Abstract
Atopic dermatitis (AD) is the most common chronic inflammatory skin disease. Genetic predisposition, epidermal barrier disruption, and dysregulation of the immune system are some of the critical components of AD. An impaired skin barrier may be the initial step in the development of the atopic march as well as AD, which leads to further skin inflammation and allergic sensitization. Type 2 cytokines as well as interleukin 17 and interleukin 22 contribute to skin barrier dysfunction and the development of AD. New insights into the pathophysiology of AD have focused on epidermal lipid profiles, neuroimmune interactions, and microbial dysbiosis. Newer therapeutic strategies focus on improving skin barrier function and targeting polarized immune pathways found in AD. Further understanding of AD pathophysiology will allow us to achieve a more precision medicine approach to the prevention and the treatment of AD.
Keywords: Atopic dermatitis, epidermal barrier, immune dysregulation, microbiome, skin lipid
Atopic dermatitis (AD) is the most common chronic inflammatory skin disease.1 The U.S. prevalence of AD was reported to be 11.3–12.7% and 6.9–7.6% in children and in adults, respectively.2 The Hanifin and Rajka criteria and the American Academy of Dermatology Consensus Criteria are useful diagnostic tools based on features of AD.3,4 AD severity can be assessed by using validated methods such as Scoring Atopic Dermatitis or the Eczema Area and Severity Index.5
Although the pathophysiology of AD is not completely understood, numerous studies demonstrated that skin barrier dysfunction and immune dysregulation contribute to the pathobiology of AD.6–8 The epidermis plays a crucial role as a physical and functional barrier, and skin barrier defects are the most significant pathologic findings in AD skin.1,9,10 Filaggrin (FLG), transglutaminases, keratins, and intercellular proteins are key proteins responsible for epidermal function. Defects in these proteins facilitate allergen and microbial penetration into the skin.9–11
Skin barrier dysfunction has been considered to be the first step in the development of atopic march as well as AD.7,12 However, it is also now evident that immune dysregulation, including the activation of type 2 immune responses, results in impairment of the epidermal barrier.13–16 Recently, new insights into the pathophysiology of the development of AD focused on an important role of abnormalities in epidermal lipid layer as well as neuroimmune interactions and microbial dysbiosis.17–20 These factors have been used to develop novel therapeutic and preventative strategies of AD. This review addressed recent insights into the pathophysiologic mechanism of AD and the clinical application of these factors for improved treatment and prevention of AD. This work was supported by National Institutes of Health (grant AR41256). J. Kim and B. Eui Kim contributed equally to the article.
GENETICS
The filaggrin (FLG) gene is located on chromosome 1q2, and encodes FLG (filaggrin protein), which is a major structural protein in the stratum corneum (SC).21 Pro-FLG polymers are proteolytically cleaved and dephosphorylated into FLG monomers, which are associated with the aggregation of keratin filaments and the formation of SC.13 The generation of FLG degradation products, urocanic acid and pyrrolidine carboxylic acid, contributes to SC hydration and acidic pH of skin.14 It is well known that FLG null mutations impair skin barrier function and increase the risk of AD.21,22 FLG mutations, particularly homozygous mutations, are associated with an increased risk of severe AD with earlier onset, longer persistence, and skin infections.8,22,23 Approximately 10% of European populations are heterozygous carriers of FLG mutations, which results in a 50% reduction in expressed protein.22 However, the pathophysiology of AD goes far beyond FLG mutations. For example, Japanese and Korean patients have a lower frequency of FLG mutations than do patients in Western populations.13,24 Furthermore, ∼40% of subjects with FLG-null alleles do not show characteristics of AD, and most of the patients with AD and with FLG mutations eventually outgrow the disease.25
Polymorphisms of various immune pathway genes are associated with an increased risk of AD through alternations in the T-helper (Th) type 2 signaling pathway.21,26 Upregulation of interleukin (IL) 4 and IL-13 lowers FLG expression, which leads to skin barrier defects.27,28 A gain of functional polymorphisms of type 2 cytokine receptors (IL-4R and IL-13R) are also implicated in AD pathogenesis.28,29 Other immune-related genes that contribute to the development of AD include IL-31, IL-33, signal transducer and activator of transcription (STAT) 6, thymic stromal lymphopoietin (TSLP) and its receptors (IL-7R and TSLPR), interferon regulatory factor 2, Toll-like receptor 2, and high-affinity IgE receptor (FcεRI) α gene in specific populations.21,26,30–33 Additionally, recent studies demonstrated that vitamin D receptor polymorphisms and cytochrome P450 family 27 subfamily A member 1 (CYP27A1) variant are associated with AD.34,35 CYP27A1 is known to be involved in the metabolism of vitamin D3, which plays an essential role in immune modulation.34
Epigenetic mechanisms are heritable and can regulate gene expression without changing the DNA sequence.13 There is increasing evidence that demonstrates that environmental exposures induce epigenetic changes and AD through DNA modification and micro-RNA–mediated posttranscriptional regulation.26,36 A recent study provided evidence for the importance of DNA methylation and showed the relationship between umbilical cord blood methylation at 5′-C-phosphate-G-3′ sites of IL-4R and the development of AD at 1 year of age.37 DNA methylation in one adjacent CpG site of FLG was reported to have a significant interaction with FLG sequence variants and association with the increased risk of eczema,38 whereas another study, which used buccal cells, could not show the relationship between methylation of the FLG promoter and gene expression and allergic diseases.39 Furthermore, hypomethylation of TSLP and FcεRI γ promoters contributes to gene overexpression in patients with AD.26
IMMUNE DYSREGULATION
Previous studies showed that type 2 immune cytokines, e.g., IL-4 and IL-13, play important roles in chemokine production, skin barrier dysfunction, suppression of antimicrobial peptides (AMP), and allergic inflammation.15,40 Interestingly, IL-31 was reported to enhance the release and production of brain-derived natriuretic peptide and to coordinate cytokine and chemokine release from skin cells, thereby inducing itch in patients with AD.41 In addition, TSLP is highly expressed in the epidermis of patients with AD, and its production is triggered by exposure to environmental factors such as allergens, microorganisms, diesel exhaust, cigarette smoke, and chemical irritants.13,42,43 When using skin tape samples, a Korean birth cohort study showed elevated expression of TSLP in the skin of 2 month-old infants before the development of clinical AD at 24 months of age.44
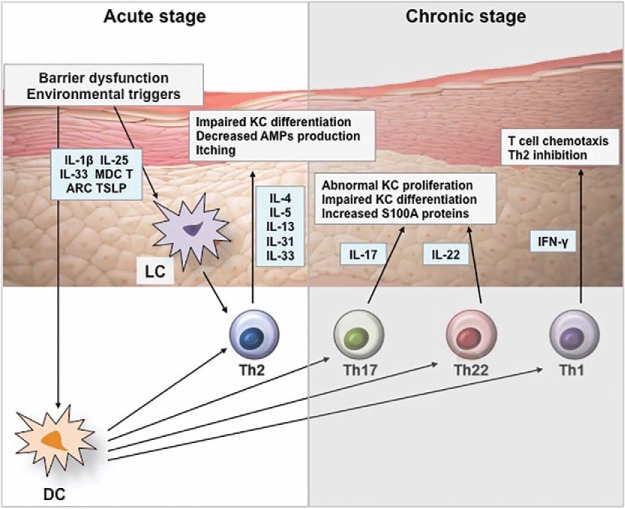
Although blockade of type 2–driven inflammation improves AD symptoms, the pathogenesis of AD is not exclusively explained by Th2 immunity. In this regard, IL-17 has been reported to reduce expression of FLG and involucrin.45,46 More prominent Th17 activation was observed in blood and acute AD skin lesions in Asian patients compared with European-American patients.47 In addition, AD is classified as the extrinsic and the intrinsic type, and production of IL-17 cytokine is higher in intrinsic AD with normal immunoglobulin E levels than in extrinsic AD.48 IL-22 is also highly upregulated in the skin of patients with AD and is associated with skin barrier dysfunction and abnormal epidermal markers, such as keratin 6 and keratin 16.49–51 In particular, transition to the chronic phase is manifested by the start of Th1-cell activation as well as the sustained activation of Th2 and Th22 cells (Fig. 1).52,53 Of interest, tumor necrosis factor α in combination with Th2 cytokines altered the expression of early and terminal differentiation products and reduced the level of long-chain free fatty acids (FFA) and ester linked ω-hydroxy (EO) ceramides.17,20
Figure 1.
Effects of cytokines on epidermis in AD. Disrupted epidermal barrier and environmental triggers stimulate keratinocytes to release IL-1β, IL-25, IL-33, MDC, TARC, and TSLP, which activate dendritic cells and Langerhans cells. Activated dendritic cells stimulate Th2 cells to produce IL-4, IL-5, IL-13, IL-31, and IL-33, which leads to barrier dysfunction, decreased AMP production, impaired keratinocyte differentiation, and itch symptoms. Chronic AD is characterized by recruitment of Th1, Th22, and Th17 subsets, which results in epidermal thickening and abnormal keratinocyte proliferation. AD = atopic dermatitis; AMP = antimicrobial peptide; DC = dendric cell; IFN = interferon; IL = interleukin; KC = keratinocyte; LC = Langerhans cell; MDC = macrophage-derived chemokine; S100A = S100 calcium-binding protein A; Th = T-helper type; TARC = thymus and activation-regulated chemokine; TSLP = thymic stromal lymphopoietin.
Recent studies showed that skin-resident group 2 innate lymphoid cells (ILC2) play a role in the pathogenesis of AD. ILC2s were found to produce IL-5 and IL-13, which result in the development of an AD-like skin lesion.54,55 Similarly, human skin ILC2s are highly enriched in lesional skin of patients with AD and activated by the epithelial cell–derived cytokines such as IL-25, IL-33, and/or TSLP.55,56 This leads to the production of type 2 cytokines and skin allergic inflammation.55,56 In contrast, epidermal ILC2s are inhibited by E-cadherin, and its downregulation recent studies showed that skin-resident.56
NEUROIMMUNOLOGIC MECHANISMS
A subset of sensory neurons that express histamine H1 receptor and histamine H4 receptor is activated by histamine, which can cause itch as well as allergic inflammation.57 H1 antihistamines have been widely used for the treatment of itch due to urticaria, but its effects are limited in the treatment of chronic itch in patients with AD. Recently, much interest has focused on the role of histamine-independent itch signaling pathways in which TSLP and type 2 cytokines, such as IL-4, IL-13, and IL-31, stimulate neurons expressing transient receptor potential cation channel subfamily A member 1 and afferent neurons via its receptors and Janus kinase (JAK) family, respectively.19 Of note, IL-31 induces sensory nerve elongation and branching, which supports its role that involves sensitivity to minimal stimuli and sustained itch in patients with AD.58 In addition, the activation of STAT3 in the astrocytes of the spinal dorsal horn has been reported to be involved in chronic pruritus via the generation of lipocalin-2.59
EPIDERMAL DYSFUNCTION
IL-4, IL-13, IL-31, IL-33, and high-mobility group box 1 downregulate the production of epidermal barrier proteins, including FLG, keratins, loricrin, involucrin, and cell adhesion molecules.14,15,60–62 A damaged epidermal barrier not only leads to the development of AD but also heightens sensitization to allergens and contributes to the risk of Food allergy (FA) and airway hyperreactivity.7,12 Impairment of skin barrier function at birth and at 2 months, as evaluated by transepidermal water loss (TEWL), can precede clinical AD by 12 months of age.63 Moreover, increased TEWL in the early newborn period is associated with a higher incidence of FA at 2 years of age, which supports the concept of transcutaneous allergen sensitization.64 Defects in epidermal barrier proteins, such as FLG, transglutaminases, keratins, and intercellular proteins, facilitate dysregulated immune responses to external antigens and drive skin and systemic inflammatory responses (Table 1).9,10 FLG is highly downregulated in both lesional and nonlesional skin of patients with AD.65
Table 1.
Epithelial skin dysfunction in atopic dermatitis
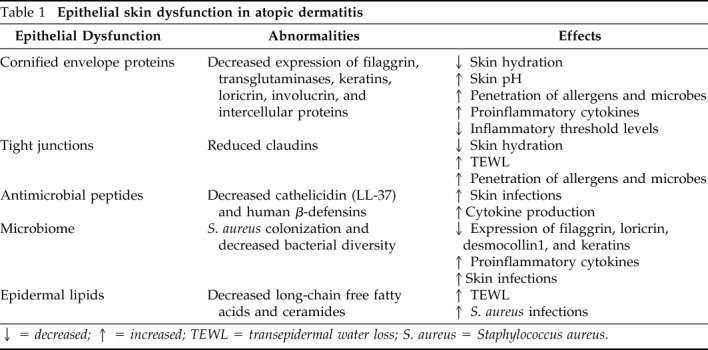
↓ = decreased; ↑ = increased; TEWL = transepidermal water loss; S. aureus = Staphylococcus aureus.
Recently, McAleer et al.66 demonstrated that FLG breakdown products in the first year of life are lowest in the cheek compared with the elbow and the nasal tip, and the slowest to achieve maturity levels, which supports the importance of FLG on the pathogenesis of infantile AD. In that study, FLG processing enzymes such as bleomycin hydrolase and calpain-1 were also increased at cheek skin by 1 month of age.64 This may explain the predilection for AD at the cheeks initially in early childhood. Epidermal FLG levels are also reduced by environmental factors, including low humidity, sunburns, diesel exhaust particles, and skin irritants.67,68 In addition, loricrin and involucrin are downregulated by overexpression of Th2 cytokines through a STAT6-dependent mechanism in AD skin.69 Corneodesmosin (CDSN) and tight junctions play a central role by supporting the adhesion between corneocytes and the integrity of the skin barrier as an intercellular protein.9,70 A recent study showed that CDSN was downregulated by IL-4, IL-13, IL-22, IL-25, and IL-31 in human keratinocytes, and the penetration of vaccinia virus was enhanced in a CDSN-deficient skin model.69 In addition, claudin 1–deficient mice were reported to die within 1 day of birth with wrinkled skin appearance and severe dehydration, which provides good evidence for the essential role of claudin for the skin barrier function.72
AMPs, including cathelicidin (LL-37) and human β-defensins, are produced by keratinocytes and play a pivotal role for host defense as well as control of host physiologic functions, such as inflammation and wound healing.73 AMP expressions are inhibited by Th2 cytokines, which are highly produced in AD skin.74 The decreased expression of AMPs is associated with a higher predisposition to Staphylococcus aureus colonization, which can aggravate AD.75 It has been reported that human β-defensins and LL-37 are chemoattractants for T lymphocytes, monocytes, dendritic cells, and neutrophils, and can induce cytokine production by monocytes and epithelial cells.76,77 These immunomodulatory properties of AMPs have important roles for host defense against infections through activation of immune cells as well as their direct antimicrobial activity.
LIPIDS
Lipids, such as ceramides, long-chain FFAs, and cholesterol, constitute the lipid matrix that is organized in lamellar bodies and located between corneocytes.78 During epidermal differentiation, precursor lipids are stored in lamellar bodies within the upper cell layers of the epidermis and extruded into the extracellular domain.79 Subsequent enzymic processing produces the major lipid classes, which are necessary to maintain the integrity of the epidermal barrier. Altered lipid composition is observed in lesional and nonlesional AD skin.20 In particular, long-chain EO ceramides are essential because they are covalently bound to cornified-envelope proteins and cover the surface of each corneocyte.79 Th2 cytokines reduce levels of long-chain FFAs and EO ceramides with a STAT6-dependent manner.17,18,20 The levels of long-chain ceramides were decreased in patients with AD and who were colonized with S. aureus when compared with those who were not colonized. TEWL was negatively correlated with levels of these ceramides.80
MICROBIOME
AD skin has decreased bacterial diversity associated with increased Staphylococcus, Corynebacterium, and with reduced Streptococcus, Propionibacterium, Acinetobacter, Corynebacterium, and Propionibacterium during AD flares.81,82 Greater bacterial diversity with increased abundance of Staphylococcus epidermidis and Streptococcus, Corynebacterium, and Propionibacterium species was observed after AD treatment and reduced eczema.82 Species-level investigation of AD has shown a higher predominance of S. aureus in patients with more-severe disease and an abundance of S. epidermidis in patients with less-severe disease.83 S. aureus colonizes AD skin and has pivotal roles in the development and exacerbation of AD.84 S. aureus can induce T-cell–independent B-cell expansion; upregulate proinflammatory cytokines, such as TSLP, IL-4, IL-12, and IL-22; and stimulate mast cell degranulation, which results in Th2 skewing and skin inflammation.85–88
A recent study demonstrated that epidermal thickening and expansion of cutaneous Th2 and Th17 cells were induced when mice were exposed to S. aureus isolates from patients with AD.83 Of note, methicillin-resistant S. aureus colonization on AD skin is associated with lower microbial diversity and a more profound reduction in the composition of commensal bacteria, such as Streptococcus and Propionibacterium, than methicillin-sensitive S. aureus colonization.89 It is presumed that the differences and shifts in skin microbiome according to AD status are associated with the production of bacteriocins and AMPs from commensal bacteria.90,91 In addition, a recent study showed a positive correlation between the abundance of propionibacteria and corynebacteria on epidermis and long-chain unsaturated FFAs, such as FA20:1, FA20:2, FA22:1, and FA24:1.92 These findings highlight the importance of the balance between S. aureus and commensal bacteria.
Patients with AD have significantly lower numbers of intestinal commensal Bifidobacterium and higher numbers of Staphylococcus than healthy control subjects.93 Overgrowth of pathogenic bacteria, such as Escherichia coli and Clostridium difficile, is postulated as being associated with a decrease in beneficial bacteria, reduced induction of regulatory T (Treg) cells, loss of immune tolerance, and increased intestinal permeability.94,95 These observations support the hypothesis that specific microbial composition in the gut prevented Th2-shifted immunity and stimulated regulatory immunity, producing regulatory dendritic cells and Treg cells.96,97 However, further studies are necessary to elucidate how dysbiosis affects epidermal barrier function and the development of AD.
CLINICAL APPLICATION
Frequent application of appropriate moisturizers, such as physiologic lipid mixtures and ceramide-dominant lipid, is known to help reduce TEWL, enhance skin hydration, decrease bacterial colonization, and improve skin barrier function, which leads to decreased need for topical corticosteroid.1,98,99 Petrolatum application has been reported to upregulate AMPs; induce key barrier differentiation markers, e.g., FLG; and reduces T-cell infiltration in AD skin.98 Of note, regular application of emollients has been reported to reduce the risk of AD development as a primary prevention strategy in infants at high risk.100,101 In addition, a recent study demonstrated that topical application of a liver X receptor agonist (VTP-38543) improved epidermal differentiation and lipids in patients with mild-to-moderate AD.102
Topical calcineurin inhibitors, such as tacrolimus and pimecrolimus, inhibit calcineurin-dependent T-cell activation, which leads to downregulation of proinflammatory cytokines.99 Systemic immunosuppressants, including cyclosporine, methotrexate, and azathioprine, are used in patients with severe and difficult-to-treat symptoms.99 However, these drugs have limitations and adverse reactions. Therefore, various biologics to target polarized immune pathways have been newly developed for patients with moderate-to-severe AD. Although omalizumab did not show beneficial effects to treat AD,103,104 dupilumab, a humanized monoclonal antibody (mAb) to block IL-4 and IL-13, has been approved by the Food and Drug Administration.105,106 Clinical efficacy of dupilumab occurred without significant safety concerns in adult patients with AD.105,106 Clinical trials are also underway with dupilumab in pediatric populations (NCT02407756, NCT02612454, NCT03054428, NCT03346434, NCT03345914). Because the upregulation of Th17 and Th22 cytokines have been identified in patients with AD, the blockade of these pathways is being investigated by using secukinumab and a human monoclonal antibody against interleukin-22 (ILV-094; NCT02594098, NCT01941537). Moreover, Guttman-Yassky et al.107 reported that an anti-IL-22 mAb (fezakinumab) showed clinical improvement in patients with severe AD.107
A recent study also showed clear trends of therapeutic effects of ustekinumab, which is an IL-12/IL-23p40 antagonist, to suppress Th1, Th17, and Th22 immune activation in adults with moderate-to-severe AD.108 However, there was no significant difference between treatment and placebo groups in that study.108 Another Japanese study also did not demonstrate meaningful efficacy of ustekinumab on AD,109 although it is known to be effective for psoriasis.110 Nemolizumab (anti–IL-31R mAb), lebrikizumab (anti–IL-13 mAb), and tralokinumab (anti–IL-13 mAb) revealed promising results.106 Other biologic agents, such as Bristol-Myers Squibb-981164 (anti–IL-31 mAb), Tezepelumab (anti–TSLP mAb), and MK-8226 (anti-TSLP receptor mAb), are studied and may offer a range of new therapeutic options of AD. In addition, topical tofacitinib (JAK1/JAK 3 inhibitor) and oral baricitinib (JAK1/ JAK2 inhibitor) were reported to have reduced skin inflammation and pruritus in patients with AD.111,112
Although topical and systemic antibiotics have been used to eradicate bacteria from AD skin, long-term use has limitations due to the induction of resistant microorganisms and the negative impact on host commensal bacteria. Recent studies reported that a bleach bath is effective for the restoration of skin microbiome and the treatment of AD.113,114 However, a recent meta-analysis did not show its additional benefits compared with water bath alone.115 Interestingly, Nakatsuji et al.116 found targeted autologous skin microbiome transplantation of S. hominis and S. epidermidis decreased S. aureus from AD skin. Another recent study showed that the topical transplantation with Roseomonas mucosa improved AD severity and reduced Staphylococcus aureus colonization.117
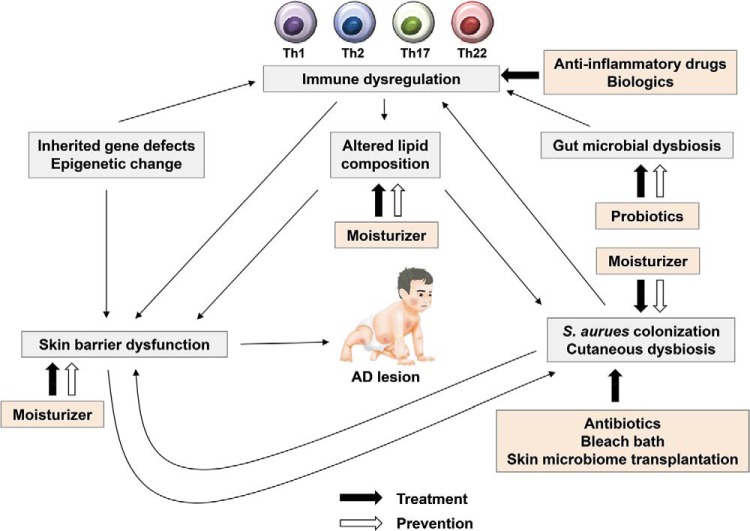
Recent studies demonstrated that appropriate probiotics are beneficial in the prevention and treatment of AD through the modulation of host immune responses.96,118,119 However, there have still been controversies regarding these clinical effects of probiotics in patients with AD, which might be due to a difference in the strains of probiotics and the characteristics of the host. It is noteworthy that the response to probiotics is greater in patients with an immunologically active state characterized by high total immunoglobulin E levels and increased expression of transforming growth factor β and Treg cells.96 Analysis of these emerging data indicated that identification of adequate AD phenotypes for the specific therapeutic option could be a key to achieve a good clinical outcome (Fig. 2).
Figure 2.
Prevention and treatment of AD. Skin barrier defects are the initial steps in the development of AD. Moisturizer prevents skin barrier defects and inhibits Staphylococcus aureus colonization in the skin. Oral probiotics may prevent the development of AD and correct gut microbial dysbiosis. Various biologics, e.g., dupilumab, target immune dysregulation. Antibiotics, bleach batch, and skin microbiome transplantation inhibit S. aureus colonization and improve cutaneous dysbiosis. AD = atopic dermatitis; Th = T helper.
CONCLUSION
Multiple factors, including epidermal gene mutations, skin barrier dysfunction, immune dysregulation, neuroinflammation, altered lipid composition, and microbial imbalance, can contribute to the development of AD. Various strategies have been used to restore skin barrier function and control skin inflammation in patients with AD. To overcome limitations of topical anti-inflammatory drugs and systemic immunosuppressants, substantial effort has been committed to the development of new therapeutic options, including biologics and microbiome transplantation. In addition, moisturizers and probiotics may prevent the development of AD in infants at high risk. Further advances in our understanding of AD pathophysiology will allow us to achieve a precision medicine approach to the prevention and the treatment of AD.
ACKNOWLEDGMENTS
We thank Samsung Medical Information and Media Services, Samsung Medical Center for the preparation of figures for this article.
Footnotes
This work was supported by NIH grant AR41256. This study was also supported by Ministry of Environment, Republic of Korea.
Presented at the Eastern Allergy Conference, June 2, 2018, Palm Beach Florida
D.Y.M. Leung has consulted for Regeneron, Sanofi, Novartis and Genzyme. The remaining authors have no conflicts of interest to declare pertaining to this article
No external funding sources reported
REFERENCES
- 1. Kim BE, Leung DYM. Significance of skin barrier dysfunction in atopic dermatitis. Allergy Asthma Immunol Res. 2018; 10:207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Silverberg JI. Public health burden and epidemiology of atopic dermatitis. Dermatol Clin. 2017; 35:283–289. [DOI] [PubMed] [Google Scholar]
- 3. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh) 1980; 92:44–47. [Google Scholar]
- 4. Eichenfield LF. Consensus guidelines in diagnosis and treatment of atopic dermatitis. Allergy 2004; 59 (Suppl 78):86–92, 2004. [DOI] [PubMed] [Google Scholar]
- 5. Schmitt J, Langan S, Deckert S, et al. Assessment of clinical signs of atopic dermatitis: a systematic review and recommendation. J Allergy Clin Immunol. 2013; 132:1337–1347. [DOI] [PubMed] [Google Scholar]
- 6. Brunner PM, Leung DYM, Guttman-Yassky E. Immunologic, microbial, and epithelial interactions in atopic dermatitis. Ann Allergy Asthma Immunol. 2018; 120:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lowe AJ, Leung DYM, Tang MLK, Su JC, Allen KJ. The skin as a target for prevention of the atopic march. Ann Allergy Asthma Immunol. 2018; 120:145–151. [DOI] [PubMed] [Google Scholar]
- 8. Kim BE, Leung DY. Epidermal barrier in atopic dermatitis. Allergy Asthma Immunol Res. 2012; 4:12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Egawa G, Kabashima K. Multifactorial skin barrier deficiency and atopic dermatitis: Essential topics to prevent the atopic march. J Allergy Clin Immunol. 2016; 138:350–358.e1. [DOI] [PubMed] [Google Scholar]
- 10. Schleimer RP, Berdnikovs S. Etiology of epithelial barrier dysfunction in patients with type 2 inflammatory diseases. J Allergy Clin Immunol. 2017; 139:1752–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Strid J, Hourihane J, Kimber I, Callard R, Strobel S. Disruption of the stratum corneum allows potent epicutaneous immunization with protein antigens resulting in a dominant systemic Th2 response. Eur J Immunol. 2004; 34:2100–2109. [DOI] [PubMed] [Google Scholar]
- 12. Dharmage SC, Lowe AJ, Matheson MC, Burgess JA, Allen KJ, Abramson MJ. Atopic dermatitis and the atopic march revisited. Allergy. 2014; 69:17–27. [DOI] [PubMed] [Google Scholar]
- 13. Thyssen JP, Kezic S. Causes of epidermal filaggrin reduction and their role in the pathogenesis of atopic dermatitis. J Allergy Clin Immunol. 2014; 134:792–799. [DOI] [PubMed] [Google Scholar]
- 14. Egawa G, Kabashima K. Barrier dysfunction in the skin allergy. Allergol Int. 2018; 67:3–11. [DOI] [PubMed] [Google Scholar]
- 15. Howell MD, Kim BE, Gao P, et al. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 2009; 124:R7–R12. [DOI] [PubMed] [Google Scholar]
- 16. Leonardi S, Rotolo N, Vitaliti G, Spicuzza L, La Rosa M. IgE values and T-lymphocyte subsets in children with atopic eczema/dermatitis syndrome. Allergy Asthma Proc. 2007; 28:529–534. [DOI] [PubMed] [Google Scholar]
- 17. Danso MO, van Drongelen V, Mulder A, et al. TNF-α and Th2 cytokines induce atopic dermatitis-like features on epidermal differentiation proteins and stratum corneum lipids in human skin equivalents. J Invest Dermatol. 2014; 134:1941–1950. [DOI] [PubMed] [Google Scholar]
- 18. Janssens M, van Smeden J, Gooris GS, et al. Increase in short-chain ceramides correlates with an altered lipid organization and decreased barrier function in atopic eczema patients. J Lipid Res. 2012; 53:2755–2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primers. 2018; 4:1. [DOI] [PubMed] [Google Scholar]
- 20. Berdyshev E, Goleva E, Bronova I, et al. Lipid abnormalities in atopic skin are driven by type 2 cytokines. JCI Insight. 2018; 3 pii: 98006 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kaufman BP, Guttman-Yassky E, Alexis AF. Atopic dermatitis in diverse racial and ethnic groups-Variations in epidemiology, genetics, clinical presentation and treatment. Exp Dermatol. 2018; 27:340–357. [DOI] [PubMed] [Google Scholar]
- 22. Irvine AD, McLean WH, Leung DY. Filaggrin mutations associated with skin and allergic diseases. N Engl J Med. 2011; 365:1315–1327. [DOI] [PubMed] [Google Scholar]
- 23. Brown SJ, McLean WH. One remarkable molecule: filaggrin. J Invest Dermatol. 2012; 132:751–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yu HS, Kang MJ, Jung YH, et al. Mutations in the filaggrin are predisposing factor in Korean children with atopic dermatitis. Allergy Asthma Immunol Res. 2013; 5:211–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O'Regan GM, Sandilands A, McLean WH, McLean WHI, Irvine AD. Filaggrin in atopic dermatitis. J Allergy Clin Immunol. 2008; 122:689–693. [DOI] [PubMed] [Google Scholar]
- 26. Bin L, Leung DY. Genetic and epigenetic studies of atopic dermatitis. Allergy Asthma Clin Immunol. 2016; 12:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Howell MD, Kim BE, Gao P, et al. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 2007; 120:150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hussein YM, Shalaby SM, Nassar A, Alzahrani SS, Alharbi AS, Nouh M. Association between genes encoding components of the IL-4/IL-4 receptor pathway and dermatitis in children. Gene. 2014; 545:276–281. [DOI] [PubMed] [Google Scholar]
- 29. Namkung JH, Lee JE, Kim E, et al. Association of polymorphisms in genes encoding IL-4. IL-13 and their receptors with atopic dermatitis in a Korean population. Exp Dermatol. 2011; 20:915–919. [DOI] [PubMed] [Google Scholar]
- 30. Esaki H, Ewald DA, Ungar B, et al. Identification of novel immune and barrier genes in atopic dermatitis by means of laser capture microdissection. J Allergy Clin Immunol. 2015; 135:153–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lee YL, Yen JJ, Hsu LC, et al. Association of STAT6 genetic variants with childhood atopic dermatitis in Taiwanese population. J Dermatol Sci. 2015; 79:222–228. [DOI] [PubMed] [Google Scholar]
- 32. Gao PS, Leung DY, Rafaels NM, et al. Genetic variants in interferon regulatory factor 2 (IRF2) are associated with atopic dermatitis and eczema herpeticum. J Invest Dermatol. 2012; 132:650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Salpietro C, Rigoli L, Miraglia Del Giudice M, et al. TLR2 and TLR4 gene polymorphisms and atopic dermatitis in Italian children: a multicenter study. Int J Immunopathol Pharmacol. 2011; 24(Suppl):33–40. [DOI] [PubMed] [Google Scholar]
- 34. Suzuki H, Makino Y, Nagata M, et al. A rare variant in CYP27A1 and its association with atopic dermatitis with high serum total IgE. Allergy. 2016; 71:1486–1489. [DOI] [PubMed] [Google Scholar]
- 35. Heine G, Hoefer N, Franke A, et al. Association of vitamin D receptor gene polymorphisms with severe atopic dermatitis in adults. Br J Dermatol. 2013; 168:855–858. [DOI] [PubMed] [Google Scholar]
- 36. Thurmann L, Grutzmann K, Klos M, et al. Early-onset childhood atopic dermatitis is related to NLRP2 repression. J Allergy Clin Immunol. 2018; 141:1482–1485.e16. [DOI] [PubMed] [Google Scholar]
- 37. Barton SJ, Ngo S, Costello P, et al. DNA methylation of Th2 lineage determination genes at birth is associated with allergic outcomes in childhood. Clin Exp Allergy. 2017; 47:1599–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ziyab AH, Karmaus W, Holloway JW, Zhang H, Ewart S, Arshad SH. DNA methylation of the filaggrin gene adds to the risk of eczema associated with loss-of-function variants. J Eur Acad Dermatol Venereol. 2013; 27:e420–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tan HT, Ellis JA, Koplin JJ, et al. Methylation of the filaggrin gene promoter does not affect gene expression and allergy. Pediatr Allergy Immunol. 2014; 25:608–610. [DOI] [PubMed] [Google Scholar]
- 40. Boguniewicz M. Biologic therapy for atopic dermatitis: moving beyond the practice parameter and guidelines. J Allergy Clin Immunol Pract. 2017; 5:1477–1487. [DOI] [PubMed] [Google Scholar]
- 41. Meng J, Moriyama M, Feld M, et al. New mechanism underlying IL-31-induced atopic dermatitis. J Allergy Clin Immunol. 2018; 141:1677–1689.e8. [DOI] [PubMed] [Google Scholar]
- 42. Landheer J, Giovannone B, Mattson JD, et al. Epicutaneous application of house dust mite induces thymic stromal lymphopoietin in nonlesional skin of patients with atopic dermatitis. J Allergy Clin Immunol. 2013; 132:1252–1254. [DOI] [PubMed] [Google Scholar]
- 43. Takai T. TSLP expression: cellular sources, triggers, and regulatory mechanisms. Allergol Int. 2012; 61:3–17. [DOI] [PubMed] [Google Scholar]
- 44. Kim J, Kim BE, Lee J, et al. Epidermal thymic stromal lymphopoietin predicts the development of atopic dermatitis during infancy. J Allergy Clin Immunol. 2016; 137:1282–1285.e4. [DOI] [PubMed] [Google Scholar]
- 45. Tan Q, Yang H, Liu E, Wang H. P38/ERK MAPK signaling pathways are involved in the regulation of filaggrin and involucrin by IL-17. Mol Med Rep. 2017; 16:8863–8867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Leonardi S, Cuppari C, Manti S, et al. Serum interleukin 17, interleukin 23, and interleukin 10 values in children with atopic eczema/dermatitis syndrome (AEDS): association with clinical severity and phenotype. Allergy Asthma Proc. 2015; 36:74–81. [DOI] [PubMed] [Google Scholar]
- 47. Koga C, Kabashima K, Shiraishi N, Kobayashi M, Tokura Y. Possible pathogenic role of Th17 cells for atopic dermatitis. J Invest Dermatol. 2008; 128:2625–2630. [DOI] [PubMed] [Google Scholar]
- 48. Suárez-Fariñas M, Dhingra N, Gittler J, et al. Intrinsic atopic dermatitis shows similar TH2 and higher TH17 immune activation compared with extrinsic atopic dermatitis. J Allergy Clin Immunol. 2013; 132:361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nograles KE, Zaba LC, Shemer A, et al. IL-22-producing “T22” T cells account for upregulated IL-22 in atopic dermatitis despite reduced IL-17-producing TH17 T cells. J Allergy Clin Immunol. 2009; 123:1244–1252.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Boniface K, Bernard FX, Garcia M, Gurney AL, Lecron JC, Morel F. IL-22 inhibits epidermal differentiation and induces proinflammatory gene expression and migration of human keratinocytes. J Immunol. 2005; 174:3695–3702. [DOI] [PubMed] [Google Scholar]
- 51. Esaki H, Brunner PM, Renert-Yuval Y, et al. Early-onset pediatric atopic dermatitis is TH2 but also TH17 polarized in skin. J Allergy Clin Immunol. 2016; 138:1639–1651. [DOI] [PubMed] [Google Scholar]
- 52. Guttman-Yassky E, Krueger JG, Lebwohl MG. Systemic immune mechanisms in atopic dermatitis and psoriasis with implications for treatment. Exp Dermatol. 2018; 27:409–417. [DOI] [PubMed] [Google Scholar]
- 53. Gittler JK, Shemer A, Suárez-Fariñas M, et al. Progressive activation of T(H)2/T(H)22 cytokines and selective epidermal proteins characterizes acute and chronic atopic dermatitis. J Allergy Clin Immunol. 2012; 130:1344–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Roediger B, Kyle R, Yip KH, et al. Cutaneous immunosurveillance and regulation of inflammation by group 2 innate lymphoid cells. Nat Immunol. 2013; 14:564–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kim BS, Siracusa MC, Saenz SA, et al. TSLP elicits IL-33-independent innate lymphoid cell responses to promote skin inflammation. Sci Transl Med. 2013; 5:170ra16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Salimi M, Barlow JL, Saunders SP, et al. A role for IL-25 and IL-33-driven type-2 innate lymphoid cells in atopic dermatitis. J Exp Med. 2013; 210:2939–2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rerknimitr P, Otsuka A, Nakashima C, Kabashima K. The etiopathogenesis of atopic dermatitis: barrier disruption, immunological derangement, and pruritus. Inflamm Regen. 2017; 37:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Feld M, Garcia R, Buddenkotte J, et al. The pruritus- and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J Allergy Clin Immunol. 2016; 138:500–508.e524. [DOI] [PubMed] [Google Scholar]
- 59. Shiratori-Hayashi M, Koga K, Tozaki-Saitoh H, et al. STAT3-dependent reactive astrogliosis in the spinal dorsal horn underlies chronic itch. Nat Med. 2015; 21:927–931. [DOI] [PubMed] [Google Scholar]
- 60. Cornelissen C, Marquardt Y, Czaja K, et al. IL-31 regulates differentiation and filaggrin expression in human organotypic skin models. J Allergy Clin Immunol. 2012; 129:426–433, 433.e1–8. [DOI] [PubMed] [Google Scholar]
- 61. Nygaard U, van den Bogaard EH, Niehues H, et al. The “Alarmins” HMBG1 and IL-33 downregulate structural skin barrier proteins and impair epidermal growth. Acta Derm Venereol. 2017; 97:305–312. [DOI] [PubMed] [Google Scholar]
- 62. Cuppari C, Manti S, Salpietro A, et al. HMGB1 levels in children with atopic eczema/dermatitis syndrome (AEDS). Pediatr Allergy Immunol. 2016; 27:99–102. [DOI] [PubMed] [Google Scholar]
- 63. Kelleher M, Dunn-Galvin A, Hourihane JO, et al. Skin barrier dysfunction measured by transepidermal water loss at 2 days and 2 months predates and predicts atopic dermatitis at 1 year. J Allergy Clin Immunol. 2015; 135:930–935.e1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 64. Kelleher MM, Dunn-Galvin A, Gray C, et al. Skin barrier impairment at birth predicts food allergy at 2 years of age. J Allergy Clin Immunol. 2016; 137:1111–1116.e8. [DOI] [PubMed] [Google Scholar]
- 65. Pellerin L, Henry J, Hsu CY, et al. Defects of filaggrin-like proteins in both lesional and nonlesional atopic skin. J Allergy Clin Immunol. 2013; 131:1094–1102. [DOI] [PubMed] [Google Scholar]
- 66. McAleer MA, Jakasa I, Raj N, et al. Early life regional and temporal variation in filaggrin-derived natural moisturising factor, filaggrin processing enzyme activity, corneocyte phenotypes and plasmin activity: implications for atopic dermatitis. Br J Dermatol. 2018; 179:431–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Katagiri C, Sato J, Nomura J, Denda M. Changes in environmental humidity affect the water-holding property of the stratum corneum and its free amino acid content, and the expression of filaggrin in the epidermis of hairless mice. J Dermatol Sci. 2003; 31:29–35. [DOI] [PubMed] [Google Scholar]
- 68. Bernerd F, Asselineau D. Successive alteration and recovery of epidermal differentiation and morphogenesis after specific UVB-damages in skin reconstructed in vitro. Dev Biol. 1997; 183:123–138. [DOI] [PubMed] [Google Scholar]
- 69. Kim BE, Leung DY, Boguniewicz M, Howell MD. Loricrin and involucrin expression is down-regulated by Th2 cytokines through STAT-6. Clin Immunol. 2008; 126:332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lundström A, Serre G, Haftek M, Egelrud T. Evidence for a role of corneodesmosin, a protein which may serve to modify desmosomes during cornification, in stratum corneum cell cohesion and desquamation. Arch Dermatol Res. 1994; 286:369–375. [DOI] [PubMed] [Google Scholar]
- 71. Lee UH, Kim BE, Kim DJ, Cho YG, Ye YM, Leung DY. Atopic dermatitis is associated with reduced corneodesmosin expression: role of cytokine modulation and effects on viral penetration. Br J Dermatol. 2017; 176:537–540. [DOI] [PubMed] [Google Scholar]
- 72. Furuse M, Hata M, Furuse K, et al. Claudin-based tight junctions are crucial for the mammalian epidermal barrier: a lesson from claudin-1-deficient mice. J Cell Biol. 2002; 156:1099–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Nakatsuji T, Gallo RL. Antimicrobial peptides: old molecules with new ideas. J Invest Dermatol. 2012; 132:887–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Nomura I, Goleva E, Howell MD, et al. Cytokine milieu of atopic dermatitis, as compared to psoriasis, skin prevents induction of innate immune response genes. J Immunol. 2003; 171:3262–3269. [DOI] [PubMed] [Google Scholar]
- 75. Miller LS, Sørensen OE, Liu PT, et al. TGF-alpha regulates TLR expression and function on epidermal keratinocytes. J Immunol. 2005; 174:6137–6143. [DOI] [PubMed] [Google Scholar]
- 76. Niyonsaba F, Iwabuchi K, Someya A, et al. A cathelicidin family of human antibacterial peptide LL-37 induces mast cell chemotaxis. Immunology. 2002; 106:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. De Yang, Chen Q, Schmidt AP, et al. LL-37, the neutrophil granule- and epithelial cell-derived cathelicidin, utilizes formyl peptide receptor-like 1 (FPRL1) as a receptor to chemoattract human peripheral blood neutrophils, monocytes, and T cells. J Exp Med. 2000; 192:1069–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Elias PM. Structure and function of the stratum corneum extracellular matrix. J Investig Dermatol. 2012; 132:2131–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Holleran WM, Takagi Y, Uchida Y. Epidermal sphingolipids: metabolism, function, and roles in skin disorders. FEBS Lett. 2006; 580:5456–5466. [DOI] [PubMed] [Google Scholar]
- 80. Li S, Villarreal M, Stewart S, et al. Altered composition of epidermal lipids correlates with Staphylococcus aureus colonization status in atopic dermatitis. Br J Dermatol. 2017; 177:e125–e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bjerre RD, Bandier J, Skov L, Engstrand L, Johansen JD. The role of the skin microbiome in atopic dermatitis: a systematic review. Br J Dermatol. 2017; 177:1272–1278. [DOI] [PubMed] [Google Scholar]
- 82. Kong HH, Oh J, Deming C, et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 2012; 22:850–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Byrd AL, Deming C, Cassidy SKB, et al. Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis. Sci Transl Med. 9, 2017l 9. pii: eaal4651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Brauweiler AM, Hall CF, Goleva E, Leung DYM. Staphylococcus aureus lipoteichoic acid inhibits keratinocyte differentiation through a p63-mediated pathway. J Invest Dermatol. 2017; 137:2030–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Nakatsuji T, Chen TH, Two AM, et al. Staphylococcus aureus exploits epidermal barrier defects in atopic dermatitis to trigger cytokine expression. J Invest Dermatol. 2016; 136:2192–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Bekeredjian-Ding I, Inamura S, Giese T, et al. Staphylococcus aureus protein A triggers T cell-independent B cell proliferation by sensitizing B cells for TLR2 ligands. J Immunol. 2007; 178:2803–2812. [DOI] [PubMed] [Google Scholar]
- 87. Leung DY, Guttman-Yassky E. Deciphering the complexities of atopic dermatitis: shifting paradigms in treatment approaches. J Allergy Clin Immunol. 2014; 134:769–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Nakamura Y, Oscherwitz J, Cease KB, et al. Staphylococcus δ-toxin induces allergic skin disease by activating mast cells. Nature. 2013; 503:397–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Shi B, Leung DYM, Taylor PA, Li H. Methicillin-resistant Staphylococcus aureus colonization is associated with decreased skin commensal bacteria in atopic dermatitis. J Invest Dermatol. 2018; 138:1668–1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Lai Y, Cogen AL, Radek KA, et al. Activation of TLR2 by a small molecule produced by Staphylococcus epidermidis increases antimicrobial defense against bacterial skin infections. J Invest Dermatol. 2010; 130:2211–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Cogen AL, Yamasaki K, Muto J, et al. Staphylococcus epidermidis antimicrobial delta-toxin (phenol-soluble modulin-gamma) cooperates with host antimicrobial peptides to kill group A Streptococcus. PLoS One. 2010; 5:e8557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Baurecht H, Ruhlemann MC, Rodriguez E, et al. Epidermal lipid composition, barrier integrity, and eczematous inflammation are associated with skin microbiome configuration. J Allergy Clin Immunol. 2018, 141:1668–1676.e16. [DOI] [PubMed] [Google Scholar]
- 93. Watanabe S, Narisawa Y, Arase S, et al. Differences in fecal microflora between patients with atopic dermatitis and healthy control subjects. J Allergy Clin Immunol. 2003; 111:587–591. [DOI] [PubMed] [Google Scholar]
- 94. Penders J, Thijs C, van den Brandt PA, et al. Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut. 2007; 56:661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Rook GA, Brunet LR. Microbes, immunoregulation, and the gut. Gut. 2005; 54:317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kim J, Lee BS, Kim B, et al. Identification of atopic dermatitis phenotypes with good responses to probiotics (Lactobacillus plantarum CJLP133) in children. Benef Microbes. 2017; 8:755–761. [DOI] [PubMed] [Google Scholar]
- 97. Kwon HK, Lee CG, So JS, et al. Generation of regulatory dendritic cells and CD4+Foxp3+ T cells by probiotics administration suppresses immune disorders. Proc Natl Acad Sci U S A. 2010; 107:2159–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Czarnowicki T, Malajian D, Khattri S, et al. Petrolatum: Barrier repair and antimicrobial responses underlying this “inert” moisturizer. J Allergy Clin Immunol. 2016; 137:1091–1102.e.7. [DOI] [PubMed] [Google Scholar]
- 99. Boguniewicz M, Fonacier L, Guttman-Yassky E, Ong PY, Silverberg J, Farrar JR. Atopic dermatitis yardstick: practical recommendations for an evolving therapeutic landscape. Ann Allergy Asthma Immunol. 2018; 120:10–22.e2. [DOI] [PubMed] [Google Scholar]
- 100. Simpson EL, Chalmers JR, Hanifin JM, et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014; 134:818–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Horimukai K, Morita K, Narita M, et al. Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol. 2014; 134:824–830.e6. [DOI] [PubMed] [Google Scholar]
- 102. Czarnowicki T, Dohlman AB, Malik K, et al. Effect of short-term liver X receptor activation on epidermal barrier features in mild to moderate atopic dermatitis: a randomized controlled trial. Ann Allergy Asthma Immunol. 2018; 120:631–640.e11. [DOI] [PubMed] [Google Scholar]
- 103. Andreae DA, Wang J. Immunologic effects of omalizumab in children with severe refractory atopic dermatitis: a randomized, placebo-controlled clinical trial. Pediatrics. 2014; 134(Suppl 3):S160. [DOI] [PubMed] [Google Scholar]
- 104. Heil PM, Maurer D, Klein B, Hultsch T, Stingl G. Omalizumab therapy in atopic dermatitis: depletion of IgE does not improve the clinical course - a randomized, placebo-controlled and double blind pilot study. J Dtsch Dermatol Ges. 2010; 8:990–998. [DOI] [PubMed] [Google Scholar]
- 105. Thaçi D, Simpson EL, Beck LA, et al. Efficacy and safety of dupilumab in adults with moderate-to-severe atopic dermatitis inadequately controlled by topical treatments: a randomised, placebo-controlled, dose-ranging phase 2b trial. Lancet. 2016; 387:40–52. [DOI] [PubMed] [Google Scholar]
- 106. Snast I, Reiter O, Hodak E, Friedland R, Mimouni D, Leshem YA. Are biologics efficacious in atopic dermatitis? a systematic review and meta-analysis. Am J Clin Dermatol. 2018; 19:145–165. [DOI] [PubMed] [Google Scholar]
- 107. Guttman-Yassky E, Brunner PM, Neumann AU, et al. Efficacy and safety of fezakinumab (an IL-22 monoclonal antibody) in adults with moderate-to-severe atopic dermatitis inadequately controlled by conventional treatments: a randomized, double-blind, phase 2a trial. J Am Acad Dermatol. 2018; 78:872–881.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Khattri S, Brunner PM, Garcet S, et al. Efficacy and safety of ustekinumab treatment in adults with moderate-to-severe atopic dermatitis. Exp Dermatol. 2017; 26:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Saeki H, Kabashima K, Tokura Y, et al. Efficacy and safety of ustekinumab in Japanese patients with severe atopic dermatitis: a randomized, double-blind, placebo-controlled, phase II study. Br J Dermatol. 2017; 177:419–427. [DOI] [PubMed] [Google Scholar]
- 110. Griffiths CE, Strober BE, van de Kerkhof P, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010; 362:118–128. [DOI] [PubMed] [Google Scholar]
- 111. Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016; 175:902–911. [DOI] [PubMed] [Google Scholar]
- 112. Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study. J Am Acad Dermatol. 2018. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 113. Maarouf M, Shi VY. Bleach for Atopic Dermatitis. Dermatitis. 2018; 29:120–126. [DOI] [PubMed] [Google Scholar]
- 114. Eriksson S, van der Plas MJA, Mörgelin M, Sonesson A. Antibacterial and antibiofilm effects of sodium hypochlorite against Staphylococcus aureus isolates derived from patients with atopic dermatitis. Br J Dermatol. 2017; 177:513–521. [DOI] [PubMed] [Google Scholar]
- 115. Chopra R, Vakharia PP, Sacotte R, Silverberg JI. Efficacy of bleach baths in reducing severity of atopic dermatitis: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2017; 119:435–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Nakatsuji T, Chen TH, Narala S, et al. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Sci Transl Med. 2017; 9 pii: eaah4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Myles IA, Earland NJ, Anderson ED, et al. First-in-human topical microbiome transplantation with Roseomonas mucosa for atopic dermatitis. JCI Insight 2018; 3 pii: 120608. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Han Y, Kim B, Ban J, et al. A randomized trial of Lactobacillus plantarum CJLP133 for the treatment of atopic dermatitis. Pediatr Allergy Immunol. 2012; 23:667–673. [DOI] [PubMed] [Google Scholar]
- 119. Kim JY, Kwon JH, Ahn SH, et al. Effect of probiotic mix (Bifidobacterium bifidum, Bifidobacterium lactis, Lactobacillus acidophilus) in the primary prevention of eczema: a double-blind, randomized, placebo-controlled trial Pediatr Allergy Immunol. 2010; 21:e386–393. [DOI] [PubMed] [Google Scholar]