Significance
Loneliness (i.e., feeling alone) and social isolation (i.e., being alone) are among the most robust known risk factors for poor health and accelerated mortality. Yet mitigating these social risk factors is challenging, as few interventions have been effective for both reducing loneliness and increasing social contact. Mindfulness interventions, which train skills in monitoring present-moment experiences with an orientation of acceptance, have shown promise for improving social-relationship processes. This study demonstrates the efficacy of a 2-wk smartphone-based mindfulness training for reducing loneliness and increasing social contact in daily life. Importantly, this study shows that developing an orientation of acceptance toward present-moment experiences is a critical mechanism for mitigating these social risk factors.
Keywords: mindfulness, social relationships, loneliness, acceptance, ambulatory assessment
Abstract
Loneliness and social isolation are a growing public health concern, yet there are few evidence-based interventions for mitigating these social risk factors. Accumulating evidence suggests that mindfulness interventions can improve social-relationship processes. However, the active ingredients of mindfulness training underlying these improvements are unclear. Developing mindfulness-specific skills—namely, (i) monitoring present-moment experiences with (ii) an orientation of acceptance—may change the way people perceive and relate toward others. We predicted that developing openness and acceptance toward present experiences is critical for reducing loneliness and increasing social contact and that removing acceptance-skills training from a mindfulness intervention would eliminate these benefits. In this dismantling trial, 153 community adults were randomly assigned to a 14-lesson smartphone-based intervention: (i) training in both monitoring and acceptance (Monitor+Accept), (ii) training in monitoring only (Monitor Only), or (iii) active control training. For 3 d before and after the intervention, ambulatory assessments were used to measure loneliness and social contact in daily life. Consistent with predictions, Monitor+Accept training reduced daily-life loneliness by 22% (d = 0.44, P = 0.0001) and increased social contact by two more interactions each day (d = 0.47, P = 0.001) and one more person each day (d = 0.39, P = 0.004), compared with both Monitor Only and control trainings. These findings describe a behavioral therapeutic target for improving social-relationship functioning; by fostering equanimity with feelings of loneliness and social disconnect, acceptance-skills training may allow loneliness to dissipate and encourage greater engagement with others in daily life.
Feeling alone (i.e., loneliness) and being alone (i.e., lack of social ties) are among the most robust known risk factors for poor health and accelerated mortality (1–3). Furthermore, loneliness and social isolation are increasingly common, situating these social risk factors as a significant public health concern (1). From an evolutionary perspective, social isolation threatens survival; loneliness evolved to motivate social-connection behaviors, yet this threatened state also triggers negative social biases and antagonistic behaviors that reinforce loneliness and social isolation (4). Therefore, to effectively reduce social risk, both the subjective experience of loneliness as well as objective social-interaction behaviors must be addressed (1, 4). However, despite efforts to develop evidence-based interventions, few interventions have been effective for mitigating both loneliness and social isolation (5, 6). Mindfulness meditation interventions, which commonly train intrapersonal skills in monitoring present-moment experiences with an orientation of acceptance, have shown promise for improving a variety of interpersonal processes. Initial evidence shows that mindfulness interventions may reduce loneliness (7–9), improve communication and relationship satisfaction (10, 11), and foster compassion toward others (12–14). Although promising, no well-controlled studies have tested whether mindfulness interventions can reduce loneliness and increase social contact or evaluated the active ingredients of mindfulness interventions that drive social-relationship effects.
The present work aims to test the hypothesis that learning acceptance skills in mindfulness interventions is a central mechanism for combating loneliness and social isolation. We use “acceptance” as an umbrella term to encompass an attitude of receptivity, openness, and equanimity toward present-moment experiences. Although the study of experiential acceptance and equanimity is quite new (15), this orientation has been described as an emotion-regulation skill that may help foster more effective social functioning (16, 17). Specifically, acceptance-skills training offered in mindfulness interventions can help people learn to be equanimous with difficult feelings of loneliness or social disconnect, thereby reducing social threat and obstacles that hinder social engagement (e.g., distress, avoidance, negative biases, or social anxiety) (18, 19). Indeed, we demonstrated that acceptance training is a necessary component of mindfulness interventions for lowering biological reactivity to social evaluative threat (20), an effect that may extend to daily-life social behavior. Here, we tested the idea that acceptance-skills training is necessary for mitigating loneliness and social isolation in this same three-arm randomized controlled dismantling trial. In particular, the present analyses tested whether removing acceptance training from a mindfulness intervention would eliminate mindfulness-training improvements in loneliness and social-interaction behaviors.
A smartphone intervention and assessment approach was used to test this aim; implementing the study using mobile devices in everyday life provided several unique features. First, smartphone-based mindfulness interventions are scalable and widely used (21); this study tested the efficacy of a remote, individually delivered mindfulness intervention for improving social-relationship outcomes (also see ref. 14). Although the social context of many group-based mindfulness interventions may play a role, the smartphone format controlled for the influence of social factors (as well as other nonspecific treatment components using an active control intervention). Overall, this approach allowed us to isolate mindfulness-skill instruction to test how purported active components of mindfulness—attention monitoring and acceptance—impact loneliness and social isolation. Second, this study’s smartphone approach permitted us to test how mindfulness interventions impact social processes in daily life. Specifically, an ambulatory assessment approach was used to measure subjective perceptions of loneliness and objective social behaviors (numbers of social interactions and interaction partners) in participants’ natural environments. Ambulatory assessments can provide sensitive measures of how social processes unfold in daily life and are closely tied with health-relevant physiological processes (22–24). We additionally measured changes in loneliness, social isolation, and social support using retrospective global scales, as well as reactions to daily-life social interactions.
In this preregistered trial, community adults reporting above-average stress were randomly assigned to complete one of three structurally equivalent, 14-lesson, smartphone-based interventions: (i) training in both monitoring and acceptance (Monitor+Accept; MA), (ii) training in monitoring only (Monitor Only; MO), or (iii) active control training (Coping control), the latter of which controlled for positive treatment expectancies by providing guidance in free reflection, analytic thinking, and problem solving, and contained no explicit mindfulness content. For 3 d before and after the intervention, social processes (subjective perceptions of loneliness; objective number of social interactions and interaction partners) were assessed in daily life by using both Ecological Momentary Assessments (EMAs) and end-of-day diary measures. Global measures of loneliness, social isolation, and social support were also taken in the laboratory at preintervention and postintervention, and exploratory measures of reactions to social interactions were assessed in a subset of EMA data (SI Appendix). This report describes secondary outcome analyses to test the prediction that MA mindfulness training would decrease loneliness and increase social interactions in daily life compared with MO and control training programs.
Results
Preliminary Analyses.
First, success of randomization on major demographic characteristics in the full randomized sample (n = 153) was evaluated. There were no preexisting-condition differences on age, sex, race, ethnicity, or education (SI Appendix, Table S1). Second, there were no condition differences in intervention adherence, intervention dropouts, treatment expectancies, ambulatory-assessment compliance, or ambulatory-assessment counterbalance (SI Appendix, SI Text and Table S2). Participants in all conditions were highly adherent to the training programs (96% adherence) and ambulatory assessments (89% compliance). Finally, there were no baseline condition differences on any of the primary or exploratory outcomes (SI Appendix, Table S2).
Primary Analyses.
We predicted that MA training would decrease loneliness and increase social interactions in daily life compared with MO and control trainings, with no differences between MO and control. To evaluate these hypotheses, multilevel mixed-effect linear models (MLMs) focused on time × condition interactions in EMA-sampled and daily-diary-assessed loneliness and social isolation outcomes [using all available data and controlling for day of week (diary and EMA analyses) and time of assessment (EMA analyses)]. See SI Appendix for secondary analyses testing for time × condition differences on retrospective global measures of loneliness, social isolation, and social support [which are more susceptible to bias (25)] and exploratory analyses of reactions to social interactions (measured in a subset of EMA data).
Subjective perceptions of loneliness.
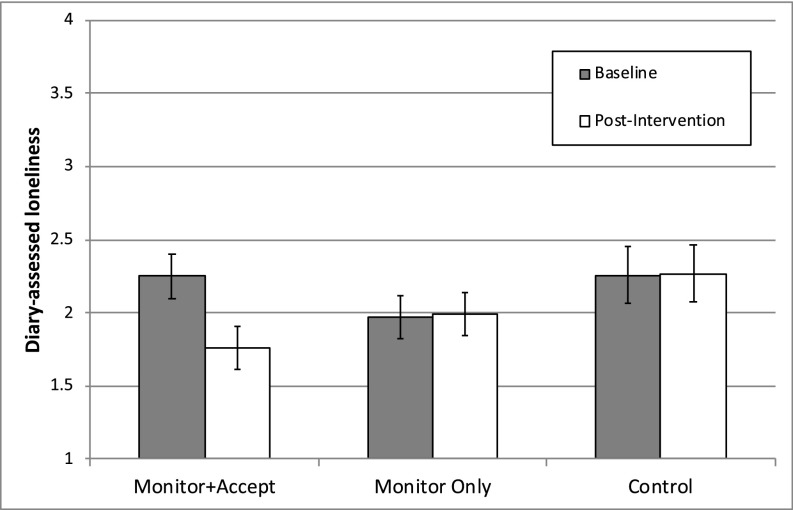
Diary MLM analyses supported the prediction that MA would reduce the subjective experience of loneliness compared with both MO and control trainings. There was a significant time × condition effect on diary ratings of loneliness [χ2(2) = 11.46, P = 0.003] (Fig. 1). Specifically, MA-trained participants showed significant decreases in loneliness from preintervention to postintervention (mean change = −0.49, P = 0.0001, d = 0.44); in contrast, MO and control participants did not change (MO mean change = 0.02, P = 0.837, d = −0.02; control mean change = 0.00, P = 0.981, d = −0.01) (Table 1). Consistent with predictions, MA-trained participants became significantly less lonely from preintervention to postintervention compared with MO-trained participants [B = 0.51, SE = 0.17; χ2(1) = 9.54, P = 0.002, d = 0.46] and control-trained participants [B = 0.49, SE = 0.19; χ2(1) = 6.83, P = 0.009, d = 0.45], whereas MO and control participants did not differ in pre–post loneliness change [B = −0.02, SE = 0.19; χ2(1) = 0.01, P = 0.912, d = −0.01] (SI Appendix, Table S4A).
Fig. 1.
Baseline and postintervention diary ratings of loneliness by condition. Error bars depict SEM.
Table 1.
EMA and end-of-day diary assessment of loneliness and social isolation in each condition
| Outcome | MA (n = 58) | MO (n = 58)* | Control (n = 37) | Time × condition difference | ||||||
| Pre | Post | d | Pre | Post | d | Pre | Post | d | ||
| Subjective perceptions of loneliness | ||||||||||
| Diary loneliness | 2.25 (0.15) | 1.76 (0.15) | 0.44† | 1.97 (0.15) | 1.99 (0.15) | −0.02 | 2.26 (0.19) | 2.27 (0.19) | −0.01 | χ2(2) = 11.46, P = 0.003 |
| Objective social isolation | ||||||||||
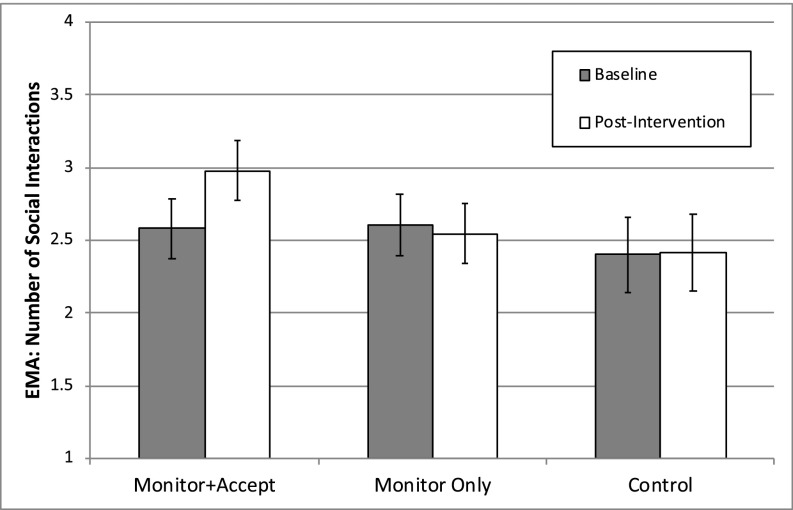
| EMA social interactions | 2.58 (0.21) | 2.98 (0.21) | 0.31† | 2.60 (0.21) | 2.55 (0.21) | −0.04 | 2.40 (0.26) | 2.42 (0.26) | 0.02 | χ2(2) = 8.36, P = 0.015 |
| Diary social interactions‡ | 9.06 (0.77) | 10.82 (0.77) | 0.47† | 10.19 (0.77) | 10.72 (0.77) | 0.13 | 10.55 (0.95) | 10.52 (0.96) | −0.05 | χ2(2) = 6.06, P = 0.048 |
| Diary interaction partners‡ | 6.92 (0.60) | 8.26 (0.60) | 0.39† | 7.79 (0.60) | 7.51 (0.60) | −0.04 | 8.84 (0.74) | 8.03 (0.75) | −0.15 | χ2(2) = 11.23, P = 0.004 |
Data are reported as means (SE) adjusted for day of week (EMA and diary) and time of day (EMA only). d = Cohen’s d effect size estimate.
*n = 57 in diary analyses.
P < 0.05.
Means calculated from estimated number of social interactions; time × condition differences and effect sizes calculated from raw data (Measures).
Objective social isolation: Social interactions.
EMA and diary MLM analyses supported the prediction that MA would decrease objective social isolation compared with MO and control trainings. First, EMA-based MLM analyses revealed a significant time × condition effect on the number of social interactions reported throughout the day [χ2(2) = 8.36, P = 0.015] (Fig. 2). MA-trained participants reported significantly more social interactions throughout the day from preintervention to postintervention (mean change = 0.40, P = 0.001, d = 0.31), whereas MO and control participants did not change (MO mean change = −0.06, P = 0.622, d = −0.04; control mean change = 0.02, P = 0.914, d = 0.02) (Table 1). As predicted, MA-trained participants reported significantly more social interactions from preintervention to postintervention compared with MO-trained participants [B = −0.46, SE = 0.17; χ2(1) = 7.51, P = 0.006, d = 0.35] and control-trained participants [B = −0.38, SE = 0.19; χ2(1) = 4.23, P = 0.040, d = 0.29], whereas MO and control participants did not differ in pre–post social interaction change [B = 0.07, SE = 0.19; χ2(1) = 0.16, P = 0.690, d = −0.02] (SI Appendix, Table S4B).
Fig. 2.
Baseline and postintervention social interaction frequency by condition, assessed via EMA. Error bars depict SEM.
Consistent with the number of social interactions reported throughout the day via EMA, end-of-day diary MLM analyses revealed a significant time × condition effect on total number of social interactions reported [χ2(2) = 8.70, P = 0.013]. Again, only MA-trained participants had a significant increase in their total number of social interactions (estimated mean change = 1.76 interactions, P = 0.001, d = 0.47); in contrast, MO and control participants did not significantly change (MO estimated mean change = 0.54, P = 0.269, d = 0.13; control estimated mean change = −0.03, P = 0.960, d = −0.05) (Table 1). MA-trained participants had a significantly higher number of social interactions at postintervention compared with preintervention than MO-trained participants [B = −0.27, SE = 0.13; χ2(1) = 4.13, P = 0.042, d = 0.34] and control-trained participants [B = −0.42, SE = 0.15; χ2(1) = 7.97, P = 0.005, d = 0.52] (SI Appendix, Table S4C). MO and control participants did not differ in pre–post social interaction change [B = −0.15, SE = 0.15; χ2(1) = 1.04, P = 0.307, d = 0.18].
Similarly, MLM analyses revealed a significant time × condition effect on total number of interaction partners reported in end-of-day diaries [χ2(2) = 11.47, P = 0.003]. Again, only MA participants had a significant increase in the total number of interaction partners (estimated mean change = 1.34 people, P = 0.004, d = 0.39), with no significant changes after MO and control training (MO estimated mean change = −0.28, P = 0.530, d = −0.04; control estimated mean change = −0.81, P = 0.142, d = −0.15) (Table 1). Supporting the primary hypothesis, MA-trained participants interacted with a significantly greater number of individuals from preintervention to postintervention compared with MO-trained participants [B = −0.34, SE = 0.13; χ2(1) = 7.12, P = 0.008, d = 0.43] and control-trained participants [B = −0.43, SE = 0.14; χ2(1) = 9.38, P = 0.002, d = 0.54]; as in previous analyses, MO and control participants did not differ [B = −0.10, SE = 0.14; χ2(1) = 0.49, P = 0.486, d = 0.11] (SI Appendix, Table S4C).
Discussion
Social connection is argued to be a basic psychological need (26, 27), and experiences of loneliness and social isolation are a growing public health concern (1). So far, few interventions are known to both mitigate loneliness and increase social ties (5, 6, 28); the most promising interventions targeting loneliness provide skills to address maladaptive thought patterns about social interactions (6), and the most promising interventions targeting social isolation provide opportunities for social contact (5, 28). Extending this literature, we show that a 2-wk smartphone-based mindfulness training (which provides intrapersonal skills but not social contact) both reduces loneliness and increases social interactions in daily life compared with an active control program. Specifically, participants trained in both attention-monitoring and acceptance, core elements of secular mindfulness training (29), reported having approximately two more interactions each day and interacting with one more person each day from preintervention to postintervention and experienced a 22% reduction in loneliness. The individually delivered smartphone trainings eliminated the influence of social factors common to standardized group-based mindfulness interventions, supporting the idea that mindfulness-specific monitoring and acceptance skills (rather than a supportive social context) are responsible for the observed effects. Thus, building from the interpersonal perspective that individuals’ social biases, emotions, and behaviors shape interpersonal cycles which impact health (30), this study demonstrates how mindfulness interventions train unique intrapersonal skills that foster more adaptive perceptions and behaviors in interpersonal contexts. By strengthening intrapersonal resources that influence interpersonal dynamics, mindfulness interventions hold promise for mitigating both subjective and objective social risk factors. More broadly, mindfulness skills may initiate ripple effects (31), with benefits extending to a range of personal and social outcomes that can improve health (16, 32).
Notably, acceptance training appears to be a central mechanism of mindfulness interventions for mitigating loneliness and social isolation. In particular, mindfulness training in both monitoring and acceptance skills (MA) reduced loneliness and increased social contact compared with a matched mindfulness training in monitoring skills only (MO) and an active control program. These results are consistent with some long-standing traditions of Buddhist contemplative training, where equanimity practices (i.e., acceptance) foster an equal attitude of compassion toward oneself and all others, and thus promote social connectivity (15). This study directly tested the importance of experiential acceptance in secular mindfulness interventions. Simply bringing greater awareness to the present moment (in the MO condition) was not enough to impact loneliness or social interactions; it appears critical to learn how to attend to experiences through a lens of acceptance (MA condition). Maintaining acceptance and equanimity toward experiences in daily life may decrease social threat in ways that increase engagement in social interactions and diminish feelings of loneliness.
How might monitoring and acceptance skills reduce loneliness and social isolation? Evolutionarily, both loneliness and social isolation represent threats to survival (33); this social threat increases vigilance, bias, and reactivity toward negative social interactions, which can impact social behavior in ways that fulfill expectations of social distance and reinforce feelings of loneliness (34). Bringing greater awareness (i.e., monitoring) to social interactions may increase attentiveness to social cues and one’s own emotional reactions to them, while also adopting an open and nonreactive attitude (i.e., acceptance) toward these experiences may aid in regulating emotions, thus reducing perceptions of social threat. Similarly, monitoring uncomfortable feelings of loneliness while maintaining an impersonal and nonevaluative attitude (i.e., acceptance) may allow lonely feelings to dissipate. Together, monitoring and acceptance may reduce social distress, allow for more flexible and less biased responding to social interactions, and encourage greater engagement with others. In short, maintaining equanimity toward pleasant and unpleasant experiences alike may change how people relate to their experiences, ultimately changing social perceptions and behaviors in ways that reduce loneliness and increase social contact.
Future research might untangle which process begins to change first as mindful acceptance skills develop: seeking more social interactions or relating differently with (and thus diminishing) feelings of loneliness. Mindfulness may interact with feelings of loneliness to motivate greater social engagement, which then reduces loneliness. Or, mindfulness may regulate the distress associated with loneliness, which reduces social threat and inspires people to seek more social interactions. It is also possible that these processes change relatively independently. Furthermore, mindfulness could change practitioners’ perceptions of their partners’ responsiveness (35) and lead them to seek out more social interactions because they feel more rewarding (and less threatening); it is also possible that developing new habits of relating mindfully with others could attract relationship partners for more interactions.
This study also provides a foundation for future work to investigate plausible chains of mechanistic processes leading from acceptance training to social functioning. Practice in welcoming and accepting all momentary experiences without interfering or identifying with them may foster important downstream psychological processes. For example, acceptance training may lead to insights about the nature of the self and of reality, which may be important for the changes in social perceptions and behaviors observed here. In particular, dereification—the recognition that one’s thoughts and experiences are not true reflections of reality (36)—may be a key insight that shifts one’s perspective toward social cognitions and transforms social functioning. However, to examine dereification as a potential mechanism, validated measures are needed to assess phenomenological experiences among beginning meditators. The dismantling design used here bypassed measurement issues that continue to challenge contemplative research (37, 38), and the results establish that acceptance training is a necessary component of mindfulness interventions for tackling social risk. This initial demonstration opens opportunities to further characterize mindfulness-intervention mechanisms.
Notably, the supplementary analyses show that the effects of mindfulness training were specific to loneliness and social interactions measured in daily life via ambulatory assessment. Retrospective global self-report measures of loneliness and social support captured improvements across all active treatment conditions, and social-network size (a measure of social isolation) remained stable. In contrast, ambulatory assessment outcomes appeared to be sensitive to condition-specific changes in dynamic social processes in daily life (39). This pattern, wherein results showed specific training effects on ambulatory-assessed social outcomes but nonspecific effects of training on global social outcomes, makes an important methodological point, demonstrating the sensitivity of ambulatory approaches for capturing ecologically valid changes in psychosocial processes that are less prone to common retrospective self-report biases (25, 40). Moreover, accumulating evidence suggests that ambulatory assessment approaches more tightly link emotions and experiences with health-relevant biological processes (22) and show promise for predicting long-term health outcomes (41).
In hopes of guiding further research that builds on the present findings, we highlight several considerations about the study design and interventions that may prove important for replication and extension. Although this study carefully controlled for nonspecific intervention factors, acceptance training may build on several of these contextual features. First, it is important to reiterate that monitoring and acceptance—rather than acceptance alone—act synergistically to reduce social risk factors. Just as lesioning a particular brain region does not mean that region is solely responsible for the function lost, but, rather, that it is a necessary component of a dynamic system (42), acceptance alone is likely not sufficient for improving social functioning, but is instead a necessary component of mindfulness interventions. Second, to specifically impact social processes through mindfulness intervention, it may be important to bring awareness to social dynamics in daily life before beginning mindfulness training (e.g., via EMA) and/or to explicitly practice mindful acceptance in the context of social interactions (the focus of one lesson in each intervention). Finally, other features of mindfulness interventions may play important roles in supporting acceptance-skill development; for example, the ethical framework presented in all interventions—that the ultimate goal is to positively impact others—may be important for promoting prosocial vs. antisocial tendencies (43).
We note several limitations of this study. First, we recruited a sample of stressed community adults and did not specifically target lonely or socially isolated populations. However, the study sample tended to be lonely, with participants on average reporting moderate to high loneliness compared with normative samples (44). This pattern reflects the epidemiology of loneliness as a risk factor that is increasing in the United States (1, 45). Nonetheless, further research is needed to test whether smartphone-based mindfulness training can reduce loneliness and increase social interactions in socially isolated populations; individually delivered mindfulness training may be more or less effective among people at high social risk. Future work is also needed to understand whether mindfulness encourages people to reach out more to their existing contacts (thus strengthening existing relationships) or to new contacts (engaging more with strangers and acquaintances) on a daily basis. To this end, future research could utilize reports from close informants to help clarify how participants’ social behaviors and attitudes change through the course of mindfulness training. Finally, this study is limited by its lack of follow-up assessment; to evaluate the public health implications of mindfulness interventions for reducing social risk factors, more work is needed to test the maintenance of social-functioning benefits over time. Mindfulness skills developed through meditation practice may transfer into daily life and build over time, or effects may fade without continued practice. Conveniently, smartphone-based mindfulness apps provide a promising way to promote continued practice following the 2-wk foundational mindfulness program.
Overall, this preregistered trial provides promising evidence that individually delivered mindfulness training can decrease loneliness and increase social contact in daily life. In particular, developing an accepting attitude toward present experiences translated to improvements in social functioning. Learning acceptance skills reduced perceptions of loneliness and increased daily social-interaction frequency and variety. Experiential acceptance has received relatively little scientific scrutiny (15), despite the fact that acceptance is embedded in many cultural practices [including Buddhist, Christian, Jewish, Islamic, Taoist, yogic, and shamanic contemplative practices and rituals (46)]. As such, this work provides promising directions for exploring psychological skills that target social risk factors and may ultimately promote health.
Materials and Methods
Participants and Procedure.
Enrolled participants were 153 stressed adults (Mage = 32 y, SD = 14; see SI Appendix, Table S1 for baseline characteristics) recruited from the Pittsburgh community for a study testing smartphone training programs for managing stress. Primary analyses are reported using all available preintervention and postintervention data (n = 153 in EMA analyses; n = 152 in diary analyses). See SI Appendix, Fig. S1 for a CONSORT flowchart.
The study design and outcomes described here were preregistered with Clinical Trials identifier NCT02433431 (47), and this report describes social-functioning outcome data (secondary trial outcomes). Eligible participants were healthy English-speaking smartphone owners (Android or iPhone) between the ages of 18 and 70 y who scored >5 on the four-item Perceived Stress Scale [reflecting higher-than-average perceived stress (48–50)]. See SI Appendix for the full list of exclusion criteria. Written informed consent was obtained from all participants, and all study procedures were approved by the Carnegie Mellon University IRB. Sample size was determined for this clinical trial (20) by estimating a medium effect (d = 0.52) in G*Power (51). At 80% power, n = 147 participants were needed to detect omnibus differences between three study conditions (group × time interaction) using ANOVAs.
In this three-arm parallel trial, interested participants were prescreened for eligibility by telephone, then further screened at an in-person baseline assessment. Subject IDs were assigned to a condition by using a 3:3:2 randomization sequence (MA:MO:control). At the baseline assessment, enrolled participants provided a dried blood spot (DBS) sample, completed a questionnaire and task battery (including global measures of loneliness, social network, and social support; SI Appendix), and were oriented to the at-home study assessments and intervention. During 3 wk of at-home study activities, participants completed three consecutive days of preintervention EMA and diary assessments (Measures and SI Appendix), a 14-d intervention period (Interventions and SI Appendix), and three consecutive days of postintervention EMA and diary assessments immediately following the intervention period. Participants received standardized study reminder texts and phone calls throughout the at-home period and were able to call or text the study hotline to ask questions or resolve technical issues. Participants returned for a postintervention assessment an average of 4.66 d (SD = 1.88 d) after the completion of training. They provided a DBS sample (to be reported elsewhere), completed questionnaires and tasks (including a measure of treatment expectancies and global measures of loneliness, social network, and social support; Measures and SI Appendix), and underwent the Trier Social Stress Task and assessments (reported in ref. 20). After all outcome measures were collected, participants were funnel-debriefed, informed of the primary aims of the study (to test the active ingredients of mindfulness training), given access to the training program of their choice, and compensated for their time.
Interventions.
Participants were randomly assigned to receive one of three 14-lesson smartphone-based interventions: MA, MO, or Coping control. The intervention programs were developed in collaboration with leading mindfulness teacher S.Y. and were based on his Unified Mindfulness system (52). The two mindfulness meditation programs were designed to systematically parse mindfulness instruction in (i) present-focused attention monitoring and (ii) acceptance, while the control program was designed to be useful for managing stress without training either mindfulness skill (instead covering common reappraisal and coping strategies). All interventions were matched on structure, length, attentional demand, expectancies, and delivery tone of voice. During the 14-d intervention period, participants were expected to complete one 20-min audio lesson (tied to their condition assignment) each day, plus brief homework practice (3–10 min per day). The theme of social relationships was covered in lesson 4 or 5 of each intervention program, emphasizing key skills (acceptance/equanimity in MA; monitoring/clarity in MO; and reflection and analytic thinking in control) to practice in the context of social interactions. See SI Appendix for details on the full content of each intervention.
Measures.
The primary outcomes assessing loneliness and social isolation in participants’ natural environments were assessed at preintervention and postintervention. A two-pronged ambulatory assessment approach involving EMA and end-of-day diary assessments was used to sample social processes in participants’ daily lives. Ambulatory assessments were administered on participants’ own smartphones by using Qualtrics surveys delivered through SurveySignal text links. EMA surveys were administered at four quasirandom times each day (totaling 24 surveys across 3 d preintervention and 3 d postintervention); and text links were sent during each of four 2.5-h blocks distributed between 9:00 AM and 7:00 PM, with links expiring after 45 min. Links for daily diary surveys (six surveys in total across preintervention and postintervention) were sent at 8:30 PM and remained active until 11:30 PM. Ambulatory assessments were administered on two weekdays and one weekend day (Thursday–Saturday or Sunday–Tuesday) counterbalanced at preintervention and postintervention; this schedule enabled the collection of postintervention EMA and diary data immediately following intervention completion. In addition, retrospective global measures of loneliness, social isolation, and social support assessed in the laboratory and exploratory measures of reactions to social interactions assessed in a subset of EMA data are described in SI Appendix. See Dataset S1 for raw data.
Subjective perceptions of loneliness.
The subjective experience of loneliness was assessed with one diary item prompted each evening for 3 d preintervention and postintervention. Specifically, diary assessments measured feelings of loneliness (“How lonely did you feel today?”) experienced on average across the entire day on 7-point Likert scales ranging from 1 (not at all) to 7 (extremely).
Objective social isolation: Social interactions.
Objective social isolation was assessed by using (i) one EMA item, prompted four times daily for 3 d preintervention and 3 d immediately postintervention, and (ii) two diary items, prompted once each evening for 3 d preintervention and postintervention.
EMA surveys assessed the total number of social interactions since the last survey (∼2.5 h apart). Social interactions were defined as in-person, phone, or online conversations lasting at least 3 min; interactions had to involve back-and-forth communication (e.g., sustained text-message conversations counted as interactions, but sending emails did not). Participants used a drop-down menu to indicate the total number of social interactions (options: 0, 1, 2, 3, 4, 5, 6, 7, 8, 9, or 10+) in response to a single item (“Since you completed the last survey, how many social interactions have you had?”).
End-of day diary surveys assessed the total number of social interactions each day and the total number of interaction partners each day. Participants were prompted to call to mind each social interaction over the course of the entire day before responding to questions. Number of social interactions was assessed from a single item (“Please estimate the total number of social interactions you had today. If you interacted with the same person or people more than once today, count each of those interactions.”) using a drop-down menu (options: 0, 1–2, 3–5, 6–10, 11–20, and 21+ interactions). To maintain the normal distribution of responses across subjects, primary analyses were conducted by using codes to represent these ranges (0–5). To visualize the actual number of social interactions reported each day, an estimated number of social interactions was calculated by using the middle of each range (0, 1.5, 4, 8, 15.5, and 21). Number of interaction partners was assessed from a single item (“How many different people did you interact with today?”) with the same drop-down response options (0, 1–2, 3–5, 6–10, 11–20, and 21+ people). Again, primary analyses were conducted by using coded ranges (0–5), and the actual number of interaction partners was estimated (0, 1.5, 4, 8, 15.5, or 21) for illustrative purposes.
Analyses.
Analyses were conducted with SPSS Statistics (Version 21.0; IBM) and Stata software (Version 14.2; StataCorp). Preliminary analyses (conducted in SPSS) tested for condition differences in demographics and other baseline characteristics using χ2 (for categorical variables) and ANOVA tests (for continuous variables). Treatment expectancies, treatment adherence, EMA compliance, and EMA counterbalance were evaluated as covariates using ANOVA to test for significant condition differences.
MLMs were used to test for time (pre or post) × condition (MA, MO, or control) differences on the primary, secondary, and exploratory outcomes using Stata’s mixed command with restricted maximum likelihood estimation. The assumption of dependence in ambulatory assessment data was confirmed in unconditional models, with 33–58% of variance occurring between individuals and 42–64% occurring within individuals (SI Appendix). Because very little variance was explained at the day level in EMA models (2%), two-level models were used for both diary and EMA data.
In sum, models followed this general equation:
with β0i reflecting the intercept for the reference group (MA) at preintervention compared with MO and control groups, and β1i accounting for time (pre or post) and time × condition interactions. Time (pre or post) and day of week were modeled at level 1, while study condition was modeled at level 2; rti and u0i represented error at the within- and between-subject levels, respectively. In EMA models, time of day (first, second, third, or fourth survey), which varied at the observation level, was also included at level 1 to account for temporal dependency between proximal observations.
Within-group effect sizes were calculated by dividing the prepost mean difference in each condition by that condition’s preintervention SD (53) adjusted to account for the overall prepost correlation for each outcome (see equation 8 in refs. 54 and 55). Between-group effect sizes for each contrast were calculated by subtracting within-group effect sizes (56, 57).
Supplementary Material
Acknowledgments
This research was supported by the Yoga Science Foundation; the Mind & Life Institute Varela and 1440 award programs; the American Psychological Association; and the National Institutes of Health (NIH) National Center for Complementary and Integrative Health Grants F32AT009508, R21AT008493, and R01AT008685 and National Center for Advancing Translational Sciences Grant UL1TR000005. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the foundation funders.
Footnotes
Conflict of interest statement: S.Y. owns a portion of 01 Expert Systems, which will be releasing a modified and extended version of the Monitor+Accept mindfulness intervention as a commercial app.
This article is a PNAS Direct Submission. S.C. is a guest editor invited by the Editorial Board.
Database deposition: A complete dataset has been uploaded as a Supporting Information file.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1813588116/-/DCSupplemental.
References
- 1.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cacioppo JT, Cacioppo S, Boomsma DI. Evolutionary mechanisms for loneliness. Cogn Emotion. 2014;28:3–21. doi: 10.1080/02699931.2013.837379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: A systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masi CM, Chen H-Y, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Creswell JD, et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain Behav Immun. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis MC, Zautra AJ. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: Results of a randomized controlled trial. Ann Behav Med. 2013;46:273–284. doi: 10.1007/s12160-013-9513-7. [DOI] [PubMed] [Google Scholar]
- 9.Zhang N, Fan FM, Huang SY, Rodriguez MA. Mindfulness training for loneliness among Chinese college students: A pilot randomized controlled trial. Int J Psychol. 2018;53:373–378. doi: 10.1002/ijop.12394. [DOI] [PubMed] [Google Scholar]
- 10.Barnes S, Brown KW, Krusemark E, Campbell WK, Rogge RD. The role of mindfulness in romantic relationship satisfaction and responses to relationship stress. J Marital Fam Ther. 2007;33:482–500. doi: 10.1111/j.1752-0606.2007.00033.x. [DOI] [PubMed] [Google Scholar]
- 11.Carson JW, Carson KM, Gil KM, Baucom DH. Mindfulness-based relationship enhancement. Behav Ther. 2004;35:471–494. [Google Scholar]
- 12.Berry DR, et al. Mindfulness increases prosocial responses toward ostracized strangers through empathic concern. J Exp Psychol Gen. 2018;147:93–112. doi: 10.1037/xge0000392. [DOI] [PubMed] [Google Scholar]
- 13.Condon P, Desbordes G, Miller WB, DeSteno D. Meditation increases compassionate responses to suffering. Psychol Sci. 2013;24:2125–2127. doi: 10.1177/0956797613485603. [DOI] [PubMed] [Google Scholar]
- 14.Lim D, Condon P, DeSteno D. Mindfulness and compassion: An examination of mechanism and scalability. PLoS One. 2015;10:e0118221. doi: 10.1371/journal.pone.0118221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desbordes G, et al. Moving beyond mindfulness: Defining equanimity as an outcome measure in meditation and contemplative research. Mindfulness (N Y) 2014;2014:356–372. doi: 10.1007/s12671-013-0269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindsay EK, Creswell JD. Mechanisms of mindfulness training: Monitor and acceptance theory (MAT) Clin Psychol Rev. 2017;51:48–59. doi: 10.1016/j.cpr.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quaglia JT, Goodman RJ, Brown KW. From mindful attention to social connection: The key role of emotion regulation. Cogn Emotion. 2015;29:1466–1474. doi: 10.1080/02699931.2014.988124. [DOI] [PubMed] [Google Scholar]
- 18.Adair KC, Fredrickson BL, Castro-Schilo L, Kim S, Sidberry S. Present with you: Does cultivated mindfulness predict greater social connection through gains in decentering and reductions in negative emotions? Mindfulness. 2017;9:737–749. [Google Scholar]
- 19.Hayes-Skelton S, Graham J. Decentering as a common link among mindfulness, cognitive reappraisal, and social anxiety. Behav Cogn Psychother. 2013;41:317–328. doi: 10.1017/S1352465812000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindsay EK, Young S, Smyth JM, Brown KW, Creswell JD. Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology. 2018;87:63–73. doi: 10.1016/j.psyneuen.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 21.Wahbeh H, Svalina MN, Oken BS. Group, one-on-one, or internet? Preferences for mindfulness meditation delivery format and their predictors. Open Med J. 2014;1:66–74. doi: 10.2174/1874220301401010066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conner TS, Barrett LF. Trends in ambulatory self-report: The role of momentary experience in psychosomatic medicine. Psychosom Med. 2012;74:327–337. doi: 10.1097/PSY.0b013e3182546f18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hawkley LC, Preacher KJ, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychol. 2010;29:124–129. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joseph NT, Kamarck TW, Muldoon MF, Manuck SB. Daily marital interaction quality and carotid artery intima-medial thickness in healthy middle-aged adults. Psychosom Med. 2014;76:347–354. doi: 10.1097/PSY.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smyth JM, Juth V, Ma J, Sliwinski M. A slice of life: Ecologically valid methods for research on social relationships and health across the life span. Soc Personal Psychol Compass. 2017;11:e12356. [Google Scholar]
- 26.Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117:497–529. [PubMed] [Google Scholar]
- 27.Ryan RM, Deci EL. Self-Determination Theory: Basic Psychological Needs in Motivation, Development, and Wellness. Guilford Publications; New York: 2017. [Google Scholar]
- 28.Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: An integrative review. Health Soc Care Community. 2018;26:147–157. doi: 10.1111/hsc.12367. [DOI] [PubMed] [Google Scholar]
- 29.Kabat-Zinn J. Mindfulness. Mindfulness. 2015;6:1481–1483. [Google Scholar]
- 30.Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. J Pers. 2004;72:1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- 31.Wilson DK. Behavior matters: The relevance, impact, and reach of behavioral medicine. Ann Behav Med. 2015;49:40–48. doi: 10.1007/s12160-014-9672-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindsay EK, et al. How mindfulness training promotes positive emotions: Dismantling acceptance skills training in two randomized controlled trials. J Pers Soc Psychol. 2018;115:944–973. doi: 10.1037/pspa0000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66:733–767. doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adair KC, Boulton AJ, Algoe SB. The effect of mindfulness on relationship satisfaction via perceived responsiveness: Findings from a dyadic study of heterosexual romantic partners. Mindfulness. 2018;9:597–609. [Google Scholar]
- 36.Lutz A, Jha AP, Dunne JD, Saron CD. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. Am Psychol. 2015;70:632–658. doi: 10.1037/a0039585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams JM, Russell I, Russell D. Mindfulness-based cognitive therapy: Further issues in current evidence and future research. J Consult Clin Psychol. 2008;76:524–529. doi: 10.1037/0022-006X.76.3.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Dam NT, et al. Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci. 2018;13:36–61. doi: 10.1177/1745691617709589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 40.Nisbett RE, Wilson TD. Telling more than we can know: Verbal reports on mental processes. Psychol Rev. 1977;84:231–259. [Google Scholar]
- 41.Steptoe A, Wardle J. Positive affect measured using ecological momentary assessment and survival in older men and women. Proc Natl Acad Sci USA. 2011;108:18244–18248. doi: 10.1073/pnas.1110892108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adolphs R. Human lesion studies in the 21st century. Neuron. 2016;90:1151–1153. doi: 10.1016/j.neuron.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monteiro LM, Musten RF, Compson J. Traditional and contemporary mindfulness: Finding the middle path in the tangle of concerns. Mindfulness. 2015;6:1–13. [Google Scholar]
- 44.Russell DW. UCLA loneliness scale (version 3): Reliability, validity, and factor structure. J Pers Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 45. Cigna (2018) U.S. Loneliness Index (Cigna, Philadelphia)
- 46.Young S. The Science of Enlightenment: How Meditation Works. Sounds True; Louisville, CO: 2016. [Google Scholar]
- 47.Lindsay EK, Creswell JD. 2015 Mechanisms of mindfulness and stress resilience: A mobile app mindfulness training study. Clinical trial. Available at https://clinicaltrials.gov/ct2/show/NCT02433431. Accessed January 25, 2019.
- 48.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 49.Cohen S, Williamson G. Perceived stress in a probability sample of the US. In: Spacapam S, Oskamp S, editors. The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Sage; Thousand Oaks, CA: 1988. pp. 31–67. [Google Scholar]
- 50.Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the short form perceived stress scale (PSS-4) J Health Psychol. 2013;18:1617–1628. doi: 10.1177/1359105313508346. [DOI] [PubMed] [Google Scholar]
- 51.Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 52.Young S. What is mindfulness? A contemplative perspective. In: Schonert-Reichl KA, Roeser RW, editors. Handbook of Mindfulness in Education. Springer; New York: 2016. pp. 29–45. [Google Scholar]
- 53.Morris SB. Estimating effect sizes from pretest-posttest-control group designs. Organ Res Methods. 2008;11:364–386. [Google Scholar]
- 54.Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7:105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- 55.Wiseheart M. 2014 Effect size calculator. Available at https://www.yorku.ca/ncepeda/effectsize.html. Accessed July 5, 2018.
- 56.Klauer KJ. 2001. Handbuch Kognitives Training (Hogrefe, Boston). German.
- 57.Lenhard W, Lenhard A. 2016 Calculation of effect sizes. Psychometrica. Available at https://www.psychometrica.de/effect_size.html. Accessed May 16, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.