approved the entirety of the submitted material and contributed actively to the study: all of them meet the journal's criteria for authorship.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Elhai M, Meune C, Boubaya M, et al. . Mapping and predicting mortality from systemic sclerosis. Ann Rheum Dis 2017;76:1897–905. 10.1136/annrheumdis-2017-211448 [DOI] [PubMed] [Google Scholar]
- 2. Moore OA, Goh N, Corte T, et al. . Extent of disease on high-resolution computed tomography lung is a predictor of decline and mortality in systemic sclerosis-related interstitial lung disease. Rheumatology 2013;52:155–60. 10.1093/rheumatology/kes289 [DOI] [PubMed] [Google Scholar]
- 3. Cottin V, Nunes H, Brillet PY, et al. . Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J 2005;26:586–93. 10.1183/09031936.05.00021005 [DOI] [PubMed] [Google Scholar]
- 4. Sugino K, Ishida F, Kikuchi N, et al. . Comparison of clinical characteristics and prognostic factors of combined pulmonary fibrosis and emphysema versus idiopathic pulmonary fibrosis alone. Respirology 2014;19:239–45. 10.1111/resp.12207 [DOI] [PubMed] [Google Scholar]
- 5. Cottin V, Nunes H, Mouthon L, et al. . Combined pulmonary fibrosis and emphysema syndrome in connective tissue disease. Arthritis Rheum 2011;63:295–304. 10.1002/art.30077 [DOI] [PubMed] [Google Scholar]
- 6. Tzouvelekis A, Zacharis G, Oikonomou A, et al. . Increased incidence of autoimmune markers in patients with combined pulmonary fibrosis and emphysema. BMC Pulm Med 2013;13 10.1186/1471-2466-13-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Antoniou KM, Margaritopoulos GA, Goh NS, et al. . Combined pulmonary fibrosis and emphysema in Scleroderma-Related lung disease has a major confounding effect on lung physiology and screening for pulmonary hypertension. Arthritis Rheumatol 2016;68:1004–12. 10.1002/art.39528 [DOI] [PubMed] [Google Scholar]
- 8. Saketkoo LA, Steen VD, Lammi MR. Reliance on pulmonary function tests in assessment of systemic sclerosis patients for pulmonary hypertension: Comment on the article by Antoniou et al. Arthritis Rheumatol 2017;69:239–40. 10.1002/art.39928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van den Hoogen F, Khanna D, Fransen J, et al. . 2013 classification criteria for systemic sclerosis: an American College of rheumatology/European League against rheumatism collaborative initiative. Ann Rheum Dis 2013;72:1747–55. 10.1136/annrheumdis-2013-204424 [DOI] [PubMed] [Google Scholar]
- 10. Walsh SL, Sverzellati N, Devaraj A, et al. . Connective tissue disease related fibrotic lung disease: high resolution computed tomographic and pulmonary function indices as prognostic determinants. Thorax 2014;69:216–22. 10.1136/thoraxjnl-2013-203843 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2018-000820supp001.pdf (354.9KB, pdf)