Abstract
This study incorporates intersectionality theory to address potential effects of age on other documented risk factors for current smoking and menthol cigarette use in young adults aged 18–34 using Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study (2013–2014). We explored known correlates of current cigarette and menthol cigarette smoking and interaction analyses by age group (18–24 vs. 25–34), accounting for survey weighting. Use of non-cigarette tobacco products and e-cigarettes was characterized among current cigarette smokers. Young adults experience multiple vulnerabilities to smoking beyond age and some of these known risk factors for smoking place those aged 18–24 at different risk of cigarette smoking compared to their 25–34 year old counterparts. These include lower odds of cigarette smoking by age for sex (female; AOR = 0.62 in those aged 18–24 vs. 0.72 in those aged 25–34) and Hispanic ethnicity (vs. White; AOR = 0.77 vs. 0.45), and higher odds of smoking among past 30-day alcohol users aged 18–24 vs. 25–34 (AOR = 1.62 vs. 1.32). Correlations between lower education and smoking were nearly two-fold higher in 25–34 than 18–24 year olds. Having any medical comorbidity had opposite effects on current smoking by age (18–24 positive correlation, AOR = 1.17; 25–34 negative correlation, AOR = 0.84). Lower education was correlated with menthol cigarette use among young adult smokers. This study suggests that higher smoking prevalence among young adults is associated with the intersection of multiple vulnerabilities to smoking.
Keywords: Socioeconomic factors, Health status disparities, Smoking, Tobacco use, Young adult
1. Introduction
Despite historic declines in adult cigarette smoking prevalence in the U.S., reductions have not occurred equally throughout the population (Jamal et al., 2016; U.S. National Cancer Institute, 2017). As of 2015, one of the groups in which smoking prevalence estimated from the National Health Interview Survey (NHIS) remained higher was younger adults (Jamal et al., 2016). Findings from the 2013–2014 Population Assessment of Tobacco and Health (PATH) Study support differences in tobacco use by age with higher prevalence of most tobacco and e-cigarette product use in young adults aged 18–24 compared to adults aged 25 or older (Kasza et al., 2017). This coincides with recent changes in the timing of smoking onset with greater uptake of cigarette smoking occurring in young adulthood than in adolescence (Thompson et al., 2017).
Young adulthood is a distinct and important developmental period, typically spanning ages 18–29 (Arnett, 2000, 2001) marked by a period of heightened vulnerability to escalation and persistence of substance use (Arnett, 2005; Staff et al., 2010; Sussman and Arnett, 2014). It is also a period that often involves psychological distress and significant changes in social and environmental factors as young adults transition from living at home and attending school to living independently (Bonnie et al., 2014). As a result, young adults concurrently experience multiple known risk factors for cigarette smoking and these risk factors may coincide to produce greater risk for smoking among certain subgroups (U.S. National Cancer Institute, 2017). Additionally, the relationship between educational attainment and cigarette smoking may differ in young adults, as many are in the midst of completing their education (Williams et al., 2017).
Intersectionality theory posits that societies are defined by social divisions across multiple axes, including race, class, and gender, that influence each other (Collins and Bilge, 2016). Health disparities research, informed by intersectionality, may help to uncover how these axes of social identities co-occur to produce increased risk for given health behaviors or outcomes (López and Gadsden, 2016). Previous work has highlighted that education, race/ethnicity, and gender act summatively to increase smoking risk in vulnerable populations (Higgins et al., 2016). However, in line with standard biomedical approaches (Kelly, 2009), many population studies have largely focused on individual risk factors for smoking, identifying increased risk in young adults (Jamal et al., 2016; Kasza et al., 2017; Phillips et al., 2017) and within young adults, by sociodemographic characteristics (Green et al., 2007; Lariscy et al., 2013; Rath et al., 2013; U.S. Department of Health and Human Services, 2012; Villanti et al., 2017b). Studies in younger adults also identify relationships between medical comorbidities (e.g., cancer, Kaul et al., 2016), mental illness (Smith et al., 2014), substance use (Cohn et al., 2015) and smoking.
One potential reason for higher smoking prevalence in younger adults may be use of menthol cigarettes. Menthol cigarette consumption (Delnevo et al., 2014) and prevalence have remained largely stable over time in both young adults and adults (Giovino et al., 2015; Villanti et al., 2016) despite rapid declines in non-menthol cigarette consumption and prevalence. As a result, menthol cigarette use has eclipsed non-menthol use in young adults (Villanti et al., 2016). Risk factors for menthol cigarette use and cigarette smoking are similar in youth adults (Cohn et al., 2016a; Rath et al., 2016). However, while males and white young adults have a higher prevalence of cigarette smoking (U.S. Department of Health and Human Services, 2012), correlates of menthol versus non-menthol cigarette use include being female and Black (Rath et al., 2016).
The goal of this study was to examine whether there were unique risk factors for cigarette smoking and menthol cigarette use in young adults aged 18–24 compared to 25–34 and how risk factors combine within these age classes. This approach incorporates intersectionality theory to underscore potential interaction effects of age on other documented risk factors for cigarette smoking and menthol cigarette use in young adults aged 18–34. It supplements traditional regression modeling with classification and regression tree (CART) analysis to examine the relative contribution of these factors in explaining risk for smoking by age group.
2. Methods
Data are from Wave 1 of the PATH Study conducted from September 12, 2013 to December 15, 2014. The PATH Study is a nationally-representative, longitudinal cohort study of 45,971 adults and youth in the US, ages 12 years and older. The National Institutes of Health, through the National Institute on Drug Abuse, is partnering with the Food and Drug Administration’s Center for Tobacco Products to conduct the PATH Study under a contract with Westat. The PATH Study used Audio-Computer Assisted Self-Interviews (ACASI) available in English and Spanish to collect information on tobacco-use patterns and associated health behaviors. This analysis draws from the 32,320 Adult Interviews (ages 18 years and older), focusing on a subpopulation of young adults aged 18–34 (n = 15,448). Recruitment employed addressbased, area-probability sampling, using an in-person household screener to select youths and adults. Adult tobacco users, young adults ages 18 to 24 and African Americans were oversampled relative to population proportions. The weighting procedures adjusted for oversampling and nonresponse; combined with the use of a probability sample, the weighted data allow the estimates produced by Wave 1 of the PATH Study to be representative of the non-institutionalized, civilian US population. The weighted response rate for the household screener was 54.0%. Non-response analysis showed few differences with referent national surveys. Among households that were screened, the overall weighted response rate was 74.0% for the Adult Interview and 78.4% for the Youth Interview. Further details regarding the PATH Study design and methods are available elsewhere (Hyland et al., 2017); Wave 1 questionnaires and information on accessing the data are available at https://doi.org/10.3886/ICPSR36231. The PATH Study was conducted by Westat and approved by Westat’s Institutional Review Board.
2.1. Measures
2.1.1. Cigarette use
Current smoking was defined as having ever smoked cigarettes and currently smoking cigarettes some days or every day. Current established smokers had also smoked at least 100 cigarettes in their lifetime; current experimental smokers did not meet that threshold. Similarly, former cigarette smokers were defined as having ever used the product and not smoking at the time of the survey. Former established smokers had also smoked at least 100 cigarettes in their lifetime; former experimental smokers had smoked at least all or part of a cigarette but < 100 cigarettes. Never users were defined as those who reported never having smoked cigarettes, even one or two puffs. Westat-derived variables for each of these states were combined to create a single variable to describe cigarette smoking with five mutually-exclusive categories: never use, former experimental use, former established use, current experimental use, and current established use.
2.1.2. Menthol cigarette use
Current established smokers of manufactured and roll-your-own cigarettes were asked whether their regular brand was “flavored to taste like menthol or mint” (yes/no). Respondents answering yes were classified as current menthol cigarette smokers.
2.1.3. Risk factors for cigarette smoking
Sociodemographic variables used in these analyses included selfreported age group (18–24 and 25–34), gender, sexual orientation (heterosexual/straight and lesbian, gay, bisexual, or questioning (LGBQ)), race/ethnicity, educational attainment, poverty status, and region. Past 30-day substance use (alcohol, marijuana, heroin, cocaine, stimulants, prescription drugs) was also assessed. Respondents reporting any heart condition, any lung condition, diabetes, sugar diabetes, high blood sugar, or borderline diabetes, or cancer were classified as having medical comorbidities. Respondents also completed the Global Appraisal of Individual Needs -Short Screener (GAIN-SS; Dennis et al., 2006), which measures severity of symptoms of internalizing problems (e.g., depression, anxiety, trauma), externalizing problems (e.g., attention deficits, hyperactivity, impulsivity, conduct problems), and substance use problems (e.g., dependence) in the past year (i.e., 0–1 symptoms (low), 2–3 symptoms (moderate), and 4/4+ symptoms (high), depending on the scale).
2.2. Statistical analyses
Analyses were conducted using SVY procedures in Stata/MP version 15.1 using balanced repeated replication (BRR) replicate weights and Fay’s adjustment. Bivariate analyses, including crude logistic regression models, examined the correlation between smoking risk factors and age group, in addition to cigarette smoking status and age group. Next, multivariable logistic regression models were run stratified by age group to examine correlations between smoking risk factors and two outcomes: 1) current cigarette smoking (full sample) and 2) current menthol cigarette use (current established cigarette smokers). Post-hoc interaction models examined whether the magnitude of the correlation between each risk factor and smoking differed significantly by age group, controlling for all other variables in the model. All multivariable models included sex, sexual orientation, race/ethnicity, education, region, past 30-day alcohol, marijuana, and other drug use, any medical comorbidity, and the GAIN-SS subscales for internalizing and externalizing behavior and substance use problems. Poverty status was excluded from multivariable models due to the amount of missing data (9.3%), though sensitivity analyses examined the likely effect of this exclusion on study results.
Classification and regression tree (CART) analysis (Breiman et al., 1984; Lemon et al., 2003) was conducted to supplement regression modeling, using all smoking risk factors to predict current smoking and menthol cigarette use as done in earlier work on the intersection of risk factors for smoking in the U.S. adult population (Higgins et al., 2016). CART analysis is a nonparametric procedure for dividing a population of interest into mutually exclusive subgroups (risk factor profiles) based on a dependent variable of interest (e.g., current smoking) and, in the process, identifying independent variables with the most explanatory power in accounting for that dependent variable within each subgroup. The tree was built using R’s rpart package (R Core Team, 2017; Therneau et al., 2018) and the classification method, given the binary outcome. We included person-level survey weights, but could not uti-lize replicate weights as done in the multivariable models. Fully saturated trees were produced initially for each age group (18–24 and 25–34), and then pruned by selecting the complexity parameter that minimized cross-validation error to identify the risk factors with the greatest effect on smoking behavior.
3. Results
Participant characteristics are presented in Table 1. Approximately half of young adults aged 18–34 were male and 7.8% were lesbian, gay, bisexual or questioning (LGBQ). More than half (56.8%) were white, 39.1% had a high school education or less, and 36.8% lived below the poverty level. A quarter of young adults (24.6%) lived in the West, 37.3% in the Midwest, 21.4% in the South, and 16.8% in the Northeast. Prevalence of past 30-day substance use was 57.3% for alcohol, 13.4% for marijuana, and 5.8% for any other drugs; 21% (21.4%) were moderate or high on the GAIN-SS substance use scale. A larger proportion of young adults were moderate or high on the GAIN-SS internalizing behavior (40.2%) or externalizing behavior (43.1%) subscales. The prevalence of current cigarette smoking was 27.1% (25.5% in 18–24, 28.4% in 25–34) in young adults, with 40.9% reporting never cigarette use.
Table 1.
Characteristics of young adults aged 18–34, Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014.
| Aged 18–24 (n = 9110; 42.3%) |
Aged 25–34 (n = 6338; 57.7%) |
Total (n = 15,448) |
Aged 18–24 vs. 25–34 | ||
|---|---|---|---|---|---|
| % | % | % | OR | (95% CI) | |
| Sex | |||||
| Male | 50.2 | 50.5 | 50.4 | Ref. | |
| Female | 49.8 | 49.5 | 49.6 | 1.01 | (0.97, 1.06) |
| Sexual orientation | |||||
| Heterosexual/straight | 91.2 | 93.0 | 92.2 | Ref. | |
| LGBQ | 8.8 | 7.0 | 7.8 | 1.29 | (1.12, 1.49) |
| Race/ethnicity | |||||
| White | 54.8 | 58.2 | 56.8 | Ref. | |
| Black | 13.3 | 12.4 | 12.8 | 1.14 | (1.02, 1.27) |
| Other | 11.2 | 9.4 | 10.2 | 1.26 | (1.04, 1.53) |
| Hispanic | 20.7 | 19.9 | 20.2 | 1.10 | (1.00, 1.22) |
| Education | |||||
| Less than high school | 10.8 | 9.2 | 9.9 | 2.90 | (2.55, 3.31) |
| High school graduate/GED | 32.8 | 26.7 | 29.2 | 3.04 | (2.74, 3.38) |
| Some college/associate’s degree | 43.2 | 31.5 | 36.4 | 3.40 | (3.01, 3.84) |
| Bachelor’s/advanced degree | 13.2 | 32.7 | 24.5 | Ref. | |
| Poverty status | |||||
| Below poverty level (< 100% of poverty guideline) | 47.4 | 29.6 | 36.8 | 2.14 | (1.95, 2.36) |
| At or above poverty level (≥100% of poverty guideline) | 52.6 | 70.4 | 63.2 | Ref. | |
| Region | |||||
| Northeast | 17.2 | 16.5 | 16.8 | Ref. | |
| South | 20.6 | 21.9 | 21.4 | 0.90 | (0.77, 1.04) |
| Midwest | 37.8 | 36.9 | 37.3 | 0.98 | (0.87, 1.10) |
| West | 24.4 | 24.7 | 24.6 | 0.94 | (0.82, 1.08) |
| Past 30-day alcohol use | |||||
| No | 45.7 | 40.7 | 42.7 | Ref. | |
| Yes | 54.3 | 59.3 | 57.3 | 0.82 | (0.74, 0.90) |
| Past 30-day marijuana use | |||||
| No | 82.4 | 89.8 | 86.6 | Ref. | |
| Yes | 17.6 | 10.2 | 13.4 | 1.87 | (1.65, 2.12) |
| Past 30-day use of any other drugs | |||||
| No | 93.9 | 94.3 | 94.2 | Ref. | |
| Yes | 6.1 | 5.7 | 5.8 | 1.07 | (0.93, 1.23) |
| Medical comorbidities | |||||
| No | 76.1 | 71.9 | 73.7 | Ref. | |
| Yes | 23.9 | 28.1 | 26.3 | 0.80 | (0.73, 0.88) |
| Internalizing behavior | |||||
| Low | 53.7 | 64.3 | 59.8 | Ref. | |
| Moderate | 26.8 | 21.6 | 23.8 | 1.48 | (1.34, 1.64) |
| High | 19.5 | 14.1 | 16.4 | 1.65 | (1.48, 1.84) |
| Externalizing behavior | |||||
| Low | 49.2 | 62.5 | 56.9 | Ref. | |
| Moderate | 30.1 | 24.7 | 27.0 | 1.55 | (1.41, 1.70) |
| High | 20.8 | 12.8 | 16.2 | 2.07 | (1.83, 2.34) |
| Substance use scale | |||||
| Low | 76.0 | 80.5 | 78.6 | Ref. | |
| Moderate | 17.0 | 14.0 | 15.3 | 1.29 | (1.16, 1.43) |
| High | 7.0 | 5.5 | 6.1 | 1.35 | (1.17, 1.55) |
| Cigarette smoking status | |||||
| Never | 46.9 | 36.5 | 40.9 | Ref. | |
| Former experimental | 23.0 | 22.3 | 22.6 | 0.81 | (0.71, 0.91) |
| Former established | 4.6 | 12.8 | 9.3 | 0.28 | (0.24, 0.33) |
| Current experimental | 5.9 | 3.5 | 4.5 | 1.29 | (1.10, 1.51) |
| Current established | 19.6 | 24.9 | 22.6 | 0.62 | (0.55, 0.68) |
Missing: Sex (0.05%), sexual orientation (1.4%), race/ethnicity (0%), education (0.6%), poverty status (9.4%), region (0%), past 30-day alcohol use (3.6%), past 30-day marijuana use (1.0%), past 30-day any other drug use (0.1%), medical comorbidities (0.5%), internalizing behavior (0%), externalizing behavior (0%), substance use scale (0%), cigarette smoking status (0.3).
3.1. Correlation between smoking risk factors and age group
Bivariate analyses highlighted differences in the distribution of smoking risk factors by age group (18–24 vs. 25–34; Table 1). There were higher odds of being LGBQ (vs. heterosexual), black or other race (vs. white), having lower educational attainment, living below the poverty level (vs. above), and having higher internalizing and externalizing behaviors for 18–24 year olds compared to 25–34 year olds. Higher substance use scale scores and past 30-day marijuana use were positively correlated with being 18–24 as well, though past 30-day alcohol was negatively correlated with being in the younger age group. Having any medical comorbidity was also negatively correlated with being 18–24 versus 25–34. Former (experimental and established) and current established cigarette smoking were negatively correlated with younger age; however, the odds of current experimental smoking were higher in those aged 18–24 compared to those aged 25–34 (OR = 1.29).
3.2. Intersection of age group and smoking risk factors on current cigarette smoking
Table 2 presents correlates of current cigarette smoking, stratified by age group. In both age groups, males (vs. females), whites (vs. blacks and Hispanics), LGBQ respondents (vs. heterosexual), those with less than BA/Advanced degree (vs. BA/Advanced degree), past 30-day substance users (vs. non-users), and those with higher scores on the substance use and internalizing behavior scales had higher odds of current smoking. There were three differences in correlates between age groups: first, residing in the Midwest was positively correlated with current smoking in 18–24 year olds but not 25–34 year olds while residing in the West was negatively correlated with smoking in 25–34 year olds but not 18–24 year olds. Second, having any medical comorbidity was positively correlated with smoking in 18–24 year olds and negatively correlated with smoking in 25–34 year olds. Third, higher externalizing behavior was negatively correlated with smoking in 18–24 year olds, but had no relationship in 25–34 year olds. Sensitivity analyses showed that poverty status was positively correlated with current cigarette smoking in both models, but it had minimal impact on the magnitude of most estimates.
Table 2.
Intersection of age group and current cigarette smoking among young adults aged 18–34, Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014.
| Current cigarette smokers, aged 18–24 (n=3236; 25.5%) |
Current cigarette smoking vs. never/former cigarette smoking among 18–24year olds (n=9089) |
Current cigarette smokers, aged 25–34 (n=2948; 28.4%) |
Current cigarette smoking vs. never/former cigarette smoking among 25–34year olds (n=6320) |
|||
|---|---|---|---|---|---|---|
| % | AOR | (95% CI) | % | AOR | (95% CI) | |
| Sex | ||||||
| Male | 59.9 | Ref. | 59.2 | Ref. | ||
| Female | 40.1 | 0.62 | (0.55, 0.69) | 40.8 | 0.72 | (0.61, 0.84) |
| Sexual orientation | ||||||
| Heterosexual/straight | 86.9 | Ref. | 90.4 | Ref. | ||
| LGBQ | 13.1 | 1.67 | (1.38, 2.01) | 9.6 | 1.42 | (1.09, 1.86) |
| Race/ethnicity | ||||||
| White | 59.6 | Ref. | 63.6 | Ref. | ||
| Black | 12.1 | 0.68 | (0.58, 0.81) | 14.0 | 0.66 | (0.54, 0.82) |
| Other | 8.9 | 0.86 | (0.67, 1.11) | 6.9 | 1.01 | (0.71, 1.43) |
| Hispanic | 19.4 | 0.77 | (0.66, 0.88) | 15.5 | 0.45 | (0.36, 0.56) |
| Education | ||||||
| Less than high school | 15.3 | 4.56 | (3.60, 5.78) | 13.8 | 9.96 | (7.76, 12.77) |
| High school graduate/GED | 39.3 | 3.58 | (2.95, 4.34) | 39.1 | 7.34 | (5.95, 9.06) |
| Some college/associate’s degree | 38.4 | 2.01 | (1.69, 2.40) | 34.7 | 3.89 | (3.25, 4.65) |
| Bachelor’s/advanced degree | 7.0 | Ref. | 12.4 | Ref. | ||
| Region | ||||||
| Northeast | 16.6 | Ref. | 17.0 | Ref. | ||
| South | 21.8 | 1.16 | (0.91, 1.47) | 23.6 | 1.03 | (0.85, 1.26) |
| Midwest | 40.1 | 1.24 | (1.01, 1.53) | 40.5 | 1.01 | (0.82, 1.25) |
| West | 21.4 | 0.81 | (0.63, 1.03) | 18.9 | 0.55 | (0.45, 0.67) |
| Past 30-day alcohol use | ||||||
| No | 34.0 | Ref. | 35.8 | Ref. | ||
| Yes | 66.0 | 1.62 | (1.40, 1.87) | 64.2 | 1.32 | (1.11, 1.56) |
| Past 30-day marijuana use | ||||||
| No | 62.8 | Ref. | 76.5 | Ref. | ||
| Yes | 37.2 | 2.96 | (2.55, 3.44) | 23.5 | 3.87 | (3.09, 4.86) |
| Past 30-day use of any other drugs | ||||||
| No | 87.4 | Ref. | 88.0 | Ref. | ||
| Yes | 12.6 | 1.65 | (1.30, 2.09) | 12.0 | 2.24 | (1.68, 2.97) |
| Medical comorbidities | ||||||
| No | 73.1 | Ref. | 69.5 | Ref. | ||
| Yes | 26.9 | 1.17 | (1.02, 1.35) | 30.5 | 0.84 | (0.73, 0.98) |
| Internalizing behavior | ||||||
| Low | 45.5 | Ref. | 51.9 | Ref. | ||
| Moderate | 25.7 | 1.03 | (0.90, 1.17) | 23.8 | 1.44 | (1.19, 1.76) |
| High | 28.8 | 1.71 | (1.48, 1.98) | 24.2 | 2.64 | (2.06, 3.39) |
| Externalizing behavior | ||||||
| Low | 44.2 | Ref. | 69.4 | Ref. | ||
| Moderate | 28.5 | 0.77 | (0.68, 0.87) | 19.6 | 0.82 | (0.67, 1.01) |
| High | 27.3 | 0.79 | (0.66, 0.95) | 11.1 | 0.85 | (0.66, 1.09) |
| Substance use scale | ||||||
| Low | 58.9 | Ref. | 69.4 | Ref. | ||
| Moderate | 25.3 | 1.46 | (1.25, 1.69) | 19.6 | 1.32 | (1.05, 1.65) |
| High | 15.8 | 2.61 | (2.16, 3.16) | 11.1 | 1.61 | (1.13, 2.29) |
Post-hoc analyses supported that the magnitude of the correlations between some risk factors and smoking differed by age group. There were significant interactions for sex (i.e., stronger negative correlation between being female and smoking in 18–24 year olds vs. 25–34 year olds; AOR = 0.83), being Hispanic (i.e., attenuated negative effect of Hispanic ethnicity on smoking in 18–24 year olds compared to 25–34 year olds; AOR = 1.68), education (i.e., smaller magnitude of correlations between lower education and smoking in 18–24 year olds vs. 25–34 year olds; AORs range from 0.53 to 0.54), past 30-day alcohol use (stronger positive correlation in 18–24 vs. 25–34 year olds; AOR = 1.27), medical comorbidities (cross-over effect in 18–24 vs. 25–34; AOR = 1.28), and internalizing behavior (i.e., smaller magnitude of correlation between internalizing behavior in 18–24 vs 25–34 year olds; AOR = 0.74 for moderate, 0.70 for high).
Results from the CART analyses identified the relative contribution of risk factors associated with current smoking in each age group. The pruned tree for young adults aged 18–24 showed past 30-day marijuana use as the most important correlate of current smoking, followed by scoring high on the substance use scale, having a high school education or less, and scoring moderate or high on the internalizing behavior scale (Fig. 1). Smoking prevalence varied 3.5 fold from a low of 20% to a high of 70% across the five risk-factor profiles identified. Among young adults aged 25–34, the strongest correlate of current smoking was having less than a BA/Advanced degree, followed by past 30-day marijuana use, being non-white, living below the poverty level, and having higher internalizing behavior, externalizing behavior and substance use problems, with smoking prevalence varying 7.8 fold from a low of 9% to a high of 70% across 13 different risk-factor profiles (Fig. 2).
Fig. 1.
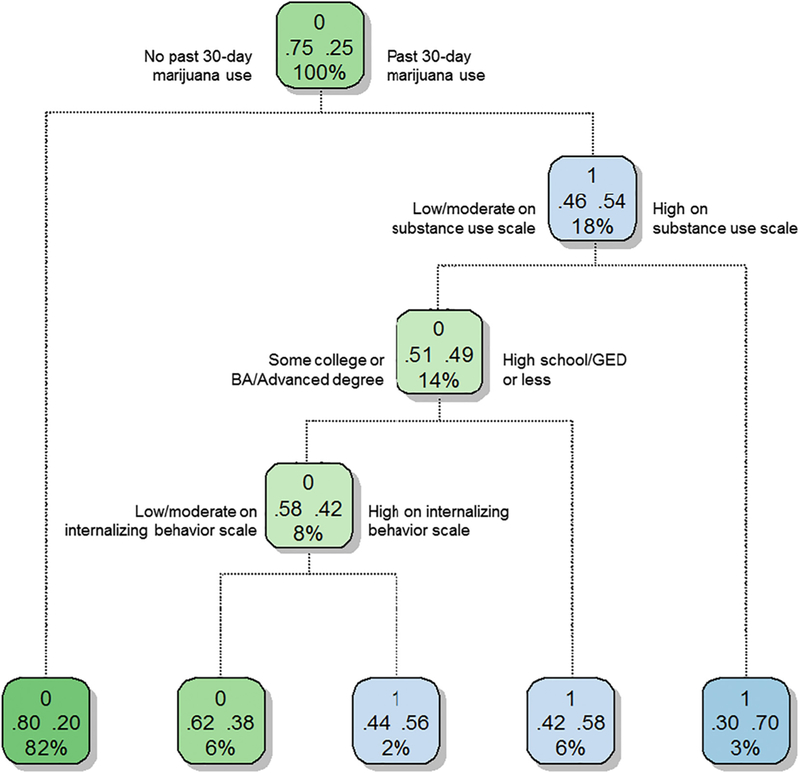
Young adults aged 18–24, Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014. Pruned, weighted classification and regression tree (CART) model of associations between current cigarette smoking and the following risk factors: sex, LGBQ status, race/ethnicity, educational attainment, poverty status, census region, past 30-day alcohol use, past 30-day marijuana use, past 30-day any other drug use, any medical comorbidity, and the GAIN-SS internalizing, externalizing, and substance use scales. Results from a saturated model were “pruned” using CART analytic software to reduce complexity (R Core Team, 2017). Rectangles (nodes) represent smoking prevalence for the entire population (top-most node) or population subgroups (all others nodes). Nodes also list the proportion of the adult population represented. Green nodes depict subpopulations where the majority of the population is non-smokers and blue nodes, subpopulations where the majority of the population is current smokers. Using the root node as an example, 75% of young adults aged 18–24 are non-smokers, 25% current smokers, and this node represents 100% of the U.S. young adults aged 18–24. Lines below nodes represent the binary branching around particular risk factors and risk-factor levels. The bottom row comprises terminal nodes (i.e., final partitioning for a particular subgroup). Terminal nodes contain the same information as the other nodes plus the percent of all adult current smokers represented by that node. Percent of current smokers represented is calculated by the following equation: % total population represented by a node × smoking prevalence in that node/smoking prevalence in the entire study sample × 100. Tallying % current smokers represented across all terminal nodes should equal 100% of smokers in the U.S adult population, save rounding error. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 2.
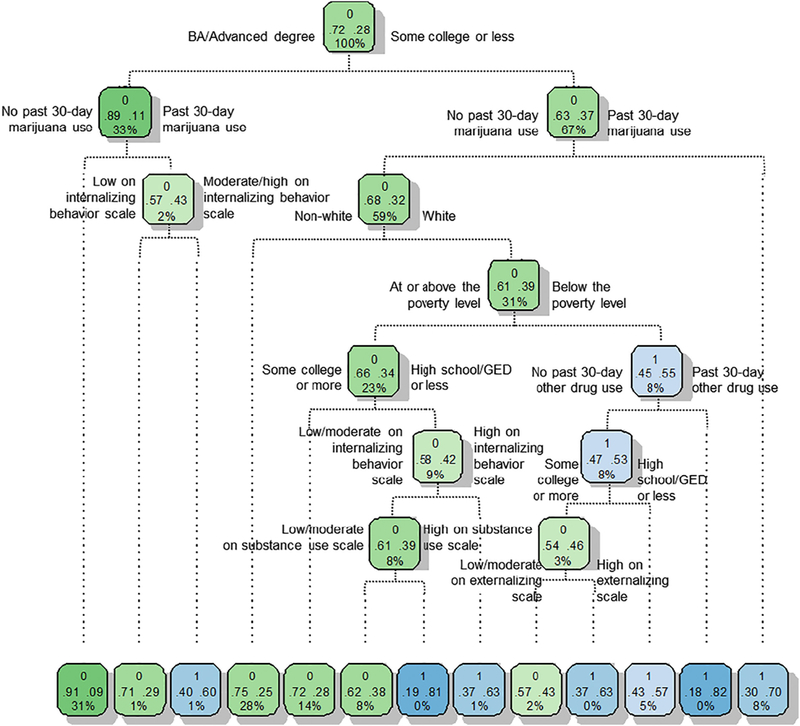
Young adults aged 25–34, Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014. Pruned, weighted classification and regression tree (CART) model of associations between current cigarette smoking and the following risk factors: sex, LGBQ status, race/ethnicity, educational attainment, poverty status, census region, past 30-day alcohol use, past 30-day marijuana use, past 30-day any other drug use, any medical comorbidity, and the GAIN-SS internalizing, externalizing, and substance use scales. Results from a saturated model were “pruned” using CART analytic software to reduce complexity (R Core Team, 2017). Rectangles (nodes) represent smoking prevalence for the entire population (top-most node) or population subgroups (all others nodes). Nodes also list the proportion of the adult population represented. Green nodes depict subpopulations where the majority of the population is non-smokers and blue nodes, subpopulations where the majority of the population is current smokers. Using the root node as an example, 72% of young adults aged 25–34 are non-smokers, 28% current smokers, and this node represents 100% of the U.S. young adults aged 25–34. Lines below nodes represent the binary branching around particular risk factors and risk-factor levels. The bottom row comprises terminal nodes (i.e., final partitioning for a particular subgroup). Terminal nodes contain the same information as the other nodes plus the percent of all adult current smokers represented by that node. Percent of current smokers represented is calculated by the following equation: % total population represented by a node × smoking prevalence in that node/smoking prevalence in the entire study sample × 100. Tallying % current smokers represented across all terminal nodes should equal 100% of smokers in the U.S adult population, save rounding error. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.3. Intersection of age group and smoking risk factors on menthol use within current cigarette smokers
Current female smokers (vs. males), black and Hispanic smokers (vs. whites), and smokers with less than BA/Advanced degree (vs. having a BA/Advanced degree) had greater odds of menthol cigarette use compared to non-menthol use in both age groups (Table 3). Smokers residing in the West had lower odds of using menthol cigarettes in both age groups compared to smokers residing in the Northeast. There were two differences in correlates of menthol cigarette use by age group in young adult smokers: first, smokers residing in the Midwest (vs. Northeast) had lower odds of menthol use in the 25–34 age group. Second, other race was positively correlated with menthol use in 25–34 year old smokers. Sensitivity analyses showed that poverty status was not correlated with menthol cigarette use among current smokers and had minimal effect on estimates in the original model.
Table 3.
Intersection of age group and menthol cigarette smoking among young adult current smokers aged 18–34, Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study, 2013–2014.
| Current menthol cigarette use, aged 18–24 (n = 1316; 47.3%) |
Current menthol vs. non-menthol use among 18–24 year old current established cigarette smokers (n = 2708) |
Current menthol cigarette use, aged 25–34 (n = 1284; 44.7%) |
Current menthol vs. non-menthol use among 25–34 year old current established cigarette smokers (n = 2801) |
|||
|---|---|---|---|---|---|---|
| % | AOR | (95% CI) | % | AOR | (95% CI) | |
| Sex | ||||||
| Male | 53.0 | Ref. | 54.0 | Ref. | ||
| Female | 47.0 | 1.79 | (1.48, 2.17) | 46.0 | 1.56 | (1.29, 1.89) |
| Sexual orientation | ||||||
| Heterosexual/straight | 84.6 | Ref. | 89.6 | Ref. | ||
| LGBQ | 15.4 | 1.25 | (0.94, 1.67) | 10.4 | 1.07 | (0.75, 1.53) |
| Race/ethnicity | ||||||
| White | 57.7 | Ref. | 54.4 | Ref. | ||
| Black | 16.1 | 5.01 | (3.38, 7.42) | 22.9 | 11.20 | (7.47, 16.81) |
| Other | 7.0 | 1.12 | (0.73, 1.73) | 6.0 | 1.73 | (1.19, 2.52) |
| Hispanic | 19.1 | 1.95 | (1.49, 2.56) | 16.7 | 2.63 | (1.90, 3.65) |
| Education | ||||||
| Less than high school | 16.6 | 2.38 | (1.49, 3.81) | 12.2 | 2.08 | (1.32, 3.28) |
| High school graduate/GED | 39.1 | 1.69 | (1.14, 2.52) | 40.6 | 2.12 | (1.44, 3.13) |
| Some college/associate’s degree | 39.8 | 1.80 | (1.19, 2.72) | 39.6 | 2.27 | (1.59, 3.23) |
| Bachelor’s/advanced degree | 4.5 | Ref. | 7.6 | Ref. | ||
| Region | ||||||
| Northeast | 18.2 | Ref. | 19.1 | Ref. | ||
| South | 22.6 | 0.84 | (0.57, 1.24) | 22.9 | 0.69 | (0.48, 1.01) |
| Midwest | 42.9 | 0.91 | (0.63, 1.33) | 43.8 | 0.73 | (0.55, 0.98) |
| West | 16.3 | 0.60 | (0.42, 0.87) | 14.3 | 0.44 | (0.31, 0.64) |
| Past 30-day alcohol use | ||||||
| No | 33.2 | Ref. | 36.2 | Ref. | ||
| Yes | 66.8 | 1.10 | (0.89, 1.36) | 63.8 | 0.94 | (0.77, 1.15) |
| Past 30-day marijuana use | ||||||
| No | 64.6 | Ref. | 76.2 | Ref. | ||
| Yes | 35.4 | 0.83 | (0.67, 1.02) | 23.8 | 0.93 | (0.74, 1.16) |
| Past 30-day use of any other drugs | ||||||
| No | 87.8 | Ref. | 87.8 | Ref. | ||
| Yes | 12.2 | 0.99 | (0.72, 1.36) | 12.2 | 1.03 | (0.79, 1.34) |
| Medical comorbidities | ||||||
| No | 70.9 | Ref. | 68.0 | Ref. | ||
| Yes | 29.1 | 1.13 | (0.91, 1.40) | 32.0 | 1.09 | (0.89, 1.32) |
| Internalizing behavior | ||||||
| Low | 43.1 | Ref. | 51.9 | Ref. | ||
| Moderate | 27.6 | 1.04 | (0.79, 1.38) | 23.1 | 0.90 | (0.72, 1.13) |
| High | 29.4 | 0.94 | (0.72, 1.23) | 25.0 | 1.11 | (0.85, 1.46) |
| Externalizing behavior | ||||||
| Low | 44.5 | Ref. | 68.8 | Ref. | ||
| Moderate | 29.1 | 0.88 | (0.70, 1.10) | 20.3 | 0.86 | (0.69, 1.06) |
| High | 26.4 | 0.92 | (0.69, 1.25) | 10.9 | 0.82 | (0.62, 1.08) |
| Substance use scale | ||||||
| Low | 59.3 | Ref. | 68.8 | Ref. | ||
| Moderate | 22.6 | 0.88 | (0.71, 1.10) | 20.3 | 1.26 | (0.94, 1.68) |
| High | 18.1 | 1.19 | (0.91, 1.56) | 10.9 | 1.07 | (0.75, 1.53) |
The pruned tree from CART analyses in current smokers highlighted non-white race/ethnicity as the most important correlate of menthol cigarette use in 18–24 year olds, followed by being female, living in the Northeast, Midwest or South, and having less than a BA/Advanced degree (Supplemental Fig. 1). Among young adult smokers aged 25–34, the strongest correlate of menthol cigarette use was again being nonwhite, followed by having less than a BA/Advanced degree with no other predictors in the model (Supplemental Fig. 2).
Post hoc interaction analysis showed a significant interaction for black race (i.e., smaller magnitude of correlations between black race and menthol use in 18–24 year old smokers vs. 25–34 year old smokers; AOR = 0.42). Scoring moderate (vs. low) on the substance use scale was correlated with a lower odds of menthol cigarette use in 18–24 year old smokers and a higher odds of menthol cigarette use in 25–34 year old smokers; AOR = 0.68).
4. Discussion
As reported in national studies of adults (Higgins et al., 2016; Jamal et al., 2016; Phillips et al., 2017), being male, white, LGBQ, having lower education, and reporting higher substance use, internalizing behavior and markers of psychological distress, were positively correlated with current cigarette smoking in the present subgroup of young adults aged 18–34. The present study also provides novel information on differences in the importance and magnitude of these correlates among those aged 18–24 versus 25–34. First, there are greater sex differences in smoking among young adults, with females aged 18–24 having significantly lower odds of smoking than females aged 25–34. Second, while Hispanic young adults are still less likely to smoke than whites in both age groups, this difference was attenuated in the younger age group. Both of these findings are consistent with data showing although there were declines in smoking uptake among white young adult males and females from 2006 to 2013, rates of smoking onset increased over this period among black and Hispanic young adult males and declined more slowly in black and Hispanic young adult females compared to whites (Thompson et al., 2017). Third, the magnitude of the positive correlation between lower education and current cigarette smoking was almost two-fold higher in the 25–34 year olds than the 18–24 year olds. This may be explained by the younger group being less likely to have completed their education (Williams et al., 2017), but was not previously reported in a study examining the relationship between education and smoking in young adults (Green et al., 2007). Educational attainment less than a BA was the strongest predictor and the only stand-alone risk profile in two prior studies in the overall U.S. adult population perhaps suggesting that its predictive utility grows in importance with age (Gaalema et al., in press; Higgins et al., 2016). Fourth, past 30-day alcohol use was more strongly correlated with cigarette smoking in those aged 18–24 than in those aged 25–34, in line with studies in this age group documenting the prevalence of alcohol and cigarette co-use (Cohn et al., 2015; Cohn et al., 2016b), as well as the relationship between alcohol use and social smoking (Lisha et al., 2015; Villanti et al., 2017c). Fifth, the magnitude of the relationship between internalizing behavior and cigarette smoking was greater in the older age group than the 18–24 year olds. This may be attributable to later onset of mood disorders, like depression, though half of lifetime cases of psychiatric disorders start by adolescence and 7% by age 24 (Kessler et al., 2005). Finally, this study provides the first estimates of the relationship between any medical comorbidity and cigarette smoking in young adults, finding opposite effects in the two age groups.
Classification and regression tree analyses support the intersectionality of smoking risk factors in young adults, as seen in the general adult population (Higgins et al., 2016). The strength of this approach is its ability to illustrate how the risk factors of interest intersect corresponding to their relative strengths accounting for large differences in smoking risk, and the associated risk profiles that have the potential to guide targeted tobacco control and regulatory efforts. Past 30-day marijuana use, education, and internalizing behavior explained a large proportion of current smoking in both age groups. The substance use scale was identified as an important correlate of smoking in the 18–24 year olds and race/ethnicity and poverty status were identified as important correlates of smoking in the 25–34 year olds. The strength of the positive association between past 30-day marijuana use in predicting current smoking in both age groups but especially the 18–24 year olds warrants further monitoring in light of the liberalization of marijuana use laws in the U.S. and globally.
Menthol cigarette use is associated with smoking progression, increased nicotine dependence, and reduced smoking cessation and as such, poses a threat to public health (Villanti et al., 2017a). In this study, correlates of menthol cigarette use were largely consistent with previous studies (Rath et al., 2016), documenting higher odds of menthol use in female and non-White young adult smokers. They differed, however, in finding no correlation between being a sexual minority and menthol cigarette use (Rath et al., 2016) and no correlation between psychiatric symptoms and menthol cigarette use in young adult smokers (Cohn et al., 2016a). Novel findings from the current study document significantly higher odds of menthol use among young adult smokers with lower education and the emergence of region as a correlate of menthol cigarette use in young adults. Prior studies have shown no correlation between lower income and menthol cigarette use (Giovino et al., 2015; Villanti et al., 2016). The relationship between education and menthol cigarette use may remain confounded with race/ethnicity given differential exposure to targeted marketing of menthol cigarettes in low-income minority communities (Seidenberg et al., 2010; Widome et al., 2013; Yerger et al., 2007). Potential differences by region are consistent with Reynolds American’s 2016 categorization of the Northeast and South as “core” markets, the Midwest as an “emerging” market, and the West as an “opportunity” market for Newport cigarettes, the country’s leading menthol brand (Reynolds American Inc., 2016).
Limitations of this study include its cross-sectional nature, which precludes conclusions about the directionality of these correlations. Exclusion of poverty status from the multivariable models, while justified based on the proportion of missing data, may have resulted in overestimating the magnitude of the relationships between education and current cigarette smoking. On balance, this study has a number of strengths. It provides a comprehensive examination of smoking risk factors in a large, national sample, rarely included in a single dataset. The PATH Study’s oversampling of young adults allows for greater confidence in the stability of the estimated correlations between these risk factors and the smoking outcomes. Furthermore, the explicit focus on the intersection of age and smoking risk factors in young adults highlights differential effects of certain correlates among those 18–24, a group particularly vulnerable to smoking onset (Thompson et al., 2017) and targeted marketing by tobacco companies (Biener and Albers, 2004; Ling and Glantz, 2002).
5. Conclusions
Young adults experience multiple vulnerabilities to smoking beyond age and some of these known risk factors for smoking (i.e., being male, Hispanic, using alcohol, and having a medical comorbidity) place those aged 18–24 at greater risk of cigarette smoking compared to their 25–34 year old counterparts. In both age groups, smoking was concentrated in those with more than one risk factor and marijuana use, lower education, and internalizing behavior emerged as important correlates of smoking. These data also highlight education as a strong correlate of menthol cigarette use in young adults, which has not been documented in previous work in this age group (Rath et al., 2016). Findings support the importance of intervening on co-use with other substances, particularly alcohol and marijuana, to reduce tobacco use. The high proportion of young adult menthol cigarette users in this study reinforce that banning menthol in cigarettes could reduce tobacco use in this vulnerable group.
Supplementary Material
Acknowledgments
Funding
The authors were supported by the Tobacco Centers of Regulatory Science (TCORS) award P50DA036114 from the National Institute on Drug Abuse and Food and Drug Administration (FDA), the Centers of Biomedical Research Excellence P20GM103644 award from the National Institute of General Medical Sciences, and a grant from the National Institute on Drug Abuse and the Food and Drug Administration, Center for Tobacco Products (U54DA031659). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2018.06.001.
Footnotes
Conflict of interest statement
The authors have no conflicts to declare.
References
- Arnett JJ, 2000. Emerging adulthood. A theory of development from the late teens through the twenties. Am. Psychol 55, 469–480. [PubMed] [Google Scholar]
- Arnett JJ, 2001. Conceptions of the transition to adulthood: perspectives from adolescence through midlife. J. Adult Dev 8, 133–143. [Google Scholar]
- Arnett JJ, 2005. The developmental context of substance use in emerging adulthood. J. Drug Issues 35, 235–254. [Google Scholar]
- Biener L, Albers AB, 2004. Young adults: vulnerable new targets of tobacco marketing. Am. J. Public Health 94, 326–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnie RJ, Stroud C, Breiner H, National Research Council (U.S.) Board on Children, Youth and Families, 2014. Investing in the Health and Well-Being of Young Adults The National Academies Press, Washington, D.C. [PubMed] [Google Scholar]
- Breiman L, Friedman J, Stone CJ, Olshen RA, 1984. Classification and Regression Trees Chapman & Hall/CRC, Boca Raton, FL. [Google Scholar]
- Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, Mermelstein R, 2015. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict. Behav 48, 79–88. [DOI] [PubMed] [Google Scholar]
- Cohn AM, Johnson AL, Hair E, Rath JM, Villanti AC, 2016a. Menthol tobacco use is correlated with mental health symptoms in a national sample of young adults: implications for future health risks and policy recommendations. Tob. Induc. Dis 14 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn AM, Johnson AL, Rath JM, Villanti AC, 2016b. Patterns of the co-use of alcohol, marijuana, and emerging tobacco products in a national sample of young adults. Am. J. Addict 25 (8), 634–640. [DOI] [PubMed] [Google Scholar]
- Collins PH, Bilge S, 2016. Intersectionality Polity Press, Malden, MA. [Google Scholar]
- Delnevo CD, Villanti AC, Giovino GA, 2014. Trends in menthol and non-menthol cigarette consumption in the U.S.A.: 2000–2011. Tob. Control 23, e154–e155. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Chan YF, Funk RR, 2006. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am. J. Addict 15 (Suppl 1), 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaalema DE, Leventhal AM, Priest JS, Higgins ST, in press Understanding individual differences in vulnerability to cigarette smoking will require attention to the intersection of common risk factors. Prev. Med [DOI] [PMC free article] [PubMed]
- Giovino GA, Villanti AC, Mowery PD, Sevilimedu V, Niaura RS, Vallone DM, Abrams DB, 2015. Differential trends in cigarette smoking in the USA: is menthol slowing progress? Tob. Control 24, 28–37. [DOI] [PubMed] [Google Scholar]
- Green MP, McCausland KL, Xiao H, Duke JC, Vallone DM, Healton CG, 2007. A closer look at smoking among young adults: where tobacco control should focus its attention. Am. J. Public Health 97, 1427–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Kurti AN, Redner R, White TJ, Keith DR, Gaalema DE, Sprague BL, Stanton CA, Roberts ME, et al. , 2016. Co-occurring risk factors for current cigarette smoking in a U.S. nationally representative sample. Prev. Med 92, 110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, Taylor K, Crosse S, Fong GT, et al. , 2017. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob. Control 26, 371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM, 2016. Current cigarette smoking among adults -United States, 2005–2015. MMWR Morb. Mortal. Wkly Rep 65, 1205–1211. [DOI] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, et al. , 2017. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med 376, 342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaul S, Veeranki SP, Rodriguez AM, Kuo YF, 2016. Cigarette smoking, comorbidity, and general health among survivors of adolescent and young adult cancer. Cancer 122, 2895–2905. [DOI] [PubMed] [Google Scholar]
- Kelly UA, 2009. Integrating intersectionality and biomedicine in health disparities research. ANS. Adv. Nurs. Sci 32, E42–E56. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE, 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Lariscy JT, Hummer RA, Rath JM, Villanti AC, Hayward MD, Vallone DM, 2013. Race/ethnicity, nativity, and tobacco use among US young adults: results from a nationally representative survey. Nicotine Tob. Res 15, 1417–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W, 2003. Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann. Behav. Med 26, 172–181. [DOI] [PubMed] [Google Scholar]
- Ling PM, Glantz SA, 2002. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am. J. Public Health 92, 908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisha NE, Delucchi KL, Ling PM, Ramo DE, 2015. Prevalence and correlates of social smoking in young adults: comparisons of behavioral and self-identified definitions. Nicotine Tob. Res 17, 1076–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López N, Gadsden VL, 2016. Health Inequities, Social Determinants, and Intersectionality. National Academy of Medicine Perspectives: Expert Voices in Health and Health Care
- Phillips E, Wang TW, Husten CG, Corey CG, Apelberg BJ, Jamal A, Homa DM, King BA, 2017. Tobacco product use among adults-United States, 2015. MMWR Morb. Mortal. Wkly Rep 66, 1209–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team, 2017. R: A Language and Environment for Statistical Computing R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Rath JM, Villanti AC, Rubenstein RA, Vallone DM, 2013. Tobacco use by sexual identity among young adults in the United States. Nicotine Tob. Res 15, 1822–1831. [DOI] [PubMed] [Google Scholar]
- Rath JM, Villanti AC, Williams VF, Richardson A, Pearson JL, Vallone DM, 2016. Correlates of current menthol cigarette and flavored other tobacco product use among U.S. young adults. Addict. Behav 62, 35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds American Inc., 2016. RAI Investor Day: Business Update Reynolds American Inc, London, England. [Google Scholar]
- Seidenberg AB, Caughey RW, Rees VW, Connolly GN, 2010. Storefront cigarette advertising differs by community demographic profile. Am. J. Health Promot 24, e26–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Mazure CM, McKee SA, 2014. Smoking and mental illness in the U.S. population. Tob. Control 23, e147–e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL, Johnston LD, 2010. Substance use changes and social role transitions: proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Dev. Psychopathol 22, 917–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S, Arnett JJ, 2014. Emerging adulthood: developmental period facilitative of the addictions. Eval. Health Prof 37, 147–155. [DOI] [PubMed] [Google Scholar]
- Therneau T, Atkinson B, Ripley B, 2018. rpart: Recursive Partitioning. R Package Version 4.1–12
- Thompson AB, Mowery PD, Tebes JK, McKee SA, 2017. Time trends in smoking onset by sex and race/ethnicity among adolescents and young adults: findings from the 2006–2013 National Survey on Drug Use and Health. Nicotine Tob. Res 20 (3), 312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2012. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta, GA. [Google Scholar]
- U.S. National Cancer Institute, 2017. A Socioecological Approach to Addressing Tobacco-Related Health Disparities National Cancer Institute Tobacco Control Monograph 22. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, Bethesda, MD. [Google Scholar]
- Villanti AC, Mowery PD, Delnevo CD, Niaura RS, Abrams DB, Giovino GA, 2016. Changes in the prevalence and correlates of menthol cigarette use in the USA, 2004–2014. Tob. Control 25, ii14–ii20. [DOI] [PubMed] [Google Scholar]
- Villanti AC, Collins LK, Niaura RS, Gagosian SY, Abrams DB, 2017a. Menthol cigarettes and the public health standard: a systematic review. BMC Public Health 17, 983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanti AC, Johnson AL, Rath JM, 2017b. Beyond education and income: identifying novel socioeconomic correlates of cigarette use in U.S. young adults. Prev. Med 104, 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanti AC, Johnson AL, Rath JM, Williams V, Vallone DM, Abrams DB, Hedeker D, Mermelstein RJ, 2017c. Identifying “social smoking” U.S. young adults using an empirically-driven approach. Addict. Behav 70, 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widome R, Brock B, Noble P, Forster JL, 2013. The relationship of neighborhood demographic characteristics to point-of-sale tobacco advertising and marketing. Ethn. Health 18, 136–151. [DOI] [PubMed] [Google Scholar]
- Williams VF, Smith AA, Villanti AC, Rath JM, Hair EC, Cantrell J, Teplitskaya L, Vallone DM, 2017. Validity of a subjective financial situation measure to assess socioeconomic status in US young adults. J. Publ. Health Manag. Pract 23, 487–495. [DOI] [PubMed] [Google Scholar]
- Yerger VB, Przewoznik J, Malone RE, 2007. Racialized geography, corporate activity, and health disparities: tobacco industry targeting of inner cities. J. Health Care Poor Underserved 18, 10–38. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


