Abstract
Introduction:
Chronic low back pain (cLBP) is prevalent, especially among military veterans. Many cLBP treatment options have limited benefits and are accompanied by side effects. Major efforts to reduce opioid use and embrace nonpharmacological pain treatments have resulted. Research with community cLBP patients indicates that yoga can improve health outcomes and has few side effects. The benefits of yoga among military veterans were examined.
Design:
Participants were randomized to either yoga or delayed yoga treatment in 2013–2015. Outcomes were assessed at baseline, 6 weeks, 12 weeks, and 6 months. Intention-to-treat analyses occurred in 2016.
Setting/Participants:
One hundred and fifty military veterans with cLBP were recruited from a major Veterans Affairs Medical Center in California.
Intervention:
Yoga classes (with home practice) were led by a certified instructor twice weekly for 12 weeks, and consisted primarily of physical postures, movement, and breathing techniques.
Main outcome measures:
The primary outcome was Roland–Morris Disability Questionnaire scores after 12 weeks. Pain intensity was identified as an important secondary outcome.
Results:
Participant characteristics were mean age 53 years, 26% were female, 35% were unemployed or disabled, and mean back pain duration was 15 years. Improvements in Roland–Morris Disability Questionnaire scores did not differ between the two groups at 12 weeks, but yoga participants had greater reductions in Roland–Morris Disability Questionnaire scores than delayed treatment participants at 6 months −2.48 (95% CI= −4.08, −0.87). Yoga participants improved more on pain intensity at 12 weeks and at 6 months. Opioid medication use declined among all participants, but group differences were not found.
Conclusions:
Yoga improved health outcomes among veterans despite evidence they had fewer resources, worse health, and more challenges attending yoga sessions than community samples studied previously. The magnitude of pain intensity decline was small, but occurred in the context of reduced opioid use. The findings support wider implementation of yoga programs for veterans.
INTRODUCTION
Low back pain becomes chronic (lasting more than 12 weeks1) in about 20%–30% of those afflicted.2 Both military veterans3,4 and active-duty military personnel5,6 have higher rates of chronic pain than the general U.S. population, with back pain being the most frequently reported location of chronic pain.7 In addition to pain, individuals with chronic low back pain (cLBP) often report symptoms and functional limitations, including increased disability,8 psychological symptoms,9–12 and reduced quality of life.13,14 In the U.S., cLBP is the leading cause of lost productivity,15 the second most common reason for physician visits,16 and billions of dollars are spent on back pain–related health care annually.17
Guidelines for treating cLBP recommend a stepped care approach,18,19 beginning with the provision of selfcare information,20 followed by medications as needed.20,21 However, addiction, overdose deaths, and other consequences have become a major concern with opioid medications.22,23 Thus, interest in nonpharmacological treatments for cLBP has increased dramatically in recent years.24,25
A 2007 review26 found that yoga produced benefits similar to other conventional nonpharmacological treatments for cLBP. Since the publication of the cLBP care guidelines in 2007, two large RCTs on yoga for cLBP have been completed. However, these samples27,28 were recruited in community settings, were 65%–70% female, and there was no evidence of elevated rates of psychological or other medical comorbid disorders. Conversely, about 90% of U.S. veterans are male, and Veterans Affairs (VA) patients are more likely than the general U.S. population to be disabled, have lower incomes,29 and have elevated rates of psychological disorders or substance use, and more total comorbidity.30 Thus, the extent to which the results of the two prior RCTs27,28 would generalize to VA patients or U.S. military veterans as a whole may be limited. Prior yoga studies with VA patients were nonrandomized preliminary studies.31,32 The objective of the current study is to examine the effectiveness of yoga for improving function and reducing pain intensity among VA patients with cLBP.
METHODS
Study Design
The study design and methods have been previously published in greater detail.33 The study randomized 150 VA patients to either a yoga intervention or to a delayed yoga treatment (DT) comparison group. Participants randomized to yoga were scheduled to attend a 12-week yoga program immediately after randomization, whereas comparison participants were invited to attend the yoga intervention after 6 months. Outcomes were assessed via patient self-report at baseline, 6 weeks, 12 weeks, and 6 months. The study was conducted at a VA Medical Center in California.
Participants were recruited via referral by VA clinicians. Study staff notified care providers about study recruitment via e-mail, brief presentations, and word of mouth. Primary care, physical medicine, pain medicine, and psychology were the main clinics targeted for recruitment. In addition, flyers were posted in common areas and waiting rooms at the medical center. VA patients receiving study information from providers or from flyers contacted study personnel to learn about study enrollment criteria. Those interested were scheduled for a screening exam.
Informed consent and Health Insurance Portability and Accountability Act of 1996 waiver was provided at the screening visit. Medical record information and a physical examination were used to evaluate eligibility criteria. Inclusion and exclusion criteria for the study were published previously.33 In summary, inclusion criteria consisted of VA patients, aged ≥18 years, cLBP diagnosis of ≥6 months, English literacy, no new pain treatments in the last month, willing to attend yoga or be assigned to DT, willing to attend four assessments, and willing to not change pain treatments unless medically necessary. Exclusion criteria included recent back surgery (in the last 12 months), back pain from systemic conditions, morbid obesity, acute sciatica/nerve compression, chronic lumbar radicular pain, serious unstable coexisting medical or psychiatric conditions, potential metastatic disease, positive Romberg test, or practiced yoga more than one time in the last year.
Participants were recruited in six cohorts, with 26–30 potential participants in each cohort being scheduled to attend a group baseline assessment. After the baseline assessment was complete, the study coordinator used a secure, web-based data management system to randomly assign participants to one of two groups (yoga or DT). Participants were notified of group assignment the following day. The binary non-stratified randomization sequence was computer generated, at a 1:1 allocation ratio in blocks of 10 participants to facilitate balanced group assignment. Assessors were initially blinded to group assignment and did not have access to group assignment data. Prior to assessments, the study coordinator asked participants to not discuss their group assignment or experiences with any study staff at the assessments. All participants were enrolled from 2013 to 2015.
Interventions
All participants continued to receive usual care. To avoid confounding effects, all participants were asked to refrain from changing treatments for their cLBP during the study period unless medically necessary (provider determined). DT during this time period varied, but most commonly consisted of prescription and nonprescription pain medications, physical therapy, spinal manipulation, exercise, and various other self-help treatments. Participants randomized to the experimental group began yoga within 1 week. Participants assigned to the DT group were asked to not practice yoga until completion of their 6-month assessment. Compliance with these instructions was assessed at each time point.
The 12-week yoga intervention consisted of two 60-minute, instructor-led yoga sessions per week. The intervention was hatha yoga, consisting of physical yoga postures, movement sequences, and regulated breathing. Directed attention and brief meditation were also included. Yoga sessions were led by a single certified yoga instructor with over 7 years of experience teaching yoga to people with cLBP. Instructors used a prescriptive manual to guide each session, but were allowed to change the order of poses to provide some variety. Yoga sessions were videotaped and multiple sessions were reviewed by study investigators to ensure adherence to the manualized protocol. The sessions were designed for individuals with cLBP at the yoga beginner level, but were adaptable for varied functional abilities and for progression over the 24 sessions. Yoga participants received a home practice manual recommending 15–20 minutes of yoga home practice on days that instructor-led sessions were not held. The home manual included basic postures taught in class. Safety was emphasized for home practice and participants were encouraged to consult with the instructor about any home practice concerns. The intervention has been described in more detail previously.33 Yoga manuals are available by e-mailing the corresponding author.
The importance of attendance at instructor-led yoga sessions and adherence to the recommended yoga home practice was emphasized at the baseline randomization visit and reinforced by the yoga instructor during yoga sessions. With many VA patients having transportation challenges, participants were reimbursed $5 per yoga session attended to offset travel costs. This is consistent with the assistance and resources provided to VA patients for travel to clinical care appointments. Yoga participants were contacted by study staff if they missed more than one yoga session without explanation. Basic refreshments such as bottled water and small healthy snacks were provided at yoga sessions and assessments. All participants were contacted by the project coordinator at least monthly to validate contact information and remind them of their next assessment window. Additional reminder letters and phone calls were provided preceding assessments.
Data were collected via VA medical records and questionnaires in accordance with IRB and Health Insurance Portability and Accountability Act of 1996 requirements. Participants attended their choice of two group appointments for each of the four assessments (baseline, 6 weeks, 12 weeks, 6 months). Individual assessment appointments were provided to accommodate scheduling conflicts. During each assessment, participants spent 30–45 minutes completing a packet of self-report questionnaires. Participants were compensated $20–$30 for completing each of the assessments.
Measures
A brief self-report questionnaire assessed sociodemographic characteristics. Medical record data were accessed to apply enrollment criteria and confirm medication use.
The primary outcome was the mean Roland–Morris Disability Questionnaire (RMDQ) score at 12 weeks34; consisting of 24 questions concerning back pain–specific functional limitations experienced “today.” The scale has established psychometric properties34 and was the primary outcome in other yoga for cLBP trials, allowing for comparisons.27,28,35 The short version of the Brief Pain Inventory was used to assess pain intensity as the main secondary outcome of interest.36 The 13-item measure has been validated with low back pain patients.37 Nonstudy treatments and medications were assessed using self-report questionnaires.38 Medication use was verified using medical records.
Attendance of yoga sessions was tracked with a sign-in sheet that was checked and verified by the yoga instructor each week. All yoga practice outside of the instructor-led yoga sessions was tracked using weekly home practice logs. Participants indicated the days home practice occurred, the duration of practice, the estimated physical exertion level, and whether an instructor, video, or other guide was used.
Adverse event information was collected via in-person contact with participants, telephone, a program evaluation, and medical records. All participants were instructed to contact study staff if they experienced any serious health problems or nonserious health problems that they attributed to the yoga intervention during the informed consent process. They received the contact information for the project coordinator and the principal investigator, or could talk with the yoga instructor who was available the 15 minutes before and after each yoga class. Medical records were reviewed if patients could not be contacted to complete assessments, and a program evaluation asked about participants’ experiences and the effects of the yoga intervention on health.
Statistical Analysis
The Wilcoxon rank sum and Fisher’s exact tests were used to compare demographic and baseline clinical variables between study groups, and also between the subset of study group participants with missing data. An “intent-to-treat” approach was followed for all study outcomes and all analyses were conducted using statistical software R, version 3.3.0 in 2016. The primary outcome was change in the RMDQ score34 and the primary hypothesis was that participants randomized to yoga would have significantly greater decreases in back pain-specific disability scores at 12 weeks than DT participants. Secondary outcomes include the change in pain intensity and interference, depressed mood, physical and mental quality of life, fatigue, opioid medication use, and other pain treatments. Linear mixed-effects modeling was used to examine the change score across measured time points. A main effect of group (yoga versus DT), a main effect of time (categorically coded for baseline, 6 weeks, 12 weeks, and 6 months) and an interaction between group X time were included in the model. The number of yoga classes attended, the proportion of high attendance, and home practice sessions were summarized using descriptive statistics. For the primary outcome (RMDQ) and the main secondary outcome (pain intensity), the authors also compared the proportion of subjects with clinically meaningful improvement (≥30% decrease RMDQ39; ≥1.0 point decrease Brief Pain Inventory pain rating40) between groups using Fisher’s exact test.
For baseline characteristics, the authors assessed the association with each outcome using a linear mixed-effects model first. If a variable was significantly associated with the outcome or significantly different between two study groups, the variable was included as a covariate in the multivariate mixed-effects model. A backward model selection was used to remove insignificant covariates from the multivariate model. The variable with the largest p-value was removed from the model each time and only covariates that were significant at p<0.10 were kept in the final model. Both random intercept and random slope were considered and the significance of random effects were assessed using the likelihood ratio test.
The proportion of participants with missing data at follow-up assessments for each group was compared using Fisher’s exact test. The authors also compared the baseline characteristics of participants with missing data by group to examine whether attrition was related to baseline characteristics. The sensitivity of the results to missing data was also examined using imputation by carrying the last data point forward, a conservative method commonly used in clinical trials.41
A minimum sample size of 144 subjects (72 per group) was selected to provide an 80% chance of detecting a moderate effect size of d=0.50 for the difference in mean change of RMDQ score over 12 weeks between the yoga and DT groups. This effect size (0.50) was gauged from a large previous trial of yoga for cLBP.28 Analyses assumed a Type I error of 0.05, a correlation of 0.6 between RMDQ score at baseline and week 12, clustering effects, and an attrition rate of 15% at week 12. During the study, the recruitment target was increased from 144 to 150 participants (75 per group) because of slightly higher than expected attrition rates. Power analysis was performed using the statistical package R, version 3.3.0 (www.r-project.org).
RESULTS
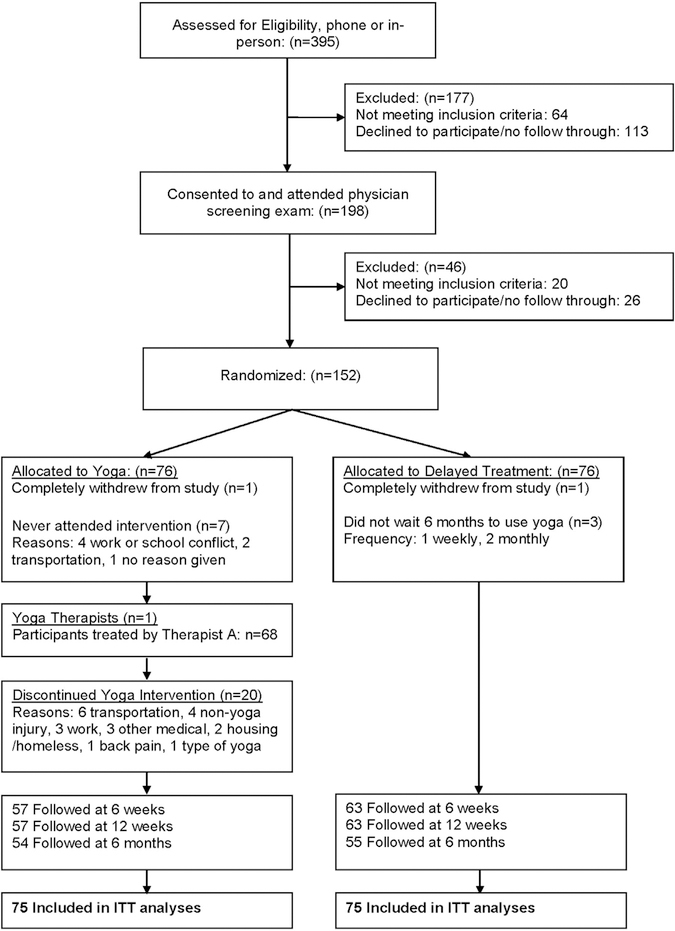
Participant flow is depicted in Figure 1. Study staff responded to 395 individuals over 30 months. Upon reviewing eligibility criteria and willingness to attend a physician screening examination, 64 individuals declined participation. Another 113 individuals were interested, but either postponed or failed to attend the screening examination. The remaining 198 potential participants attended the screening. Twenty were not eligible and 26 were eligible but never attended the baseline assessment and randomization. Of the 152 assessed and randomized, two participants later requested complete study withdrawal, including all data. This resulted in 75 participants being randomized to each study arm. Attrition from follow-up assessment periods was 20% attrition at the 6- and 12-week assessments and 27.3% attrition at the 6-month assessment. Attrition rates were not significantly different between groups at any time point. (p=0.31–0.99) No differences were found on any baseline characteristics between attriters for each group, suggesting data was missing at random. Participant characteristics are presented in Table 1.
Figure 1.
Flowchart of study participants.
ITT, intention to treat.
Table 1.
Patient Baseline Characteristics
| Characteristic | Total (n=150) | Yoga (n=75) | Delayed treatment (n=75) | p-value |
|---|---|---|---|---|
| Age, years, M (SD) | 53.4 (13.3) | 53.3 (12.7) | 53.6 (13.9) | 0.55 |
| Sex | ||||
| Male | 111 (74) | 55 (73) | 56 (75) | 1 |
| Race/ethnicity | ||||
| African American or black | 26 (17) | 16 (21) | 10 (13) | 0.75 |
| White | 74 (49) | 35 (47) | 39 (52) | |
| Native American | 2 (1.3) | 1 (1.3) | 1 (1.3) | |
| Hispanic | 30 (20) | 15 (20) | 15 (20) | |
| Asian/Pacific Islander | 9(6) | 3(4) | 6(8) | |
| Other | 9 (6) | 5 (6.7) | 4 (5.3) | |
| Marital status | ||||
| Single | 38 (26) | 17 (23) | 21 (28) | 0.31 |
| Married | 50 (34) | 24 (32) | 26 (35) | |
| Separated | 4 (2.7) | 4 (5.3) | 0 (0) | |
| Divorced | 52 (35) | 28 (37) | 24 (32) | |
| Widowed | 5 (3.4) | 2 (2.7) | 3 (4.1) | |
| Education | ||||
| Grade school | 1 (0.7) | 0(0) | 1 (1.4) | 0.47 |
| High school diploma/GED | 10 (6.8) | 6 (8.1) | 4 (5.5) | |
| Some college | 56 (38) | 30 (41) | 26 (36) | |
| College grad | 46 (31) | 19 (26) | 27 (37) | |
| Post grad | 34 (23) | 19 (26) | 15 (21) | |
| Employment | ||||
| Full-time | 29 (21) | 16 (23) | 13 (18) | 0.82 |
| Part time | 19 (14) | 8 (12) | 11 (15) | |
| Unemployed | 29 (21) | 13 (19) | 16 (22) | |
| Disabled | 19 (14) | 10 (15) | 9(13) | |
| Retired or volunteer | 32 (23) | 14 (20) | 18 (25) | |
| Other | 13 (9.2) | 8 (12) | 5 (6.9) | |
| Homeless in last 5 years | ||||
| Yes | 25 (18) | 12 (17) | 13 (19) | 1 |
| Living situation | ||||
| Homeless | 5 (3.5) | 3 (4.2) | 2 (2.8) | 0.90 |
| Group living | 16 (11) | 9 (13) | 7 (9.7) | |
| Own house | 67 (47) | 32 (44) | 35 (49) | |
| Apartment | 56 (39) | 28 (39) | 28 (39) | |
| Transportation to VA | ||||
| Own vehicle | 107 (75) | 53 (74) | 54 (76) | 0.91 |
| Ride with family/friends | 7 (4.9) | 3 (4.2) | 4(5.6) | |
| Public transport | 21 (15) | 11 (15) | 10(14) | |
| Other | 8 (5.6) | 5 (6.9) | 3 (4.2) | |
| Travel time to VA Medical Center | ||||
| ≤30 minutes | 63 (42) | 35 (47) | 28 (37) | 0.20 |
| 30–60 minutes | 65 (43) | 27 (36) | 38 (51) | |
| >60 minutes | 22 (15) | 13 (17) | 9(12) | |
| Ever practiced yoga? | ||||
| No | 91 (61) | 39 (52) | 52 (69) | 0.045 |
| Clinical characteristics, M (SD) | ||||
| Years since first sought medical care for cLBP | 15.0 (12.0) | 15.4 (10.4) | 14.6 (13.5) | 0.71 |
| Narcotic medication-current, yes | 30 (20) | 14 (19) | 16 (21) | 0.84 |
| Using other pain treatments, yes | 77 (51) | 42 (56) | 35 (47) | 0.39 |
| Using self-help pain treatments, yes | 111 (74) | 57 (76) | 54 (72) | 0.83 |
| RMDQ score, M (SD) | 9.85 (5.52) | 9.40 (5.15) | 10.3 (5.87) | 0.38 |
| Pain intensity (BPI), M (SD) | 4.66 (1.96) | 4.64 (1.76) | 4.68 (2.16) | 0.99 |
Note: Values are n (%) unless otherwise indicated. Boldface indicates statistical significance (p<0.05).
BPI, Brief Pain Inventory (scale 0–10); cLBP, chronic low back pain; GED, General Educational Development test; RMDQ, Roland-Morris Disability Questionnaire (scale 0–24); VA, Veterans Affairs.
The median number of instructor-led sessions attended by subjects randomized to yoga was 14 of 24 classes (58%; mean=12.3 classes). Among those who attended at least one class (n=68), the median number of classes attended was 15 of 24 classes (63%; mean=13.5 classes). One or more home practice logs were turned in by 40 of 75 yoga participants (59% attending one or more classes). A mean of 156 total minutes and 4.2 days of yoga home practice/week were reported via logs.
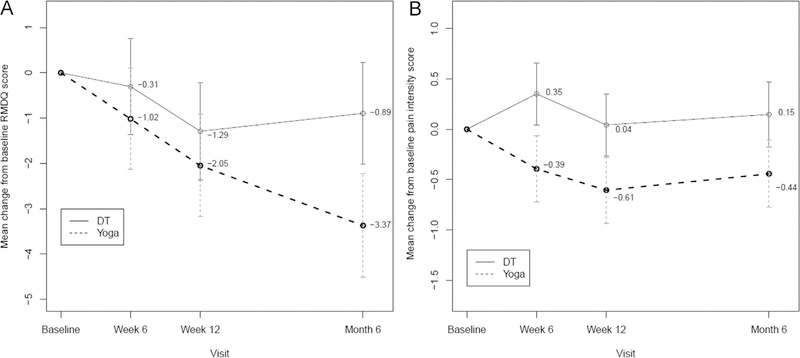
For the primary outcome, both study groups had significant reductions in RMDQ scores after 12 weeks with a 2.05-point reduction in the yoga group (95% CI= −3.18, −0.92) and 1.29-point reduction in the DT group (95% CI= −2.36, −0.22), and no significant differences between groups (p=0.34, Table 2). However, significant differences emerged at the 6-month assessment (p=0.003), with RMDQ scores continuing to drop in the yoga group and increasing toward baseline in the DT group (Figure 2A). A 30% decrease in RMDQ scores is considered a clinically meaningful outcome and has been the primary outcome in recent studies.35,40 For comparison purposes, the authors reanalyzed data using this cutoff. At 6 weeks, 12 weeks, and 6 months respectively, 21%, 33%, and 24% of the DT group and 33%, 44%, and 57% of the yoga group had a 30% decrease in RMDQ scores. The proportion achieving this clinical outcome was significantly higher in the yoga group only at 6 months (57% versus 24%; p<0.001). The results did not change when covariates were omitted from the model, or when missing data were imputed.
Table 2.
Linear Mixed-Effects Model for Change at Post Baseline Visit in Primary and Secondary Outcomes
| Variable | Baseline score, M (SD) | Change at 6 weeks, M (95% CI) | p-value | Change at 12 weeks, M (95% CI) | p-value | Change at 6 months, M (95% CI) | p-value |
|---|---|---|---|---|---|---|---|
| Back-related disability (RMDQ) | |||||||
| Yoga | 9.4 (5.15) | −1.02 (−2.13, 0.10) | −2.05 (−3.18, 0.92) | −3.37 (−4.51, −2.23) | |||
| Usual care | 10.3 (5.87) | −0.31 (−1.37, 0.76) | −1.29 (−2.36, −0.22) | −0.89 (−2.02, 0.23) | |||
| Between-group difference | - | −0.71 (−2.25, −0.83) | 0.370 | −0.76 (−2.31, 0.80) | 0.340 | −2.48 (−4.08, −0.87) | 0.003 |
| Pain intensity (BPI) | |||||||
| Yoga | 4.64 (1.76) | −0.39 (−0.72, −0.07) | −0.61 (−0.94, −0.28) | −0.44 (−0.78, −0.11) | |||
| Usual care | 4.68 (2.16) | 0.35 (0.05, −0.66) | 0.04 (−0.27, 0.35) | 0.15 (−0.18, 0.47) | |||
| Between-group difference | - | −0.75 (−1.20, −0.30) | 0.001 | −0.65 (−1.10, −0.20) | 0.005 | −0.59 (−1.05, −0.13) | 0.013 |
Note: Boldface indicates statistical significance (p<0.05).
BPI, Brief Pain Inventory (scale 0–10); RMDQ, Roland-Morris Disability Questionnaire (scale 0–24).
Figure 2.
(A) Mean change in RMDQ scores; (B) mean change in pain-intensity scores.
RMDQ, Roland–Morris Disability Questionnaire; DT, delayed treatment.
For the main secondary outcome (pain intensity), significant differences were observed at all three time points (p=0.001 for 6 weeks, 0.005 for 12 weeks, 0.013 for 6 months), with larger decreases in mean pain intensity for yoga participants (Table 2; Figure 2B). The effect size was relatively small (d=0.30–0.38), and the mean change did not reach clinical significance values of at least 1.0 point.42 When comparing the group proportions of a 1.0-point change or greater, 35% and 39% of the yoga groups versus 18% and 18% of the DT group met this cut off at 12 weeks (p=0.037) and 6 months (p=0.020), respectively.
Analyses examining changes in the use of narcotic pain medication (Appendix Table 1, available online) indicate there were no significant differences between groups, but for the sample as a whole, the proportion of participants using opioid pain medications dropped significantly from 20% to 11% at 12 weeks (p=0.007) and 8% after 6 months (p<0.001). Significant decreases in other medical pain treatments (p=0.001) and self-help pain treatments (p=0.020) were also found across groups after 6 months.
No serious adverse events were reported during the 6-month follow-up period for study participants. Two adverse events were identified. One participant reported increased levels of back pain after one session and declined to attend further. A second participant attended seven consecutive yoga sessions and stopped attending because his “back went out.” Neither participant directly attributed the event to yoga practice.
DISCUSSION
In a sample of VA patients with cLBP, a hatha yoga intervention consisting of postures, breathing, and focused attention did not result in significantly greater improvements at the prespecified primary endpoint of 12 weeks, but the yoga group had significantly greater improvements after 6 months. Participants assigned to the yoga group also had significantly greater reductions in pain intensity than DT participants at all time points, but the magnitude of the reduction in pain was somewhat small. With the exception of the effect of yoga on disability not emerging until 6 months, these findings are generally similar to those described in prior large RCTs of yoga for cLBP27,28 and the conclusions of subsequent meta-analytic reviews.43–45 In a study by Tilbrook et al.,28 yoga participants had greater improvements on the RMDQ than usual-care participants, but no differences were found on pain intensity. Sherman and colleagues27 found that yoga was superior to self-care for improving back-pain specific disability (RMDQ) at 12 weeks and 26 weeks, and for improving pain bother-someness at 12 weeks. The yoga group also had greater reductions in medication use in the Sherman et al. study.
This study extends the major findings on yoga effectiveness for cLBP to a sample of VA patients. VA patients are predominantly male and, on average, are older, have higher rates of psychological disorders and substance use,30 have fewer economic resources, are less educated, more likely identify as a racial/ethnic minority, and are less likely to be employed than the general U.S. population or non–VA veterans.29 Thus, VA patients as a whole face many health challenges, with >62% having a service-connected disability after serving their country.46 As a result, VA patients may require unique approaches to medical care and research. When compared with participants from two previous RCTs of yoga for cLBP (Appendix Table 2, available online), the current sample had a higher mean age, less education, were less likely to be employed, had cLBP 4–5 years longer, had higher rates of opioid medication use, and 18% of participants had been homeless in the last 5 years. Although attendance rates in this study were lower than in previous studies with community samples, many of the same positive effects emerged. This result highlights the importance of yoga home practice, which cannot fully replace instructor-led yoga sessions, but can mitigate attendance challenges when travel is required.
By contrast with the two previous RCTs where an effect was found earlier, significant differences on the RMDQ did not emerge until the 6-month (26 weeks) time point. In the current study, both groups showed reductions in RMDQ scores at the 6-week and 12-week time points, which is not unexpected with comparison groups receiving placebo or usual care in cLBP trials.35,47 However, the initial improvement in RMDQ scores among DT participants was not reflected in the pain-intensity scores. Pain intensity increased slightly and never improved over baseline in the DT group. This finding may be related to the back pain–specific nature of the RMDQ, or the fact that it refers to functional impairment occurring on the day it is administered. This pattern may also suggest that in older participants with a long duration of cLBP, back pain–specific disability may take longer to respond to yoga interventions, while other benefits are more immediate.
In the current study, the size of decreases in RMDQ scores were slightly smaller than those in the Sherman et al.27 study and similar to those in the Tilbrook and colleagues28 study, yet are considered clinically significant.40 The mean decrease in pain intensity for all yoga participants was not clinically significant (1.0 point).39 Among other studies of VA patients with cLBP, a study of walking and online assistance had smaller decreases on the RMDQ at 6 months (1.9 points), but larger decreases in pain intensity than the present study.48 However, reductions in disability and pain intensity for the current study were found despite significant reductions in opioid use (all assessments) and use of other medical and self-help pain treatments at 6 months (Appendix Table 1, available online). Participants were asked not to change any pain treatment unless medically necessary, but many participants sought to reduce medication use and had previously tried many other medical pain treatments with limited success. The size of effects may also have been reduced by some experimental group contamination, with three participants in the DT group acknowledging they had done some yoga during the intervention period despite being asked not to.
Other factors that may have contributed to the magnitude of the health improvements in this study were lower attendance, longer duration of cLBP, and older VA patients. Although definitions of adequate adherence vary, previous full-scale RCTs of yoga for cLBP27,28 reported 60%–67% attending at least half of the 12 sessions. Of note, these studies provided once-weekly yoga. In another RCT, significantly lower adherence rates among twice-weekly yoga sessions were found when compared to once-weekly sessions, but because twice as many sessions were offered, twice-weekly yoga participants attended a median of 16 (of 24) sessions versus 10 (of 12) sessions for once-weekly participants.49 Thus, given the characteristics and challenges faced by VA patients who are older, have more comorbidity, lower incomes, and higher rates of homelessness50,51 than the general U.S. population,29 the attendance rates for this trial were sufficient and not unexpected.
Limitations
A study limitation was that a single yoga instructor taught all intervention classes. The instructor can potentially influence participant receptivity, attendance, and outcomes, and it is unknown whether similar effects would be found for other instructors. This concern may be mitigated by the accumulation of generally similar results across multiple RCTs of yoga for cLBP. Attrition was also higher than expected in the current study, but did not exceed suggested guidelines, at which bias is more likely.52
The delayed treatment comparison group might be viewed as a less rigorous comparator because the groups differ in the amount of professional attention and social contact. However, these differential effects are likely reduced with participants already receiving ongoing health care and engaging in various types of self-care, like exercise. The study was designed prior to the publication of two previous RCTs and yoga for cLBP did not have established efficacy and had not been adequately studied in veterans. Also, yoga is multidimensional and the components that target cLBP have not been identified. Thus, choosing an aspect of yoga (stretching, breathing, meditative, social) to control for remains a challenge.53
CONCLUSIONS
The current study confirms the findings of two prior RCTs showing that yoga interventions are safe and can reduce pain and disability among adults with cLBP. The study also demonstrates the effectiveness of yoga in a sample of military veterans, a population that faces more challenges and may be harder to treat than non-VA populations. When considering future implementation efforts, results suggest that although home practice is important, efforts to facilitate transportation and access to instructor-led sessions should be emphasized. As with other nonpharmacological treatments for cLBP, the effects are small to moderate in size, but can likely be maintained long-term with yoga home practice. Yoga is being offered at >50% of VA facilities nationwide,54 yet most programs are not well integrated into primary care services, may not be delivered with a systematic protocol, capacity may be limited, and awareness of the programs may be low.55 By demonstrating that yoga is an evidence-based treatment for cLBP in military veterans, complementary and integrative health researchers and VA administrators are in a position to begin implementing yoga programs more formally.
Supplementary Material
ACKNOWLEDGMENTS
This research was funded by a grant from Veteran Affairs Rehabilitation Research and Development (Grant #RX000474).
The authors would like to thank Camilla Sinclair, who served as the lead yoga instructor for all main intervention cohorts; Ilanit Young and Eric Eichler who donated time as yoga instructors for delayed treatment sessions; and Debora Goodman, Meghan Maiya, Neil Yetz, and Danielle Casteel who assisted with assessments.
EJG, DGC, JLW, JEB, JHA, and SB were involved in the conceptualization and design of the study. EJG, LL, and LS were involved in the analysis of the data and the initial draft of the manuscript. All authors were involved in interpretation of data, revision of the manuscript, and approved the final version.
Footnotes
No financial disclosures were reported by the authors of this paper.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2017.05.019.
Trial registration: This study is registered at www.clinicaltrials.gov NCT02524158.
REFERENCES
- 1.Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C.An updated overview of clinical guidelines for the management of nonspecific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094. 10.1007/s00586-010-1502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Von Korff M, Saunders K. The course of back pain in primary care. Spine (Phila Pa 1976). 1996;21(24):2833–2837. 10.1097/00007632-199612150-00004. [DOI] [PubMed] [Google Scholar]
- 3.Goulet JL, Kerns RD, Bair M, et al. The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain. 2016;157 (8):1696–1703. 10.1097/j.pain.0000000000000567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehab R D. 2003;40(5):371–379. 10.1682/JRRD.2003.09.0371. [DOI] [PubMed] [Google Scholar]
- 5.Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ. The incidence of low back pain in active duty United States military service members. Spine (Phila Pa 1976). 2011;36(18):1492–1500. 10.1097/BRS.0b013e3181f40ddd. [DOI] [PubMed] [Google Scholar]
- 6.Roy TC. Diagnoses and mechanisms of musculoskeletal injuries in an infantry brigade combat team deployed to Afghanistan evaluated by the brigade physical therapist. Mil Med. 2011;176(8):903–908. 10.7205/MILMED-D-11-00006. [DOI] [PubMed] [Google Scholar]
- 7.Lew HL, Otis JD, Tun C, Kerns RD, Clark ME Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehab R D. 2009;46(6):697–702. 10.1682/JRRD.2009.01.0006. [DOI] [PubMed] [Google Scholar]
- 8.Guo HR, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in U.S. industry and estimates of lost workdays. Am J Public Health. 1999;89(7):1029–1035. 10.2105/AJPH.89.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Currie SR, Wang J. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107(1–2):54–60. 10.1016/j.pain.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 10. Sullivan MJ, Reesor K, Mikail S, Fisher R. The treatment of depression in chronic low back pain: review and recommendations. Pain. 1992;50 (1):5–13. 10.1016/0304-3959(92)90107-M. [DOI] [PubMed] [Google Scholar]
- 11. Manchikanti L, Pampati V, Beyer C, Damron K, Barnhill RC. Evaluation of psychological status in chronic low back pain: comparison with general population. Pain Physician. 2002;5(2):149–155. [PubMed] [Google Scholar]
- 12.Thompson JM, Chiasson R, Loisel P, Besemann LCM, Pranger T. A sailor’s pain Veterans’ musculoskeletal disorders, chronic pain, and disability. Can Fam Physician. 2009;55(11):1085–1088. [PMC free article] [PubMed] [Google Scholar]
- 13.Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res. 2001;10(7):621–635. 10.1023/A:1013171831202. [DOI] [PubMed] [Google Scholar]
- 14.Kosinski MR, Schein JR, Vallow SM, et al. An observational study of health-related quality of life and pain outcomes in chronic low back pain patients treated with fentanyl transdermal system. Curr Med Res Opin. 2005;21(6):849–862. 10.1185/030079905X46377. [DOI] [PubMed] [Google Scholar]
- 15.Murray CJ, Atkinson C, Bhalla K, et al. The state of U.S. health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310 (6):591–608. 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine. 2006;31(23):2724–2727. 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 17.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976). 2004;29(1):79–86. 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 18.Lee D Low back pain intervention: conservative or surgical? J Surg Orthop Adv. 2003;12(4):200–202. [PubMed] [Google Scholar]
- 19.Von Korff M, Moore JC. Stepped care for back pain: activating approaches for primary care. Ann Intern Med. 2001;134(9 Pt 2):911–917. 10.7326/0003-4819-134-9_Part_2-200105011-00016. [DOI] [PubMed] [Google Scholar]
- 20.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147 (7):478–491. 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 21.Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):505–514. 10.7326/0003-4819-147-7-200710020-00008. [DOI] [PubMed] [Google Scholar]
- 22.Banerjee G, Edelman EJ, Barry DT, et al. Non-medical use of prescription opioids is associated with heroin initiation among U.S. veterans: a prospective cohort study. Addiction. 2016;111(11):2021–2031. 10.1111/add.13491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller M, Barber CW, Leatherman S, et al. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175(4):608–615. 10.1001/jamainternmed.2014.8071. [DOI] [PubMed] [Google Scholar]
- 24.Di Iorio D, Henley E, Doughty A. A survey of primary care physician practice patterns and adherence to acute low back problem guidelines. Arch Fam Med. 2000;9(10):1015–1021. 10.1001/archfami.9.10.1015. [DOI] [PubMed] [Google Scholar]
- 25.Freburger JK, Carey TS, Holmes GM. Physician referrals to physical therapists for the treatment of spine disorders. Spine J. 2005;5(5):530–541. 10.1016/j.spinee.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an APS/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):A492–A504. 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 27.Sherman KJ, Cherkin DC, Wellman RD, et al. A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch Intern Med. 2011;171(22):2019–2026. 10.1001/archinternmed.2011.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain: a randomized trial. Ann Intern Med. 2011;155(9):569–578. 10.7326/0003-4819-155-9-201111010-00003. [DOI] [PubMed] [Google Scholar]
- 29.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160 (21):3252–3257. 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 30.Finney JW, Willenbring ML, Moos RH. Improving the quality of VA care for patients with substance-use disorders: the Quality Enhancement Research Initiative (QUERI) substance abuse module. Med Care. 2000;38 (6 suppl 1):I105–I113. 10.1097/00005650-200006001-00011. [DOI] [PubMed] [Google Scholar]
- 31.Groessl EJ, Weingart KR, Aschbacher K, Pada L, Baxi S. Yoga for veterans with chronic low-back pain. J Altern Complement Med. 2008;14(9):1123–1129. 10.1089/acm.2008.0020. [DOI] [PubMed] [Google Scholar]
- 32.Groessl EJ, Weingart KR, Johnson N, Baxi S. The benefits of yoga for women veterans with chronic low back pain. J Altern Complement Med. 2012;18(9):832–838. 10.1089/acm.2010.0657. [DOI] [PubMed] [Google Scholar]
- 33.Groessl EJ, Schmalzl L, Maiya M, et al. Yoga for veterans with chronic low back pain: design and methods of a randomized clinical trial. Contemp Clin Trials. 2016;48:110–118. 10.1016/j.cct.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 34.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000;25(24): 3115–3124. 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 35.Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016;315(12):1240–1249. 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 37.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5): 309–318. 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Wetherell JL, Afari N, Rutledge T, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain. 2011;152(9):2098–2107. 10.1016/j.pain.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 39.Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001;28(2):431–438. [PubMed] [Google Scholar]
- 40.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33(1):90–94. 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 41.Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of Longitudinal Data. Oxford, UK: Oxford University Press, 2002. [Google Scholar]
- 42.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Chou R, Deyo R, Friedly J, et al. Noninvasive Treatments for Low Back Pain. February Report No.: 16-EHC004-EF. Rockville, MD: Agency for Healthcare Research and Quality, 2016. [PubMed] [Google Scholar]
- 44. Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29(5):450–460. 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 45.Goode AP, Coeytaux RR, McDuffie J, et al. An evidence map of yoga for low back pain. Complement Ther Med. 2016;25:170–177. 10.1016/j.ctim.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 46.Department of Veterans Affairs. Annual Benefits Reports, 2000 to 2013; Veterans Health Administration, Table A: VHA Enrollment, Expenditures, and Patients National Vital Signs, September Reporting 2000 to 2013. Washington, DC: Veterans Benefits Administration, National Center for Veterans Analysis and Statistics, 2015. [Google Scholar]
- 47.Atkinson JH, Slater MA, Williams RA, et al. A placebo-controlled randomized clinical trial of nortriptyline for chronic low back pain. Pain. 1998;76(3):287–296. 10.1016/S0304-3959(98)00064-5. [DOI] [PubMed] [Google Scholar]
- 48.Krein SL, Kadri R, Hughes M, et al. Pedometer-based internet-mediated intervention for adults with chronic low back pain: randomized controlled trial. J Med Internet Res. 2013;15(8):e181 10.2196/jmir.2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saper RB, Boah AR, Keosaian J, Cerrada C, Weinberg J, Sherman KJ. Comparing once- versus twice-weekly yoga classes for chronic low back pain in predominantly low income minorities: a randomized dosing trial. Evid Based Complement Alternat Med. 2013;2013:658030 10.1155/2013/658030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Office of Planning and Community Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress, Part 1: Point-in-Time Estimates of Homelessness. Washington, DC: Department of Housing and Urban Development, 2013. [Google Scholar]
- 51.Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100(7):1326–1333. 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34(18):1929–1941. 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 53.Park CL, Groessl E, Maiya M, et al. Comparison groups in yoga research: a systematic review and critical evaluation of the literature. Complement Ther Med. 2014;22(5):920–929. 10.1016/j.ctim.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cottreau M, Kotar T, Schelach K, et al. FY 2015 VHA Complementary and Integrative Health (CIH) Services. Washington DC: Healthcare Analysis & Information Group, Department of Veterans Affairs, 2015. [Google Scholar]
- 55.Taylor S, Bolton R, Huynh A, Dvorin K, Elwy R, Bokhour BG. Facilitators, Challenges and Strategies to Adopting and Implementing Complementary and Integrative Health Therapies. Washington, DC: Department of Veterans Affairs, Office of Patient-Centered Care and Cultural Transformation and Health Services Research and Development, Quality Enhancement Research Initiative, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.