Abstract
The enhanced differentiation and activation of osteoclasts (OCs) in the inflammatory arthritis such as rheumatoid arthritis (RA) and gout causes not only local bone erosion, but also systemic osteoporosis, leading to functional disabilities and morbidity. The induction and amplification of NFATc1, a master regulator of OC differentiation, is mainly regulated by receptor activator of NF-κB (RANK) ligand-RANK and calcium signaling which are amplified in the inflammatory milieu, as well as by inflammatory cytokines such as TNFα, IL-1β and IL-6. Moreover, the predominance of CD4+ T cell subsets, which varies depending on the condition of inflammatory diseases, can determine the fate of OC differentiation. Anti-citrullinated peptide antibodies which are critical in the pathogenesis of RA can bind to the citrullinated vimentin on the surface of OC precursors, and in turn promote OC differentiation and function via IL-8. In addition to adaptive immunity, the activation of innate immune system including the nucleotide oligomerization domain leucine rich repeat with a pyrin domain 3 inflammasome and TLRs can regulate OC maturation. The emerging perspectives about the diverse and close interactions between the immune cells and OCs in inflammatory milieu can have a significant impact on the future direction of drug development.
Keywords: Osteoclasts; Arthritis, rheumatoid; Osteolysis; Osteoimmunology
INTRODUCTION
Bone erosion and joint destruction is a characteristic finding of some inflammatory arthritis including rheumatoid arthritis (RA), psoriatic arthritis, and gout, and is associated with functional disability and increased mortality (1,2). The activation of osteoclasts (OCs), which is differentiated from myeloid OC precursors of the monocyte-macrophage lineage, is responsible for bone erosion in inflammatory arthritis (3). The origin of OCs in RA which is mainly located at the junction of synovial pannus and bone is not clear until now. Immature dendritic cells being rich in inflamed synovium can directly transdifferentiated into OCs in the inflammatory condition of RA (4). The presence of tartrate-resistant acid phosphatase-positive OCs on both synovial and marrow sides of subchondral bone suggests that subchondral bone marrow also can be the origin of OCs in RA (5). The treatment goal for bone-erosive inflammatory arthritis is to minimize the structural joint damage as well as suppress inflammation itself (6). To achieve this goal, the mechanisms for differentiation and activation of OCs under inflammatory milieu have been actively investigated and its therapeutic application to inhibit the functions of OCs has been in the limelight. In this review, we will address the scientific achievements about the molecular mechanisms involving OC differentiation under an inflammatory condition, especially in RA.
ENHANCED EXPRESSION OF RANK LIGAND (RANKL) AND OSTEOCLAST-ASSOCIATED RECEPTOR (OSCAR) IN INFLAMMATORY ARTHRITIS
Interaction between the RANK and RANKL is critical for triggering OC precursors to differentiate into OCs (7). RANKL binds to RANK on the surface of OC precursors results in the recruitment of the adaptor molecule, TNF receptor-associated factor 6 (TRAF6), which activates NF-κB, AP-1 (c-Fos and c-Jun), MAP kinases, and phospholipase Cγ (7) (Fig. 1A). RANKL is mainly released by osteoblast and osteocyte during the process of physiologic bone remodeling (8,9). However, this role can be replaced by immune cells and fibroblast-like synoviocytes (FLS) in RA condition (10,11,12,13). Synovial B cells from RA patients are enriched with switched memory B cells (CD27+IgD−) and spontaneously express RANKL which is much higher than that of synovial T cells (10). Actually, B cell depletion therapy with rituximab significantly abrogates the joint erosion, which is associated with a decrease of synovial OC precursors and RANKL expression (14,15). In terms of T cells, Th17 cells express a significant amount of RANKL, but Th1 and Th2 cells express only a minimal amount (11,12). FLS can also be the major source of RANKL which is induced by inflammatory cytokines such as TNFα, IL-17, and IL-6 in RA (13). Recent study using conditional deletion of RANKL in T cells or FLS revealed that RANKL of FLS has a primary role compared to RANKL of T cells in bone erosion of inflammatory arthritis (16).
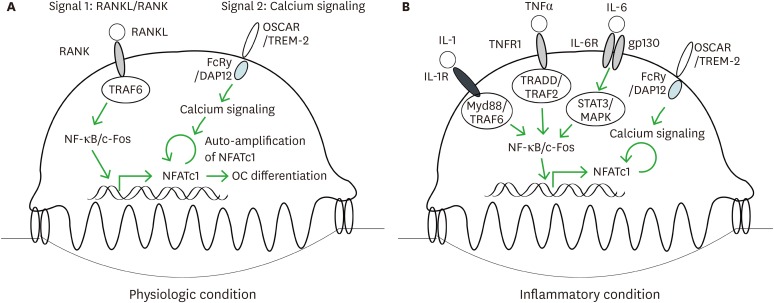
Figure 1. Inflammatory cytokines such as TNFα, IL-1β, and IL-6 can replace the function of RANKL/RANK signaling during OC differentiation. (A) Schematic signaling pathways being critical for OC differentiation in physiologic condition. RANKL/RANK signaling activates NF-κB and c-Fos through TRAF6, leading to the transcription of NFATc1. Calcium signaling through ITAM motif of FcRγ or DAP12 increases nuclear translocation of NFATc1 through its dephosphorylation, and NFATc1 in turn promotes its own transcription within the nucleus, forming auto-amplification loop. (B) TNFα together with IL-1β or IL-6 can substitute for RANKL/RANK signaling through the activation of NFkB, c-Fos and NFATc1 which are essential transcription factors for OC differentiation.
Together with RANKL-RANK signaling, the immunoglobulin-like receptor, OSCAR and triggering receptor expressed on myeloid cells (TREM)-2 that is associated with the immunoreceptor tyrosine-based activation motif (ITAM)-containing FcRγ and DAP12, respectively, leads to the activation of calcium signaling, which induces the auto-amplification of the NFATc1, master transcription factor for osteoclast differentiation (17,18) (Fig. 1A). Compared to controls, peripheral blood monocytes from RA patients express a higher level of OSCAR which is mainly induced by TNFα and associated with disease activity of RA (19). Actually, synovial tissues from active RA patients express higher levels of OSCAR than OA and control. OSCAR is mainly expressed by OCs at the erosion and by mononuclear cells around synovial microvessels (19,20). Ligands for OSCAR is mainly type I (ColI) and type II collagen (ColII) which are the most abundant collagen of bone and cartilage, respectively (21). Among collagens, ColII peptides efficiently stimulate RANKL-dependent OC differentiation (21). In addition to OCs, ITAM signaling from OSCAR-ColI/II interaction promotes survival and cytokine production of monocytes (22), and dendritic cells (23). TREM-2 is also highly expressed in the synovial tissue of RA, but it is not well elucidated the pathologic role in OC differentiation of RA (20).
INFLAMMATORY CYTOKINES AND OC DIFFERENTIATION: INTERACTION BETWEEN TNFα, IL-6, AND IL-1
RA is a prototype of chronic autoimmune arthritis with an increase of inflammatory cytokines including TNFα, IL-6, and IL-1 which can also affect the OC differentiation (24). TNFα can dramatically enhance OC differentiation in the presence of low level of RANKL that is insufficient to induce OC formation, while TNFα alone without RANKL failed to induce the differentiation of OCs (25). However, TNFα can induce OC differentiation in the recombination signal binding protein for immunoglobulin kappa J region (RBP-J)-deficient cells even in the absence of RANKL, suggesting RBP-J, a key mediator of signaling by the canonical Notch pathway, acts as upstream negative regulator of TNFα-mediated OC differentiation (26). In addition, the higher dose of TNFα (20 ng/ml) can induce OC differentiation without RANKL, but it fails for OCs to have a resorbing capacity of dentin slice (27).
Considering RANKL is a member of TNF superfamily, it is not surprising the induction or enhancement of OC differentiation by TNFα sharing signaling pathways with RANKL (28,29). However, TNFα alone cannot produce complete OCs with resorption function (27). These limits of TNFα in OC differentiation are overcome by the presence of other inflammatory cytokines such as IL-1 and IL-6 (27,30). IL-1 and IL-6 can promote OC differentiation in the presence of RANKL in vitro, but they cannot differentiate OC on its own without RANKL (31,32). However, IL-1 together with TNFα can differentiate mouse bone marrow macrophages (BMMs) into functional OCs (27). IL-6 in the presence of TNFα also generates functional OCs in vitro which is independent to RANK/RANKL signaling (30). This TNFα and IL-6-mediated OC differentiation does not occur in the BMMs from NFATc1 or DAP12-defective mice (30), meaning that the differentiation into OC is possible regardless of ligand and receptor specificity when NFATc1 is induced by NF-κB and AP-1 (Jun/Fos complex) signaling, and is auto-amplified by the calcium signaling (Fig. 1B).
T-CELL-MEDIATED REGULATION OF OC DIFFERENTIATION
Bone erosion of the involved joints is a characteristic finding in RA, but it rarely occur in the arthritis of systemic lupus erythematosus (SLE), even in the 5%–15% of patients with long-standing lupus arthritis who develop deformities by a subluxation of ligaments, known as Jaccoud's arthropathy (33). The synovial inflammation of RA is mainly driven by M1 macrophages and Th17 cells, and the main pathogenic mechanism of SLE is humoral immunity characterized by autoantibodies against nuclear and cytoplasmic antigens (34,35). This suggests that even if there is synovitis in both RA and SLE, the development of bone erosions depends on the context of inflammatory milieu determined by T cell subsets and their cytokines.
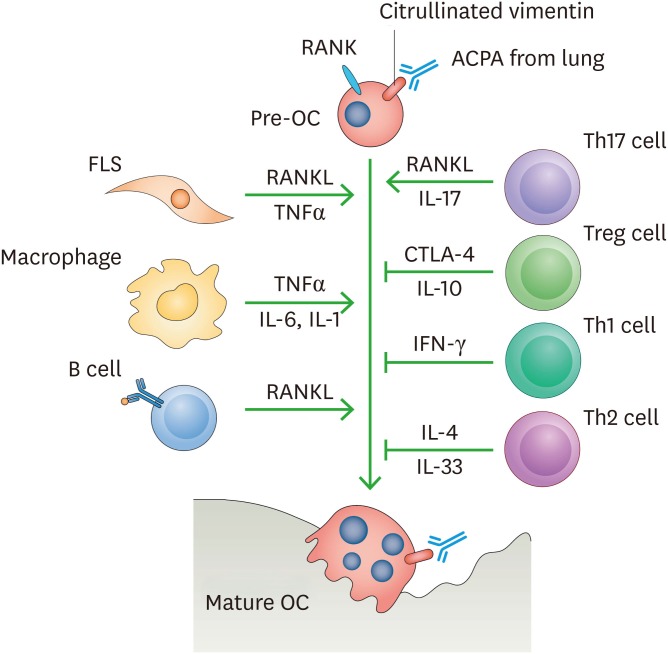
INFγ, the main Th1 cytokine, strongly suppresses OC differentiation in vitro through the proteosomal degradation of TRAF6 (36). It also downregulates RANKL-mediated cathepsin K expression in OC precursors which is critical for both differentiation and function of OCs (37). IL-4 as a Th2 cytokine is known to suppress OC differentiation through PPARγ and STAT6 activation (38,39). On the other hand, the co-culture with Th17 cells enhances OC differentiation through not only the action of IL-17, but also RANKL expression (11). Th17 cytokines including IL-17, IL-21, and IL-22 is mainly responsible for the bone erosion in RA through direct induction of OC differentiation as well as RANKL production from FLS and osteoblast (11,40,41). The blocking antibody against IL-17A inhibits OC differentiation in vivo, which is associated with the induction of IL-12 and IL-4, and the increase of Th2 and Tregs (42). Another T cell subset, Tregs, suppresses OC formation. Co-culture of Tregs suppresses OC differentiation from OC precursors as well as their bone resorbing function in vitro (43). The transgenic mice of Foxp3 that is the master regulator of Tregs revealed an osteopetrotic phenotype by the suppression of OC (44). Treg-mediated inhibition of OC differentiation is largely dependent on direct cell-cell contact via the CTLA-4, whereas TGFβ and IL-10, the major cytokines of Tregs, did not have an essential role (43). Abatacept that is a fusion protein with the extracellular domain of CTLA-4 inhibited OC formation in a dose-dependent manner in vitro, and successfully attenuated the bone erosion in the arthritis of TNF transgenic mice (45). Taken together, these evidences suggest that the distribution of T cell subsets that is different according to inflammatory diseases can influence the cytokine milieu, and the net effects of T cell subsets and their cytokines can determine the differentiation of OC and consequently the erosive phenotype of the individual inflammatory diseases (Fig. 2).
Figure 2. Osteoclastogenesis is carefully orchestrated by various cytokines and immune cells in RA environment. FLS produces RANKL and TNFα which is induced by inflammation milieu, and macrophages are the main source of inflammatory cytokines such as TNFα, IL-1β, and IL-6 which can induce OC differentiation. B cells mainly express RANKL in RA synovium. In terms of T cell subset, Th17 cells increase OC differentiation through RANKL and IL-17 production, while Treg, Th1, and Th2 cells suppress it.
OC DIFFERENTIATION BY ANTI-CITRULLINATED PEPTIDE ANTIBODY (ACPA)
Citrullination is the post-translational modification of the amino acid arginine with positive charge at a neutral pH into the citrulline with neutral charge by peptidylarginine deiminase (PAD) enzyme in a calcium-dependent manner (46,47). The citrullinated target proteins such as filaggrin and vimentin lose their positive charge that was maintained by arginine, and consequently induce conformational changes of proteins (47). Arginine is essentially incapable of anchoring within the first binding pocket of all HLA-DR proteins because of its charge and relatively large size (48). Whereas the citrullinated peptides can have preferential but weak binding to HLA-DR proteins and it can make the citrullinated self-antigen-specific T cells escape the thymic negative selection (49,50). These CD4+ T cells actively contribute to the production of ACPA which is highly specific for the RA (46,47). Mounting evidences suggest the mucosal site such as lung and gingiva can be responsible for the initial ACPA production which is associated with long-term exposure to cigarette smoking and chronic periodontitis by Porphyromonas gingivalis (51,52).
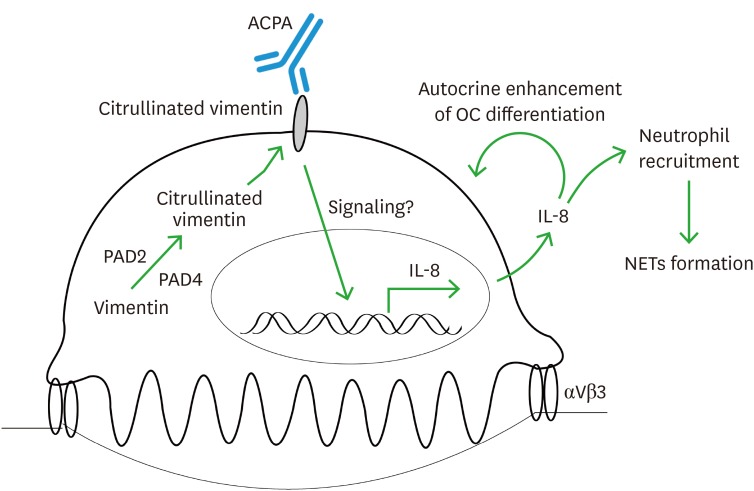
RA is chronic inflammatory disorder characterized by periarticular bone erosion that is associated with disease severity and poor functional outcome (53). Recent evidences found that ACPA is involved in the development of RA as well as bone erosion through OC differentiation (54,55). Even the subjects with ACPA who have no clinical symptom of RA, namely preclinical RA, showed a reduced bone mineral density which was mainly by cortical bone thinning and porosity, and a higher incidence of erosions in metacarpophalangeal joints compared to ACPA-negative controls (56). This result suggests that ACPA alone can trigger OC activation even in the absence of active inflammation. OCs and OC precursors express not only vimentin in their cytoplasm, but also PAD2 and PAD4 enzymes, which is unique for OCs and OC precursors, but not other cells in the joint tissue (55,57,58). Treatment of ACPA against mutated citrullinated vimentin (MCV) not only bound to osteoclast surfaces, but also led to robust induction of in vitro OC differentiation and bone-resorptive activity (54). This enhanced OC differentiation was reproduced in adoptive transfer model of MCV-ACPA in vivo, resulting in osteopenic phenotype (54). ACPA-mediated enhancement of OC differentiation was blocked by PAD enzyme inhibitor in a dose-dependent manner (55). Collectively, these evidences suggest that the vimentin is citrullinated by PAD enzyme in OCs and OC precursors, and this citrullinated vimentin expressed on the cell surface allows ACPA to bind to OC, which promotes OC differentiation and activation (Fig. 3).
Figure 3. ACPA with specificity to citrullinated vimentin induces the differentiation of OC precursors as well as promotes the inflammatory response in RA. The vimentin located in the cytoplasm of OC precursors and OCs is citrullinated by PDA enzymes in the presence of calcium and it is expressed on the cell surface. ACPA, which appears to have been generated in the inflammatory environment of lung or gingiva, binds to this citrullinated vimentin and it increases the expression of IL-8 from OC precursors and OCs. IL-8 increases the differentiation of OC precursors in an autocrine manner and is also involved in the recruitment of neutrophils as a chemokine. NETs formation by recruited neutrophils acts to amplify the inflammation of synovial tissue and thus to develop RA.
Although the precise signaling mechanisms are not well known, the binding of ACPA to the citrullinated vimentin on OC surface triggers the production of IL-8, also known as CXCL8 (55,58). ACPA-mediated OC differentiation is completely abolished by IL-8 neutralization or its chemical inhibitor, suggesting that IL-8 acts as an autocrine growth factor for OCs in the presence of ACPA (55). In addition, IL-8 as a potent chemokine can recruit neutrophils to the joint tissue. These activated neutrophils release neutrophil extracellular traps (NETs) consisted of processed chromatin bound to granular and selected cytoplasmic proteins (59). NETs can not only be a huge source of citrullinated antoantigen, but also stimulate inflammatory response through cytokine release, and activation of FLS and macrophage in RA (60).
Collectively, the osteoclast differentiation normally controlled by osteoblast- or osteocyte-secreted RANKL can be amplified under inflammatory condition of RA. The osteoclast-mediated bone destruction in RA is finely regulated not only by immune cells such as T cells, B cells and macrophages, and their cytokines, but also by FLS and RA-specific antibody of ACPA.
INNATE IMMUNE SYSTEM AND OC DIFFERENTIATION
Gout, along with RA, is another inflammatory arthritis characterized by bone erosion, which is caused by precipitation of monosodium urate (MSU) crystal in the joint (61). MSU crystal as a damage-associated molecular patterns (DAMPs) triggers innate immune response through pattern recognition receptors, such as nucleotide oligomerization domain (NOD)-like receptors and Toll-like receptors (TLRs), which implicates a role of innate immune system in OC differentiation (61,62).
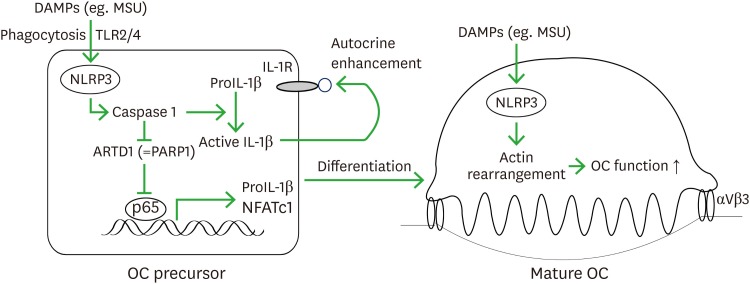
MSU crystals phagocytosed by macrophages are recognized by the NOD leucine rich repeat with a pyrin domain 3 (NLRP3) inflammasome involving the activation of procaspase-1, which in turn cleaves proIL-1β to active IL-1β (61). Actually, MSU-mediated enhancement of OC differentiation is significantly attenuated by the knockdown of IL-1β (63). NLRP3-induced activation of procaspase-1 can also trigger the cleavage of ADP-ribosyltransferase diphtheria toxin-like 1 (ARTD1), also known as poly(ADP-ribose) polymerase 1 (PARP1), into 89 kDa- and 24 kDa-sized fragments, leading to the loss of its enzyme function (64). This inhibition of ARTD1 results in the activation of canonical NF-κB signaling, which enhances the expression of IL-1β and NFATc1 in OC precursors (65). In addition, the OC-specific gain-of-function mutation of NLRP3 increases osteolysis in vivo resulting in 50% lower bone mass without systemic inflammation compared to control mice which is responsible for the enhanced reorganization of actin cytoskeleton (66). This result suggests a direct role of NLRP3 inflammasome in the function of mature OCs (Fig. 4).
Figure 4. DAMPs-NLRP3 inflammasome in OC differentiation and function. DAMPs such as MSU are endocytosed into OC precursors where TLRs may have a role. Upon exposure to DAMP, NLRP3 inflammasome is activated and in turn catalyses the conversion of procaspase-1 to caspase-1, which contributes to the production and secretion of the mature IL-1β. The activated caspase-1 also breaks down ARTD1, also known as PARP1, which leads to loss of its inhibitory role against canonical NF-κB signaling. The enhanced NF-κB activity can increase the transcription of IL-1β and NFATc1 that potentiate OC differentiation from OC precursors. In mature OC, NLPR3 inflammasome enhances bone resorbing ability through reorganization of actin cytoskeleton.
OC precursors also express TLRs, especially TLR2 and TLR4 (67). Although the ligands for TLR2 and TLR4 induces NF-κB activation and up-regulates TNFα expression in OC precursors, it strongly inhibits the OC differentiation in vitro (67). It is explained by the TLR-mediated suppression of RANK and TRME-2 expression through down-regulating cell surface c-Fms, the receptor for M-CSF, in OC precursors (68). However, OC precursors from TLR-2- and TLR-4-deficient mice have impaired capacity to uptake MSU crystals and differentiate to OC, implicating the indirect enhancement of OC differentiation by MSU crystal in the perspective of TLRs (69).
CONCLUDING REMARKS
Studies published over the past decade have found extensive evidences on the control of OC differentiation by immune cells and their cytokines (Fig. 2). Bone erosion and joint damage can proceed even though there is no evidence of active joint inflammation with effective medication for RA, so called uncoupling between clinical synovitis and damage progression (6,70). Recently, the antibody for RANKL, denosumab, has been known to be effective for reducing bone erosion, while it failed to show any difference in almost all parameters of disease activity compared with the placebo group (71). Moreover, there is an emerging interest in the enhancement of systemic bone loss in inflammatory diseases (72). Given the close interplay between the immune cells and OCs in inflammatory milieu, it is considered ideal the treatment strategy with agents that not only target the inflammation but also suppress OC differentiation, and this approach could potentially have significant impact on the future direction of drug development (Table 1).
Table 1. Critical mechanism-related implications and future directions for a new research agenda in bone erosion of inflammatory arthritis.
| Critical mechanisms | Implications discussed in this paper | Research agenda and future therapeutic targets |
|---|---|---|
| Enhanced expression of RANKL and OSCAR in inflammatory arthritis | RANKL is expressed in B cells, Th17 cells and FLS in RA synovium. | Inhibition of OSCAR and TREM-2 signaling in the progression of bone erosion. |
| Cytokine-stimulated monocytes express a higher level of OSCAR in RA. | Cathepsin K inhibitor in the prevention of bone erosion in RA. | |
| The pathologic role of TREM-2 in bone destruction in RA. | ||
| Other cellular source of RANKL in inflammatory arthritis such as Th22 cells etc. | ||
| Inflammatory cytokines and OC differentiation | The combination of inflammatory cytokines such as TNFα/IL-1β or TNFα/IL-6 can induce OC differentiation even if without RANKL. | Role of inflammatory cytokines in osteoblast activation which affects OC differentiation through RANKL expression. |
| Therapeutic effect of JAK inhibitors in bone erosion of RA (the comparison with TNFα/IL-6 inhibitors). | ||
| T-cell-mediated regulation of OC differentiation | Th17 cells induce OC differentiation through IL-17 and RANKL production. | Role of Th9, Th22 and Tr1 subsets in OC differentiation. |
| Th1/INFγ, Th2/IL-4, Treg/CTLA-4 suppress OC differentiation. | The molecular mechanism for non-destructive phenotype in lupus arthritis (why is the lupus arthritis resistant to bone erosion?). | |
| Bone production mechanism in spondyloarthropathy (over-activation of osteoblast by OC in the perspective of OC-OB coupling). | ||
| OC differentiation by ACPA | Not only does ACPA induce OC differentiation through IL-8 but it also involves the initiation and exacerbation of inflammation in RA. | Role of non-vimentin citrullinated proteins in OC differentiation and initiation of arthritis. |
| Mechanisms leading from systemic autoimmunity to joint-specific disease in RA. | ||
| Role of non-ACPA autoantibodies in OC activation and systemic osteoporosis in autoimmune disease such as lupus. | ||
| Innate immune system and OC differentiation | NLRP3 inflammasome system promotes OC differentiation via IL-1β activation and ARTD1 inactivation. | Role of other innate immunity-related receptors such as NOD-like receptor, mannose-binding lectin and mannose receptor in OC differentiation. |
| NLRP3 enhances reorganization of actin cytoskeleton leading to increase of osteolysis. | The connection of microbiota and OC differentiation in local and systemic inflammation. |
ACKNOWLEDGEMENTS
This research was supported by a grant to S.H. from the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant numbers NRF-2016R1D1A1B03932036).
Abbreviations
- ACPA
anti-citrullinated peptide antibody
- ARTD1
ADP-ribosyltransferase diphtheria toxin-like 1
- BMM
bone marrow macrophage
- DAMP
damage-associated molecular pattern
- FLS
fibroblast-like synoviocytes
- ITAM
immunoreceptor tyrosine-based activation motif
- MCV
mutated citrullinated vimentin
- MSU
monosodium urate
- NET
neutrophil extracellular trap
- NLRP3
NOD leucine rich repeat with a pyrin domain 3
- NOD
nucleotide oligomerization domain
- OC
osteoclast
- OSCAR
osteoclast-associated receptor
- PAD
peptidylarginine deiminase
- PARP1
poly(ADP-ribose) polymerase 1
- RA
rheumatoid arthritis
- RANKL
RANK ligand
- RBP-J
recombination signal binding protein for immunoglobulin kappa J region
- SLE
systemic lupus erythematosus
- TRAF6
TNF receptor-associated factor 6
- TREM
triggering receptor expressed on myeloid cells
Footnotes
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- Conceptualization: Jung YK, Kang YM, Han S.
- Data curation: Jung YK, Han S.
- Formal analysis: Jung YK, Han S.
- Funding acquisition: Han S.
- Investigation: Jung YK, Kang YM, Han S.
- Methodology: Jung YK, Han S.
- Project administration: Han S.
- Supervision: Kang YM.
- Validation: Jung YK, Kang YM, Han S.
- Writing - original draft: Jung YK, Han S.
- Writing - review & editing: Jung YK, Kang YM, Han S.
References
- 1.Schett G, Gravallese E. Bone erosion in rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev Rheumatol. 2012;8:656–664. doi: 10.1038/nrrheum.2012.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ødegård S, Landewé R, van der Heijde D, Kvien TK, Mowinckel P, Uhlig T. Association of early radiographic damage with impaired physical function in rheumatoid arthritis: a ten-year, longitudinal observational study in 238 patients. Arthritis Rheum. 2006;54:68–75. doi: 10.1002/art.21548. [DOI] [PubMed] [Google Scholar]
- 3.Udagawa N, Takahashi N, Akatsu T, Tanaka H, Sasaki T, Nishihara T, Koga T, Martin TJ, Suda T. Origin of osteoclasts: mature monocytes and macrophages are capable of differentiating into osteoclasts under a suitable microenvironment prepared by bone marrow-derived stromal cells. Proc Natl Acad Sci U S A. 1990;87:7260–7264. doi: 10.1073/pnas.87.18.7260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rivollier A, Mazzorana M, Tebib J, Piperno M, Aitsiselmi T, Rabourdin-Combe C, Jurdic P, Servet-Delprat C. Immature dendritic cell transdifferentiation into osteoclasts: a novel pathway sustained by the rheumatoid arthritis microenvironment. Blood. 2004;104:4029–4037. doi: 10.1182/blood-2004-01-0041. [DOI] [PubMed] [Google Scholar]
- 5.Bugatti S, Caporali R, Manzo A, Vitolo B, Pitzalis C, Montecucco C. Involvement of subchondral bone marrow in rheumatoid arthritis: lymphoid neogenesis and in situ relationship to subchondral bone marrow osteoclast recruitment. Arthritis Rheum. 2005;52:3448–3459. doi: 10.1002/art.21377. [DOI] [PubMed] [Google Scholar]
- 6.Molenaar ET, Voskuyl AE, Dinant HJ, Bezemer PD, Boers M, Dijkmans BA. Progression of radiologic damage in patients with rheumatoid arthritis in clinical remission. Arthritis Rheum. 2004;50:36–42. doi: 10.1002/art.11481. [DOI] [PubMed] [Google Scholar]
- 7.Jones DH, Kong YY, Penninger JM. Role of RANKL and RANK in bone loss and arthritis. Ann Rheum Dis. 2002;61(Suppl 2):ii32–ii39. doi: 10.1136/ard.61.suppl_2.ii32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, Bonewald LF, Kodama T, Wutz A, Wagner EF, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17:1231–1234. doi: 10.1038/nm.2452. [DOI] [PubMed] [Google Scholar]
- 9.Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O'Brien CA. Matrix-embedded cells control osteoclast formation. Nat Med. 2011;17:1235–1241. doi: 10.1038/nm.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meednu N, Zhang H, Owen T, Sun W, Wang V, Cistrone C, Rangel-Moreno J, Xing L, Anolik JH. Production of RANKL by memory B cells: a link between B cells and bone erosion in rheumatoid arthritis. Arthritis Rheumatol. 2016;68:805–816. doi: 10.1002/art.39489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sato K, Suematsu A, Okamoto K, Yamaguchi A, Morishita Y, Kadono Y, Tanaka S, Kodama T, Akira S, Iwakura Y, et al. Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J Exp Med. 2006;203:2673–2682. doi: 10.1084/jem.20061775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidson MG, Alonso MN, Yuan R, Axtell RC, Kenkel JA, Suhoski MM, González JC, Steinman L, Engleman EG. Th17 cells induce Th1-polarizing monocyte-derived dendritic cells. J Immunol. 2013;191:1175–1187. doi: 10.4049/jimmunol.1203201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hashizume M, Hayakawa N, Mihara M. IL-6 trans-signalling directly induces RANKL on fibroblast-like synovial cells and is involved in RANKL induction by TNF-α and IL-17. Rheumatology (Oxford) 2008;47:1635–1640. doi: 10.1093/rheumatology/ken363. [DOI] [PubMed] [Google Scholar]
- 14.Boumans MJ, Thurlings RM, Yeo L, Scheel-Toellner D, Vos K, Gerlag DM, Tak PP. Rituximab abrogates joint destruction in rheumatoid arthritis by inhibiting osteoclastogenesis. Ann Rheum Dis. 2012;71:108–113. doi: 10.1136/annrheumdis-2011-200198. [DOI] [PubMed] [Google Scholar]
- 15.Wheater G, Hogan VE, Teng YK, Tekstra J, Lafeber FP, Huizinga TW, Bijlsma JW, Francis RM, Tuck SP, Datta HK, et al. Suppression of bone turnover by B-cell depletion in patients with rheumatoid arthritis. Osteoporos Int. 2011;22:3067–3072. doi: 10.1007/s00198-011-1607-0. [DOI] [PubMed] [Google Scholar]
- 16.Danks L, Komatsu N, Guerrini MM, Sawa S, Armaka M, Kollias G, Nakashima T, Takayanagi H. RANKL expressed on synovial fibroblasts is primarily responsible for bone erosions during joint inflammation. Ann Rheum Dis. 2016;75:1187–1195. doi: 10.1136/annrheumdis-2014-207137. [DOI] [PubMed] [Google Scholar]
- 17.Takayanagi H. Osteoimmunology and the effects of the immune system on bone. Nat Rev Rheumatol. 2009;5:667–676. doi: 10.1038/nrrheum.2009.217. [DOI] [PubMed] [Google Scholar]
- 18.Koga T, Inui M, Inoue K, Kim S, Suematsu A, Kobayashi E, Iwata T, Ohnishi H, Matozaki T, Kodama T, et al. Costimulatory signals mediated by the ITAM motif cooperate with RANKL for bone homeostasis. Nature. 2004;428:758–763. doi: 10.1038/nature02444. [DOI] [PubMed] [Google Scholar]
- 19.Herman S, Müller RB, Krönke G, Zwerina J, Redlich K, Hueber AJ, Gelse H, Neumann E, Müller-Ladner U, Schett G. Induction of osteoclast-associated receptor, a key osteoclast costimulation molecule, in rheumatoid arthritis. Arthritis Rheum. 2008;58:3041–3050. doi: 10.1002/art.23943. [DOI] [PubMed] [Google Scholar]
- 20.Crotti TN, Dharmapatni AA, Alias E, Zannettino AC, Smith MD, Haynes DR. The immunoreceptor tyrosine-based activation motif (ITAM)-related factors are increased in synovial tissue and vasculature of rheumatoid arthritic joints. Arthritis Res Ther. 2012;14:R245. doi: 10.1186/ar4088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barrow AD, Raynal N, Andersen TL, Slatter DA, Bihan D, Pugh N, Cella M, Kim T, Rho J, Negishi-Koga T, et al. OSCAR is a collagen receptor that costimulates osteoclastogenesis in DAP12-deficient humans and mice. J Clin Invest. 2011;121:3505–3516. doi: 10.1172/JCI45913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schultz HS, Guo L, Keller P, Fleetwood AJ, Sun M, Guo W, Ma C, Hamilton JA, Bjørkdahl O, Berchtold MW, et al. OSCAR-collagen signaling in monocytes plays a proinflammatory role and may contribute to the pathogenesis of rheumatoid arthritis. Eur J Immunol. 2016;46:952–963. doi: 10.1002/eji.201545986. [DOI] [PubMed] [Google Scholar]
- 23.Schultz HS, Nitze LM, Zeuthen LH, Keller P, Gruhler A, Pass J, Chen J, Guo L, Fleetwood AJ, Hamilton JA, et al. Collagen induces maturation of human monocyte-derived dendritic cells by signaling through osteoclast-associated receptor. J Immunol. 2015;194:3169–3179. doi: 10.4049/jimmunol.1402800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Braun T, Zwerina J. Positive regulators of osteoclastogenesis and bone resorption in rheumatoid arthritis. Arthritis Res Ther. 2011;13:235. doi: 10.1186/ar3380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL. TNF-α induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest. 2000;106:1481–1488. doi: 10.1172/JCI11176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao B, Grimes SN, Li S, Hu X, Ivashkiv LB. TNF-induced osteoclastogenesis and inflammatory bone resorption are inhibited by transcription factor RBP-J. J Exp Med. 2012;209:319–334. doi: 10.1084/jem.20111566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kobayashi K, Takahashi N, Jimi E, Udagawa N, Takami M, Kotake S, Nakagawa N, Kinosaki M, Yamaguchi K, Shima N, et al. Tumor necrosis factor α stimulates osteoclast differentiation by a mechanism independent of the ODF/RANKL-RANK interaction. J Exp Med. 2000;191:275–286. doi: 10.1084/jem.191.2.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong BR, Rho J, Arron J, Robinson E, Orlinick J, Chao M, Kalachikov S, Cayani E, Bartlett FS, 3rd, Frankel WN, et al. TRANCE is a novel ligand of the tumor necrosis factor receptor family that activates c-Jun N-terminal kinase in T cells. J Biol Chem. 1997;272:25190–25194. doi: 10.1074/jbc.272.40.25190. [DOI] [PubMed] [Google Scholar]
- 29.Anderson DM, Maraskovsky E, Billingsley WL, Dougall WC, Tometsko ME, Roux ER, Teepe MC, DuBose RF, Cosman D, Galibert L. A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature. 1997;390:175–179. doi: 10.1038/36593. [DOI] [PubMed] [Google Scholar]
- 30.O'Brien W, Fissel BM, Maeda Y, Yan J, Ge X, Gravallese EM, Aliprantis AO, Charles JF. RANK-independent osteoclast formation and bone erosion in inflammatory arthritis. Arthritis Rheumatol. 2016;68:2889–2900. doi: 10.1002/art.39837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim JH, Jin HM, Kim K, Song I, Youn BU, Matsuo K, Kim N. The mechanism of osteoclast differentiation induced by IL-1. J Immunol. 2009;183:1862–1870. doi: 10.4049/jimmunol.0803007. [DOI] [PubMed] [Google Scholar]
- 32.Axmann R, Böhm C, Krönke G, Zwerina J, Smolen J, Schett G. Inhibition of interleukin-6 receptor directly blocks osteoclast formation in vitro and in vivo. Arthritis Rheum. 2009;60:2747–2756. doi: 10.1002/art.24781. [DOI] [PubMed] [Google Scholar]
- 33.Santiago MB, Galvão V. Jaccoud arthropathy in systemic lupus erythematosus: analysis of clinical characteristics and review of the literature. Medicine (Baltimore) 2008;87:37–44. doi: 10.1097/MD.0b013e3181632d18. [DOI] [PubMed] [Google Scholar]
- 34.Brennan FM, McInnes IB. Evidence that cytokines play a role in rheumatoid arthritis. J Clin Invest. 2008;118:3537–3545. doi: 10.1172/JCI36389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arbuckle MR, McClain MT, Rubertone MV, Scofield RH, Dennis GJ, James JA, Harley JB. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med. 2003;349:1526–1533. doi: 10.1056/NEJMoa021933. [DOI] [PubMed] [Google Scholar]
- 36.Takayanagi H, Ogasawara K, Hida S, Chiba T, Murata S, Sato K, Takaoka A, Yokochi T, Oda H, Tanaka K, et al. T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-γ. Nature. 2000;408:600–605. doi: 10.1038/35046102. [DOI] [PubMed] [Google Scholar]
- 37.Pang M, Martinez AF, Jacobs J, Balkan W, Troen BR. RANK ligand and interferon gamma differentially regulate cathepsin gene expression in pre-osteoclastic cells. Biochem Biophys Res Commun. 2005;328:756–763. doi: 10.1016/j.bbrc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 38.Abu-Amer Y. IL-4 abrogates osteoclastogenesis through STAT6-dependent inhibition of NF-κB. J Clin Invest. 2001;107:1375–1385. doi: 10.1172/JCI10530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bendixen AC, Shevde NK, Dienger KM, Willson TM, Funk CD, Pike JW. IL-4 inhibits osteoclast formation through a direct action on osteoclast precursors via peroxisome proliferator-activated receptor γ1. Proc Natl Acad Sci U S A. 2001;98:2443–2448. doi: 10.1073/pnas.041493198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim KW, Kim HR, Kim BM, Cho ML, Lee SH. Th17 cytokines regulate osteoclastogenesis in rheumatoid arthritis. Am J Pathol. 2015;185:3011–3024. doi: 10.1016/j.ajpath.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 41.Kotake S, Udagawa N, Takahashi N, Matsuzaki K, Itoh K, Ishiyama S, Saito S, Inoue K, Kamatani N, Gillespie MT, et al. IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis. J Clin Invest. 1999;103:1345–1352. doi: 10.1172/JCI5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zwerina K, Koenders M, Hueber A, Marijnissen RJ, Baum W, Heiland GR, Zaiss M, McLnnes I, Joosten L, van den Berg W, et al. Anti IL-17A therapy inhibits bone loss in TNF-α-mediated murine arthritis by modulation of the T-cell balance. Eur J Immunol. 2012;42:413–423. doi: 10.1002/eji.201141871. [DOI] [PubMed] [Google Scholar]
- 43.Zaiss MM, Axmann R, Zwerina J, Polzer K, Gückel E, Skapenko A, Schulze-Koops H, Horwood N, Cope A, Schett G. Treg cells suppress osteoclast formation: a new link between the immune system and bone. Arthritis Rheum. 2007;56:4104–4112. doi: 10.1002/art.23138. [DOI] [PubMed] [Google Scholar]
- 44.Zaiss MM, Sarter K, Hess A, Engelke K, Böhm C, Nimmerjahn F, Voll R, Schett G, David JP. Increased bone density and resistance to ovariectomy-induced bone loss in FoxP3-transgenic mice based on impaired osteoclast differentiation. Arthritis Rheum. 2010;62:2328–2338. doi: 10.1002/art.27535. [DOI] [PubMed] [Google Scholar]
- 45.Axmann R, Herman S, Zaiss M, Franz S, Polzer K, Zwerina J, Herrmann M, Smolen J, Schett G. CTLA-4 directly inhibits osteoclast formation. Ann Rheum Dis. 2008;67:1603–1609. doi: 10.1136/ard.2007.080713. [DOI] [PubMed] [Google Scholar]
- 46.van Venrooij WJ, Pruijn GJ. Citrullination: a small change for a protein with great consequences for rheumatoid arthritis. Arthritis Res. 2000;2:249–251. doi: 10.1186/ar95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stenberg P, Roth B, Wollheim FA. Peptidylarginine deiminases and the pathogenesis of rheumatoid arthritis: a reflection of the involvement of transglutaminase in coeliac disease. Eur J Intern Med. 2009;20:749–755. doi: 10.1016/j.ejim.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 48.James EA, Moustakas AK, Berger D, Huston L, Papadopoulos GK, Kwok WW. Definition of the peptide binding motif within DRB1*1401 restricted epitopes by peptide competition and structural modeling. Mol Immunol. 2008;45:2651–2659. doi: 10.1016/j.molimm.2007.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Koning F, Thomas R, Rossjohn J, Toes RE. Coeliac disease and rheumatoid arthritis: similar mechanisms, different antigens. Nat Rev Rheumatol. 2015;11:450–461. doi: 10.1038/nrrheum.2015.59. [DOI] [PubMed] [Google Scholar]
- 50.Scally SW, Petersen J, Law SC, Dudek NL, Nel HJ, Loh KL, Wijeyewickrema LC, Eckle SB, van Heemst J, Pike RN, et al. A molecular basis for the association of the HLA-DRB1 locus, citrullination, and rheumatoid arthritis. J Exp Med. 2013;210:2569–2582. doi: 10.1084/jem.20131241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Catrina AI, Ytterberg AJ, Reynisdottir G, Malmström V, Klareskog L. Lungs, joints and immunity against citrullinated proteins in rheumatoid arthritis. Nat Rev Rheumatol. 2014;10:645–653. doi: 10.1038/nrrheum.2014.115. [DOI] [PubMed] [Google Scholar]
- 52.Holers VM, Demoruelle MK, Kuhn KA, Buckner JH, Robinson WH, Okamoto Y, Norris JM, Deane KD. Rheumatoid arthritis and the mucosal origins hypothesis: protection turns to destruction. Nat Rev Rheumatol. 2018;14:542–557. doi: 10.1038/s41584-018-0070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, Kavanaugh A, McInnes IB, Solomon DH, Strand V, et al. Rheumatoid arthritis. Nat Rev Dis Primers. 2018;4:18001. doi: 10.1038/nrdp.2018.1. [DOI] [PubMed] [Google Scholar]
- 54.Harre U, Georgess D, Bang H, Bozec A, Axmann R, Ossipova E, Jakobsson PJ, Baum W, Nimmerjahn F, Szarka E, et al. Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J Clin Invest. 2012;122:1791–1802. doi: 10.1172/JCI60975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Krishnamurthy A, Joshua V, Haj Hensvold A, Jin T, Sun M, Vivar N, Ytterberg AJ, Engström M, Fernandes-Cerqueira C, Amara K, et al. Identification of a novel chemokine-dependent molecular mechanism underlying rheumatoid arthritis-associated autoantibody-mediated bone loss. Ann Rheum Dis. 2016;75:721–729. doi: 10.1136/annrheumdis-2015-208093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kleyer A, Finzel S, Rech J, Manger B, Krieter M, Faustini F, Araujo E, Hueber AJ, Harre U, Engelke K, et al. Bone loss before the clinical onset of rheumatoid arthritis in subjects with anticitrullinated protein antibodies. Ann Rheum Dis. 2014;73:854–860. doi: 10.1136/annrheumdis-2012-202958. [DOI] [PubMed] [Google Scholar]
- 57.Faloni AP, Sasso-Cerri E, Rocha FR, Katchburian E, Cerri PS. Structural and functional changes in the alveolar bone osteoclasts of estrogen-treated rats. J Anat. 2012;220:77–85. doi: 10.1111/j.1469-7580.2011.01449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wigerblad G, Bas DB, Fernades-Cerqueira C, Krishnamurthy A, Nandakumar KS, Rogoz K, Kato J, Sandor K, Su J, Jimenez-Andrade JM, et al. Autoantibodies to citrullinated proteins induce joint pain independent of inflammation via a chemokine-dependent mechanism. Ann Rheum Dis. 2016;75:730–738. doi: 10.1136/annrheumdis-2015-208094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brinkmann V, Zychlinsky A. Neutrophil extracellular traps: is immunity the second function of chromatin? J Cell Biol. 2012;198:773–783. doi: 10.1083/jcb.201203170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khandpur R, Carmona-Rivera C, Vivekanandan-Giri A, Gizinski A, Yalavarthi S, Knight JS, Friday S, Li S, Patel RM, Subramanian V, et al. NETs are a source of citrullinated autoantigens and stimulate inflammatory responses in rheumatoid arthritis. Sci Transl Med. 2013;5:178ra40. doi: 10.1126/scitranslmed.3005580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.So AK, Martinon F. Inflammation in gout: mechanisms and therapeutic targets. Nat Rev Rheumatol. 2017;13:639–647. doi: 10.1038/nrrheum.2017.155. [DOI] [PubMed] [Google Scholar]
- 62.Major TJ, Dalbeth N, Stahl EA, Merriman TR. An update on the genetics of hyperuricaemia and gout. Nat Rev Rheumatol. 2018;14:341–353. doi: 10.1038/s41584-018-0004-x. [DOI] [PubMed] [Google Scholar]
- 63.Choe JY, Park KY, Kim SK. Monosodium urate in the presence of RANKL promotes osteoclast formation through activation of c-Jun N-terminal kinase. Mediators Inflamm. 2015;2015:597512. doi: 10.1155/2015/597512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang C, Qu C, Alippe Y, Bonar SL, Civitelli R, Abu-Amer Y, Hottiger MO, Mbalaviele G. Poly-ADP-ribosylation-mediated degradation of ARTD1 by the NLRP3 inflammasome is a prerequisite for osteoclast maturation. Cell Death Dis. 2016;7:e2153. doi: 10.1038/cddis.2016.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Robaszkiewicz A, Qu C, Wisnik E, Ploszaj T, Mirsaidi A, Kunze FA, Richards PJ, Cinelli P, Mbalaviele G, Hottiger MO. ARTD1 regulates osteoclastogenesis and bone homeostasis by dampening NF-κB-dependent transcription of IL-1β. Sci Rep. 2016;6:21131. doi: 10.1038/srep21131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qu C, Bonar SL, Hickman-Brecks CL, Abu-Amer S, McGeough MD, Peña CA, Broderick L, Yang C, Grimston SK, Kading J, et al. NLRP3 mediates osteolysis through inflammation-dependent and -independent mechanisms. FASEB J. 2015;29:1269–1279. doi: 10.1096/fj.14-264804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Takami M, Kim N, Rho J, Choi Y. Stimulation by Toll-like receptors inhibits osteoclast differentiation. J Immunol. 2002;169:1516–1523. doi: 10.4049/jimmunol.169.3.1516. [DOI] [PubMed] [Google Scholar]
- 68.Ji JD, Park-Min KH, Shen Z, Fajardo RJ, Goldring SR, McHugh KP, Ivashkiv LB. Inhibition of RANK expression and osteoclastogenesis by TLRs and IFN-γ in human osteoclast precursors. J Immunol. 2009;183:7223–7233. doi: 10.4049/jimmunol.0900072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu-Bryan R, Scott P, Sydlaske A, Rose DM, Terkeltaub R. Innate immunity conferred by Toll-like receptors 2 and 4 and myeloid differentiation factor 88 expression is pivotal to monosodium urate monohydrate crystal-induced inflammation. Arthritis Rheum. 2005;52:2936–2946. doi: 10.1002/art.21238. [DOI] [PubMed] [Google Scholar]
- 70.Rezaei H, Saevarsdottir S, Forslind K, Albertsson K, Wallin H, Bratt J, Ernestam S, Geborek P, Pettersson IF, van Vollenhoven RF. In early rheumatoid arthritis, patients with a good initial response to methotrexate have excellent 2-year clinical outcomes, but radiological progression is not fully prevented: data from the methotrexate responders population in the SWEFOT trial. Ann Rheum Dis. 2012;71:186–191. doi: 10.1136/annrheumdis-2011-200038. [DOI] [PubMed] [Google Scholar]
- 71.Takeuchi T, Tanaka Y, Ishiguro N, Yamanaka H, Yoneda T, Ohira T, Okubo N, Genant HK, van der Heijde D. Effect of denosumab on Japanese patients with rheumatoid arthritis: a dose-response study of AMG 162 (Denosumab) in patients with RheumatoId arthritis on methotrexate to Validate inhibitory effect on bone Erosion (DRIVE)-a 12-month, multicentre, randomised, double-blind, placebo-controlled, phase II clinical trial. Ann Rheum Dis. 2016;75:983–990. doi: 10.1136/annrheumdis-2015-208052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Redlich K, Smolen JS. Inflammatory bone loss: pathogenesis and therapeutic intervention. Nat Rev Drug Discov. 2012;11:234–250. doi: 10.1038/nrd3669. [DOI] [PubMed] [Google Scholar]