Abstract
The increasing need for pulmonary resection by video‐assisted thoracoscopic surgery (VATS) has presented a greater opportunity to detect small‐sized pulmonary nodules by computed tomography (CT). In cases where it is difficult to identify tumor localization intraoperatively, it is necessary to place the VATS marker near the pulmonary nodules before surgery. Conventional percutaneous or bronchoscopic VATS marker placement under local anesthesia is accompanied by patient pain. We clinically applied a new technique to place VATS markers using a bronchoscope under general anesthesia in a hybrid operating room. Multiple pulmonary nodules were successfully marked and securely excised simultaneously by VATS. This technique enables secure, minimally invasive resection of multiple small‐sized pulmonary nodules without causing distress to the patient.
Keywords: Lung neoplasm, thoracic surgery, video‐assisted tomography, X‐ray computed
Background
Wedge resection under video‐assisted thoracoscopic surgery (VATS) for multiple subcentimeter pulmonary nodules is challenging. In cases of small pulmonary lesions with no change in the visceral pleura, it may be difficult to identify their localization during VATS. To reliably identify such small lung lesions during surgery, a VATS marker is placed in advance percutaneously near the target pulmonary nodule under computed tomography (CT) guidance.
Various VATS marking materials are used, such as hook wire1 and metallic microcoil2 colored dyes, such as indigo carmine and indocyanine green (ICG);3 and radiographic contrast agents, such as barium4 and Iopamiron.5
In addition to the CT‐guided approach of VATS marking,1, 2, 3, 6, 7 bronchoscopic marking has also been proposed.8, 9, 10, 11 The bronchoscopic approach does not injure visceral pleura and therefore can prevent the occurrence of secondary pneumothorax. However, these marking methods are carried out under local anesthesia, which causes patient pain.
In this report, we introduce a newly developed, minimally invasive VATS marking method for micro pulmonary nodules. In a hybrid operating room (OR) under general anesthesia, simultaneous bronchoscopic VATS marking is performed under the guidance of cone beam CT (CBCT) and augmented X‐ray fluoroscopy, thus enabling VATS wedge resection of multiple small pulmonary nodules.
Methods and results
Patients with non‐solid, partly solid, or solid pulmonary nodules with a maximum nodule diameter < 20 mm and without radiological changes in the visceral pleura on CT scheduled for VATS wedge resection were enrolled in this study.
In the hybrid OR, the patient is administered general anesthesia, and the tracheal tube is intubated. The first CBCT (Artis Q, Siemens, Iselin, NJ, USA) is performed to obtain a three‐dimensional (3D) image of the thorax (Fig 1a). Multiple target pulmonary lesions are identified, and the 3D coordinates of each lesion are registered in the system to make them visible on the X‐ray fluoroscopic image so that the position of the lesions is consistently displayed on X‐ray fluoroscopy. The thin bronchoscope (Olympus BF‐P190, Olympus Corporation, Tokyo, Japan) is inserted into the sub‐subsegmental bronchus following the target pulmonary nodule. A transbronchial aspiration cytology (TBAC) needle (Fig 1b) is inserted near the target by X‐ray fluoroscopic guidance (Fig 1c). The TBAC needle tip is pierced into the lung parenchyma (Fig 1d) and 0.05 mL of a 0.025 mg/mL (100 times diluted from the original concentration) ICG/Iopamidol mixture is injected (Fig 1e) using a method reported previously.12 The second CBCT is performed to confirm that the VATS marker has been injected in the vicinity of the lesion (Fig 1f). In a representative case that had three multiple pulmonary nodules in rt. S1, S9, and S7 (Fig 2a–c), VATS markers were injected near the target pulmonary nodules (Fig 2d–f). The right lateral view of the 3DCT image of the right lung shows both target pulmonary nodules (in red) and VATS markers (in green) for reference during surgery (Fig 2g). In the representative case shown in Figure 2, the surgeon's exposure dose was 35.8 mGy as a result of X‐ray fluoroscopy‐guided bronchoscopic VATS marking. The patient had undergone CBCT scanning twice – before and after VATS marking – and therefore the patient's exposure dose was 245.8 mGy in total.
Figure 1.
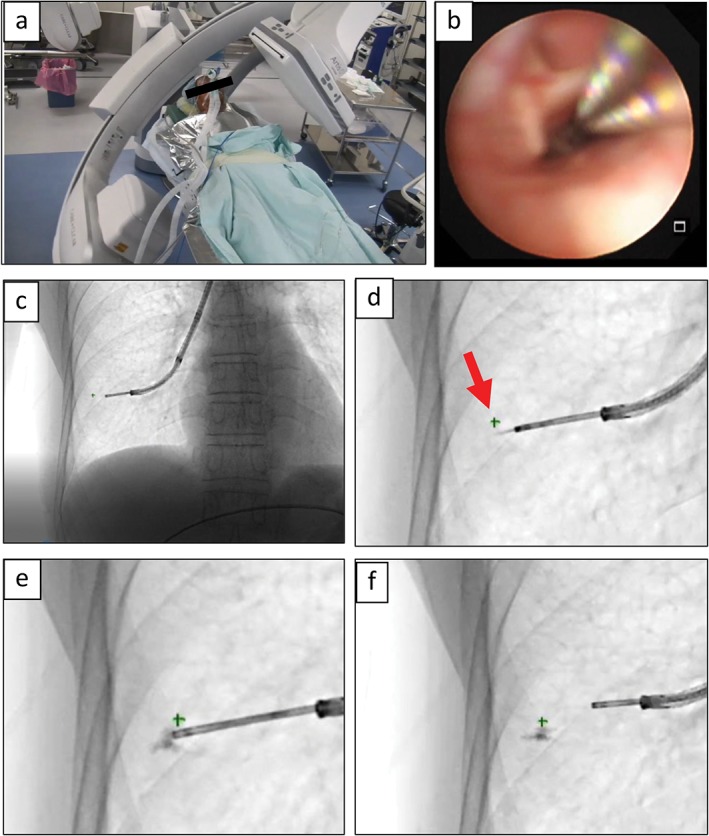
Bronchoscopic video‐assisted thoracoscopic surgery (VATS) marker injection under cone beam computed tomography (CBCT)‐augmented X‐ray fluoroscopy guidance. (a) CBCT is performed to obtain three‐dimensional positions of multiple pulmonary nodules. (b) Bronchoscopic fluorescent marking after introduction of general anesthesia in a hybrid operating room. (c) X‐ray fluoroscopic image with the transbronchial aspiration cytology needle inserted into the peripheral lung. (d) The X‐ray‐invisible pulmonary nodule is indicated as “+” on X‐ray fluoroscopy (red arrow). (e) VATS marker solution is injected near the target. (f) The VATS marker is placed successfully.
Figure 2.
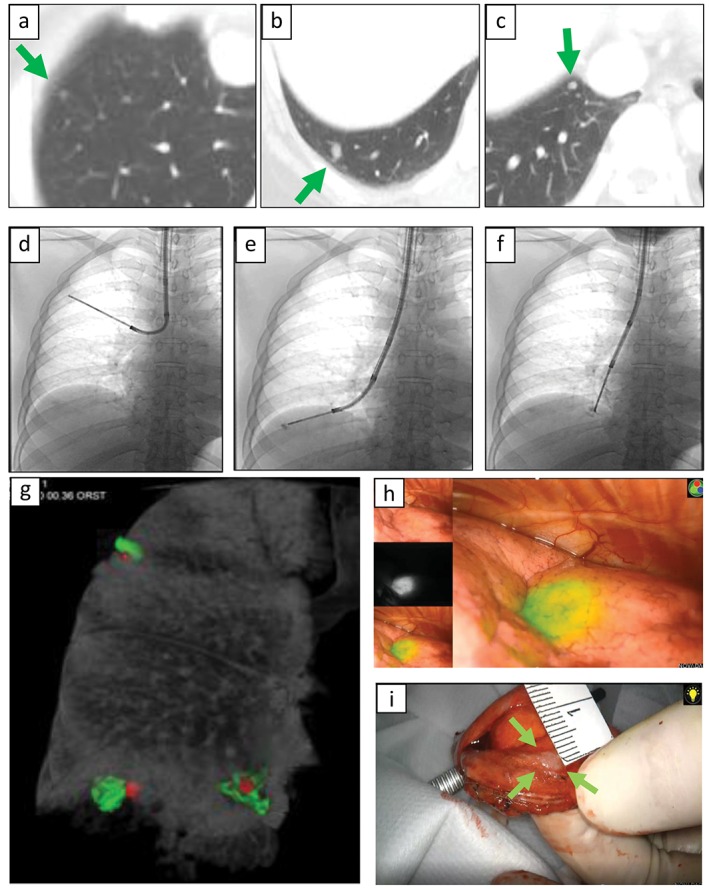
An example of the procedure in a patient with three multiple pulmonary nodules in the right lung. (a–c) The patient had three small pulmonary nodules < 3 mm in right S1, S9, and S7. (d–f) Video‐assisted thoracoscopic surgery (VATS) markers were injected in each target nodule. (g) Cone beam computed tomography (CBCT) performed a second time to create a three‐dimensional CT image of the right lung, including the target tumors (colored in red) and VATS markers (colored in green) for preoperative planning. The surgeon refers to this three‐dimensional image and performs VATS while confirming the positional relationship between the VATS marker(s) and pulmonary nodule(s). (h) VATS marker visualized by a near‐infrared thoracoscope. (i) Successful resection of the target nodule confirmed macroscopically by cross‐section. The pathological diagnosis for all three lesions was consistent with pulmonary metastases from cervical squamous cell carcinoma.
A bronchial blocker was inserted into the tracheal tube for one‐lung ventilation and the patient was placed in the lateral decubitus position for VATS. A near‐infrared thoracoscope was used to visualize the near‐infrared fluorescence of the ICG VATS marker (Fig 2h). The lung, including the target lesion, was excised by VATS. Successful removal was confirmed using both gross observation and rapid pathological diagnosis of the excised lung specimen (Fig 2i).
Discussion
Bronchoscopic marking does not damage visceral pleura and therefore can be used to mark more than one target lesion without causing secondary pneumothorax. However, VATS markers can only be inserted along the anatomical branch of the peripheral bronchus. Factors defining marking accuracy include the positional relationship between the bronchial branch and the lesion, the accuracy of the bronchoscopic examination technique of the operator, and the accuracy of the image guidance technique. On the basis of CT data, a bronchial route closest to the target lesion was created as a virtual bronchoscopy movie using the dedicated software Synapse Vincent (Fuji Film, Tokyo, Japan).12 If the target lesion cannot completely be reached by the bronchoscope, a VATS marker is placed at a point as close as possible to the target, and the surgeon is able to localize the target by confirming the relative positional relationship by 3DCT (Fig 2g).
In our technique, we first perform CBCT and register the 3D position of the lesion. Even if the pulmonary nodule itself is not X‐ray invisible, the position of the target lesion can be continuously displayed on the X‐ray fluoroscopy screen as long as the patient's position remains unchanged. The induction of general anesthesia ensures that the position of the target does not change during the procedure. CBCT‐augmented X‐ray fluoroscopy can also tilt to obtain an oblique fluoroscopic image so that the tip of the TBAC needle can be accurately led to the vicinity of the target lesion.
In this procedure, only 0.05 mL of 100 times diluted ICG was used as a VATS marker. Clinically available near‐infrared thoracoscopes, such as D‐light P (Karl Stortz, Tuttlingen, Germany) and PINPOINT (Stryker, Kalamazoo, MI, USA) can visualize the fluorescence of ICG at this concentration.13 In the dilated lung, ICG fluorescence injected into the deep part 2 cm from the visceral pleura can be visualized with a thoracoscope.13 A 100‐time dilution (0.025 mg/mL) of ICG is adequate for the purpose of VATS marking. In addition, the smaller the volume injected into the lung parenchyma, the fewer the complications, such as local tissue destruction and pulmonary bleeding.
We introduce a novel thoracoscopic surgical technique that uses a hybrid OR to lead the bronchoscope tip accurately to the target lesion and to place the VATS marker near the lesion. Using a hybrid OR not only improves the accuracy of bronchoscopic marking but also dramatically improves the physical suffering of the patient because all procedures can be performed after the induction of general anesthesia. This method is extremely useful to excise multiple small‐sized pulmonary nodules.
References
- 1. Gossot D, Miaux Y, Guermazi A, Celerier M, Friga J. The hook‐wire technique for localization of pulmonary nodules during thoracoscopic resection. Chest 1994; 105: 1467–9. [DOI] [PubMed] [Google Scholar]
- 2. Lizza N, Eucher P, Haxhe JP, De Wispelaere JF, Johnson PM, Delaunois L. Thoracoscopic resection of pulmonary nodules after computed tomographic‐guided coil labeling. Ann Thorac Surg 2001; 71: 986–8. [DOI] [PubMed] [Google Scholar]
- 3. Lenglinger FX, Schwarz CD, Artmann W. Localization of pulmonary nodules before thoracoscopic surgery: Value of percutaneous staining with methylene blue. AJR Am J Roentgenol 1994; 163: 297–300. [DOI] [PubMed] [Google Scholar]
- 4. Moon SW, Wang YP, Jo KH et al Fluoroscopy‐aided thoracoscopic resection of pulmonary nodule localized with contrast media. Ann Thorac Surg 1999; 68: 1815–20. [DOI] [PubMed] [Google Scholar]
- 5. Watanabe K, Nomori H, Ohtsuka T, Kaji M, Naruke T, Suemasu K. Usefulness and complications of computed tomography‐guided lipiodol marking for fluoroscopy‐assisted thoracoscopic resection of small pulmonary nodules: Experience with 174 nodules. J Thorac Cardiovasc Surg 2006; 132: 320–4. [DOI] [PubMed] [Google Scholar]
- 6. Torre M. A new safe and stable spiral wire needle for thoracoscopic resection of lung nodules. Chest 2004; 125: 2289–93. [DOI] [PubMed] [Google Scholar]
- 7. Sancheti MS, Lee R, Ahmed SU et al Percutaneous fiducial localization for thoracoscopic wedge resection of small pulmonary nodules. Ann Thorac Surg 2014; 97: 1914–8. [DOI] [PubMed] [Google Scholar]
- 8. Bolton WD, Howe H, Stephenson JE. The utility of electromagnetic navigational bronchoscopy as a localization tool for robotic resection of small pulmonary nodules. Ann Thorac Surg 2014; 98: 471–6. [DOI] [PubMed] [Google Scholar]
- 9. Sato M, Omasa M, Chen F et al Use of virtual assisted lung mapping (VAL‐MAP), a bronchoscopic multispot dye‐marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014; 147: 1813–9. [DOI] [PubMed] [Google Scholar]
- 10. Anantham D, Feller‐Kopman D, Shanmugham LN et al Electromagnetic navigation bronchoscopy‐guided fiducial placement for robotic stereotactic radiosurgery of lung tumors. Chest 2007; 132: 930–5. [DOI] [PubMed] [Google Scholar]
- 11. Kojima F, Sato T, Takahata H et al A novel surgical marking system for small peripheral lung nodules based on radio frequency identification. J Thorac Cardiovasc Surg 2014; 147: 1384–9. [DOI] [PubMed] [Google Scholar]
- 12. Anayama T, Hirohashi K, Miyazaki R et al Near‐infrared dye marking for thoracoscopic resection of small‐sized pulmonary nodules: Comparison of percutaneous and bronchoscopic injection techniques. J Cardiothorac Surg 2018; 13: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Anayama T, Qiu J, Chan H et al Localization of pulmonary nodules using navigation bronchoscope and a near‐infrared fluorescence thoracoscope. Ann Thorac Surg 2015; 99: 224–30. [DOI] [PubMed] [Google Scholar]


