Abstract
Background:
This study served as an initial investigation of the role hopelessness may play in the relationship between PTSD symptom change and suicide intent, among a trauma-exposed, treatment-seeking sample. We explored whether the effect of PTSD symptom change on self-reported likelihood of a future suicide attempt (FSA) varies as a function of pre-treatment hopelessness, and whether reductions in hopelessness serve as a mechanism through which PTSD symptom change influences FSA likelihood.
Methods:
Data was collected from participants (N = 159) in a larger randomized clinical trial of a suicide risk-factor intervention. Self-report questionnaires assessed hopelessness, PTSD symptoms, depression symptoms, and FSA likelihood at pre-treatment and one-month follow-up.
Results:
Pre-treatment hopelessness emerged as a significant moderator, such that overall PTSD symptom reductions were related to overall decreases in FSA likelihood among those at or above (but not those below) the sample mean of pre-treatment hopelessness. In a subsample of individuals who reported FSA likelihood > 0 and elevated hopelessness at pre-treatment, overall pre-treatment-to-month-one reductions in hopelessness significantly mediated the relationship between overall PTSD symptom reductions and decreased FSA likelihood during this same time period, even after accounting for depression symptom changes.
Limitations:
Data were limited to self-report measures (i.e., hopelessness, FSA likelihood). The intervention was not PTSD-specific. Mediation analyses were strictly statistical due to overlapping time-points.
Conclusions:
This preliminary investigation suggests pre-treatment hopelessness may serve to identify trauma-exposed individuals for whom PTSD treatment would significantly reduce FSA likelihood. Moreover, reductions in FSA likelihood during treatment may be due in part to reduced hopelessness.
1. Introduction
Suicide presents a significant public health problem, accounting for over 40,000 annual deaths in the United States (Centers for Disease Control and Prevention, 2016). Suicide risk is demonstrably higher among individuals with a history of trauma exposure and posttraumatic stress disorder (PTSD) (Panagioti et al., 2009). Though psychological treatments reduce PTSD (e.g., Cognitive Processing Therapy [CPT]) and suicidality (Tarrier et al., 2008) independently, a paucity of research has investigated the relationship between reductions in posttraumatic stress symptoms (PTSS) and suicidality throughout treatment, or factors which may influence these outcomes.
A comprehensive review of PTSD and suicide underscored the need for investigating psychological variables related to suicide risk, such as post-traumatic sequelae, so to appropriately identify and successfully treat those for whom suicide risk is elevated (Panagioti et al., 2009). Subsequent research suggests that PTSD-specific treatments effectively minimize suicide ideation via global PTSS reduction (Cox et al., 2016; Gradus et al., 2013). However, it may be useful to consider concomitant psychological determinants by which PTSS reductions influence suicidality.
Hopelessness, often described as negative expectancies regarding one's prospects of symptom relief, is a potential mechanism through which PTSS change may influence suicidality. Hopelessness is a robust predictor of suicidal behavior (Beck, 1986; Beck et al., 1990, 1975). Furthermore, hopelessness and suicidality are elevated among veterans with subthreshold and threshold PTSD compared to those with minimal PTSD symptoms (Jakupcak et al., 2011). Paramount to treating these conditions, initial evidence suggests hopelessness is a mechanism through which PTSS reductions occur during treatment (Gallagher and Resick, 2012). Seemingly important, the degree to which hopelessness affects how PTSS reductions influence suicidality is poorly understood; this in spite of Beck postulating decades ago that, “By focusing on reducing sources of a patient's hopelessness, the professional may be able to alleviate suicidal crises more effectively” (Beck et al., 1975).
This study was an initial investigation of the role of hopelessness in determining how PTSS reductions affect self-reported likelihood of making a future suicide attempt among a trauma-exposed, treatmentseeking sample. Specifically, we explored whether the effect of PTSS reductions on future suicide attempt (FSA) likelihood varies as a function of pre-treatment hopelessness, and whether reductions in hopelessness serve as a mechanism through which PTSS reduction influences FSA likelihood. We hypothesized that PTSS reduction would influence FSA likelihood most among those high in pre-treatment hopelessness; and that, among those with elevated hopelessness and suicidality, reductions in hopelessness would partially account for the degree to which PTSS reductions affect FSA likelihood.
2. Methods
Individuals (N = 376) in the Southeastern United States were assessed for eligibility for a larger randomized clinical trial (RCT). Of those eligible (N = 303), the present analyses includes only participants randomized to one of three treatment arms, who reported trauma exposure during the baseline interview (N = 195); 30.8% of these participants met diagnostic criteria for PTSD. Participants were primarily female (55.9%), 18–79 years old (M = 36.94, SD = 16.15). Ethnic composition was 59.0% Caucasian, 26.2% African American, 1.5% Asian/Pacific Islander, and 13.3% ‘Other’.
The 21-item Beck Depression Inventory-II (BDI-II) assessed depression symptom severity (Beck et al., 1996). Reliability was excellent at baseline (α = .93) and follow-up (α = .95).
The PTSD Checklist-Civilian Version (PCL-C) assessed the past-month severity of the 17 DSM-IV PTSD symptoms (Weathers et al., 1991). PCL-C reliability was excellent at baseline (α = .94) and followup (α = .95).
Self-reported likelihood of FSA was assessed using item four of the Suicide Behaviors Questionnaire Revised (SBQ-R) (Osman et al., 2001), which asked participants to rate how likely they would be to attempt suicide “someday” from 0 to 6 (never-very likely). This item was used in lieu of the full SBQ-R because the remaining questions index past suicidality without an established time-frame, which presumably provide little information about suicide risk changes throughout treatment. Baseline to month-one test-retest reliability for this item was calculated via partial correlation, controlling for treatment condition, and base-line-to-month-one PCL-C, BHS, and BDI-II change; which was deemed questionable (r = .67).
Hopelessness was assessed using a 3-item (items 8, 12, 14) version of the 20-item Beck Hopelessness Scale (BHS) (Beck et al., 1974). These items were included as required by the RCT's funding agency, from which data (Ringer et al., 2017) indicate that the three-item version and full BHS are similarly correlated with the SBQ-R (z = 1.29, p = .20) and PCL-C (z = 1.62, p = .11). Reliability for the 3-item version was acceptable at baseline (α = .70) and follow-up (α = .68).
The Structured Clinical Interview for DSM-5-Research Version (SCID-5–RV) was administered by trained doctoral students to evaluate diagnostic status and trauma history at baseline (First et al., 2015).
Participants completed an eligibility interview for a RCT of a computerized intervention targeting cognitive-affective risk factors for suicide. Participants were randomized to one of three intervention conditions; each involved three weekly, one-hour sessions. Condition one comprised a one-session cognitive AS treatment (CAST), and two sessions of an AS cognitive bias modification (CBM), as previously reported (Schmidt et al., 2017). Condition two comprised a one-session intervention based in principles of cognitive behavioral therapy to address problematic ideas and behaviors central to depression, and two sessions of a positive CBM paradigm (Holmes et al., 2006). Condition three combined all components of the first and second conditions described above. Participants returned for a follow-up appointment one month after their last intervention appointment. Participants completed self-report questionnaires at baseline and month-one follow-up. All procedures were approved by the Florida State University Institutional Review Board.
2.1. Data analytic strategy
Data was screened for missingness, skewness, kurtosis, and outliers. Outliers were trimmed to +/− twice the interquartile range from the median. To account for skew, SBQR item 4 was natural log transformed (1 + original SBQ-R item-4 response), following previous procedures (Kimbrel et al., 2016). Among the study variables, 9.5% of data was missing, including .4% of baseline PCL-C scores and 20.8% of all follow-up measures. To account for missing data, multiple imputation by fully conditional specification was executed using SPSS version 22. Moderation and mediation analyses were conducted via the Process macro for SPSS, with 5000 bootstrap resamples for mediation analyses.
The moderating effect of hopelessness on the relationship between baseline-to month-one PCL-C change and month-one SBQR item 4 was assessed, controlling for intervention condition and baseline BDI-II scores (accounting for depression symptoms, including suicidality [i.e., item 9]).
A statistical mediation model was conducted to test baseline-to-month-one hopelessness change as a mechanism through which base-line-to-month-one PTSS reductions mitigate month-one FSU likelihood. As evidence suggests scores ≥ 9 on the full BHS (i.e., endorsing half the items, or roughly similar to endorsing two of our three items) strongly predict FSA (Beck et al., 1990), this analysis was conducted in a subsample (N = 69) who, at baseline: 1) reported > 0 FSA likelihood, and 2) scored ≥ 2 on the three-item BHS. Baseline-to-month-one BDI-II changes were included as a simultaneous mediator to test the specificity of hopelessness change as a mediator. The indirect effect of PTSS change on FSA likelihood through these mediators is considered significant if their respective 95% confidence interval does not include 0.
3. Results
Full descriptive statistics and bivariate correlations for self-report symptom data are reported in Table 1. Bivariate correlations between treatment condition and all symptom measures were nonsignificant (p's > .25).
Table 1.
Bivariate correlations and descriptive statistics for symptom measures at baseline and month-one follow-up.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1. | BL BDI-II | – | |||||||
| 2. | BL PCL-C | .65** | |||||||
| 3. | BL BHS-3 | .35** | .26** | ||||||
| 4. | BL SBQ-R 4 | .28** | .17* | .18* | |||||
| 5. | M1 BDI-II | .66** | .56** | .34** | .25** | ||||
| 6. | M1 PCL-C | .57** | .74** | .23** | .16* | .71** | |||
| 7. | M1 BHS-3 | .35** | .30** | .51** | .15* | .51** | .40** | ||
| 8. | M1 SBQ-R 4 | .27** | .22** | .19** | .54** | .42** | .31** | .32** | – |
| Mean | 23.32 | 47.72 | 1.88 | .22 | 16.09 | 37.10 | 1.75 | .17 | |
| (SD) | (12.11) | (16.58) | (1.14) | (.25) | (12.67) | (15.56) | (1.06) | (.21) | |
| Skewness | .45 | .18 | −.44 | .54 | .73 | .58 | −.20 | .91 | |
| Kurtosis | −.24 | −.84 | −1.29 | −1.11 | −.22 | −.50 | −1.27 | −.23 |
Note. BL = Baseline time point; M1 = Month-One Follow-Up time point; BDI-II = Beck Depression Inventory-II; PCL-C = PTSD Checklist- Civilian Version; BHS-3 = Hopelessness Scale (items 8, 12, 14); SBQ-R 4 = Suicide Behaviors Questionnaire- Revised item 4 score; SD = Standard Deviation.
p < .05.
p < .01.
3.1. Moderation
The overall model was significant (F[5,189] = 5.74, p < .001, r2 = .13). Baseline BDI-II (B = .004, SE = .001, p < .001), baseline BHS (B = .053, SE = .019, p < .01), and the PCL-C change by BHS interaction (B = .003, SE = .001, p = .02; Δr2 = .03) significantly predicted month-one SBQR item-4 FSA likelihood. Conditional effects of PCL-C change on month-one FSA likelihood were significant for individuals at (BHS = 1.88; B = .003, SE = .001, p = .02) and + 1SD (BHS = 3.00; B = .007, SE = .002, p < .01) of the BHS mean, but not — 1 SD of the mean (BHS = .742; B < − .001, SE = .002, p = .95). PCL-C change (B = − .002, SE = .002, p = .34) and intervention condition (B = .014, SE = .018, p = .42) were non-significant predictors.
3.2. Statistical mediation1
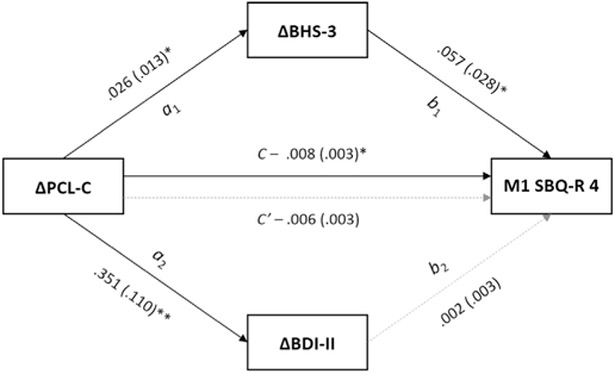
The full model (Fig. 1) accounted for a significant amount of variance in month-one FSA likelihood (r2 = .18; F[4,64] = 3.61, p = .01). The effects of PTSS change on hopelessness change (α1) and depression change (α2) were significant. The effect of hopelessness change on month-one FSA likelihood (b1) was significant, but the effect of depression change on month-one FSA likelihood (b2) was not. The total effect of PTSS change on FSA likelihood (c) was significant, but the direct effect (c’) was not. Indirect effects of PTSS change on month-one FSA likelihood through hopelessness change (B = .002, SE = .001, 95%CI[.0001, .0046]) were significant, but not through depression change (B = .001, SE = .001, 95%CI[− .0010, .0032]). The partial effect of the control variable, condition, on FSA likelihood was not significant (B = .016, SE = .032, p = .62).
Fig. 1.
Multiple statistical mediation model of total and indirect effects of baseline-to-month-one changes in PTSD symptoms (PCL-C) on self-reported likelihood of a future suicide attempt (FSA; SBQ-R item 4) at month-one follow-up. Unstandardized path coefficients are displayed for the mediating effect of baseline-to-month-one hopelessness change (BHS-3; a1, b1) and baseline-to-month-one depression symptom change (BDI-II; a2, b2), with standard errors provided in parentheses. Intervention condition (not depicted) was included as a covariate, but was not significantly related to month-one likelihood of FSA (p = .62). *p < .05; **p < .01.
4. Discussion
This study investigated two ways in which hopelessness may impact the degree to which PTSS reductions following a brief suicide risk-factor intervention influence FSA likelihood. Though PTSS reductions were not correlated with FSA likelihood at month-one, moderation analyses revealed that, for individuals at or above the sample hopelessness mean, greater PTSS reductions were significantly related to lower FSA likelihood. As this was a relatively severe sample, mean BHS scores were roughly equivalent to the suggested cutoff indicative of risk for a FSA (Beck et al., 1990). Though, ostensibly, PTSS and suicidality may be more strongly related for individuals high in hopelessness, the association between PTSS reductions and lower likelihood of FSA is noteworthy; specifically, because these individuals are most at risk for FSAs. Therefore, identifying trauma victims high in hopelessness is important given their risk for suicide, but also because treating PTSS offers subsequent benefits for reducing suicidality.
Moreover, among individuals high in hopelessness for whom baseline suicide risk was elevated, hopelessness changes significantly mediated the relationship between PTSS changes and FSA likelihood. This extends findings that hopelessness changes mediate the effect of CPT on PTSS, which were suggested to occur via indirect effects of CPT on cognitive schema associated with hopelessness (Gallagher and Resick, 2012). Though the intervention in this study differs from CPT could be hypothesized. For instance, initial PTSS relief may reduce hopelessness regarding one's prospect of improved mental health, which in turn would render suicide less desirable. Notably, changes in hopelessness significantly mediated the PTSS-suicide relationship, while change in depression did not. Though hopelessness is a common feature of PTSD and depression, it may operate as an independent mechanism through which suicide intent is reduced. With further replication and extension, this finding holds relevance for informing approaches to treatment for patients suffering comorbid PTSD and suicidality.
Several methodological limitations must be considered. The full BHS was unavailable in this data set, though initial evidence suggests the 3-item version is comparable to the constructs discussed in this investigation. FSA likelihood was indexed via a single, albeit validated, item, which presents issues of measurement error. In the interest of measuring self-reported FSA likelihood only, we make no claims as to whether these results extend to other behaviors (e.g., ideation, plans). During a limited follow-up period, hopelessness and PTSS were measured simultaneously, allowing tests of statistical mediation but not temporal mediation, which would better indicate the mechanistic function of hopelessness in PTSS reduction and suicidality. The intervention conditions were not PTSD-specific. Further research should attempt to replicate these findings using PTSD-specific treatments, though the current data suggest multiple treatment formats may yield the observed effects. These results should also be extended to additional suicide behaviors (e.g., ideation, actual attempts), over increased follow-up duration.
These limitations notwithstanding, this study marks an initial investigation of the complex role hopelessness may play as a psychological determinant of the relationship between PTSS and suicide among trauma-exposed treatment-seekers. Critically, these findings point to the importance of identifying individuals with a trauma history and elevated hopelessness; if not because these two factors increase risk for suicide, but moreover, mitigating PTSS and hopelessness appear to influence likelihood of FSAs. Best practices for evidence-based PTSD treatments should be considered for those with comorbid suicide risk (Foa et al., 2008). For patients whom degree of suicide intent may preclude initiating PTSD-specific treatment, this study suggests supplemental interventions may be useful for reducing suicide risk in conjunction with, and potentially through, hopelessness and PTSS.
Acknowledgments
Role of the funding source
This research was supported by the Military Suicide Research Consortium (MSRC), funded through the Office of the Assistant Secretary of Defense for Health Affairs (W81XWH-10-2-0181/FSU 030969). Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the MSRC or the Department of Defense.
Footnotes
A separate mediation model did not support PTSS change as a mediator of the relationship between hopelessness change and likelihood of future SAs.
References
- Beck AT, 1986. Hopelessness as a predictor of eventual suicide. Ann. N. Y. Acad. Sci 487 (1), 90–96. 10.1111/j.1749-6632.1986.tb27888.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA, 1990. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am. J. Psychiatry 147 (2), 190–195. 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A, 1975. Hopelessness and suicidal behavior: an overview. JAMA 234 (11), 1146–1149. 10.1001/jama.1975.03260240050026. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK, 1996. Beck Depression Inventory-II. San Antonio, TX, pp. 78204–72498. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L, 1974. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol. 42 (6), 861. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC], 2016. WISQARS; Web-based Injury Statistics Query and Reporting System. [Google Scholar]
- Cox KS, Mouilso ER, Venners MR, Defever ME, Duvivier L, Rauch SAM, Tuerk PW, 2016. Reducing suicidal ideation through evidence-based treatment for post-traumatic stress disorder. J. Psychiatr. Res 80, 59–63. 10.1016/j-jpsychires.2016.05.011. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL, 2015. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV). American Psychiatric Association, Arlington, VA. [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, Cohen JA, 2008. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. Guilford Press, New York, NY. [Google Scholar]
- Gallagher MW, Resick PA, 2012. Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: preliminary evidence for the differential effects of hopelessness and habituation. Cogn. Ther. Res 36 (6), 750–755. 10.1007/s10608-011-9423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradus JL, Suvak MK, Wisco BE, Marx BP, Resick PA, 2013. Treatment of posttraumatic stress disorder reduces suicidal ideation. Depress. Anxiety 30 (10), 1046–1053. 10.1002/da.22117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, Mathews A, Dalgleish T, Mackintosh B, 2006. Positive interpretation training: effects of mental imagery versus verbal training on positive mood. Behav. Ther 37 (3), 237–247. 10.1016/j.beth.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Hoerster KD, Varra A, Vannoy S, Felker B, Hunt S, 2011. Hopelessness and suicidal ideation in Iraq and Afghanistan war Veterans reporting subthreshold and threshold posttraumatic stress disorder. J. Nerv. Ment. Dis 199 (4), 272–275. 10.1097/NMD.0b013e3182124604. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Pennington ML, Cammarata CM, Leto F, Ostiguy WJ, Gulliver SB, 2016. Is cumulative exposure to suicide attempts and deaths a risk factor for suicidal behavior among firefighters? A preliminary study. Suicide Life-Threat. Behav 46 (6), 669–677. 10.1111/sltb.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX, 2001. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 8 (4), 443–454. 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Panagioti M, Gooding P, Tarrier N, 2009. Post-traumatic stress disorder and suicidal behavior: a narrative review. Clin. Psychol. Rev 29 (6), 471–482. 10.1016/j.cpr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Ringer FB, Soberay KA, Roger ML, Hagan CR, Chu C, Schneider M, Podlogar MC, Witte T, Holm-Denoma J, Plant EA, Gutierrez PM, Joiner TE, 2017. Initial validation of brief measures of suicide risk factors: common data elements used by the Military Suicide Research Consortium. Psychol. Assess, 10.1037/pas0000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, Capron DW, 2017. A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. J. Consult. Clin. Psychol 10.1037/ccp0000195. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Taylor K, Gooding P, 2008. Cognitive-behavioral interventions to reduce suicide behavior. Behav. Modif. 32 (1), 77–108. 10.1177/0145445507304728. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Huska JA, Keane TM, 1991. PCL-C for DSM-IV. National Center for PTSD-Behavioral Science Division, Boston. [Google Scholar]