Abstract
A temporal decline in human and dog sperm quality is thought to reflect a common environmental aetiology. This may reflect direct effects of seminal chemicals on sperm function and quality. Here we report the effects of diethylhexyl phthalate (DEHP) and polychlorinated biphenyl 153 (PCB153) on DNA fragmentation and motility in human and dog sperm. Human and dog semen was collected from registered donors (n = 9) and from stud dogs (n = 11) and incubated with PCB153 and DEHP, independently and combined, at 0x, 2x, 10x and 100x dog testis concentrations. A total of 16 treatments reflected a 4 × 4 factorial experimental design. Although exposure to DEHP and/or PCB153 alone increased DNA fragmentation and decreased motility, the scale of dose-related effects varied with the presence and relative concentrations of each chemical (DEHP.PCB interaction for: DNA fragmentation; human p < 0.001, dog p < 0.001; Motility; human p < 0.001, dog p < 0.05). In both human and dog sperm, progressive motility negatively correlated with DNA fragmentation regardless of chemical presence (Human: P < 0.0001, r = −0.36; dog P < 0.0001, r = −0.29). We conclude that DEHP and PCB153, at known tissue concentrations, induce similar effects on human and dog sperm supporting the contention of the dog as a sentinel species for human exposure.
Introduction
Over the last four decades, there has been increasing concern over declining human male reproductive health. Reduced sperm counts have been widely used as an index of male subfertility and meta-analytical studies indicate a 50% global reduction in quality from 1938 to 20111–3. Sperm morphology has also been reported to decrease over a period of 17 years in France with some geographical regional variation; Aquitaine and Midi-Pyrenees having the lowest morphology combined with the lowest concentrations4,5. These data are indicative of an environmental aetiology and, in support of this, epidemiological studies showing increased incidences of testicular cancer and malformations at birth have been linked to regions with reduced sperm counts6,7.
Temporal trends in human semen quality are paralleled by a similar trend in dogs that live in the human household, where sperm motility declined by 30% over a 26 year period8. In this latter study, all data was generated from a single laboratory using consistent techniques and thus did not suffer from changes in methodology and quality assurance over the time span encompassed in human meta-analytical studies9. These observations support the hypothesis that temporal trends in semen quality, both in the human and dog, are due to shared environmental factors and that the dog may be a sentinel for human exposure to such factors. Access to a controlled breeding population of assistance dogs that are routinely sampled for sperm quality provides a cost-effective means of sperm analyses without the stigma and social complications that accompany analogous human studies. Furthermore, there is considerable potential to extend these analyses to any individual or population of dogs. For example, although not investigated in the current study, this could be achieved by semen collection from the tail of the epididymis10 immediately after removal of dog testes at routine surgical neutering; a procedure that is performed on hundreds of thousands of dogs worldwide each year. In addition, semen collections from live dogs is a procedure that is tolerated by a majority of breeds11 unaccustomed to routine fertility monitoring and can therefore easily be carried out by a trained technician.
Declining sperm quality has been linked with the exposure to persistent anthropogenic chemicals, many of which exhibit endocrine disrupting activity6. Although the mechanisms underlying these putative effects are uncertain, historically, the period of fetal development has been highlighted as being particularly sensitive to chemicals with endocrine disrupting activity12. However, a number of studies have shown that environmental chemicals (ECs) are present in semen in a range of species, including the human, raising the possibility of a direct acute effect of chemicals on sperm13–15. In support of this theory, an elevated concentration of seminal bisphenol A (BPA) has been associated with infertility in men15,16 and elevated human seminal phthalate metabolites have been associated with reduced sperm counts17. In a separate study, the phthalates DEHP and di-n-butyl-phthalate (DBP) in human semen were reported to be inversely associated with motility and this was confirmed by the direct application of the same phthalates, at seminal concentrations, to sperm in vitro18. By contrast, PCB congeners 118, 126 and 153 were reported to have no negative effect on human sperm motility in vitro, both individually and in combination19. Similar findings have been reported in the dog where DEHP and PCB153, at concentrations detected in dog semen and testis, exhibited inhibitory and stimulatory effects respectively when tested on sperm motility in vitro8. In the same study, both DEHP and PCB153 were detected in a range of dry and wet dog foods indicative of a dietary source. Both DEHP and PCB153 are widely present in the environment and have been detected in tissues/fluids ranging from human breast milk to ovine liver. DEHP is a widely used plasticizer that leaches out into food and liquids and PCBs are lipophilic, and are therefore present in fatty foods20–22. Consequently, exposure occurs largely through the diet and these chemicals are deemed as risk factors for reproductive function23–25. In support of this, our own published study has shown that DEHP, PCB153 and other PCB congeners are present within both dry and wet dog food sources8 [DEHP: wet and dry food, 0.37 ± 0.10 and 0.20 ± 0.03 μg/g respectively; ∑PCBs: wet and dry food, 1.35 ± 0.5792 and 0.78 ± 0.223 μg/kg respectively; PCB153: wet and dry food, 0.39 ± 0.193 and 0.22 ± 0.11 μg/kg respectively].
Another parameter of ejaculate quality is the proportion of sperm that exhibit DNA fragmentation26. Environmental chemicals have been shown to induce both human and dog sperm DNA fragmentation8,27 and a commercial mixture of PCBs (Arochlor), administered to rats in vivo and added to sperm in vitro, also increased sperm DNA fragmentation28.
In total, these data suggest that environmental chemicals induce similar acute effects on human and dog sperm in vitro: measurement of sperm motility and DNA fragmentation are tried and tested measures of such chemical effects. Since sperm concentration would not alter during the period of in vitro culture and morphology is confounded by abnormality classification, partly due to swelling that may occur during culture and the generation of artefacts during processing, these parameters were not selected for testing acute chemical effects in vitro29,30. Notwithstanding, testing the effects of individual chemicals on sperm functional parameters does not represent “real-life” exposure to a mixture of chemicals, many of which exhibit synergistic, antagonistic or additive effects. Two chemicals known to be present in dog seminal plasma and testis were therefore selected and their effects tested both independently and in combination, on sperm motility and DNA fragmentation in both the human and dog.
Results
Chemical effects on percentage normal sperm motility in human and dog
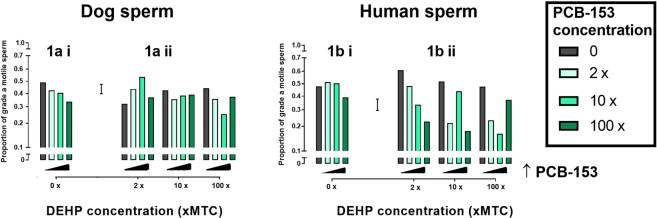
The analyses of both the human and the dog sperm motility data found the interaction terms between PCB and DEHP to be significant (human p < 0.001; dog p < 0.05). This indicates that the dose response to either chemical was not independent of the level of the other chemical present. Figure 1 illustrates the effects of PCB153 and DEHP, individually and combined, on dog and human sperm motility. In dog sperm, PCB153 in the absence of DEHP induced a dose-dependent inhibitory effect on sperm motility (Fig. 1ai). In the presence of DEHP at 2x and 10x mean testis concentration (MTC), no dose dependent inhibitory effect of PCB153 was observed. However, reduced motility was observed in the presence of 100x DEHP co-incubated with 2x and 10x PCB153 (Fig. 1aii).
Figure 1.
Effect of DEHP and PCB153 on dog and human sperm motility. Chemicals tested individually [ai,bi: PCB only; aii,bii: grey bars: DEHP only] and in combination [aii,bii]. Graphs display fixed concentrations of DEHP with increasing concentrations of PCB153 in dog [ai,aii: p < 0.01] and human [bi,bii: p < 0.001] sperm. Grade a motility: >25 μm/s Error bar = 1 Standard Error of Difference. MTC = Mean testis concentration.
In contrast to the dog, neither PCB153 nor DEHP, in the absence of the other chemical, influenced human sperm motility (Fig. 1bi,bii). However, in the presence of 2x DEHP, a dose dependent inhibitory effect in response to PCB153 was observed (Fig. 1bii). The inhibitory effect of PCB153 was broadly maintained in the presence of 10x and 100x DEHP with the exception of 10x PCB153/10x DEHP and 100x PCB153/100x DEHP, where no inhibition was observed (Fig. 1bii).
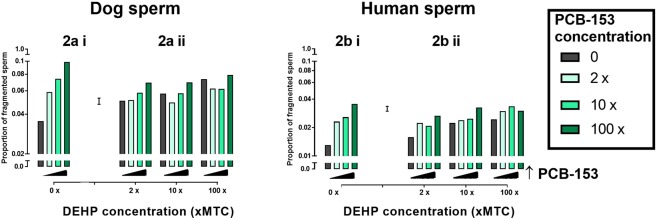
Chemical effects on sperm DNA integrity in human and dog
For both the human and dog DNA fragmentation data, significant (P < 0.001) PCB.DEHP interaction terms were found. Again, this indicates that the response of DNA integrity to one chemical is not independent of the presence or level of the other chemical. Figure 2 illustrates the effects of PCB153 and DEHP, individually and combined, on both dog and human sperm DNA fragmentation using the sperm chromatin dispersion assay. In the dog, PCB153 in the absence of DEHP induced a dose-dependent increase in sperm DNA fragmentation (Fig. 2ai). A similar dose-dependent increase in DNA fragmentation was observed in response to DEHP in the absence of PCB153 (Fig. 2aii). When PCB153 and DEHP were tested in combination, DNA fragmentation was still increased at higher concentrations of PCB153 but the dose-dependent response was blunted (Fig. 2aii). The response of human sperm to PCB153 and DEHP independently and combined, paralleled that observed in the dog. Figure 2b illustrates that human sperm incubated with PCB153 or DEHP in the absence of the other chemical, exhibited a dose-dependent increase in DNA fragmentation (Fig. 2bi,bii). In addition, DNA fragmentation was increased in response to both chemicals tested in combination although additive effects were not apparent.
Figure 2.
Effect of DEHP and PCB153 on dog and human sperm DNA fragmentation. Chemicals tested individually [ai,bi: PCB only; aii,bii: grey bars: DEHP only] and in combination [aii,bii]. Graphs display fixed concentrations of DEHP with increasing concentrations of PCB153 in dog [ai,aii: p ≤ 0.001] and human [bi,bii: p ≤ 0.001] sperm. Error bar = 1 Standard Error of difference between means. MTC = Mean testis concentration.
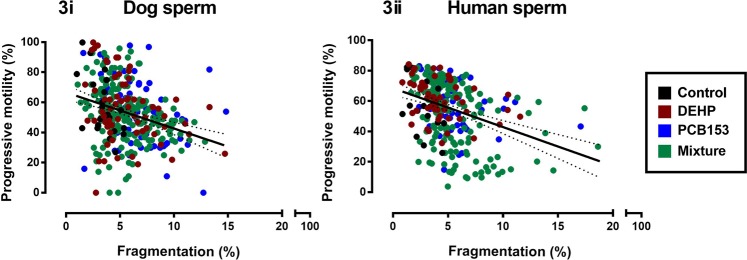
Sperm DNA fragmentation and motility correlations
Figure 3 illustrates the relationship between progressive motility and DNA fragmentation in the presence and absence of each chemical independently and combined. Despite chemical effects on sperm motility (Fig. 1) and DNA fragmentation (Fig. 2), the relationship between these two parameters remained the same regardless of the nature of the chemical exposure. All correlations were significant except the human control samples [Dog (Fig. 3i, n = 352): Control; p < 0.05, r = −0.527, n = 22; DEHP; p < 0.05, r = −0.2862, n = 66; PCB-153; p < 0.01, r = −0.3276, n = 66; Mixture; p < 0.0001, r = −0.2826, n = 198; vs Human (Fig. 3ii, n = 288): Control; p > 0.05, r = −0.4374, n = 18; DEHP; p < 0.05, r = −0.3118, n = 54; PCB-153; p < 0.05, r = −0.2994, n = 54; Mixture; p < 0.0001, r = −0.4037, n = 162].
Figure 3.
Correlation between progressive motility and DNA fragmentation in both dog and human sperm. Values from 32 sperm assessments (16 treatments, two time points). Each point represents a different sperm culture equating to a total n = 352 [dog] and n = 288 [human]. Colours denote culture media constituents to demonstrate spread: Control (black), DEHP (red), PCB153 (blue) and mixture (green). Dog (i, n = 352): Control; p < 0.05, r = −0.527, n = 22; DEHP; p < 0.05, r = −0.2862, n = 66; PCB153; p < 0.01, r = −0.3276, n = 66; Mixture; p < 0.0001, r = −0.2826, n = 198; vs Human (ii, n = 288): Control; p > 0.05, r = −0.4374, n = 18; DEHP; p < 0.05, r = −0.3118, n = 54; PCB153; p < 0.05, r = −0.2994, n = 54; Mixture; p < 0.0001, r = −0.4037, n = 162]. Confidence bands (95%) plotted for visual purposes only. Progressive motility based on WHO pre-2010 where sperm swimming grades a and b are combined: ≥5 µm/s.
Discussion
Data presented in this paper are significant because we conclusively demonstrate that a selected phthalate (DEHP) and PCB congener (PCB153), at concentrations relevant to environmental exposure, reduce dog sperm motility and increase DNA fragmentation in vitro. In the human, our data showing reduced motility and increased DNA fragmentation are indicative of similar sensitivities to these chemicals in both species. Furthermore, when the chemicals were combined and co-incubated with dog or human sperm, the overall impact on motility or DNA fragmentation was dependent on the concentration ratio. This is the first study to select two environmental chemicals and to test them at four concentrations in all possible combinations representative of those found in the male reproductive tract and fluids. In addition, a negative correlation between motility and DNA fragmentation, that incorporates chemical variables, is described in both species.
Our data on the sensitivity of sperm to short term chemical exposure support similar studies using a range of environmentally relevant chemical challenges in vitro. For example, DEHP, DBP and mono-n-butyl phthalate (MBP), are reported to reduce sperm motility in vitro when added at seminal concentrations measured in infertile men18,31. A mixture of PCBs are also reported to reduce sperm motility in both the human and pig32,33 and in the human, p,p’-dichloro-diphenyl-dichloro-ethylene (p,p’-DDE) has been shown to increase Ca2+ uptake by sperm in a mechanism that involves the CatSper channel34.
To minimise the effects of pre-exposure to chemicals present in ejaculates collected for culture, the current study used a concentration range that encompassed the reported variability in seminal concentrations and reduced pre-existing chemical concentrations by sperm processing and washing prior to culture. The subsequent comparison to controls, with no further chemical added, provided a means of testing chemical effects. Despite these steps, pre-exposure differences will inevitably exist between, and within, species. For example, in the current study, when DEHP is present at twice the concentration found in testis, dog sperm appears to be less sensitive to lower PCB concentrations than human sperm. In populations of men from Greenland, Sweden, Poland and the Ukraine, increased seminal PCB153 has been consistently associated with reduced sperm motility but not concentration or morphology35,36. In addition, sperm DNA fragmentation was positively associated with PCB153 in European populations but not in samples from Greenlandic men: an observation that likely reflects different pre-exposures.
In the current study, our intention was not to measure and equate chemical concentrations in each individual sample with sperm motility and fragmentation, but to use a concentration range previously established in the dog as a ballpark estimate of chemical concentrations in the male reproductive tract8. That is, concentrations found in the dog reproductive tract and seminal plasma, used as an indicator of those likely present in the human. In support of this contention, human seminal PCB (total) and DEHP concentrations reported in populations of fertile men [total PCB: up to 5.8 ng/ml, DEHP: mean of 0.61 μg/ml]37,38 are comparable to those detected in the dog [PCB: 0.26–13.2 ng/ml; DEHP: 0.75–37.5 μg/ml]8.
Notably, elevated concentrations of both chemicals have been linked with reduced human male fertility18. Semen PCB concentrations have been reported to be higher in a population of ‘infertile’ men (parameters stated as <20 million/ml or <25% progressive motility and/or <30% normal morphology)25. Further, a research group in China reported an association between increased urinary phthalate metabolites, reduced sperm count and increased sperm DNA damage14. Although the mechanism was not proven, the authors suggest that this likely reflects chemical effects on testicular Sertoli and germ cells as reported in animal studies39–42.
Although both DEHP and PCB153 have been reported to reduce sperm motility and increase sperm DNA fragmentation individually in the human8,18,37, they have not been assessed in combination, at environmentally relevant concentrations, as reported here. A limited number of studies have investigated some combinations of environmental chemicals for their effect on human sperm function32. Real-life exposure is to a complex mixture of chemicals that are likely to exhibit synergistic or antagonistic, as well as additive effects, on sperm. Mixtures of endocrine disrupting chemicals have been shown to cooperatively increase Ca2+ concentrations in sperm through the activation of the principle calcium channel CatSper43.
In the current study, the mechanisms that underlie the concentration ratio-dependent effects of the two chemicals combined remain uncertain. PCBs and DEHP are considered to be pro-estrogenic and anti-androgenic respectively raising the possibility that a change in concentration ratio may alter the relative activation of sperm estrogen or androgen receptors44,45. Indeed, in a population of ‘infertile’ men (parameters stated as sperm count < 20 × 106, motility < 50%, morphology < 14% normal) androgen receptor expression is reported to positively correlate with sperm motility46 and PCBs are reported to affect sperm concentration and motility relative to the number of CAG repeats in the androgen receptor gene47. This may account for PCB influences on motility even in the presence of DEHP. Estrogenic compounds have also been reported to reduce human sperm motility in vitro via an induction in redox activity and this mechanism has also been linked to the induction of DNA fragmentation by 2-hydroxy estradiol48.
The greater consistency of chemical effects on human and dog sperm DNA fragmentation compared to motility is interesting and emphasises the importance of looking at more than one sperm functional/viability parameter when assessing environmental effects. It is important to note however that despite this subtle difference, the two sperm parameters were highly correlated in both species and remained so in the presence of the chemicals independently and combined. This is an important observation since it has been reported that human male infertility is associated with increased levels of sperm DNA damage and that sperm motility defects are highest in samples with increased DNA fragmentation49,50. This raises the possibility that there may be a similar relationship between sperm DNA fragmentation, motility and fertility in the dog.
In conclusion, we have demonstrated that the use of low dose tissue relevant concentrations of DEHP and PCB153, independently and in combination, negatively impact on sperm motility and DNA fragmentation in samples obtained from humans and dogs. Since these effects are broadly similar in both species, this raises the possibility that the environmental impact of chemicals in the dog may provide a means of investigating pollutant effects on mammalian fertility in a species in which external influences, such as diet, are better controlled than in an equivalent human study.
Methods
Ethical Approval
Human
Semen donations were obtained from anonymous HFEA registered donors (n = 9) attending the fertility unit at Nottingham University Hospitals. Donors provided informed consent for the use of samples in this research project ensuring ‘General Data Protection Regulation’ compliance. Each donor was initially screened following HFEA and British Fertility Society protocols51. No samples from fertility patients were used and all donors completed HFEA consent forms. Ethical approval was obtained from the School of Veterinary Medicine Ethical Review Committee [Reference 1511,150723]. The HFEA consent forms completed by donors and ethical approval documents were also approved by the Chair of the Ethical Review Committee of the Faculty of Medicine and Health Sciences, University of Nottingham. In accordance with the Royal College of Pathologists guidance on the use of pathological specimens [https://www.rcpath.org/resourceLibrary/the-retention-and-storage-of-pathological-records-and-specimens-5th-edition-.html], no further ethical approval was required.
Dog
Semen was collected as part of routine reproductive examination of stud dogs subject to owner consent with full GDPR compliance. Due to dog sperm being collected as part of routine reproductive health checks, the economical outlay associated with sample collection was minimised. The dogs resided in the same region of the UK and lived in the modern household with owners briefed on use of controlled diet and exercise regimes. All semen collections were performed in accordance with relevant guidelines and regulations and the collection protocol was approved by the School of Veterinary Medicine Ethical Review Committee (Refs: 208 101012, 513 120117 and 1097 140227).
Human sperm collection and preparation
Samples were liquefied for 20 minutes at room temperature prior to semen preparation. Ejaculate underwent density gradient centrifugation using a Universal 320 R Hettich centrifuge (DJB Labcare, Newport Pagnell, UK) at 25 °C. Briefly, one millilitre of 40% isotonic density gradient was loaded onto one millilitre of 80% isotonic medium [PureSperm 40/80, Nidacon, Sweden]. Two millilitres of liquefied semen were loaded onto both isotonic mediums and reagents centrifuged at 300 × g for 22 minutes. On completion, the sperm rich pellet was re-suspended using 1.5 ml PureSperm wash (pH range of 7.3–8.5; osmolality: 290–300 mOsm/kg H2O, Nidacon, Sweden).
Dog sperm collection
Ejaculate was collected from stud dogs (n = 11) by routine digital manipulation. The sperm rich fraction (fraction 2) was collected into sterile plastic 15 millilitre Greiner centrifuge tubes [Sigma-Aldrich, Dorset, UK]. INRA extending medium [INRA, Nouzilly, France] was added to sperm at a 2:1 ratio to aid sperm survival.
Chemical preparation
The two chemicals selected for co-culture with sperm were diethylhexyl phthalate (DEHP) and polychlorinated biphenyl congener 153 (PCB153) and concentrations were calculated relative to those present in dog testicular tissue8. The rationale for this was (1) dog testis concentrations of both chemicals have been established and standardised in our previous study and are reflective of exposure of the male reproductive tract8 (2) dog and human semen PCB concentrations are variable but generally higher than testis and in range of the concentrations tested in vitro8,25,52 (3) although dog semen DEHP concentrations have not been determined, due to the large amount of dry material required, reported human DEHP concentrations are in range of established dog testis measurements14,18,53. On this basis, dog testis concentrations were used as a standardised measure of environmental exposure relevant to both species. DEHP (CAS no: 117-81-7) and PCB153 (CAS no: 35065-27-1) [Sigma-Aldrich, Dorset, U.K.] were dissolved in 100% dimethylsulphoxide (DMSO) and diluted with PBS to 4x, 20x and 200x mean testis concentration containing 0.02% DMSO. Chemical preparations were co-incubated with sperm at a 1:1 ratio with a final exposure concentration of 2x, 10x and 100x mean testis concentration. Sperm were incubated with each chemical at each concentration individually and with a mixture of the two chemicals in all 16 combination ratios (Table 1). Acute treatment effects were assessed at 10 minutes and 3 hours and control incubations carried out with 0.01% DMSO only.
Table 1.
Chemical concentrations present in culture media. aMTC = mean testis concentration.
| Culture | DEHP culture concentration (µg/ml) [multiple of MTCa] | PCB153 culture concentration (ng/ml) [multiple of MTCa] |
|---|---|---|
| Control | 0.00 | 0.00 |
| DEHP | 0.75 [2x] | — |
| 3.75 [10x] | — | |
| 37.53 [100x] | — | |
| PCB153 | — | 0.26 [2x] |
| — | 1.32 [10x] | |
| — | 13.22 [100x] | |
| Mixture | 0.75 [2x] | 0.26 [2x] |
| 0.75 [2x] | 1.32 [10x] | |
| 0.75 [2x] | 13.22 [100x] | |
| 3.75 [10x] | 0.26 [2x] | |
| 3.75 [10x] | 1.32 [10x] | |
| 3.75 [10x] | 13.22 [100x] | |
| 37.53 [100x] | 0.26 [2x] | |
| 37.53 [100x] | 1.32 [10x] | |
| 37.53 [100x] | 13.22 [100x] |
Motility assessment
Sperm motility was assessed using Computer Assisted Sperm Analysis (CASA) software. Sperm were acclimatised for two minutes on a 37 °C stage prior to assessment. Five µl of sperm, irrespective of species, were pipetted into a specialised 20 µl cellvision glass slide counting chamber (Code CV1020-2CV; CellVision, the Netherlands). A minimum of 200 sperm were assessed for each treatment. For human sperm, motility was tracked by use of the diagnostic software ‘SAMi’ (Procreative Diagnostics Ltd, Staffordshire, UK) and an Olympus BH2 Microscope [KeyMed (Medical and Industrial Equipment) Ltd, Essex, UK]. Dog sperm motility was assessed using the Hobson’s CASA tracking system (Hobson’s tracking systems Ltd., Sheffield, UK) and viewed using a negative-high phase contrast objective (x20) on an Olympus BH2 microscope fitted with a camera ocular. For both species, sperm motility was assessed according to WHO 199954 where grade a motility was classified as ≥ 25 µm/s and progressive motility ≥ 5 µm/s (grades a & b combined).
DNA fragmentation
Sperm DNA fragmentation was quantified by defragmentation index (sDFI %) measured using the sperm chromatin dispersion assay55. Sperm were assessed based on the size of the halos, indicative of sperm that exhibited nuclei with non-fragmented DNA. Sperm with denatured or fragmented DNA were identified by the absence of a halo, or a halo that was exceedingly small. Briefly, equal volumes of intact, unfixed sperm and 1% agarose solution were combined. Fifteen microliter aliquots of sperm-agarose suspensions were pipetted onto agarose pre-coated poly-L-lysine slides (CAS: P4981; ThermoFisher Scientific Ltd. UK), covered with a 22 mm × 22 mm cover-slip, and placed in a 4 °C environment for five minutes to fix the sample. After an acid treatment (0.08 M HCl) of seven minutes, sperm were incubated in a lysing reagent (0.8 M DTT, 0.4 M Tris, 2 M NaCl, 1% triton-X) for 20 minutes. Slides were then submerged in dH2O for a period of five minutes followed by dehydration through a series of ethanol solutions (70%, 90% and 100% respectively). Visualisation was obtained using Diff-Quick staining reagents (eosinophilic and basophilic stains; CAS 9990700, ThermoFisher Scientific Ltd, Paisley, UK) and analysis undertaken using oil immersion, at 1000x magnification [Leica DM 5000 B microscope; Leica Microsystems, Milton Keynes, UK]. A minimum of 200 sperm were assessed for each treatment. Positive controls were incubated with 300 µm H2O2 before denaturation and negative controls by omission of the denaturation step. To determine the defragmentation index, the number of fragmented sperm was divided by the total number of sperm counted. This provided a value for the proportion of sperm that were fragmented. This proportion was then plotted on the logit scale.
Experimental design and Statistical analysis
For both the human and dog experiments, sperm samples were treated with PCB153 at one of four concentrations in combination with DEHP, also at one of four concentrations. The concentrations used for both chemicals corresponded to 0x, 2x, 10x and 100x the baseline concentration measured from dog testes. Thus there were 16 possible combinations of PCB153 and DEHP. Each combination was randomly allocated to one of 16 separate sub-samples of sperm, from each replicate donor.
Statistical analysis was undertaken using GenStat 17th edition (VSN International Ltd, Hempstead, UK). The proportions out of known numbers of sperm that had a particular characteristic were analysed as grouped binary data by fitting a generalised linear mixed model with a logit link function, assuming a binomial error distribution. The fixed effects included in the statistical model were PCB, DEHP and the PCB.DEHP interaction term. Another fixed effect, TIME, and its interaction terms were included when two repeated samples from the same tube were measured three hours apart. The random effects were donor and culture-tube within donor.
The statistical significance of a fixed effect was tested using an F-Ratio test. The analysis output provided predicted mean proportions and standard errors of difference between means which were graphically represented on a logit scale. Logit values were converted back into proportions and graphically plotted [GraphPad Prism 7.0, GraphPad Ltd, California, USA]. A single error bar on each figure represents the standard error of the difference between means. Where correlations were investigated, data was assumed to be non-normally distributed and a Spearman’s rank correlation analysis was undertaken to provide correlation coefficients between motility and DNA fragmentation.
Acknowledgements
We thank Karen Pooley for the management of the human donors attending the Fertility Unit at Nottingham University Hospital and for expert technical advice and assistance. We also thank Natasha White for the collection of ejaculates from a population of assistance dogs. The work was supported by University of Nottingham internal funds.
Author Contributions
R.G.L. and R.N.S. conceived of and designed the study. M.T. managed the human donors and collection of human semen samples and G.C.W.E. managed the collection of canine samples. All authors provided academic input into the paper. R.N.S. carried out the computer assisted sperm analysis, chromatin dispersion assay and subsequent analysis. J.C. provided expert statistical advice and contributed to the analysis. R.G.L. and R.N.S. wrote the paper.
Data Availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305:609–613. doi: 10.1136/bmj.305.6854.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swan SH, Elkin EP, Fenster L. The question of declining sperm density revisited: an analysis of 101 studies published 1934–1996. Environ. Health Perspect. 2000;108:961–966. doi: 10.1289/ehp.00108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levine H, et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum. Reprod. Update. 2017;23:646–659. doi: 10.1093/humupd/dmx022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rolland, M., Le Moal, J., Wagner, V., Royere, D. & De Mouzon, J. Decline in semen concentration and morphology in a sample of 26,609 men close to general population between 1989 and 2005 in France. Hum. Reprod. 28, 462–470 (2013). [DOI] [PMC free article] [PubMed]
- 5.Le Moal J, et al. Semen quality trends in French regions are consistent with a global change in environmental exposure. Reproduction. 2014;147:567–574. doi: 10.1530/REP-13-0499. [DOI] [PubMed] [Google Scholar]
- 6.Bay K, Asklund C, Skakkebaek NE, Andersson A-M. Testicular dysgenesis syndrome: possible role of endocrine disrupters. Best Pract. Res. Clin. Endocrinol. Metab. 2006;20:77–90. doi: 10.1016/j.beem.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Skakkebaek NE. Sperm counts, testicular cancers, and the environment. BMJ (Clinical research ed.) 2017;359:j4517. doi: 10.1136/bmj.j4517. [DOI] [PubMed] [Google Scholar]
- 8.Lea RG, et al. Environmental chemicals impact dog semen quality in vitro and may be associated with a temporal decline in sperm motility and increased cryptorchidism. Sci. Rep. 2016;6:31281. doi: 10.1038/srep31281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pacey AA. Are sperm counts declining? Or did we just change our spectacles? Asian J. Androl. 2013;15:187–190. doi: 10.1038/aja.2012.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ponglowhapan S, Chatdarong K, Sirivaidyapong S, Lohachit C. Freezing of epididymal spermatozoa from dogs after cool storage for 2 or 4 days. Theriogenology. 2006;66:1633–1636. doi: 10.1016/j.theriogenology.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Hermansson U, Linde Forsberg C. Freezing of stored, chilled dog spermatozoa. Theriogenology. 2006;65:584–593. doi: 10.1016/j.theriogenology.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Lea, R. G. et al. Endocrine disruptors and ovine reproductive development. In Reproduction in Domestic Ruminants Vol.VIII (eds Juengel, J. et al.) 209–227 (Context Products Ltd., UK, 2014).
- 13.Kamarianos A, Karamanlis X, Theodosiadou E, Goulas P, Smokovitis A. The presence of environmental pollutants in the semen of farm animals (bull, ram, goat, and boar) Reprod. Toxicol. 2003;17:439–445. doi: 10.1016/S0890-6238(03)00031-5. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y-X, et al. Phthalate exposure and human semen quality: Results from an infertility clinic in China. Environ. Res. 2015;142:1–9. doi: 10.1016/j.envres.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 15.La Rocca C, et al. Exposure to Endocrine Disruptors and Nuclear Receptors Gene Expression in Infertile and Fertile Men from Italian Areas with Different Environmental Features. Int. J. Environ. Res. Public Health. 2015;12:12426–12445. doi: 10.3390/ijerph121012426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vitku J, et al. Difflerences in bisphenol A and estrogen levels in the plasma and seminal plasma of men with different degrees of infertility. Physiol. Res. 2015;64(Suppl 2):S303–11. doi: 10.33549/physiolres.933090. [DOI] [PubMed] [Google Scholar]
- 17.Chang W-H, Wu M-H, Pan H-A, Guo P-L, Lee C-C. Semen quality and insulin-like factor 3: Associations with urinary and seminal levels of phthalate metabolites in adult males. Chemosphere. 2017;173:594–602. doi: 10.1016/j.chemosphere.2017.01.056. [DOI] [PubMed] [Google Scholar]
- 18.Pant N, et al. Environmental and experimental exposure of phthalate esters: the toxicological consequence on human sperm. Hum. Exp. Toxicol. 2011;30:507–514. doi: 10.1177/0960327110374205. [DOI] [PubMed] [Google Scholar]
- 19.Pflieger-Bruss S, et al. Effects of single non-ortho, mono-ortho, and di-ortho chlorinated biphenyls on human sperm functions in vitro. Reprod. Toxicol. 2006;21:280–284. doi: 10.1016/j.reprotox.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Kastner J, Cooper DG, Maric M, Dodd P, Yargeau V. Aqueous leaching of di-2-ethylhexyl phthalate and ‘green’ plasticizers from poly(vinyl chloride) Sci. Total Environ. 2012;432:357–364. doi: 10.1016/j.scitotenv.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 21.Erythropel HC, Maric M, Nicell JA, Leask RL, Yargeau V. Leaching of the plasticizer di(2-ethylhexyl)phthalate (DEHP) from plastic containers and the question of human exposure. Appl. Microbiol. Biotechnol. 2014;98:9967–9981. doi: 10.1007/s00253-014-6183-8. [DOI] [PubMed] [Google Scholar]
- 22.Faroon O, Ruiz P. Polychlorinated biphenyls: New evidence from the last decade. Toxicol. Ind. Health. 2016;32:1825–1847. doi: 10.1177/0748233715587849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pocar P, et al. Exposure to di(2-ethyl-hexyl) phthalate (DEHP) in utero and during lactation causes long-term pituitary-gonadal axis disruption in male and female mouse offspring. Endocrinology. 2012;153:937–948. doi: 10.1210/en.2011-1450. [DOI] [PubMed] [Google Scholar]
- 24.Oskam IC, et al. Effects of long-term maternal exposure to low doses of PCB126 and PCB153 on the reproductive system and related hormones of young male goats. Reproduction. 2005;130:731–742. doi: 10.1530/rep.1.00690. [DOI] [PubMed] [Google Scholar]
- 25.Rozati R, Reddy PP, Reddanna P, Mujtaba R. Role of environmental estrogens in the deterioration of male factor fertility. Fertil. Steril. 2002;78:1187–1194. doi: 10.1016/S0015-0282(02)04389-3. [DOI] [PubMed] [Google Scholar]
- 26.Rex AS, Aagaard J, Fedder J. DNA fragmentation in spermatozoa: a historical review. Andrology. 2017;5:622–630. doi: 10.1111/andr.12381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evenson DP, Wixon R. Environmental toxicants cause sperm DNA fragmentation as detected by the Sperm Chromatin Structure Assay (SCSA) Toxicol. Appl. Pharmacol. 2005;207:532–537. doi: 10.1016/j.taap.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Aly HAA. Aroclor 1254 induced oxidative stress and mitochondria mediated apoptosis in adult rat sperm in vitro. Environ. Toxicol. Pharmacol. 2013;36:274–283. doi: 10.1016/j.etap.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Mortimer D, Menkveld R. Sperm morphology assessment—historical perspectives and current opinions. J. Androl. 2001;22:192–205. [PubMed] [Google Scholar]
- 30.Boersma A, Rasshofer R, Stolla R. Influence of sample preparation, staining procedure and analysis conditions on bull sperm head morphometry using the morphology analyser integrated visual optical system. Reprod. Domest. Anim. 2001;36:222–229. doi: 10.1046/j.1439-0531.2001.00291.x. [DOI] [PubMed] [Google Scholar]
- 31.Xie F, et al. Effects of two environmental endocrine disruptors di-n-butyl phthalate (DBP) and mono-n-butyl phthalate (MBP) on human sperm functions in vitro. Reprod. Toxicol. 2019;83:1–7. doi: 10.1016/j.reprotox.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Jiang L-G, et al. Toxic effects of polychlorinated biphenyls (Aroclor 1254) on human sperm motility. Asian J. Androl. 2017;19:561–566. doi: 10.4103/1008-682X.186876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campagna C, Guillemette C, Ayotte P, Bailey JL. Effects of an environmentally relevant organochlorine mixture and a metabolized extract of this mixture on porcine sperm parameters in vitro. J. Androl. 2009;30:317–324. doi: 10.2164/jandrol.108.006478. [DOI] [PubMed] [Google Scholar]
- 34.Tavares RS, Escada-Rebelo S, Correia M, Mota PC, Ramalho-Santos J. The non-genomic effects of endocrine-disrupting chemicals on mammalian sperm. Reproduction. 2016;151:R1–R13. doi: 10.1530/REP-15-0355. [DOI] [PubMed] [Google Scholar]
- 35.Toft G. Persistent organochlorine pollutants and human reproductive health. Dan. Med. J. 2014;61:B4967. [PubMed] [Google Scholar]
- 36.Toft G, et al. Semen quality and exposure to persistent organochlorine pollutants. Epidemiology. 2006;17:450–458. doi: 10.1097/01.ede.0000221769.41028.d2. [DOI] [PubMed] [Google Scholar]
- 37.Bush B, Bennett AH, Snow JT. Polychlorobiphenyl congeners, p,p’-DDE, and sperm function in humans. Arch. Environ. Contam. Toxicol. 1986;15:333–341. doi: 10.1007/BF01066399. [DOI] [PubMed] [Google Scholar]
- 38.Han SW, et al. An exposure assessment of di-(2-ethylhexyl) phthalate (DEHP) and di-n-butyl phthalate (DBP) in human semen. J. Toxicol. Environ. Heal. Part A. 2009;72:1463–1469. doi: 10.1080/15287390903212972. [DOI] [PubMed] [Google Scholar]
- 39.Jones S, Boisvert A, Francois S, Zhang L, Culty M. In utero exposure to di-(2-ethylhexyl) phthalate induces testicular effects in neonatal rats that are antagonized by genistein cotreatment. Biol. Reprod. 2015;93(92):1–14. doi: 10.1095/biolreprod.115.129098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richburg JH, Boekelheide K. Mono-(2-ethylhexyl) phthalate rapidly alters both Sertoli cell vimentin filaments and germ cell apoptosis in young rat testes. Toxicol. Appl. Pharmacol. 1996;137:42–50. doi: 10.1006/taap.1996.0055. [DOI] [PubMed] [Google Scholar]
- 41.Ungewitter E, et al. From the Cover: Teratogenic Effects of in Utero Exposure to Di-(2-Ethylhexyl)-Phthalate (DEHP) in B6:129S4 Mice. Toxicol. Sci. 2017;157:8–19. doi: 10.1093/toxsci/kfx019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang T, et al. Melatonin protects prepuberal testis from deleterious effects of bisphenol A or diethylhexyl phthalate by preserving H3K9 methylation. J. Pineal Res. 2018;65:e12497. doi: 10.1111/jpi.12497. [DOI] [PubMed] [Google Scholar]
- 43.Schiffer C, et al. Direct action of endocrine disrupting chemicals on human sperm. EMBO Rep. 2014;15:758–765. doi: 10.15252/embr.201438869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aquila S, et al. Estrogen receptor (ER)alpha and ER beta are both expressed in human ejaculated spermatozoa: evidence of their direct interaction with phosphatidylinositol-3-OH kinase/Akt pathway. J. Clin. Endocrinol. Metab. 2004;89:1443–1451. doi: 10.1210/jc.2003-031681. [DOI] [PubMed] [Google Scholar]
- 45.Aquila S, et al. Human sperm express a functional androgen receptor: effects on PI3K/AKT pathway. Hum. Reprod. 2007;22:2594–2605. doi: 10.1093/humrep/dem243. [DOI] [PubMed] [Google Scholar]
- 46.Zalata AA, et al. Androgen receptor expression relationship with semen variables in infertile men with varicocele. J. Urol. 2013;189:2243–2247. doi: 10.1016/j.juro.2012.11.112. [DOI] [PubMed] [Google Scholar]
- 47.Giwercman A, Rylander L, Lundberg Giwercman Y. Influence of endocrine disruptors on human male fertility. Reprod. Biomed. Online. 2007;15:633–642. doi: 10.1016/S1472-6483(10)60530-5. [DOI] [PubMed] [Google Scholar]
- 48.Bennetts LE, et al. Impact of estrogenic compounds on DNA integrity in human spermatozoa: evidence for cross-linking and redox cycling activities. Mutat. Res. 2008;641:1–11. doi: 10.1016/j.mrfmmm.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 49.Velez de la Calle JF, et al. Sperm deoxyribonucleic acid fragmentation as assessed by the sperm chromatin dispersion test in assisted reproductive technology programs: results of a large prospective multicenter study. Fertil. Steril. 2008;90:1792–1799. doi: 10.1016/j.fertnstert.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 50.Belloc S, et al. Sperm deoxyribonucleic acid damage in normozoospermic men is related to age and sperm progressive motility. Fertil. Steril. 2014;101:1588–1593. doi: 10.1016/j.fertnstert.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 51.Hamilton M, et al. Working Party on Sperm Donation Services in the UK. Hum. Fertil. 2008;11:147–158. doi: 10.1080/14647270802170174. [DOI] [PubMed] [Google Scholar]
- 52.Dallinga JW, et al. Decreased human semen quality and organochlorine compounds in blood. Hum. Reprod. 2002;17:1973–1979. doi: 10.1093/humrep/17.8.1973. [DOI] [PubMed] [Google Scholar]
- 53.Zhang Y-H, Zheng L-X, Chen B-H. Phthalate exposure and human semen quality in Shanghai: a cross-sectional study. Biomed. Environ. Sci. 2006;19:205–209. [PubMed] [Google Scholar]
- 54.WHO. Laboratory Manual for the examination of human semen and sperm – cervical mucus interaction. (Cambridge University Press, Cambridge, 1999).
- 55.Fernandez JL, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil. Steril. 2005;84:833–842. doi: 10.1016/j.fertnstert.2004.11.089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.