Abstract
Vertebral osteomyelitis can result in serious complications if diagnosis is delayed. Magnetic resonance imaging (MRI) is considered the most useful modality for the early diagnosis of vertebral osteomyelitis. We examined three patients with vertebral osteomyelitis whose initial MRI (obtained <2 weeks after the onset of symptoms) did not reveal obvious findings of pyogenic vertebral osteomyelitis. However, follow‐up MRI clearly demonstrated typical findings of the disease. This case series illustrates that a repeat MRI must be performed 2‐4 weeks after the onset of symptoms in patients presenting with clinical manifestations and microbiological findings suggestive of vertebral osteomyelitis.
Keywords: diagnosis, infection, magnetic resonance imaging, osteomyelitis, vertebral osteomyelitis
1. INTRODUCTION
Vertebral osteomyelitis requires accurate diagnosis and long‐term treatment with appropriate antibiotics for at least 6 weeks as it causes spinal deformities, persisting pain, neurologic impairment, and even death. Magnetic resonance imaging (MRI) is more useful for the early diagnosis than other modalities. Here, we report three cases of vertebral osteomyelitis in patients whose MRI showed no abnormalities in the disks and vertebrae in the early phase of the disease.
2. CASE REPORTS
2.1. Case 1
A 77‐year‐old man with diabetes mellitus and a history of drug‐induced hypersensitivity syndrome on 30 mg/day oral prednisolone for 2 weeks was referred to our hospital because of low back pain and high fever (>39°C). Physical examination revealed tenderness on the lower lumbar spine. Blood test results revealed a leukocyte count of 8400/μL and C‐reactive protein level of 7.7 mg/dL. Methicillin‐resistant Staphylococcus aureus (MRSA) was isolated from multiple blood cultures (Table 1). A contrast‐enhanced abdominal computed tomography (CT) scan obtained on the third day after developing low back pain revealed low‐density areas, indicating the presence of abscess behind the right iliopsoas muscle. A noncontrast MRI of the lumbar spine was performed on the fifth day after the patient developed low back pain. However, no abnormalities were detected on short time inversion recovery (STIR) images (Figure 1A). Transthoracic echocardiogram showed no valvular vegetations. A repeat noncontrast MRI of the lumbar spine was performed 27 days after developing low back pain. STIR images showed high‐intensity lesions in the vertebral bodies of L5 and S1 (Figure 1B), and these findings led to the diagnosis of vertebral osteomyelitis.
Table 1.
Results of laboratory tests and cultures
| Variables | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| White blood cell counts (/μL) | 8400 | 10 500 | 5100 |
| Neutrophils (%) | 57.0 | 93.3 | 82.5 |
| Hemoglobin (g/dL) | 9.2 | 14.0 | 9.6 |
| ESR (mm/h) | NT | 17 | 82 |
| Creatinine (mg/dL) | 1.31 | 0.63 | 2.21 |
| CRP (mg/dL) | 7.76 | 5.39 | 13.33 |
| Glucose (mg/dL) | 262 | 149 | 119 |
| Hemoglobin A1c (%) | 7.9 | NT | 6.2 |
| Cultures | |||
| Blood | MRSA | Streptococcus pneumoniae | Negative |
| Urine | NT | Negative | Klebsiella pneumoniae |
| CT‐guided biopsy specimen | NT | NT | K. pneumoniae |
CRP, C‐reactive protein; CT, computed tomography; ESR, erythrocyte sedimentation rate; MRSA, methicillin‐resistant Staphylococcus aureus; NT, not tested.
Figure 1.
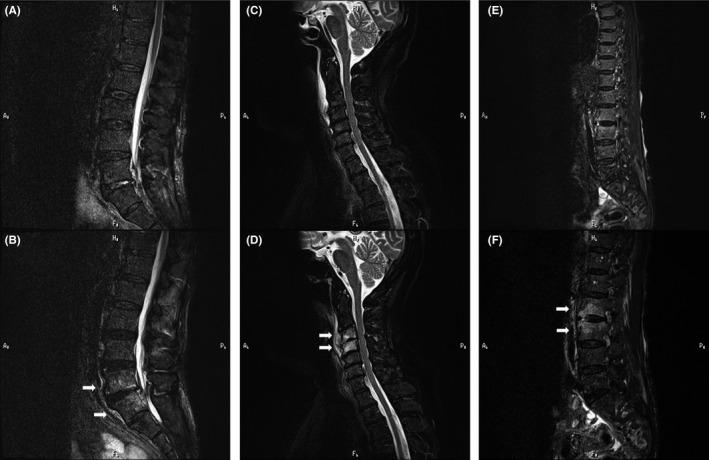
Initial magnetic resonance (short time inversion recovery) images obtained <2 wk after the onset of symptoms showed no obvious abnormalities: A, case 1; C, case 2; and E, case 3. Follow‐up magnetic resonance images performed 2‐4 wk after the onset of symptoms detected high‐intensity lesions in the vertebral bodies. Arrows indicate the lesion: B, case 1; D, case 2; and F, case 3
2.2. Case 2
A 74‐year‐old woman with no significant history or underlying diseases was admitted to our hospital because of newly developed neck pain in addition to preexisting hip pain. She had fever (>38°C) 2 days before her evaluation. Neck pain occurred on the day of admission. Hip pain persisted for 2 years and worsened a day before admission. Lateral rotation of her neck triggered severe neck pain. Neurologic examination revealed no abnormalities. The patient had never received pneumococcal vaccine. Blood test results are given in Table 1. Streptococcus pneumoniae was isolated from blood cultures; the serotype of this strain was not evaluated. Analysis of the cerebrospinal fluid (CSF) showed no abnormalities. Contrast‐enhanced CT scans of the neck, chest, abdomen, and pelvis revealed bone sclerosis of the left sacroiliac joint but no obvious abscess. A contrast‐enhanced MRI of the cervical spine performed the day after her admission showed enhanced fluid accumulations in the retropharyngeal and intervertebral space, although vertebral osteomyelitis was not detected on STIR images (Figure 1C). A repeat contrast‐enhanced CT scan was performed 11 days after the onset of symptoms and showed retropharyngeal abscess, left iliopsoas abscess, and right renal abscess. With follow‐up contrast‐enhanced MRI obtained 15 days after the onset of neck pain, a STIR image revealed high‐intensity lesions in the vertebral bodies of C3 and C4 (Figure 1D), suggestive of vertebral osteomyelitis. For this patient, we recommended pneumococcal vaccines following treatment of invasive pneumococcal disease.
2.3. Case 3
An 83‐year‐old woman was admitted because of exacerbation of low back pain and low‐grade fever. The patient's low back pain persisted for 2 years and worsened 13 days before admission. She had a history of cervical cancer that was treated with extended hysterectomy and radiotherapy 19 years before and had a long‐term urethral catheter for bladder atrophy caused by the radiotherapy. Furthermore, she had a history of pubic osteomyelitis due to Enterococcus faecalis and Staphylococcus epidermidis 2 years before, as well as lumbar spinal canal stenosis. Neurologic examination showed muscle weakness of the lower extremities. A noncontrast MRI of the thoracic and lumbar spine was performed on the day of admission, but besides degenerative spinal stenosis, no abnormalities were detected on STIR images (Figure 1E). Blood test results indicated an inflammatory process (Table 1). Blood cultures were negative. A repeat noncontrast MRI of the lumbar spine was performed 20 days after the exacerbation of low back pain, and STIR images revealed high‐intensity lesions in the vertebral bodies of L2 and L3 (Figure 1F), suggestive of vertebral osteomyelitis. She underwent CT‐guided biopsy of the involved vertebra and disk space. Klebsiella pneumoniae was identified in cultures of aspirated materials.
In these cases, we decided to repeat MRI based on the high clinical suspicion of vertebral osteomyelitis, which led to the correct diagnosis and treatment.
3. DISCUSSION
Adequate imaging examination is required for diagnosing vertebral osteomyelitis, and plain radiography, CT, and MRI are utilized in clinical situations. Because of its availability, plain radiography is generally the first step in evaluating back or neck pain. However, it takes weeks to months to detect typical findings of vertebral osteomyelitis, and plain radiography has low sensitivity and specificity for the diagnosis.1, 2 MRI is the most useful tool for the early diagnosis of vertebral osteomyelitis.3 MRI can detect abnormalities in the early phase of the disease,1, 2, 3, 4, 5 and its sensitivity, specificity, and accuracy are above 90%.1, 3 Initial MRI findings reveal bone marrow edema in the adjacent vertebral bodies and endplates, which can be detected as early as 48 hours after the onset of the disease.3 Typically, vertebral osteomyelitis shows low and high signal intensities on T1‐ and T2‐weighted images, respectively, in the vertebral body and intervertebral disk. Morrison et al6 reported that the sensitivity of MRI in diagnosing osteomyelitis increased from 79% using nonenhanced MRI to 88% using fat‐suppressed T1‐weighted contrast‐enhanced MRI. In addition, STIR is highly sensitive in detecting early inflammatory edema of bone structures.4 In our case series, MRI contrast agents could not be used in 2 of the 3 patients (patients 1 and 3) because of underlying chronic kidney disease. Thus, STIR sequences, which are commonly obtained without contrast, may be a useful diagnostic tool, especially for cases in which contrast agents cannot be used.
On rare occasions, however, abnormalities on MRI do not appear at the same time when clinical symptoms appear. In our three patients, no obvious abnormalities in the vertebra were detected by initial MRI (obtained <2 weeks after the onset of symptoms). Moreover, MRI in the early phase may tend to show nonspecific and nontypical findings of spinal infection.7, 8 In a previous case series of four patients with vertebral osteomyelitis/diskitis whose initial MRI did not suggest the disease, repeat MRI (mean time to repeat examination, 17 days; range, 8‐22 days) clearly showed typical features of osteomyelitis/diskitis.8 In a retrospective cohort study of 103 patients with pyogenic vertebral osteomyelitis, MRI findings of 93.2% of patients were suggestive of pyogenic vertebral osteomyelitis. MRI performed in the early periods of illness (<2 weeks) was associated with a less specific diagnosis.9 Based on the previous study8 and our case series, repeat MRI 2‐4 weeks after the onset of symptoms is suggested for cases with high clinical suspicion of vertebral osteomyelitis.
Vertebral osteomyelitis should be suspected in patients with new or worsening back or neck pain, especially those with fever, elevated erythrocyte sedimentation rate, bloodstream infection or infective endocarditis, new neurologic symptom, and recent episode of S. aureus bloodstream infection.10 In our series, the patients had new or worsening back or neck pain, high‐ or low‐grade fever, and inflammatory findings on blood tests. Vertebral osteomyelitis was detected on follow‐up MRI performed 2‐4 weeks after the onset of symptoms, which led to the definitive diagnosis.
It is important to understand that MRI in the early phase can occasionally fail to demonstrate findings of vertebral osteomyelitis, despite MRI having a high sensitivity for detecting bone lesions. In this study, a repeat MRI 2‐4 weeks after the onset of symptoms was recommended for patients with suspected vertebral osteomyelitis and microbiological findings, even if typical MRI findings were not observed in the early phase of the disease. Clinicians should pay attention to the exclusive diagnosis of vertebral osteomyelitis.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Kamiya N, Hatakeyama S, Kanda N, et al. Significance of repeat magnetic resonance imaging in diagnosing vertebral osteomyelitis. J Gen Fam Med. 2019;20:68–71. 10.1002/jgf2.226
REFERENCES
- 1. An HS, Seldomridge JA. Spinal infections. Clin Orthop Relat Res. 2006;444:27–33. [DOI] [PubMed] [Google Scholar]
- 2. Simpfendorfer CS. Radiologic approach to musculoskeletal infections. Infect Dis Clin North Am. 2017;31:299–324. [DOI] [PubMed] [Google Scholar]
- 3. Palestro CJ, Love C, Miller TT. Infection and musculoskeletal conditions: imaging of musculoskeletal infections. Best Pract Res Clin Rheumatol. 2006;20:1197–218. [DOI] [PubMed] [Google Scholar]
- 4. Jevtic V. Vertebral infections. Eur Radiol. 2004;14:E43–52. [DOI] [PubMed] [Google Scholar]
- 5. Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother. 2010;65:iii11–24. [DOI] [PubMed] [Google Scholar]
- 6. Morrison WB, Schweitzer ME, Bock GW, et al. Diagnosis of osteomyelitis: utility of fat‐suppressed contrast‐enhanced MR imaging. Radiology. 1993;189:251–7. [DOI] [PubMed] [Google Scholar]
- 7. McHenry MC, Easley KA, Locker GA. Vertebral osteomyelitis: long‐term outcome for 253 patients from 7 Cleveland‐area hospitals. Clin Infect Dis. 2002;34:1342–50. [DOI] [PubMed] [Google Scholar]
- 8. Dunbar JA, Sandoe JA, Rao AS, Crimmins DW, Baig W, Rankine JJ. The MRI appearances of early vertebral osteomyelitis and discitis. Clin Radiol. 2010;65:974–81. [DOI] [PubMed] [Google Scholar]
- 9. Carragee EJ. The clinical use of magnetic resonance imaging in pyogenic vertebral osteomyelitis. Spine (Phila Pa 1976). 1997;22:780–5. [DOI] [PubMed] [Google Scholar]
- 10. Berbari EF, Kanj SS, Kowalski TJ, et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults. Clin Infect Dis. 2015;61:e26–46. [DOI] [PubMed] [Google Scholar]


