Abstract
Objectives:
The purpose of this work was to improve the clinical versatility of high-speed real-time MRI studies of temporomandibular joint (TMJ) dynamics by simultaneous recordings of multiple MRI movies in different sections.
Methods:
Real-time MRI at 3 T was realized using highly undersampled radial FLASH acquisitions and image reconstruction by regularized nonlinear inversion (NLINV). Multi-slice real-time MRI of two, three or four slices at 0.75 mm resolution and 6 to 8 mm thickness was accomplished at 50.0 ms, 33.3 ms or 25.5 ms temporal resolution, respectively, yielding simultaneous movies at 2 × 10, 3 × 10 or 4 × 10 frames per second in a frame-interleaved acquisition mode. Real-time MRI movies were evaluated by three blinded raters for visibility of the anterior and posterior border of disc, shape of the disk body and condyle head as well as movement of the disc and condyle (1 = excellent, 5 = no visibility).
Results:
Effective delineation of the disk atop the mandibular condyle was achieved by T 1-weighted images with opposed-phase water-fat contrast. Compared to 8 mm sections, multi-slice recordings with 6 mm thickness provided sharper delineation of relevant structures as confirmed by inter-rater evaluation. Respective dual-slice and triple-slice recordings of a single TMJ as well as dual-slice recordings of both joints (one slice per TMJ) received the highest visibility ratings of ≤ 2 corresponding to high confidence in diagnostic content.
Conclusions:
The improved access to TMJ dynamics by multi-slice real-time MRI will contribute to more effective treatment of temporomandibular disorders.
Introduction
The temporomandibular joint (TMJ) is one of the important structures aiding in the opening and closing of the mouth during articulation, chewing and swallowing. Temporomandibular disorders (TMD) refer to impaired functioning of the TMJ and frequently involve an abnormal disk-condyle relationship and pain.1 The diagnosis of TMD usually involves conventional MRI at several static positions of the closed and opened mouth. The procedure is considered as gold standard2 despite the fact that it lacks dynamic information regarding the movement of the joint. This problem may be overcome by recent advances toward high-speed real-time MRI which treat the reconstruction of a series of undersampled gradient-echo images as the solution to a nonlinear inverse (NLINV) problem with temporal regularization.3 The method has been shown to offer high spatiotemporal fidelity4 for cross-sectional imaging in a large variety of scientific and clinical settings, in particular MRI studies ranging from articulation5 or brass playing6 to swallowing,7 , 8 cardiac function9, through-plane flow of blood10 , 11 and cerebrospinal fluid.12 , 13
The aim of this work is a further development of the NLINV method to extend previous single-slice real-time MRI studies of the TMJ14 , 15 by multi-slice recordings with even shorter acquisition times and improved contrast. While previous applications14 , 15 mainly focused on the evaluation of T 2/T 1-weighted or T 1-weighted contrasts, their temporal resolution of 67 ms was already significantly faster than alternative approaches to “dynamic” MRI of the TMJ with acquisition times on the order of 1s.16-20 Multi-slice approaches have been suggested as advantageous for real-time cardiac imaging,21 fetal imaging,22 swallowing,23 and the visualization of speech processes.24 However, these studies were compromised by limited spatial and temporal resolution, while nominally high frames rates were only obtained by data sharing with use of sliding-window techniques. For example, the recent work by Kim et al24 proposed a dual-slice (triple-slice) protocol at 2.4 × 2.4 × 6.0 mm3 (3.0 × 3.0 × 6.0 mm3) spatial resolution within an acquisition time of 156 ms (163 ms). In contrast, the present work offers real-time TMJ studies at 0.75 × 0.75 × 6.0 mm3 spatial resolution and up to 25.5 ms temporal resolution yielding four simultaneous movies each at 10 frames per second (fps).
Methods and materials
The study was approved by the institutional review board of the University Medical Center Göttingen and all participants gave written informed consent before MRI. 10 volunteers without TMJ disorders (7 males, 3 females, age 29.3 ± 10.1 years, range 21–56 years) were recruited from the local University after clinical examination according to RDC/TMD criteria. MRI was conducted on a commercial 3.0 T MRI system (Prisma Fit, Siemens Healthcare, Erlangen, Germany) with use of a dedicated dental 15-channel RF coil (NORAS MRI Products, Hochberg, Germany).
Multi-slice real-time MRI
Real-time MRI was based on highly undersampled radial FLASH acquisitions with spoiling of transverse magnetizations by randomized RF phases25 and image reconstruction by NLINV with temporal regularization.3, 9,10 Post-processing involved the application of a modified non-local means algorithm for spatial filtering.26 Apart from the data presented here, the actual development of a multi-slice real-time MRI technique relied on extensive phantom studies and in vivo trials to optimize image quality, disk contrast, and artifact-free representations of jaw movements under natural physiological conditions. In particular, the possibility to enhance the signal-to-noise ratio (SNR) by increasing the flip angle of the FLASH acquisition for spokes-interleaved multi-slice acquisitions with prolonged TR was discarded, because of the concomitant increase of the acquisition time per frame, i.e. the temporal footprint probing the TMJ movement. Instead, interleaved multi-slice acquisitions with a maximum temporal footprint of 50 ms per frame were considered necessary to properly monitor TMJ mechanics. All protocols proposed here therefore employ frame-interleaved multi-slice acquisition modes for real-time MRI of the TMJ.
The request for high in-plane resolution and adequate SNR led to the choice of a minimum acquisition time of about 25 ms. Based on previous high-speed real-time MRI studies4, 6 the resulting acquisition of 11 spokes per frame represents a robust degree of undersampling for reliable NLINV reconstructions of moderately sized data matrices. Finally, in contrast to preceding TMJ studies favoring a darkened T 2/T 1 contrast with use of refocused FLASH acquisitions,14, 15 a bright signal intensity of the disk and an improved contrast of its anterior and posterior border during movement were achieved by a T 1-weighted spoiled FLASH acquisition25 in combination with a short gradient-echo time that ensured opposed-phase conditions for water-fat contributions. Moreover, the resulting short TE values markedly reduced residual susceptibility differences, e.g. due to the vicinity of the air-filled ear canal, and further improved overall image quality.
Four different multi-slice real-time MRI protocols of potential clinical utility were evaluated in the course of this study. Technical details are summarized in Table 1: (1) Dual-slice recordings of a single TMJ at 50.0 ms resolution, (2) triple-slice recordings (lateral, central, medial position) of a single TMJ at 33.3 ms resolution, (3) dual-slice recordings at 50.0 ms resolution with one central slice covering each joint, and (4) quadruple-slice recordings at 25.5 ms resolution with two slices covering each TMJ. All real-time MRI movies were acquired using T 1 contrast with opposed-phase water-fat condition (i.e. TE = 1.33 ms at 3 T), a rate of 10 fps, and a temporal footprint of 25 to 50 ms.
Table 1.
Acquisition parameters for multi-slice real-time MRI of the TMJ
| Single joint | Single joint | Both joints | Both joints | |
| Number of slices | 2 | 3 | 2 | 4 |
| Field-of-view/mm2 | 128 × 128 | |||
| Image matrix size | 170 × 170 | |||
| Resolution/mm2 | 0.75 × 0.75 | |||
| Flip angle/degree | 14 | |||
| Slice thickness/mm | 8/6 | 6 | 8/6 | 8/6 |
| Repetition time/ms | 2.38 | 2.21 | 2.38 | 2.32 |
| Echo time/ms | 1.33 | 1.33 | 1.34 | 1.33 |
| Bandwidth/Hz pixel−1 | 820 | 1090 | 980 | 1090 |
| Number of spokes | 2 × 21 | 3 × 15 | 2 × 21 | 4 × 11 |
| Acquisition time per frame/ms | 50.0 | 33.2 | 50.0 | 25.5 |
| Frame rate/fps | 2 × 10 | 3 × 10 | 2 × 10 | 4 × 10 |
fps, frames per second; TMJ, temporomandibular joint.
Online reconstruction and display of real-time images was achieved by a parallelized version of the NLINV algorithm27, 28 and a bypass computer (sysGen/TYAN Octuple-GPU, 2 × Intel Westmere E5620 processor, 48 GB RAM, Sysgen, Bremen, Germany) equipped with two processors (CPUs, SandyBridge E5- 2650, Intel, Santa Clara, CA) and eight graphical processing units (GPUs, GeForce GTX, TITAN, NVIDIA, Santa Clara, CA). This system is fully integrated into the reconstruction pipeline of the commercial MRI system via a 1 GBit network connection. Overall online reconstruction speed was about 20 fps for dual-slice recordings and 28 fps for triple- and quadruple-slice recordings.
Study protocol
All MRI measurements were performed in supine position. A timing protocol which schematically visualized the opening and closing of the mouth was shown to the subjects during scanning using an LCD monitor inside the scanner room about 1 m behind the patient table. Subjects viewed the visual instruction with use of a mirror atop the head coil. Each measurement had a total duration of 60 s and consisted of two times opening and closing of the mouth (8 s for each of the four movements).
Slice orientations, perpendicular to the condyles, were chosen according to a set of rapid localizer scans (1 s per section) performed in sagittal, transversal, and coronal orientations. The actual study started with triple-slice recordings at a slice thickness of 6 mm of both the right and left TMJ. Subsequently, dual-slice recordings (two slices on a single TMJ, one slice on each TMJ) and quadruple-slice recordings (two slices on each TMJ) were performed with a slice thickness of 6 and 8 mm. These recordings were positioned according to the functional information obtained from the triple-slice recordings. The total duration of all measurements per subject, including subject preparation and coil positioning, was about 30 min.
Data evaluation
Real-time MRI movies were evaluated by three independent raters with extensive experience in TMD diagnostics using MRI. All raters were blinded to both subjects and clinical examinations. The TMJ internals evaluated were anterior and posterior border of the disc, shape of the disk body and condyle head, and movement of the disc and condyle. Disc location and condyle movement were evaluated regarding disorders of the TMJ. Inter-rater scores were defined as 1 = excellent visibility and very high confidence in diagnostic content, 2 = good visibility and high confidence in diagnostic content, 3 = just visible, 4 = poor visibility without confidence in diagnostic content, and 5 = no visibility of TMJ structures. The mean and standard deviation were evaluated separately for the left and right TMJ. The inter-rater reliability for the evaluation of the quality of visualized TMJ structures was calculated using Kendall’s coefficient of concordance (W), defined as: weak agreement with a coefficient between 0.11 and 0.30, moderate agreement between 0.30 and 0.50, strong agreement between 0.51 and 0.70 and extremely strong agreement between 0.71 and 0.90.29 In addition, Bland-Altman analysis was performed to compare the different multi-slice real-time MRI recordings. Further, p values were evaluated for all real-time MRI movies with the significance level set to 5% for all statistical tests. All analyses were performed with the statistics software R (v. 3.1.2, www.r-project.org) and XLSTAT software (Addinsoft company, Paris, France).
Results
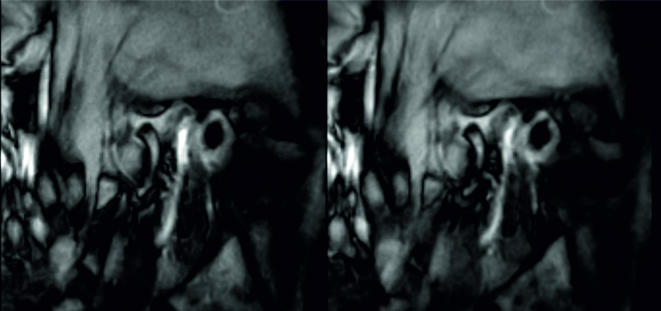
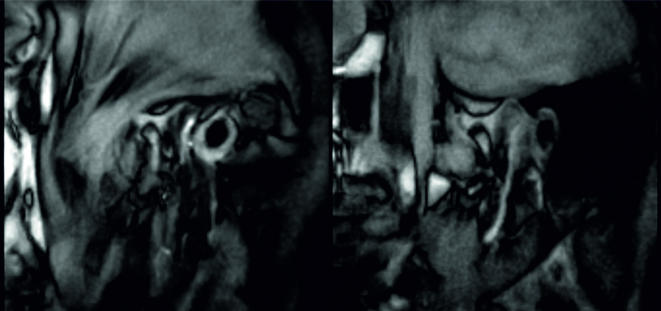
After clinical examination and radiological evaluation of real-time MRI data none of the subjects presented with a TMJ disorder. Figure 1 shows selected images at 6 and 8 mm slice thickness taken from simultaneous dual-slice recordings of both joints (i.e. one central slice per TMJ) at an intermediate time point during opening of the mouth (Supplementary Video 1). In T 1-weighted images the condyle and disk are represented by low and high intensities, respectively. Although slightly better SNR was observed for acquisitions with 8 mm slice thickness, recordings at 6 mm slice thickness resulted in sharper borders of TMJ structures, especially of the disk and condyle. Figure 2 shows images at 6 mm slice thickness selected from triple-slice recordings in a medial, central and lateral position (Supplementary Video 2). As observed in previous single-slice real-time MRI studies,14, 15 a double-oblique central orientation perpendicular to the top of the condyle provides the most comprehensive information about the movement of the disk and condyle.
Figure 1.
Effect of slice thickness. Dual-slice real-time MRI of the right and left temporomandibular joint of a healthy subject during voluntary opening of the mouth (2 × 10 frames per second, 0.75 mm resolution): Selected frames (oblique sagittal views) of only one of two simultaneous real-time MRI movies (right TMJ) with (left) 6 mm and (right) 8 mm slice thickness. For experimental details see Table 1. TMJ, temporomandibular joint.
Figure 2.
Triple-slice real-time MRI of the right temporomandibular joint of a healthy subject during voluntary opening of the mouth (3 × 10 frames per second, 0.75 mm resolution, 6 mm section thickness): Selected frames (oblique sagittal view) of three simultaneous real-time MRI movies in a (left) lateral, (middle) central, and (right) medial section of the TMJ. For experimental details see Table 1. TMJ, temporomandibular joint.
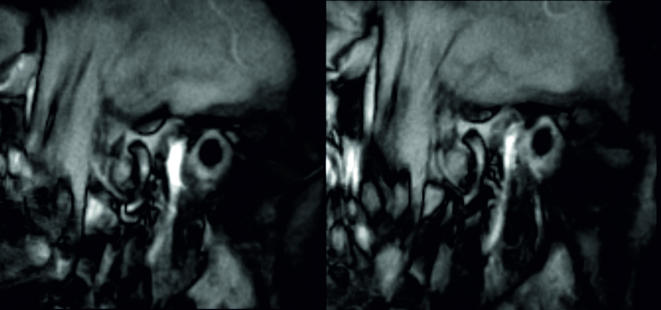
Figure 3 depicts images from a dual-slice recording in a medial and central position of the right TMJ at 6 mm slice thickness and 50 ms temporal resolution (Supplementary Video 3). Alternatively, Figure 4 (Supplementary Video 4) presents images from a corresponding dual-slice recording of both joints (one central slice per TMJ). This latter approach offers excellent SNR for both joints as well as more information regarding the dynamics of the entire jaw during physiological action.
Figure 3.
Dual-slice real-time MRI of the right temporomandibular joint of a healthy subject during voluntary opening of the mouth (2 × 10 frames per second, 0.75 mm resolution, 6 mm slice thickness): Selected frames (oblique sagittal view) of two simultaneous real-time MRI movies in a (left) central and (right) lateral position of the TMJ. For experimental details see Table 1. TMJ, temporomandibular joint.
Figure 4.
Dual-slice real-time MRI of the (left) right and (right) left temporomandibular joint of a healthy subject during voluntary opening of the mouth (2 × 10 frames per second, 0.75 mm resolution, 6 mm slice thickness): Selected frames (oblique sagittal views) of two simultaneous real-time MRI movies. For experimental details see Table 1.
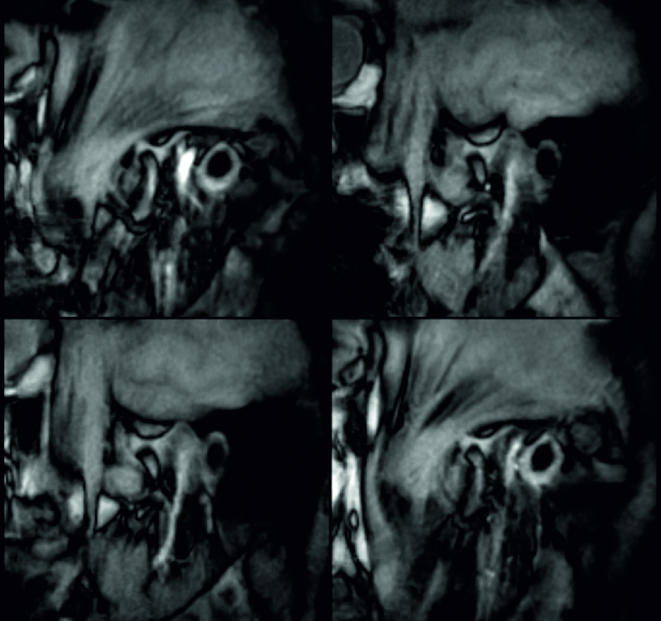
Figure 5 shows quadruple-slice recordings, i.e. two medial and two central slices of both joints at 6 mm slice thickness (Supplementary Video 5). Although the use of a higher degree of data undersampling per frame causes a slightly lower SNR in comparison to other multi-slice recordings, the TMJ structures were clearly recognizable to allow for a good diagnostic evaluation. This protocol best covers the regions of both joints and thereby provides the maximum information.
Figure 5.
Quadruple-slice real-time MRI recording of the (top) right and (bottom) left temporomandibular joint (two slices each) of a healthy subject during voluntary opening of the mouth (4 × 10 frames per second, 0.75 mm in-plane resolution, 6 mm slice thickness): Selected frames (oblique sagittal views) of four simultaneous real-time MRI movies in a central and lateral position of both joints. For experimental details see Table 1.
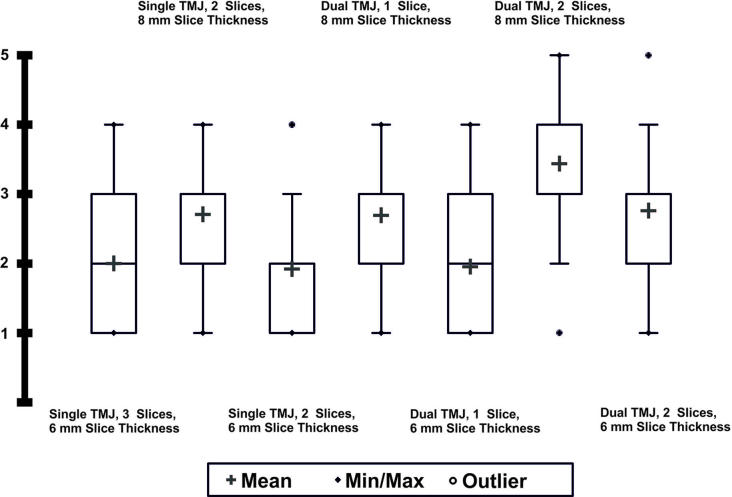
Figure 6 summarizes the ratings of the multi-slice real-time recordings by three raters. In general, multi-slice real-time MRI at 6 mm slice thickness received a higher rating. A comparison of all 6 mm protocols evaluated in this study resulted in the highest ratings for dual-slice and triple recordings of a single TMJ as well as for dual-slice recordings of both joints (one slice per TMJ). The ratings of 2 or even slightly lower correspond to good visibility of TMJ structures and high confidence in diagnostic content.
Figure 6.
Ratings (three observers) of the multi-slice real-time MRI protocols used for studying TMJ dynamics (10 subjects): 1 = excellent visibility, 2 = good visibility, 3 = just visible, 4 = poor visibility, 5 = no visibility.
Kendall’s W values were between 0.74 and 0.91 for all multi-slice real-time MRI protocols. High Kendall’s W values indicate extremely strong inter-observer agreement. Bland-Altman analyses showed higher ratings for acquisitions with 6 mm slice thickness compared to 8 mm slice thickness over all recording modalities. The bias between the compared approaches lay between ± 0.63 and ± 0.80 which was interpreted as clinically significant. Further, the statistical tests indicated high significance (p values < 0.0001) for all real-time MRI movies.
Discussion
This study successfully extends single-slice real-time MRI assessments of TMJ dynamics14,15 to simultaneous movie recordings in multiple sections and with improved disk contrast and overall image quality during movement. The proposed methods offer comprehensive and time-efficient volume coverage, preferably at a slice thickness of only 6 mm, and in particular allow for an accurate dynamic characterization of the entire jaw by simultaneous real-time MRI recordings of both joints. In this context the proposed triple-slice real-time MRI recordings of a single TMJ served as a very effective functional localizer for subsequent dual-joint measurements at similar quality. In fact, despite some loss in SNR, even quadruple-slice acquisitions with two real-time MRI movies covering each TMJ resulted in a comprehensive visualization of jaw dynamics at clinically acceptable image quality.
Further, such data will be advantageous for post-processing strategies which aim at four-dimensional visualization and biomechanical analyses of all TMJ structures during physiological movement. In turn this could aid in better understanding physiological and pathological processes, designing improved TMD treatment methods or even allow for image-guided intervention.
A limitation of this work is the restriction to a group of normal subjects. While adequate for evaluating methodological progress and demonstrating in vivo feasibility under normal physiological conditions, future extensive studies on a large cohort of patients are warranted in order to further develop clinically optimized sequence versions and measurement protocols that best match different clinical questions. Moreover, the current online visualization of multi-slice real-time MRI acquisitions relied on the integration of a GPU-equipped bypass computer into the commercial MRI system to achieve highly accelerated NLINV reconstructions. Finally, the entire study benefited from the use of a dedicated 15-channel RF coil.
In conclusion, this study demonstrates the technical feasibility and potential clinical usefulness of multi-slice real-time MRI for studying TMJ dynamics. Simultaneous access to real-time MRI movies in multiple sections at a rate of 10 fps each promises a comprehensive and time-efficient characterization of TMJ dynamics and extended TMD diagnostics.
Footnotes
Acknowledgements: The authors thank NORAS MRI Products, Hochberg, Germany, for lending a dedicated 15-channel RF coil.
Disclosure: JF holds a patent about the real-time MRI acquisition and reconstruction technique used here.
The authors Sebastian Krohn and Arun A Joseph contributed equally to the work.
Funding: Financial support by the DZHK (German Centre for Cardiovascular Research) and BMBF (German Ministry of Education and Research) is gratefully acknowledged.
REFERENCES
- 1. Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. . Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 2014; 28: 6–27. doi: 10.11607/jop.1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Behr M, Held P, Leibrock A, Fellner C, Handel G. Diagnostic potential of pseudo-dynamic MRI (CINE mode) for evaluation of internal derangement of the TMJ. Eur J Radiol 1996; 23: 212–5. doi: 10.1016/S0720-048X(96)01075-3 [DOI] [PubMed] [Google Scholar]
- 3. Uecker M, Zhang S, Voit D, Karaus A, Merboldt KD, Frahm J. Real-time MRI at a resolution of 20 ms. NMR Biomed 2010; 23: 986–94. doi: 10.1002/nbm.1585 [DOI] [PubMed] [Google Scholar]
- 4. Frahm J, Schätz S, Untenberger M, Zhang S, Voit D, Merboldt KD, et al. . On the temporal fidelity of nonlinear inverse reconstructions for real-time MRI – The motion challenge. Open Med Imaging J 2014; 8: 1–5. doi: 10.2174/1874347101408010001 [DOI] [Google Scholar]
- 5. Niebergall A, Zhang S, Kunay E, Keydana G, Job M, Uecker M, et al. . Real-time MRI of speaking at a resolution of 33 ms: undersampled radial FLASH with nonlinear inverse reconstruction. Magn Reson Med 2013; 69: 477–85. doi: 10.1002/mrm.24276 [DOI] [PubMed] [Google Scholar]
- 6. Iltis PW, Frahm J, Voit D, Joseph AA, Schoonderwaldt E, Altenmüller E. High- speed real-time MRI of fast tongue movements in elite horn players. Quant Imaging Med Surg 2015; 5: 374–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Olthoff A, Carstens PO, Zhang S, von Fintel E, Friede T, Lotz J. Evaluation of dysphagia by novel real-time magnetic resonance imaging. Neurology 2016; 87: 1–7. [DOI] [PubMed] [Google Scholar]
- 8. Zhang S, Joseph AA, Gross L, Ghadimi M, Frahm J, Beham AW. Diagnosis of gastroesophageal reflux disease using real-time magnetic resonance imaging. Sci Rep 2015; 5: 12112. doi: 10.1038/srep12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang S, Joseph AA, Voit D, Schaetz S, Merboldt KD, Unterberg-Buchwald C, et al. . Real-time magnetic resonance imaging of cardiac function and flow-recent progress. Quant Imaging Med Surg 2014; 4: 313–29. doi: 10.3978/j.issn.2223-4292.2014.06.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Untenberger M, Tan Z, Voit D, Joseph AA, Roeloffs V, Merboldt KD, et al. . Advances in real-time phase-contrast flow MRI using asymmetric radial gradient echoes. Magn Reson Med 2016; 75: 1901–8. doi: 10.1002/mrm.25696 [DOI] [PubMed] [Google Scholar]
- 11. Tan Z, Roeloffs V, Voit D, Joseph AA, Untenberger M, Merboldt KD, et al. . Model-based reconstruction for real-time phase-contrast flow MRI: Improved spatiotemporal accuracy. Magn Reson Med 2017; 77: 1082–93. doi: 10.1002/mrm.26192 [DOI] [PubMed] [Google Scholar]
- 12. Dreha-Kulaczewski S, Joseph AA, Merboldt KD, Ludwig HC, Gärtner J, Frahm J. Inspiration is the major regulator of human CSF flow. J Neurosci 2015; 35: 2485–91. doi: 10.1523/JNEUROSCI.3246-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dreha-Kulaczewski S, Joseph AA, Merboldt KD, Ludwig HC, Gärtner J, Frahm J. Identification of the upward movement of human CSF In Vivo and its relation to the brain venous system. J Neurosci 2017; 37: 2395–402. doi: 10.1523/JNEUROSCI.2754-16.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krohn S, Gersdorff N, Wassmann T, Merboldt KD, Joseph AA, Buergers R, et al. . Real-time MRI of the temporomandibular joint at 15 frames per second- a feasibility study. Eur J Radiol 2016; 85: 2225–30. doi: 10.1016/j.ejrad.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 15. Krohn S, Frahm J, Merboldt KD, Wassmann T, Joseph AA, Bürgers R. Diagnosis of disk displacement using real-time MRI: Clinical report of two patients. J Prosthet Dent 2018; 119: 206–9. doi: 10.1016/j.prosdent.2017.03.022 [DOI] [PubMed] [Google Scholar]
- 16. Chen YJ, Gallo LM, Meier D, Palla S. Dynamic magnetic resonance imaging technique for the study of the temporomandibular joint. J Orofac Pain 2000; 14: 65–73. [PubMed] [Google Scholar]
- 17. Wang EY, Mulholland TP, Pramanik BK, Nusbaum AO, Babb J, Pavone AG, et al. . Dynamic sagittal half-Fourier acquired single-shot turbo spin-echo MR imaging of the temporomandibular joint: initial experience and comparison with sagittal oblique proton-attenuation images. AJNR Am J Neuroradiol 2007; 28: 1126–32. doi: 10.3174/ajnr.A0487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shimazaki Y, Saito K, Matsukawa S, Onizawa R, Kotake F, Nishio R, et al. . Image quality using dynamic MR imaging of the temporomandibular joint with true-FISP sequence. Magn Reson Med Sci 2007; 6: 15–20. doi: 10.2463/mrms.6.15 [DOI] [PubMed] [Google Scholar]
- 19. Molinari F, Gentile L, Manicone P, Ursini R, Raffaelli L, Stefanetti M, et al. . Interobserver variability of dynamic MR imaging of the temporomandibular joint. Radiol Med 2011; 116: 1303–12. doi: 10.1007/s11547-011-0699-0 [DOI] [PubMed] [Google Scholar]
- 20. Sun Q, Dong MJ, Tao XF, Yu Q, Li KC, Yang C. Dynamic MR imaging of temporomandibular joint: an initial assessment with fast imaging employing steady-state acquisition sequence. Magn Reson Imaging 2015; 33: 270–5. doi: 10.1016/j.mri.2014.10.013 [DOI] [PubMed] [Google Scholar]
- 21. Nayak KS, Pauly JM, Nishimura DG, Hu BS. Rapid ventricular assessment using real-time interactive multislice MRI. Magn Reson Med 2001; 45: 371–5. doi: [DOI] [PubMed] [Google Scholar]
- 22. Neustadter DM, Chiel HJ. Imaging freely moving subjects using continuous interleaved orthogonal magnetic resonance imaging. Magn Reson Imaging 2004; 22: 329–43. doi: 10.1016/S0730-725X(03)00184-X [DOI] [PubMed] [Google Scholar]
- 23. Paine TL, Conway CA, Malandraki GA, Sutton BP. Simultaneous dynamic and functional MRI scanning (SimulScan) of natural swallows. Magn Reson Med 2011; 65: 1247–52. doi: 10.1002/mrm.22824 [DOI] [PubMed] [Google Scholar]
- 24. Kim YC, Proctor MI, Narayanan SS, Nayak KS. Improved imaging of lingual articulation using real-time multislice MRI. J Magn Reson Imaging 2012; 35: 943–8. doi: 10.1002/jmri.23510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Roeloffs V, Voit D, Frahm J. Spoiling without additional gradients: Radial FLASH MRI with randomized radiofrequency phases. Magn Reson Med 2016; 75: 2094–9. doi: 10.1002/mrm.25809 [DOI] [PubMed] [Google Scholar]
- 26. Klosowski J, Frahm J. Image denoising for real-time MRI. Magn Reson Med 2017; 77: 1340–52. doi: 10.1002/mrm.26205 [DOI] [PubMed] [Google Scholar]
- 27. Schätz S, Uecker M. A multi-GPU programming library for real-time applications. In: algorithms and architectures for parallel processing (Springer). Lect Notes Comp Sci 2012; 7439: 114–28. [Google Scholar]
- 28. Schaetz S, Voit D, Frahm J, Uecker M. Accelerated computing in magnetic resonance imaging – real-time imaging using non-linear inverse reconstruction. Comput Math Methods Med 2017; 2017: 1–11. doi: 10.1155/2017/3527269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kendall M, Gibbons JD. Rank correlation methods. 5th Edition London: The British Institute of Radiology.; 1990. [Google Scholar]