Abstract
Long noncoding RNAs (lncRNAs) are non-protein coding RNAs of more than 200 nucleotides in length. Despite the term “noncoding”, lncRNAs have been reported to be involved in gene expression. Accumulating evidence suggests that lncRNAs play crucial roles in the regulation of immune system and the development of autoimmunity. lncRNAs are expressed in various immune cells including T lymphocytes, B lymphocytes, macrophages, neutrophils, dendritic cells, and NK cells, and are also involved in the differentiation and activation of these immune cells. Here, we review recent studies on the role of lncRNAs in immune regulation and the differential expression of lncRNAs in various autoimmune diseases.
Keywords: RNA, long noncoding; Immune system; Autoimmunity; Autoimmune diseases
INTRODUCTION
Large portions of the human genome, which had previously been considered as ‘transcriptional noise’ with no coding capacity as protein-coding genes, are estimated to be less than 2% of whole genome (1). The ENCyclopedia of DNA Element Consortium reported that most of the genome is transcribed as non-protein coding RNA (ncRNA) (2). Many recent studies have revealed that ncRNAs are important regulators of gene expression and also play important roles in the pathogenesis of various diseases. ncRNAs are largely categorized into small ncRNAs (<200 nucleotides [nt]) and long ncRNAs (lncRNAs) (>200 nt) according to their transcript size (3). A great deal of research has been focused on microRNAs (miRNAs), one type of small ncRNA. miRNAs have been reported to be involved in the regulation of gene expression and development of autoimmune diseases including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), systemic sclerosis, Sjögren's syndrome (SS), multiple sclerosis, and type 1 diabetes mellitus (4,5).
Recently, researchers have started to pay more attention to lncRNAs, which account for major portion of ncRNAs. Compared with miRNAs, the mechanisms of lncRNA function are more diverse due to structural complexity of lncRNAs (3,6). Early studies primarily showed that lncRNAs are related to diverse cellular responses, including cell differentiation, cell proliferation, and apoptosis (7,8,9). Cancer, along with cardiovascular and neurological diseases, was the main focus of lncRNA research (10). However, more recently, accumulating evidence that lncRNAs participate in immune cell differentiation and immune responses, suggests that lncRNAs are essential components in the development of autoimmune diseases (11,12,13,14,15). In this review, we are going to introduce classification, and mechanism of action of lncRNAs, the influences of lncRNAs on various immune cells, and the role of lncRNAs in autoimmune diseases such as SLE, RA, polymyositis (PM)/dermatomyositis (DM), and SS.
CATEGORIZATION OF LNCRNAS
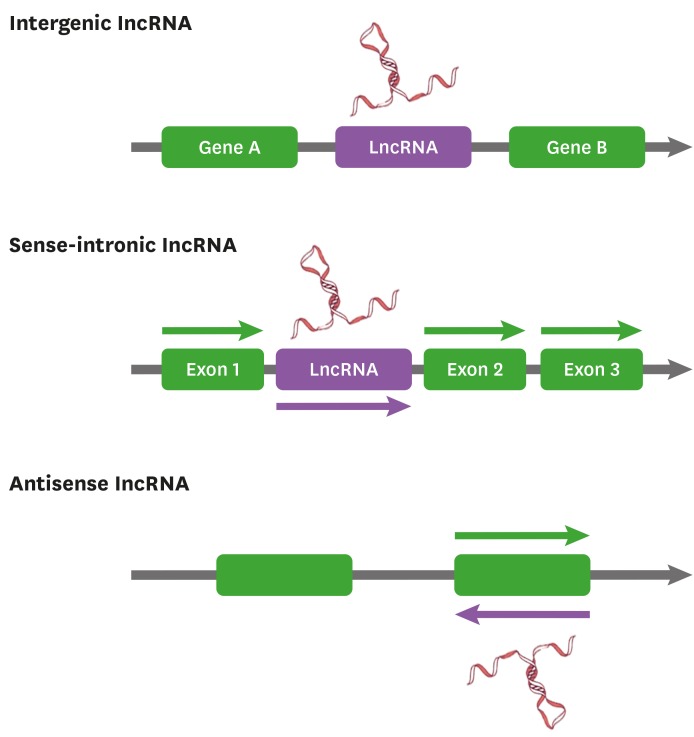
The lncRNAs are more categorized according to various genomic architectures as well as functional mechanisms (Fig. 1). Based on location in the genome, lncRNAs can be divided into intergenic lncRNAs (lincRNAs) and intronic lncRNAs (3,16). LincRNAs are transcribed inter genetically from both DNA strands which do not overlap protein-coding genes. Whereas intronic lncRNAs are transcribed from introns of protein-coding genes in either direction and terminate without overlapping exons. Thus, lincRNAs and intronic lncRNAs could be regulated via different transcription activation mechanisms. In addition, lncRNAs are also classified regarding the product orientation of the DNA strand (17,18). Sense lncRNAs are transcribed from the sense strand of protein-coding genes and contain exons that overlap with part of protein-coding genes or cover the entire sequence of a protein-coding gene containing an intron. On the contrary, antisense lncRNAs are transcribed from the antisense strand of the protein-coding genes that overlap with exon or intron regions, which cover the entire protein-coding gene. Interestingly, most of the lncRNAs are discovered from protein-coding genes or the antisense of the protein-coding genes using cap-analysis gene expression and oligo-dT guided reverse transcription, suggesting that they also possess 5′ cap and 3′ poly-A tail like mRNA (19).
Figure 1. Classification of lncRNAs. The lncRNAs can be classified based upon genomic structures and product orientation of the DNA strand. Based on genomic location, lncRNAs are divided into lincRNAs and intronic lncRNAs. And, according to the direction of transcription, lncRNAs can be classified into sense and antisense lncRNAs.
LNCRNAS AS POTENT GENE REGULATORS
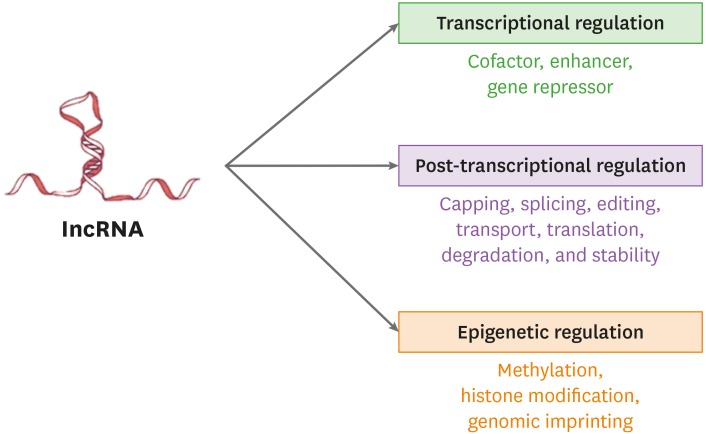
Recent studies have shown that lncRNAs are involved in various gene transcription regulation mechanisms through interactions with transcription factors or epigenetic modifiers (Fig. 2). lncRNAs can play as cofactors to modify the activity of transcription factors. For instance, NF-κB-interacting lncRNA binds NF-κB/IκB in a ternary complex, which inhibits IKK-mediated IκB phosphorylation by directly masking the phosphorylation sites (20). lncRNA-Evf2 is transcribed from conserved distal enhancer and recruits the transcription factor DlX2 to the same enhancer to induce expression of adjacent protein-coding genes (21). Some lncRNAs are also involved in post-transcriptional regulation of mRNAs such as capping, splicing, editing, transport, translation, degradation, and stability at various control sites. The lncRNA metastasis-associated lung adenocarcinoma transcript 1 is known to regulate alternate splicing by interacting with multiple splicing factors (22). In addition, lncRNA Gomafu/myocardial infarction-associated transcript is localized to a nuclear domain, which may block spliceosome formation and affect the mRNA splicing by sequestering splicing factor 1 (23).
Figure 2. Functions of lncRNAs. lncRNAs regulate gene transcription through interactions with transcription factors or epigenetic modifications. lncRNAs can change activity of transcription factor, or regulate post-transcriptional events of mRNAs, or modify epigenetically.
Epigenetic modifications are widely known important gene transcription regulation mechanism. In this context, lncRNAs (antisense non-coding RNA in the INK4 locus [ANRIL], X-inactive specific transcript, HOX transcript antisense RNA [HOTAIR], and KCNQ1 opposite strand/antisense transcript 1 [KCNQ1OT1]) have crucial roles as epigenetic regulators. lncRNA KCNQ1OT1 binds to polycomb repressive complex 2 (PRC2) and the methyl-transferase G9a (EHMT2), whereas ANRIL binds to PRC1 and PRC2 (24). lncRNA HOTAIR forms histone modifying complexes, which coordinates the targeting of specific repressive histone modifying complexes (25). Additionally, lncRNAs have also been proven to X chromosome inactivation, gene silencing, and gene imprinting via regulation of DNA methyltransferases (24,26).
REGULATION OF THE IMMUNE SYSTEM BY LNCRNAS
Dysregulation of the immune system can be a major cause of the development of various autoimmune diseases, as well as infectious diseases and cancers. The regulation of gene expression involved in the immune system is particularly crucial for making decisions between immune tolerance and autoimmunity. Recently, increasing evidence has revealed that lncRNAs play an important role in the regulation of the immune system. However, to date, the study of lncRNAs in immune system regulation remains challenging due to the complexity and diversity of the immune system. The immune system is roughly divided into innate and adaptive immunities. Coordination of innate and adaptive immune responses has a critical role in biological and pathological immune responses. Here, we are going to review the roles of lncRNAs in immune responses. Table 1 shows representative lncRNAs that regulate immune responses.
Table 1. Summary of lncRNAs involved in immune responses.
| Type of immunity | Source | lncRNAs | Function | Mechanism of action | Reference |
|---|---|---|---|---|---|
| Innate immunity | Myeloid cell | Morrbid | Control lifespan of short-lived myeloid cells (neutrophils, eosinophils, monocytes) | Inhibiting Bcl2l11 (Bim) transcription | (30) |
| DC | lnc-DC | DC differentiation | Phosphorylating STAT3 | (13) | |
| DC macrophage | lincRNA-Cox2 | Regulate expression of proinflammatory genes | Interacting with hnRNP-A/B and hnRNP-A2/B1 | (15) | |
| Macrophage | THRIL | Positively regulate TNF-α expression | Interacting with hnRNPL | (37) | |
| Macrophage | mcircRasGEF1B | Positively regulate ICAM-1 expression | Acting as a miRNA sponge | (38) | |
| Monocyte | PACER | Induce PTGS2 expression | Sequestrating NF-κB subunit p50 | (39) | |
| Monocyte macrophage | lincRNA-EPS | Restrain inflammation | Binding to hnRNPL | (40) | |
| Erythrocyte | |||||
| Macrophage | lnc13 | Restrain inflammation | Binding to hnRNPL | (41) | |
| Fibroblast | Lethe | Restrain inflammation | Binding to NF-κB subunit RelA | (42) | |
| Adaptive immunity | Th1 cell | linc-MAF-4 | Induce Th1 cell differentiation | Suppressing MAF expression | (43) |
| Th2 cell | lincR-Ccr2-5′AS | Induce Th2 cell migration | In a GATA-3 dependent manner | (44) | |
| Th2 cell | TH2-LCR | Positively regulate the transcription of Th2 cytokine gene | Recruiting WDR5-containing complexes | (14) | |
| Th1 cell CD8+ T cell | NeST (Tmevpg1) | Enhance IFN-γ expression | Binding to WDR5 | (47) | |
| CD8+ T cell | lncRNA-CD244 | Suppress TNF-α and IFN-γ expression | Recruiting EZH2 to the Ifng and Tnf promoters | (50) | |
| T cell | NRON | Maintain resting state of T cells | Sequestering phosphorylated NFAT in the cytoplasm | (51) | |
| Treg cell | lnc-EGFR | Stimulate Treg differentiation | Binding to EGFR and inhibiting interaction between EGFR and c-CBL | (53) | |
| B cell | FAS-AS1 | Enhance Fas-mediated apoptosis in B cell lymphoma | Binding to RBM5 and inhibiting RBM5-mediated alternative splicing of FAS pre-mRNA | (54) |
The role of lncRNAs as regulators of innate immunity
Innate immunity is defined as the first line of host defense against pathogens and induces adaptive immune system to conduct effector functions (27,28). The innate immune system is mainly mediated by dendritic cells (DCs), macrophages, and NK cells (29).
There is a lncRNA associated with the regulation of the life span in short-lived myeloid cells. Myeloid RNA regulator of Bim-induced death (Morrbid) is a lncRNA which is highly expressed in short-lived myeloid cells such as neutrophils, eosinophils, and ‘classical’ monocytes (30). These short-lived myeloid cells provide the first line of defense against pathogens and the regulation of their life span is vital for protective host immune responses (31,32). Morrbid has been reported to control the lifespan of these cells by repressing the transcription of the pro-apoptotic gene, Bcl2l11, which encodes Bim (30). The expression of Morrbid can be induced by cytokines of the common β-chain receptor family (IL-3, IL-5, and GM-CSF) in vitro (30). Eosinophils from patients with high plasma concentrations of IL-5, who have hypereosinophilic syndrome, show high expression of Morrbid compared with eosinophils from healthy controls (30,33). The expression of Morrbid in eosinophils is also positively correlated with plasma IL-5 concentrations (30). The findings suggest that Morrbid might have a significant role in diseases which are related with altered lifespans of short-lived myeloid cells.
DCs are the primary antigen presenting cells for T cells and act as initiators of innate and adaptive immunity (34). Human DCs exclusively express the lncRNA lnc-DC, which was discovered by transcriptome microarray analysis and RNA sequencing (13). When common myeloid progenitor cells or monocytes differentiate into DCs, the expression of lnc-DC is upregulated. lnc-DC knockdown causes considerable change in the regulation of DC function-related genes. Knockdown of lnc-DC diminishes the ability of DCs to uptake antigens and results in the downregulation of molecules associated with T cell activation, including CD40, CD80, CD86, and HLA-DR, and the impairment of CD4+ T cell proliferation and attenuation of IL-12 production upon LPS stimulation (13). lnc-DC, which usually functions in the cytoplasm, interacts with STAT3 required for DC development and function, preventing it from binding to the tyrosine-phosphatase SHP1. Phosphorylation of STAT3 at Tyr705 by lnc-DC leads to translocation of STAT3 to the nucleus, and consequently promotes DC differentiation and activation of the immune system (13,35). These data suggest that lnc-DC is crucial for DC differentiation and functions.
There are lncRNAs involved in the induction of inflammation. The expression of lincRNA-cyclooxygenase 2 (Cox2) is markedly upregulated after stimulation with TLR4 agonist in CD11C+ bone marrow-derived human DCs (36). TLR2 ligation induces the expression of lincRNA-Cox2 in murine bone marrow-derived macrophages (15). TLR4 and TLR7/8 ligands also leads to increased expression of both lincRNA-Cox2 and the Ptgs2 (also known as Cox2) gene via the Myd88-NF-kB signaling pathway (15). LincRNA-Cox2 controls the transcription of genes associated with the inflammatory response by interacting with heterogeneous nuclear ribonucleoprotein (hnRNP)-A/B and -A2/B1 (15).
The lncRNA TNF-α and hnRNPL related immunoregulatory lincRNA (THRIL) (also known as linc1992), which is induced by activation of TLR2 signaling in human THP1 macrophages, is a regulator of TNF-α induction. Knockdown of THRIL results in reduced expression of TNF-α mRNA and protein in macrophage cells (37). THRIL binds to hnRNPL and upregulates TNF-α gene transcription (37). Knockdown of Hnrpl leads to a reduction in the levels of TNF-α produced by macrophages.
Mouse circRasGEF1B (mcircRasGEF1B), which is a kind of circular RNA, is expressed in macrophages induced by LPS. LPS-induced expression of mcircRasGEF1B is dependent on NF-κB. The action of mcircRasGEF1B is like a ‘sponge’ for miRNA, which targets intercellular adhesion molecule 1 (ICAM-1) (38). Knockdown of mcircRasGEF1B in LPS-activated macrophages reduces ICAM-1, which is important to initiate inflammation by homing leukocytes to inflammatory sites (38).
The lncRNA p50-associated COX-2 extragenic RNA (PACER) is expressed in human monocytes after stimulation with LPS (39). PACER induces PTGS2, which encodes Cox-2, by sequestrating the NF-κB subunit p50 away from the PTGS2 promoter (39). PACER acts as an activator of the inflammatory response.
There are also lncRNAs associated with restrain inflammatory responses. LincRNA erythroid prosurvival (lincRNA-EPS) is expressed in DCs, macrophages, and erythrocytes. lincRNA-EPS is thought to repress inflammation by binding to hnRNPL. A previous study showed that inflammation was induced in lincRNA-EPS-deficient mice (40).
Similar to lincRNA-EPS, lnc13 functions as a suppressor of inflammation. The expression of lnc13 is observed in macrophages and TLR4 ligation downregulates its expression (41). By binding hnRNPD, lnc13 inhibits immune response genes (41).
The pseudogene lncRNA Lethe, which is named after the ‘river of forgetfulness’ in Greek mythology, is induced in mouse embryonic fibroblasts stimulated by proinflammatory cytokines such as IL-1β and TNF-α (42). Lethe exerts negative regulatory functions upon NF-κB; knockdown of Lethe results in the upregulation of NF-κB targets while overexpression of Lethe decreases the activity of an NF-κB reporter (42). Lethe acts by binding to the NF-κB subunit RelA, inhibiting the formation of active NF-κB complexes. Lethe functions as a restrictor of inflammatory responses.
The role of lncRNAs as regulators of adaptive immunity
Adaptive immunity is highly specific. Pathogen-induced innate immune responses trigger antigen-specific adaptive immune responses. The adaptive immune system mainly consists of T and B cells. Emerging evidence indicates that lncRNAs are associated with adaptive immune responses, although their role is not yet fully understood.
lncRNAs in T cell responses
The lncRNA linc-MAF-4 represses the expression of MAF, a Th2-associated transcription factor and drives T cell differentiation into Th1 cells (42). Downregulation of linc-MAF-4 induces T cell differentiation toward the Th2 cell lineage (43). The linc-MAF-4 recruits chromatin modifiers such as lysine-specific demethylase 1 and enhancer of zeste homolog 2 (EZH2) and inhibits MAF transcription (43). These results suggest that linc-MAF-4 is an important regulator of CD4+ T cell differentiation.
The lncRNA lincR-Ccr2-5′AS is specifically expressed in Th2 cells (44). The lincR-Ccr2-5′AS, which is located at the 5′ end of Ccr2 and expressed via antisense transcription, plays a crucial role in controlling the migration of Th2 cells. GATA-3, the transcription factor of Th2 cells, regulates the expression of lincR-Ccr2-5′AS. The genes, which undergo changes in their expression following lincR-Ccr2-5′AS knockdown, considerably overlap with GATA-3-dependent genes. lincRNA-Ccr2-5′AS is closely related with genes encoding Th2 cell chemokines, including Ccr1, Ccr2, Ccr3, and Ccr5. A previous murine experiment demonstrated that lincR-Ccr2-5′AS-depleted Th2 cells showed impaired migration to lung tissue after in vivo transfer, as compared with lincR-Ccr2-5′AS-sufficient Th2 cells (44).
lncRNA TH2-locus control region (LCR) is located at the 3′ end of the RAD50 gene that encodes a double-strand-break repair protein (45). TH2-LCR positively regulates the transcription of genes that encode Th2 cell cytokines including IL-4, IL-5, and IL-13 (14). The function of TH2-LCR might be associated with the recruitment of the WD40 repeat protein 5 (WDR5)-containing complex to the targeted genomic elements. A previous study has revealed that depletion of TH2-LCR reduces WDR5 recruitment to IL-4 and IL-13, but no changes were found for IL-5 (45).
The lncRNA nettoie Salmonella pas Theiler's (NeST, also known as Theiler's murine encephalomyelitis virus persistence candidate gene 1 [Tmevpg1]) is expressed in Th1 cells, CD8+ T cells, and NK cells (46,47,48). NeST, which is located in the adjacent region to the IFN-γ encoding gene, is the lncRNA associated with T cell activation (49). The expression of NeST depends on the activities of the Th1 transcription factors STAT4 and T-bet, and NF-κB (44,47,48). The expression of NeST leads to the enhancement of IFN-γ production from activated CD8+ T cells. NeST binds to WDR5 and recruits the transcription-activation complex to the Ifng promoter, inducing the transcription of Ifng.
The lncRNA lncRNA-CD244, which functions in CD8+ T cells, is associated with the inhibition of T cell activation (50). CD244, a T cell inhibitory molecule, induces the expression of lncRNA-CD244 and lncRNA-CD244 mediates the suppression of TNF-α and IFN-γ by interacting with EZH2. In contrast, knockdown of lncRNA-CD244 increases the expression TNF-α and IFN-γ and improves CD8+ T cell function.
The lncRNA noncoding repressor of NFAT (NRON) was one of the first lncRNAs discovered in T cells. NRON represses T cell activation by inactivating the calcium-dependent transcription factor, NFAT (51). NFAT exists in a phosphorylated state under steady-state condition, but becomes dephosphorylated when the concentration of intracellular calcium increases (51,52). Dephosphorylated NFAT then translocates to the nucleus, inducing T cell activation. NRON sequesters phosphorylated NFAT in the cytoplasm, preventing its translocation to the nucleus. Depletion of NRON, therefore, leads to the nuclear translocation of NFAT, resulting in T cell activation (52).
There is a report that the lncRNA lnc-epidermal growth factor receptor (lnc-EGFR) stimulates Treg differentiation in hepatocellular carcinoma (HCC) tissues (53). Jiang et al. (53) revealed that increased expression of lnc-EGFR in CD4+ T cells was linked with Treg polarization in HCC. lnc-EGFR, which binds to EGFR specifically, blocks EGFR ubiquitination by inhibiting the interaction between EGFR and ubiquitin ligase, casitas B-lineage lymphoma (c-CBL). As EGFR ubiquitination by c-CBL leads to EGFR degradation, blocking EGFR ubiquitination results in maintenance of EGFR activation. So, lnc-EGFR maintains activation of EGFR by inhibiting the interaction between EGFR and c-CBL, leading to the stimulation of Treg differentiation.
lncRNAs in B cell responses
There is a report showing that the lncRNA Fas-antisense 1 (FAS-AS1) regulates B cell function indirectly (54). In human B cell lymphoma, the expression of FAS-AS1 induces Fas-mediated apoptosis. FAS-AS1 binds to RNA-binding motif protein 5 (RBM5) and inhibits RBM5-mediated alternative splicing of FAS pre-mRNA. Alternative splicing of FAS pre-mRNA leads to the inhibition of cell apoptosis.
THE ROLE OF LNCRNAS IN AUTOIMMUNE DISEASES
Autoimmune diseases are thought to be caused by a complex combination of interactions involving genetic, immunological, and environmental factors. In the past, autoimmune diseases were considered to be rare, but now the overall prevalence of autoimmune diseases is reported to be about 3%–5% in the general population, according to improved diagnostic modalities (55,56). Despite significant advances in revealing the pathogenesis of autoimmune diseases, the pathogenesis of autoimmune diseases is not yet fully understood. The evidence that lncRNA is involved in immunological responses indicates that the dysregulation of lncRNAs participates in the pathogenesis of autoimmune diseases. Table 2 shows representative lncRNAs that are involved in the development of autoimmune diseases.
Table 2. Summary of lncRNAs involved in autoimmune diseases.
| Autoimmune disease | lncRNAs | Source | Clinical application | Reference |
|---|---|---|---|---|
| SLE | NEAT1 | PBMCs | Positively correlate with SLEDAI | (61) |
| Gas5 | Plasma | Negatively correlate with ESR and SLEDAI-2K | (65) | |
| CD4+ T cell | ||||
| B cell | ||||
| RA | HOTAIR | PBMCs | Overexpressed in PBMCs, serum exosome of RA | (71) |
| Serum exosome | Suppressed in differentiated osteoclast and rheumatoid synoviocytes | |||
| Osteoclast | ||||
| Synoviocyte | ||||
| H19 | Synovial tissue | Overexpressed in RA synovial tissue | (72) | |
| lincRNA-p21 | Whole blood | Suppressed in RA | (73) | |
| LOC100652951 | T cell | Overexpressed in RA | (74) | |
| LOC100506036 | ||||
| ENST00000483588 | FLS | Overexpressed in RA | (87) | |
| Positively correlated with C-reactive protein and simplified disease activity index score | ||||
| ENST00000438399 | FLS | Suppressed in RA | (87) | |
| uc004afb.1 | ||||
| ENST00000452247 | ||||
| GAPLINC | FLS | Overexpressed in RA | (75) | |
| DM | ENST00000541196.1 | Muscle | Overexpressed in DM | (81) |
| uc011ihb.2 | ||||
| linc-DGCR6-1 | ||||
| ENST00000551761.1 | Muscle | Decreased in DM | (81) | |
| ENST00000583156.1 | ||||
| SS | Tmevpg1 | CD4+ T cell | Overexpressed in SS | (86) |
| Correlate with SSA, ESR, IgG |
lncRNAs in SLE
SLE is a systemic autoimmune disease characterized by generation of multiple autoantibodies and immune complex deposition, resulting in damage to organs including the kidneys, lungs, brain, and heart (57). Although the pathogenesis of SLE remains unclear, accumulating evidence suggests that lncRNAs might contribute to its development.
Dysregulated TLR4 signaling have been reported to be associated with the development of SLE (58,59,60). There is a lncRNA, which is associated with SLE by the regulation of TLR4 signaling. A previous study found that the lncRNA nuclear enriched abundant transcript 1 (NEAT1) is associated with the pathogenesis of SLE (61). NEAT1 was upregulated in PBMCs of patients with SLE compared to that in the PBMCs of healthy controls. The expression of NEAT1 was positively correlated with SLE Disease Activity Index (SLEDAI) score which is an index for measuring clinical disease activity of SLE. In vitro study with human monocytic cell line, NEAT1 expression was increased after LPS stimulation. Silencing NEAT1 with siRNA in LPS-stimulated human monocytic cell line led to reduced expression of IL-6, CCL2, and CXCL10, which are reported to be involved in the pathogenesis of SLE. NEAT1 is also involved in the TLR4-mediated inflammatory response by affecting the activation of late mitogen-activated protein kinase signaling pathways.
Recent genome-wide association studies showed that chromosomal region 1q25 is an SLE-susceptible locus (62). The genetic evidence that the lncRNA growth arrest-specific transcript 5 (Gas5) is located within chromosome region 1q25 indicates a possible relationship between Gas5 and SLE susceptibility (63). In the murine model of SLE, Gas5 was linked with increased SLE susceptibility (64). Moreover, in human SLE, the expression of Gas5 in plasma, as well as in CD4+ T cells and B cells, was decreased in patients with SLE compared with healthy controls (65). Furthermore, the plasma expression levels of Gas5 were negatively correlated with erythrocyte sedimentation rates (ESR) and SLEDAI-2K scores in patients with SLE (65).
lncRNAs in RA
RA is a chronic autoimmune disease characterized by synovial inflammation and proliferation, which leads to severe joint destruction. The main clinical symptoms of RA include peripheral joint pain, swelling, and joint deformity, though RA can also affect systemic organs including the lungs, heart, and eyes. RA is a multifactorial disease in which host genetic factors, aberrant immune responses, and environmental factors can all contribute to its development (66,67,68). Recently, several studies have demonstrated that dysregulated lncRNAs play a critical role in the pathogenesis of RA.
One of the first mentioned lncRNAs in RA is HOTAIR. HOTAIR was previously reported as playing an important role in the pathogenesis of cancers (69,70). In 2015, Song et al. (71) reported that expression of HOTAIR was upregulated in PBMCs and the serum exosome of patients with RA compared to healthy controls. Moreover, upregulated HOTAIR can promote the migration of active macrophages while downregulated HOTAIR, which was observed in differentiated osteoclasts and rheumatoid synoviocytes, can inhibit the production of matrix metalloproteinase (MMP)-2 and MMP-13. These results indicate that aberrant expression of HOTAIR is involved in the pathogenesis of RA.
H19 was reported to be overexpressed in the synovial tissues of patients with RA compared with those from normal/joint trauma controls (72). Song et al. (71) also reported that high expression of H19 was observed in PBMCs from patients with RA compared to normal PBMCs based on microarray analysis, but microarray analysis data produced from serum exosomes did not support the results. Further studies are therefore needed to determine the role of H19 in the pathogenesis of RA.
A previous study reported that there is a relationship between depressed levels of lincRNA-p21 and increased NF-κB activity in patients with RA (73). In the study, Spurlock et al. (73) demonstrated that the expression of lincRNA-p21 was lower in whole blood from patients with RA, while expression of phosphorylated p65 (RelA), which is a marker of NF-κB activation, was higher compared to that in control subjects. Methotrexate (MTX)-untreated RA patients showed reduced expression levels of lincRNA-p21 and increased levels of p65 compared to MTX-treated RA patients. An in vitro study using primary cells and transformed cell lines showed that MTX upregulated the expression of lincRNA-p21 via DNA-dependent protein kinase catalytic subunit (DNA PKcs). In addition, MTX suppressed NF-κB activity in TNF-α-treated cells in a DNA PKcs-dependent manner, through the induction of lincRNA-p21.
Lu et al. (74) found that lncRNAs, LOC100652951 and LOC100506036, were overexpressed in T cells from patients with RA compared to controls. Use of biological agents reduced the expression levels of LOC100652951 in patients with RA. After activation of Jurkat cells with phorbol 12-myristate 13-acetate and ionomycin, upregulated expression of LOC100506036, but not LOC100652951, was observed. Furthermore, knockdown of LOC100506036 in activated Jurkat cells leads to the downregulation of sphingomyelin phosphodiesterase 1 and NFAT, both of which contribute to inflammatory responses.
There was a report that the expression of lncRNA ENST00000483588 was increased and that the expression of three lncRNAs, including ENST00000438399, uc004afb.1, and ENST00000452247, were decreased in fibroblast-like synoviocytes (FLS) from patients with RA compared to controls (74). Among four lncRNAs, the expression level of ENST00000483588 showed a positive relationship with C-reactive protein and the disease activity index score of RA. The results suggest that those lncRNAs may play a role in the pathogenesis of RA, although further studies are needed to confirm this.
Recently, Mo et al. (75) reported the relationship between lncRNA gastric adenocarcinoma predictive long intergenic noncoding RNA (GAPLINC) and RA. The expression level of GPALINC was higher in FLS from patients with RA than in FLS from patients with traumatic injuries. GPALINC knockdown suppressed proliferation, migration, invasion, and the production of inflammatory cytokines and proteinases in RA FLS. Given that silencing of GAPLINC led to the increased expression of miR-382-5p and miR-575, GAPLINC is thought to play a role as a miRNA sponge. The results suggest the possibility that aberrant regulation of lncRNA GAPLINC contributes to the development of RA.
lncRNAs in PM/DM
PM and DM are idiopathic inflammatory myopathies which share some clinical features and show increased serum levels of muscle enzymes (76,77,78). PM and DM both present with symmetric, proximal muscle weakness and can also present with interstitial lung disease. However, they differ in some clinical aspects such as the presence of skin lesions, the histopathology of affected muscle, and prognosis.
There is a report that PM/DM are related with lncRNA 7SL expression, which is the RNA component of signal recognition particle (SRP) (79). It is well-known that patients with DM or PM can have autoantibodies against SRP (80). In the study, PM/DM patients with anti-SRP antibodies were shown to also possess autoantibodies against 7SL RNA. The presence of autoantibodies against 7SL RNA is also related with ethnic background, clinical manifestations, and seasonal onset of the disease. The study suggests that autoantibodies against 7SL RNA may be used as a serological marker for a subset of PM/DM.
Peng et al. (81) found 1,198 differentially expressed lncRNAs in muscles from patients with DM compared with muscles from healthy controls, using a microarray analysis. Among those lncRNAs, they validated five lncRNAs, including ENST00000541196.1, uc011ihb.2, linc-DGCR6-1, ENST00000551761.1, and ENST00000583156.1. According to their bioinformatics prediction, linc-DGCR6-1 regulates the USP18 gene, which is type 1 interferon-inducible gene and is mainly found in perifascicular areas of muscle fibers in patients with DM. These results indicate that dysregulated lncRNAs can play a role in the pathogenesis of DM.
lncRNAs in SS
SS is a chronic, systemic autoimmune disease characterized by dry eye and dry mouth symptoms resulting from inflammation of exocrine glands (82). In addition to glandular manifestations, patients with SS can have various extraglandular manifestations which include pulmonary, skin, articular, renal, and neurological manifestations (83). The production of autoantibodies against SSA or SSB is one of the hallmarks of SS (84). The pathogenesis of SS is multifactorial and is not yet fully understood.
Among various immunologic factors causing SS, Th1 response has been reported to be play an important role in the development of SS (85). There is a study that lncRNA Tmevpg1, which is known to regulate Th1 responses, is implicated in the pathogenesis of SS. The study suggests that there is a relationship between SS and lncRNA Tmevpg1 (86). Increased expression of Tmevpg1 was observed in CD4+ T cells in patients with SS compared with CD4+ T cells of healthy donors. The study also revealed that the expression levels of Tmevpg1 were correlated with the presence of SSA, as well as the levels of ESR and IgG. This study indicates that lncRNA Tmevpg1 can play a role in the pathogenesis of SS.
CONCLUSION
We have reviewed lncRNAs associated with immune cell functions and the pathogenesis of autoimmune diseases. Accumulating evidence suggests the possibility that lncRNAs may be strong candidates for immune regulators and could also be prime suspects in the development of autoimmune diseases. However, only a few studies have been conducted in autoimmune diseases so far. Therefore, further studies on lncRNAs in autoimmune diseases will be essential to answer questions about their role in the pathogenesis of autoimmune diseases. Moreover, future studies may provide novel molecular targets for accurate diagnosis and treatment of autoimmune diseases.
ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. 2016R1C1B1016617).
Abbreviations
- ANRIL
antisense non-coding RNA in the INK4 locus
- AS
antisense
- c-CBL
casitas B-lineage lymphoma
- Cox2
cyclooxygenase 2
- DCs
dendritic cells
- DM
dermatomyositis
- DNA PKcs
DNA-dependent protein kinase catalytic subunit
- EGFR
epidermal growth factor receptor
- ESR
erythrocyte sedimentation rates
- EZH2
enhancer of zeste homolog 2
- FAS-AS1
Fas-antisense 1
- FLS
fibroblast-like synoviocytes
- GAPLINC
gastric adenocarcinoma predictive long intergenic noncoding RNA
- Gas5
growth arrest-specific transcript 5
- HCC
hepatocellular carcinoma
- hnRNP
heterogeneous nuclear ribonucleoprotein
- HOTAIR
HOX transcript antisense RNA
- ICAM-1
intercellular adhesion molecule 1
- KCNQ1OT1
KCNQ1 opposite strand/antisense transcript 1
- LCR
locus control region
- lincRNA
intergenic long noncoding RNA
- lincRNA-EPS
lincRNA erythroid prosurvival
- lncRNAs
long noncoding RNAs
- miRNAs
microRNAs
- MMP
matrix metalloproteinase
- Morrbid
myeloid RNA regulator of Bim-induced death
- MTX
methotrexate
- ncRNA
non-protein coding RNA
- NEAT1
nuclear enriched abundant transcript 1
- NeST
nettoie Salmonella pas Theiler's
- NFAT
nuclear factor of activated T cells
- NRON
noncoding repressor of nuclear factor of activated T cells
- nt
nucleotides
- PRC2
polycomb repressive complex 2
- RA
rheumatoid arthritis
- PACER
p50-associated COX-2 extragenic RNA
- RBM5
RNA-binding motif protein 5
- PM
polymyositis
- SLE
systemic lupus erythematosus
- SLEDAI
systemic lupus erythematosus disease activity index
- SS
Sjögren's syndrome
- SRP
signal recognition particle
- THRIL
tumor necrosis factor-α and heterogenous nuclear ribonucleoprotein L related immunoregulatory lincRNA
- Tmevpg1
Theiler's murine encephalomyelitis virus persistence candidate gene 1
- mcircRasGEF1B
mouse circRasGEF1B
- WDR5
WD40 repeat protein 5
Footnotes
Conflicts of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Hur K, Kim JM.
- Data curation: Hur K, Kim SH, Kim JM.
- Formal analysis: Hur K, Kim JM.
- Funding acquisition: Kim JM.
- Investigation: Hur K, Kim SH, Kim JM.
- Methodology: Hur K, Kim JM.
- Project administration: Hur K, Kim JM.
- Supervision: Kim JM.
- Validation: Hur K, Kim JM.
- Writing - original draft: Hur K, Kim JM.
- Writing - review & editing: Hur K, Kim SH, Kim JM.
References
- 1.ENCODE Project Consortium. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57–74. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ENCODE Project Consortium. Birney E, Stamatoyannopoulos JA, Dutta A, Guigó R, Gingeras TR, Margulies EH, Weng Z, Snyder M, Dermitzakis ET, et al. Identification and analysis of functional elements in 1% of the human genome by the ENCODE pilot project. Nature. 2007;447:799–816. doi: 10.1038/nature05874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ponting CP, Oliver PL, Reik W. Evolution and functions of long noncoding RNAs. Cell. 2009;136:629–641. doi: 10.1016/j.cell.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Singh RP, Massachi I, Manickavel S, Singh S, Rao NP, Hasan S, Mc Curdy DK, Sharma S, Wong D, Hahn BH, et al. The role of miRNA in inflammation and autoimmunity. Autoimmun Rev. 2013;12:1160–1165. doi: 10.1016/j.autrev.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez SA, Piera-Velazquez S. Potential role of human-specific genes, human-specific microRNAs and human-specific non-coding regulatory RNAs in the pathogenesis of systemic sclerosis and Sjögren's syndrome. Autoimmun Rev. 2013;12:1046–1051. doi: 10.1016/j.autrev.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmitz SU, Grote P, Herrmann BG. Mechanisms of long noncoding RNA function in development and disease. Cell Mol Life Sci. 2016;73:2491–2509. doi: 10.1007/s00018-016-2174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kretz M, Webster DE, Flockhart RJ, Lee CS, Zehnder A, Lopez-Pajares V, Qu K, Zheng GX, Chow J, Kim GE, et al. Suppression of progenitor differentiation requires the long noncoding RNA ANCR. Genes Dev. 2012;26:338–343. doi: 10.1101/gad.182121.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kretz M, Siprashvili Z, Chu C, Webster DE, Zehnder A, Qu K, Lee CS, Flockhart RJ, Groff AF, Chow J, et al. Control of somatic tissue differentiation by the long non-coding RNA TINCR. Nature. 2013;493:231–235. doi: 10.1038/nature11661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feldstein O, Nizri T, Doniger T, Jacob J, Rechavi G, Ginsberg D. The long non-coding RNA ERIC is regulated by E2F and modulates the cellular response to DNA damage. Mol Cancer. 2013;12:131. doi: 10.1186/1476-4598-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lekka E, Hall J. Noncoding RNAs in disease. FEBS Lett. 2018;592:2884–2900. doi: 10.1002/1873-3468.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Cao X. Long noncoding RNAs in innate immunity. Cell Mol Immunol. 2016;13:138–147. doi: 10.1038/cmi.2015.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzgerald KA, Caffrey DR. Long noncoding RNAs in innate and adaptive immunity. Curr Opin Immunol. 2014;26:140–146. doi: 10.1016/j.coi.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang P, Xue Y, Han Y, Lin L, Wu C, Xu S, Jiang Z, Xu J, Liu Q, Cao X. The STAT3-binding long noncoding RNA lnc-DC controls human dendritic cell differentiation. Science. 2014;344:310–313. doi: 10.1126/science.1251456. [DOI] [PubMed] [Google Scholar]
- 14.Spurlock CF, 3rd, Tossberg JT, Guo Y, Collier SP, Crooke PS, 3rd, Aune TM. Expression and functions of long noncoding RNAs during human T helper cell differentiation. Nat Commun. 2015;6:6932. doi: 10.1038/ncomms7932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carpenter S, Aiello D, Atianand MK, Ricci EP, Gandhi P, Hall LL, Byron M, Monks B, Henry-Bezy M, Lawrence JB, et al. A long noncoding RNA mediates both activation and repression of immune response genes. Science. 2013;341:789–792. doi: 10.1126/science.1240925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lander ES, Linton LM, Birren B, Nusbaum C, Zody MC, Baldwin J, Devon K, Dewar K, Doyle M, FitzHugh W, et al. Initial sequencing and analysis of the human genome. Nature. 2001;409:860–921. doi: 10.1038/35057062. [DOI] [PubMed] [Google Scholar]
- 17.Guttman M, Garber M, Levin JZ, Donaghey J, Robinson J, Adiconis X, Fan L, Koziol MJ, Gnirke A, Nusbaum C, et al. Ab initio reconstruction of cell type-specific transcriptomes in mouse reveals the conserved multi-exonic structure of lincRNAs. Nat Biotechnol. 2010;28:503–510. doi: 10.1038/nbt.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kampa D, Cheng J, Kapranov P, Yamanaka M, Brubaker S, Cawley S, Drenkow J, Piccolboni A, Bekiranov S, Helt G, et al. Novel RNAs identified from an in-depth analysis of the transcriptome of human chromosomes 21 and 22. Genome Res. 2004;14:331–342. doi: 10.1101/gr.2094104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carninci P, Kasukawa T, Katayama S, Gough J, Frith MC, Maeda N, Oyama R, Ravasi T, Lenhard B, Wells C, et al. The transcriptional landscape of the mammalian genome. Science. 2005;309:1559–1563. doi: 10.1126/science.1112014. [DOI] [PubMed] [Google Scholar]
- 20.Liu B, Sun L, Liu Q, Gong C, Yao Y, Lv X, Lin L, Yao H, Su F, Li D, et al. A cytoplasmic NF-κB interacting long noncoding RNA blocks IκB phosphorylation and suppresses breast cancer metastasis. Cancer Cell. 2015;27:370–381. doi: 10.1016/j.ccell.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Zhao J, Sun BK, Erwin JA, Song JJ, Lee JT. Polycomb proteins targeted by a short repeat RNA to the mouse X chromosome. Science. 2008;322:750–756. doi: 10.1126/science.1163045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El Bassit G, Patel RS, Carter G, Shibu V, Patel AA, Song S, Murr M, Cooper DR, Bickford PC, Patel NA. MALAT1 in human adipose stem cells modulates survival and alternative splicing of PKCδII in HT22 cells. Endocrinology. 2017;158:183–195. doi: 10.1210/en.2016-1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He Y, Meng XM, Huang C, Wu BM, Zhang L, Lv XW, Li J. Long noncoding RNAs: novel insights into hepatocelluar carcinoma. Cancer Lett. 2014;344:20–27. doi: 10.1016/j.canlet.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 24.Ferreri AJ, Illerhaus G, Zucca E, Cavalli F, International Extranodal Lymphoma Study Group Flows and flaws in primary central nervous system lymphoma. Nat Rev Clin Oncol. 2010;7:472. doi: 10.1038/nrclinonc.2010.9-c1. [DOI] [PubMed] [Google Scholar]
- 25.Somarowthu S, Legiewicz M, Chillón I, Marcia M, Liu F, Pyle AM. HOTAIR forms an intricate and modular secondary structure. Mol Cell. 2015;58:353–361. doi: 10.1016/j.molcel.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelley RL, Kuroda MI. Noncoding RNA genes in dosage compensation and imprinting. Cell. 2000;103:9–12. doi: 10.1016/s0092-8674(00)00099-4. [DOI] [PubMed] [Google Scholar]
- 27.Zimmerman LM, Vogel LA, Bowden RM. Understanding the vertebrate immune system: insights from the reptilian perspective. J Exp Biol. 2010;213:661–671. doi: 10.1242/jeb.038315. [DOI] [PubMed] [Google Scholar]
- 28.Iwasaki A, Medzhitov R. Control of adaptive immunity by the innate immune system. Nat Immunol. 2015;16:343–353. doi: 10.1038/ni.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riera Romo M, Pérez-Martínez D, Castillo Ferrer C. Innate immunity in vertebrates: an overview. Immunology. 2016;148:125–139. doi: 10.1111/imm.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kotzin JJ, Spencer SP, McCright SJ, Kumar DB, Collet MA, Mowel WK, Elliott EN, Uyar A, Makiya MA, Dunagin MC, et al. The long non-coding RNA Morrbid regulates Bim and short-lived myeloid cell lifespan. Nature. 2016;537:239–243. doi: 10.1038/nature19346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manz MG, Boettcher S. Emergency granulopoiesis. Nat Rev Immunol. 2014;14:302–314. doi: 10.1038/nri3660. [DOI] [PubMed] [Google Scholar]
- 32.Ginhoux F, Jung S. Monocytes and macrophages: developmental pathways and tissue homeostasis. Nat Rev Immunol. 2014;14:392–404. doi: 10.1038/nri3671. [DOI] [PubMed] [Google Scholar]
- 33.Simon HU, Rothenberg ME, Bochner BS, Weller PF, Wardlaw AJ, Wechsler ME, Rosenwasser LJ, Roufosse F, Gleich GJ, Klion AD. Refining the definition of hypereosinophilic syndrome. J Allergy Clin Immunol. 2010;126:45–49. doi: 10.1016/j.jaci.2010.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Steinman RM, Hemmi H. Dendritic cells: translating innate to adaptive immunity. Curr Top Microbiol Immunol. 2006;311:17–58. doi: 10.1007/3-540-32636-7_2. [DOI] [PubMed] [Google Scholar]
- 35.Laouar Y, Welte T, Fu XY, Flavell RA. STAT3 is required for Flt3L-dependent dendritic cell differentiation. Immunity. 2003;19:903–912. doi: 10.1016/s1074-7613(03)00332-7. [DOI] [PubMed] [Google Scholar]
- 36.Guttman M, Amit I, Garber M, French C, Lin MF, Feldser D, Huarte M, Zuk O, Carey BW, Cassady JP, et al. Chromatin signature reveals over a thousand highly conserved large non-coding RNAs in mammals. Nature. 2009;458:223–227. doi: 10.1038/nature07672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Z, Chao TC, Chang KY, Lin N, Patil VS, Shimizu C, Head SR, Burns JC, Rana TM. The long noncoding RNA THRIL regulates TNFα expression through its interaction with hnRNPL. Proc Natl Acad Sci U S A. 2014;111:1002–1007. doi: 10.1073/pnas.1313768111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ng WL, Marinov GK, Liau ES, Lam YL, Lim YY, Ea CK. Inducible RasGEF1B circular RNA is a positive regulator of ICAM-1 in the TLR4/LPS pathway. RNA Biol. 2016;13:861–871. doi: 10.1080/15476286.2016.1207036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krawczyk M, Emerson BM. p50-associated COX-2 extragenic RNA (PACER) activates COX-2 gene expression by occluding repressive NF-κB complexes. eLife. 2014;3:e01776. doi: 10.7554/eLife.01776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Atianand MK, Hu W, Satpathy AT, Shen Y, Ricci EP, Alvarez-Dominguez JR, Bhatta A, Schattgen SA, McGowan JD, Blin J, et al. A long noncoding RNA lincRNA-EPS acts as a transcriptional brake to restrain inflammation. Cell. 2016;165:1672–1685. doi: 10.1016/j.cell.2016.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Castellanos-Rubio A, Fernandez-Jimenez N, Kratchmarov R, Luo X, Bhagat G, Green PH, Schneider R, Kiledjian M, Bilbao JR, Ghosh S. A long noncoding RNA associated with susceptibility to celiac disease. Science. 2016;352:91–95. doi: 10.1126/science.aad0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rapicavoli NA, Qu K, Zhang J, Mikhail M, Laberge RM, Chang HY. A mammalian pseudogene lncRNA at the interface of inflammation and anti-inflammatory therapeutics. eLife. 2013;2:e00762. doi: 10.7554/eLife.00762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ranzani V, Rossetti G, Panzeri I, Arrigoni A, Bonnal RJ, Curti S, Gruarin P, Provasi E, Sugliano E, Marconi M, et al. The long intergenic noncoding RNA landscape of human lymphocytes highlights the regulation of T cell differentiation by linc-MAF-4. Nat Immunol. 2015;16:318–325. doi: 10.1038/ni.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hu G, Tang Q, Sharma S, Yu F, Escobar TM, Muljo SA, Zhu J, Zhao K. Expression and regulation of intergenic long noncoding RNAs during T cell development and differentiation. Nat Immunol. 2013;14:1190–1198. doi: 10.1038/ni.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee GR, Fields PE, Griffin TJ, 4th, Flavell RA. Regulation of the Th2 cytokine locus by a locus control region. Immunity. 2003;19:145–153. doi: 10.1016/s1074-7613(03)00179-1. [DOI] [PubMed] [Google Scholar]
- 46.Vigneau S, Rohrlich PS, Brahic M, Bureau JF. Tmevpg1, a candidate gene for the control of Theiler's virus persistence, could be implicated in the regulation of gamma interferon. J Virol. 2003;77:5632–5638. doi: 10.1128/JVI.77.10.5632-5638.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collier SP, Collins PL, Williams CL, Boothby MR, Aune TM. Cutting edge: influence of Tmevpg1, a long intergenic noncoding RNA, on the expression of Ifng by Th1 cells. J Immunol. 2012;189:2084–2088. doi: 10.4049/jimmunol.1200774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collier SP, Henderson MA, Tossberg JT, Aune TM. Regulation of the Th1 genomic locus from Ifng through Tmevpg1 by T-bet. J Immunol. 2014;193:3959–3965. doi: 10.4049/jimmunol.1401099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gomez JA, Wapinski OL, Yang YW, Bureau JF, Gopinath S, Monack DM, Chang HY, Brahic M, Kirkegaard K. The NeST long ncRNA controls microbial susceptibility and epigenetic activation of the interferon-γ locus. Cell. 2013;152:743–754. doi: 10.1016/j.cell.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y, Zhong H, Xie X, Chen CY, Huang D, Shen L, Zhang H, Chen ZW, Zeng G. Long noncoding RNA derived from CD244 signaling epigenetically controls CD8+ T-cell immune responses in tuberculosis infection. Proc Natl Acad Sci U S A. 2015;112:E3883–E3892. doi: 10.1073/pnas.1501662112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Willingham AT, Orth AP, Batalov S, Peters EC, Wen BG, Aza-Blanc P, Hogenesch JB, Schultz PG. A strategy for probing the function of noncoding RNAs finds a repressor of NFAT. Science. 2005;309:1570–1573. doi: 10.1126/science.1115901. [DOI] [PubMed] [Google Scholar]
- 52.Sharma S, Findlay GM, Bandukwala HS, Oberdoerffer S, Baust B, Li Z, Schmidt V, Hogan PG, Sacks DB, Rao A. Dephosphorylation of the nuclear factor of activated T cells (NFAT) transcription factor is regulated by an RNA-protein scaffold complex. Proc Natl Acad Sci U S A. 2011;108:11381–11386. doi: 10.1073/pnas.1019711108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jiang R, Tang J, Chen Y, Deng L, Ji J, Xie Y, Wang K, Jia W, Chu WM, Sun B. The long noncoding RNA lnc-EGFR stimulates T-regulatory cells differentiation thus promoting hepatocellular carcinoma immune evasion. Nat Commun. 2017;8:15129. doi: 10.1038/ncomms15129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sehgal L, Mathur R, Braun FK, Wise JF, Berkova Z, Neelapu S, Kwak LW, Samaniego F. FAS-antisense 1 lncRNA and production of soluble versus membrane Fas in B-cell lymphoma. Leukemia. 2014;28:2376–2387. doi: 10.1038/leu.2014.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jacobson DL, Gange SJ, Rose NR, Graham NM. Epidemiology and estimated population burden of selected autoimmune diseases in the United States. Clin Immunol Immunopathol. 1997;84:223–243. doi: 10.1006/clin.1997.4412. [DOI] [PubMed] [Google Scholar]
- 56.Eaton WW, Rose NR, Kalaydjian A, Pedersen MG, Mortensen PB. Epidemiology of autoimmune diseases in Denmark. J Autoimmun. 2007;29:1–9. doi: 10.1016/j.jaut.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med. 2008;358:929–939. doi: 10.1056/NEJMra071297. [DOI] [PubMed] [Google Scholar]
- 58.Summers SA, Hoi A, Steinmetz OM, O'Sullivan KM, Ooi JD, Odobasic D, Akira S, Kitching AR, Holdsworth SR. TLR9 and TLR4 are required for the development of autoimmunity and lupus nephritis in pristane nephropathy. J Autoimmun. 2010;35:291–298. doi: 10.1016/j.jaut.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 59.Lartigue A, Colliou N, Calbo S, François A, Jacquot S, Arnoult C, Tron F, Gilbert D, Musette P. Critical role of TLR2 and TLR4 in autoantibody production and glomerulonephritis in lpr mutation-induced mouse lupus. J Immunol. 2009;183:6207–6216. doi: 10.4049/jimmunol.0803219. [DOI] [PubMed] [Google Scholar]
- 60.Nockher WA, Wigand R, Schoeppe W, Scherberich JE. Elevated levels of soluble CD14 in serum of patients with systemic lupus erythematosus. Clin Exp Immunol. 1994;96:15–19. doi: 10.1111/j.1365-2249.1994.tb06222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang F, Wu L, Qian J, Qu B, Xia S, La T, Wu Y, Ma J, Zeng J, Guo Q, et al. Identification of the long noncoding RNA NEAT1 as a novel inflammatory regulator acting through MAPK pathway in human lupus. J Autoimmun. 2016;75:96–104. doi: 10.1016/j.jaut.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 62.Suarez-Gestal M, Calaza M, Endreffy E, Pullmann R, Ordi-Ros J, Sebastiani GD, Ruzickova S, Jose Santos M, Papasteriades C, Marchini M, et al. Replication of recently identified systemic lupus erythematosus genetic associations: a case-control study. Arthritis Res Ther. 2009;11:R69. doi: 10.1186/ar2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kino T, Hurt DE, Ichijo T, Nader N, Chrousos GP. Noncoding RNA gas5 is a growth arrest- and starvation-associated repressor of the glucocorticoid receptor. Sci Signal. 2010;3:ra8. doi: 10.1126/scisignal.2000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Haywood ME, Rose SJ, Horswell S, Lees MJ, Fu G, Walport MJ, Morley BJ. Overlapping BXSB congenic intervals, in combination with microarray gene expression, reveal novel lupus candidate genes. Genes Immun. 2006;7:250–263. doi: 10.1038/sj.gene.6364294. [DOI] [PubMed] [Google Scholar]
- 65.Wu GC, Li J, Leng RX, Li XP, Li XM, Wang DG, Pan HF, Ye DQ. Identification of long non-coding RNAs Gas5, linc0597 and lnc-DC in plasma as novel biomarkers for systemic lupus erythematosus. Oncotarget. 2017;8:23650–23663. doi: 10.18632/oncotarget.15569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365:2205–2219. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 67.Picerno V, Ferro F, Adinolfi A, Valentini E, Tani C, Alunno A. One year in review: the pathogenesis of rheumatoid arthritis. Clin Exp Rheumatol. 2015;33:551–558. [PubMed] [Google Scholar]
- 68.Zamanpoor M. The genetic pathogenesis, diagnosis and therapeutic insight of rheumatoid arthritis. Clin Genet. 2018 doi: 10.1111/cge.13498. [DOI] [PubMed] [Google Scholar]
- 69.Deng J, Yang M, Jiang R, An N, Wang X, Liu B. Long non-coding RNA HOTAIR regulates the proliferation, self-renewal capacity, tumor formation and migration of the cancer stem-like cell (CSC) subpopulation enriched from breast cancer cells. PLoS One. 2017;12:e0170860. doi: 10.1371/journal.pone.0170860. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 70.Di W, Li Q, Shen W, Guo H, Zhao S. The long non-coding RNA HOTAIR promotes thyroid cancer cell growth, invasion and migration through the miR-1-CCND2 axis. Am J Cancer Res. 2017;7:1298–1309. [PMC free article] [PubMed] [Google Scholar]
- 71.Song J, Kim D, Han J, Kim Y, Lee M, Jin EJ. PBMC and exosome-derived HOTAIR is a critical regulator and potent marker for rheumatoid arthritis. Clin Exp Med. 2015;15:121–126. doi: 10.1007/s10238-013-0271-4. [DOI] [PubMed] [Google Scholar]
- 72.Stuhlmüller B, Kunisch E, Franz J, Martinez-Gamboa L, Hernandez MM, Pruss A, Ulbrich N, Erdmann VA, Burmester GR, Kinne RW. Detection of oncofetal h19 RNA in rheumatoid arthritis synovial tissue. Am J Pathol. 2003;163:901–911. doi: 10.1016/S0002-9440(10)63450-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spurlock CF, 3rd, Tossberg JT, Matlock BK, Olsen NJ, Aune TM. Methotrexate inhibits NF-κB activity via long intergenic (noncoding) RNA-p21 induction. Arthritis Rheumatol. 2014;66:2947–2957. doi: 10.1002/art.38805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lu MC, Yu HC, Yu CL, Huang HB, Koo M, Tung CH, Lai NS. Increased expression of long noncoding RNAs LOC100652951 and LOC100506036 in T cells from patients with rheumatoid arthritis facilitates the inflammatory responses. Immunol Res. 2016;64:576–583. doi: 10.1007/s12026-015-8756-8. [DOI] [PubMed] [Google Scholar]
- 75.Mo BY, Guo XH, Yang MR, Liu F, Bi X, Liu Y, Fang LK, Luo XQ, Wang J, Bellanti JA, et al. Long non-coding RNA GAPLINC promotes tumor-like biologic behaviors of fibroblast-like synoviocytes as microRNA sponging in rheumatoid arthritis patients. Front Immunol. 2018;9:702. doi: 10.3389/fimmu.2018.00702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Findlay AR, Goyal NA, Mozaffar T. An overview of polymyositis and dermatomyositis. Muscle Nerve. 2015;51:638–656. doi: 10.1002/mus.24566. [DOI] [PubMed] [Google Scholar]
- 77.Lega JC, Fabien N, Reynaud Q, Durieu I, Durupt S, Dutertre M, Cordier JF, Cottin V. The clinical phenotype associated with myositis-specific and associated autoantibodies: a meta-analysis revisiting the so-called antisynthetase syndrome. Autoimmun Rev. 2014;13:883–891. doi: 10.1016/j.autrev.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 78.Dau PC. Plasma exchange in polymyositis and dermatomyositis. N Engl J Med. 1992;327:1030–1031. doi: 10.1056/NEJM199210013271413. [DOI] [PubMed] [Google Scholar]
- 79.Satoh T, Okano T, Matsui T, Watabe H, Ogasawara T, Kubo K, Kuwana M, Fertig N, Oddis CV, Kondo H, et al. Novel autoantibodies against 7SL RNA in patients with polymyositis/dermatomyositis. J Rheumatol. 2005;32:1727–1733. [PubMed] [Google Scholar]
- 80.Cojocaru M, Cojocaru IM, Chicos B. New insights into antisynthetase syndrome. Maedica (Buchar) 2016;11:130–135. [PMC free article] [PubMed] [Google Scholar]
- 81.Peng QL, Zhang YM, Yang HB, Shu XM, Lu X, Wang GC. Transcriptomic profiling of long non-coding RNAs in dermatomyositis by microarray analysis. Sci Rep. 2016;6:32818. doi: 10.1038/srep32818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mavragani CP, Moutsopoulos HM. Sjögren's syndrome. Annu Rev Pathol. 2014;9:273–285. doi: 10.1146/annurev-pathol-012513-104728. [DOI] [PubMed] [Google Scholar]
- 83.Both T, Dalm VA, van Hagen PM, van Daele PL. Reviewing primary Sjögren's syndrome: beyond the dryness - from pathophysiology to diagnosis and treatment. Int J Med Sci. 2017;14:191–200. doi: 10.7150/ijms.17718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martín-Nares E, Hernández-Molina G. Novel autoantibodies in Sjögren's syndrome: a comprehensive review. Autoimmun Rev. 2019;18:192–198. doi: 10.1016/j.autrev.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 85.Tzioufas AG, Kapsogeorgou EK, Moutsopoulos HM. Pathogenesis of Sjögren's syndrome: what we know and what we should learn. J Autoimmun. 2012;39:4–8. doi: 10.1016/j.jaut.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 86.Wang J, Peng H, Tian J, Ma J, Tang X, Rui K, Tian X, Wang Y, Chen J, Lu L, et al. Upregulation of long noncoding RNA TMEVPG1 enhances T helper type 1 cell response in patients with Sjögren syndrome. Immunol Res. 2016;64:489–496. doi: 10.1007/s12026-015-8715-4. [DOI] [PubMed] [Google Scholar]
- 87.Zhang Y, Xu YZ, Sun N, Liu JH, Chen FF, Guan XL, Li A, Wang F, Zhao QF, Wang HY, et al. Long noncoding RNA expression profile in fibroblast-like synoviocytes from patients with rheumatoid arthritis. Arthritis Res Ther. 2016;18:227. doi: 10.1186/s13075-016-1129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]