Abstract
Ebola virus (EBOV) pathology in humans remains incompletely understood; therefore, a number of rodent and nonhuman primate (NHP) models have been established to study the disease caused by this virus. While the macaque model most accurately recapitulates human disease, rodent models, which display only certain aspects of human disease but are more cost-effective, are widely used for initial screens during EBOV countermeasure development. In particular, mice and guinea pigs were among the first species used for the efficacy testing of EBOV vaccines and therapeutics. While mice have low predictive value, guinea pigs have proven to be a more reliable predictor for the evaluation of countermeasures in NHPs. In addition, guinea pigs are larger in size compared to mice, allowing for more frequent collection of blood samples at larger volumes. However, guinea pigs have the disadvantage that there is only a limited pool of immunological tools available to characterize host responses to vaccination, treatment and infection. In this chapter, the efficacy testing of an EBOV vaccine and a therapeutic in the guinea pig model are described.
Keywords: Ebola virus, Guinea pigs, In vivo experiment, Animal model, Countermeasures, Vaccines, Therapeutics
1. Introduction
Despite decades of research into the development of vaccines and treatment options against Ebola virus (EBOV), there is still no approved countermeasure available. In order to understand this disease and facilitate countermeasure development, several animal models for EBOV have been developed, ranging from rodents to nonhuman primates (NHPs). Macaques are considered the gold standard model in EBOV research since wildtype (wt) EBOV isolates readily cause disease in NHPs that is very similar to that observed in humans (reviewed in [1]). However, working with NHPs has its disadvantages, including the very high costs associated with these studies, the ethical considerations, and the infrastructural requirements. As a result only a few facilities worldwide work with NHPs in a biosafety level 4 (BSL4) laboratory. Accordingly, rodent models, such as the mouse, hamster and guinea pig, have been established to overcome the disadvantages presented by NHP work. Unlike NHPs, rodents are relatively cheap and easy to handle, and guinea pigs have the added advantage of being large enough to permit sequential sampling. Notably, however, wtEBOV is incapable of causing severe disease in rodents, with guinea pigs developing only a transient febrile illness and antibody response after infection with wtEBOV [2, 3]. To address this issue, wtEBOV Mayinga 1976 was serially passaged in guinea pigs until a uniformly lethal, guinea pig-adapted EBOV (GPA-EBOV) was obtained [4, 5]. During the adaptation process, the GPA-EBOV acquired nucleotide substitutions resulting in amino acid changes in the NP, GP, VP24, and L genes (reviewed in [6]).
Guinea pigs are routinely used in testing countermeasures for many viral hemorrhagic fever pathogens, including filoviruses (reviewed in [1]). In our hands, infection of Hartley guinea pigs with 10 plaque-forming-units (PFU) of GPA-EBOV [4], which equals 1000 LD50, causes lethal disease within 7–9 days [3]. In this chapter, I describe the procedures for efficacy testing of a vaccine or therapeutic against EBOV using guinea pigs in a BSL4 laboratory.
2. Materials
Hartley guinea pigs (Cavia porcellus).
Vaccine or therapeutic for efficacy testing.
Guinea pig-adapted (GPA) EBOV.
Dulbecco’s Modified Eagle’s Medium (DMEM) for inoculum preparation.
Isoflurane.
1 mL tuberculin syringe with 25 gauge × 5/8″ needle for infection and blood collection.
Micro-Chem Plus (National Chemical Laboratories) or another disinfectant approved for use in the BSL4 laboratory.
1.3 mL collection tube with 1.6 mg EDTA/mL blood for blood collection (Sarstedt).
1.1 mL Z-Gel collection tube for serum collection (Sarstedt).
BD Vacutainer Eclipse Blood collection needles, 21 gauge × 1 ¼ ″.
BD Vacutainer one use holders.
BD Vacutainer blood collection tubes, 10 mL (serum or EDTA).
Backdraft table.
Absorbent bench pads.
Carcass bags.
3. Methods
The following procedures must be performed in the animal space of a BSL4 laboratory, and they require a high level of expertise in handling animals and sharps in this environment. The procedures described here were approved by the Institutional Biosafety Committee to be carried out at the BSL4 laboratory at the Integrated Research Facility, Division of Intramural Research, National Institute for Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA. Several parameters, including the disinfectant used and protocols for disposal of carcasses may vary between BSL4 facilities.
3.1. Infection with GPA-EBOV
Acclimate the guinea pigs to the BSL4 environment for 5–7 days before infection with GPA-EBOV (see Note 1). Provide food and water ad libitum.
On the day of infection, obtain a baseline weight for each of the animal prior to infection (see Note 2).
Perform the infection on a backdraft table in the animal procedure space of the BSL4 laboratory. Cover the table section where the animal will be infected with an absorbent pad. Place the anesthesia chamber on the table and connect it to an anesthetic vaporizer such that inhalational isoflurane is administered at low doses (≤5%) (see Note 3).
Place one guinea pig at a time in the anesthesia chamber and observe until breathing is slow and deep, indicating sufficient anesthesia of the guinea pig.
Even though the animal is anesthetized, two people are required for the procedure, one person handling the syringe/needle, another person properly restraining the animal. Place the anesthetized guinea pig on its back, and while the first person restrains the upper body of the animal with long forceps, the second person straightens and holds the animal’s hind feet together and administers 1 mL GPA-EBOV (see Note 4) diluted in DMEM intraperitoneally (IP) using a 25 gauge × 5/8″ needle into two sites in the lower abdomen (0.5 mL each site) (see Note 5).
Following injection, the second person immediately disinfects the syringe and needle with 5% Micro-Chem Plus before disposal into a sharps collection container (see Note 6). The first person lays the animal on its side in the cage and monitors breathing until the guinea pig is awake.
After infection, the guinea pigs are monitored and weighed daily for signs of disease. Around day 7 post-infection, the animals will develop endstage signs of disease, including dehydration and weight loss greater than 20%. During this critical phase of the study, the animals are monitored twice daily.
Once euthanasia criteria are reached (see Note 7), animals are humanely euthanized, however, given the rapid disease progression animals will also sometimes be found dead. For euthanasia, the animal is first deeply anesthetized with inhalational isoflurane and subsequently euthanized by exsanguination (i.e., severing the jugular blood vessels with scissors) and placed in a carcass bag (see Note 8). Carcasses are stored at −80°C until removal from the BSL4 laboratory (via autoclave) and proper disposal.
After GPA-EBOV infection (usually 4–6 weeks), surviving animals are deeply anesthetized using inhalational isoflurane and a large volume (greater than 10 mL) terminal blood sample is collected via cardiac puncture using vacutainer tubes. To accomplish this, assemble the 21 gauge × 1 ¼ ″ vacutainer needle with the tube holder, but leave the needle sheath on. Place the anesthetized guinea pig on its back and continue anesthesia using a nose cone. Place a blood collection tube loosely in the tube holder, unsheathe the needle and insert it directly under the sternum of the animal at a 30–45° upward angle. When the needle is 0.5–1 cm inserted, push the vacutainer tube into place in the holder. Push the needle further into the guinea pig until the needle punctures the heart and the tube begins to fill with blood. Remove the full vacutainer tube from the holder before withdrawing the needle from the animal. Dispose of the needle/holder immediately in a sharps container. Place blood collection tubes on a tube roller (EDTA) or in a tube rack (serum) until sample processing.
The animal is euthanized by exsanguination (i.e., severing the jugular blood vessels with scissors) and placed in a carcass bag (see Note 8). Carcasses are stored at −80°C until removal from the BSL4 laboratory (via autoclave) and proper disposal.
3.2. Treatment Administration
In guinea pigs, treatment testing is usually performed using either intramuscular (IM) or IP administration of the drug while the animal is under anesthesia (see Note 9). Similar to the GPA-EBOV infection, the procedure must be carried out on a back draft table in the animal procedure space of the BSL4 laboratory. IP treatment should be at least 6–8 h before or after IP GPA-EBOV infection to allow for proper virus uptake. Single treatments like monoclonal antibody therapy are generally first tested on day 1 after infection. Depending on the success rate, a later treatment start may be assessed afterwards.
Cover the table section where the animal will be handled with an absorbent pad. Place the anesthesia chamber on the table and connect it to an anesthetic vaporizer such that inhalational isoflurane is administered at low doses (≤5%) (see Note 3).
Place one guinea pig at a time in the anesthesia chamber and observe until breathing is slow and deep, indicating sufficient anesthesia of the guinea pig.
-
Even though the animal is anesthetized, two people are required for the procedure, one person handling the syringe/needle, another person properly restraining the animal.
For IP administration, place the anesthetized guinea pig on its back, and while the first person restrains the upper body of the animal with long forceps, the second person straightens and holds the animal’s hind feet together and administers up to 1 mL of drug IP using a 25 gauge × 5/8″ needle into one site in the lower abdomen.
For IM administration, place the anesthetized guinea pig on its abdomen, and while the first person restrains the upper body of the animal with long forceps, the second person restrains the animal’s hind feet and administers up to 0.2 mL of drug IM into the thigh muscle using a 25 gauge × 5/8″ needle. Alternate the thigh muscle into which treatments are administered if giving daily treatments.
Following injection, the person holding the syringe/needle immediately disinfects the syringe/needle with 5% Micro-Chem Plus before disposal into a sharps collection container (see Note 6). The other person lays the animal on its side back in the cage and monitors breathing until the guinea pig is awake.
3.3. Sequential Blood Collection from the anterior vena cava
Some animal experiments, mainly treatment studies, may require serial blood collection in order to monitor viremia or drug levels in blood/serum over time. Small blood volumes can be drawn from guinea pigs via the marginal ear vein, lateral saphenous vein, or cephalic and tarsal veins. Larger volumes (up to 1 mL) can be collected from the jugular vein, anterior vena cava, or femoral vein. Collecting blood from the anterior vena cava is my preferred method, as the animal does not need to be very deeply anesthetized, and the risk of asphyxiation is therefore minimized.
Cover the table section where the animal will be handled with an absorbent pad. Place the anesthesia chamber on the table and connect it to an anesthetic vaporizer such that inhalational isoflurane is administered at low doses (≤5%) (see Note 3).
Place one guinea pig at a time in the anesthesia chamber and observe until breathing is slow and deep, indicating sufficient anesthesia of the guinea pig.
Even though the animal is anesthetized, two people are required for this procedure. The first person restrains the lower abdomen/hind feet of the animal by straightening the legs and holding the animal’s hind feet together while the second person is collecting the blood.
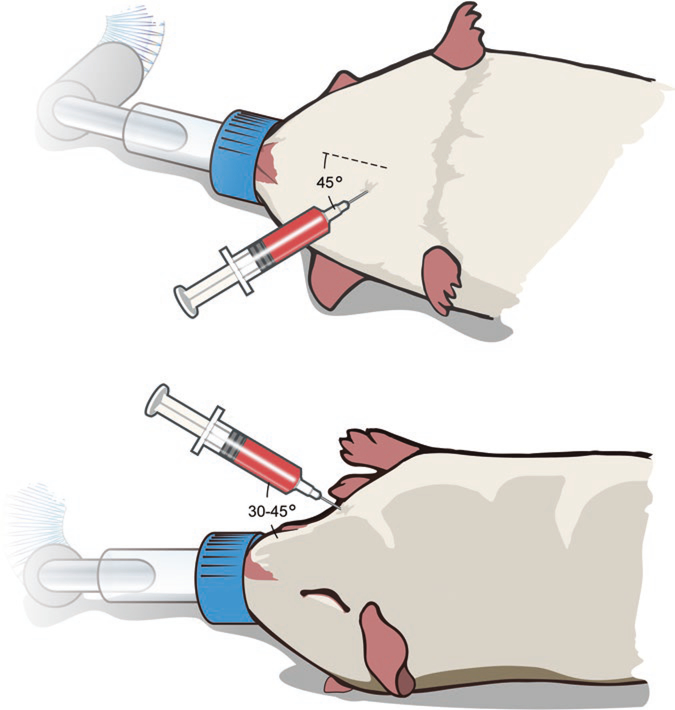
Lay the animal on its back, nose towards the person performing the procedure (Fig. 1). A nose cone providing continuous inhalational isoflurane is recommended. Use a 25 gauge × 5/8″ needle on a 1-mL tuberculin syringe to draw the blood. The needle is inserted at about a 45° angle to the sternum into the thoracic region, 30–45° angle upward (Fig. 1). As soon as the needle is inserted apply sucktion to draw blood. Once the needle is in the vein, pull the syringe plunger back slowly to achieve a slow and continuous blood draw of up to 1 mL.
After the blood draw, the wound is immedialtely covered with gauze by the person restraining the animal and pressure is applied to stop the bleeding. Once the bleeding is stopped, the animal is laid on its side in the cage and breathing is monitored until the guinea pig is awake.
The blood is immediately transferred into a serum or whole blood (EDTA) collection tube which is placed on a tube roller (EDTA) or in a tube rack (serum) until sample processing. The syringe and needle are disinfected using the 5% Micro-Chem Plus solution before disposal into a sharps collection container (see Note 6).
Fig. 1.
Blood sample collection from the anterior vena cava. The animal is laid on its back under isolfurane anesthesia via a nose cone. The needle is not fully inserted at about a 45° angle to the sternum (top panel, top view) and a 30–45° angle to the guinea pig (bottom panel, side view) for a slow blood draw from the anterior vena cava (up to 1 mL)
3.4. Terminal Sample Collection
Some studies require the determination of disease progression and viremia. If taking a serial blood sample as outlined above is insufficient and the experiment requires determination of tissue virus load and pathological changes, it is recommended to assign a small number of animals per study group for euthanasia and tissue sample collection, e.g., liver and spleen, two main target organs during GPA-EBOV infection, between days 5 and 7 after infection.
Cover the table section where the animal will be handled with an absorbent pad. Place the anesthesia chamber on the table and connect it to an anesthetic vaporizer such that inhalational isoflurane is administered at low doses (≤5%) (see Note 3).
Place one guinea pig at a time in the anesthesia chamber and observe until breathing is slow and deep, indicating sufficient anesthesia of the guinea pig.
First, a large volume (greater than 10 mL) terminal blood sample is collected via cardiac puncture using vacutainer tubes as described in Subheading 3.1, step 9.
The animal is euthanized by exsanguination as described in Subheading 3.1, step 10.
Spray the abdomen of the animal with 70% ethanol to wet the fur for surface disinfection and easier cutting. Use one set of scissors/forceps to cut the abdomen of the animal open. Use a new set of scissors/forceps to remove samples from target organs such as the liver and spleen. Place the samples immediately in proper containers. After the procedure is completed on one animal, place the used instruments in a bucket with 5% Micro-Chem Plus solution for disinfection (see Note 10).
Store the samples properly for the desired downstream application (e.g., titration, histopathology).
Carcasses are stored at −80 °C until removal from the BSL4 laboratory (via autoclave) and proper disposal.
Acknowledgments
The author is grateful to Logan Banadyga (NIAID) for critically reading the manuscript, and to Austin Athman and Ryan Kissinger (NIAID) for assistance with figure production.
Footnotes
Guinea pig caging systems often vary between biosafety level 2 laboratory and BSL4 conditions where HEPA-filtered isolator cages are required. Ideally, the animals should be housed in pairs if the BSL4 caging system allows for it. One animal should have an ear tag or some other kind of identifier as individual body weight will be followed over time.
Following challenge, weight loss and dehydration are obvious signs of GPA-EBOV infection in guinea pigs. Therefore, the individual guinea pig body weight is measured and recorded every day until at least day 14 after GPA-EBOV infection.
Guinea pigs are very sensitive to anesthesia independent of the anesthetic used (inhalational isoflurane for short anesthesia; 2–4 mg Xylazine plus 80–100 mg Ketamine injected IM for longer anesthesia). Animals should be without food for at least 2 h before anesthesia to minimize the risk of asphyxiation after waking up.
For this GPA-EBOV strain the LD50 in Hartley guinea pigs is 0.01 PFU. Generally challenge doses of 100 or 1000 LD50 per animal are used to ensure uniform lethality in the control group. I prefer 1000 LD50 (10 PFU) per animal in 1 mL.
The guinea pig, mouse, and hamster models for EBOV were developed using 2 IP injection sites in order to obtain consistent and reproducible results. If the infection is performed at only one site, variability of results increases between groups in one study and between different studies.
Prepare a 1 L bucket half full with 5% Micro-Chem Plus or any other effective and approved disinfectant. Place the syringe with attached needle in the bucket and suck up 1 mL. Leave the syringe/needle like this until the end of the procedure, when all the animals are infected; minimum contact time is 10 min. Eject Micro-Chem Plus from the syringe/needle and dispose syringe/needle in a sharps container.
Euthanasia criteria as approved by the Institutional Animal Care and Use committee at the Rocky Mountain Laboratories, DIR, NIAID, NIH: Any animal with weight loss >20%, ataxia, extreme lethargy (animal is unresponsive to touch), bloody discharge from nose, mouth, rectum or urogenital area, tachypnea, dyspnea or paralysis of the limbs will be immediately euthanized.
For this purpose medium size autoclave bags are used. We place 8–12 guinea pigs in one bag depending on their size. In addition, these animals can have sharp claws, and therefore we double-bag the carcasses before putting them into the freezer.
Unlike hamsters or mice, guinea pigs are sensitive to anesthesia. They are a great rodent model for vaccine or single-dose treatment efficacy testing, but not my model of choice for daily treatment studies. The risk of asphyxiation is very high and large animal groups are needed in order to compensate for losses while still obtaining statistically significant results. Therefore, I prefer to test drugs requiring daily administration in the hamster model.
Instruments are soaked in the 5% Micro-Chem Plus or any other effective and approved disinfectant solution for about 1 h. After a thorough rinse with water and scrubbing if needed, the instruments are placed in a sonicator. Following sonication for 60 min at 60 °C, the instrruments are removed, thoroughly rinsed with water and air-dried. A thin coat of lubricant (Miltex Spray Lube) is applied to the scissors before the instruments are sorted into dishes and autoclaved to sterilize them for the next use.
References
- 1.Safronetz D, Geisbert TW, Feldmann H (2013) Animal models for highly pathogenic emerging viruses. Curr Opin Virol 3(2):205–209. doi: 10.1016/j.coviro.2013.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowen ET, Lloyd G, Harris WJ, Platt GS, Baskerville A, Vella EE (1977) Viral haemorrhagic fever in southern Sudan and northern Zaire. Preliminary studies on the aetiological agent. Lancet 1(8011):571–573 [DOI] [PubMed] [Google Scholar]
- 3.Marzi A, Ebihara H, Callison J, Groseth A, Williams KJ, Geisbert TW, Feldmann H (2011) Vesicular stomatitis virus-based Ebola vaccines with improved cross-protective efficacy. J Infect Dis 204(Suppl 3):S1066–S1074. doi: 10.1093/infdis/jir348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connolly BM, Steele KE, Davis KJ, Geisbert TW, Kell WM, Jaax NK, Jahrling PB (1999) Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis 179(Suppl 1):S203–S217. doi: 10.1086/514305 [DOI] [PubMed] [Google Scholar]
- 5.Cross RW, Fenton KA, Geisbert JB, Mire CE, Geisbert TW (2015) Modeling the disease course of Zaire ebolavirus infection in the outbred Guinea pig. J Infect Dis 212(Suppl 2):S305–S315. doi: 10.1093/infdis/jiv237 [DOI] [PubMed] [Google Scholar]
- 6.Banadyga L, Dolan MA, Ebihara H (2016) Rodent-adapted Filoviruses and the molecular basis of pathogenesis. J Mol Biol. d oi: 10.1016/j.jmb.2016.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]