Abstract
Killian‐Jamieson diverticulum (KJD) is a rare disease of the cervical esophagus, often misidentified as thyroid nodules on ultrasonography. We performed carotid artery ultrasonography for an asymptomatic 68‐year‐old man. The ultrasound showed an oval nodule with heterogeneous echogenicity surrounded by a multilayered rim in the posterior left thyroid gland. As endoscopy and computed tomography confirmed pharyngoesophageal diverticulum in the anterolateral wall of the esophagus, we reached a final diagnosis of KJD. In cases where a thyroid nodule is detected by ultrasound, physicians should be aware of the possibility of KJD before performing invasive procedures.
Keywords: health screening, Killian‐Jamieson diverticulum, ultrasound
1. INTRODUCTION
Pharyngoesophageal diverticulum is a rare disease of the cervical esophagus. Killian‐Jamieson diverticulum (KJD) is a form of pharyngoesophageal diverticulum, representing an evagination through a muscular gap in the anterolateral wall of the proximal cervical esophagus. Several reports have described incidental detection of KJD misidentified as thyroid nodules on thyroid ultrasonography.1, 2, 3 Dysphagia is the most common symptom of KJD and may be associated with regurgitation, cough, food retention, epigastric pain, halitosis, and swelling of the neck, but 81% of KJD cases are asymptomatic.1 Many cases of KJD may thus go undiagnosed.
Ultrasound screenings of the thyroid or carotid artery may occasionally detect nodules posterior to the thyroid gland in asymptomatic individuals. In cases where such nodules are detected, physicians should be aware of the possibility of KJD before performing invasive procedures, especially when the nodules are left‐sided. We present a case of asymptomatic left‐sided KJD detected on barium esophagography 3 years prior to the ultrasound. The patient in this case provided written, informed consent for publication of the details of his condition.
2. CASE PRESENTATION
An asymptomatic 68‐year‐old man visited the clinic for a regular annual health check. His past medical history included dyslipidemia and gastrointestinal discomfort. Pharmacotherapies included rosuvastatin, polycarbophil calcium, and Lactomin probiotic (BIO‐THREE Toa Pharmaceutical, Tokyo, Japan). He had smoked 40 cigarettes/day for 30 years, but had quit smoking almost 20 years earlier. He reported no symptoms of dysphagia, halitosis, food retention, or neck swelling. Ultrasonography using a Canon Xario SSA‐660A system (Canon Medical Systems Corporation, Otawara, Japan) with a 7.5‐MHz linear transducer (PLT‐704SBT; Canon Medical Systems Corporation) showed a 14.3 × 11.1 mm oval nodule with heterogeneous echogenicity surrounded by a multilayered rim in the posterior left lobe of the thyroid gland (Figure 1A,B). The posterior border was connected to the esophagus (Figure 1A,B). Endoscopy and computed tomography (CT) subsequently confirmed pharyngoesophageal diverticulum representing KJD (Figures 1C,2A‐D). The patient remained asymptomatic as of 2 years after the ultrasound screening. The diverticulum had actually been visible on barium esophagography conducted 3 years prior to the ultrasound (Figure 2E), but that result was neither relayed to the patient nor shared with medical practitioners.
Figure 1.
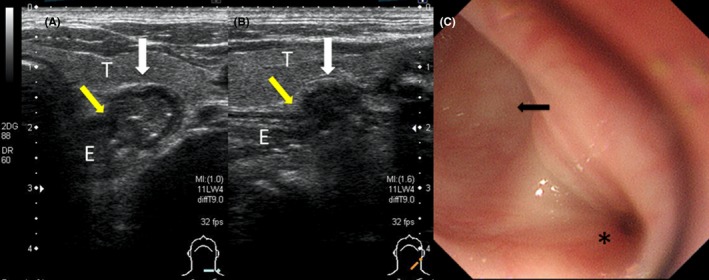
A transverse ultrasound image (A) shows a well‐demarcated, oval hypoechoic nodule (white arrow) with a multilayered rim resembling esophageal wall, along with multiple echogenic spots in the posterior left thyroid gland (T). A connection (yellow arrow) between the nodule (white arrow) and esophagus (E) is clearly visible. A longitudinal ultrasound image (B) shows an oval, hypoechoic nodule (white arrow), but no multilayered rim or multiple echogenic spots are visible. The connection (yellow arrow) between the nodule (white arrow) and esophagus (E) is clearly visible. An endoscopic view (C) shows the KJD (arrow) originating on the anterolateral wall of the cervical esophagus in the 9 o'clock direction. *, esophageal lumen
Figure 2.
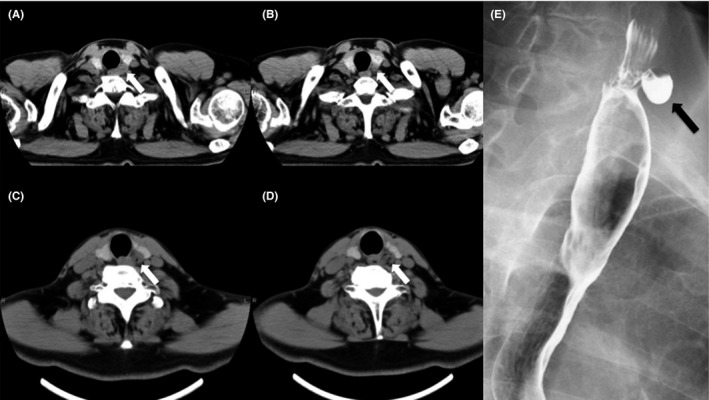
Axial computed tomography (CT) images of the chest (A,B) show a cystic lesion protruding anterolaterally from the esophagus (arrow) in the posterior left thyroid gland. Axial cervical CT images (C,D) show an air‐filled cystic lesion originating from the esophagus anterolaterally (arrow) in the posterior left thyroid gland. Esophagogram (E) confirms Killian‐Jamieson diverticulum (arrow) protruding anterolaterally to the left
3. DISCUSSION
Killian‐Jamieson diverticulum is a pharyngoesophageal diverticulum in the anterolateral wall of the proximal cervical esophagus. This pathology is less common than Zenker diverticulum arising on the posterior wall of the proximal cervical esophagus, with an incidence ratio to Zenker diverticulum of 1:4.1 Based on the epidemiology of Zenker diverticulum, the estimated annual incidence of KJD would be 1 per 200 000, with a prevalence between 0.0025% and 0.025%.4 However, these incidence and prevalence values may represent underestimations, since most patients with KJD are asymptomatic and may not seek medical advice. Most cases of KJD are left‐sided, although the reason for this laterality is unknown.1, 2, 3, 5, 6, 7 Screening ultrasonography of the thyroid or carotid artery may incidentally detect such pharyngoesophageal diverticula. Unnecessary biopsy has been performed in patients with KJD following misdiagnosis as a thyroid nodule.2, 3, 5 Medical practitioners and sonographers should be aware that KJD can mimic thyroid nodules to avoid unnecessary invasive procedures. KJD must be categorized as a risk factor for esophageal perforation, as blind insertion and advancement of a probe may injure the thin membrane during endoscopy or transesophageal echocardiography (TEE). Both endoscopists and cardiologists should thus be aware of KJD. In fact, some reports have described iatrogenic esophageal perforation.8, 9
On ultrasound, KJD can appear as an oval‐to‐round lesion with or without a hypoechoic rim, mimicking a thyroid nodule. Actually, a case of concomitant KJD and thyroid tumor has been reported.10 Real‐time ultrasound scanning is recommended to distinguish KJD from a thyroid nodule.6, 7 Barium study, endoscopy, and CT can also distinguish KJD from thyroid nodules, but are more invasive and expensive than ultrasound. Real‐time sonographic examinations can confidently differentiate thyroid from a diverticulum when the connection to the esophagus is clearly visible, along with changes in size, margins, and echogenicity during swallowing.6, 7 The drawback is that ultrasound is the most operator‐dependent imaging modality. The operator should record a video clip as well as the usual still images. In our case, no video clip was recorded because KJD was detected incidentally and the operator did not recognize this rare disease. Medical practitioners and sonographers should use the “clip store” function when nodules are identified, especially posterior to the left thyroid lobe.
4. CONCLUSIONS
Killian‐Jamieson diverticulum is a rare pharyngoesophageal diverticulum that can be found incidentally on thyroid or carotid artery ultrasound. KJD could represent a risk factor for iatrogenic esophageal perforation during invasive procedures. All medical practitioners and sonographers should be aware of the potential for KJD before performing invasive procedures such as needle biopsy or TEE.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ETHICAL STATEMENTS
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
INFORMED CONSENT
Informed consent was obtained from the patient for being included in the study.
Ota K, Onoe M, Oka M, et al. Killian‐Jamieson diverticulum mimicking a thyroid nodule: A case report. J Gen Fam Med. 2019;20:62–64. 10.1002/jgf2.222
REFERENCES
- 1. Rubesin SE, Levine MS. Killian‐Jamieson diverticula: radiographic findings in 16 patients. Am J Roentgenol. 2001;177(1):85–9. [DOI] [PubMed] [Google Scholar]
- 2. Kim HK, Lee JI, Jang HW, et al. Characteristics of Killian‐Jamieson diverticula mimicking a thyroid nodule. Head Neck. 2012;34(4):599–603. [DOI] [PubMed] [Google Scholar]
- 3. Nauschuetz KK, Ogden LL, Starling CE, Saleh MJ, Golding AC, Traweek ST. Pharyngoesophageal diverticula simulating thyroid nodules: an unusual occurrence with unique features. Diagn Cytopathol. 2018;46(2):193–7. [DOI] [PubMed] [Google Scholar]
- 4. Ferreira LEVVC, Simmons DT, Baron TH. Zenker's diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21(1):1–8. [DOI] [PubMed] [Google Scholar]
- 5. Wang Y, Song Y. Sonographic characteristics of pharyngoesophageal diverticula: report of 14 cases and review of the literature. J Clin Ultrasound. 2016;44(6):333–8. [DOI] [PubMed] [Google Scholar]
- 6. Mercer D, Blachar A, Khafif A, Weiss J, Kessler A. Real‐time sonography of Killian‐Jamieson diverticulum and its differentiation from thyroid nodules. J Ultrasound Med. 2005;24(4):557–60. [DOI] [PubMed] [Google Scholar]
- 7. Bonacchi G, Seghieri M, Becciolini M. Killian–Jamieson diverticulum: real‐time sonographic findings. J Ultrasound. 2016;19(4):295–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sainathan S, Andaz S. A systematic review of transesophageal echocardiography‐induced esophageal perforation. Echocardiography. 2013;30(8):977–83. [DOI] [PubMed] [Google Scholar]
- 9. Sobrino MA, Kozarek R, Low DE. Primary endoscopic management of esophageal perforation following transesophageal echocardiogram. J Clin Gastroenterol. 2004;38(7):581–5. [DOI] [PubMed] [Google Scholar]
- 10. Mimatsu K, Oida T, Kano H, et al. Killian‐Jamieson diverticula presenting synchronously with thyroid adenoma. Case Rep Gastroenterol. 2013;7(1):188–94. [DOI] [PMC free article] [PubMed] [Google Scholar]


