Abstract
Introduction
Biophysical stimulation is a non-invasive therapy used in orthopaedic practice to increase and enhance reparative and anabolic activities of tissue.
Methods
A sistematic web-based search for papers was conducted using the following titles: (1) pulsed electromagnetic field (PEMF), capacitively coupled electrical field (CCEF), low intensity pulsed ultrasound system (LIPUS) and biophysical stimulation; (2) bone cells, bone tissue, fracture, non-union, prosthesis and vertebral fracture; and (3) chondrocyte, synoviocytes, joint chondroprotection, arthroscopy and knee arthroplasty.
Results
Pre-clinical studies have shown that the site of interaction of biophysical stimuli is the cell membrane. Its effect on bone tissue is to increase proliferation, synthesis and release of growth factors. On articular cells, it creates a strong A2A and A3 adenosine-agonist effect inducing an anti-inflammatory and chondroprotective result. In treated animals, it has been shown that the mineralisation rate of newly formed bone is almost doubled, the progression of the osteoarthritic cartilage degeneration is inhibited and quality of cartilage is preserved. Biophysical stimulation has been used in the clinical setting to promote the healing of fractures and non-unions. It has been successfully used on joint pathologies for its beneficial effect on improving function in early OA and after knee surgery to limit the inflammation of periarticular tissues.
Discussion
The pooled result of the studies in this review revealed the efficacy of biophysical stimulation for bone healing and joint chondroprotection based on proven methodological quality.
Conclusion
The orthopaedic community has played a central role in the development and understanding of the importance of the physical stimuli. Biophysical stimulation requires care and precision in use if it is to ensure the success expected of it by physicians and patients.
Keywords: Biophysical stimulation, Bone tissue, Cartilage, PEMF, CCEF, LIPUS
Biophysical stimulation
Clinical biophysics forms the foundation of a “new pharmacology” which uses physical stimuli to treat various diseases in human beings. Biophysical stimulation techniques can be used in clinical medicine, either alone, to increase and promote the repair and anabolic activity in tissue, or in association with drug treatment, to strengthen its activity and lessen side effects. Clinical biophysics is an interdisciplinary science which:
Uses methods and theories from the field of physics to study biological systems
Studies how non-ionising physical stimuli interact with biological systems
The medical community is certainly familiar with the idea of modifying the behaviour of a certain cellular activity using a chemical agent or macromolecules, such as growth factors, genes or a part of these. The ability to modify the activity of a biological target using a physical agent, however, is a more recent and unfamiliar discovery.
The ability of biological systems to absorb energy initially led researchers to focus their attention on dose as the fundamental parameter on which “all” the effects depend. Research then moved to the biological effects dependent not only and not so much on the total energy introduced into the system, as on the other properties which describe the physical agent: frequency, amplitude and the form of the signal wave.
The complexity of the interaction between physical agents and biological systems has made the researchers’ work particularly difficult, and it is only today that we have acquired a degree of knowledge such that physics can significantly help the development of biology and lead to the opening of new horizons where the clinical use of physical means is concerned.
The methods for administrating physical energy to a biological system are known as biophysical stimulation and can be divided into electrical energy applied directly to the tissue using adhesive electrodes (capacitively coupled electrical field, CCEF), electromagnetic energy applied using coils (pulsed electromagnetic fields, PEMFs) and ultrasound energy applied directly to the tissue in the form of mechanical forces (low intensity pulsed ultrasound system, LIPUS).
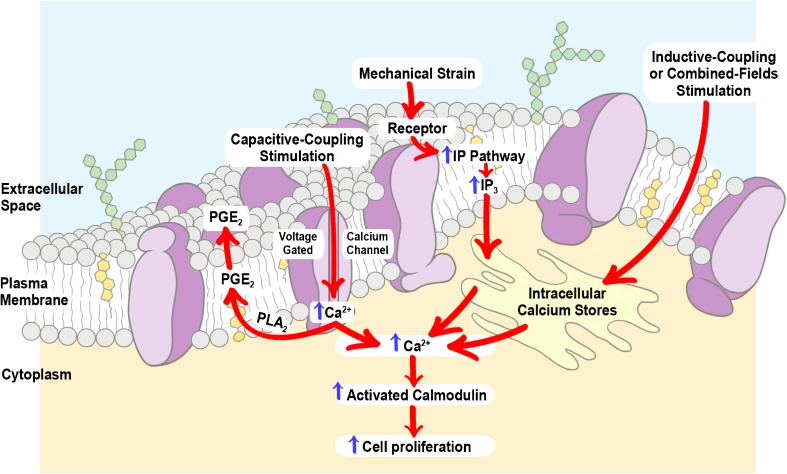
Underlying the new pharmacology is the need to identify the effects of the physical agents in terms of how these modulate a particular cell function, which will then form the basis of its clinical application. The cell membrane has been identified as a target and site of interaction, through which the physical signal activates a cascade of intracellular events; the transduction pathways have been seen to differ depending on the type of energy used (Fig. 1). Each time a physical agent is able to modulate a cell activity, the effect observed will be function-specific, rather than cell- or tissue-specific. This allows all conditions which are positively influenced by the activation or modulation of this cell function to be treated with the same physical agent.
Fig. 1.
Schematic representation of the biophysical stimuli targets on the cell surface and corresponding metabolic pathways within the cell
The key principles of biophysical stimulation are as follows:
The ability of the physical stimulus to act selectively on cell targets
Signal specificity, i.e. the effect depends on waveform, frequency, duration and energy
Identification of the dose-response effects
The signal should maintain the characteristics identified as being effective at the disease site.
Knowledge of the mechanism of action should provide the rational basis for clinical application, permitting the clinical studies and relative end-points to be designed in a coherent manner.
Biophysical stimulation: in vitro studies
Effects of biophysical stimulation on bone cells
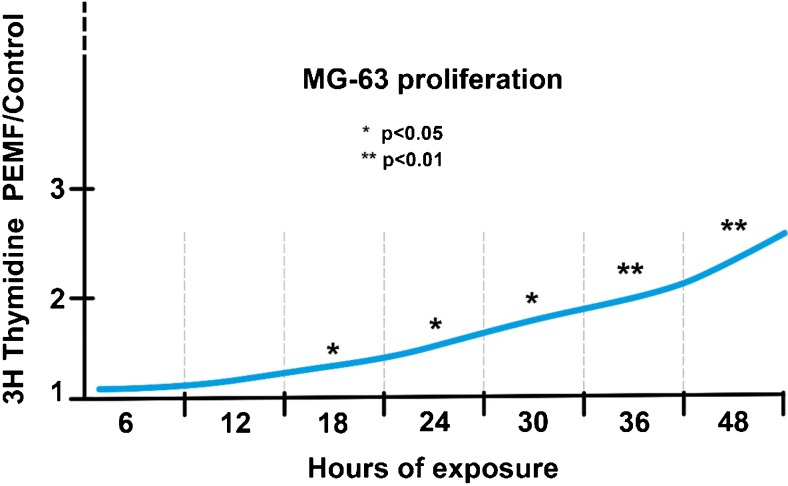
Numerous studies have analysed the effects of biophysical stimulation on osteoblast proliferation and have highlighted a dose-response effect for exposure times, PEMF intensity, frequencies and signal waveforms [1, 2] (Fig. 2). More specifically, Brighton et al. [3] showed that a CCEF of 0.1–10 mV/cm stimulates the proliferation of rat calvarial bone cells, while lower intensities proved ineffective. In human osteosarcoma cell lines and osteoblast cells in vitro, De Mattei et al. [4] identified a relationship between PEMF exposure times and the increase in proliferation, as well as differences in exposure times between different cultures. Leung et al. [5] studied the effect of LIPUS on cell cultures of human periosteal cells, along with the effects in relation to time and dosage. Total number of live cells, cell proliferation, alkaline phosphatase activity, osteocalcin secretion and expression of vascular endothelial growth factors were evaluated. The authors demonstrated a clear dose-dependent effect, the greatest efficacy being recorded at 20 minutes exposure. Similar to that reported for the proliferative effects, in vitro studies have shown that in various cell models, biophysical stimulation induces (i) an increase in osteoblast differentiation, promoting the production of collagen and of the main matrix glycoproteins osteocalcin and osteopontin [6, 7]; (ii) stimulates the mineralisation process [8, 9]; and (iii) plays an inhibitory role in the process of osteoclast differentiation and exerts a protective action against osteolysis [10]. The increases induced by biophysical stimulation in the production of bone matrix are very similar to those induced by growth factors such as TGF-β1, BMPs and growth factor IGF-I, indicating that the effects induced by a biophysical stimulus are of significant medical importance [11, 12] (Table 1).
Fig. 2.
Effect of PEMF exposure length on human osteosarcoma cell lines and human osteoblast cell (MG63) proliferation (Sollazzo et al. Electricity and Magnetism in Biology and Medicine 1997)
Table 1.
Biophysical stimulation on the regulation of bone matrix and growth factors
| Author | Physical method | In vitro models | Results |
|---|---|---|---|
| Jansen JH, BMC Musculoskelet Disord. 2010 | PEMFs | hBMSCs | ↑ TGF-β1 ↑ BMP-2mRNA ↑ Differentiation |
| Esposito M, In Vivo. 2012 | PEMFs | hBMSCs | ↑ Proliferation ↑ Differentiation |
| Ceccarelli G, Biores Open Access. 2013 | PEMFs | hBMSCs | ↑ Proliferation ↑ ECM deposition |
| Zhou J, Bioelectromagnetics. 2013 | PEMFs | Rat calvarial osteoblasts | ↑ Proliferation |
| Hartig M, Eur Biophys J. 2000 | CCEF | Osteoblast from periosteum explants | ↑ Proliferation ↑ Differentiation |
| Wang Z, J Bone Joint Surg Am. 2006 | CCEF | Osteoblastic cells (MC3T3-E1) | ↑ BMP-2,4,5,6,7 mRNA |
| Bisceglia B, Bioelectromagnetics. 2011 | CCEF | Osteoblast-like cell lines (SAOS-2) | ↑ Proliferation |
| Clark CC, J Orthop Res. 2014 | CCEF | Human calvarial osteoblasts | ↑ BMP-2,4 mRNA ↑ TGF-β1, β2, β3 mRNA ↑ FGF-2 |
| Hauser J, J Orthop Res. 2009 | LIPUS | Osteoblast-like cell lines (SAOS-2) | ↑ Proliferation |
| Fassina L, Bioinorg Chem Appl. 2010 | LIPUS | SAOS-2 human osteoblasts | ↑ Proliferation ↑ ECM deposition |
| Xue H, PLoS One. 2013 | LIPUS | Alveolar bone in vivo | ↑ BMP-2 mRNA |
| Carina V, J Appl Biomater Funct Mater. 2017 | LIPUS | Human mesenchymal stem cells | ↑ Proliferation ↑ MgHA/coll hybrid composite scaffold ↑ VEGF gene expression |
Effects of biophysical stimulation on articular cells
Extensive in vitro data reported in literature shows the effect of PEMFs on articular cells (Table 2). In bovine chondrocytes and synoviocytes [13, 14], A2A and A3 adenosine receptors, endogenous modulator of many biological processes such as inflammation, increased in number in the presence of PEMFs, reducing the release of PGE2, IL-6, IL-8 and COX-2, a result which suggests a reduction in the inflammatory state and in the degradation of cartilage associated with articular diseases. Human synoviocytes treated with PEMFs reveal a significant increase in A2A and A3 adenosine receptors, as demonstrated by the mRNA, Western blotting analysis and saturation binding experiments involving ARs, as well as a significant increase in the release of IL-10, a known anti-inflammatory cytokine [15]. The A2A and A3 receptors exert their anti-inflammatory action by inhibiting the NF-κB transcription factor pathway, which plays a central role in regulating the synthesis and activities of the inflammatory cytokines. Stimulation with PEMFs further inhibits the activation of NF-κB and is essential for regulating the synthesis and activation of the pro-inflammatory cytokines, including TNF-α and IL-1β, and also of other mediators involved in joint inflammation and bone diseases [16]. PEMFs have been shown to affect the increase of human articular chondrocyte proliferation, based on exposure time, intensity and frequency [17]. It should be stressed that the effect of PEMFs on proteoglycan synthesis in human cartilage explants is comparable in all senses to that induced by growth factor IGF-I, the principal cartilage anabolic factor [18, 19]. While the presence of IL-1β inhibits the synthesis of proteoglycans, exposure to PEMFs can curb the catabolic effect of the cytokine, increasing proteoglycan synthesis even under inflammatory conditions [20]. It is interesting to observe that these results regarding the anti-inflammatory role of PEMFs are also confirmed in the stem cell cultures [21].
Table 2.
Pulsed electromagnetic field effect in articular cells
| Culture | PEMF effects |
|---|---|
| Bovine chondrocytes and synovial fibroblasts | Increase of A2A and A3 receptors |
| Increase of cellular proliferation | |
| Inhibition PGE2 release | |
| Bovine articular cartilage explants | Increase of proteoglycan synthesis |
| Chondroprotective effect | |
| Human synovial fibroblasts | Inhibition of PGE2 IL-6, IL-8, and TNF-α release |
| Stimulation of IL-10 release | |
| Human articular cartilage explants | Increase of proteoglycan synthesis |
| Counteract the catabolic activity of IL-1b | |
| Increase of cartilage explant anabolic activities | |
| Human T/C-28a2 chondrocytes and hFOB 1.19 osteoblasts | Increase of A2A and A3 receptors |
| Inhibition of PGE2 IL-6, IL-8, and VEGF release | |
| Increase of cellular proliferation | |
| Increase of osteoprotegerin (OPG) production | |
| Inhibition of NF-κB activation | |
| Reduction of cAMP levels |
Biophysical stimulation: in vivo studies
Effects of biophysical stimulation on bone repair
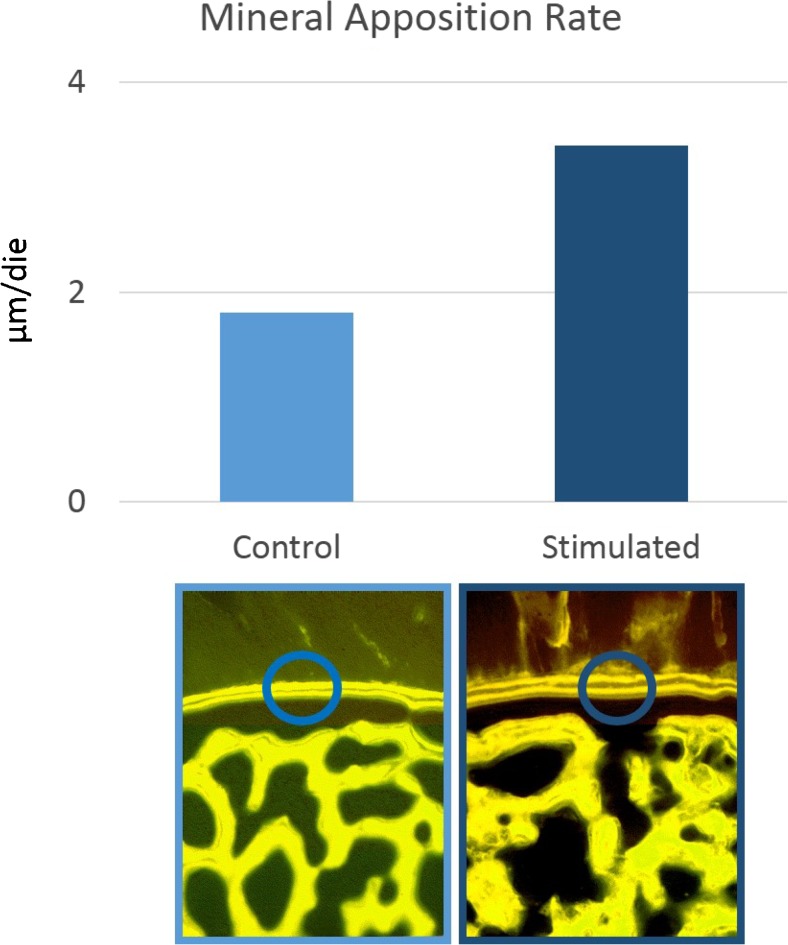
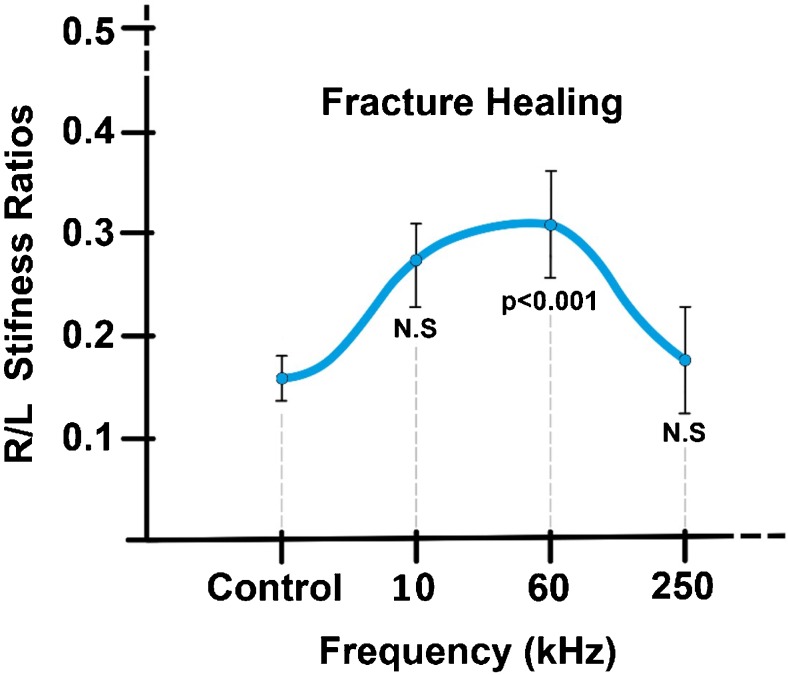
There are numerous studies in literature, performed in animal models as early as the 1970s, which attest to the osteogenic effects of biophysical stimulation in bone repair. In a 1974 study on dogs, Bassett et al. [22] demonstrated the effect of PEMFs in stimulating the repair of a bilateral fibular osteotomy, indicating the need to carry out further studies to ascertain the physical characteristics of the signal most effective in obtaining the biological effect desired. De Haas et al. [23] also published a study whose objective was to evaluate the effect of PEMFs at different frequencies in an experimental rabbit osteotomy model, showing that the treatment does not cause pathological alterations to the tissues and that different signal characteristics could result in different outcomes. In transcortical holes bored in the distal metaphysis and diaphysis of the third metacarpal bone in horses, the histological results demonstrate that PEMFs increase the quantity of newly deposited bone inside the hole from 40 to 120% more compared to the controls and that the amount of newly deposited bone and mineral apposition rate inside the holes are significantly greater in the treated limbs compared to controls [24] (Fig. 3). In 2005, Midura et al. [25] exposed rat osteotomies to PEMF stimulation at two different frequencies and intensities (15 Hz, 2 mT vs 1.5 Hz, 0.02 mT) with similar results, showing that the higher frequency (15 Hz) treatment led to a doubling of both the apposition rate and the volume of the bone callus. The importance of the signal characteristics was also studied for the CCEF and LIPUS methods. In a 1985 study involving a rabbit fibular osteotomy model, Brighton et al. [26] showed that only the 60-KHz frequency, compared to those at 10 and 250 KHz, gave significantly better results than the controls (Fig. 4). In 1994, Rijal et al. [27] created a non-union experimental model, where a DEXA bone densitometry scan showed an increase in density of 18% (p < 0.05) in the CCEF group compared to the controls. In the 1980s, Duarte [28] used LIPUS at a frequency of 1.5 MHz with intensity of 30 mW/cm2 applied for 15 minutes/day in a rabbit fibular osteotomy model, obtaining an increase of 28% in ossification in the limbs treated. A series of in vivo studies followed in the 1990s, giving a better understanding of the ultrasound signal characteristics and treatment times able to accelerate the bone healing process in fractures. In bilateral rabbit fibular osteotomies, Pilla [29] demonstrates that the application of LIPUS (200 μs impulses at 1.5 MHz, at an intensity of 30 mW/cm2 for 20 min/day) accelerates bone healing by a factor of 1.7 compared to controls in terms of mechanical resistance. The LIPUS applied have characteristics that have already been approved by the FDA for use in clinical medicine for 20 minutes/day.
Fig. 3.
Effect of PEMF stimulation on mineral apposition rate in newly formed trabeculae measured by tetracycline labelling, in transcortical holes bored in the distal metaphysis and diaphysis of the third metacarpal bone in horses (Canè V et al. J Orthop Res 1993)
Fig. 4.
Effect of CCEF frequency on fibula osteotomy healing in rabbits (Brighton CT et al. J Orthop Res 1985)
As clearly emerges from the studies illustrated, obtaining the desired biological effect depends on the type of signal used. For this reason, basic pre-clinical research is fundamental for identifying the physical characteristics of the stimulus able to interact with the biological system to be influenced and in defining its value for clinical practice.
Effects of biophysical stimulation on articular cartilage
Studies based on in vitro and ex vivo results have been performed on large and small animal models to evaluate the effect of PEMFs in preventing osteoarthrosic degeneration and in the repair of tissue damage, as an adjunct to tissue engineering methods.
In Dunkin Hartley guinea pigs [30], treatment with PEMFs was demonstrated as being capable of halting the progression of osteoarthrosis, of limiting cartilage surface clefts and fibrillation, of preserving cartilage thickness and of preventing sclerosis of the subchondral bone. These results are coherent with those of other authors, who have demonstrated an increase in TGF-β1 synthesis and an inhibition of TNF-α synthesis (with a clear anabolic and trophic effect on the articular cartilage) in the animals treated using biophysical stimulation. Autologous osteochondral autografts were performed in adult sheep [31], resulting in a significantly better osteointegration of the graft and a lesser formation of cyst-like resorption areas in the PEMF group. The synovial liquid in the stimulated animals contained significantly lower levels of pro-inflammatory cytokines IL-1β and TNF-α and a higher concentration of TGF-β1 compared to the untreated animals. PEMFs have proved effective in rabbits with osteochondral lesions [32], significantly improving the quality of the regenerated tissue in the osteochondral defects in the presence of collagen scaffold and bone marrow concentrate.
The anti-inflammatory activity of PEMFs effectively prevented the degenerative effect of IL-1β, significantly improving cartilage regeneration compared to the non-stimulated lesions, thus explaining the anti-degenerative, reparative and anti-inflammatory effects of treatment with PEMFs in in vivo models also.
Biophysical stimulation: clinical experiences on bone tissue
Osteotomy
The first studies on the effect of biophysical stimulation recognised as having level of evidence I status were three in number and were conducted by the Italian orthopaedic community as early as the 1980s, on patients undergoing osteotomy of the lower limbs. The studies report a significant increase in the density of the trabecular bone callus in the active group compared to the placebo group [33], a higher consolidation success rate [34] and a shortening of consolidation time by three months [35] (Fig. 5).
Fig. 5.
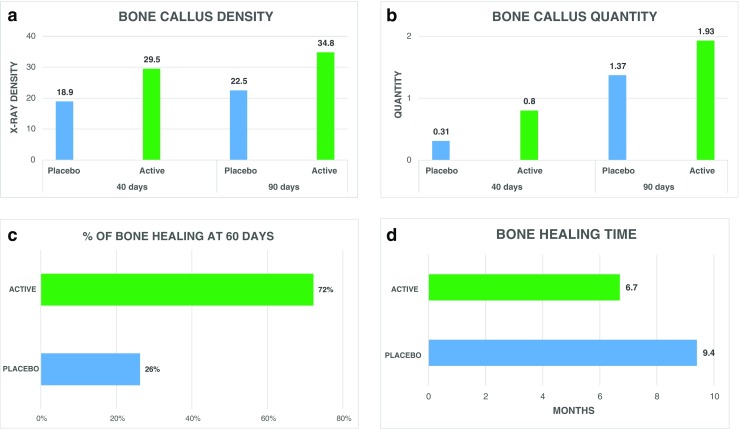
Effect of PEMF (a, b) on femoral osteotomies at 40 and 90 days from surgery (Borsalino G et al. Clin Orthop Relat Res 1988), (c) on tibia osteotomies (Mammi GI et al. Clin Orthop Relat Res 1993) and (d) in patients undergoing allograft reconstruction following tumour resection (Capanna R et al. Clin Orthop Relat Res 1994)
Fractures at risk of non-union
Biophysical stimulation has proved capable of accelerating the healing of “at-risk” fractures treated by plaster casting or internal or external fixation or complex fractures with serious damage to soft tissues and exposure of bone tissue [36, 37]. In patients with femur neck fractures, Faldini et al. [38] report a percentage of healing of 94% in the PEMF group compared to 69% in the placebo group, while Benazzo et al. [39], using the CCEF technique on athletes with stress fractures, observed a reduction in functional recovery times with a success rate of 88%. In patients with fractures immobilised using plaster casting, external fixator or intramedullary nails, various authors report a significant reduction of 38% in healing times using LIPUS [40–43].
Non-unions
There is abundant clinical evidence in international literature supporting the efficacy of biophysical stimulation on non-union fractures, particularly with PEMFs; authors have reported success rates of around 70–80% [44, 45] (Table 3). Good results have also been obtained in the treatment of non-union fractures with CCEFs and with LIPUS, albeit on a lesser scale.
Table 3.
Summary of main clinical studies using pulsed electromagnetic field therapy in non-unions
| Author | Design of the study | Non-union, treatment | Groups | Number | Results: success rate and healing time |
|---|---|---|---|---|---|
| De Haas WG, J Bone Joint Surg Br. 1980 | Case series | Tibial non-union, cast | Stimulated | 17 patients | 88.2% in 5.9 months |
| Bassett CA, J Bone Joint Surg Am. 1981 | Case series | Tibial non-union | Stimulated | 125 patients | 87% |
| Simonis RB, Injury 1984 | Case series | Non-union of long bone, external fixator | Stimulated | 15 non-unions | 87% in 4 months |
| Sedel L, Rev. Chir Orthop Reparatrice Appar Mot. 1981 | Case series | Non-union, different treatment | Stimulated | 37 patients | 83% |
| Bassett CA, JAMA. 1982 | Case series (cross-sectional international study) | Non-union and failed arthrodesis | Stimulated | 1007 non-unions, 71 failed arthrodesis | 85% |
| Sharrard WJ, J Bone Joint Surg Br. 1982 | Case series | Non-union of tibia, femur, ulna, radius, humerus, capitellum, knee, ankle | Stimulated | 53 non-unions | 71.7% (86.7% tibia) in 6 months |
| Marcer M, Clin Orthop Relat Res. 1984 | Case series | Non-union of tibia, femur, humerus, external fixator | Stimulated | 147 patients | 73% |
| Hinsenkamp M, Reconstr Surg Traumatol. 1985 | Case series | Non union | Stimulated | 308 patients | 70% |
| Frykman GK, J Hand Surg [Am]. 1986 | Case series | Non-united scaphoid fracture, cast | Stimulated | 44 non-unions | 79% |
| Traina GC, Giornale Italiano di Ortopedia. 1986 | Case series | Non-union, cast, external fixator, other | Stimulated | 248 patients | 84% in 4.3 months |
| Garland DE, Contemp Orthop. 1991 | Case series | Non-union, external and fixator | Stimulated | 139 non-unions | 80% (> 3 h/die) vs 35.7% (< 3 h/die) in 12 weeks |
| Gupta AK, Indian J Orthop. 2009 | Case series | Tibial non-union, cast | Stimulated | 45 fractures | 85%, in 4 months |
| Assiotis A, J Orthop Surg Res. 2012 | Case series | Tibial non-union, plates, nail, plaster of Paris | Stimulated | 44 patients | 77.3% |
| Punt BJ, Eur J Orthop Surg Traumatol. 2008 | Prospective comparative study | Non-union of long bone, non-long bone cast, external fixator, other | Stimulated (long bone vs non-long bone) | 93 patients | 76 vs 79% |
| Cebrian JL, International Orthopaedics. 2010 | Prospective comparative study | Tibial non-union, intramedullary nailing | Stimulated vs stimulated + surgery | 22 vs 35 patients | 91 vs 83%, in 3.3 vs 4.9 months |
| Poli G, J Bioelectricity. 1985 | Randomised controlled double-blind study | Congenital non-union, endomedullary nail fixation | Stimulated vs surgery | 6 vs 6 patients | Lengthening of the limb, stop imbalance between legs |
| Sharrard WJ, J Bone Joint Surg Br. 1990 | Randomised controlled double-blind study | Tibial non-union, cast | Active vs placebo | 20 vs 25 fractures | 45 vs 12% at 12 weeks |
| Simonis RB [44], Injury. 2003 | Randomised controlled double-blind study | Tibial non-union, osteotomy, and external fixator | Active vs placebo | 18 vs 16 patients | 89 vs 50% |
| Shi HF, BMC Musculoskelet Disord. 2013 | Randomised controlled double-blind study | Non-union of long bone, nail, plate | Active vs placebo | 31 vs 27 non-unions | 77.4 vs 48.1% in 4.8 months |
| Traina GC [45], J Bioelectricity. 1991 | Retrospective controlled | Non-union leg, femur, forearm, humerus, metatarsal, clavicle different treatment | Stimulated vs surgery | 41 vs 26 patients | 87.8 vs 69% in 5.7 vs 7.8 months |
| Vaquero DH, Revista de ortopedia y Traumatologia. 2000 | Retrospective cohort | Non-union tibia, femur, humerus, radio, other | Stimulated | 137 non-unions | 74.5% |
Hip prostheses
Biophysical stimulation is an effective treatment for improving bone ingrowth in the presence of biomaterials and to prevent complications deriving from the failure of the implant, such as osteolysis.
In patients with painful uncemented hip prostheses, Rispoli et al. [46] reported a clinically evaluated success rate of good/excellent using PEMF treatment in 91% of those who used the treatment for more than 360 hours, compared to only 12% of non-compliant patients (< 360 hours). A few years later, Kennedy et al. [47] reported a 53% success rate in patients with femoral component loosening treated with PEMFs, compared to 11% of control patients. Dallari et al. [48] demonstrate that treatment with PEMFs eases the relief of pain and aids in clinical healing and the restoration of bone mass following revision total hip replacement.
Vertebral fractures
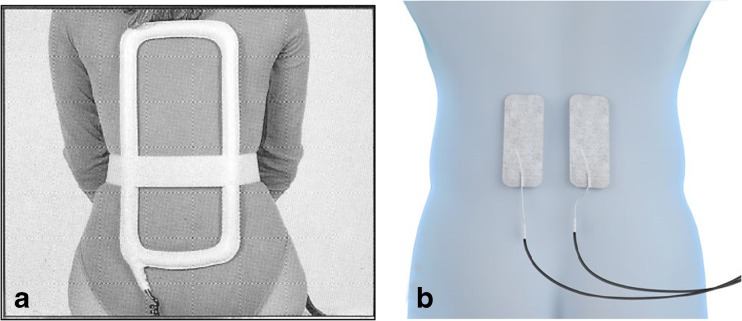
The first multi-centre study on 195 patients with anterior or posterior lumbar fusion reports a 92% success rate in the group stimulated with PEMFs, compared to 65% in the control group [49]. A few years later, Linovitz et al. [50] reported a 64% bone fusion rate in the active group after 9 months, compared to 43% in the placebo group (p < 0.003). Over the last few years, stimulation with CCEF has proved much more comfortable than inductive stimulation, due to the ease of use of the applicators, with fusion success rates of 84% [51] (Fig. 6). Beneficial effects on pain control and a reduced use of nonsteroidal anti-inflammatory drug (NSAIDs) are also described in literature. Rossini et al. [52] reported a significant pain reduction in the active group compared to placebo, with a consequent discontinuation of NSAIDs. Massari [53] and Piazzolla et al. [54] demonstrate an improvement in functional recovery following spinal fusion, and a significant reduction in the area of VBME in compression fractures respectively, with pain resolution times reduced by half.
Fig. 6.
Representation of spinal stimulation with PEMF device (a) and CCEF device (b)
Osteonecrosis
Santori et al. [55] found the association of PEMFs, core decompression and grafts of trabecular bone tissue to be a valid solution in delaying or preventing collapse of the femoral head in the presence of osteonecrosis, with an 81% and 70% success rate in patients with Steinberg stage II and Steinberg stage III osteonecrosis, respectively. The most recent Italian study was conducted on 66 patients with osteonecrosis of the hip, stimulated with PEMFs for 8 h/day [56]. At two month follow-up, 53% of patients no longer reported any pain, and only 26% reported pain of moderate intensity. Radiography results showed a progression of the degeneration in only 26% of the hips studied (Table 4), and similar percentages have also been reported by Cebrian [57].
Table 4.
Need for hip replacement by Ficat stage and progression of hip degeneration
| Ficat | Hip replacement/number of hips | Number of hips (Ficat progression) |
|---|---|---|
| I | 0/31 (0%) | 3 (I ➝ II) |
| II | 3/22 (14%) | 5 (II ➝ III) |
| III | 12/23 (52%) | 12 (III ➝ IV) |
Summary
None of the authors of these studies suggest a blanket use of biophysical stimulation. In those cases in which the site, type of exposure, morphology of the fracture or condition of the patient indicate a risk of difficulties during the healing process, the use of biophysical stimulation is justified as a treatment to activate and finalise the process of osteogenesis and to speed the recovery process.
Biophysical stimulation: clinical experience on joint
Pre-clinical research shows that treatment with PEMFs is anti-degenerative, helping to control local inflammatory phenomena and supporting cartilage repair processes in clinical setting (Table 5). Zorzi et al. [58] combined arthroscopic chondroabrasion and PEMF treatment. They showed that the percentage of patients assuming NSAIDs is significantly lower in those patients treated with PEMF compared to the placebo group and functional scores were significantly better in the PEMF-treated group 90 days after surgery. The recovery times for functionality of the knee were significantly reduced in the short term and 87.5% of patients were unable to return to full sporting activity three years after the procedure in the placebo group, compared to 37.5% in the active group (p < 0.05). Benazzo et al. [59] have demonstrated that the percentage of patients using NSAIDs following ACL reconstruction is significantly lower in the patients treated with PEMFs compared to the placebo group and that the time required for recovery of knee function is significantly reduced in the short term. Two years after the reconstruction of ACL, a complete functional recovery was achieved by 86% of the patients in the active group compared with 75% of the patients in the placebo group. Similar results have been obtained following treatment using collagen scaffold seeded with bone marrow-derived cells for talar osteochondral lesions [60]. At six and 12 months follow-up, significantly higher AOFAS score and significant lower pain were recorded in the experimental group. More recently, Collarile et al. in patients following matrix-assisted autologous chondrocyte implantation (MACI) in the treatment of chondral lesions of the knee [61] show that patients in the PEMFs group had achieved a significantly better pain relief (2 and 6 months follow-up) and clinical outcome at the time of the 60-month follow-up. Two recent Italian studies [62, 63] on patients undergoing total knee arthroplasty have shown that PEMFs led to a significantly greater and more rapid reduction in post-operative pain symptoms as early as the first month and this was maintained at all follow-ups with a significant difference compared to the control group. The same observation was made for swelling. The study by Adravanti, which includes an evaluation 36 months after the procedure, shows that at this time-point only 7% of the patients in the PEMFs group still reported a level of persistent pain requiring the use of anti-inflammatory drugs, compared to 33% of control group patients. Furthermore, no patient in the PEMFs group expressed the need for walking aids compared to approximately 20% of the control group. A study conducted on patients in the early stages of osteoarthrosic degeneration of the knee, treated conservatively with PEMFs rather than surgically, showed significantly better results in terms of functional recovery and pain resolution at 12months follow-up [64]. The author concludes that an annual repetition of the treatment may result in sustained symptomatic improvement for the patient. Similar improvements in joint function, pain resolution and time needed to return to sporting activity were found in patients with patellofemoral pain following treatment with PEMFs [65]. The effect of PEMFs has also been studied in patients in the initial stages of spontaneous osteonecrosis of the knee [66], with results showing a significantly reduced level of pain after 6 months (p < 0.0001), an improvement in functional recovery and a rapid return to sporting activity. These results remained constant even after 24 months. The MRI evaluation at 6-month follow-up showed a significant reduction of total WORMS mean score (p < 0.0001).
Table 5.
Summary of main clinical studies using pulsed electromagnetic field therapy on joint diseases
| Author | Design of the study | Disease/treatment | Groups | Patients | Results | Long-term follow-up results |
|---|---|---|---|---|---|---|
| Marcheggiani Muccioli G [66], European Journal of Radiology. 2013 | Case series | Spontaneous osteonecrosis of the knee | Stimulated | 28 | Pain relief, better functional recovery and necrosis area reduced | 86% of knees preserved from prosthetic surgery at 2 years FU |
| Gobbi A [64], Cartilage. 2014 | Case series | Early OA | Stimulated | 22 | Improvement in symptoms, knee function and activity | At 2-year follow-up, 80% of patients were satisfied and willing to repeat the treatment |
| Moretti B [62], BMC Musculoskeletal Disorders. 2012 | Prospective comparative study | Grade 4 osteoarthrosis/total knee arthroplasty | Surgery + stimulated vs surgery | 15 vs 15 | Pain, joint swelling and knee score were significantly better and lower NSAID use | |
| Adravanti P [63], International Orthopaedics. 2014 | Prospective comparative study | Grade 4 osteoarthrosis/total knee arthroplasty | Surgery + stimulated vs surgery | 16 vs 17 | Pain, knee swelling and functional score were significantly better | Severe pain and occasional walking limitations were reported in a lower number at 3 years FY (p < 0.05) |
| Cadossi M [60], Foot & Ankle International. 2014 | Prospective comparative study | Osteochondral lesions in talar/bone marrow-derived cell transplantation | Surgery + stimulated vs surgery | 15 vs 15 | Pain relief, better functional recovery | |
| Iammarrone CS [65], Bioelectromagnetics. 2016 | Prospective comparative study | Patellofemoral pain | Stimulated vs controlled | 13 vs 17 | Pain relief, better functional recovery and lower NSAID use | |
| Collarile M [61], Knee Surg Sports Traumatol Arthrosc. 2018 | Prospective comparative study | Chondral knee lesions/matrix-assisted autologous chondrocyte implantation | Surgery + stimulated vs surgery | 15 vs 15 | Pain relief, better functional recovery | Better clinical outcome up to 5 years of FU (p < 0.05) |
| Zorzi C [58], Knee Surg Sports Traumatol Arthrosc. 2007 | Randomised controlled double-blind study | Cartilage knee lesions, chondroabrasion/perforation | Active vs placebo | 19 vs 12 | Pain relief, better functional recovery and lower NSAID use | Completely recovered higher in the active group (p < 0.05) at 3 years of FU |
| Benazzo F [59], Knee Surg Sports Traumatol Arthrosc. 2008 | Randomised controlled double-blind study | Anterior cruciate ligament lesion/reconstruction and meniscectomy | Active vs placebo | 31 vs 29 | Pain relief, better functional recovery and lower NSAID use | Complete functional recovery, no knee pain and return to sport activity higher in the active group (p = ns) 2 years of FU |
| Osti L, International Orthopaedics. 2015 | Randomised controlled double-blind study | Grade III–IV cartilage knee lesions/partial medial meniscectomy and microfractures | Active vs placebo | 34 vs 34 | IKDC and Lysholm and constant scores were significantly improved in both groups with no significant intergroup differences | Clinical and functional outcomes were better in the PEMF-treated group at 5 years of FU |
| Osti L, Orthopaedics. 2017 | Randomised controlled double-blind study | Small to medium rotator cuff tears/arthroscopic rotator cuff repair | Active vs placebo | 32 vs 34 | Pain relief, better ROM and stiffness and lower NSAID use | Clinical and functional outcomes were further improved in both groups, with no significant intergroup differences at 2 years of FU |
Summary
PEMF therapy can therefore be used proactively as (i) post-surgical treatment with the objective of quickly controlling local inflammatory response due to the surgical operation and, over the long term, to maintain the mechanical and biological properties of the cartilage or engineered tissue by means of an effective chondroprotective effect; (ii) post-arthroplasty treatment to inhibit the inflammatory processes that affect the periarticular tissues and to avoid the development of chronic pain and functional limitations; and (iii) conservative treatment to limit the progression of a degenerative process such as osteoarthritis that comes with age and is accelerated by inflammatory and/or traumatic events.
Biophysical stimulation: future perspectives
Today, numerous other areas of medicine are preparing to use physical means to treat a variety of conditions or are seeing its potential. Some applications are in their infancy or are still at the stage of in vitro experimentation; however, current evidence seems to suggest that these treatment approaches will become increasingly widespread, for example in the treatment of tendinopathies or in neurology. The effects of PEMFs, in fact, have recently been studied on primary human cells isolated from semitendinosus and gracilis tendons exposed to PEMFs: results show that PEMFs do not alter cell vitality or induce apoptotic phenomena but are able to induce responses at gene expression level and to reduce the production of inflammatory cytokines in the tendon cells [67]. In MSCs isolated from the human umbilical cord and seeded in tendon differentiation medium, PEMF showed a greater production of collagen type I, scleraxis and greatest expression of tenogenic markers [68].
In neurology, there is great interest in the development of novel therapies for acute ischaemic stroke because thrombolysis is the only approved treatment. PEMFs could represent an alternative approach because of their effects on the main mechanisms of brain ischaemia. Capone et al. [69] demonstrated that PEMF can influence cortical excitability and do not produce side effects in healthy volunteers. Recently, a small, open-label, one-arm, exploratory study to evaluate the safety of PEMF stimulation in acute ischemic stroke (clinicaltrials.gov:NCT01941147) has been designed [70]. Preliminary results obtained in six patients demonstrated that a daily exposure of 120 minutes for five consecutive days is safe and tolerable.
Conclusion
Biophysical stimulation is the result of solid scientific research. As reported in 2018 by Yuan et al., biophysical stimulation, as a prospective, non-invasive and safe physical therapy strategy to accelerate bone repair, has received tremendous attention in recent decades [71]. Moreover, the promotion effect has shown strikingly positive benefits in the treatment of various skeletal diseases. In the USA and Europe, research on the use of physical energy for bone repair processes has been ongoing throughout the past century. Every year, tens of thousands of patients undergo treatment all over the world. An inquiry to medical hospitals in the USA found that 72% of interviewed were offering biophysical stimulation to patients with fractures not yet healed at three months from trauma [72]. A substantial proportion of Canadian orthopaedic surgeons (45%) currently make use of bone stimulators as part of their management strategy for at least some tibial shaft fractures (for complicated tibial shaft fractures); 80% of respondents felt that a reduction in healing time of six weeks or more, attributed to a bone stimulator, would be clinically important [73]. More recently, in consideration of the sensitivity of cartilage tissue to physical stimuli, the orthopaedic community has now focused its interest on the joint to prevent cartilage degeneration, to enhance cartilage repair and to favour patients’ function recovery. Recently, Iwasa et al. have systematically reviewed the literature on the influence of PEMF in joints, including articular cartilage, tendons and ligaments, of publications from 2000 to 2016 [74]. The authors concluded that PEMF has a beneficial effect on chondrocyte proliferation, matrix synthesis and chondrogenic differentiation by upregulation of TGF-b and BMPs, and it decreases anti-inflammatory cytokines via A2A and A3 adenosine receptors leading in clinical translational investigations, a beneficial effect on pain and functions of OA knees.
The orthopaedic community has undoubtedly played a central role in the development and understanding of the importance of physical stimuli to control biological activities. Orthopaedic research has demonstrated that the effects are dependent on physical parameters and, mediating from pharmacology, has introduced the concept of physical dynamics.
Compared to drug treatment, biophysical stimulation has the clear advantage that it can be administered locally with relative ease and reach the disease site at its maximum “concentration” and therapeutic efficacy, with no side effects. Biophysical treatment appears to be effective for the prolonged treatment of chronic degenerative conditions, while it does not seem suited to treating systemic diseases. An important aspect of treatment with physical agents is the ability to transfer the effects observed in basic research to clinical practice. Further development of the clinical use of physical agents involves overcoming numerous and complex hurdles; however, the ability to recognise and define an area with the potential for new treatment approaches, such as clinical biophysics, is a fundamental step in pointing the way for future research in various sectors.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou J, Wang JQ, Ge BF, et al. Different electromagnetic field waveforms have different effects on proliferation, differentiation and mineralization of osteoblasts in vitro. Bioelectromagnetics. 2014;35(1):30–38. doi: 10.1002/bem.21794. [DOI] [PubMed] [Google Scholar]
- 2.Clark CC, Wang W, Brighton CT. Up-regulation of expression of selected genes in human bone cells with specific capacitively coupled electric fields. J Orthop Res. 2014;32(7):894–903. doi: 10.1002/jor.22595. [DOI] [PubMed] [Google Scholar]
- 3.Brighton CT, Okereke E, Pollack SR, Clark CC (1992) In vitro bone-cell response to a capacitively coupled electrical field. The role of field strength, pulse pattern, and duty cycle. Clin Orthop Relat Res (285):255–62 [PubMed]
- 4.De Mattei M, Caruso A, Traina GC, et al. Correlation between pulsed electromagnetic fields exposure time and cell proliferation increase in human osteosarcoma cell lines and human normal osteoblast cells in vitro. Bioelectromagnetics. 1999;20(3):177–182. doi: 10.1002/(sici)1521-186x(1999)20:3<177::aid-bem4>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Leung KS, Cheung WH, Zhang C, Lee KM, Lo HK (2004) Low intensity pulsed ultrasound stimulates osteogenic activity of human periosteal cells. Clin Orthop Relat Res (418):253–9 [DOI] [PubMed]
- 6.Lohmann CH, Schwartz Z, Liu Y, et al. Pulsed electromagnetic field stimulation of MG63 osteoblast-like cells affects differentiation and local factor production. J Orthop Res. 2000;18(4):637–646. doi: 10.1002/jor.1100180417. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J, Ming LG, Ge BF, et al. Effects of 50 Hz sinusoidal electromagnetic fields of different intensities on proliferation, differentiation and mineralization potentials of rat osteoblasts. Bone. 2011;49(4):753–761. doi: 10.1016/j.bone.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 8.Wang Z, Clark CC, Brighton CT. Up-regulation of bone morphogenetic proteins in cultured murine bone cells with use of specific electric fields. J Bone Joint Surg Am. 2006;88(5):1053–1065. doi: 10.2106/JBJS.E.00443. [DOI] [PubMed] [Google Scholar]
- 9.Hartig M, Joos U, Wiesmann HP. Capacitively coupled electric fields accelerate proliferation of osteoblast-like primary cells and increase bone extracellular matrix formation in vitro. Eur Biophys J. 2000;29(7):499–506. doi: 10.1007/s002490000100. [DOI] [PubMed] [Google Scholar]
- 10.Veronesi F, Fini M, Sartori M, Parrilli A, Martini L, Tschon M (2018) Pulsed electromagnetic fields and platelet rich plasma alone and combined for the treatment of wear-mediated periprosthetic osteolysis: An in vivo study. Acta Biomater 77:106–115 [DOI] [PubMed]
- 11.Chang W, Chen LT, Sun JS, et al. Effect of pulse-burst electromagnetic field stimulation on osteoblast cell activities. Bioelectromagnetics. 2004;25(6):457–465. doi: 10.1002/bem.20016. [DOI] [PubMed] [Google Scholar]
- 12.Aaron RK, Boyan BD, Ciombor DM, et al. Stimulation of growth factor synthesis by electric and electromagnetic fields. Clin Orthop Relat Res. 2004;419:30–37. doi: 10.1097/00003086-200402000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Varani K, De Mattei M, Vincenzi F, et al. Characterization of adenosine receptors in bovine chondrocytes and fibroblast-like synoviocytes exposed to low frequency low energy pulsed electromagnetic fields. Osteoarthr Cartil. 2008;16:292–304. doi: 10.1016/j.joca.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 14.De Mattei M, Varani K, Masieri FF, et al. Adenosine analogs and electromagnetic fields inhibit prostaglandin E2 release in bovine synovial fibroblasts. Osteoarthr Cartil. 2009;17:252–262. doi: 10.1016/j.joca.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Ongaro A, Varani K, Masieri FF, et al. Electromagnetic fields (EMFs) and adenosine receptors modulate prostaglandin E2 and cytokine release in human osteoarthritic synovial fibroblasts. J Cell Physiol. 2012;227:2461–2469. doi: 10.1002/jcp.22981. [DOI] [PubMed] [Google Scholar]
- 16.Vincenzi F, Targa M, Corciulo C, et al. Pulsed electromagnetic fields increased the anti-inflammatory effect of A2A and A3 adenosine receptors in human T/C-28a2 chondrocytes and hFOB 1.19 osteoblasts. PLoS One. 2013;8(5):e65561. doi: 10.1371/journal.pone.0065561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Mattei M, Fini M, Setti S, et al. Proteoglycan synthesis in bovine articular cartilage explants exposed to different low-frequency low-energy pulsed electromagnetic fields. Osteoarthr Cartil. 2007;15(2):163–168. doi: 10.1016/j.joca.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Ongaro A, Pellati A, Masieri FF, et al. Chondroprotective effects of pulsed electromagnetic fields on human cartilage explants. Bioelectromagnetics. 2011;32:543–551. doi: 10.1002/bem.20663. [DOI] [PubMed] [Google Scholar]
- 19.De Mattei M, Pellati A, Pasello M, et al. Effects of physical stimulation with electromagnetic field and insulin growth factor-I treatment on proteoglycan synthesis of bovine articular cartilage. Osteoarthr Cartil. 2004;12(10):793–800. doi: 10.1016/j.joca.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 20.De Mattei M, Pasello M, Pellati A, et al. Effects of electromagnetic fields on proteoglycan metabolism of bovine articular cartilage explants. Connect Tissue Res. 2003;44:154–159. [PubMed] [Google Scholar]
- 21.Ongaro A, Pellati A, Setti S, et al. Electromagnetic fields counteract IL-1β activity during chondrogenesis of bovine mesenchymal stem cells. J Tissue Eng Regen Med. 2015;9(12):E229–E238. doi: 10.1002/term.1671. [DOI] [PubMed] [Google Scholar]
- 22.Bassett CA, Pawluk RJ, Pilla AA. Augmentation of bone repair by inductively coupled electromagnetic fields. Science. 1974;184:575–577. doi: 10.1126/science.184.4136.575. [DOI] [PubMed] [Google Scholar]
- 23.De Haas WG, Lazarovici MA, Morrison DM. The effect of low frequency magnetic fields on the healing of the osteotomized rabbit radius. Clin Orthop Relat Res. 1979;145:245–251. [PubMed] [Google Scholar]
- 24.Canè V, Botti P, Soana S. Pulsed magnetic fields improve osteoblast activity during the repair of an experimental osseous defect. J Orthop Res. 1993;11:664–670. doi: 10.1002/jor.1100110508. [DOI] [PubMed] [Google Scholar]
- 25.Midura RJ, Ibiwoye MO, Powell KA, et al. Pulsed electromagnetic field treatments enhance the healing of fibular osteotomies. J Orthop Res. 2005;23:1035–1046. doi: 10.1016/j.orthres.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 26.Brighton CT, Hozack WJ, Brager MD, et al. Fracture healing in the rabbit fibula when subjected to various capacitively coupled electrical fields. J Orthop Res. 1985;3:331–340. doi: 10.1002/jor.1100030310. [DOI] [PubMed] [Google Scholar]
- 27.Rijal KP, Kashimoto O, Sakurai M. Effect of capacitively coupled electric fields on an experimental model of delayed union of fracture. J Orthop Res. 1994;12:262–267. doi: 10.1002/jor.1100120216. [DOI] [PubMed] [Google Scholar]
- 28.Duarte LR. The stimulation of bone growth by ultrasound. Arch Orthop Trauma Surg. 1983;101:153–159. doi: 10.1007/BF00436764. [DOI] [PubMed] [Google Scholar]
- 29.Pilla AA, Mont MA, Nasser PR, et al. Noninvasive low-intensity pulsed ultrasound accelerates bone healing in the rabbit. J Orthop Trauma. 1990;4:246–253. doi: 10.1097/00005131-199004030-00002. [DOI] [PubMed] [Google Scholar]
- 30.Fini M, Torricelli P, Giavaresi G, et al. Effect of pulsed electromagnetic field stimulation on knee cartilage, subchondral and epyphiseal trabecular bone of aged Dunkin Hartley guinea pigs. Biomed Pharmacother. 2008;62(10):709–715. doi: 10.1016/j.biopha.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 31.Benazzo F, Cadossi M, Cavani F, et al. Cartilage repair with osteochondral autografts in sheep: effect of biophysical stimulation with pulsed electromagnetic fields. J Orthop Res. 2008;26(5):631–642. doi: 10.1002/jor.20530. [DOI] [PubMed] [Google Scholar]
- 32.Veronesi F, Cadossi M, Giavaresi G, et al. Pulsed electromagnetic fields combined with a collagenous scaffold and bone marrow concentrate enhance osteochondral regeneration: an in vivo study. BMC Musculoskelet Disord. 2015;16:233. doi: 10.1186/s12891-015-0683-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borsalino G, Bagnacani M, Bettati E, et al. Electrical stimulation of human femoral intertrochanteric osteotomies. Double-blind study. Clin Orthop Relat Res. 1988;237:256–263. [PubMed] [Google Scholar]
- 34.Mammi GI, Rocchi R, Cadossi R, et al. The electrical stimulation of tibial osteotomies. Double-blind study. Clin Orthop Relat Res. 1993;288:246–253. [PubMed] [Google Scholar]
- 35.Capanna R, Donati D, Masetti C, et al. Effect of electromagnetic fields on patients undergoing massive bone graft following bone tumor resection. A double blind study. Clin Orthop Relat Res. 1994;30:213–221. [PubMed] [Google Scholar]
- 36.Hinsenkamp M, Burny F, Donkerwolcke M, et al. Electromagnetic stimulation of fresh fractures treated with Hoffmann external fixation. Orthopedics. 1984;7:411–416. doi: 10.3928/0147-7447-19840301-08. [DOI] [PubMed] [Google Scholar]
- 37.Fontanesi G, Traina GC, Giancecchi F et al (1986) La lenta evoluzione del processo riparativo di una frattura puo’ essere prevenuta? GIOT XII(3):389–404
- 38.Faldini C, Cadossi M, Luciani D et al (2010) Electromagnetic bone growth stimulation in patients with femoral neck fractures treated with screws: prospective randomized double-blind study. Current Orthopaedic Practice 21(3):282–7
- 39.Benazzo F, Mosconi M, Beccarisi G, et al. Use of capacitive coupled electric fields in stress fractures in athletes. Clin Orthop Relat Res. 1995;310:145–149. [PubMed] [Google Scholar]
- 40.Heckman JD, Ryaby JP, McCabe J, et al. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone Joint Surg Am. 1994;76(1):26–34. doi: 10.2106/00004623-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Kristiansen TK, Ryaby JP, McCabe J, et al. Accelerated healing of distal radial fractures with the use of specific, low-intensity ultrasound. A multicenter, prospective, randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am. 1997;79(7):961–973. doi: 10.2106/00004623-199707000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Mayr E, Rudzki MM, Rudzki M, et al. Does low intensity, pulsed ultrasound speed healing of scaphoid fractures? Handchir Mikrochir Plast Chir. 2000;32(2):115–122. doi: 10.1055/s-2000-19253. [DOI] [PubMed] [Google Scholar]
- 43.Leung KS, Lee WS, Tsui HF, et al. Complex tibial fracture outcomes following treatment with low-intensity pulsed ultrasound. Ultrasound Med Biol. 2004;30(3):389–395. doi: 10.1016/j.ultrasmedbio.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 44.Simonis RB, Parnell EJ, Ray PS, et al. Electrical treatment of tibial non-union: a prospective, randomised, double-blind trial. Injury. 2003;34(5):357–362. doi: 10.1016/s0020-1383(02)00209-7. [DOI] [PubMed] [Google Scholar]
- 45.Traina GC, Fontanesi G, Costa P, et al. Effect of electromagnetic stimulation on patients suffering from nonunion. A retrospective study with a control group. J Bioelectricity. 1991;10:101–117. [Google Scholar]
- 46.Rispoli FP, Corolla FM, Mussner R. The use of low frequency pulsing electromagnetic fields in patients with painful hip prosthesis. J Bioelectricity. 1988;7:181. [Google Scholar]
- 47.Kennedy WF, Roberts CG, Zuege RC, et al. Use of pulsed electromagnetic fields in treatment of loosened cemented hip prostheses. A double-blind trial. Clin Orthop. 1993;286:198–205. [PubMed] [Google Scholar]
- 48.Dallari D, Fini M, Giavaresi G, et al. Effects of pulsed electromagnetic stimulation on patients undergoing hip revision prostheses: a randomized prospective double-blind study. Bioelectromagnetics. 2009;30(6):423–430. doi: 10.1002/bem.20492. [DOI] [PubMed] [Google Scholar]
- 49.Mooney V. A randomized double-blind prospective study of the efficacy of pulsed electromagnetic fields for interbody lumbar fusions. Spine. 1990;15(7):708–712. doi: 10.1097/00007632-199007000-00016. [DOI] [PubMed] [Google Scholar]
- 50.Linovitz RJ, Pathria M, Bernhardt M, et al. Combined magnetic fields accelerate and increase spine fusion: a double-blind, randomized, placebo controlled study. Spine (Phila Pa 1976) 2002;27(13):1383–1389. doi: 10.1097/00007632-200207010-00002. [DOI] [PubMed] [Google Scholar]
- 51.Goodwin CB, Brighton CT, Guyer RD, et al. A double-blind study of capacitively coupled electrical stimulation as an adjunct to lumbar spinal fusions. Spine. 1999;24(13):1349–1356. doi: 10.1097/00007632-199907010-00013. [DOI] [PubMed] [Google Scholar]
- 52.Rossini M, Viapiana O, Gatti D, et al. Capacitively coupled electric field for pain relief in patients with vertebral fractures and chronic pain. Clin Orthop Relat Res. 2010;468(3):735–740. doi: 10.1007/s11999-009-1088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Massari L (2011) Algorithm for employing physical forces in metabolic bone diseases. Aging Clin Exp Res 23(Suppl. to No. 2):52–53 [PubMed]
- 54.Piazzolla A, Solarino G, Bizzoca D, et al. Capacitive coupling electric fields in the treatment of vertebral compression fractures. J Biol Regul Homeost Agents. 2015;29(3):637–646. [PubMed] [Google Scholar]
- 55.Santori FS, Vitullo A, Montemurro G. Necrosi asettica della testa del femore: associazione tra intervento di svuotamento e innesti autoplastici e CEMP. In: Traina GC, Pipino F, Massari L, Molfetta L, Cadossi R, editors. Modulazione biofisica della osteogenesi mediante campi elettromagnetici pulsati. Lugo di Romagna (Ravenna): Walter Berti Editore; 1999. pp. 93–102. [Google Scholar]
- 56.Massari L, Fini M, Cadossi R, et al. Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):56–60. doi: 10.2106/JBJS.F.00536. [DOI] [PubMed] [Google Scholar]
- 57.Cebrián JL, Milano GL, Alberto F, et al. Role of electromagnetic stimulation in the treatment of osteonecrosis of the femoral head in early stages. J Biomed Sci Eng. 2014;7:252–257. [Google Scholar]
- 58.Zorzi C, Dall’Oca C, Cadossi R, et al. Effects of pulsed electromagnetic fields on patients’ recovery after arthroscopic surgery: prospective, randomized and double-blind study. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):830–834. doi: 10.1007/s00167-007-0298-8. [DOI] [PubMed] [Google Scholar]
- 59.Benazzo F, Zanon G, Pederzini L, et al. Effects of biophysical stimulation in patients undergoing arthroscopic reconstruction of anterior cruciate ligament: prospective, randomized and double blind study. Knee Surg Sports Traumatol Arthrosc. 2008;16(6):595–601. doi: 10.1007/s00167-008-0519-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cadossi M, Buda RE, Ramponi L, et al. Bone marrow-derived cells and biophysical stimulation for talar osteochondral lesions: a randomized controlled study. Foot Ankle Int. 2014;35(10):981–987. doi: 10.1177/1071100714539660. [DOI] [PubMed] [Google Scholar]
- 61.Collarile M, Sambri A, Lullini G, et al. Biophysical stimulation improves clinical results of matrix-assisted autologous chondrocyte implantation in the treatment of chondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1223–1229. doi: 10.1007/s00167-017-4605-8. [DOI] [PubMed] [Google Scholar]
- 62.Moretti B, Notarnicola A, Moretti L, et al. I-ONE therapy in patients undergoing total knee arthroplasty: a prospective, randomized and controlled study. BMC Musculoskelet Disord. 2012;13(1):88. doi: 10.1186/1471-2474-13-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Adravanti P, Nicoletti S, Setti S, et al. Effect of pulsed electromagnetic field therapy in patients undergoing total knee arthroplasty: a randomised controlled trial. Int Orthop. 2014;38(2):397–403. doi: 10.1007/s00264-013-2216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gobbi A, Lad D, Petrera M, et al. Symptomatic early osteoarthritis of the knee treated with pulsed electromagnetic fields: two-year follow-up. Cartilage. 2014;5(2):76–83. doi: 10.1177/1947603513515904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Iammarrone Servodio C, Cadossi M, Sambri A, et al. Is there a role of pulsed electromagnetic fields in management of patellofemoral pain syndrome? Randomized controlled study at one year follow-up. Bioelectromagnetics. 2016;37(2):81–88. doi: 10.1002/bem.21953. [DOI] [PubMed] [Google Scholar]
- 66.Marcheggiani Muccioli GM, Grassi A, Setti S, et al. Conservative treatment of spontaneous osteonecrosis of the knee in the early stage: pulsed electromagnetic fields therapy. Eur J Radiol. 2013;82(3):530–537. doi: 10.1016/j.ejrad.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 67.de Girolamo L, Viganò M, Galliera E, et al. In vitro functional response of human tendon cells to different dosages of low-frequency pulsed electromagnetic field. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3443–3453. doi: 10.1007/s00167-014-3143-x. [DOI] [PubMed] [Google Scholar]
- 68.Marmotti A, Peretti MP, Mattia S et al (2018) Pulsed electromagnetic fields improve tenogenic commitment of umbilical cord-derived mesenchymal stem cells: a potential strategy for tendon repair—an in vitro study. Stem Cells Int. Research Article ID 9048237, 10.1155/2018/9048237 [DOI] [PMC free article] [PubMed]
- 69.Capone F, Dileone M, Profice P, et al. Does exposure to extremely low frequency magnetic fields produce functional changes in human brain? J Neural Transm. 2009;116(3):257–265. doi: 10.1007/s00702-009-0184-2. [DOI] [PubMed] [Google Scholar]
- 70.Capone F, Liberti M, Apollonio F, et al. An open-label, one-arm, dose-escalation study to evaluate safety and tolerability of extremely low frequency magnetic fields in acute ischemic stroke. Sci Rep. 2017;7(1):12145. doi: 10.1038/s41598-017-12371-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuan J, Xin F, Jiang W. Underlying signaling pathways and therapeutic applications of pulsed electromagnetic fields in bone repair. Cell Physiol Biochem. 2018;46(4):1581–1594. doi: 10.1159/000489206. [DOI] [PubMed] [Google Scholar]
- 72.Huang AJ, Gemperli MP, Bergthold L, et al. Health plans’ coverage determinations for technology-based interventions: the case of electrical bone growth stimulation. Am J Manag Care. 2004;10(12):957–962. [PubMed] [Google Scholar]
- 73.Busse JW, Morton E, Lacchetti C, et al. Current management of tibial shaft fractures: a survey of 450 Canadian orthopedic trauma surgeons. Acta Orthop. 2008;79(5):689–694. doi: 10.1080/17453670810016722. [DOI] [PubMed] [Google Scholar]
- 74.Iwasa K, Reddi AH. Pulsed electromagnetic fields and tissue engineering of the joints. Tissue Eng Part B Rev. 2018;24(2):144–154. doi: 10.1089/ten.teb.2017.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]