Abstract
The evidence for cannabis’s treatment efficacy across different conditions varies widely, and comprehensive data on the conditions for which people use cannabis is lacking. We analyzed state registry data to provide nationwide estimates characterizing the qualifying conditions for which patients are licensed to use cannabis medically. We also compared the prevalence of medical cannabis qualifying conditions to recent evidence from the National Academies of Sciences, Engineering, and Medicine report on cannabis’s efficacy in treating each condition. Twenty states and Washington DC had available registry data on patient number, and fourteen states had data on patient-reported qualifying conditions. Chronic pain is currently and historically the most common qualifying condition reported by medical cannabis patients (67.5% in 2016). 85.5% of patient-reported qualifying conditions had either substantial or conclusive evidence of therapeutic efficacy. As medical cannabis use continues to increase, creating a nationwide patient registry will facilitate better understanding of use trends and potential effectiveness.
Introduction
Thirty-three states and the District of Columbia in the United States (US) have legalized cannabis for medical use since 1996, and nine states have legalized cannabis for recreational use since 2012.(1) To qualify for a cannabis license, patients must both have a doctor certify that they have a qualifying condition and obtain their license from the state. Despite the existence of medical cannabis patient registries to monitor these individuals, there are wide variations in registry implementation.(2) Some states, such as California and Maine, collect minimal or no data in voluntary registries, while others, such as Arizona and Colorado, collect and publish detailed reports. One prior study aggregated and examined prevalence of medical cannabis cardholders nationwide from 2001–2015, showing generally increasing total numbers of licensed medical cannabis patients.(3) However, nationwide documentation on the qualifying conditions for which people are actually using cannabis medically is lacking. Thus, characterizing the national scope and implications of such use remains challenging and is important to the policy implications regarding cannabis as a potential therapeutic agent.
In 2017, the National Academies of Sciences, Engineering and Medicine (NASEM) published a comprehensive review of the risks and therapeutic benefits of cannabis and cannabinoids (active compounds in cannabis) for a wide range of conditions.(4) There was conclusive or substantial evidence that chronic pain, nausea and vomiting due to chemotherapy, and multiple sclerosis (MS) spasticity symptoms were improved as a result of cannabis treatment. However, there was limited, insufficient, or no evidence of therapeutic value for many conditions allowed under state law, including post-traumatic stress disorder, anxiety, cancer, epilepsy, and irritable bowel syndrome, among others.
Given the lack of detailed registry data and widely variable evidence of cannabis efficacy for different qualifying conditions, we aimed to provide an up-to-date set of estimates characterizing the conditions for which individuals have obtained medical cannabis licenses nationwide. We hypothesized that the proportion of medical cannabis licenses issued for a given condition would be consistent with both the efficacy of cannabis and the population prevalence of that condition in the US. For example, we expected that chronic pain (substantial evidence of efficacy, affects 100 million Americans(5)) would be a common condition for which people use cannabis. In contrast, we hypothesized that amyotrophic lateral sclerosis (no evidence of efficacy, rare condition) would be rarely approved or used for treatment with cannabis.
Using the recent 2017 NASEM report as a guideline, we examined the relationship between published evidence for cannabis’s efficacy with the relative prevalence of those qualifying conditions as well as the number of states allowing medical use for those conditions. Finally, we compared enrollment rates and qualifying conditions between states based on their medical cannabis legislation, i.e., whether there were differences between states that provided a medicalized vs. non-medicalized model, as these terms have been defined in prior work.(6)
Methods
We collected registry statistics up to April 2018 from states with legalized medical cannabis using publicly available reports through state websites and by contacting the relevant state departments via phone and email. Registry data was obtained from Washington, DC and 20 states: Alaska, Arizona, California, Colorado, Delaware, Hawaii, Illinois, Maine, Massachusetts, Michigan, Minnesota, Montana, Nevada, New Hampshire, New Jersey, New Mexico, Oregon, Rhode Island, and Vermont (Exhibit 1). Some states publish monthly reports, while others publish annual reports. See Appendix A1 for a list of which reports were used for data analysis.(7) Connecticut does not publish reports and officials did not respond to data requests. Eight states (Washington, West Virginia, Pennsylvania, Ohio, North Dakota, Florida, Maryland, and Arkansas) reported not having any statistics available. California and Maine have voluntary registries, so it is very unlikely that the numbers reported are representative of the total number of licensed patients and qualifying conditions.(8) This is especially true for California, which reported a maximum of 12,659 cardholders was reported in 2009–2010, despite having the oldest medical cannabis legislation in the country (1996), and the largest population of any state. Thus, these states were excluded from analyses. Finally, two states do not publish reports every year: Michigan (missing 2010 and 2013) and Rhode Island (missing 2007, 2009, 2011, 2013, 2015, and 2016).
Exhibit 1 (table):
Patient enrollment in state medical cannabis programs by year, 1999–2017
| 2009* | 2010* | 2011* | 2012 | 2013* | 2014* | 2015*` | 2016* | 2017 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of active patients per state per year | Alaska (1998) | 1431 | 1743 | 1773 | 1084 | 1053 | ||||
| Arizona (2010) | 17852 | 34699 | 43148 | 61272 | 92838 | 102040 | 152979 | |||
| Colorado (2000) | 41039 | 116198 | 82089 | 108526 | 110979 | 115467 | 107534 | 94577 | 93372 | |
| Delaware (2011) | 36 | 102 | 370 | 1414 | 3274 | |||||
| Hawaii (2000) | 13150 | 15334 | 19858 | |||||||
| Illinois (2013) | 2663 | 7707 | 21800 | |||||||
| Massachusetts (2012) | 4881 | 18476 | 39581 | 49505 | ||||||
| Michigan (2008) | 1717 | 56685 | 124131 | 96408 | 182091 | 218556 | 269553 | |||
| Minnesota (2014) | 2806 | 7022 | ||||||||
| Montana (2004) | 8681 | 7785 | 21881 | |||||||
| Nevada (2000) | 4989 | 8055 | 13561 | 25358 | 23489 | |||||
| New Hampshire (2013) | 2089 | 3493 | ||||||||
| New Jersey (2010) | 1670 | 3727 | 6960 | 12154 | 16937 | |||||
| New Mexico (2007) | 8206 | 10708 | 12419 | 19629 | 29046 | 46645 | ||||
| New York (2014) | 4998 | |||||||||
| Oregon (1998) | 29289 | 39301 | 45456 | 50259 | 54884 | 66311 | 78045 | 68032 | 59137 | |
| Rhode Island (2006) | 3069 | 8044 | 11914 | 18533 | ||||||
| Vermont (2004) | 3800 | |||||||||
| Washington DC (2010) | 4815 | 5386 | ||||||||
| Total per year | 72045 | 158568 | 202082 | 342546 | 227845 | 382299 | 537090 | 641176 | 813917 |
Notes. SOURCE: Author’s analysis of state medical cannabis registry data, collected from state reports over time as detailed in Appendix A1. (7) The year each law was passed is indicated in parentheses next to each state, and many states do not have data until one or more years after the law passed. Number of patients enrolled per state over time. Oregon’s program began in 1999 with 113 patients and had 19,302 patients by 2008. Rhode Island’s program began in 2006 with 192 patients and had 561 in 2008.
: indicates the years with missing values.
We use the terms “patient”, “qualifying condition”, and “patient-reported qualifying condition” to describe data from these registries. “Patient” refers to the number of people enrolled in medical cannabis programs. “Qualifying condition” refers to the medical conditions that states recognize as allowing patients to obtain cannabis licenses. “Patient-reported qualifying condition” refers to the number of reported medical conditions that have allowed patients to obtain medical cannabis licenses. Thus, patients obtain medical cannabis licenses under one or more qualifying conditions, often resulting in a greater number of patient-reported qualifying conditions than total number of patients.
We classified qualifying conditions from each state report into the 2017 NASEM report categories, combining or keeping separate certain symptoms or conditions when clinically appropriate according to the advice of an MD (Dr. Clauw, co-author). See Appendix A2 for the full list of qualifying conditions and report categories.(7) We then graphically represented the total number of patient-reported qualifying conditions of each type from each year (Exhibit 2). Patient-reported qualifying conditions with <1.5% of the total were consolidated into an “other” category. In 2016 (the most recent year with complete data), we graphically examined patient-reported qualifying conditions in states with “medicalized” laws compared to those with “non-medicalized” laws (Exhibit 3). Based on prior work, medicalized laws are those that include requirements for more than one of the following, while non-medicalized laws include one or fewer requirements: doctor-patient relationship, regulations on manufacturing/dispensing, testing/labeling, refills, physician training, smoked vs. unsmoked products, and prescription drug monitoring programs.(6) Finally, also using data from 2016, we examined the number of patient-reported qualifying conditions in each NASEM report category compared to the level of evidence associated with that condition (Exhibit 4).
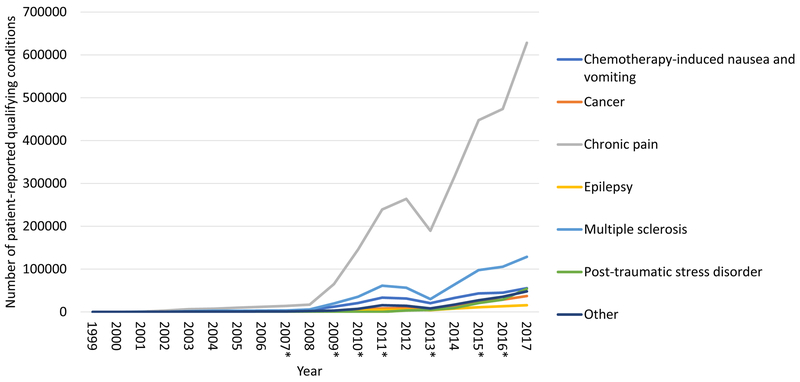
Exhibit 2:
Changes in number of patient-reported qualifying conditions by year, 1999–2017
Notes. SOURCE: Author’s analysis of state medical cannabis registry data. Number of patient-reported qualifying conditions over time. *: indicates the years with missing values. For Michigan, data are missing for 2010 and 2013. For Rhode Island, data are missing for 2007, 2009, 2011, 2013, 2015, and 2016. A sharp dip in qualifying conditions exhibited in 2013 is attributable to the large number of patients in Michigan unaccounted for in this year.
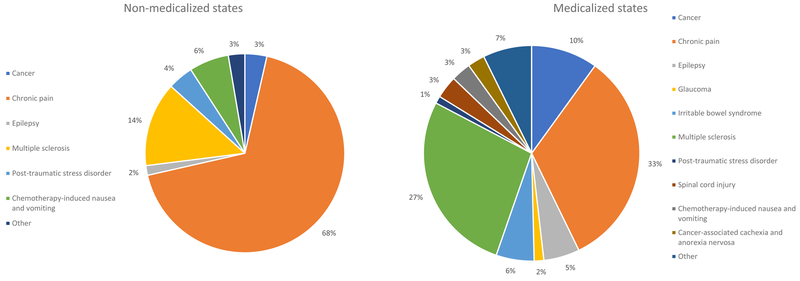
Exhibit 3:
Differences in patient-reported qualifying conditions between medicalized and non-medicalized states in 2016
Notes. SOURCE: Author’s analysis of state medical cannabis registry data. Differences in patient-reported qualifying conditions between medicalized and non-medicalized states using active patient data from 2016. (6) There were n=46,386 patient-reported qualifying conditions and n=31,168 patients in medicalized states, where states have more than one requirements pertaining to doctor-patient relationship, physician training, supply chain, etc. There were n=675,475 qualifying conditions and n=560,728 patients in non-medicalized states, which have zero or one similar requirements. Not all 20 states with registries are included because several do not provide data on qualifying conditions. Non-medicalized states include: Arizona, Colorado, Hawaii, Michigan, Montana, Nevada, New Mexico, and Oregon. Medicalized states include Delaware, Illinois, Minnesota, New Hampshire, New Jersey, and New York.
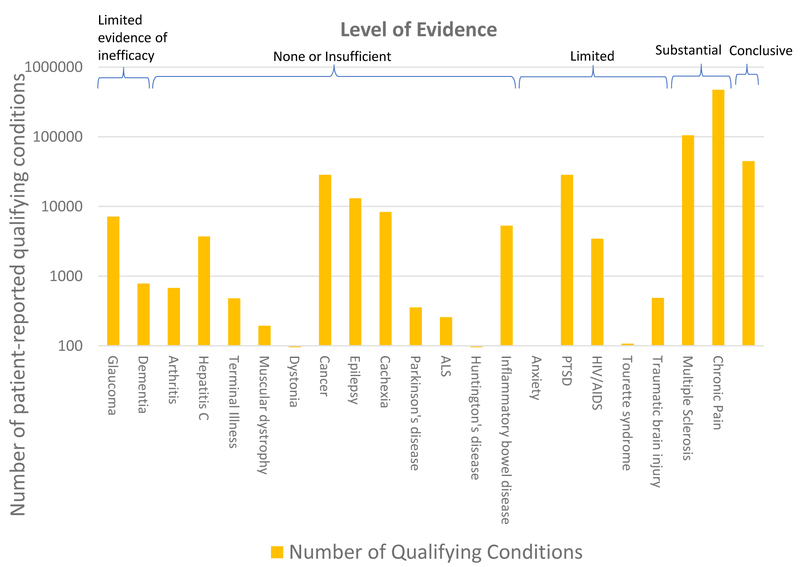
Exhibit 4.
Medical cannabis: qualifying conditions counts, level of evidence, and state regulations.
Notes. SOURCE: Author’s analysis of state medical cannabis registry data as of 2016. The number of patient-reported qualifying conditions is portrayed in gold. The level of evidence from the 2017 NASEM report is displayed in brackets at the top of the exhibit. All conditions had at least one associated patients except anxiety, which is currently allowed as a qualifying condition in West Virginia (a state with no available data) and was recently added in New Jersey.
Limitations
This study has several limitations. First, we were unable to access data for all states with medical cannabis registries, and some historical and current data were missing in certain states from which we did access data. This is especially concerning in the case of California, as some estimates suggest that California may have as many patients as the entire rest of the country.(2) However, an observational study of 2,897 medical cannabis users in California found that 63% used cannabis for pain, which is consistent with our results.(9) Second, in the context of new recreational cannabis laws, some medical cannabis users may choose not to obtain licenses, representing a different type of missing data concern that may have affected data reported from five states (Colorado, Oregon, Nevada, Alaska, and Massachusetts) and Washington DC in our analysis. Third, as patients often have co-morbid medical conditions, there are consistently more patient-reported qualifying conditions than patients, so it is uncertain for which condition/symptom patients are primarily using cannabis. Fourth, given the range of conditions for which cannabis is legal and the broad categories defined by the NASEM 2017 report, our reconciliation of conditions into different categories may oversimplify clinical and disease-specific differences. For example, conditions such as spinal cord injury or muscular dystrophy likely have a pain component, so placing them in a category of no or insufficient evidence may be problematic. Fifth, there are some qualifying conditions for which additional evidence has come since the 2017 NASEM report was published. For example, the cannabinoid cannabidiol (CBD) was recently approved by the FDA for the treatment of epileptic conditions Dravet syndrome and Lennox-Gastaut syndrome. Finally, there is mixed evidence of efficacy within certain conditions; e.g., there is substantial evidence for analgesia in chronic pain but some evidence of inefficacy for managing depression and anxiety in chronic pain.
Results
Exhibit 1 shows trends in the total patient enrollment over time in all medical cannabis states with available data. Including states that did not have data on patient-reported qualifying conditions, there were 641,176 registered medical cannabis patients in 2016 (all states), and 813,917 in 2017. This 2017 estimate does not include Vermont and New York, and likely underestimates the total by >70,000 patients based on changes in the New York patient number since 2016. By comparison, there were 729,843 patient-reported qualifying conditions in 2016, and 967,067 in 2017 (Exhibit 2), reflecting that multiple states report patients counts but not patient-reporting qualifying conditions and that individuals can have more than one patient-reported qualifying condition in a given year.
From a current and historical perspective, chronic pain has consistently been the most common patient-reported qualifying condition, accounting for 62.2% of the total patient-reported qualifying conditions on average (range of 33.3–73% between 1999–2016). Muscle spasms in multiple sclerosis is the second most common, followed by chemotherapy-induced nausea and vomiting, post-traumatic stress disorder, and cancer (Exhibit 2). As described in the Methods, the missing data from Rhode Island and Michigan are apparent in this exhibit, with the sharpest decrease in trends due to the lack of Michigan data in 2013.
In 2016, the last year with complete data, chronic pain accounted for 67.6% of patient-reported qualifying conditions (n=473,794/729,843) among active cardholders. We examined whether this trend was similar in states with and without “medicalized” programs.(6) Chronic pain was most common (68% of total patient-reported qualifying conditions) in older, non-medicalized state programs, such as Michigan, Colorado, and Arizona (Exhibit 3). These non-medicalized programs have far more patients (n=560,728) and patient-reported qualifying conditions (n=675,475) than medicalized ones, accounting for 94% of the total. By contrast, medicalized states have far fewer patients (n=31,168) and patient-reported qualifying conditions (n=46,386) Although chronic pain is still the most common patient-reported qualifying condition in medicalized states (33%), other conditions such as MS (27.4%), cancer (10%), and irritable bowel syndrome (5.7%) make up a substantial portion of the total in medicalized states.
Overall, 85.5% of patient-reported qualifying conditions are supported by conclusive or substantial evidence of therapeutic effectiveness according to the 2017 NASEM report – i.e., chronic pain, chemotherapy-induced nausea and vomiting, and multiple sclerosis spasticity symptoms. This percentage is quite consistent across the time-frame of available registry data (mean=87.8%, SD=6.2%). However, there are many other, less well-supported qualifying conditions, including some for which there is either no/insufficient evidence for efficacy (Hepatitis C, muscular dystrophy) or even evidence suggesting that cannabis is ineffective (glaucoma) for treating them (Exhibit 4). See Appendix Exhibit A3 for a visualization of the number of states that allow medical cannabis licensure for each qualifying condition.(7)
Discussion
In this investigation, we report the number of patients who use medical cannabis for the various qualifying conditions allowed under state law, and track changes in the conditions for which patients medically use cannabis over time. Though our reported values likely underestimate the true number of patients and qualifying conditions due to lack of data (especially in California and Washington State), our data show that the number of medical cannabis patients has risen dramatically over time as more states legalize medical cannabis.
While substantial or conclusive evidence exists to establish the efficacy of cannabis to treat 85.5% of patient-reported qualifying conditions, there is a mismatch between many of the qualifying conditions allowed under state law and the level of evidence supporting use of cannabis for each condition. This may be due to several factors. First, as noted in the 2017 NASEM report, the legal status of cannabis as a Schedule I substance makes clinical trials challenging to conduct to establish evidence of efficacy.(4) Second, there is a funding bias, as government funding has typically been used to examine harm due to cannabis use and abuse rather than therapeutic benefits.(4, 10) Third, groups representing certain conditions (e.g., veterans advocating for PTSD) have effectively advocated for certain qualifying conditions to be added in select states.(11) Recently, such advocacy has also been successful in obtaining resources to do more relevant clinical trials that examine efficacy, which may address some of the funding bias in the future.(12)
Chronic pain was by far the most currently and historically prevalent patient-reported qualifying condition. This finding is consistent with the prevalence of chronic pain, which affects an estimated 100 million Americans.(5) Further, many drugs do not effectively manage pain symptoms or have side effects that preclude their long-term use,(13) and fear of addiction and side effects (especially with opioids) may incentivize patients to use cannabis. Problems with pain management and dissatisfaction with current treatment options are substantiated by nationwide studies that have shown decreased opioid overdose deaths, prescriptions, and hospitalizations in states with medical cannabis legislation,(14–21) as well as reports of individuals with chronic pain substituting cannabis for opioids.(9, 22–30) Finally, chronic pain is an extremely common symptom in many medical conditions, so if patients have conditions that are not covered but also have chronic pain, it is possible that they may use chronic pain as the umbrella condition under which they obtain a license. If this is true, the pattern of chronic pain registrations may change as data emerge from states with newer medical cannabis laws, which now tend to be more medicalized and have more stringent definitions of qualifying conditions/symptoms.(8) For example, New York and Illinois have recently added opioid substitution/replacement therapy as a qualifying condition.(31)
Colorado, Oregon, Alaska, and Nevada exhibit a decline in medical cannabis patient enrollees following legalization of recreational cannabis between 2012–2016. In contrast, Massachusetts and Washington DC exhibit increased numbers of enrollees, although this may be because the recreational law in Massachusetts had not yet been implemented at the time of data collection and Washington DC does not have any active recreational cannabis dispensaries. (Vermont, California, Washington DC, and Maine do not have available or reliable data to analyze since their recreational laws have passed.) The data from Colorado, Oregon, Nevada, and Alaska are in keeping with the blurred lines between types of cannabis use, as many people use cannabis recreationally, medically, or both.(32, 33) These declines in medical cannabis patient enrollment suggest that in states where cannabis becomes legal for recreational adult use, people who use cannabis may no longer feel the need to obtain a license to protect themselves from legal reprisals; moreover, medical users may no longer wish to incur licensing costs, including those associated with doctor approval and license fees, when they can otherwise obtain cannabis legally. As no states with medicalized laws have yet legalized cannabis for recreational use, it remains to be seen whether they will follow similar enrollment patterns to the non-medicalized states.
Given the wide variability in the number of patients using cannabis for different conditions, these results suggest that it may be important to account for patient-reported qualifying conditions, rather than simply patient number, when examining effects of cannabis legislation on public health effects (e.g., medication prescribing, which varies based on medical condition). They also highlight the importance of compiling a nationwide database of medical cannabis users to evaluate the risks and benefits of medical cannabis for different medical conditions and symptoms. Such a registry could guide state legislation on allowable qualifying conditions and track risks associated with specific products (e.g., cannabis concentrates or edibles). Finally, our results suggest the need to monitor how medical cannabis and recreational cannabis regimes co-evolve, as early data indicate that recreational marijuana legalization could render medical marijuana laws moot over time. If legal marijuana use is increasingly de-coupled from medical need or oversight at the state level, then a larger role for federal government oversight regarding product safety and information, for instance by the Food and Drug Administration, may be warranted.(34)
Conclusions
We provide an historical and current view of qualifying conditions for which medical cannabis patients obtain their licenses. Our results highlight many inconsistencies in data quality between states, suggesting the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are utilized, which would help guide both research and policy needs. For example, funneling resources into relevant clinical or epidemiological studies that determine cannabis’s risks and benefits compared to other medications could influence insurance coverage for cannabis products, and thus warrant improved federal oversight.
85.5% of conditions for which patients are licensed to use medical cannabis have either substantial or conclusive evidence of efficacy according to the categories outlined in the 2017 NASEM report. Given this overwhelming use of cannabis for conditions that are supported by clinical evidence, we believe that not only is it inappropriate for cannabis to remain a Schedule I substance, but that it is also important for state and federal policy makers to seriously consider how to integrate cannabis research and products in an evidence-based way into the healthcare system.(34)
Supplementary Material
Acknowledgments
Disclosures: Kevin Boehnke’s work on this article was supported by the National Institute of Dental and Craniofacial Research (Grant No. 12DE023574), and Rebecca Haffajee’s work on this article was supported by funding from the National Center for Advancing Translational Sciences (Grant No. KL2TR002241). Daniel Clauw has consulted for Pfizer Inc., Eli Lilly and Company, Tonix Pharmaceuticals, Aptinyx, Regeneron, IMC, and Intec.
References:
- 1.Procon.org. 33 Legal Medical Marijuana States and DC. 2018.
- 2.Procon.org. Number of Legal Medical Marijuana Patients. 2018.
- 3.Fairman BJ. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug Alcohol Depend. 2016;159:72–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids. 2017. Report No.: 978–0-309-45304-2.
- 5.Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 6.Williams AR, Olfson M, Kim JH, Martins SS, Kleber HD. Older, less regulated medical marijuana programs have much greater enrollment rates than newer ‘medicalized’ programs. Health Affairs. 2016;35(3):480–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Appendix. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 8.Procon.org. 31 Legal Medical Marijuana States and DC - Medical Marijuana - ProCon.org. 2018. [Google Scholar]
- 9.Reiman A, Welty M, Solomon P. Cannabis as a Substitute for Opioid-Based Pain Medication: Patient Self-Report. Cannabis and Cannabinoid Research. 2017;2(1):160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chesler J, Ard A. Feds limit research on marijuana for medical use. USA: Today. 2015. August/18/2015. [Google Scholar]
- 11.StarTribune.com. PTSD is added to Minnesota’s medical pot program as qualifying condition. January-19-2018.
- 12.O’Neil ME, Nugent SM, Morasco BJ, Freeman M, Low A, Kondo K, et al. Medicine Benefits and Harms of Plant-Based Cannabis for Posttraumatic Stress Disorder. 2017;167(5). [DOI] [PubMed] [Google Scholar]
- 13.Clauw DJ. Pain management: Fibromyalgia drugs are ‘as good as it gets’ in chronic pain. Nat Rev Rheumatol. 2010;6(8):439–40. [DOI] [PubMed] [Google Scholar]
- 14.Powell D, Pacula RL, Jacobson M. Do Medical Marijuana Laws Reduce Addictions and Deaths Related to Pain Killers? Journal of Health Economics. 2018;58:29–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bachhuber MA, Saloner B, Cunningham CO, Barry CL, Rolland B. Medical Cannabis Laws and Opioid Analgesic Overdose Mortality in the United States, 1999–2010. JAMA Internal Medicine. 2014;174(10):1668–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradford AC, Bradford WD. Medical marijuana laws reduce prescription medication use in medicare part d. Health Affairs. 2016;35(7):1230–6. [DOI] [PubMed] [Google Scholar]
- 17.Bradford AC, Bradford WD. Medical Marijuana laws may be associated with a decline in the number of prescriptions for medicaid enrollees. Health Affairs. 2017;36(5):945–51. [DOI] [PubMed] [Google Scholar]
- 18.Bradford AC, Bradford WD, Abraham A, Adams GB. Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Internal medicine. 2018;30602:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wen H, Hockenberry JM. Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA internal medicine. 2018;11:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi Y Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 2017;173:144–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pacula RL, Powell D, Heaton P, Sevigny EL, Pacula RL, Powell D, et al. Assessing the Effects of Medical Marijuana Laws on Marijuana and Alcohol Use: The Devil Is in the Details. 2013. Report No.: 1520–6688.
- 22.Boehnke KF, Litinas E, Clauw DJ. Medical cannabis associated with decreased opiate medication use in retrospective cross-sectional survey of chronic pain patients. The Journal of Pain. 2016;17(6):739–44. [DOI] [PubMed] [Google Scholar]
- 23.Lucas P, Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: A survey of authorized medical cannabis patients. International Journal of Drug Policy. 2017;42:30–5. [DOI] [PubMed] [Google Scholar]
- 24.Piper BJ, DeKeuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. 2017;31(5):569–75. [DOI] [PubMed] [Google Scholar]
- 25.Abuhasira R, Schleider LB-l, Mechoulam R, Novack V. Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. European Journal of Internal Medicine. 2018;49:44–50. [DOI] [PubMed] [Google Scholar]
- 26.Sexton M, Cuttler C, Finnell JS, Mischley LK. A Cross-Sectional Survey of Medical Cannabis Users: Patterns of Use and Perceived Efficacy. Cannabis and Cannabinoid Research. 2016;1(1):131–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corroon JM, Mischley LK, Sexton M. Cannabis as a substitute for prescription drugs - A cross-sectional study. Journal of Pain Research. 2017;10:989–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schleider LB-l, Mechoulam R, Lederman V, Hilou M. Prospective analysis of safety and efficacy of medical cannabis in large unselected population of patients with cancer. European Journal of Internal Medicine. 2018;49:37–43. [DOI] [PubMed] [Google Scholar]
- 29.Vigil JM, Stith SS, Adams IM, Reeve AP. Associations between medical cannabis and prescription opioid use in chronic pain patients : A preliminary cohort study. PLoS ONE. 2017;12(11):e0187795–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stith SS, Vigil JM, Adams IM, Reeve AP. Effects of Legal Access to Cannabis on Scheduled II–V Drug Prescriptions. Journal of the American Medical Directors Association. 2018;19(1):59–64. [DOI] [PubMed] [Google Scholar]
- 31.Voelker R States Move to Substitute Opioids With Medical Marijuana to Quell Epidemic. JAMA. 2018. [DOI] [PubMed] [Google Scholar]
- 32.Lin LA, Ilgen MA, Jannausch M, Bohnert KM. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict Behav. 2016;61:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sznitman SR. Do recreational cannabis users, unlicensed and licensed medical cannabis users form distinct groups? Int J Drug Policy. 2017;42:15–21. [DOI] [PubMed] [Google Scholar]
- 34.Haffajee RL, MacCoun RJ, Mello MM. Behind Schedule - Reconciling Federal and State Marijuana Policy. N Engl J Med. 2018;379(6):501–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.